Supplementary Appendix for the article
advertisement

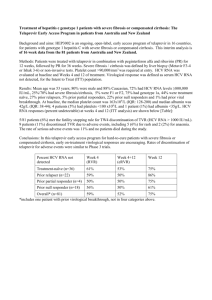
Supplementary Appendix for the article This material supplements but does not replace the content of the peer-reviewed paper published in AIDS. INTRODUCTION The analyses reported in the main manuscript utilize the Hepatitis C Cost-Effectiveness (HEP-CE) model of screening, care, and treatment for chronic (or acute) hepatitis C virus (HCV) infection. HEP-CE is a detailed micro-simulation of HCV epidemiology, screening, linkage to care, treatment, and outcomes. The HEP-CE model tracks clinical outcomes including number of detected HCV antibodies, number linked to HCV care, number of cases of chronic HCV identified, number of HCV-infected people initiating therapy, number achieving sustained viral response (SVR), HCV-related mortality, quality-of-life (QoL), undiscounted life expectancy, and discounted quality adjusted life expectancy (QALE). In addition, the model generates estimates of discounted, lifetime medical costs from the health system perspective. To incorporate outcomes and costs associated with HIV-infection, we used the CostEffectiveness of Preventing AIDS Complications (CEPAC) model, a computer simulation of the clinical management and economics of HIV infection, to provide estimates of mortality, costs and quality-of-life in a cohort of HIV-infected individualsreceiving U.S. guideline-concordant HIV care [1,2]. The CEPAC model generated estimates of HIV-related, as well as non-HIV/nonHCV related mortality (competing risk mortality), QoL, and medical costs in the simulated cohort of HIV-infected individuals. These estimates reflected the average experience of HIVinfected individuals without HCV infection. The HEP-CE model then used the CEPAC output as 1 model inputs and simulated HCV-related mortality, QoL, and costs.We used a standard multiplicative assumption to estimate utility functions for joint health states reflecting both HIV and HCV disease. CEPAC HIV disease model The CEPAC Model is a Monte Carlo simulation of the progression and outcomes of HIV disease in a hypotheticalcohort of patients. The model follows each individual’s clinical course from the time of entry into the model until death and keeps a running tally of clinical events, the length of time spent in each health state, costs, and QoL. Upon the patient’s death, summary statistics arerecorded and a new patient enters the model. This process is repeated over a largenumber of patients (statistical convergence can typically be achieved with cohort sizes of2 to 5 million), at which point overall performance measures such as average projected lifeexpectancy, quality-adjusted life expectancy, and cost are computed. The CEPAC model definesthree general categories of health states: chronic HIVinfection, acute AIDS-related events, and death. Patients generally reside in the chronic HIVinfection health state. In the absence of antiretroviral therapy (ART),HIV disease progresses, with characteristic immunesystem deterioration (CD4 count decline). The model treats HIV RNA as the primarydriver of immune system deterioration, with current RNA leveldeterminingthe rate of CD4 decline. Incidence of AIDS-related events is a function of CD4 count and prior AIDS-related events. Patients who develop an acute AIDS-related complication temporarily move to an acute healthstate, where quality-of-life is lower and both resource consumption and mortalityare 2 higher. Deaths mayoccur while in a chronic or an acute state and can beattributed to a particular opportunistic infection (OI), chronic AIDS, or non-AIDS-related causes. The model includes 6 lines of ART modeling efficacy as the probability of achieving an HIV RNA less than the level of detection typically by week 24 of therapy (Supplemental Table 1). With suppressed HIV RNA, CD4 count rises as a function of time on ART, with an initial rapid rise, followed by two periods of progressively slower CD4 count change. Individuals on suppressive ART face a monthly risk of experiencing virologic breakthrough related to poor adherence. With rising HIV RNA, CD4 rapidly falls to the individual’s CD4 count nadir prior to initiating therapy. The model distinguishes between the “true” time of virologic failure, and the time that such failure is clinically identified. With two successive office visits documenting elevated HIV RNA, the individual is advanced to the next line of ART. Input data for the CEPACmodel are from published reports and public use datasets. Model inputs have been described and published previously [1,3]. We used the CEPAC model to project life expectancy, quality of life, and medical costs in a cohort of HIV-infected individuals with demographic characteristics matching those of the cohort we planned to model for the cost-effectiveness analysis of HCV therapy (same mean age, sex distribution, prevalence of injection drug use). CEPAC simulated the lifetime of each cohort member, and provided output tables, stratified by sex and simulation month. For example, the first table was a “lifetable” that provided the monthly probability of death from HIV-attributable, as well as non-HIV and non-HCV related causes, conditional on being alive at the beginning of the simulation month, stratified by sex and time in the simulation. This CEPAC output table became an input table for the HEP-CE model, informing the monthly probability of death from causes other than HCV. Similarly, CEPAC generated a table of the cohort’s average medical cost 3 in each simulation month, stratified by sex. HEP-CE used this “cost table” to inform non-HCV related costs in every month. Finally, CEPAC generated a table of the cohort’s average quality of life in every simulation month, again stratified by sex. HEP-CE used this “quality of life table” to look up the cohort’s quality of life in each month, to which HEP-CE then applied utility weights related to HCV infection. HEP-CEMODEL The HEP-CE model is a Monte Carlo simulation of HCV infection designed to estimate the outcomes and costs associated with various strategies of screening, treatment, and improving HCV care. The model includes 5 components: 1) HCV epidemiology, 2) HCV screening and linkage to care, 3) HCV disease progression, 4) HCV therapy, and 5) Non-HCV mortality (Supplemental Figure 1). HCV epidemiology The incidence of HCV is a model input. In each monthly cycle, individuals in the model who are not HCV-infected face a risk of acquiring HCV that is a function of their age and HCV risk behaviors (typically interpreted as current injection drug use versus no current use). Once HCV-infected, individuals begin the simulation of HCV disease progression (see below). For the purpose of this analysis, which simulates the progression of a group of chronically HIV/HCV coinfected individuals, all individuals were HCV-infected at the start of the simulation. HCV disease progression 4 Chronic HCV is characterized in the model by 3 linear stages of fibrosis progression: mild-to-moderate fibrosis, cirrhosis, and decompensated cirrhosis. At all stages of fibrosis, HCVinfection is associated with increased costs and decreased QoL. Mortality attributable to HCV infection does not occur until an individual reaches his/her unique time of developing cirrhosis. Once an individual reaches the cirrhosis stage, (s)he faces a probability of liver-related mortality that remains constant unless s(he) initiates treatment and attains SVR. To estimate critical disease progression event times, including the time at which an individual develops cirrhosis (tcirrhosis) and decompensated cirrhosis (tdecomp), the model uses a stochastic process to draw 4 critical parameter values: 1) ageat HCV infection (AgeHCV); 2) age at simulation base line (Agebase); 3) months from infection to cirrhosis (mcirrhosis); and 4) months from cirrhosis to first liver decompensation event (mdecomp). For those with prevalent HCV infection at simulation baseline: tcirrhosis = mcirrhosis – (Agebase - AgeHCV) tdecomp = tcirrhosis + mdecomp For those who contract incident HCV during the simulation: tcirrhosis = mcirrhosis tdecomp = tcirrhosis + mdecomp As a result of the stochastic process that defines time to cirrhosis and decompensation, not all HCV-infected patients in the model develop cirrhosis, and not all patients with cirrhosis die of HCV-attributable causes. 5 With spontaneous clearance or successful HCV treatment, disease progression ceases, and QoL, costs, and mortality risk return to that of HCV-uninfected individuals of the same age, sex, and HCV risk behaviors. Re-infected individuals resume the course of fibrosis progression at the stage reached during prior infection. HCV screening and linkage to care The model distinguishes between an individual’s true infection status and clinical awareness of infection. Only individuals with identified HCV infection are eligible for HCV therapy. The model provides flexibility to define various strategies for screening based on different screening modalities and intervals. All screening tests are characterized by a cost, sensitivity, and specificity. Test characteristics are a function of time since infection. The analysis of HCV therapy in HIV/HCV co-infection did not utilize the HCV screening features of the model as this cohort has already been identified as chronically infected with HCV. HCV Therapy The model provides flexibility to simulate a variety of algorithms for HCV therapy, including distinct treatment protocols for acute and chronic HCV infection, as well as for genotype 1 vs. genotype 2/3 infection. Treatment efficacy is modeled using 6 key parameters, each of which is stratified by cirrhosis status: 1. Probability of developing HCV RNA >1,000 copies/ml = Pfail 2. Probability of attaining HCV RNA < assay at treatment week W4 = Prvr 6 3. Probability of attaining HCV RNA < assay at treatment week W12 = Pervr 4. Probability of attaining HCV RNA< assay 24 weeks after therapy end = P SVR 5. Probability of withdrawing from therapy for any cause = Pwithdraw 6. Proportion of all therapy withdraws that are attributable to major treatment toxicity = Ptox The user can define an algorithmic response to events such as virologic failure, attaining both 4 and 12 week HCV RNA < assay (extended rapid virologic response), or having HCV RNA detectable, but less than 1,000 copies/ml. For example, when modeling response guided therapy using peginterferon, ribavirin, and an HCV protease inhibitor, having an HCV RNA > 1,000 copies/ml leads to treatment cessation, having detectable HCV RNA that is <1,000 copies/ml at either treatment week 4 or 12 leads to the course of therapy being extended from 24 to 48 weeks. Having undetectable HCV RNA at both weeks 4 and 12 leads to a 24-week total treatment course. In every month that a simulated individual is taking HCV therapy, (s)he accrues costs associated with physician visits, as well as the cost of HCV medications and additional medications used to manage non-treatment ending toxicities such as mild to moderate anemia, neutropenia, and rash (Supplemental Table 2). The approach to modeling non-treatment ending toxicity is to determine the cost of managing a given complication, as well as an estimate of the proportion of patients in a given month who have a specific non-treatment ending toxicity type. The “average” cost of HCV therapy is taken as the sum of all antiviral medications, plus the weighted average of non-treatment ending toxicity costs, using the proportion of each toxicity type in the cohort as the weight. 7 In every month while on HCV treatment, individuals face a probability of withdraw for toxicity, inability to tolerate adverse effects of interferon, or non-adherence. Among those who withdraw for any reason, the model determines whether that withdraw from therapy was the result of treatment-ending toxicity. Those who experience treatment-ending toxicity have a onemonth decrement in quality of life related to the toxicity, as well as a one-time cost associated with managing the toxicity (Supplemental Table 3). Individuals who stop treatment due to toxicity accrue a cost that reflects the cost of an “average” toxicity event. This cost is calculated by identifying the most common toxicity event types, estimating the cost of managing each type of toxicity event, and taking the weighted average cost of all toxicity event types using the proportion of toxicity events attributable to each toxicity type as the weight. Non-HCV morbidity and mortality In addition to the HCV-attributable causes of death, in every month individuals in the model are exposed to risk of death from causes other than HCV, as well as costs associated with non-HCV related healthcare. Competing risk mortality is stratified by age and sex, and is informed by U.S. vital statistics data [4]. Competing risk mortality is adjusted using standardized mortality ratios, to reflect elevated competing risks of death in persons with a history of HCV risk-behaviors such as IDU [5]. Costs 8 The model generates estimates of discounted, lifetime medical costs from the health system perspective. Component costs include those of HCV-related physician and nursing visits, HCV medications, medications used for management of treatment toxicity, and the cost of additional medical visits and hospitalizations associated with HCV-infection. Costs include estimates of age and sex stratified “background” costs, which reflect healthcare utilization unrelated to HCV. Quality of life Quality of life in HEP-CE is a function of HCV fibrosis stage. To simulate HIV/HCV coinfection for this analysis, the HEP-CE model integrated quality of life functions for both HIV and HCV-infections. The CEPAC model provided an actuarial table of the mean QoL of the cohort in each simulation month. HEP-CE combined the CEPAC estimated of average HIVassociated QoL, with HCV health state-specific estimates of QoL, using a multiplicative assumption[6-10]. 9 Supplemental Table 1. HIV drug costs and efficacies Regimen Base case Range Reference(s) Efficacy 86.0%, 73.1%-98.9% [11] Monthly cost $1,500 $800-$2,300 [12] Efficacy 73.3%, 62.3%-84.3% [13] Monthly cost $2,100 $1,100-$3,200 [12] Efficacy 61.3%, 52.1%-70.5% [13] Monthly cost $2,000 $1,000-$3,000 [12] Efficacy 64.5%, 54.8%-74.2% [14] Monthly cost $2,800 $1,400-$4,300 [12] Efficacy 40.0% 34.0%-46.0% [15,16] Monthly cost $4,800 $2,400-$7,200 [12] First line Second line Third line Fourth line Fifth line 10 Regimen Base case Range Reference(s) Efficacy 15.0% 12.8%-17.3% [15] Monthly cost $1,900 $1,000-$2,900 [12] Sixth line 11 000251659264251660288251661312251662336Supplemental Figure 1. HEP-CE model flow diagram Individual enters HEP-CE model Random numbers assign unique values for: Age Sex HCV genotype Age of infection Time to cirrhosis Time from cirrhosis to first decompensation event No Does the individual complete therapy? HCV disease progression No chance for future therapy Chance of death from competing mortality Yes No Does the individual achieve SVR? Yes HCV uninfected Chance of death from competing mortality 12 Supplemental Table 2. HCV therapy costs (2011 US $) Drug Standard dose Frequency Cost per month Reference(s) Standard HCV treatment a,b 1200 mg 1/day $1,371 [17,18] Anemia (dose reduction) c 600 mg 1/day $685 [17] Standard HCV treatment d 180 mcg/ml 1/week $2,097 [17,18] Neutropenia (dose reduction) 135 mcg/ml 1/week $1,572 [17] 750 mg 3/day $15,154 [18] 300 mcg/ml 2/week $1,900 [17], Expert opinion 150 g 1/month $160 [17,18], Expert opinion Ribavirin Peginterferon alfa-2a Telaprevir Standard HCV treatment e Filgrastim Neutropeniad Clobetasol propionate Rash f 13 Note: the monthly cost estimate is based on the average wholesale price[12], less 23%[19], assuming a standard dosage and number of pills for 1 month.12.0%[20] incur an additional cost of 19.75[21]for a nurse visit to treat adverse event. a 18.0% receive ribavirin dose reduction to 600 mg/day to treat anemia (months 1-3 only) b 8.5% receive ribavirin dose reduction to 600 mg/day to treat anemia (months 4-12 only) c 8.5% receive ribavirin dose reduction to 600 mg/day to treat anemia (all months) d 6.5% receive peginterferon alfa-2a dose reduction from 180 to 135 mcg/ml to treat neutropeniaand 300 mg of filgastrim twice per week (all months) e For those on triple therapy(months 1-3 only) f 28.0%receive 150 g of 0.05% clobetasolpropionate to treat rash (months 1-3 only) 14 Supplemental Table 3.Costs of treatment ending toxicity events (2011 US $) Resource utilized CPT code Unit cost # Utilized Total cost Source(s) Anemia Epoteinalfa N/A 485.10 1 485.10 [12,22], Expert opinion Complete blood count 85025 10.94 3 32.82 [22,23], Expert opinion Bilirubin 82247 7.06 1 7.06 [22,23], Expert opinion Uric acid 84550 6.36 1 6.36 [22,23], Expert opinion Reticulocytes 85045 5.63 3 16.89 [22,23], Expert opinion Transfusion 96365 54.37 1 54.37 [22,23], Expert opinion Packed red blood cells P9021 231.50 2 463.00 [22,24], Expert opinion Clinic visit and injection 99211 19.74 2 39.48 [21,22], Expert opinion Moderately complex clinic visit 99214 104.16 2 208.32 [21,22], Expert opinion Proportion with anemia (dual therapy) __ __ __ 0.176 [25] Proportion with anemia (triple therapy) __ __ __ 0.097 [20] Total cost of anemia __ __ __ $1,313.40 Rash 15 Resource utilized Clobetasol propionate cream (30g) CPT code Unit cost # Utilized Total cost Source(s) N/A 35.86 1 35.86 [12,22], Expert opinion Simple clinic visit 99213 70.46 2 140.92 [21,22], Expert opinion Dermatology consultation 99243 119.81 1 119.81 [21,22], Expert opinion Proportion with rash (dual therapy) __ __ __ 0 [25] Proportion with rash (triple therapy) __ __ __ 0.387 [20] Total cost of rash __ __ __ $296.59 Moderately complex clinic visit 99214 104.16 2 208.32 [21], Expert opinion Complete blood count 85025 10.94 1 10.94 [23], Expert opinion Liver function test 80069 12.22 1 12.22 [23], Expert opinion Other SAE Proportion with other SAE (dual therapy) __ __ __ 0.824 [20,25] Proportion with other SAE (triple therapy) __ __ __ 0.516 [20] Total cost of other SAE __ __ __ $231.48 16 Resource utilized CPT code Unit cost # Utilized Total cost Total cost of treatment endingtoxicity for dual therapya $421.90 Total cost of treatment endingtoxicity for triple therapya $361.36 Source(s) CPT = current procedural terminology; SAE= Serious Adverse Event a Total costs equal weighted average of toxicity costs: (Proportion with anemia*total cost of treating anemia+ proportion with rash*total cost of treating rash + proportion with other SAE * total cost of treating other SAE) 17 Supplemental Table 4. Incremental cost-effectiveness ratios of projected cost-containing strategies utilizing IFN-free treatment Strategy % Attaining SVR Undiscounted Life Expectancy Discounted Cost ($) QALY Incremental Cost ($) QALY CER ($/QALY) No treatment 0 13.240 198,700 6.760 --- --- --- Dual therapy 30.8 13.761 221,900 7.599 23,200 0.839 27,700 PEG/RBV trial* 88.7 14.728 306,500 9.233 84,600 1.634 51,800 IL28B triage* 89.6 14.737 312,800 9.284 6,300 0.051 123,700 IFN-free therapy 90.3 14.745 325,300 9.323 12,500 0.039 322,200 HIV: human immunodeficiency virus; HCV: hepatitis Cvirus; IFN: interferon; QALY: quality-adjusted life year; CER: cost-effectiveness ratio; PEG/RBV: Peginterferon and Ribavirin; IL28B: interleukin-28B Note: all costs and QALYs are lifetime and discounted at an annual rate of 3%. Costs are in 2011 US dollars and rounded to the nearest $100. All life-years and QALYs are rounded to the nearest thousandth *These strategies utilize PEG/RBV and IFN-free therapy instead of PEG/RBV/TVR in the base case 18 REFERENCES 1. Freedberg KA, Losina E, Weinstein MC, Paltiel AD, Cohen CJ, Seage GR, et al. The cost effectiveness of combination antiretroviral therapy for HIV disease. N Engl J Med 2001,344:824-831. 2. Paltiel AD, Weinstein MC, Kimmel AD, Seage GR, 3rd, Losina E, Zhang H, et al. Expanded screening for HIV in the United States--an analysis of cost-effectiveness. N Engl J Med 2005,352:586-595. 3. Paltiel AD, Walensky RP, Schackman BR, Seage GR, 3rd, Mercincavage LM, Weinstein MC, et al. Expanded HIV screening in the United States: effect on clinical outcomes, HIV transmission, and costs. Ann Intern Med 2006,145:797-806. 4. Centers for Disease Control and Prevention. United States Life Tables, from: http://www.cdc.gov/nchs/products/life_tables.htm. 2008. 5. Arendt M, Munk-Jorgensen P, Sher L, Jensen SO. Mortality among individuals with cannabis, cocaine, amphetamine, MDMA, and opioid use disorders: a nationwide followup study of Danish substance users in treatment. Drug Alcohol Depend 2011,114:134139. 6. Chong CA, Gulamhussein A, Heathcote EJ, Lilly L, Sherman M, Naglie G, et al. Healthstate utilities and quality of life in hepatitis C patients. Am J Gastroenterol 2003,98:630638. 7. Grieve R, Roberts J, Wright M, Sweeting M, DeAngelis D, Rosenberg W, et al. Cost effectiveness of interferon alpha or peginterferon alpha with ribavirin for histologically mild chronic hepatitis C. Gut 2006,55:1332-1338. 19 8. Paltiel AD, Scharfstein JA, Seage GR, 3rd, Losina E, Goldie SJ, Weinstein MC, et al. A Monte Carlo simulation of advanced HIV disease: application to prevention of CMV infection. Med Decis Making 1998,18:S93-105. 9. Schackman BR, Goldie SJ, Freedberg KA, Losina E, Brazier J, Weinstein MC. Comparison of health state utilities using community and patient preference weights derived from a survey of patients with HIV/AIDS. Med Decis Making 2002,22:27-38. 10. Stein K, Dalziel K, Walker A, McIntyre L, Jenkins B, Horne J, et al. Screening for hepatitis C among injecting drug users and in genitourinary medicine clinics: systematic reviews of effectiveness, modelling study and national survey of current practice. Health Technol Assess 2002,6:1-122. 11. Gallant JE, DeJesus E, Arribas JR, Pozniak AL, Gazzard B, Campo RE, et al. Tenofovir DF, emtricitabine, and efavirenz vs. zidovudine, lamivudine, and efavirenz for HIV. N Engl J Med 2006,354:251-260. 12. Micromedex 2.0. Drug Topics Red Book Online. Accessed Feburary 1st, 2013. from: http://www.micromedexsolutions.com. 13. Johnson M, Grinsztejn B, Rodriguez C, Coco J, DeJesus E, Lazzarin A, et al. Atazanavir plus ritonavir or saquinavir, and lopinavir/ritonavir in patients experiencing multiple virological failures. AIDS 2005,19:685-694. 14. Grinsztejn B, Nguyen B, Katlama C, Gatell J, Lazzarin A, Vittecog D, et al. Safety and efficacy of the HIV-1 integrase inhibitor raltegravir (MK-0518) in treatment-experienced patients with multidrug-resistant virus: a phase II randomised controlled trial. Lancet 2007,369:1261-1269. 20 15. Nelson M, Arasteh K, Clotet B, Cooper DA, Henry K, Katlama C, et al. Durable Efficacy of Enfuvirtide Over 48 Weeks in Heavily Treatment-Experienced HIV-1–Infected Patients in the T-20 Versus Optimized Background Regimen Only 1 and 2 Clinical Trials. JAIDS 2005,40:404-412. 16. Lalezeri J, Goodrich J, De Jesus E, Lampiris H, Gulick R, Saag M. Efficacy and safety of maraviroc plus optimized background therapy in viremic ART experienced patients infected with CCR5-tropic HIV-1: 24-week results of a phase 2b/3 study in the US and Canada. 17. Physician's Desk Reference. from: http://www.pdr.net. 2011. 18. Food and Drug Administration. Telaprevir package insert. from: http://www.fda.gov. 2012. 19. Levinson D. Medicaid drug price comparisons: Average manufacturer price to published prices; Department of Health and Human Services. from: http://www.oig.hhs.gov/oei/reports/oei-05-05-00240.pdf. 2005. 20. McHutchison JG, Lawitz EJ, Shiffman ML, Muir AJ, Galler GW, McCone J, et al. Peginterferon alfa-2b or alfa-2a with ribavirin for treatment of hepatitis C infection. N Engl J Med 2009,361:580-593. 21. United States Department of Health and Human Services Center for Medicare Services. Physician Fee Schedule. Accessed January 15th, 2013. from: http://www.cms.gov/Medicare/Medicare-Fee-for-ServicePayment/PhysicianFeeSched/index.html?redirect=/PhysicianFeeSched. 2011. 22. Gao B. Interaction of alcohol and hepatitis viral proteins: implication in synergistic effect of alcohol drinking and viral hepatitis on liver injury. Alcohol 2002,27:69-72. 21 23. United States Department of Health and Human Services Center for Medicare Services. Clinical Diagnostic Laboratory Fee Schedule. Accessed February 1st, 2013. From: http://www.cms.gov/ClinicalLabFeesched/02_clinlab.asp. 2011. 24. Whitaker B, Sullivan M. The 2005 Nationwide Blood Collection and Utilization Survey Report. 25. Torriani FJ, Rodriguez-Torres M, Rockstroh JK, Lissen E, Gonzalez-Garcia J, Lazzarin A, et al. Peginterferon Alfa-2a plus ribavirin for chronic hepatitis C virus infection in HIV-infected patients. N Engl J Med 2004,351:438-450. 22