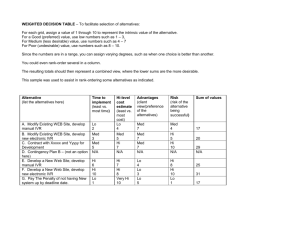
Annotated Bibliography of relevant literature []
advertisement
![Annotated Bibliography of relevant literature []](http://s3.studylib.net/store/data/008947629_1-69d08999efea1afb610ef4f7ef9dd831-768x994.png)
Regional Framework Annotated Bibliography 2008 The report “It Takes A Region: Creating a Framework to Improve Chronic Disease Care” found on this DVD describes the evidence that supported the development of the Regional Framework in 2005. Since that time, new work has been published in the peer-reviewed literature and elsewhere that helps better illuminate some of the elements of Framework. The following annotated bibliography updates the evidence on the most controversial elements of the Framework or areas where the literature was most sparse in 2005. Leadership The elements that this bibliography covers are: Collaboration among Stakeholders Shared Data & Performance Measurement Engaging Consumers: Public Disclosure Improving Healthcare Delivery: Information Technology Improving Healthcare Delivery: Provider Networks Aligning Benefits/ Financing A robust summary of the evidence base for consumer education and quality improvement strategies including consensus guidelines and care management is provided on our first DVD, and therefore is not included here. Admittedly the data are still sparse on many of the elements covered below. As Regional Collaborations continue to grow and mature, so too will our understanding of how these ideas work in practice. Methods We undertook the literature review for this bibliography in two parts. First, we updated the search that was conducted as part of “It Takes A Region: Creating a Framework to Improve Chronic Disease Care” by using the following search criteria in Pub Med. Limits: English, humans, clinical trial, meta-analysis, RCT, review articles, 2005-2007 Search Terms: “Regional Health Planning” [MeSH] : 168 articles, title search 32 “Community networks” [MeSH]: 43 articles, title search 13, abstract search below “Community Coalitions” : 9 articles, title search 7, abstract search below “Diffusion of Innovation”: 157 articles, title search 37, abstract search below Then we conducted a full literature review on those particular elements of the Framework that were most relevant to current policy discussions. Articles in this bibliography are empirical studies + , dated 2000 to 2007, published in English, focused on humans, indexed in PubMed or part of the Cochrane Collaboration. High impact articles are briefly summarized and bolded Framework Limits Search Terms & Results Element Shared Data Key words - “performance measurement” 93 articles, title & Humans, English, Randomized search 13 Performance Control Trial, Clinical Trial, measurement Review, Meta-analysis, 2000-2007 Related Articles - Kupersmith J, Francis J, Kern E, et al. Humans, English, 2000 – 2007 "Advancing Evidence-Based Care for Diabetes” 79 articles, title search 32 - Weis KB, Wagner R. “Performance Measurement through Audit, Feedback and profiling as tools for improving clinical care” 89 articles, title search 34 Information Technology Key Words Humans, English, 2000- 2007 - Provider Networks Key Words Humans, English, 2000-2007 - Public Disclosure Key Words Humans, English, Randomized Control Trial, Clinical Trial, Review, Meta-analysis, 2005- 2007. Related Articles Humans, English 2000 – 2007 - Key Words Humans, English, Randomized Control Trial, Clinical Trial, Review, Meta-analysis, 2005- 2007. - Aligning Benefits/ Financing - - “RHIO” 29 articles, title search 20 “Regional Health Informatics” 118 articles, title search 4 “PBRN” 29 articles, title search 23 “Primary Care Case Management” 40 articles, title search 17 “Public Disclosure” 11 articles, title search 1 Hamblin, R. “Publishing ‘quality’ measures, how it works and when it does not?” 85 articles, title search 55 “pay for performance” 60 articles, title search 31 “financial incentive” 199 articles, title search 44 Collaboration among Stakeholders 1. Fleming B, Silver A, Ocepek-Welikson K, Keller D. The relationship between organizational systems and clinical quality in diabetes care. Am J Manag Care 2004; 10(12):934-44. In this cross-sectional study, the authors found that greater use of systems interventions, such as use of clinicalguideline software, was related to higher quality diabetes care in Medicare managed care organizations. 2. Shortell SM, Zukoski AP, Alexander JA et al. Evaluating partnerships for community health improvement: tracking the footprints. J Health Polit Policy Law 2002; 27(1):49-91. In this evaluation of the Community Care Network Demonstration program, the authors emphasize that a shared, explicit vision of what is to be accomplished and a capable management model that focuses on the challenges of a multi-stakeholder collaborative are predictive of successful coalitions. 3. Reduction in central line-associated bloodstream infections among patients in intensive care units--Pennsylvania, April 2001-March 2005. MMWR Morb Mortal Wkly Rep 2005; 54(40):1013-6. 4. Blancquaert I. Managing partnerships and impact on decision-making: the example of health technology assessment in genetics. Community Genet 2006; 9(1):27-33. 5. Cohen D, McDaniel RR Jr, Crabtree BF et al. A practice change model for quality improvement in primary care practice. J Healthc Manag 2004; 49(3):155-68; discussion 169-70. 6. Cohen L, Baer N, Satterwhite P. Developing effective coalitions: An eight step guide. Wurzbach ME (ed). Community Health Education & Promotion: A Guide to Program Design and Evaluation. 2nd edition. Gathersburg, MD: Aspen Publishers Inc., 2002. 7. Conrad DA, Cave SH, Lucas M et al. Community care networks: linking vision to outcomes for community health improvement. Med Care Res Rev 2003; 60(4 Suppl):95-129. 8. Demakis JG, McQueen L, Kizer KW, Feussner JR. Quality Enhancement Research Initiative (QUERI): A collaboration between research and clinical practice. Med Care 2000; 38(6 Suppl 1):I17-25. 9. Farley DO, Haims MC, Keyser DJ, Olmsted SS, Curry SV, Sorbero M. Regional health quality improvement coalitions. Lessons across the life cycle. Rand Report. RAND, 2003. 10. Ford EW, Wells R, Bailey B. Sustainable network advantages: a game theoretic approach to community-based health care coalitions. Health Care Manage Rev 2004; 29(2 ):159-69. 11. Geubbels EL, Nagelkerke NJ, Mintjes-De Groot AJ, Vandenbroucke-Grauls CM, Grobbee DE, De Boer AS. Reduced risk of surgical site infections through surveillance in a network. Int J Qual Health Care 2006; 18(2):12733. 12. Halamka J, Aranow M, Ascenzo C et al. Healthcare IT Collaboration in Massachusetts: The Experience of Creating Regional Connectivity. J Am Med Inform Assoc 2005. 13. Hayward RA, Hofer TP, Kerr EA, Krein SL. Quality improvement initiatives: issues in moving from diabetes guidelines to policy. Diabetes Care 2004; 27 Suppl 2:B54-60. 14. Health Research and Educational Trust. Public-Private Partnerships to Improve Health Care. Balancing short term successes with long term plans. 15. Institute of Medicine, Committee on the Crossing the Quality Chasm: Next Steps Toward a New Health Care System. The 1st annual crossing the quality chasm summit: A focus on communities. Washington, DC: National Academies Press, 2004. 16. Kizer KW, Demakis JG, Feussner JR. Reinventing VA health care: systematizing quality improvement and quality innovation. Med Care 2000; 38(6 Suppl 1):I7-16. 17. Mays GP, Halverson PK, Kaluzny AD. Collaboration to improve community health: trends and alternative models. Jt Comm J Qual Improv 1998; 24(10):518-40. 18. Provan KG, Nakama L, Veazie MA, Teufel-Shone NI, Huddleston C. Building community capacity around chronic disease services through a collaborative interorganizational network. Health Educ Behav 2003; 30(6):64662. 19. Valente TW, Chou CP, Pentz MA. Community coalitions as a system: effects of network change on adoption of evidence-based substance abuse prevention. Am J Public Health 2007; 97(5):880-6. 20. Wagner EH, Wickizer TM, Cheadle A et al. The Kaiser Family Foundation Community Health Promotion Grants Program: findings from an outcome evaluation. Health Serv Res 2000; 35(3):561-89. 21. Wickizer TM, Wagner E, Cheadle A et al. Implementation of the Henry J. Kaiser Family Foundation's Community Health Promotion Grant Program: a process evaluation. Milbank Q 1998; 76(1):121-47. 22. Zakocs RC, Edwards EM. What explains community coalition effectiveness?: a review of the literature. Am J Prev Med 2006; 30(4):351-61. 23. Zakocs RC, Guckenburg S. What coalition factors foster community capacity? Lessons learned from the Fighting Back Initiative. Health Educ Behav 2007; 34(2):354-75. Shared Data and Performance Measurement 24. Asch SM, McGlynn EA, Hogan MM et al. Comparison of quality of care for patients in the Veterans Health Administration and patients in a national sample. Ann Intern Med 2004; 141(12):938-45. Compared to a national sample, the Veterans Health Administration performed better on measures of quality in chronic disease and preventive care, especially in areas where the VHA targeted improvement through the use of performance measurement and active monitoring. 25. Jamtvedt G, Young JM, Kristoffersen DT, O'Brien MA, Oxman AD. Audit and feedback: effects on professional practice and health care outcomes. Cochrane Database Syst Rev 2006; (2):CD000259. In this Cochrane meta-analysis, 118 articles about audit and feedback techniques were reviewed. The authors found that audit and feedback techniques were effective for quality improvement, especially when baseline performance was low and feedback was intensively delivered. 26. Kerr EA, Smith DM, Hogan MM et al. Comparing clinical automated, medical record, and hybrid data sources for diabetes quality measures. Jt Comm J Qual Improv 2002; 28(10):555-65. Data from medial records and clinical automated data were compared for 1,032 patients with diabetes from the VHA. Agreement between the electronic registry and the medical records was high, though the electronic registry tended to underestimate success in diabetes process measures. 27. Kiefe CI, Allison JJ, Williams OD, Person SD, Weaver MT, Weissman NW. Improving quality improvement using achievable benchmarks for physician feedback: a randomized controlled trial. JAMA 2001; 285(22):2871-9. For community physicians participating in the Ambulatory Care Quality Improvement Project in Alabama, incorporating feedback on achievable benchmarks enhanced the effectiveness of a multimodal quality improvement intervention that included chart review and physician feedback. 28. Reed M, Devers K, Landon B. Physicians and care management: more acceptance than you think. Issue Brief Cent Stud Health Syst Change 2003; (60):1-4. More than half of physicians affected by care management tools like practice guidelines, practice profiling, and patient satisfaction surveys, have a favorable view of how these tools have effected the quality of care delivered in their practices. Physicians are more likely to view these tools as positive when the results are risk-adjusted. 29. Veloski J, Boex JR, Grasberger MJ, Evans A, Wolfson DB. Systematic review of the literature on assessment, feedback and physicians' clinical performance: BEME Guide No. 7. Med Teach 2006; 28(2):117-28. Authors of this literature review find that feedback to physicians is effective in improving health outcomes. Characteristics associated with a greater likelihood of improvement include: feedback provided by a credible source over a longer period of time, physician’s active involvement in the process, timing of feedback, and reminder systems and incentives. 30. Measuring physician performance: enhancing quality of care, reducing costs. Am J Manag Care 2003; Suppl Decison Maker News:1-4. 31. Ayanian JZ, Quinn TJ. Quality of care for coronary heart disease in two countries. Health Aff (Millwood) 2001; 20(3):55-67. 32. Bratzler DW, Nsa W, Houck PM. Performance measures for pneumonia: are they valuable, and are process measures adequate? Curr Opin Infect Dis 2007; 20(2):182-9. 33. Chaillet N, Dube E, Dugas M et al. Evidence-based strategies for implementing guidelines in obstetrics: a systematic review. Obstet Gynecol 2006; 108(5):1234-45. 34. Clauser SB. Use of cancer performance measures in population health: a macro-level perspective. J Natl Cancer Inst Monogr 2004; (33):142-54. 35. Committee on Redesigning Health Insurance Performance Measures PaPIPBoHCS, Institute of Medicine. Performance Measurement: Accelerating Improvement. National Academies Press , 2006. 36. Damberg C, Grazier K, Greenfield S et al. Advancing physician performance measurement using administrative data to assess physician quality and efficiency. San Francisco: Pacific Business Group on Health/Lumetra, 2005. 37. Doebbeling BN, Vaughn TE, Woolson RF et al. Benchmarking Veterans Affairs Medical Centers in the delivery of preventive health services: comparison of methods. Med Care 2002; 40(6):540-54. 38. Ellis J, Cooper A, Davies D et al. Making a difference to practice: clinical benchmarking. Part 2. Nurs Stand 2000; 14(33):32-5. 39. File TM Jr, Gross PA. Performance measurement in community-acquired pneumonia: consequences intended and unintended. Clin Infect Dis 2007; 44(7):942-4. 40. Gagliardi AR, Simunovic M, Langer B, Stern H, Brown AD. Development of quality indicators for colorectal cancer surgery, using a 3-step modified Delphi approach. Can J Surg 2005; 48(6):441-52. 41. Goddard M, Davies HT, Dawson D, Mannion R, McInnes F. Clinical performance measurement: part 1--getting the best out of it. J R Soc Med 2002; 95(10):508-10. 42. Goddard M, Davies HT, Dawson D, Mannion R, McInnes F. Clinical performance measurement: part 2--avoiding the pitfalls. J R Soc Med 2002; 95(11):549-51. 43. Goulet JL, Erdos J, Kancir S et al. Measuring performance directly using the veterans health administration electronic medical record: a comparison with external peer review. Med Care 2007; 45(1):73-9. 44. Heffner JE. Altering physician behavior to improve clinical performance. Top Health Inf Manage 2001; 22(2):1-9. 45. Hersh WR. Adding value to the electronic health record through secondary use of data for quality assurance, research, and surveillance. Am J Manag Care 2007; 13(6 Part 1):277-8. 46. Hofer TP, Hayward RA, Greenfield S, Wagner EH, Kaplan SH, Manning WG. The unreliability of individual physician "report cards" for assessing the costs and quality of care of a chronic disease. JAMA 1999; 281(22):2098-105. 47. Holmboe ES, Meehan TP, Lynn L, Doyle P, Sherwin T, Duffy FD. Promoting physicians' self-assessment and quality improvement: the ABIM diabetes practice improvement module. J Contin Educ Health Prof 2006; 26(2):109-19. 48. Jones N 3rd, Jones SL, Miller NA. The Medicare Health Outcomes Survey program: overview, context, and nearterm prospects. Health Qual Life Outcomes 2004; 2:33. 49. Kmetik KS, Williams JR, Hammons T, Rosof BM. The American Medical Association and physician performance measurement: information for improving patient care. Tex Med 2000; 96(10):80-3. 50. Kogan JR, Reynolds EE, Shea JA. Effectiveness of report cards based on chart audits of residents' adherence to practice guidelines on practice performance: a randomized controlled trial. Teach Learn Med 2003; 15(1):25-30. 51. Kupersmith J, Francis J, Kerr E et al. Advancing evidence-based care for diabetes: lessons from the Veterans Health Administration. Health Aff (Millwood) 2007; 26(2):w156-68. 52. Lanier DC, Roland M, Burstin H, Knottnerus JA. Doctor performance and public accountability. Lancet 2003; 362(9393):1404-8. 53. Parkerton PH, Smith DG, Belin TR, Feldbau GA. Physician performance assessment: nonequivalence of primary care measures. Med Care 2003; 41(9):1034-47. 54. Persell SD, Wright JM, Thompson JA, Kmetik KS, Baker DW. Assessing the validity of national quality measures for coronary artery disease using an electronic health record. Arch Intern Med 2006; 166(20):2272-7. 55. Roper WL, Mays GP. Performance measurement in public health: conceptual and methodological issues in building the science base. J Public Health Manag Pract 2000; 6(5):66-77. 56. Senn GF. Benchmarking: your performance measurement and improvement tool. Gastroenterol Nurs 2000; 23(5):221-5. 57. Smylie J, Anderson I, Ratima M, Crengle S, Anderson M. Indigenous health performance measurement systems in Canada, Australia, and New Zealand. Lancet 2006; 367(9527):2029-31. 58. Spertus JA, Eagle KA, Krumholz HM, Mitchell KR, Normand SL. American College of Cardiology and American Heart Association methodology for the selection and creation of performance measures for quantifying the quality of cardiovascular care. J Am Coll Cardiol 2005; 45(7):1147-56. 59. Stark JF, Stark J. Performance measurement in congenital heart surgery: benefits and drawbacks. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu 2003; 6:171-83. 60. Sugarman JR, Frederick PR, Frankenfield DL, Owen WF Jr, McClellan WM. Developing clinical performance measures based on the Dialysis Outcomes Quality Initiative Clinical Practice Guidelines: process, outcomes, and implications. Am J Kidney Dis 2003; 42(4):806-12. 61. Tang PC, Ralston M, Arrigotti MF, Qureshi L, Graham J. Comparison of methodologies for calculating quality measures based on administrative data versus clinical data from an electronic health record system: implications for performance measures. J Am Med Inform Assoc 2007; 14(1):10-5. 62. Wallace LM, Freeman T, Latham L, Walshe K, Spurgeon P. Organisational strategies for changing clinical practice: how trusts are meeting the challenges of clinical governance. Qual Health Care 2001; 10(2):76-82. 63. Walter LC, Davidowitz NP, Heineken PA, Covinsky KE. Pitfalls of converting practice guidelines into quality measures: lessons learned from a VA performance measure. JAMA 2004; 291(20):2466-70. 64. Weiss KB, Wagner R. Performance measurement through audit, feedback, and profiling as tools for improving clinical care. Chest 2000; 118(2 Suppl):53S-8S. Engaging Consumers: Public Disclosure 65. Boscarino JA, Adams RE. Public perceptions of quality care and provider profiling in New York: implications for improving quality care and public health. J Public Health Manag Pract 2004; 10(3):241-50. In a phone survey of New York State residents, about one third of individuals said they ere “very concerned” about the quality of health care. Less than half of individuals recalled seeing information about health care quality in the last year and only 20 percent used it in medical decision making. Individuals most often obtained information from media and family or friends, and said that certain types of information carried more weight than others. Responses varied significantly by race. 66. Druss BG, Miller CL, Rosenheck RA, Shih SC, Bost JE. Mental health care quality under managed care in the United States: a view from the Health Employer Data and Information Set (HEDIS). Am J Psychiatry 2002; 159(5):860-2. This study examines the correlation between five mental health process measures and HMO financing, public reporting of data of HEDIS data, and general medical quality. Results show that failure to report data publicly predicted poorer quality mental health care. 67. Hibbard JH, Stockard J, Tusler M. Hospital performance reports: impact on quality, market share, and reputation. Health Aff (Millwood) 2005; 24(4):1150-60. In this experimental study, hospitals that received publicly reported data improved obstetrics outcomes more than hospitals receiving private reports or no reports. Consumers were also more able to correctly identify highly rated hospitals when the data were made publicly available, though no changes in market hare for low or high performing hospitals were found. 68. Werner RM, Asch DA. The unintended consequences of publicly reporting quality information. JAMA 2005; 293(10):1239-44. This article provides an overview of the proposed mechanisms through which public reporting is expected to influence quality, outlines the literature demonstrating equivocal support that public reporting does indeed improve quality, and points out the unanticipated consequences that may arise as a result of public reporting. 69. Casalino LP, Alexander GC, Jin L, Konetzka RT. General internists' views on pay-for-performance and public reporting of quality scores: a national survey. Health Aff (Millwood) 2007; 26(2):492-9. The authors report findings from a survey of general internists. 73% of providers agreed that “if the measures are accurate, physicians should be given financial incentives for quality.” Yet, 70% disagreed that data reported at present are accurate. Less than one third supported the notion of public reporting. Concerns about avoidance of high-risk patients and diverting attention from non-measured care were raised as serious concerns. 70. Ackermann RT, Thompson TJ, Selby JV et al. Is the number of documented diabetes process-of-care indicators associated with cardiometabolic risk factor levels, patient satisfaction, or self-rated quality of diabetes care? The Translating Research into Action for Diabetes (TRIAD) study. Diabetes Care 2006; 29(9):2108-13. 71. Baker DW et al. The Effect of Publicly Reporting Hospital Performance on Market Share and Risk Adjusted Mortality at High-Mortality Hospitals. Medical Care 2003; 41(6): 729-740. 72. Bentley, JM Nash DB. How Pennsylvania Hospitals Have Responded to Publicly Released Reports on Coronary Artery Bypass Graft Surgery. Joint Commission Journal on Quality Improvement 1998; 24(1): 40-49. 73. Burack JH, Impellizzeri P, Homel P, Cunningham JN Jr. Public reporting of surgical mortality: a survey of New York State cardiothoracic surgeons. Ann Thorac Surg 1999; 68(4):1195-200; discussion 1201-2. 74. Chassin MR. Achieving and Sustaining Improved Quality: Lessons from New York State and Cardiac Surgery. Health Aff (Millwood) 2002;21(4): 40-51. 75. Dranove D. , Kessler D. , McClellan M. , Satterwaite M. Is more information better? The effects of "report cards" on health care providers. J Polit Econ 2003; 111:555-88. 76. Hamblin R. Publishing 'quality' measures: how it works and when it does not? Int J Qual Health Care 2007; 19(4):183-6. 77. Hannan EL, Kilburn H Jr, Racz M, Shields E, Chassin MR. Improving the outcomes of coronary artery bypass surgery in New York State. JAMA 1994; 271(10):761-6. 78. Hibbard JH, Stockard J, Tusler M. Does publicizing hospital performance stimulate quality improvement efforts? Health Aff (Millwood) 2003; 22(2):84-94. 79. Jha AK, Li Z, Orav EJ, Epstein AM. Care in U.S. hospitals--the Hospital Quality Alliance program. N Engl J Med 2005; 353(3):265-74. 80. Keating NL, Landrum MB, Landon BE et al. The influence of physicians' practice management strategies and financial arrangements on quality of care among patients with diabetes. Med Care 2004; 42(9):829-39. 81. Krumholz HM, Rathore SS, Chen J, Wang Y, Radford MJ. Evaluation of a consumer-oriented internet health care report card: the risk of quality ratings based on mortality data. JAMA 2002; 287(10):1277-87. 82. Laschober M, Maxfield M, Felt-Lisk S, Miranda DJ. Hospital response to public reporting of quality indicators. Health Care Financ Rev 2007; 28(3):61-76. 83. Marshall MN, Hiscock J, Sibbald B. Attitudes to the public release of comparative information on the quality of general practice care: qualitative study. BMJ 2002; 325(7375):1278. 84. Marshall MN, Shekelle PG, Leatherman S, Brook RH. The public release of performance data: what do we expect to gain? A review of the evidence. JAMA 2000; 283(14):1866-74. 85. Mehrotra A, Bodenheimer T, Dudley RA. Employers' efforts to measure and improve hospital quality: determinants of success. Health Aff (Millwood) 2003; 22(2):60-71. 86. Neuhauser D, Harper DL. Too good to last: did Cleveland Health Quality Choice leave a legacy and lessons to be learned? Qual Saf Health Care 2002; 11(2):202-3. 87. Peters E, Dieckmann N, Dixon A, Hibbard JH, Mertz CK. Less is more in presenting quality information to consumers. Med Care Res Rev 2007; 64(2):169-90. 88. Schneider EC , Epstein AM. Use of public performance reports: a survey of patients undergoing cardiac surgery. JAMA 1998; 279(20):1638-42. 89. Shahian DM, Normand SL, Torchiana DF. Cardiac surgery report cards: comprehensive review and statistical critique. Ann Thorac Surg 2001; 72(6):1845-8. 90. Shaller D, Sofaer S, Findlay SD, Hibbard JH, Lansky D, Delbanco S. Consumers and quality-driven health care: a call to action. Health Aff (Millwood) 2003; 22(2):95-101. 91. Werner RM, Asch DA, Polsky D. Racial profiling: the unintended consequences of coronary artery bypass graft report cards. Circulation 2005; 111(10):1257-63. 92. Williams SC, Schmaltz SP, Morton DJ, Koss RG, Loeb JM. Quality of care in U.S. hospitals as reflected by standardized measures, 2002-2004. N Engl J Med 2005; 353(3):255-64. Improving Health Care Delivery: Information Technology 93. Adler-Milstein J, McAfee AP, Bates DW, Jha AK. The State Of Regional Health Information Organizations: Current Activities And Financing. Health Aff (Millwood) 2007. Despite the promise of RHIOs, by early 2007 nearly one in four were defunct. Of 145 programs surveyed, only 20 were of modest size and exchanging clinical data. 94. Lorenzi NM. Strategies for creating successful local health information infrastructure initiatives. 2003. Lorenzi notes that despite conceptual support, organizational barriers such as lack of buy-in from stakeholders, perceived loss of control and trust, lack of ownership, lack of clarity around financing, and a perceived need for centralized data repositories underlie the collapse of the Community Health Information Network. A model for success is proposed. 95. Overhage JM, Dexter PR, Perkins SM et al. A randomized, controlled trial of clinical information shared from another institution. Ann Emerg Med 2002; 39(1):14-23. This randomized controlled trial showed that clinical information exchange between two hospital emergency departments if feasible, if not convenient. Some cost savings could be demonstrated in one hospital, but not in the other, likely due to a difference in work flows. No improvements in quality of care were noted. 96. Sidorov J. It Ain't Necessarily So: The Electronic Health Record And The Unlikely Prospect Of Reducing Health Care Costs. Health Aff (Millwood) 2006; 25(4):1079-85. The potential of EHRs to reduce costs, avoid medical and pharmaceuticals, and improve health care quality has not been realized. A critical eye needs to be cast on the ability of EHRs alone to transform healthcare. 97. Steiner V, Hartmann J, Ronau T. MedReach: building an Area Health Education Center medical information outreach system for northwest Ohio. J Med Libr Assoc 2002; 90(3):317-22. To reach underserved areas in northwest Ohio, the AHEC and other partners have come together to connect distant sites to the Medical College of Ohio enabling them to search electronic textbooks, databases, and other information to support medical diagnosis, treatment, and research. Feedback on this program has been quite positive. 98. Bartschat W, Burrington-Brown J, Carey S et al. Surveying the RHIO landscape. A description of current RHIO models, with a focus on patient identification. J AHIMA 2006; 77(1):64A-D. 99. Brailer DJ. Interoperability: The Key To The Future Health Care System. Health Aff 2005; . 100. Brennan PF, Ferris M, Robinson S, Wright S, Marquard J. Modeling participation in the NHII: operations research approach. AMIA Annu Symp Proc 2005; 76-80. 101. Carr K, Bangalore D, Benin A, Holmboe ES. Leveraging the benefits of Health Information Technology to support healthcare delivery model redesign. J Healthc Inf Manag 2006; 20(1):31-41. 102. Casalino L, Gillies R, Shortell SM et al. External Incentives, Information Technology, and Organized Processes to Improve Health Care Quality for Patients With Chronic Diseases. JAMA 2003; 289(4):434-41. 103. Conn J. Brailer's IT plans draw fire. Privacy, RHIO concerns surface as contracts awarded. Mod Healthc 2005; 35(42):14. 104. Doebbeling BN, Chou AF, Tierney WM. Priorities and strategies for the implementation of integrated informatics and communications technology to improve evidence-based practice. J Gen Intern Med 2006; 21 Suppl 2:S50-7. 105. Doebbeling BN, Vaughn TE, McCoy KD, Glassman P. Informatics implementation in the Veterans Health Administration (VHA) healthcare system to improve quality of care. AMIA Annu Symp Proc 2006; 204-8. 106. Duvvuri VR, Jianhong W. Information and communication technology developments in asthma management: a systematic review. Indian J Med Sci 2007; 61(4):221-41. 107. Frohlich J, Karp S, Smith MD, Sujansky W. Retrospective: lessons learned from the Santa Barbara project and their implications for health information exchange. Health Aff (Millwood) 2007; 26(5):w589-91. 108. Fung CH, Woods JN, Asch SM, Glassman P, Doebbeling BN. Variation in implementation and use of computerized clinical reminders in an integrated healthcare system. Am J Manag Care 2004; 10(11 Pt 2):878-85. 109. Grannis SJ, Biondich PG, Mamlin BW, Wilson G, Jones L, Overhage JM. How disease surveillance systems can serve as practical building blocks for a health information infrastructure: the Indiana experience. AMIA Annu Symp Proc 2005; 286-90. 110. Green CJ, Fortin P, Maclure M, Macgregor A, Robinson S. Information system support as a critical success factor for chronic disease management: Necessary but not sufficient. Int J Med Inform 2006; 75(12):818-28. 111. Guerra A. RHIO & vendor growing together. The Utah Health Information Network continues to work in tandem with Columbus, Ohio-based HTP. Healthc Inform 2006; 23(8):61. 112. Hagland M. From struggles to success. Part technology, part cooperation and part good old fashioned trial and error are what it taikes to build--or break--a RHIO. Healthc Inform 2007; 24(9):34, 36-7. 113. Halamka J, Aranow M, Ascenzo C et al. Health care IT collaboration in Massachusetts: the experience of creating regional connectivity. J Am Med Inform Assoc 2005; 12(6):596-601. 114. Hillestad R, Bigelow J, Bower A et al. Can electronic medical record systems transform health care? Potential health benefits, savings, and costs. Health Aff (Millwood) 2005; 24(5):1103-17. 115. Holmquest DL. Another lesson from Santa Barbara. Health Aff (Millwood) 2007; 26(5):w592-4. 116. Joshy G, Simmons D. Diabetes information systems: a rapidly emerging support for diabetes surveillance and care. Diabetes Technol Ther 2006; 8(5):587-97. 117. Kaushal R, Blumenthal D, Poon EG et al. The costs of a national health information network. Ann Intern Med 2005; 143(3):165-73. 118. Kemper AR, Uren RL, Clark SJ. Adoption of electronic health records in primary care pediatric practices. Pediatrics 2006; 118(1):e20-4. 119. Koval D. Real-world RHIO. A regional health information organization blazes a trail in Upstate New York. J AHIMA 2005; 76(3):44-8. 120. Lagoe RJ, Westert GP. Community wide electronic distribution of summary health care utilization data. BMC Med Inform Decis Mak 2006; 6:17. 121. Lawrence D. Doing it right. While the key to the perfect RHIO may still be a mystery, a number of them are off and running. Healthc Inform 2007; 24(9):38, 40. 122. Lawrence D. RHIO or not--it works. A pilot program on medication histories in EDs is first for Vermont Health Information Exchange. Healthc Inform 2007; 24(9):46. 123. Leatt P, Shea C, Studer M, Wang V. IT solutions for patient safety--best practices for successful implementation in healthcare. Healthc Q 2006; 9(1):94-104. 124. Leviss J. Identity and access management: the starting point for a RHIO. Health Manag Technol 2006; 27(1):64, 63. 125. Lovis C, Spahni S, Cassoni N, Geissbuhler A. Comprehensive management of the access to the electronic patient record: towards trans-institutional networks. Int J Med Inform 2007; 76(5-6):466-70. 126. Marchibroda J, Covich Bordenick J. Emerging trends and issues in health information exchange. Selected findings from Ehealth Initiative Foundation's Second Annual Survey of State, Regional and Community-based Health Information Exchange Initiatives and Organizations 2005eHealth Initiative Foundation, 2005. 127. Markle Foundation, Robert Wood Johnson Foundation. Achieving Electronic Connectivity In Healthcare: A Preliminary Roadmap from the Nation’s Public and Private-Sector Healthcare Leaders. 2004. 128. Marquard J, Brennan PF, Grindrod D, Zayas-Caban T. Health information exchange networks: understanding stakeholder views. AMIA Annu Symp Proc 2005; 1044. 129. Martin Z. Virginia RHIO taking baby steps. Health Data Manag 2007; 15(2):120, 122. 130. Miller RH, Miller BS. The Santa Barbara County Care Data Exchange: what happened? Health Aff (Millwood) 2007; 26(5):w568-80. 131. Miller RH, West CE. The value of electronic health records in community health centers: policy implications. Health Aff (Millwood) 2007; 26(1):206-14. 132. Murray E, Burns J, See Tai S, Lai R, Nazareth I. Interactive Health Communication Applications for people with chronic disease (Review). The Cochrane Collaboration 2007; (4). 133. Orlova AO, Dunnagan M, Finitzo T et al. Electronic health record - public health (EHR-PH) system prototype for interoperability in 21st century healthcare systems. AMIA Annu Symp Proc 2005; 575-9. 134. Overhage JM, Evans L, Marchibroda J. Communities' readiness for health information exchange: the National Landscape in 2004. J Am Med Inform Assoc 2005; 12(2):107-12. 135. Raths D. Real solutions for RHIO problems. Pioneering data exchange groups seek sustainability by solving business problems for members. Healthc Inform 2006; 23(8):26-9. 136. Sackett KM, Erdley WS, Jones J. The Western New York regional electronic health record initiative: Healthcare informatics use from the registered nurse perspective. Stud Health Technol Inform 2006; 122:248-52. 137. Shapiro JS, Kannry J, Lipton M et al. Approaches to patient health information exchange and their impact on emergency medicine. Ann Emerg Med 2006; 48(4):426-32. 138. Sittig DF, Shiffman RN, Leonard K et al. A draft framework for measuring progress towards the development of a National Health Information Infrastructure. BMC Med Inform Decis Mak 2005; 5(1):14. 139. Solomon MR. Regional health information organizations: a vehicle for transforming health care delivery? J Med Syst 2007; 31(1):35-47. 140. Walker J, Pan E, Johnston D, Adler-Milstein J, Bates DW, Middleton B. The Value Of Health Care Information Exchange And Interoperability. Health Aff (Millwood) 2005. Improving Health Care Delivery: Provider Networks 141. Community Care of North Carolina. Asthma Disease Management Program Summary. 2007. This issue brief outlines the successful North Carolina Asthma program, including its multimodal engagement of physicians from the identification of best practices to regular performance measurement and reporting to substantial practice and provider supports including the development of provider networks. 142. Cotter JJ, McDonald KA, Parker DA et al. Effect of different types of Medicaid managed care on childhood immunization rates. Eval Health Prof 2000; 23(4):397-408. Variation in primary preventive care, specifically immunization rates in children, is substantial between different types of Medicaid managed care programs in Virginia. Rates of childhood immunization were highest in the PCCM program and lowest in the mandatory HMO program. 143. Green LA, White LL, Barry HC, Nease DE Jr, Hudson BL. Infrastructure requirements for practice-based research networks. Ann Fam Med 2005; 3 Suppl 1:S5-11. Practice-based research networks have the potential to support timely, relevant research for patients and the public, yet well-designed infrastructure needs to be in place to support these networks. Green and colleagues outline the “must haves” and the “nice to haves” in terms of infrastructure requirements for successful PBRNs. Thought must be given to patient privacy, compliance with regulations, and developing a strong network of participating practices. 144. Adams EK, Bronstein JM, Florence CS. Effects of primary care case management (PCCM) on Medicaid children in Alabama and Georgia: provider availability and race/ethnicity. Med Care Res Rev 2006; 63(1):58-87. 145. Adams EK, Bronstein JM, Florence CS. The impact of Medicaid primary care case management on office-based physician supply in Alabama and Georgia. Inquiry 2003; 40(3):269-82. 146. Anderko L, Bartz C, Lundeen S. Practice-based research networks: nursing centers and communities working collaboratively to reduce health disparities. Nurs Clin North Am 2005; 40(4):747-58, xi-xii. 147. Anderko L, Lundeen S, Bartz C. The Midwest Nursing Centers Consortium Research Network: translating research into practice. Policy Polit Nurs Pract 2006; 7(2):101-9. 148. Bronstein JM, Adams EK, Florence CS. Children's service use during the transition to PCCM in two states. Health Care Financ Rev 2005; 26(4):95-108. 149. Carpenter WR, Weiner BJ, Kaluzny AD, Domino ME, Lee SY. The effects of managed care and competition on community-based clinical research. Med Care 2006; 44(7):671-9. 150. Demiris G. The diffusion of virtual communities in health care: concepts and challenges. Patient Educ Couns 2006; 62(2):178-88. 151. Dluhy N, Christopher K, Gramling K, Leffers J, Russell GE, Sethares K. Embedded, engaged, evolving: a consortium of nurse researchers and clinicians. Nurs Outlook 2007; 55(2):79-84. 152. Garrett B, Davidoff AJ, Yemane A. Effects of Medicaid managed care programs on health services access and use. Health Serv Res 2003; 38(2):575-94. 153. Graham DG, Spano MS, Stewart TV, Staton EW, Meers A, Pace WD. Strategies for planning and launching PBRN research studies: a project of the Academy of Family Physicians National Research Network (AAFP NRN). J Am Board Fam Med 2007; 20(2):220-8. 154. Hurley RE, Freund DA, Taylor DE. Emergency room use and primary care case management: evidence from four Medicaid demonstration programs. Am J Public Health 1989; 79(7):843-6. 155. Hurley RE, Freund DA, Taylor DE. Gatekeeping the emergency department: impact of a Medicaid primary care case management program. Health Care Manage Rev 1989; 14(2):63-71. 156. Kho A, Zafar A, Tierney W. Information technology in PBRNs: the Indiana University Medical Group Research Network (IUMG ResNet) experience. J Am Board Fam Med 2007; 20(2):196-203. 157. Love MM, Pearce KA, Williamson MA, Barron MA, Shelton BJ. Patients, practices, and relationships: challenges and lessons learned from the Kentucky Ambulatory Network (KAN) CaRESS clinical trial. J Am Board Fam Med 2006; 19(1):75-84. 158. Mold JW, Peterson KA. Primary care practice-based research networks: working at the interface between research and quality improvement. Ann Fam Med 2005; 3 Suppl 1:S12-20. 159. Momany ET, Flach SD, Nelson FD, Damiano PC. A cost analysis of the Iowa Medicaid primary care case management program. Health Serv Res 2006; 41(4 Pt 1):1357-71. 160. Pace WD, Staton EW. Electronic data collection options for practice-based research networks. Ann Fam Med 2005; 3 Suppl 1:S21-9. 161. Pace WD, Staton EW, Holcomb S. Practice-based research network studies in the age of HIPAA. Ann Fam Med 2005; 3 Suppl 1:S38-45. 162. Pearce KA, Love MM, Barron MA, Matheny SC, Mahfoud Z. How and why to study the practice content of a practice-based research network. Ann Fam Med 2004; 2(5):425-8. 163. Petersen DJ, Bronstein J, Pass MA. Assessing the extent of medical home coverage among Medicaid-enrolled children. Matern Child Health J 2002; 6(1):59-66. 164. Schneider EC, Landon BE, Tobias C, Epstein AM. Quality oversight in medicaid primary care case management programs. Health Aff (Millwood) 2004; 23(6):235-42. 165. Schoenman JA, Evans WN, Schur CL. Primary care case management for Medicaid recipients: evaluation of the Maryland Access to Care program. Inquiry 1997; 34(2):155-70. 166. Schulman ED, Sheriff DJ, Momany ET. Primary care case management and birth outcomes in the Iowa Medicaid program. Am J Public Health 1997; 87(1):80-4. 167. Shields AE, Comstock C, Finkelstein JA, Weiss KB. Comparing asthma care provided to Medicaid-enrolled children in a Primary Care Case Manager plan and a staff model HMO. Ambul Pediatr 2003; 3(5):253-62. 168. Siegel RM, Bien J, Lichtenstein P et al. A safety-net antibiotic prescription for otitis media: the effects of a PBRN study on patients and practitioners. Clin Pediatr (Phila) 2006; 45(6):518-24. 169. Smith WR, Cotter JJ, McClish DK, Bovbjerg VE, Rossiter LF. Access, satisfaction, and utilization in two forms of Medicaid managed care. Clin Perform Qual Health Care 2000; 8(3):150-7. 170. Sprague L. Primary care case management: lessons for Medicare? Issue Brief Natl Health Policy Forum 2001; (768):1-11. 171. Tierney WM, Oppenheimer CC, Hudson BL et al. A national survey of primary care practice-based research networks. Ann Fam Med 2007; 5(3):242-50. 172. van Weel C, de Grauw W. Family practices registration networks contributed to primary care research. J Clin Epidemiol 2006; 59(8):779-83. 173. Vessey JA. Development of the Massachusetts School Nurse Research Network (MASNRN): A Practice-Based Research Network to improve the quality of school nursing practice. J Sch Nurs 2007; 23(2):65-72. 174. Walsh EG, Osber DS, Nason CA, Porell MA, Asciutto AJ. Quality improvement in a primary care case management program. Health Care Financ Rev 2002; 23(4):71-84. 175. Westfall JM, VanVorst RF, Main DS, Herbert C. Community-based participatory research in practice-based research networks. Ann Fam Med 2006; 4(1):8-14. 176. Wolf LE, Walden JF, Lo B. Human subjects issues and IRB review in practice-based research. Ann Fam Med 2005; 3 Suppl 1:S30-7. Aligning Benefits/ Financing Beaulieu N, Cutler, DM, Ho, K, et al. The Business Case for Diabetes Disease Management for Managed Care Organizations. Forum for Health Economics and Policy 2006;9(1): 1-36. The authors analyze the net return to HealthPartners of a diabetes disease management program. They find that the return was positive and grew over each of the 10 years of the study period. The authors go on to identify four factors that contribute to the under-provision of these services in some areas: adverse selection, churn in enrollees of a given plan; contracting difficulties that focuses almost exclusively on cost rather than cost and quality, network externalities like spill over in quality initiatives. 177. Rosenthal MB , Frank RG. What is the empirical basis for paying for quality in health care? Med Care Res Rev 2006; 63(2):135-57. This literature review provides a summary of the seven peer reviewed, empirical studies of the effect of paying for performance. They found that despite excitement from payers and policy-makers about the potential of pay-forperformance, there is little empirical evidence to support its effectiveness. Structure of the pay for performance programs – small bonuses, threshold structure, small percentage of a physician’s panel participating – could account for the equivocal findings. 178. Ahmann AJ. Guidelines and performance measures for diabetes. Am J Manag Care 2007; 13 Suppl 2:S41-6. 179. Armour BS, Pitts MM, Maclean R et al. The effect of explicit financial incentives on physician behavior. Arch Intern Med 2001; 161(10):1261-6. 180. Beaulieu ND, Horrigan DR. Putting smart money to work for quality improvement. Health Serv Res 2005; 40(5 Pt 1):1318-34. 181. Cannon MF. Pay-for-performance: is Medicare a good candidate? Yale J Health Policy Law Ethics 2007; 7(1):138. 182. Coleman K, Reiter KL, Fulwiler D. “The impact of pay-for-performance in a large network of community health centers.” J Health Care Poor Underserved. 2007 Nov;18(4):966-83. 183. Damberg CL, Raube K, Williams T, Shortell SM. Paying for performance: implementing a statewide project in California. Qual Manag Health Care 2005; 14(2):66-79. 184. Dixon J, Lewis R, Rosen R, Finlayson B, Gray D. Can the NHS learn from US managed care organisations? BMJ 2004; 328(7433):223-5. 185. Drebing CE, Van Ormer EA, Krebs C et al. The impact of enhanced incentives on vocational rehabilitation outcomes for dually diagnosed veterans. J Appl Behav Anal 2005; 38(3):359-72. 186. Epstein AM, Lee TH, Hamel MB. Paying physicians for high-quality care. N Engl J Med 2004; 350(4):406-10. 187. Freed GL, Uren RL. Pay-for-performance: an overview for pediatrics. J Pediatr 2006; 149(1):120-4. 188. Hillman AL, Ripley K, Goldfarb N, Nuamah I, Weiner J, Lusk E. Physician financial incentives and feedback: failure to increase cancer screening in Medicaid managed care. Am J Public Health 1998; 88(11):1699-701. 189. Kouides RW, Bennett NM, Lewis B, Cappuccio JD, Barker WH, LaForce FM. Performance-based physician reimbursement and influenza immunization rates in the elderly. The Primary-Care Physicians of Monroe County. Am J Prev Med 1998; 14(2):89-95. 190. Levin-Scherz J, DeVita N, Timbie J. Impact of pay-for-performance contracts and network registry on diabetes and asthma HEDIS measures in an integrated delivery network. Med Care Res Rev 2006; 63(1 Suppl):14S-28S. 191. McDonald R, Harrison S, Checkland K, Campbell SM, Roland M. Impact of financial incentives on clinical autonomy and internal motivation in primary care: ethnographic study. BMJ 2007; 334(7608):1357. 192. Millett C, Gray J, Saxena S, Netuveli G, Majeed A. Impact of a pay-for-performance incentive on support for smoking cessation and on smoking prevalence among people with diabetes. CMAJ 2007; 176(12):1705-10. 193. Petersen LA, Woodard LD, Urech T, Daw C, Sookanan S. Does pay-for-performance improve the quality of health care? Ann Intern Med 2006; 145(4):265-72. 194. Rosenthal MB , Frank RG, Li Z, Epstein AM. Early experience with pay-for-performance: from concept to practice. JAMA 2005; 294(14):1788-93. 195. Roski J, Jeddeloh R, An L et al. The impact of financial incentives and a patient registry on preventive care quality: increasing provider adherence to evidence-based smoking cessation practice guidelines. Prev Med 2003; 36(3):291-9. 196. Rye CB, Kimberly JR. The adoption of innovations by provider organizations in health care. Med Care Res Rev 2007; 64(3):235-78. 197. Steel N, Maisey S, Clark A, Fleetcroft R, Howe A. Quality of clinical primary care and targeted incentive payments: an observational study. Br J Gen Pract 2007; 57(539):449-54. 198. Tahrani AA, McCarthy M, Godson J et al. Diabetes care and the new GMS contract: the evidence for a whole county. Br J Gen Pract 2007; 57(539):483-5. 199. Town R, Kane R, Johnson P, Butler M. Economic incentives and physicians' delivery of preventive care: a systematic review. Am J Prev Med 2005; 28(2):234-40. 200. Volpp KG, Gurmankin Levy A, Asch DA et al. A randomized controlled trial of financial incentives for smoking cessation. Cancer Epidemiol Biomarkers Prev 2006; 15(1):12-8.