Eric's Fungal Notes
advertisement

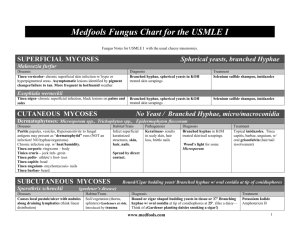
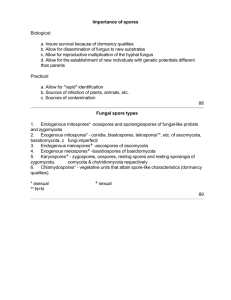
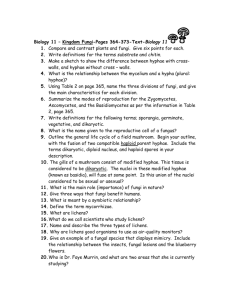
INTRODUCTION MYCOLOGY •the separation of the fungi from the bacteria is based on the fundamental difference in nuclear structure of eukaryotes and prokaryotes •fungi = eukaryotes (mb bound nucleus, chromosomes, mitochondria...) vs. bacteria = prokaryotes •fungi cell walls contain complex polysaccharides (chitin, chitosan, glucans, mannans) •fungi cell wall stains = Periodic Acid Schiff (PAS), Gomori’s Methenamine Silver stain (GMS), Calcifluor stain (CF) •fungi plasma mb contains sterols, principally ergosterol (site of action of antifungal drugs/drug resistence) Growth •Yeasts are unicellular fungi (reproduce by budding or fission) •Molds are multicellular fungi (germination » germ tube which grows from the tip (apical extension) » side branching » hyphae (network of filaments) » mycelium or thallus •Hyphae: Nonseptate (=coenocytic or multinucleated) OR Septate Reproduction •Sexual vs. Asexual (not exclusive, one species may reproduce in one way, the other, or both ways) •Asexual (Vegetative (special propagules not required) vs. Asexual Reproduction with Propagules (Conidia or Spores) Asexual Reproduction with Propagules: A. Conidia: develop from fertile hyphae via the blastic process (portion of hyphae blows-out before being separated by a septum) OR the thallic process (conversion of an entire segment of hypha into a conidium) 1. Arthroconidum (thallic conidia which break loose from each other @ maturity to initiate growth by germination) 2. Blastoconidum (blastic conidia; most yeasts reproduce in this fashion so yeast cell = blastoconidium; pseudohyphae are formed when blastoconidia do not separate @ maturity; molds also produce blastoconidia) 3. Chlamydoconidium (thallic conidia; thick-walled for survival, not multiplication) 4. Macroconidium (some fungi produce conidia of 2 separate sizes = microconidia & macroconidia; note terms do not indicate anything about conidiogenesis) B. Sporangiospore: produced by cytoplasmic cleavage within a structure called a sporangium; nonseptate hyphae for the most part in sporangiospore formers Sexual Reproduction: (not known to play a role in pathogenesis) Miscellaneous • Dimorphism: Zoopathogenic fungi may grow differently in tissue vs. nature/culture; often dictated by temperature (thermally dimorphic) •Opportunistic Fungus Diseases: (diabetes, lymphomas, broad spectrum antibiotic therapy, immunosuppressed (HIV/AIDS, corticosteroids, x-irradiation, cytotoxic drugs) - Coccidioides, Candida, Cryptococcus, Aspergillus, Mucor, Rhizopus, Pneumocystis Page 1 MYCOLOGY DISEASE DEFINITIONS EPIDEMIOLOGY CLINICAL LAB DX THERAPY DERMATOMYCOSES (any infectious disease of skin caused by fungus) Epidermophyton, Trichophyton, Microsporum (DERMATOPHYTOSES - ringworm) Ringworm or Tinea 6 Common Species: •M. canis •M. gypsum •T. mentagrophytes •T. rubrum •T. tousurans •E. foccusum •confined almost exclusively to cutaneous layers of body (hair, nails) •humans & other animals •dermatophytes use keratin in metabolism » keratinophiles Source: (worldwide) •Anthropophilic species = humans only; reduced conidiation •Zoophilic species = mainly other animals, but sometimes humans •Geophilic species = found in soil •Differentiate Genera by their large, multiseptate, elongate macroconidia (thallic conidia): 1. Microsporum - echinulate (spiky), spindle-shaped, thickwalled, borne singly 2. Trichophyton - cylindrical, smooth, thin-walled, borne singly 3. Epidermophyton - smooth, clubshaped, mod thick-walled, borne in clusters of 2 or 3 (microconidia are absent) Transmission: •direct contact w/lesions OR infected materials (hair, etc.) on fomites (inanimate objects) •contagious (almost all other mycoses are not) •involve the non-viable keratinized layers of skin •Tinea capitis (scalp/hair) •Tinea barbae (chronic; bearded area) •Tinea corporis (glabrous / smooth skin) •Tinea cruris (“jock strap itch”; groin, perineum, perianal) •Tinea pedis (“athlete’s foot”; feet, toe webs, soles) •Tinea unguim (nails) General: •definitive dx depends on the demonstration of a dermatophyte by: 1. direct mount (scraping, KOH to dissolve keratin, branching hyphae w/arthroconidia is diagnostic, false negatives but not false positives, ectothrix or endothrix from tinea capitis/barbae) 2. Wood’s Light (some species of Microsporum cause hairs to flouresce a greenish-yellow color upon UV light (365 nm) exposure; only 10% of tinea capitis in humans is diagnosable w/Wood’s light Prescription drugs: •Griseofulvin concentrates in keratinized skin » virtually eradicated tinea capitis in children •Ketoconazole systemically & topically Nonprescription drugs: •applied topically •usually effective •recurrences common •ingredients = undecylenic acid, tolnoftate, miconazole 3. Culture (Sabouraud’s dextrose agar OR some similar recipe of dextrose & peptone w/ agar; add chloramphenical & cycloheximide for selectivity YEAST INFECTIONS Candida Candidiasis (or candidosis) •acute or subacute superficial disease of skin, nails, & mucous mbs •rarely, it involves other deep-seated areas of the body Source/Transmission: •endogenous/opportunistic •Candida species are commensals of the GI tract, vagina, & oral mucosae •very common & may occasionally be contagious (sexual contact) •opportunistic during: early infancy/pregnancy, traumatic changes, endocrine dystrophies (DM), malnutrition, malignancy, anemia, changes induced by antibacterial or immunosuppressive drugs, or immunosuppressed pts •involve the skin, nails, and mucous mbs, or rarely disseminate to other organs Cutaneous lesions: •resemble dermatophytoses •involve area around the nail » clubshaped fingers •affect moist areas (groin, between fingers, etc.) •most common cause of diaper rash Mucous Membranes: •thrush (AIDS pts.) •perleche (corners of mouth) •vulvovaginitis •Chronic mucocutaneous candidiasis (CMC) affects individuals w/ deficient CMI; recurrent, but does not spread to deep tissues Systemic Disseminated Disease: •neutropenia predisposes •advanced malignancies (bladder or bowel cancer) •Hodgkin’s Disease •BM Transplant PULMONARY MYCOSES Cryptococcus neoformans Page 2 Appearance in Tissue & Exudates: •yeast cells (blastoconidia) & hyphal elements •hyphae normally pseudohyphae, but may be true hyphae w/ C. albicans •C. glabrata does not form hyphae •C. ggilliermondii forms pseudohyphae sparingly Appearance in Cultures: •soft, cream-colored colonies •often form pseudohyphae •C. albicans can form germ tubes when incubated @ 37°C in serum, etc. » true mycelium (but short-lived) ID of Candida in Lab: 1. Germ Tube Test: rapid ID of C. albicans 2. Formation of Pseudohyphae: most Candida species (except C. glabrata) form pseudohyphae when grown on Corn Meal Agar (CMA) w/ Tween-80; Chlamydoconidia (neither a conidium or a spore) are formed on CMA by C. albicans 3. Substrate Assimilation: species ID on basis of morphology on CMA & carbon source assimilation products •Fluconazole for oropharyngeal or esophageal thrush •Clotrimazole or nystatin for skin infections (topical) •Ketoconazole for mucocutaneous candidiasis •Amphotericin B, w/ or without flucytosine, or ketoconazole for disseminated candidiasis •Reduce predisposing factors •Thrush may be prevented by oral clotrimazole troches OR nystatin “swish & swallow” MYCOLOGY DISEASE Cryptococcosis “yeast meningitis” or Cryptococcal meningitis DEFINITIONS EPIDEMIOLOGY CLINICAL •chronic, wasting, frequently fatal disease (untreated/ immunosuppressed) characterized by a pronounced predilection for the central nervous system •most often in immunocompromised hosts (but Fluconazole has drastically decreased the incidence) •caused by a single species that has both an anamorphic & teleomorphic form of growth •anamorphic form is an encapsulated yeast w/ 2 biotypes, each of which has 2 serotypes (discerned based on antigenic epitopes within the capsule) Source: (worldwide) •2 biotypes of diff. geographic distribution & diff. ecological associations: 1. C. neoformans var. neoformans (serotypes A & D): avian habitats, esp. pigeons 2. C. neoformans var. gatii (serotypes B & C): tropical & subtropical; Eucalyptus trees •Transmission: inhalation of infectious conidia from an exogenous source •pulmonary cryptococcosis is usually subclinical, but may disseminate » meninges & brain parenchyma (common sites) •Skin lesions in 20% of disseminated cases LAB DX THERAPY Appearance in Tissue: •blastoconidium w/capsule •India ink stains the capsule for visualization •Amphotericin B + Flucytosine for meningitis or other disseminated disease Appearance in Culture: •mucoid colonies that contain encapsulated yeast cells (India ink as stain) •C. neoformans deposits melanin (via phenoloxidase) when grown in media (bird seed agar) containing certain catecholamines •Fluconazole in AIDS pts. used prophylactically is effecetive @ preventing infection Immunology/Serologic Tests: •Latex Agglutination Test reveals presence of capsular antigenic material from spinal fluid, urine, or serum (93% sensitive, more reliable than India ink smear of spinal fluid) Histoplasma capsulatum (var. capsulatum) Histoplasmosis 3 varietiesof H. capsulatum: 1. var. capsulatum 2. var. duboisii 3. var. farciminosum •Variety of clinical manifestations •Primary disease may be asymptomatic, subclinical, or a self-limited pulmonary disease of varying degrees of severity that leaves multiple areas of calcification •Dissemination (rare) » emaciation leukopenia, hepatosplenomegaly, and irregular fevers Source: (worldwide) •intensity in USA, esp. around major river valleys of Missouri, Mississippi, & Ohio rivers •organism can be isolated from soils contaminated w/ bird droppings (esp. chickens & starlings) and also bats •Animals other than humans can become infected: bats, cats, skunks, etc. (does not cause disease in birds) •Transmission: inhalation of infectious microconidia from an exogenous source (disease is not contagious though) •95% asymptomatic •5% symptomatic •All infected convert to positive skin test though Clinical Symptoms: •influenza-like w/ fever & pulmonary congestion (10-15% cavitate) •self-limiting in large portion of cases •Calcifications in the lung & sometimes in the spleen are common (cf. coccidioides) •small percentage disseminate » involvement of RES (liver, spleen, lymph nodes) » hepatosplenomegaly common Page 3 Dimorphism of H. capsulatum: •37°C (in vivo & in vitro) = ovoid budding yeast cell (blastoconidium) •25°C (Room Temp, in vitro) = mycelium w/ hyphae that produce characteristic tuberculate macroconidia (with finger-like projections on their walls) and small spherical microconidia that are infectious Appearance in Tissue: •inhaled microconidia undergo morphologic changes » direct budding » blastoconidia » yeast cells in mononuclear phagocytes in tissue (may be extracellular, but organism is a facultative intracellular parasite) •Oral Ketoconazole for progressive lung lesions •Amphotericin B for disseminated disease •Oral itraconazole is used to treat pulmonary or disseminated disease, as well as for chronic suppression in AIDS pts •only way to avoid is to avoid travel to endemic areas MYCOLOGY DISEASE DEFINITIONS EPIDEMIOLOGY CLINICAL LAB DX THERAPY •Transmission: inhalation of infectious arthroconidia from an exogenous source (disease is not contagious though) Dimorphism of C. immitis: •37°C (in vivo & in vitro) = large spherules containing many small endospores •25°C (Room Temp, in vitro) = mycelium w/ hyphae that form arthroconidia that are highly infectious (handle cultures w/ precaution) •Amphotericin B for persisting lung lesions or disseminated disease Coccidioides immitis Coccidioidomycosis (Valley Fever) •Primary infection may be asymptomatic, subclinical, or a self-limited, pulmonary disease of varying degrees of severity •Dissemination in small percentage of chronically ill » chronic or acute malignant disease that may involve nearly any tissue of the body Source: •New World organism •soil of North, Central, & South America •mostly SW USA - 10-15% outside endemic area • soil-inhabiting fungus of semiarid regions (alkaline soil, freedom from severe frosts, very hot, dry season followed by some rain = good) •Significant difference among the ethnic groups w/ regard to likelihood of disseminated disease (Filipinos especially susceptible due to assumptive genetic differences) •60% asymptomatic •40% symptomatic •All infected convert to positive skin test though Clinical Symptoms: •influenza-like (mild to severe) •self-limiting in large portion of cases •15% cavitate •small percentage disseminate Appearance in Tissue: •endospore-filled spherule found in tissue or exudates (sputum, CSF, pus) •spherules rupture » release of endospores » cycle of enlargement & nuclear replication General Immunology: •antigens are obtained from culture filtrates of both saprobic (mycelial) & parasitic (spherules) forms •saprobic growth filtrate = coccidioidin (most commonly used) •parasitic growth filtrate = spherulin Serologic & Immunologic Tests: 1. The Skin Test: inject coccidioidin (or spherulin) intradermally » rxn measures delayed type hypersensitivity (DTH) to C. immitis antigens •takes 3 wks to develop + test •Negative due to: too early, not coccidioidomycosis, or disseminated (anergy) •Positive: previous exposure (therefore immune to second attack) 2. Antibody Tests: IgM, IgG, IgA, and IgE classes •Tube Preciptin (TP): TP Ab of IgM isotype seen early in symptomatic illness and then wanes •Complement Fixation (CF): CF Ab of IgG isotype is produced later in disease & persists; titer correlated w/severity of disease Page 4 •Ketoconazole is also effective in lung disease •Fluconazole for meningitis (intrathecal Amphotericin B may be required) •only way to avoid is to avoid travel to endemic areas MYCOLOGY DISEASE DEFINITIONS EPIDEMIOLOGY CLINICAL LAB DX Source: (worldwide) •intensity in USA, esp. around major river valleys of Missouri, Mississippi, & Ohio rivers (like Histoplasma) •males > females in numbers affected (10:1) •some correlation w/occupation •age & race are of no importance •no reagent available for skin testing (so no estimate of the # of asymptomatic or subclinical cases) •Transmission: inhalation of infectious conidia from an exogenous source (disease is not contagious though) Dimorphism of B. dermatitidis: •37°C (in vivo & in vitro) = multiplies as blastoconidia (which are much larger than those of Histoplasma) w/thick cell walls & a wide base @ the juncture of budding daughter cells •25°C (Room Temp, in vitro) = white mycelium w/ hyphae upon which are produced ovoid, lateral conidia which are infectious •teleomorphic form of growth as well (Ajellomyces dermatitidis) THERAPY Blastomyces dermatitidis Blastomycosis •Chronic infection •Primary disease is a pulmonary infection acquired by inhalation of infectious conidia •Dissemination may involve any part of body but marked predilection for lungs, skin, and bone Clinical Symptoms: •first stage in infection is pulmonary which may resolve spontaneously, but does so less than pulmonary coccidioido-mycosis and histoplasmosis •chronic infection of the skin (face, leg, & foot) - may last many years •lesions are suppurative granulomas that heal spontaneously or by therapy w/ pronounced scar formation •Itraconazole for most patients •Amphotericin B for severe disease •Surgical excision may be helpful •no means of prevention Appearance in Tissue: •infectious conidia inhaled » large, solitary yeast cells embedded in abscesses w/single buds that have a broad basal attachment to the mother cell •generally not intracellular PURELY OPPORTUNISTIC INFECTIONS Aspergillus species (esp. Aspergillus fumigatus) Aspergillosis •Aspergillus spp. exist only as molds (they are not dimorphic) •Aspergillus spp. produce blastic conidia arranged on a special conidiophore •cause pulmonary infections of a localized or invasive type (rarely disseminated), allergy, or toxemias due to ingestion of secondary metabolites •Also, imp. causes of pulmonary disease in wild & domesticated animals & a cause of mycotic abortion in cattle Source: (worldwide) •all ages & sexes •becoming increasingly important as pathogens of immunocompromised hosts Transmission: •by airborne conidia Interact with animal hosts: 1. by inducing allergies 2. by infectious invasion of tissues 3. by forming toxins that contaminate feed or food & induce toxemias in those who ingest the products 3 General forms of disease: 1. Pulmonary aspergillosis: rare in immunocompetent, but extraordinarily common in birds (chickens, penguins) 2. Cavitary colonization: Aspergillus not uncommonly colonizes pulmonary cavities formed by other diseases (“fungus ball”) 3. Disseminated aspergillosis: occurs in immunocompromised hosts; route= pulmonary » skin, CNS, heart, lung, & nasal-orbital areas; Surgical contamination/inoculation may also occur Page 5 A. fumigatus as example: Appearance in Cultures: •produces a moderately fast growing, flat, velvety, bluish green colony, becoming brown on aging •chains of enteroblastic phialoconidia produced by one row of phialides pointing upward from the upper part of the vesicle Appearance in Tissue: •Septate hyphae that branch @ acute angles •Amphotericin B for invasive aspergillosis, but results may be poor •Surgical removal of fungus ball