CanTox Report - Council for Responsible Nutrition
advertisement

SAFETY ASSESSMENT AND DETERMINATION OF A
TOLERABLE UPPER LIMIT FOR EPHEDRA
Prepared for:
Council for Responsible Nutrition
1875 Eye St., N.W. - Suite 400
Washington, DC 2006-5409
Prepared by:
CANTOX HEALTH SCIENCES
INTERNATIONAL
2233 Argentia Road, Suite 308
Mississauga, Ontario, Canada
L5N 2X7
December 19, 2000
CANTOX Offices:
Mississauga
Calgary
Halifax
Vancouver
New Jersey
905-542-2900
403-237-0275
902-429-0278
604-688-8255
908-429-9202
SAFETY ASSESSMENT AND DETERMINATION OF A TOLERABLE UPPER LIMIT
FOR EPHEDRA
Table of Contents
Page
ABSTRACT
EXECUTIVE OVERVIEW
i
iii
1.0
INTRODUCTION
2.0
EPHEDRA/EPHEDRINE ALKALOIDS
2.1
Origin and History
2.2
Chemical Characteristics
2.3
Absorption, Distribution, Metabolism, and Excretion of Ephedrine
2.4
Pharmacokinetics of Ephedra or Ephedrine
2.4.1 Clinical Pharmacokinetic Studies
2.5
Pharmacology of Ephedra and Ephedrine
2.5.1 Clinical Pharmacology - Cardiovascular Activity
2.5.2 Clinical Pharmacology - Central Nervous System Activity
2.5.3 Clinical Pharmacology - Respiratory System Activity
2.5.4 Clinical Pharmacology - Sensitive Populations and Drug Interactions
2.6
Characterization of Dietary Supplements Containing Ephedra
4
4
4
6
8
9
14
15
16
16
16
17
3.0
ANIMAL TOXICOLOGICAL STUDIES ON EPHEDRA AND EPHEDRINE
ALKALOIDS
3.1
Acute Studies
3.2
Repeated Dose Studies
3.2.1 Short-Term Repeated Dose Studies
3.2.2 Subchronic Studies
3.3
Carcinogenicity Studies
3.3.1 103-Week Rat Feeding Study
3.3.2 103-Week Mouse Feeding Study
3.4
Reproductive and Teratogenicity Studies
3.5
Mutagenicity Studies
3.6
Other Studies
3.7
Discussion/Summary of Animal Data
20
20
29
29
38
42
42
46
49
52
55
55
4.0
HUMAN STUDIES RELATED TO THE SAFETY OF EPHEDRA AND
EPHEDRINE ALKALOIDS
4.1
Adverse Event Reports from CFSAN SN/AEMS/Published Case Reports
4.1.1 Adverse Event Reports for Dietary Supplements Containing Ephedrine
Alkaloids Reported to FDA SN/AEMS
4.1.2 Published Case Reports
Council for Responsible Nutrition
December 19, 2000
1
58
59
59
64
4.2
5.1
5.2
5.3
5.4
5.5
5.6
5.7
5.8
6.0
7.0
Clinical Studies
4.2.1 Clinical Trials and Investigations in Normal Healthy Individuals
4.2.2 Clinical Trials and Investigations of Ephedrine Together with
Physical Exercise/Temperature in Normal Healthy Individuals
4.2.3 Obesity Clinical Trials
4.2.4 Asthmatic Patients
4.2.5 Hypertensive Patients
4.2.6 Smoking Population
Are Results with Ephedrine Applicable for Extrapolation to Ephedra/
Ephedrine Alkaloids?
Conservatism Built into the Risk Assessment
Individual Risk Factors
Uncertainties Pertaining to Study Findings
Uncertainties Pertaining to Group Characteristics
Uncertainties in Ephedrine Content in Botanically-Derived Supplements
Uncertainties in Related Ephedrine Alkaloid Content in BotanicallyDerived Supplements
Uncertainties of Combination Herbal Products or Concomitant Use of
Other Products
71
87
98
105
134
136
139
141
142
142
143
144
146
146
149
DOSE RESPONSE ASSESSMENT/CONCLUSIONS FOR THE GENERAL
POPULATION
6.1
Data Selection
6.2
Identification of a NOAEL and a LOAEL
6.3
Uncertainty Assessment
6.4
Upper Limit (UL)
151
152
156
158
162
REFERENCES
176
List of Tables
Table 2.4.1-1
Table 2.4.1-2
Table 3.1-1
Table 3.2.1-1
Table 3.2.2-1
Table 3.3.1-1
Table 3.3.2-1
Table 3.5-1
Table 4.1.2-1
Table 4.2-1
Table 4.2.1-1
Elimination Kinetics of Ephedrine after Ingestion (Gurley et al.,
1998a)
Summary of Ephedrine Pharmacokinetics in Man
Summary of the Results of Acute Toxicity Studies Performed on
Ephedrine
Summary of Repeated Dose Studies on Ephedrine or Ephedra
Summary of Repeated Dose Studies on Ephedrine/Ephedra
Treatment Related Increases in Neoplasms in Rats
Treatment Related Increases in Neoplasms in Mice
Summary of Mutagenicity Studies on Ephedrine or Ephedra
Criteria for Development of Concepts of Causality
Index of All Clinical Studies Reviewed
Summary of Ephedrine Intake in Humans and Safety
Council for Responsible Nutrition
December 19, 2000
10
11
21
30
39
45
48
52
64
73
88
Table 4.2.2-1
Table 4.2.3-1
Table 4.2.3-2
Table 4.2.3-3
Table 4.2.3-4
Table 4.2.3-5
Table 4.2.2-6
Table 4.2.5-1
Table 6.2-1
Table 6.2-2
Table 6.2-3
Summary of Ephedrine Intake Together with Physical Parameters in
Healthy Normal Individuals
Summary of Clinical Trials with Obese Subjects Taking Ephedrine
Group Assignments for Huber, 2000
Reasons for Patient Withdrawal (Astrup et al., 1992; Quaade et al.,
1992; Toubro et al., 1993a)
Time Course of Effects
Frequency of Effects in All Patients
Reasons for Patient Withdrawal during Week 26 to 50(Toubro et
al., 1993b)
Summary of Study Design of Ingerslev et al. (1997)
Summary of Strengths and Weaknesses in Healthy Human
Population Study Design
Summary of Strengths and Weaknesses Ephedrine Intake Together
with Physical Parameters in Healthy Normal Individuals
Summary of Strengths and Weaknesses in Study Design in Obese
Individuals Taking Ephedrine
99
106
118
127
128
129
130
137
163
166
169
List of Figures
Figure 1
Chemical Structures of Ephedrine Alkaloids
List of Appendices
APPENDIX A
ANALYSIS OF THE AVAILABLE ADVERSE EVENT REPORTS
(AERs) FOR EPHEDRA
APPENDIX B
REVIEW OF PUBLISHED CASE REPORTS
APPENDIX C
BOOZER ET AL., (2000) ABSTRACT AND ANALYSIS
Council for Responsible Nutrition
December 19, 2000
6
ABSTRACT
The present report critically reviews the available information related to the safety of
ephedra/ephedrine alkaloids and establishes a safe upper intake based on the National Academy
of Sciences Upper Limit Model (UL) for nutrients. Information that was evaluated included
nNonclinical and clinical studies, published case reports, and animal data, along with adverse
event reports (AERs) from the medical literature and the voluntary FDA reporting system.
called Special Nutritionals/Adverse Event Monitoring System (SN/AEMS) under the direction of
the Center for Food Safety and Applied Nutrition (CFSAN) were evaluated. The term Tolerable
Upper Intake Level is defined as the maximum level of total chronic daily intake of a substance
judged unlikely to pose a risk of adverse health effects to most members of the healthy
population, including sensitive individuals, throughout the life stage, except in some discrete
subpopulations (for example, those with genetic predispositions or certain disease states) that
may be especially vulnerable to one or more adverse effects. Although the model was developed
for application to nutrients, these food components are like all chemical agents in that they can
produce adverse health effects if intakes are excessive. This UL is intended to provide a safety
standard for dietary supplements containing ephedrine ephedra such that no significant or
unreasonable risk of illness or injury would arise at or below this intake level under specified
conditions of use.
The data evaluation process for the UL method requires the selection of the most appropriate or
critical dataset(s) for deriving the UL. In the data evaluation process, and high quality human
data are generally preferable to animal data; however, in the absence of appropriate human data,
information from an animal species whose biological responses are most like those of humans is
used. The available human data provide the most relevant kind of information for hazard
identification potential of ephedra/ephedrine alkaloids. In terms of assessing the health effects
of chemicals in humans, controlled, prospective clinical investigations provide the most reliable
source of information. Following the assessment of the most critical dataset(s), a NOAEL dose
or intake level for humans is identified. Based on the strengths of the study design, duration of
study, number of subjects enrolled, and endpoints evaluated, 19 studies conducted in adultobese
individuals were determined of sufficient quality and extent for inclusion as the critical dataset
for the determination of a UL. A No Adverse Effect Level (NOAEL) was identified as 90
mg/day of ephedrine alkaloids in an herbal ephedra supplement, in a recent, well-conducted,
placebo-controlled, long-term 6-month investigation by Boozer et al. (2000).
Council for Responsible Nutrition
December 19, 2000
i
Following characterization of the NOAEL, safety factors or uncertainty factors (UF) are typically
applied. Judgments are made regarding uncertainties associated with extrapolating from the
observed data to the healthy population. The UF is typically applied to a NOAEL to derive the
UL, which generally represents a lower estimate of the threshold above which the there may be a
risk of adverse effects may increase. The UFs allocated are dependent on the nature and extent
of the toxicity safety database. A UF of 1 was judged appropriate, based on considerations of
pharmacokinetics of ephedrine, use patterns, duration of expected use, and animal studies, and
the strong scientific findings reported by Boozer et al. (2000) in the 6-month ephedra study, and
support ed by the of the clinical findings on ephedrine from Pasquali et al. (1985), Krieger et al.
(1990), Astrup et al. (1992), Quaade et al., (1992), Daly et al. (1993), Toubro et al. (1993a,b),
Nasser et al. (1999) and Molnár et al., 2000.
Application of the UF of 1 to the NOAEL of 90 derived a UL of 90 mg of ephedrine alkaloids in
ephedra per day for a generally healthy population. This daily level of intake is unlikely to pose
a risk of adverse health effects. The UL for ephedrine alkaloids in ephedra does not apply to
specific groups of persons, and other conditions of use include label instructions that: consumers
should check with their healthcare provider about taking the product; direct the consumer to split
the daily dose into at least three parts, so that no dose exceeds 30 mg; the product is intended for
use of not more than 6 months; and provide information to facilitate post-market monitoring.
Council for Responsible Nutrition
December 19, 2000
ii
EXECUTIVE OVERVIEW
Background
The use of herbal products in the United States has increased dramatically, as evidenced by sales
trends. Consumers annually spend approximately $14 billion on dietary supplements. The
dietary supplement industry estimates that as many as 2 to 3 billion doses of dietary supplements
containing ephedrine alkaloids as part of botanical ingredients are consumed each year in the
United States (GAO, 1999; AHPA, 2000) primarily for weight loss and/or energy enhancement.
Many botanical ingredients found in herbal products are generally regarded as safe; however,
when not used properly, they can result in effects that are distinct from expected physiological
responses to the agent.
Ephedra refers to a plant genus containing approximately 40 species throughout regions of
Europe, Asia, and America. Only a few Ephedra species contain the alkaloid ephedrine, which
was first isolated in 1885. In most species used commercially, the dominant alkaloid is
ephedrine, which usually comprises between 40 to 90% of total alkaloids in the plant, depending
on the species and other factors. Other related alkaloids are also present, such as
pseudoephedrine, N-methylephedrine, N-methylpseudoephedrine, norpseudoephedrine and
norephedrine (phenylpropanolamine). These alkaloids have been collectively termed ephedrinetype alkaloids, or simply ephedrine alkaloids. Proportions and total levels can vary from one
species to another, time of year of harvest, weather conditions and altitude. Ephedrine content
generally is 4 to 5 times greater than pseudoephedrine, but some sources of ephedra contain a 2:1
ratio of ephedrine and pseudoephedrine.
In general, all the ephedrine-type alkaloids (also referred to herein as “ephedrine alkaloids”)
contained in Ephedra species show significant differences between diastereomers (e.g.,
ephedrine and pseudoephedrine) with regard to pharmacokinetic and pharmacodynamic effects.
All have effects on the cardiovascular and respiratory system, but not to the same degree. It is
important to note that the pharmacokinetic and toxicokinetic behavior of any isomer cannot be
used with precision to predict that of any other ephedrine alkaloid isomers. In the literature,
statements regarding ephedrine alkaloids sometimes consider them to be synonymous, which
implies that the pharmacological activity of a particular alkaloid is equipotent and that the
toxicity of all diasteromers is equivalent, which is not the case. In the assessment of all the
evidence relevant to the safety of ephedra, literature on ephedrine is evaluated and the differences
or similarities are recognized.
Council for Responsible Nutrition
December 19, 2000
iii
The physiological characteristics of Ephedra species are dependent upon its chemical
composition. Since ephedrine is the dominant ephedrine alkaloid isomer of most Asian Ephedra
species, the characteristics of ephedrine would provide a good indicator of the expected
chemistry, pharmacology, and toxicology. Ephedra, for the purposes of this report, will generally
refer to the complex mixtures that are extracts of the branchlets of Asian Ephedra species known
as ma huang, or products containing these extracts. These ephedra extracts typically contain 68% ephedrine alkaloids. As with any mixture, the characteristics of only one, albeit major,
component cannot account for all the constituents of ephedra, but ephedrine represents a
significant portion of ephedra’s activity. Furthermore, since the effects of pseudoephedrine are
somewhat weaker with respect to hypertensive effects and stimulation of the central nervous
system, an assessment based on the ephedrine as a surrogate for total ephedrine alkaloid content
provides a conservative evaluation of risk. Recently released data from the six-month,
randomized, placebo-controlled clinical trial on ephedra performed by Columbia and Harvard
universities (Boozer et al., 2000) made a major contribution to the database. Thus, information
on ephedra itself, in addition to that on ephedrine, is relied upon in the risk assessment.
Objective of Risk Assessment
The purpose of the present report is to critically review the available information related to the
safety of ephedra/ephedrine alkaloids. Nonclinical and clinical studies, published case reports,
and animal data, along with adverse event reports (AERs) from the medical literature and the
voluntary reporting system called Special Nutritionals/Adverse Event Monitoring System
(SN/AEMS) under the direction of the Center for Food Safety and Applied Nutrition (CFSAN),
were evaluated. The objective of this review was to establish a safe upper intake based on the
National Academy of Sciences Upper Limit Model for nutrients. This Upper Limit (UL) is
intended to provide a safety standard for dietary supplements containing ephedrine such that no
significant or unreasonable risk of illness or injury would arise at or below this intake level. No
attempt was made to review or comment on findings related to the potential benefits of
ephedra/ephedrine alkaloids, or any risk versus benefit considerations.
The UL Model
The method used to establish a UL for ephedra/ephedrine alkaloids intake is the Tolerable Upper
Intake Level risk assessment model (Food and Nutrition Board, 1998). The term Tolerable
Upper Intake Level is defined as the maximum level of total chronic daily intake of a substance
Council for Responsible Nutrition
December 19, 2000
iv
judged unlikely to pose a risk of adverse health effects to the most sensitive members of the
healthy population. Although the model was developed for application to nutrients, these food
components are like all chemical agents in that they can produce adverse health effects if intakes
are excessive. In the UL model, as in all other risk assessment models, it is not possible to
identify a single, realistic “risk-free” intake level for a nutrient that can be applied with certainty
to all members of a population. It is possible to develop intake levels that are unlikely to pose
risks of adverse health effects to most members of the healthy population, including sensitive
individuals, throughout the life stage, except in some discrete subpopulations (for example, those
with genetic predispositions or certain disease states) that may be especially vulnerable to one or
more adverse effects.
The UL for ephedrine alkaloids in ephedra does not apply to specific groups of persons. In
particular, ephedrine and related agents should not be taken by individuals with coronary
thrombosis, diabetes, glaucoma, heart disease, hypertension, thyroid disease, impaired circulation
of the cerebrum, pheochromocytoma (a type of adrenal cancer that releases epinephrine), or
enlarged prostate. Patients with renal impairment may be at special risk for toxicity. Persons
taking ephedrine alkaloid drugs, due to cumulative intake, should not consume ephedracontaining dietary supplements, and ephedra is contraindicated for persons taking monomine
oxidase inhibitor drugs. Furthermore, ephedrine is not intended for use in infants, children,
adolescents younger than 18 years, and pregnant or lactating women.
Data Evaluation
The data evaluation process for the UL method, as well as other common risk assessment
techniques, requires the selection of the most appropriate or critical dataset(s) for deriving the
UL. In the data evaluation process, high quality human data are generally preferable to animal
data; however, in the absence of appropriate human data, information from an animal species
whose biological responses are most like those of humans is used. The available human data
provide the most relevant kind of information for hazard identification of ephedrine. Although
the typical focus of the majority of clinical studies was efficacy, taken collectively with the recent
clinical trial on safety and benefit (Boozer et al., 2000) they are of sufficient quality and extent to
draw conclusions on the safety of ephedra. Observational data in the form of case reports were
evaluated for their usefulness in developing hypotheses/relationships between exposure and
effect.
Council for Responsible Nutrition
December 19, 2000
v
The analysis of the clinical database involved a review of published case reports and of clinical
trials and investigations involving normal healthy individuals, under special conditions (i.e.,
exercise) and special populations (e.g., obese, asthmatic). Spontaneous adverse events captured
and reported by FDA were analyzed in Appendix A of the full report. Examination of clinical
trials involving the use of ephedrine was limited to studies that investigated safety parameters.
While valid and pertinent human data were considered superior to data derived from animals
when assessing the potential risks to humans from exposure to chemicals, any data deficiencies
in the human data must be explicitly considered.
In terms of assessing the health effects of chemicals in humans, controlled, prospective clinical
investigations provide the most reliable source of information. For example, studies of this type
are used to provide information related to the efficacy and safety of new pharmaceuticals (after
appropriate animal testing has defined potential risks and supported the investigational dosing of
humans). For most chemicals to which humans are exposed, prospective human studies are
unavailable, and as a result, relevant information related to their health effects must be obtained
retrospectively through the use of epidemiological methods, using standard principles, in an
attempt to establish causation and dose-response relationships. Another source of information on
the adverse effects of agents in humans is case reports. These are typically based upon
observations in individuals or small groups and they serve the critical function of alerting the
medical/scientific community to possible adverse events. Individual case reports generally
cannot be relied upon to establish a cause-effect relationship, but confidence in the findings of
individual reports increases when there is consistency in the observations published by different
authors. As with all scientific investigations, case-reports must be carefully reviewed for
limitations in methodology and the findings interpreted in the light of the weight-of-evidence.
Finally, with respect to the FDA AER database for ephedra, reviewed in Appendix A, the
reliability of the reported information was a major concern, (e.g., missing information, elapsed
time before reporting). Only 10% of the reported AERs contained a minimally sufficient
quantity of information, and no conclusive determination of unexpected effects or causality was
possible.
Toxicology Studies
The nonclinical toxicology of ephedrine and ephedra was reviewed to assess its consistency with
data obtained from clinical studies. The studies evaluated addressed the acute, subchronic and
chronic safety, carcinogenicity, reproductive toxicity, and mutagenicity of ephedrine. Where
available, data related to ephedra are emphasized; however, the database on ephedrine makes a
Council for Responsible Nutrition
December 19, 2000
vi
significant contribution to the total evidence relevant to ephedra, and thus was considered in the
risk assessment.
It is interesting to note that one study in the nonclinical literature compared the acute toxicity of
ephedrine to that of botanical ephedra extract. Although only one study was located in the
literature which compared the effects of ephedra versus ephedrine, these results support the
conservative assumption that ephedrine can be used in a safety assessment as a surrogate for
ephedra, since the potency of ephedrine overestimates the potential potency of ephedra itself.
The National Toxicology Program (NTP) studies, given the quality of the investigations, were
used to support for the derivation of a UL based on the clinical data. Rat carcinogenicity data
(103-week duration) were used, since mice were less sensitive to the effects of ephedrine. Thus,
the use of the rat species conservatively estimates a lifetime No-Observed-Adverse-Effect Level
(NOAEL) value. A NOAEL value was obtained in male rats, at an average daily consumption of
approximately 9 mg/kg body weight/day. A dose of 9 mg/kg body weight/day from the male rat
data extrapolated to a 60 kg (132 lb) person would be 540 mg/day.
Clinical Studies
Nine studies in normal healthy individuals investigated the effects of ephedrine intake (Bye et al.,
1974; Drew et al., 1978; Kuitunen et al., 1984; Astrup et al., 1991; Astrup and Toubro, 1993;
Liu et al., 1995; White et al., 1997; Gurley et al., 1998a; Shannon et al., 1999). Ephedrine
exposures involved oral administration over a short-duration such as 24-hours. The range of
total doses within these 9 studies was from 10 to 150 mg/day, given at a frequency of 1 to 3
times/day to achieve daily maximum specified. The foremost weakness in this healthy
population dataset was its limited duration (<24 h) that reduces the utility of these data in the
assessment of the UL. Nevertheless, these data are used to support the database in obese but
healthy subjects.
Five studies in healthy normal individuals investigated the effects of exercise/physical
parameters together with ephedrine use (Sidney and Lefcoe, 1977; Strömberg et al., 1992;
Vanakoski et al., 1993; Bell et al., 1998; Bell and Jacobs, 1999). The range of total doses within
these 5 studies was from 24 to 81 mg/day together with exercise, or some physical parameters,
over a short duration of exposure (typically 24 hours).
Council for Responsible Nutrition
December 19, 2000
vii
Twenty studies in obese, but otherwise reportedly healthy individuals (19 in adults and 1 in
children), investigated the effects of ephedrine intake (Astrup et al., 1985, 1992; Pasquali et al.,
1985, 1987, 1992; Krieger et al., 1990; Daly et al., 1993; Molnár, 1993; Toubro et al., 1993a,b;
Breum et al., 1994; Buemann et al., 1994; Kaats and Adelman, 1994; Moheb et al., 1998;
Waluga et al., 1998; Nasser et al., 1999; Huber, 1999,2000; Boozer et al., 2000; Molnár et al.,
2000 ). Ephedrine exposures involved oral administration over durations from 10 days to 26
months. The range of total doses within these studies was from 50 to 150 mg/day, given at
frequencies of 1 to 3 times/day to achieve the daily maximum specified. Based on the strengths
of the study design, duration of study, number of subjects enrolled and endpoints evaluated,
studies conducted in obese individuals were determined to be of sufficient quality and extent for
inclusion as the critical dataset for the determination of a UL. In particular, given the quality of
design and protocol, the Columbia/Harvard clinical trial conducted by Boozer et al. (2000), was
used to derive the UL which is supported by several other studies from the clinical literature.
The clinical database that has been considered involved administration of ephedrine singly,
ephedrine together with other components such as caffeine and/or acetylsalicylic acid (ASA) or
ephedra with caffeine. Since many dietary supplements which contain ephedrine often contain
other ingredients, including these data in the safety assessment of ephedrine is relevant,
especially given that these other ingredients are major components of ephedra preparations. The
pharmacology of individual ephedrine-type alkaloids has been well characterized, but the effects
of combinations of these other compounds are less well known. In addition, interactions between
ephedrine-type alkaloids and xanthine alkaloids (e.g., caffeine), as well as biologically active
compounds in other plant species that are constituents of many dietary supplements, have yet to
be fully characterized. This risk assessment assumes that a combination product (i.e., ephedra
together with a caffeine-containing ingredient) would be no more or less active than an
equivalent dose of ephedrine singly. Since combination products were given in many of the
clinical studies, this report evaluated the contribution/interaction of other ingredients typically
contained in ephedrine preparations, insofar as they contribute to the analysis of ephedra itself.
Determination of Upper Limit (UL)
Following the assessment of the most appropriate or critical dataset(s), a NOAEL dose or intake
level for humans is identified. In the absence of a NOAEL determination, a Lowest Observed
Adverse Effect Level (LOAEL) is chosen. In principle, the primary aim of safety studies is to
recognize the potential hazards associated with a particular chemical and identify a NOAEL or
LOAEL from the dose-response data. Monitoring data for adverse effects following ephedra
Council for Responsible Nutrition
December 19, 2000
viii
intake in obese individuals were used to identify the NOAEL of 90 mg/day, with the ephedra
clinical trial by Boozer et al. (2000) identified as the critical study.
Following characterization of the NOAEL, safety factors or uncertainty factors are typically
applied. Judgments are made regarding uncertainties associated with extrapolating from the
observed data to the healthy population. The UF is typically applied to a NOAEL or LOAEL to
derive the UL, which generally represents a lower estimate of the threshold above which the risk
of adverse effects may increase. The application of safety factors or uncertainty factors has been
used for over 30 years in the determination of a safe level of exposure to chemicals based on the
studies in experimental animals and humans (Renwick, 1995). The UFs allocated are dependent
on the nature and extent of the toxicity database.
A UF of 1 was judged appropriate, based on considerations of pharmacokinetics of ephedrine,
use patterns, duration of expected use, and animal studies and the strong scientific findings
reported by Boozer et al. (2000) and supported by the clinical findings from Pasquali et al.
(1985), Krieger et al. (1990), Astrup et al. (1992), Quaade et al., (1992), Daly et al. (1993),
Toubro et al. (1993a,b), Nasser et al. (1999) and Molnár et al., 2000. Given the quality of the
long-term investigation of ephedrine alkaloids in an herbal ephedra supplement by Boozer et al.
(2000), this study represents a pivotal clinical study in the safety evaluation of ephedra.
Application of the UF of 1 to the NOAEL of 90 derived a UL of 90 mg of ephedrine alkaloids in
ephedra per day for a generally healthy population. This daily level of intake is unlikely to pose a
risk of adverse health effects. Label instructions together with considerations of
pharmacokinetics of ephedrine, use patterns, duration of expected use, and supportive animal
studies further support a UF of 1. Label instructions would include statements that (1)
consumers should check with their healthcare provider about taking the product; (2) use is
contraindicated for certain people; (3) direct the consumer to split the daily dose into at least
three parts, so that no dose exceeds 30 mg; (4) the product is intended for use of not more than 6
months; (5) persons younger than 18 years should not use the product; (6) pregnant and lactating
women should not use the product; and (7) provide information to facilitate post-market
monitoring.
Council for Responsible Nutrition
December 19, 2000
ix
Conclusion
For healthy adults:
NOAEL = 90 mg/day, and UF =1
UL = 90 mg/day total ephedrine alkaloids from ephedra
Council for Responsible Nutrition
December 19, 2000
x
1.0
INTRODUCTION
The use of herbal products in the United States has increased dramatically, as evidenced by sales
trends. Consumers annually spend approximately $14 billion on dietary supplements according
to industry reports. The dietary supplement industry estimates that as many as 2 to 3 billion
doses of dietary supplements containing ephedrine alkaloids are consumed each year in the
United States (GAO, 1999; APHA, 2000). Many botanical ingredients found in herbal products
are generally regarded as safe; however, when not used properly, they can result in adverse
effects which are distinct from physiological responses to the agent.
At the request of the Council for Responsible Nutrition, CANTOX HEALTH SCIENCES
INTERNATIONAL (CANTOX) has reviewed the current nonclinical and clinical safety
database, published case reports, and adverse event report (AER) data from Food and Drug
Administration (FDA) monitoring system called Special Nutritionals/Adverse Event Monitoring
System (SN/AEMS) on ephedra/ephedrine alkaloids. The purpose of the present report is to
critically review the information available related to the safety of ephedra/ephedrine alkaloids in
humans and animals, including nonclinical and clinical studies, published case reports, and AER
data from the CFSAN SN/AEMS database. The objective of this review is to provide and justify
a safe upper intake level for ephedrine alkaloids from ephedra used as a dietary supplement
through use of the National Academy of Sciences Upper Limit Model for nutrients. This task
involved characterization of effects considered adverse through identification of a NOAEL and
application of an appropriate safety factor or uncertainty factor based on a weight-of-evidence
approach. Furthermore, this UL would provide a safety standard for dietary supplements
containing ephedra such that no significant or unreasonable risk of illness or injury would arise
from this intake under labeled conditions of use. No attempt was made to review or comment on
findings related to the potential benefits of ephedra/ephedrine alkaloids or any risk versus benefit
considerations. Information on ephedrine in bronchodilators was considered in the safety
assessment; but was not included. The FDA OTC monograph on ephedrine reflects a safety
assessment and analysis of risk versus benefit for bronchodilation. The health benefits of
ephedra/ephedrine alkaloids were specifically excluded from the CANTOX report.
The framework for developing a UL for ephedra/ephedrine alkaloids intake involves the use of
the National Academy of Sciences Upper Limit Model for nutrients. Since ephedra as a dietary
supplement is classified as a food, it is appropriate to use the NAS UL model to evaluate ephedra
data. Furthermore, the principles embodied in the NAS UL model are recognized and used by
many regulatory authorities to evaluate food and food ingredients.
Council for Responsible Nutrition
December 19, 2000
1
The term Tolerable Upper Intake Level is defined as the maximum level of total chronic daily
intake of a substance judged unlikely to pose a risk of adverse health effects to the most sensitive
members of a healthy population. Although the model was intended to be used for nutrients,
nutrients are like all chemical agents which can produce adverse health effects if intakes are
excessive. Furthermore, although in the NAS UL model the agents of interest are nutrients, this
risk assessment process is stated to be generally applicable to other food components.
As for traditional models for safety evaluation of food ingredients, the principles involve the
following :
Hazard identification
-evidence of adverse effect in humans
-causality
-relevance of experimental data
-animal data
-route of exposure
-duration of exposure
-mechanism of toxic action
-quality and completeness of the data base
-identification of distinct and highly sensitive subpopulations
Dose-response assessment
-data selection
-identification of a NOAEL (or LOAEL) and critical endpoint
-uncertainty assessment
-derivation of a UL
-characterization of the estimate and special considerations
Exposure assessment
Risk characterization
Consistent with the principles concluded by the Life Sciences Research Office in a report entitled
“Alternative and Traditional Models for Safety Evaluation of Food Ingredients”, (LSRO, 1998)
the reliability of management of risk is dependent on the generation of a quantitative measure of
the risk of an adverse effect. A principal feature of the risk assessment process for
noncarcinogens is the long-standing acceptance that no risk of adverse effects is expected unless
a threshold dose (or intake) is exceeded. Generation of this quantitative measure traditionally has
been based on the determination of a NOAEL and the use of an uncertainty factor (UF). The
Council for Responsible Nutrition
December 19, 2000
2
precision of the NOAEL is dependent on three factors, 1) the sensitivity of the endpoints used to
define the hazard, 2) the increments between the doses in the dose response dataset, and 3) the
number of subjects used to define the NOAEL. The critical issues concern the methods used to
identify the approximate threshold of toxicity for the larger and diverse human population. It is
essential that the magnitude of the UF be based on sound experimental or observational data. In
the NAS UL model the method for identifying thresholds for a healthy population ensures that
almost all members of the population will be protected. There is considerable confidence that the
population threshold derived by application of the model, which becomes the UL, lies very near
the low end of the theoretical distribution, and is the end representing the most sensitive
members of the population. In the UL model, it is not possible to identify a single, realistic “riskfree” intake level for a nutrient or other food component that can be applied with certainty to all
members of a population. It is possible to identify intake levels that are unlikely to pose risks of
adverse health effects to most members of the healthy population, including sensitive individuals,
at specific life stages, except in some discrete subpopulations (for example, those with genetic
predispositions or certain disease states) who may be especially vulnerable to one or more
adverse effects. Distinct subpopulations are not included in the general distribution because of
their unusual predispositions to toxicity. Such distinct groups may not be protected by the UL.
The following sections are summarized as follows: Section 2.0 reviews the chemical
characteristics, the pharmacokinetic and metabolic profile of ephedra/ephedrine alkaloids;
Section 3.0 reviews the nonclinical literature on ephedra/ephedrine alkaloids; Section 4.0 reviews
the clinical data on ephedra/ephedrine alkaloids; Section 5.0 is the evaluation of uncertainties,
and; Section 6.0 is the dose-response assessment of the UL and conclusions for the general
population.
Council for Responsible Nutrition
December 19, 2000
3
2.0
EPHEDRA/EPHEDRINE ALKALOIDS
2.1
Origin and History
Ephedra is a genus of plants (in the family Ephedraceae) which include 40 species which are
distributed throughout the temperate and subtropical regions of Europe, Asia and America.
Many of these Ephedra species contain the alkaloid ephedrine (Chen et al., 1929a,b; Chen and
Schmidt, 1930; Leung and Foster, 1996). In particular, ephedrine an active component of the
herb, can be obtained from Ephedra sinica Stapf., Ephedra intermedia Schrenk et C.A. Mey and
Ephedra equisetina Bge; the dried young branchlets of which are collectively referred to as ma
huang. The various other species of Asian Ephedra are also known as ma huang, even though
that name properly reserved for species grown in China (Namba et al., 1976).
Ephedra has a long history of use in Chinese medicine. Fifteenth century texts recommended ma
huang as an antipyretic and antitussive agent (Karch, 2000). Ephedrine was first isolated from
ephedra in 1885, by Nagyoshi Nagi, a German-trained, Japanese-born chemist who isolated and
synthesized ephedrine. International interest in the pharmacological activity was stimulated
when Chen and Schmidt published a monograph recommending ephedrine as the treatment of
choice for asthma (Chen and Schmidt, 1930).
2.2
Chemical Characteristics
Ephedrine can be synthesized, or isolated from the Asian Ephedra species. Typically, the content
of ephedrine alkaloids in ma huang account for 0.5 to 2.5% by dry weight. Proportions and total
levels can vary from one species to another, time of year of harvest, weather conditions and
altitude. In most species used commercially, the dominant alkaloid is ephedrine, which usually
comprises between 40 to 90% of total alkaloids in the plant, depending on the species (Tyler,
1993; Bruneton, 1996; Leung and Foster, 1996; Sheu, 1997). In addition to ephedrine and
pseudoephedrine, other closely related alkaloids have been isolated from ephedra such as Nmethylephedrine, N-methylpseudoephedrine, norpseudoephedrine and norephedrine
(phenylpropanolamine) (see Figure 1 for chemical structures). One of the most common Chinese
cultivars was found to contain 1.39% ephedrine, 0.361% pseudoephedrine and 0.069%
methylephedrine (Sagara et al., 1983). This mix is fairly typical for commercially grown ephedra
plants. Noncommercial varieties of ephedra may contain no ephedrine at all (Zhang et al., 1993).
The source of ephedrine alkaloids in dietary supplements can be from the whole herb or herb
extract; however, for pharmaceutical uses ephedrine itself can be easily synthesized.
Council for Responsible Nutrition
December 19, 2000
4
The physiological characteristics of ephedra are dependent upon its chemical composition. Since
the dominant ephedrine alkaloid isomer of most Ephedra species is ephedrine, the characteristics
of ephedrine would provide a good indicator of the expected chemistry, pharmacology, and
toxicology. As with any mixture, the characteristics of only one, albeit major, component cannot
define all of the characteristics of ephedra. However, in the case of ephedra, understanding the
effects of ephedrine provides insight into the biological activities of the herb itself. Furthermore,
Lee et al. (1999, 2000) recently reported that the potency of adrenergic activity and cytotoxicity
of ma huang extracts correlated with the ephedrine content; however, the cytotoxicity of all ma
huang extracts could not be totally accounted for by their ephedrine contents.
Ephedrine is known chemically as alpha-[1-(Methylamino)ethyl]benzene-methanol, or 1methylamino-ethyl-benzyl alcohol, or 2-methylamino-1-phenyl-1-propanol. It contains 2
asymmetric carbon atoms, so that there are 4 possible stereoisomers comprised of 2 pairs of
enantiomers. Only 2 stereoisomers actually occur in nature, namely l-ephedrine, which is the
ephedrine typically used clinically, and d-pseudoephedrine; these compounds are diastereomers.
These alkaloids can be extracted from the plant with alcohol, benzene and other organic solvents
using standard alkaloid extraction techniques. Purified ephedrine is obtained as odorless,
colorless crystals or as a white-crystalline powder with a bitter taste. Ephedrine and
pseudoephedrine have been shown to be highly stable. For laboratory and clinical uses, the
hydrochloride and sulphate salts of ephedrine are most commonly used.
Chemical Name:
Molecular Formula:
Molecular Weight:
Isomeric Forms:
Ephedrine
C10H15NO
165.24
Include d- and l-ephedrine
Council for Responsible Nutrition
December 19, 2000
5
Figure 1
Chemical Structures of Ephedrine Alkaloids
H
H
OH
OH
CH3
H
N
H
CH3
(-)-ephedrine
H
CH3
H
N
H
(+)-pseudoephedrine
H
OH
OH
CH3
CH3
H
N
H
CH3
(-)-methylephedrine
OH
CH3
NH2
(-)-norephedrine
2.3
CH3
(+)-methylpseudoephedrine
H
OH
H
N
H3C
H3C
H
CH3
CH3
H
NH2
(+)-norpseudoephedrine
Absorption, Distribution, Metabolism, and Excretion of Ephedrine
After oral administration, ephedrine is rapidly and completely absorbed from the gastrointestinal
tract (Wilkinson and Beckett, 1968a,b; Warot et al., 2000). The major route of elimination for
ephedrine in humans is urinary excretion. Up to 95% of an oral dose may be excreted in the
urine within 24 hours; 55 to 75% as unchanged and the rest as metabolites (Dollery, 1991a).
Ephedrine is metabolized in humans by N-demethylation to norephedrine
(phenylpropanolamine), at 8 to 20%. Ephedrine also undergoes oxidative deamination yielding
Council for Responsible Nutrition
December 19, 2000
6
1-phenylpropan-1,2-diol and further side-chain oxidation to benzoic acid and hippuric acid at 4
to 13% of an oral dose (Wilkinson and Beckett, 1968a,b; Sever et al., 1975). In general, the
pharmacokinetics of pseudoephedrine and phenylpropanolamine are similar to ephedrine
(Dollery, 1991a,b,c). The urinary excretion of ephedrine is pH-dependent due to the presence of
an ionizable group in the ephedrine molecule and is increased in acidic urine (May et al., 1975).
In alkaline urine, excretion is reduced to 20 to 35% of the dose (Wilkinson and Beckett,
1968a,b). In those with renal disease, the half-life would also likely be increased due to impaired
elimination.
Human pharmacokinetic studies show that absorption of oral ephedrine is complete within 2 to
2.5 hours (Wilkinson and Beckett, 1968a,b; Welling et al., 1971). It has been reported that
absorption of ephedrine is much slower when it is given as a component of ma huang, rather than
in its pure form (White et al., 1997). Ephedrine ingested in the form of ma huang had a time to
maximum plasma concentration (tmax) of almost 4 hours, compared to only 2 hours when pure
ephedrine was given; however, these findings were not confirmed in a subsequent study by the
same investigators which showed no difference (Gurley et al., 1998a). Ephedrine is rapidly and
extensively distributed throughout the body, with distribution to the liver, lungs, kidneys, spleen,
and brain. Wide interindividual variation in plasma levels has been observed after oral dosing.
The metabolism of ephedrine in humans, dogs and several species of rodents proceeds primarily
by 3 reactions; aromatic hydroxylation, N-demethylation and oxidative deamination. The extent
to which ephedrine is metabolized and the major metabolites vary quantitatively between species
(Axelrod, 1953; Sinsheimer et al., 1973; Williams et al., 1973). The extent of aromatic
hydroxylation is greatest in rats, followed by rabbits, guinea pigs, and dogs, with no aromatic
hydroxylation observed in humans. N-demethylation of ephedrine is greatest in rabbits followed
by dogs, guinea pigs, rats, and humans. Deamination is greatest in rabbits, followed by humans
and rats.
After oral administration, ephedrine is well absorbed from the gastrointestinal tract of rodents
and is rapidly excreted in the urine (Marvola and Kivirinta, 1978). Direct measurement of
ephedrine concentration in plasma showed that the peak blood level was reached within 5 to 6
minutes after oral administration of ephedrine hydrochloride to mice. Elimination from plasma
was reported to occur monoexponentially, with a half-life of 30.6 minutes. Ephedrine is
extensively metabolized by rabbits (Feller and Malspeis, 1977). Analysis of the radioactivity in
urine collected for 24 hours after administration of [14C] ephedrine revealed that the parent
compound accounted for only 3.4% of the total radioactivity excreted by rabbits administered d-
Council for Responsible Nutrition
December 19, 2000
7
ephedrine, and 0.7% of the radioactivity excreted by rabbits administered the l-ephedrine.
Hippuric and benzoic acids accounted for approximately 47 to 50% of the urinary [14C].
1-phenyl-1,2-propanediol accounted for 4 to 16%, either free or conjugated of the urinary [14C].
Radioactivity was excreted more rapidly from rabbits given the (+)-(S,R) isomer than from
rabbits given the (-)-(R,S) isomer. The urinary metabolites identified in this study were hippuric
acid, benzoic acid, norephedrine and l-phenyl-1,2-propanediol. The amounts of each metabolite
excreted following treatment with the different isomers were slightly different.
The biotransformation of ephedrine stereoisomers in vitro by rabbit liver microsomes was
investigated (Feller and Malspeis, 1977). All 4 isomers were N-demethylated at approximately
the same rate, and the rate of N-demethylation was observed to be faster than the rate of benzoic
acid formation.
2.4
Pharmacokinetics of Ephedra or Ephedrine
There are no clear relationships between plasma levels of ephedrine and particular
pharmacological effects (Dollery, 1991a). No change in disposition kinetics occurs after
repeated dosing has been observed, suggesting that the observed tolerance is due to
pharmacodynamic rather then pharmacokinetic factors (Hughes et al., 1985). Ephedrine is highly
lipophilic and crosses the blood-brain barrier. Placental transfer of ephedrine occurs and fetal
blood levels are approximately 70% that of the maternal blood levels (Hughes et al., 1985).
Ephedrine is also excreted in breast milk. Excretion patterns may be much more rapid in
children, and a greater dosage is usually required to achieve therapeutic effects.
Pharmacokinetic Profile of Ephedrine in Humans1
Oral absorption
100%
Plasma half life
3-11 hours
mean T1/2
6 hours
Apparent Volume of Distribution
122-320 litres
Plasma Protein Binding
None
1
Dollery, 1991a
A single 22 mg dose of ephedrine hydrochloride has been reported to give a maximum plasma
concentration in the range of 45 to 140 ng/mL: bronchodilation has been seen with plasma
concentration of 20 to 80 ng/mL (Dollery, 1991a). Ingestion of 375 mg of ma huang containing
Council for Responsible Nutrition
December 19, 2000
8
19.4 mg of ephedrine resulted in a blood concentration of 81 ng/ml, which was similar to peak
ephedrine levels observed after the peak ephedrine administration of an equivalent amount of
pure ephedrine (White et al., 1997). Vanakoski et al. (1993) gave 50 mg of ephedrine orally to 6
healthy, 21-year old women. The mean peak plasma concentration was measured at 168 ng/ml at
127 minutes after ingestion. These findings collectively are consistent with pharmacokinetic
studies conducted by Wilkinson and Beckett in 1968.
2.4.1
Clinical Pharmacokinetic Studies
Six clinical studies investigated the pharmacokinetics of ephedrine (Costello et al., 1975; Pickup
et al., 1976; Strömberg et al., 1992; Vanakoski et al., 1993; White et al., 1997; Gurley et al.,
1998a; Warot et al., 2000). The pharmacokinetic findings are summarized below.
The pharmacokinetics of 50 mg ephedrine administered orally was reported by Warot et al.
(2000). Sixteen healthy Caucasian males received 50 mg ephedrine. Ephedrine pharmacokinetic
and pharmacodynamic measures of subjective feelings, visual analogue scale, and cardiovascular
parameters were performed. Ephedrine was associated with significant increases in supine
systolic and diastolic blood pressure. The pharmacokinetic parameters showed that Tmax was 2
hours (1 - 4); Cmax (ng/ml) 137.8 33.1 (80.2 – 206.9), AUC 0-8 hour exp (nghr/ml) 778.2
201.3 (476 – 1284.4) and t1/2 (hr) was 7.1 1.9 (4.0 – 9.8).
Gurley et al. (1998a) examined the pharmacokinetics in humans after the ingestion of a dietary
supplement containing ephedra extract. Ten subjects were enrolled in a randomized, crossover
study with 4 phases which aimed at characterizing the pharmacokinetics of ephedrine after the
ingestion of 3 commercially available ma huang products compared with a 25 mg ephedrine
capsule. Eligibility was determined by the results of a medical history, brief physical
examination, medication history, and a pregnancy test for female subjects. Those candidates who
were in good health, not pregnant, and not taking continuous medications were selected.
Subjects agreed not to consume any medication or alcohol for the duration of the study. The
dietary supplements contained one or more of the following ingredients; astragalus, bee pollen,
caffeine, Camellia sinensis, Centella asiatica, Cola nitida, d-alpha tocopherol, Ginkgo biloba,
Glycyrrhiza glabra, Panx ginseng, Paullinia cupana, Spirulina pratensis, and Triticum aestivum.
On Day 1, after an 8-hour fast, an oral dose of medication and 8 oz of water was administered at
7 am. Subjects were then asked to refrain from eating for an additional 4 hours. A venous
catheter was placed in the forearm, and 5 ml of blood was drawn for determining ephedrine
concentrations at 0.25, 0.5, 0.75, 1, 1.5, 2, 3, 4, 6, 8, 10, 12, and 18 hours. There was a 1-week
Council for Responsible Nutrition
December 19, 2000
9
washout phase between ingestion of each of the 4 products. Pharmacokinetic parameters for
ephedrine from botanically derived products were similar to those for synthetic ephedrine
hydrochloride. It was reported that all subjects experienced minor effects typical of ephedrine
alkaloids. These effects included tachycardia, anxiety, headache, irritability, insomnia, and loss
of appetite (frequency not reported). The study results indicated that when ephedrine was
supplied as ephedra extract in combination with other botanicals, the absorption and disposition
characteristics were similar to those observed for a single-ingredient ephedrine capsule. When
compared with the results of previously published studies, it appears that the administration of
ephedra extract, in combination with other botanicals and stimulants, has little bearing on the
distribution and elimination of ephedrine (Gurley et al., 1998a). Gender comparison between
Vss/F and CL/f revealed a trend toward larger values for the female subjects for all products;
however, the difference was not statistically significant. Results are summarized in Table 2.4.11.
Table 2.4.1-1
Elimination Kinetics of Ephedrine after Ingestion (Gurley et al.,
1998a)
Dose (mg)
of
ephedrine
Ka (hr-1)
Vss/F
CL/F
(l/hr)
tmax (hr)
Cmax
(ng/ml)
AUC 0-
(ng/hrml)
t1/2
Ephedrine
HCL
capsules
25
1.16
(1.03)
218.8
(71.5)
28.5
(5.92)
2.81
(1.35)
86.5
(15.4)
908.6
(182.5)
5.37
(1.67)
“Escalation”
27
1.67
(1.34)
231.2
(71.5)
25.5
(4.79)
2.68
(1.03)
100.1
(25.5)
1133.5
(231.6)
6.47
(2.26)
“Excel”
25.6
1.45
(1.45)
229.0
(64.2)
33.9
(10.1)
2.61
(0.77)
86.2
(22.5)
827.7
(242.6)
4.93
(1.58)
“Up Your
Gas”
23.6
0.97
(0.53)
239.1
(66.5)
34.1
(8.24)
3.05
(0.84)
73.4
(20.3)
746.1
(208.1)
4.85
(0.79)
Product
mean +/- SD
The pharmacokinetics of ma huang at doses recommended by package labeling in normotensive
adults were evaluated (White et al., 1997). In addition, the study authors measured the
variability of ephedrine and pseudoephedrine content among capsules of the same lot to
determine the agreement among stated doses. Twelve normotensive volunteers, 6 women and 6
men, participated in the study. All participants were nonsmokers and were classified as
normotensive based on mean systolic and diastolic blood pressures. Participants were not taking
any other medications known to cause changes in blood pressure or heart rate. In Phase I (control
phase), all participants underwent ambulatory blood pressure monitoring every 15 minutes from
7 am until 8 pm In Phase II (treatment phase), the participants again wore the ambulatory blood
Council for Responsible Nutrition
December 19, 2000
10
pressure monitor for the same time period. At 8 hours, each participant ingested 4 capsules of a
powdered ma huang product. At 17 hours, participants ingested another 4 capsules with their
evening meals. Caffeine intake was also monitored to ensure that it remained consistent from
Phase I to Phase II. Study participants were moderately mobile but stayed on site during the
study. Pharmacokinetic parameters of ephedrine were determined from plasma concentrationtime profiles. The daily dose was 2 doses of 4 capsules each which administered a daily dose of
38.8 mg ephedrine/day. The ephedrine alkaloid content of each dose (4 capsules labeled 375 mg
E. sinica)was determined by HPLC to be 19.4 mg ephedrine, 4.9 mg pseudoephedrine and 1.2
mg methylephedrine. The data in Table 2.4.1-2 demonstrate that elimination kinetics of
ephedrine after ingestion of ma huang were similar to those from an immediate-release tablet and
an oral solution in terms of T1/2, CL/F and Vss/F. For comparative purposes, data from Pickup
et al. (1976) were presented. The pharmacokinetics of ephedrine after administration of 20 mg
immediate-release tablet and an oral solution (a dose similar to that administered in this study)
were also presented. The administered doses were similar, demographics of participant
population were similar, and ephedrine was taken with a meal of similar composition.
Absorption kinetics of ephedrine, however, were dramatically different for ma huang. A
comparison of Ka and Tmax values indicated that ephedrine was absorbed much slower when
administered as powdered ma huang herb. Despite the slower absorption rate, the onset and
extent of absorption of ephedrine evident in Tlag, AUC and Cmax values did not differ
significantly (White et al., 1997).
Table 2.4.1-2
Parameter
Summary of Ephedrine Pharmacokinetics in Man
Pickup et al., 1976
Pickup et al., 1976
White et al., 1997
Gurley et al., 1998a
Dose
22 mg solution
20 mg tablet
19.4 mg capsule
containing
powdered
ephedrine
25 mg ephedrine
HCL capsule
Route
oral
oral
oral
oral
Ka (absorption rate
constant)
2.35
1.73
0.49
1.16
Tlag lag time
0.18
0.38
0.25
AUC (ng·hr/ml)
814
638
798
908.6
T1/2
6.75
5.74
5.2
5.37
Vss/F (L) apparent
volume of distribution
at steady state
215.6
213.7
182.3
218.8
Council for Responsible Nutrition
December 19, 2000
11
Table 2.4.1-2
Parameter
a
b
Summary of Ephedrine Pharmacokinetics in Man
Pickup et al., 1976
Pickup et al., 1976
White et al., 1997
Gurley et al., 1998a
Cl/F apparent
clearance
23.3
28.7
24.3
28.5
Cmax ng/ml
79.4
73.9
81
86.5
Tmax (hr)
1.81
1.69
3.9
2.81
Bioavailability
100%
NR
NR
NR
Plasma protein
binding, total (%)
NR
NR
NR
NR
Excretion: urine
55-75%
55-75%
NR
NR
Not reported.
single 24 mg dose (Baselt .,1982a)
In contrast to the results from Gurley et al. (1998a) which showed no difference using ephedra
extracts, the absorption rate of ephedrine appears to be slowed for ephedra herb (Tmax of almost 4
hours) compared to only 2 hours for pure ephedrine was given. Peak plasma concentration and
the areas under the time-concentration curves were similar for both types of products which
would indicate pharmacodynamics would be similar for ephedrine in dietary supplements which
are botanically derived versus manufactured from synthetic sources. The particle size of the herb
preparation was not specified but might have had an effect on the intestinal dissolution and
absorption.
The pharmacokinetics of ephedrine were investigated in healthy female volunteers before and
after exercise (Strömberg et al., 1992). Before entering the study, the subjects were ascertained
to be healthy by a clinical examination, including resting ECG and maximal exercise test on a
treadmill. All subjects were regularly engaged in physical activity, but none of them participated
in competitive sports. The subjects received single doses of 50 mg ephedrine or placebo. All
treatments were given twice; before exercise (control session) and during exercise. Relevant
safety/tolerability assessments included heart rate, blood pressure, critical flicker fusion
frequency which measures sedative effects of psychotropic drugs, Maddox wing test used to
measure external eye muscle balance, visual analog scales relating to mood and feelings of
tiredness were included in the sessions as pharmacodynamic measures. The pharmacokinetics of
ephedrine were not altered by exercise. Ephedrine increased heart rate and systolic blood
pressure 2 hours after administration. It was reported that the heart rate response was even
higher after the exercise, whereas exercise abolished the blood pressure response.
Council for Responsible Nutrition
December 19, 2000
12
In a related study, the effects of a sauna on the pharmacokinetics and pharmacodynamics of
ephedrine in healthy young women was investigated (Vanakoski et al., 1993). Six, healthy 21
year-old women of normal weight volunteered for the study. Before entering the trial, they
underwent a physical examination and an ECG. With the exception of one subject, who used
oral contraceptives, the subjects took no medication during the trial and all were non-smokers.
Blood samples were taken for clinical laboratory tests. Each subject received in a double-blind
and cross-over fashion single oral doses of 50 mg ephedrine and placebo for control and sauna
sessions. Relevant safety/tolerability assessments included heart rate; blood pressure; critical
flicker fusion frequency and binocular flicker fusion frequency which measures sedative effects
of psychotropic drugs; Maddox wing test used to measure external eye muscle balance; and
visual analog scales relating to mood and feelings of tiredness were included in the sessions as
pharmacodynamic measures. The sauna modified the pharmacokinetics of ephedrine. Ephedrine
was absorbed more rapidly and the maximum plasma concentration occurred earlier than in the
control sessions; however, no differences were found between the elimination half-lives and
AUC values. Ephedrine did not significantly modify the results of the critical flicker fusion or
Maddox wing tests in test sauna condition or placebo. Increased systolic blood pressure was
observed in both conditions. Systolic blood pressure was significantly higher in the sauna than in
the control session (p<0.01). Subjectively, ephedrine induced alertness and nervousness (0.001 <
p<0.05 vs. placebo) in both conditions. Ephedrine abolished the sauna-induced calmness. The
authors proposed that the greater systolic blood pressure and heart rate in the sauna due to
ephedrine can better be explained by additional sympathetic activity triggered by greater heat
stress than by increased ephedrine concentration. Increased effects on cardiovascular parameters
suggest a pharmacodynamic interaction and also that the effects of sympathomimetics may be
more marked in a sauna.
In another study, the pharmacokinetics of ephedrine following acute and repeated treatment were
evaluated (Costello et al., 1975). Ten asthmatic volunteers were selected (criteria for selection
were not reported). Plasma levels occurring in patients given ephedrine alone or Franol®, a
tablet containing 11 mg of ephedrine, 120 mg theophylline and 8 mg phenobarbitone for the
treatment of asthma were measured. Ephedrine plasma levels were measured on Day 1 (at 22
mg) and after 2 weeks of 11 mg 3 times a day. Pharmacokinetic assessment indicated no
significant intrasubject changes in kinetic parameters with repeated treatment. In addition, no
change was observed between ephedrine given alone or in combination with theophylline or
phenobarbitone.
Council for Responsible Nutrition
December 19, 2000
13
2.5
Pharmacology of Ephedra and Ephedrine
The pharmacology of ephedra is dependent upon its chemical composition. The two main active
components of ephedra are ephedrine and pseudoephedrine, which are prototypical
sympathomimetic agents which have alpha and beta adrenergic activity (Hoffman and Lefkowitz,
1996). Both products are weak bases and act like phenylpropanolamine, stimulating adrenergic
receptors as well as releasing norepinephrine. Pseudoephedrine’s activity is similar to ephedrine,
but the hypertensive effects and stimulation of the central nervous system are somewhat weaker.
In general, all the alkaloids contained in ephedra show significant differences with regard to
pharmacokinetic and pharmacodynamic effects. All have effects on the cardiovascular and
respiratory system, but not to the same degree.
The pharmacological effect of ephedra is associated with the presence of ephedrine which occurs
at high concentrations compared to other alkaloids. The pharmacology of ephedra or its extracts
cannot be accounted for solely by the pharmacology of ephedrine; however, ephedrine itself is
responsible for a major portion of the activities attributed to ephedra.
In particular, the pharmacological activity of ephedrine is due to indirect adrenergic stimulation
by releasing the neurotransmitters norepinephrine and dopamine from neuronal storage sites in
the sympathetic nerves and direct action on alpha and beta postsynaptic receptors at effector
organs. Therapeutic doses of ephedrine typically result in respiratory bronchodilatation, cardiac
stimulation, and an elevation of systolic and diastolic blood pressure. Ephedrine and
pseudoephedrine also result in central nervous system stimulation, relaxation of gastrointestinal
smooth muscle tone, urinary retention, and can cause mydriasis (with no affect on the light
reflex) (Boston, 1928; Hoffman and Lefkowitz, 1996). Ephedrine exhibits substantial effects in
reserpine-treated animals and man. Tachyphylaxis occurs due to depletion of neurotransmitter
from storage sites.
Current promoted uses of ephedrine in a prescription/hospital setting include intravenous
ephedrine for the prophylaxis and treatment of hypotension resulting from spinal anesthesia in
caesarian section (Yap et al., 1998) as well as in initial treatment of hemorrhagic shock (Eldor,
1991). Ephedrine (as the hydrochloride salt, sulfate or tannate) is included as a component of
prescription asthma and cough medications, although ephedrine use has been largely replaced by
more selective beta2-bronchodilators. In the past, ephedrine was used to treat Stokes-Adams
attacks and was also recommended as a treatment for narcolepsy (Pomerantz and O’Rourke,
1969). Ephedrine can also be found in over-the-counter cold remedies for the treatment of acute
Council for Responsible Nutrition
December 19, 2000
14
congestion of rhinitis, sinusitis, and rhinopharyngitis. An area of interest for ephedrine use is
weight loss which has been investigated by European researchers (Astrup et al.,1992; Quaade et
al., 1992; Toubro et al. 1993a,b).
2.5.1
Clinical Pharmacology - Cardiovascular Activity
Ephedrine can stimulate heart rate, as well as cardiac output, and increase peripheral resistance,
thereby producing a lasting rise in blood pressure. The cardiovascular effects of ephedrine can
persist up to 10 times as long as that of epinephrine (Hoffman and Lefkowitz, 1996).
Cardiovascular responses to ephedrine have been reported to be variable. In some cases, arterial
blood pressure is not elevated and the peripheral resistance has been reported as increased,
decreased or unchanged. In humans, a single oral 25 mg dose of ephedrine (as hydrochloride
salt) has been shown to increase heart rate and systolic blood pressure and reduce diastolic blood
pressure without significant effects on psychomotor performance (Nuotto, 1983). A dose of 60
to 90 mg of ephedrine (as hydrochloride salt) was required to produce a diastolic blood pressure
of 90 mm Hg or above in healthy volunteers in a dose-ranging study using 30 to 90 mg
ephedrine. The greatest change in heart rate found in this study was 12 beats per minute after a
90 mg dose (Drew et al., 1978). Cetaruk and Aaron (1994) reviewed ephedrine data and reported
that significant increases in blood pressure were seen at two to three times the recommended
dose of 15 to 30 mg. In a review of the literature, Chau and Benrimoj (1988) summarized the
findings of several single oral dose studies in normotensive subjects. McLaurin et al. (1961) and
Laitinen et al. (1982) found 25 mg of ephedrine produced no significant effect on blood pressure
and heart rate of normotensive patients. Tashkin et al. (1975) obtained similar results when
comparing the cardiovascular and bronchial effects of terbulatine with ephedrine. In another
study, Bye et al. (1974) demonstrated a significant rise in systolic blood pressure of 7 mm Hg
and 17 mm Hg with 25 mg and 50 mg of ephedrine, respectively, but no effect on diastolic blood
pressure. The discrepancy between the different results with respect to cardiovascular effects
was attributed to study methodology with respect to parameters analyzed and the time intervals
assessed (Chau and Benrimoj, 1988). Furthermore, in a review by Karch (2000), doses of 50 mg
or less did not cause predictable increases in blood pressure, although modest increases in pulse
rate may be observed (Wilkinson and Beckett, 1968a,b; White et al., 1997; Waluga et al., 1998).
The therapeutic dose for treatment of bronchodilation, nasal decongestant is 15 to 60 mg
ephedrine given 3 times daily (Dollery, 1991a). Ephedrine toxicity is characterized by
overstimulation of the adrenergic system. The major cardiovascular toxicities are hypertension
and tachydysrhythmias (Tang, 1996).
Council for Responsible Nutrition
December 19, 2000
15
2.5.2
Clinical Pharmacology - Central Nervous System Activity
Ephedrine is a potent stimulator of the central nervous system. The effects of the compound may
last for several hours after oral administration. Due to this long-lasting effect, preparations
containing ephedrine have been promoted for use in weight reduction and thermogenesis, or fat
burning (Astrup et al., 1985; Astrup and Toubro, 1993; Daly et al., 1993). Other effects include
mydriasis after local application of 3 to 5% solutions of ephedrine to the eyes. Ephedrine also
stimulates the alpha-adrenoceptors of the smooth muscle cells of the bladder base, which
increases the resistance to the outflow of urine. In the past, it has been used to promote urinary
continence. Ephedrine toxicity in the CNS is manifested by overstimulation of the adrenergic
system, which could result in headache, anxiety, insomnia, restlessness, psychosis, and seizures.
Additional symptoms of toxicity include giddiness, nausea, vomiting, sweating and thirst,
palpitations, difficulty in micturition, muscular weakness, and tremors (Pentel, 1984).
Significant, but mild, stimulation of the human central nervous system occurs following a 50 mg
oral dose, as assessed by increased tapping rates and ability of subjects to detect that they had
received an active compound (Bye et al., 1974).
2.5.3
Clinical Pharmacology - Respiratory System Activity
Ephedrine relaxes bronchial muscles and is a potent bronchodilator owing its activation to betaadrenoceptors in the lungs (Hoffman and Lefkowitz, 1996). Ephedrine, like other
sympathomimetics with alpha-receptor activity, causes vasoconstriction and blanching when
applied topically to nasal and pharyngeal muscosal surfaces. Oral doses also produce similar
effects.
Ephedrine produces a significant increase in specific airway conductance one hour after
administration of a 25 mg dose to patients with obstructive airways disease. The significant
brochodilatory effect was maintained over 4 hours. Mean heart rate was significantly raised at 2
to 5 hours (Tashkin et al., 1975).
2.5.4
Clinical Pharmacology - Sensitive Populations and Drug Interactions
Ephedrine and related agents should not be administered to individuals with coronary
thrombosis, diabetes, glaucoma, heart disease, hypertension, thyroid disease, impaired circulation
of the cerebrum, autonomic insufficiency, pheochromocytoma, chronic anxiety/ psychiatric
Council for Responsible Nutrition
December 19, 2000
16
disorders or enlarged prostate (Dollery, 1991a; Hoffman and Lefkowitz, 1996). Patients with
renal impairment may be at special risk for toxicity. Co-administration of ephedrine-containing
preparations, including ephedra products with monoamine oxidase inhibitors is contraindicated
as the combination may cause severe, possibly fatal, hypertension (Hoffman and Lefkowitz,
1996). Also, ephedra supplements and ephedrine alkaloid drugs should not be co-administered
because of the summation of total intake.
The duration and magnitude of ephedrine activity are known to be affected by antacids and
agents which alter the pH of urine thus affecting absorption and excretion, respectively.
Ephedrine is also known to interact with corticosteroids and theophylline (Upton, 1991).
Alcohol may be expected to antagonize the central stimulant effects of ephedrine (Dollery,
1991a).
Other risk groups may include neonates and breast-fed infants secondary to maternal exposure,
pregnant women, children and the elderly. These groups are potentially at risk because of their
known increased sensitivity to the effects of sympathomimetic stimulation and because the
potential effects of ephedrine and related compounds in these populations have not been wellstudied. Placental transfer of ephedrine occurs, resulting in fetal blood levels of 70% of the
maternal blood levels. Ephedrine is also excreted in breast milk. No clinical studies have been
conducted with ephedrine in pregnant or nursing mothers. In the clinical literature, fetal
tachycardia has been associated with maternal use of a related alkaloid, pseudoephedrine, and the
administration of intramuscular ephedrine to treat maternal hypotension resulted in increases in
fetal heart rate and beat-to-beat variability (Anastario and Haston, 1992). Toxicity has been
reported in a breast-fed infant, whose mother had been prescribed a long acting oral decongestant
containing d-isoephedrine and dexbrompheniramine for allergic rhinitis (Mortimer, 1977).
Other possible drug interactions have been speculated. Caffeine has been shown to increase the
absorption rate of ASA (Yoovathaworn et al., 1986); however, in an evaluation of the effects of
caffeine on the absorption rate of phenylpropanolamine, a structurally-related ephedrine alkaloid,
the findings were inconclusive (Brown et al., 1991). Phenylpropanolamine can be found in
ephedra, but only in very small amounts.
2.6
Characterization of Dietary Supplements Containing Ephedra
Most ephedra product labels indicate how much ephedra herb or extract is contained in each
dosage form; however, not all make a claim of ephedrine alkaloid(s) content. It was recently
Council for Responsible Nutrition
December 19, 2000
17
reported that ephedrine alkaloid content varied by as much as 5-fold between commercially
available ma huang products, with brands exhibiting lot-to-lot differences in from 44% - 260%
(Gurley et al.,1997b, 1998b, 2000). This natural inconsistency gives rise to commercial products
with significant interproduct and intraproduct variability (Betz et al., 1997; Gurley et al.,
1997a,b, 2000). The test material in a recent ephedra clinical trial (Boozer et al., 1997) contained
90 mg ephedrine alkaloids with ephedrine and pseudoephedrine in a 2:1 ratio accounting for 9698 percent of the ephedrine alkaloid content. Norephedrine (phenylpropanolamine, or PPA)
content was less than 1.8 mg per 90 mg of ephedrine alkaloid.
Products containing ephedra or ephedra extracts, alone or in combination with other ingredients,
are marketed as dietary supplements in the United States. In these products, kola nut, guarana,
and other botanicals are used as natural caffeine sources. Willow bark is used as a natural source
of salicylates. The pharmacology of most of the individual ephedrine-type alkaloids has been
well characterized, but the effects of combinations of these other compounds are less well
known. In addition, interactions between ephedrine-type alkaloids and xanthine alkaloids, as
well as biologically active compounds in other plant species that are constituents of many dietary
supplements, have yet to be fully examined. The possibility of effects contributed by other
agents, such as caffeine, should be considered since they are often a major component of herbal
preparations at far greater concentrations than the ephedrine alkaloids. In addition to caffeine,
dietary supplements can contain mixtures of other products such as chromium picolinate, St.
John’s Wort, White Willow bark, diuretics, or cathartics. Investigators have found that
concomitant ingestion of other botanicals and stimulants can affect the pharmacokinetic profile
of ephedrine (Shenfield, 1982; Upton, 1991; Kanfer et al., 1993). Reactions to ephedrine-type
alkaloid combinations have been reported (Lake et al., 1990a,b).
In a recent survey conducted by Arthur Andersen for the American Herbal Products Association
(AHPA), information regarding the number of servings sold, the number of serious adverse
events reported and other information for products containing ephedra were compiled from
companies that sold dietary supplements containing ephedrine alkaloids (AHPA, 2000). Arthur
Andersen mailed the survey to 42 companies who were known companies in the industry that
distribute dietary supplements containing ephedrine alkaloids and whose products were listed in
the FDA’s Initial Adverse Events Report. Both members and non-members of AHPA were
solicited. Of the 42 companies solicited, Arthur Andersen received responses from 14
companies which represents a response rate of 33%. Since this survey is based on findings from
14 companies, the conclusions may not be representative of the entire ephedra industry; however,
Council for Responsible Nutrition
December 19, 2000
18
this survey does provide good data on information related to number of products sold, adverse
events reported to these manufacturers, labeling and manufacturing methods.
All manufacturers reported that they have a system for collecting reports of serious adverse
events related to the consumption of their products containing ephedrine alkaloids. Furthermore,
all respondents include a cautionary statement on products containing ephedrine alkaloids, which
includes contraindicated populations, use instructions, and age restrictions (1 respondent does not
state age restriction). Aggregate number of servings sold from 13 of the 14 companies (1
company declined to respond) was 3,086,041,072 in 1999. The aggregate number of reported
“serious adverse events” from the firms was 25 in 1999; thus the number of reported events per
million servings sold is 0.0081. All products were reported to be manufactured by GMP which
includes lot identification and use of outside laboratories to test amount of ephedrine alkaloids in
the finished product. None of the respondents includes any synthetic ephedrine as an ingredient
in any of their products. The amount of ephedrine alkaloids contained in the product is declared
on the label by all the respondents.
The clinical database that has been considered involved administration of ephedra, ephedrine
singly, or in combination with other components such as caffeine or ASA-containing ingredients.
Since many dietary supplements which contain ephedra often contain other ingredients such as
botanicals, including these data in the safety assessment of ephedra is relevant especially given
that these other ingredients are major components of ephedra preparations. The pharmacology of
most of the individual ephedrine-type alkaloids has been well characterized, but the effects of
combinations of these other compounds are less well known. In addition, interactions between
ephedrine-type alkaloids and xanthine alkaloids, as well as biologically active compounds in
other plant species that are constituents of many dietary supplements, have yet to be fully
characterized. The assessment of ephedrine together with other ingredients is expected to
provide a more conservative assessment of the safety of ephedra, as it is assumed that the safety
profile would not improve with the addition of other ingredients. The assumption is made that a
combination product (i.e., ephedrine alkaloid together with caffeine) would be no more or less
active than an equivalent dose of the ephedrine alkaloids singly. Since combination products
were given in many of the clinical studies, this report evaluates the contribution/interaction of
other ingredients typically contained in many ephedra preparations, insofar as they contribute to
the analysis of the effects of ephedrine alkaloids.
Council for Responsible Nutrition
December 19, 2000
19
3.0
ANIMAL TOXICOLOGICAL STUDIES ON EPHEDRA AND
EPHEDRINE ALKALOIDS
In the determination of the probable safe doses of chemicals to which humans can safely be
exposed, animal toxicology data are relied upon in the absence of relevant clinical information.
In the absence of clinical data, the determination of a safe limit of exposure usually involves the
application of large safety factors, or uncertainty factors, to account, in part, for the fact that
inter-species extrapolation is required (i.e., the doses in chronic animal studies, expressed as the
dose per kilogram of body weight, that produce no observed effects can be divided by, for
example, 100 to estimate the acceptable UL in the human population). The 100-fold factor is
based on historical use of 10-fold for inter-species extrapolation, and 10-fold for variability in
sensitivity amongst individuals, rather than empirical data. However, depending upon the nature
and quality of available clinical, epidemiology and case-report data and non-clinical data can be
used to support conclusions on safe ULs of exposure derived from clinical databases (WHO,
1987). In such cases, it is not necessary to apply large, if any, safety or uncertainty factors to
animal data.
The nonclinical toxicology of ephedrine was reviewed to assess its consistency with data
obtained from clinical studies. Furthermore, since the metabolic data in humans and animals
show adequate similarity, the assessment of animal species is relevant for supporting human
safety. Where available, data related to ephedra are discussed; however, there are only limited
data, so information available related to the safety of ephedrine must be relied upon.
3.1
Acute Studies
The objectives of acute toxicity testing are to define the intrinsic toxicity of the chemical,
determine the most susceptible species, identify target organs, provide information for risk
assessment of acute exposure to the chemical, and provide information for the design and
selection of dose levels for longer term studies. A well-designed acute toxicity study includes
consideration of the dose-response relationship of both lethal and nonlethal parameters.
Twelve published studies are available in which the effects of acute administration of ephedrine
or ephedra extracts, via several different routes of administration and under different
experimental conditions, have been examined. A range of LD50 values have been reported for
various species and routes of administration. These studies are summarized by species in Table
3.1-1, and certain studies are described in more details in the following pages.
Council for Responsible Nutrition
December 19, 2000
20
Table 3.1-1
Species
Summary of the Results of Acute Toxicity Studies Performed on
Ephedrine
Route of Exposure, Doses Tested
and Composition of Test Material
Duration
(hours)
Results
Reference
Mice (strain
not specified)
-subcutaneous and oral
-doses not specified and details not
provided
-ephedrine isolated from ephedra
sinica Staph
not
specified
LD50: 1 - 1.4 g/kg
Ueng et al., 1997
Mice (ICR)
-oral (gavage)
-doses tested: 2.25, 3.38, 5.07, 7.61,
or 11.47 g/kg
-ephedra extract
24 hr
LD50: 5.30 g/kg (as
extract)
LD50: 24.0 g/kg (as
crude ephedra)
Minamatsu et al.,
1991
Mice (ICR)
-oral (gavage)
-doses tested: 335, 482, 694, 1,000,
1,440, 2,074 mg/kg
-ephedrine hydrochloride
24 hr
LD50: 841 mg/kg
(hydrochloride)
LD50: 689 mg/kg (as
free base)
Minamatsu et al.,
1991
Mice (B6C3F1)
-oral (gavage )
-doses tested at 125, 250, 500,
1,000, or 2,000 mg/kg
-ephedrine sulfate
24 hr
LD50: males = 812
mg/kg
LD50: females = 1,072
mg/kg
NTP, 1986
Mice (strain
not specified)
-intraperitoneal injection
-doses not specified
-Ephedra gerardiana Wall. ex
Staph
not
specified
LD50: 681 mg/kg
Aswal et al.,
1984
Mice (strain
not specified)
-oral (gavage)
-doses tested at 0, 1,000, 2,000,
3,000, 4,000 or 5,000 mg/kg
-ephedra herb extract
24 hr
LD50 for males: 4,350
mg/kg
LD50 for females:
5,000 mg/kg
[Japanese], 1978
Mice (male
MNRI)
-intravenous injection
-dose not specified
-ephedrine hydrochloride
24 hr
LD50: 74 mg/kg
Marvola, 1976
Mice (Albino Swiss)
-intraperitoneal injection
-doses tested at 165, 205, or 250
mg/kg
-l-ephedrine and d-ephedrine
24 hr
ED50: 44 mg/kg
LD50: d-ephedrine:
244 mg/kg
LD50: l-ephedrine: 246
mg/kg
Fairchild and
Alles, 1967
MICE
Council for Responsible Nutrition
December 19, 2000
21
Table 3.1-1
Summary of the Results of Acute Toxicity Studies Performed on
Ephedrine
Species
Route of Exposure, Doses Tested
and Composition of Test Material
Duration
(hours)
Results
Reference
Mice (male
SwissWebster)
-intraperitoneal injection at various
temperatures
-ephedrine sulfate
24 hr
LD50: group housed
18C: 360 mg/kg
22C: 350 mg/kg
26C: 357 mg/kg
30C: 55 mg/kg
34C: 13.5 mg/kg
LD50: individually
housed
18C: 325 mg/kg
22C: 385 mg/kg
26C: 380 mg/kg
30C: 273 mg/kg
34C: 14 mg/kg
Peterson and
Hardinge, 1967
Mice (strain
not specified)
-intraperitoneal injection
-dose not specified
-ephedrine hydrochloride
not
specified
LD50: 340 mg/kg
Grunberg et al.,
1949
Mice (strain
not specified)
-intravenous injection
-dose not specified
-ephedrine hydrochloride
not
specified
LD50: 95 mg/kg
Grunberg et al.,
1949
Mice (Swiss)
-subcutaneous injection
-dose not specified
-ephedrine hydrochloride
2-week
observed
period
LD50: 600 mg/kg
Warren and
Werner, 1945a
Rats (F344/N)
-oral (gavage )
-doses at 75,150, 200, 600 or 1,200
mg/kg
-ephedrine sulfate
24 hr
LD50 not determined
Deaths occurred in all
dose groups
NTP, 1986
Rats (strain not
specified)
-oral (details not specified)
-dose not specified
24 hr
LD50 : 600 mg/kg
NIOSH, 1997
Rats (strain not
specified)
-oral (gavage)
-doses tested at 0, 500, 1000, 2000,
or 4000 mg/kg
-ephedra herb extract
24 hr
LD50 for males:4,000
mg/kg
LD50 for females:
3,500 mg/kg
[Japanese],1978
Rats (strain not
specified)
-intraperitoneal injection
-dose not specified
-ephedrine hydrochloride
not
specified
LD50: 290 mg/kg
Grunberg et al.,
1949
Rats (strain not
specified)
-subcutaneous injection
-dose not specified
-ephedrine hydrochloride
not
specified
LD50: 1150 mg/kg
Grunberg et al.,
1949
RATS
Council for Responsible Nutrition
December 19, 2000
22
Table 3.1-1
Summary of the Results of Acute Toxicity Studies Performed on
Ephedrine
Species
Route of Exposure, Doses Tested
and Composition of Test Material
Duration
(hours)
Results
Reference
Rat (White strain not
specified)
-subcutaneous injection
-dose not specified
-ephedrine hydrochloride:
24 hr
LD50: 800 mg/kg
Warren and
Werner, 1945b
Rats (Wistar
White -heavy:
300-500g)
-intraperitoneal injection
-dose not specified
-ephedrine hydrochloride
2-week
observed
period
LD50: 165 mg/kg
Warren and
Werner, 1945a
Rats (Wistar
White - light:
190-250 g)
-subcutaneous injection
-dose not specified
-ephedrine hydrochloride
2-week
observed
period
LD50:650 mg/kg
Warren and
Werner, 1945a
Rats (Wistar
White - heavy
300-500 g)
-subcutaneous injection
-dose not specified
-ephedrine hydrochloride
2-week
observed
period
LD50:320 mg/kg
Warren and
Werner, 1945a
Rat (White strain not
specified)
-intravenous injection
-dose not specified
-ephedrine sulfate
24 hr
MLD1: 135-140 mg/kg
body weight/day
Chen, 1925a;
Chen, 1926a
Rabbits (strain
not specified)
-intravenous
-dose not specified
-ephedrine hydrochloride
not
specified
LD50: 65 mg/kg
Grunberg et al.,
1949
New Zealand
White Rabbits
-intravenous injection
-dose not specified
-ephedrine hydrochloride
-2 week
observed
period
LD50: 60 mg/kg
Warren and
Werner, 1945a
New Zealand
White rabbits
-intramuscular injection
-dose not specified
-ephedrine hydrochloride
2 week
LD50: 175 mg/kg
Warren and
Werner, 1945a
New Zealand
White rabbits
-subcutaneous injection
-dose not specified
-ephedrine hydrochloride
2 week
LD50: 165 mg/kg
Warren and
Werner, 1945a
Rabbits (strain
not specified)
-intravenous injection
-dose not specified
-ephedrine sulfate
24 hr
MLD1: 66-70 mg/kg
body weight/day
Chen, 1925a;
Chen, 1926a
Rabbits (strain
not specified)
-oral
-dose not specified
-ephedrine sulfate
24 hr
MLD1: 590-600 mg/kg
body weight/day
Chen, 1925a;
Chen, 1926a
Rabbits (strain
not specified)
-intramuscular injection
-dose not specified
-ephedrine sulfate
24 hr
MLD1: 340 mg/kg
body weight/day
Chen, 1925a;
Chen, 1926a
RABBITS
Council for Responsible Nutrition
December 19, 2000
23
Table 3.1-1
Summary of the Results of Acute Toxicity Studies Performed on
Ephedrine
Species
Route of Exposure, Doses Tested
and Composition of Test Material
Duration
(hours)
Results
Reference
Rabbits (strain
not specified)
-subcutaneous injection
-dose not specified
-ephedrine sulfate
24 hr
MLD1: 320-360 mg/kg
body weight/day
Chen, 1925a;
Chen, 1926a
Rabbits (strain
not specified)
-intraperitoneal injection
-dose not specified
-ephedrine sulfate
24 hr
MLD1: 310-390 mg/kg
body weight/day
Chen, 1925a;
Chen, 1926a
-intravenous injection
-dose not specified
-ephedrine sulfate
24 hr
MLD1: 70 mg/body
weight day
Chen, 1925a;
Chen, 1926a
-intravenous injection
-dose not specified
-ephedrine sulfate
24 hr
MLD1: 75 mg body
weight/day
Chen, 1925a;
Chen, 1926a
DOGS
Dogs (breed
not specified)
CATS
Cats (breed not
specified)
MLD = minimum lethal dose
In an overview of the toxicology of commonly used traditional Chinese medicines, Ueng et al.
(1997) reported the LD50 value of ephedrine isolated from Ephedra sinica Staph to be 1 to
1.4 g/kg via subcutaneous or oral routes of administration in mice [strain(s) not specified].
Details on the methodology were not provided since this report was intended to be a toxicology
screen of a number of Chinese traditional medicines.
The acute toxicity of ephedra as a water extract of Ephedrae Herba was compared to the acute
toxicity of ephedrine as hydrochloride (Minamatsu et al., 1991). Groups of 10 male ICR mice
per dose group were tested. The ephedra was extracted in a 20-fold volume of distilled water,
suction filtered and then used for the studies. The contents of the extract measured by HPLC
included 2.27% ephedrine, 2.14% pseudoephedrine and 0.057% norephedrine. The first part of
the study was to evaluate the LD50 of ephedra extract and ephedrine hydrochloride. The second
part of the study was to evaluate the differences in acute toxicity between the 2 different test
articles at their approximate LD50 values. General physical symptoms, body weight gain, food
consumption and water intake were observed for 7 days subsequent to test article administration.
At necropsy on Day 7, liver, lung, heart, spleen, kidney, and testes were isolated and
histopathological examinations were performed.
Council for Responsible Nutrition
December 19, 2000
24
Ephedra extract was given orally via gavage at doses of 2.25, 3.38, 5.07, 7.61, or 11.47 g/kg.
The LD50 determined for ephedra extract was 5.30 g/kg as the extract, and 24.0 g/kg as crude
herb. Ephedrine hydrochloride was given orally via gavage to groups of 10 mice at doses of 335,
482, 694, 1,000, 1,440, or 2,074 mg/kg. The LD50 determined for ephedrine hydrochloride was
841 mg/kg as the hydrochloride and 689 mg/kg as the free base. The ephedrine hydrochloride
also contained pseudoephedrine. The onset of deaths after administration of the ephedra extract
was markedly delayed in comparison with ephedrine. Immediately after administration of
ephedrine, an increase of spontaneous motor activity, rearing, and Straub tail phenomenon were
observed in most cases. Following these symptoms, tremor and/or tonic convulsions were
observed, subsequent to death. These symptoms were also observed with extract administration,
but were milder than those of ephedrine. The markedly delayed onset of deaths may be attributed
to the differences in absorption among ephedrine and ephedra (White et al., 1997).
In Part II of the study, groups of 10 mice were given 4 g of ephedra extract/kg or 520 mg of
ephedrine (as free base)/kg, respectively. The dosages employed were designed to be about 75%
of the calculated LD50 values for these test articles. The symptoms observed at 75% LD50 values
were essentially the same between the 2 groups. The body weight gain, food consumption and
water intake on Day 1 and water intake on Days 2, 3, and 4 were significantly decreased after
administration of ephedrine, but not after the extract. Histopathological changes were mainly
observed in the heart and kidneys. Degenerative lesions in the myocardium were observed after
ephedrine administration but not after ephedra extract administration. More specifically, the
authors observed myocytolysis to necrosis with resorption and reparative fibrosis in the wall and
papillary muscle of the left ventricle. In addition, renal tubular cells showed various stages of
degeneration and hyaline-droplet formation.
These above findings indicated differences between the observed toxicity of the ephedra extract
and of its active ingredient ephedrine in all aspects of the study. The reported LD50 value for
ephedra extract was higher than ephedrine, the general symptoms observed were milder in nature
and time to death was longer than that of ephedrine. More apparent differences between the
toxicity of the extract and ephedrine were indicated in histopathological examinations. Lesions
in the kidneys after treatment with ephedrine revealed reduced renal blood flow as indicated by
degeneration of renal tubular cells which was suggested by the authors to be a reflection of
vasoconstriction on adrenergic synapses. The authors suggested that the necrosis in the
myocardium was due to the sympathomimetic action of ephedrine followed by local ischemia.
Council for Responsible Nutrition
December 19, 2000
25
The National Toxicology Program (NTP) investigated the toxicology of ephedrine sulphate in
single-administration studies in rats and mice (NTP, 1986). Groups of 5 male and 5 female
F344/N rats were administered single doses of ephedrine sulfate in water via gavage at doses of
75, 150, 300, 600, or 1,200 mg/kg. The volume of solution administered was 10 ml/kg body
weight. Rats were fasted for 4 hours before dosing; controls were not used. Animals were
observed 2 times per day for 14 days for general observations. Body weights were measured 2
days before dosing; however, final body weights were not recorded. Necropsy was performed on
any premature deaths before termination of study. No histopathologic evaluations were
conducted.
Findings from the rat study showed that lethality occurred in all dose groups. All but 1 death
occurred on Day 1. Rats that died exhibited hyperkinesia that progressed to convulsive seizures,
ataxia and lethargy. Epistaxis occurred at the 300, 600, and 1,200 mg/kg doses. Mild portalhepatic congestion, mild pulmonary congestion and epistaxis were found in animals that died
before the end of the studies. An LD50 was not determined for this study.
In the mouse study, groups of 5 B6C3F1 mice of each sex were administered single doses of 125,
250, 500, 1,000, or 2,000 mg/kg by oral gavage. The volume of solution administered was 10
ml/kg body weight. Mice were fasted 18 hours before dosing; controls were not used. Animals
were observed 2 times per day for 14 days for general observations. Body weights were
measured 2 days before dosing; however, final body weights were not recorded. A necropsy was
performed on any premature deaths before termination of study. No histopathologic evaluations
were conducted.
Findings from the mouse study showed that all mice that received 2,000 mg/kg and 4/5 males
and 2/5 females that received 1,000 mg/kg were dead by Day 2. Mice that died exhibited
hyperkinesis that progressed to convulsive seizures, ataxia and lethargy. Epistaxis was observed
in mice that received 1,000 or 2,000 mg/kg. Mild portal-hepatic congestion, mild pulmonary
congestion and epistaxis were found in animals that died. The LD50 value that was determined
was 812 mg/kg for males and 1,072 mg/kg for females.
Aswal et al. (1984) screened 294 plant materials for biological activity. It was reported that the
LD50 in mice from intraperitoneal injection for Ephedra gerardiana Wall. ex Staph
(Ephedraceae) was 681 mg/kg. Since this report was a screen, details on methodology of the
acute toxicity study were not reported.
Council for Responsible Nutrition
December 19, 2000
26
The acute oral toxicity of an extract of ephedra herb in rodents (rats and mice - strains not
specified) was assessed ([Japanese], 1978). In the rat study, groups of 10 male and female rats
(strain not specified) were given doses of 0, 500, 1,000, 2,000, 3,000, or 4,000 mg/kg by oral
gavage. The LD50 value determined for male rats was 4,000 mg/kg, and the LD50 for female rats
was determined to be 3,500 mg/kg. In the mouse study, groups of 10 male and female mice
(strain not specified) were given doses of 0, 1,000, 2,000, 3,000, 4,000, or 5,000 mg/kg. The
LD50 determined for male and female mice was 4,350 mg/kg and 5,000 mg/kg, respectively. No
information related to alkaloid content of extract was provided.
Marvola (1976) studied the effect of acetylated derivatives of sympathomimetic amines on the
acute toxicity in mice. Although the focus of the study was to study the effects of O- and Nacetylation, the acute toxicity of ephedrine hydrochloride itself was evaluated for comparison.
Groups of 10 male NMRI strain mice per dose were given a single dose of ephedrine
hydrochloride intravenously (dose levels tested were not specified). The intravenous LD50 of
ephedrine hydrochloride was determined to be 74 mg/kg.
The acute toxicity of ephedrine in mice was evaluated by Fairchild and Alles (1967). Groups of
8 adult male albino mice of the Swiss strain were injected intraperitoneally with normal saline
and placed in holding units for 75 minutes; they were then removed, weighed, given either a
second injection of saline or ephedrine l- or d- form at 200, 252, or 303 mg/kg and returned to
their cages. The LD50 values of the d- and l-ephedrine forms were found to be essentially the
same: the LD50 value for l-ephedrine was 244 mg/kg and the LD50 value for d-ephedrine was 246
mg/kg. The ED50 dose was calculated for l-ephedrine hydrochloride as 44 mg/kg. It is
interesting to note that the different l and d-forms of ephedrine had similar LD50 values.
An acute toxicity study in Swiss-Webster male mice examined the effect of ambient temperature
and housing (group or individual) on the LD50 values for intraperitoneally administered
ephedrine sulfate (Peterson and Hardinge, 1967). Thirty degrees centigrade was determined to be
the temperature at which group housing was first noted to have a significant effect on toxicity
compared with individual housing. The effect of forced exercise on animals housed individually
at this temperature was also examined. When animals were forced to exercise, the LD50 values
dropped from 273 mg/kg to 28 mg/kg. These findings are supported by earlier studies that
showed that ephedrine was 5 to 6 times more toxic in mice housed 10/cage than when they were
housed singly in the same area (Chance, 1946) and similarly reported by Wolf et al. (1964).
Furthermore, Warren and Werner (1945c) reported that raising the environmental temperature of
mice from 26 to 32C lowered the LD50 of l-ephedrine 7.2-fold. These data indicate an
Council for Responsible Nutrition
December 19, 2000
27
involvement of environmental factors in the potency of ephedrine in animals, probably based on
the adrenergic tone of the animals at the time of treatment.
In a screening study, the acute toxicity of ephedrine hydrochloride was determined in mice, rats,
and rabbits by various routes of administration (Grunberg et al., 1949). LD50 values reported for
mice were: intraperitoneal, 340 mg/kg; intravenous, 95 mg/kg. For rats: intraperitoneal, 290
mg/kg; subcutaneous, 1,150 mg/kg and for rabbits: intravenous, 65 mg/kg. Details on study
methodology were not reported.
A comparative analysis of the toxicity of ephedrine hydrochloride via different routes of
administration, weight of animals/age and different species was examined (Warren and Werner,
1945a,b). New Zealand white rabbits, Wistar rats and Swiss mice were used to determine LD50
values. Intravenous injections in rabbits were made into the marginal ear vein. Concentrations
employed were such that doses equivalent to the LD50 were administered every 1 to 2 minutes.
Intramuscular injections in the rabbits were made into the thigh muscles. Subcutaneous
injections in all species were made in the mid-dorsal region. Intraperitoneal injections in rats
were made in order to prevent injection into internal organs. Subcutaneous LD50 values were
reported in mice to be 600 mg/kg and 800 mg/kg in rats. In heavy rats (300 to 500g), the
subcutaneous LD50 was 650 mg/kg vs. in a light rat (190 to 250g) at 320 mg/kg. In rabbits, the
intravenous, intramuscular and subcutaneous LD50 values were reported to be 60, 175, and 165
mg/kg, respectively.
The acute toxicity of ephedrine was tested in a series of species using ephedrine sulphate (Chen,
1925a; 1926a). Measuring the minimum lethal dose (MLD), ephedrine sulphate was injected
intravenously into rabbits, dogs, cats, and white rats (all strains were unspecified), and dose
levels were unspecified. It was reported that death following the MLD dosage was almost
immediate and followed clonic convulsions. In addition, the MLD resulted in an immediate and
permanent fall in blood pressure accompanied by significant decrease of intestinal and kidney
volumes. Sinus rhythm disappeared with the occurrence of bundle-branch block which was
followed by ventricular fibrillation. It was reported that recovery was always complete after
administration of sublethal doses (doses and data not reported). Evaluation of different methods
of administration showed that intravenous injection produced the lowest MLD. Following
intravenous administration, convulsions occurred approximately 1 to 2½ hours after, and death in
2 to 7 hours after initial administration.
Council for Responsible Nutrition
December 19, 2000
28
Summary of Acute Dose Studies
A range of LD50 values were reported for ephedrine as salts, via different routes of administration
and species. Some of the studies could not be assessed due to lack of reporting. Values were
reported in mice via the subcutaneous route (600 mg/kg), oral route (689 to 1,072 mg/kg),
intravenous route (74 to 95 mg/kg), and intraperitoneal route (13 to 681 mg/kg; depending on
environmental conditions). Particular emphasis is placed on studies conducted in mice by the
NTP. Oral LD50 values of 812 mg/kg and 1,072 mg/kg were obtained for males and females,
respectively. In rats, the LD50 ranges were reported as follow: subcutaneous route (320 to 1,150
mg/kg); oral route (600 mg/kg: no LD50 reported by NTP); and intraperitoneal route (165 to 290
mg/kg). In the NTP study, no LD50 value was estimated for ephedrine in rats. The acute toxicity
of the herb was assessed in one mouse study in which the subcutaneous LD50 was 1 to 1.4 g/kg,
whereas oral administration was 5.30 g herb extract/kg and 24 g crude herb/kg. Furthermore, in
a comparative study between ephedra and ephedrine, there was further indication that there is a
difference in toxicity. The LD50 value for ephedra extract was higher than ephedrine when
normalized based on ephedrine content, and the general symptoms observed were milder in
nature and time to death was longer than that of ephedrine. These results highlight the
conservative assumption that ephedrine content be used to characterize effects of ephedra since
the toxicity assessment of ephedrine shows that this approach overestimates the potential toxicity
of ephedra itself.
3.2
Repeated Dose Studies
3.2.1
Short-Term Repeated Dose Studies
Short-term repeated dosing is conducted for a few weeks to screen for potential adverse effects of
a substance, while subchronic toxicity studies are conducted over a longer portion of the average
lifespan of an animal. Many variables associated with the health of the test species are monitored
in these studies, resulting in the ability to detect a variety of adverse effects.
Seven published studies are available in which the effects of repeated oral administration of
ephedrine or ephedra preparations were studied in animals. In particular, the NTP conducted 4
studies on the repeated-dose toxicity of ephedrine sulfate in drinking water and feeding studies.
All studies are summarized in Table 3.2.1-1.
Council for Responsible Nutrition
December 19, 2000
29
Table 3.2.1-1
Summary of Repeated Dose Studies on Ephedrine or Ephedra
Species and
Strain
Route and Dose
Duration
Results
Reference
Rats
(SpragueDawley
males)
-intravenous injection
of 0, 10, 20, or 40
mg/kg
-intravenous injection
of 20 or 40 mg/kg
-l-ephedrine form
-11 days of
test article
administration
-no ephedrine dose-dependent
changes in animal body weights were
observed throughout the course of
repeated compound exposure
-no adverse effects were noted in this
study
Miller et al.,
1998
Monkeys
(strain not
specified)
(comparison
of lean and
obese)
-oral via capsules
hidden in food
-ephedrine (6mg) and
caffeine (50 mg) 3
times /day
- 8-week
treatment
period
-decrease in body weight in obese
animals due to a decrease in body fat
-food intake also reduced in obese
animals
Ramsey et
al., 1998
Mice
(BALB/c)
-ma huang preparation
containing 9% lephedrine
orally via gavage at 80,
800, 4000 or 8,000
mg/day divided into 2
equal doses
-2 weeks of
test article
administration
-LD50 for ma huang was observed at
the highest dose (8,000 mg/kg) or
(4,000 mg/kg given twice per day)
-gastrointestinal bleeding was
observed at the LD50 value
-no changes in liver weight were
observed
-test article was well tolerated at
doses up to 4,000 mg/kg/day
-14-day LD50 for ephedrine was
determined to be 720 mg/kg/day in
mice
Law et al.,
1996
Rats
(F344/N)
-ephedrine sulfate via
drinking water at 0, 75,
150, 300, 600 or 1,000
ppm equivalent to
approximately 0, 15,
25, 50, 75 and 125
mg/kg bw/day in males
and 0, 9, 21, 32, 55 and
79 mg/kg bw/day
-14 days
-no mortality
-no significant changes in mean body
weight
-hyperexcitability in animals at the 3
highest doses groups
-no histology was performed
-no compound-related effects at
necropsy
NTP, 1986
Rats
(F344/N)
-ephedrine sulfate via
dietary admix at 0, 90,
190, 280, 750, or 1,500
ppm equivalent to
approximately in males:
0, 15, 20, 50, 100, and
140 mg/kg bw/day and
in females: 0, 12, 25,
50, 97, and 165 mg/kg
bw/day
-14 days
-final body weight was 10% lower in
the high-dose male group with no
significant differences in female
body weight
-hyperexcitability and rough hair
coats at the top 3 doses
-no histology was performed
-no compound related effects were
observed at necropsy
NTP, 1986
Council for Responsible Nutrition
December 19, 2000
30
Table 3.2.1-1
Summary of Repeated Dose Studies on Ephedrine or Ephedra
Species and
Strain
Route and Dose
Duration
Results
Reference
Mice
(B6C3F1)
-ephedrine sulfate via
drinking water at 0,
312.5, 625, 1,250,
2,500, or 5,000 ppm
equivalent to
approximately in males:
0, 89, 93, 151, 243 and
372 mg/kg bw/day in
males and in females: 0,
62, 112, 149, 184, and
377 mg/kg bw/day
-14 days
-final mean body weight was 12%
lower in males and 5% lower in
females at the top dose
-hyperexcitability, arched back,
rough coat and dehydration at top 3
doses
-no histology was performed
-no compound related effects were
observed at necropsy
NTP, 1986
Mice
(B6C3F1)
-ephedrine sulfate via
dietary admix at 0, 300,
600, 1,250, 2,500, or
5,000 ppm equivalent
to approximately 56,
88, 212, 489, and 968
in males and in females:
57, 102, 252, 573, and
943 mg/kg bw/day
-14 days
-one male and one female at 2,500
died before termination of study
-final body weight was 11% lower in
males and 10% in females at top
dose
-hyperexcitability, arched back,
rough coat and dehydration at top 3
doses
-no histology was performed
-no compound related effects
observed at necropsy
NTP, 1986
Mice
(viable
yellow
obese mice
Avy/a)
-ephedrine sulfate via
diet at 0.1% feed
-39 days
-ephedrine reduced body weight by
19% compared to starting weight
-treated mice ate less than control
mice; however, when a diet-restricted
experiment was conducted, control
animals consuming the same amount
of feed as ephedrine-treated animals
showed no changes in body weight
which indicated that the reduced feed
consumption alone could not account
for all of the weight loss
Yen et al.,
1981
Council for Responsible Nutrition
December 19, 2000
31
Table 3.2.1-1
Summary of Repeated Dose Studies on Ephedrine or Ephedra
Species and
Strain
Route and Dose
Duration
Results
Reference
-normal lean
mice (CBA
strain)
-obese mice
induced by
gold
thioglucose
-obese mice
induced by
MSG
-obese mice
induced by
diet
-genetically
obese mice
(obob)
-obese rats
induced by
diet
-genetically
obese rats
-ephedrine sulfate in
diet at 1 g/kg
- 5-weeks
treatment in
mice
-ephedrine treatment resulted in a
loss in body weight and body fat
without increasing food intake
-elevated oxygen consumption
compared with untreated controls
that consumed the same quantity of
feed
Massoudi
and Miller,
1977
Rabbits
(groups of
10 animals;
strain not
specified)
-intramuscular injection
of 25 mg/day of
ephedrine sulfate
-4 weeks of
test article
administration
(except
Sundays) and
maintained
until Day 140
-Fibrosis at the site of injection,
which disappeared over time after
cessation of daily injections.
-At necropsy, lungs, liver, spleen,
adrenal body, and kidney tissues
were examined. It was reported by
the study authors that no treatmentrelated gross pathology was
observed, and that no demonstrable
abnormality in the structures of these
visceral organs were observed.
Chen,
1925b;
Chen 1926
b
Rabbits
(groups of
10 animals;
strain not
specified)
-oral ingestion of 25
mg/day of ephedrine
sulfate
-4 weeks of
test article
administration
(except
Sundays) and
maintained
until Day 140
-No lesions were observed in the
gastrointestinal tract from
postmortem examination.
-At necropsy, lungs, liver, spleen,
adrenal body, and kidney tissues
were examined. It was reported by
the study authors that no gross
pathology was observed, and that no
demonstrable abnormality in the
structures of these visceral organs
were observed.
-Cloudy swelling of kidneys but
these were common to control
animals.
Chen,
1925b;
Chen 1926
b
- 8-weeks
treatment in
rats
Council for Responsible Nutrition
December 19, 2000
32
Table 3.2.1-1
Summary of Repeated Dose Studies on Ephedrine or Ephedra
Species and
Strain
Route and Dose
Duration
Results
Reference
Rats (strain
not
specified)
-intravenous injection
at 101 mg/kg of
ephedrine sulfate
-not specified
-It was reported that their body
weight was constant or somewhat
decreased 2 to 3 days after the
injection, but in all cases it
subsequently increased.
-No marked pathological lesions
were observed.
Chen,
1925b;
Chen 1926
b
Miller et al. (1998) studied the repeated intravenous administration of ephedrine in rats. The
main focus of the study was the investigation of systemic effects of ephedrine in drug-naive rats;
however, some safety information was also evaluated. Male Sprague-Dawley rats received
injections of 0, 10, 20, or 40 mg/kg l-ephedrine on Day 1 of testing and activity was recorded for
60 minutes. This procedure was repeated for 10 additional days. In experiment II; 20 or 40
mg/kg d-ephedrine was given on Days 1 through 11. No ephedrine dose-dependent changes in
animal body weights were noted through the course of repeated compound exposure. No adverse
effects were reported in the study.
The administration of ephedrine (6 mg) combined with caffeine (50 mg) 3 times a day was
evaluated in lean and obese monkeys studied during an 8-week treatment period (Ramsey et al.,
1998). There were 3 treatment periods, a 7-week control period, an 8-week compound treatment
period, and a 7-week placebo period. A dose of 18 mg/day of ephedrine and 150 mg/day of
caffeine was given in a capsule hidden in a piece of fruit for administration. At the end of each
period, a glucose tolerance test, energy expenditure and body composition were determined.
Treatment with ephedrine and caffeine resulted in a decrease in body weight in obese animals
primarily due to a 19% decrease in body fat. Treatment also resulted in a decrease in body fat in
the lean group. Food intake was only reduced by ephedrine and caffeine in the obese group.
Twenty-four hour energy expenditure was higher in both groups during treatment. The weight
loss was associated with reduced fat, increased energy expenditure and reduced feed intake.
The safety of a concentrated ma huang herbal preparation which contained 9% l-ephedrine was
addressed in a repeated-dose toxicity study in BALB/c mice (Law et al., 1996). Five-week old
male and female mice, (5/sex/dose), were given the herb orally by gavage at 20, 200, 1,000,
2,000, and 4,000 mg/kg twice daily for 2 weeks. Two control groups were used and untreated
animals were gavaged with water. Deaths and any signs of toxicity such as tremors, lethargy,
hunching, ruffled fur, diarrhea and prostration were noted daily, and as they occurred. The
Council for Responsible Nutrition
December 19, 2000
33
animals were sacrificed at the end of the study and necropsied to look for treatment-related organ
abnormalities. The liver weights of the controls and the 2 highest dose levels were also
determined. The lethal dose for 50% of the test animals was observed at the highest dose (4,000
mg/kg twice daily, or 8,000 mg/kg/day total dose), with gastrointestinal bleeding observed upon
necropsy. Similar toxicity findings, but to a lesser degree, were observed in the 2,000 mg/kg
b.i.d. group; however, no significant differences were noted in the liver weights of these animals
when compared to the control group. The sex of the animal did not appear to be a factor among
the groups exhibiting signs of toxicity. The authors concluded that the findings indicated that ma
huang was well tolerated in mice orally, regardless of sex, in doses as high as 2,000 mg/kg twice
daily. From these data, the 14-day LD50 of l-ephedrine in this herbal preparation was determined
to be 360 mg/kg twice daily in mice. The authors further projected LD50 values in a 70 kg human
to be 2.1 grams and 23.3 grams twice daily of l-ephedrine and ma huang, respectively based on
surface area differences. These LD50 values greatly exceed normal and traditional usages.
The NTP investigated the toxicology of ephedrine sulphate in 4 rodent 14-day studies (NTP,
1986). Ephedrine sulfate was administered via drinking water or in the feed of both rats and
mice.
Groups of 5 F344/N rats of each sex were given drinking water containing 0, 75, 150, 300, 600,
or 1,000 ppm ephedrine sulfate, which is equivalent to approximately 0, 13, 25, 50, 75, and 120
mg/kg body weight/day in males, and 0, 9, 21, 32, 55, and 80 in females, based on mean body
weights and mean water consumption. In the feed study, groups of 5 rats of each sex were fed
diets containing 0, 90, 190, 280, 750, or 1,500 ppm ephedrine sulfate, which is equivalent to
approximately 0, 15, 29, 55, 100, or 140 mg/kg body weight/day in males, and 0, 12, 25, 50, 100,
or 165 mg/kg body weight/day in females, based on mean body weight and mean feed
consumption. The experimental design in both the feed study and drinking water study were
similar. The rats were approximately 8 weeks old upon commencement of the study. Rats were
observed twice per day and were weighed on Days 1 ( weighed on Day 7 for water study only and
15). Water consumption or feed consumption (depending on study) were measured weekly. The
period of chemical exposure was 14 consecutive days followed by 1 day of observation before
the scheduled necropsy. Blood for the determination of packed cell volume was taken from the
external jugular vein at the scheduled kill. Necropsy was performed on all animals, and 10% of
the animals were examined histologically.
In the drinking water study, there was no mortality reported before the end of the study. The
final mean body weights were not significantly altered by ephedrine sulfate treatment. Average
Council for Responsible Nutrition
December 19, 2000
34
water consumption decreased with increasing dose. Water consumption by male rats that
received 1,200 ppm was 50% that of the controls. Water consumption by female rats that
received 1,200 ppm was 25% that of the controls. Hyperexcitability was observed for animals
that received the 3 highest doses, and dehydration was observed for rats that received 600 or
1,200 ppm. The mean packed cell volume of female rats that received 1,200 ppm was 8% lower
than that of the controls and was statistically significant. It was reported that there were no
compound-related effects observed at necropsy or during the limited histological examinations.
In the feed study, there was no mortality reported before the end of the study. Final mean body
weights of high-dose males (1,500 ppm) were 10% lower than that of the controls. Final mean
body weights of treated females were not statistically different from controls. Feed consumption
by rats that were given diets containing 1,500 ppm ephedrine sulfate was 76% that of controls for
males and 87% for females. Hyperexcitability and rough hair coats were observed in rats that
received 380, 750, or 1,500 ppm. The mean packed cell volume was not affected by ephedrine
sulfate. It was reported that there were no compound-related effects observed at necropsy or
during the limited histological examinations.
In the mouse studies, groups of five B6C3F1 mice of each sex were given drinking water
containing 0, 312.5, 625, 1,250, 2,500, or 5,000 ppm of ephedrine sulfate. In the feed study,
groups of 5 mice of each sex were fed diets containing 0, 300, 600, 1,250, 2,500 or 5,000 ppm.
The experimental design in both the feed study and water study were similar. In both the feed
study and water study, the mice were approximately 8 weeks old upon commencement of study.
Mice were observed twice per day and were weighed on Days 1 ( weighed on Day 7 for water
study only) and 15. Water consumption or feed consumption (depending on study) was
measured weekly. The period of chemical exposure was 14 consecutive days followed by 1 day
of observation before the scheduled necropsy. Blood for the determination of packed cell
volume was taken from the external jugular vein at the scheduled kill. Necropsy was performed
on all animals, and 10% of the animals were examined histologically.
In the drinking water study, none of the mice died before the end of the study. Final mean body
weights of mice in the 5,000 ppm group were 12% lower than those of the controls for males and
5% lower for females. Mean water consumption was lower than that of the controls for all but
the lowest dose group of males and for all treated groups of females. Compound-related clinical
signs were hyperexcitability, arched backs, rough hair coats, and dehydration. Cachexia was
observed at 5,000 ppm. No compound-related gross lesions were observed at necropsy or in the
Council for Responsible Nutrition
December 19, 2000
35
limited histological examinations. Mean packed cell volume of males and females that received
5,000 ppm were 22% and 16% lower than those of the controls.
In the feed studies, one male and one female that received 2,500 ppm died before the end of the
studies on Days 3 and 2 of test article administration. There was no elaboration on the pathology
of these animals. Final mean body weights of mice that received 5,000 ppm were 11% lower
than those of the controls for males and 10% lower for females. Feed consumption was not
adversely affected by ephedrine sulfate. Hyperactivity, rough hair coats, dehydration and arched
backs were observed in both sexes at the 3 highest doses. No compound-related clinical signs
were observed at 300 or 600 ppm. No compound-related effects were observed at necropsy or in
the limited histological examinations. It was reported that mean packed cell volume was not
notably affected by administration of ephedrine sulfate.
Overall, the 14-day NTP studies determined that administration via drinking water was not a
suitable means for test-article administration. Mean water consumption was significantly
reduced at higher concentrations of ephedrine sulfate. Since reduced water consumption would
limit the amount of chemical ingested and could lead to dehydration, feed studies were used. No
difference in feed consumption was observed between animals receiving control diets and those
receiving diets containing ephedrine sulfate. Furthermore, no deaths were attributed to
compound-related toxicity. The most frequent clinical observations observed at concentrations
of 1,000 ppm or higher were hyperactivity and excitability. Compound-related reduced weight
gain was observed in each sex of both species during the 14-day studies. Feed consumption by
treated and control animals was comparable in both rodent studies, suggesting that the reduced
weight gain that occurred in chemically exposed animals was associated with the ingestion of
ephedrine sulfate.
Yen et al. (1981) studied the effect of ephedrine on the weight of viable yellow obese mice
(Avy/a). Six- to 8-month old inbred viable yellow obese mice and normal mice were used.
Ephedrine hydrochloride was given in the diet to groups of 9 mice. Feeding ephedrine in the diet
at 0.1% (w/w) resulted in a 19% reduction in body weight to the starting weight. The duration of
treatment was 39 days of test article administration. The treated Avy/a mice ate less than the
control Avy/a mice during over the course of the study. To determine if the ephedrine-treated
mice lost weight due to decreased food consumption, mice of a similar weight range were fed a
diet-restricted amount of food similar to the amount of food consumed by the ephedrine-treated
mice. These diet-restricted mice did not have decreases in body weight as much as in the
Council for Responsible Nutrition
December 19, 2000
36
ephedrine-treated mice. These results suggest that the reduced feed consumption alone could not
account for all of the weight loss.
Massoudi and Miller (1977) studied the thermogenic activity of ephedrine compared with that of
triiodothyronine by incorporating both agents into the diets. Ephedrine was given in the diet at
1 g/kg feed to groups of 4 adult animals. In mice studies, several different groups were used;
normal lean mice (CBA strain); mice made with obese with gold thioglucose; mice made obese
with monosodium glutamate diets; mice made obese by diet; and genetically obese mice (obob)
mice. In the rat studies, rats made obese by diet and rats genetically obese were used. The
duration of treatment was 5 weeks for mice and 8 weeks for rats. Food intake and body-weight
were monitored throughout, and 24-hour oxygen consumption measurements were made at least
once during the experimental period. The animals were analyzed upon termination of study. No
histology was performed. It was reported that ephedrine treatment resulted in a loss in body
weight and body fat without increasing food intake, and had elevated oxygen consumption
compared with untreated controls that consumed the same quantity of feed.
Chen (1925b; 1926b) examined the effect of repeated administration of ephedrine in rabbits and
rats. Three series of young rabbits (strain and sex not specified) were selected for
experimentation. One series of 10 rabbits were given intravenous injections of 25 mg of
ephedrine sulphate, irrespective of their body weight, daily for 4 weeks (except Sundays). The
total dose (cumulative dose) was reported to be as high as 8.2 times the minimum lethal dose
(MLD) with respect to initial body weight or 820% of the MLD. In another series of ten rabbits,
ephedrine sulphate was given intramuscularly at 25 mg daily for 4 weeks except Sundays, and
another series of ten rabbits was administered 25 mg of ephedrine orally for the same duration.
All animals were maintained for 140 days after cessation of treatment. General findings of these
studies showed that animals receiving intravenous injections developed thrombosis. In the
intramuscular administration group there was fibrosis at the site of injection which disappeared
over time after cessation of daily injections. No lesions were observed in the gastrointestinal
tract from postmortem examination. At necropsy, lungs, liver, spleen, adrenal body, and kidney
tissues were examined. It was reported by the author that no gross pathology was observed, and
that no demonstrable abnormality in the structures of these visceral organs were observed. Some
cloudy swelling in most of the kidneys was observed, but these findings were also observed in
control animals as well.
In a subsequent series, albino rats (strain and number not specified) were injected intravenously
with large doses of ephedrine every other day for 7 days. The dose was reported to be 74% of
Council for Responsible Nutrition
December 19, 2000
37
MLD (approximately 101.25 mg/kg). It was reported that their body weight was constant or
somewhat decreased 2 to 3 days after the injection, but in all cases it subsequently increased.
The study authors reported that there were no marked pathological lesions that could be
attributed to the effect of the test article.
Summary of Short-Term Repeated Dose Studies
Short-term toxicity studies demonstrated no compound-related effects at necropsy in both rats
and mice at doses up to 1,500 and 5,000 ppm, respectively, in feed or water equivalent in rats to
approximately 120 mg/kg body weight/day in water and 165 mg/kg body weight/day in feed; and
in mice 400 mg/kg body weight in water and 1,000 mg/kg body weight/day in feed. No deaths
were attributed to test article toxicity. Compound-related reductions in body weight gain were
observed. Hyperexcitability and rough coats were the only observable effects which were
noticed and only at the highest dose levels.
3.2.2
Subchronic Studies
NTP conducted two 13-week studies in rats and mice. These studies were conducted to evaluate
the cumulative toxic effects of repeated administration of ephedrine sulfate and to determine the
concentrations to be used in subsequent 2-year carcinogenicity studies (in Section 3.3).
Council for Responsible Nutrition
December 19, 2000
38
Table 3.2.2-1
Summary of Repeated Dose Studies on Ephedrine/Ephedra
Species and
Strain
Route and Dose
Duration
Results
Reference
Rats (F344/N)
-ephedrine sulfate
via feed at 0, 125,
250, 500, 1,000, or
2,000 ppm or
equivalent to
approximately 0,
7, 14, 33, 62, and
120 mg/kg bw/day
in males and in
females: 0, 9, 18,
37, 71 and 146
mg/kg bw/day
-13 weeks
-no premature mortality in this report
-mean body weights at the 2 top doses
were 20% and 23% lower than control
males, and 10% and 17% for females
-hyperexcitability and rough coats
observed in rats at 2,000 ppm
-no compound-related
histopathological effects
-dose selection for longer term study
was 125 and 250 ppm based on the
reduced weight gain at 1,000 and
2,000 ppm
NTP, 1986
Mice
(B6C3F1)
-ephedrine sulfate
via feed at 0, 310,
630, 1,250, or
5,000 ppm
equivalent to
approximately 0,
34, 78, 142, 369,
or 718 mg/kg
bw/day in males
and in females: 0,
20, 89, 192, 423
and 900 mg/kg
bw/day
-13 weeks
-several deaths occurred before
termination and were attributed to
fighting among males at 1,250, 2,500,
or 5,000 ppm
-all female mice survived until the end
-final mean body weights at top 3
doses were 14%, 17% and 12 % lower
than controls, at 630, 1,250, and 5,000
ppm
-hyperexcitability and rough coats
-no compound-related histopathologic
effects were observed
-dose selection for longer-term studies
was 125 ppm and 250 ppm based on
reduced weight gain observed
NTP, 1986
3.2.2.1
Subchronic Rat Study
Male and female F344/N rats were obtained from Charles River Breeding Laboratories, observed
for 20 days, distributed to weight classifications and then assigned to cages according to a table
of random numbers. The average age of the rats were between 4 to 5 weeks old. Groups of 10
rats of each sex were given diets containing, 0, 125, 250, 500, 1,000, or 2,000 ppm ephedrine
sulfate equivalent to approximately 0, 7, 14, 33, 62, and 120 mg/kg body weight/day in males and
in females, 0, 9, 18, 37, 71, and 146 mg/kg body weight/day in females based on mean body
weight and mean food consumption values reported in the study. Duration of study was 13
weeks. Control diets consisted of NIH 07 Rat diet. Formulated diets, control diets, and water
were available ad libitum. All animals were observed twice daily for clinical signs. Individual
animal weights were determined once weekly. Feed consumption was also measured once
weekly.
Council for Responsible Nutrition
December 19, 2000
39
Necropsy and histologic examinations were performed on all animals. Tissues examined
included tissue masses, regional lymph node, blood smear, skin, mandibular lymph node,
mammary gland, salivary gland, thigh muscle, sciatic nerve, bone marrow, costochondral
junction, thymus, larynx, trachea, lungs and bronchi, heart, thyroid gland, parathyroid,
esophagus, stomach, duodenum, jejunum, ileum, colon, rectum, mesenteric lymph node, liver,
gallbladder, pancreas, spleen, kidneys, adrenal glands, urinary bladder, seminal vesicles,
prostate/testes or ovaries/uterus, nasal cavity, brain, pituitary gland, eyes, external and middle ear
and spinal cord; adrenal gland, and heart weight measured for control and highest dose groups.
Pupil diameter was also measured.
There were no premature deaths reported in this study. Final mean body weights of rats that
received 1,000 or 2,000 ppm were 20% and 23% lower than those of controls for males,
respectively and 10% and 17% lower for females, respectively. Feed consumption by treated and
control groups was generally comparable as indicated by food consumption evaluations.
Hyperexcitability and rough coats were observed in rats that received 2,000 ppm.
Histopathology examination revealed no compound-related findings. The mean pupil diameters
for treatment and control animals were comparable. The mean packed cell volume of male rats
that received the highest dose was 6% greater than that of controls which was statistically
significant. The relative adrenal gland weight of male rats at the highest dose was significantly
greater than that of the controls, and the adrenal gland weight and heart weight of female rats that
received the highest dose was significantly lower than those of controls. Based on these findings,
the concentrations selected for the 2-year rat study were determined to be 125 and 250 ppm
ephedrine sulfate in feed. The reduced weight gain that occurred at higher concentrations was
felt by study administrators to be potentially life threatening over the duration of a 2-year study.
The No-Observed-Effect Level (NOEL) determined for this study was 250 ppm based on no
significant findings which is equivalent to approximately 14 mg/kg body weight/day in male rats
(female rats: 18 mg/kg body weight/day). The NOAEL level was determined to be 1,000 ppm
based on findings of a trend towards decreased body weight gain which was not statistically
significant when compared to controls which is equivalent to approximately 33 mg/kg body
weight/day in male rats (female rats: 37 mg/kg body weight/day).
Council for Responsible Nutrition
December 19, 2000
40
3.2.2.2
Subchronic Mouse Study
Male and female B6C3F1 mice were obtained from Charles River Breeding Laboratories,
observed for 20 days, distributed to weight classifications and then assigned to cages according
to a table of random numbers. Mice were housed 5 per cage. Groups of 10 mice of each sex
were given diets containing 0, 310, 630, 1,250, 2,500, or 5,000 ppm ephedrine sulfate equivalent
to 0, 34, 78, 142, 369, or 718 mg/kg body weight/day in males and in females, 0, 20, 89, 192,
423, and 900 mg/kg body weight/day based on mean body weight and mean food consumption.
Duration of study was 13 weeks. Control diet consisted of Mouse Ration. Formulated diets,
control diets and water were available ad libitum. All animals were observed twice daily for
clinical signs. Individual animal weights were determined once weekly. Feed consumption was
also measured once weekly.
Necropsy and histologic examinations was performed on all animals. Tissues examined included
tissue masses, regional lymph node, blood smear, skin, mandibular lymph node, mammary gland,
salivary gland, thigh muscle, sciatic nerve, bone marrow, costochondral junction, thymus, larynx,
trachea, lungs and bronchi, heart, thyroid gland, parathyroid, esophagus, stomach, duodenum,
jejunum, ileum, colon, rectum, mesenteric lymph node, liver, gallbladder, pancreas, spleen,
kidneys, adrenal glands, urinary bladder, seminal vesicles, prostate/testes or ovaries/uterus, nasal
cavity, brain , pituitary gland, eyes, external and middle ear and spinal cord; adrenal gland, and
heart weight measured for control and highest dose groups. Pupil diameter was also measured.
Several deaths occurred before termination of study. It was determined by the study authors that
the deaths in males receiving 1,250, 2,500, or 5,000 ppm were the result of fighting. All female
mice survived to the end of the study. Final mean body weights of males that received 1,250,
2,500 or 5,000 ppm were 14%, 17%, and 12% lower than controls. Final mean body weight of
female mice was more than 13% lower than that of the controls at mice receiving 1,250 ppm or
higher. Estimated feed consumption by treatment groups was greater than that of controls. The
following clinical signs were determined to be compound-related; rough coats, hyperexcitability
and fighting among males.
Histopathology examination revealed no compound-related effects. Mean pupil diameter was
not affected. The mean packed cell volume of male mice that received the highest doses was 9%
lower than that of the controls which was statistically significant. The relative heart weight and
adrenal gland weight of mice receiving 5,000 ppm were similar to controls. The reduced weight
gain observed at 310 ppm in female mice and at 620 ppm was felt by the authors to be potentially
life threatening over the duration of a 2-year study. Based on these findings, the high-dose
Council for Responsible Nutrition
December 19, 2000
41
selected for the 2-year studies was 250 ppm ephedrine sulfate in feed and the low dose at 125
ppm. The NOAEL level was determined to be 620 ppm based on the reduced body weight gain.
Summary of Subchronic Studies
Subchronic studies in rodents showed that there were no deaths attributable to test-article
toxicity. The most commonly reported clinical observations were hyperactivity and excitability
with the greatest incidence in animals treated at 1,000 ppm. Compound-related reduced weight
gain was observed in both sexes in both species during the 13-week studies. Like the findings in
the 14-day studies, feed consumption by treated and control animals was comparable in the 13week studies, suggesting that the reduced weight gain that occurred in chemically exposed
animals was associated with ingestion of ephedrine sulfate.
3.3
Carcinogenicity Studies
Ephedrine sulfate was tested for carcinogenic activity in a 103-week feeding study in rats and in a
103-week feeding study in mice.
3.3.1
103-Week Rat Feeding Study
Ephedrine sulfate was administered in the diet to groups of 50 male and 50 female F344/N rats at
dose levels of 0, 125, or 250 ppm (maintained through monitoring of food consumption and body
weight values) for a period of 2 years. Prior to dosing, all rats were randomly assigned to the
treatment and control groups. All rats were conditioned to the receiving laboratory, cages and
diet for 3 weeks. Thereafter, a complete necropsy was performed on 5 animals of each sex to
assess their health status. The rats were placed in the study at 7 to 8 weeks of age. Prior to the
conditioning period, rats were approximately 4- to 5- weeks old. Rats were housed 5 per cage.
Feed and water were available ad libitum.
Endpoints monitored included: twice daily observations for viability; observations for clinical
signs of overt toxicity once per week for the first 13 weeks and monthly thereafter during the first
year of the study. During the second year of the study, clinical signs were recorded weekly.
Body weights were measured once per week for the first 13 weeks and monthly thereafter
throughout the study. Food consumption was measured once monthly. At necropsy, gross
pathology findings were recorded for all major organs and tissues for all decedent and sacrificed
animals. Following necropsy, histopathological (microscopic) evaluations were performed on all
Council for Responsible Nutrition
December 19, 2000
42
major tissues from all treated and control animals and on all lesions identified in the gross
pathological examinations. In particular, the following tissues were examined: gross lesions,
skin, mandibular lymph node, mammary gland, salivary gland, thigh muscle, sciatic nerve,
sternebrae, vertebrae or femur including marrow, costochondral junction (rib), oral cavity,
thymus, larynx and pharynx, trachea, lungs and bronchi, heart and aorta, thyroid gland,
parathyroids, esophagus, stomach, duodenum, jejunum, tongue, regional lymph nodes, ileum,
colon, cecum, rectum, mesenteric lymph node, liver, pancreas, spleen, kidneys, adrenal glands,
seminal vesicles/prostate/testes/epididymis or ovaries/uterus, nasal cavity and nasal turbinates,
brain, pituitary gland, spinal cord, eyes, and preputial or clitoral gland. No hematological,
clinical chemistry, urinalysis, or organ weight analyses were performed, which is consistent with
a study designed to investigate only a carcinogenic potential rather than combined chronic
toxicity/carcinogenicity.
As a result of treatment, survival was found to be increased in female rats, but not in males. The
survival of the control group of female rats was significantly lower than that of the low-dose
group after 97 weeks and of the high-dose group after 102 weeks. Mean body weights of highdose male rats were 5 to 9% lower than those of the controls after Week 11. Mean body weights
of low-dose male rats were 5 to 7% lower than those of the controls after Week 34. Mean body
weights of high-dose female rats were 5% lower than those of the controls by Week 8, 10%
lower by Week 34, and 10 to 20% lower for the remainder of the study. Mean body weights of
low-dose female rats were 6 to 13% lower than those of the controls after Week 18. The average
daily feed consumption was 94% and 92% that of controls for low- and high-dose males, and
92% and 89% for females, respectively. The average amount of ephedrine sulfate consumed per
day was estimated to be 4 mg/kg and 9 mg/kg for low- and high-dose male rats, respectively and
5 mg/kg and 11 mg/kg for low- and high-dose female rats, respectively. It should be noted that
intake of ephedrine sulfate on a mg/kg/day basis is an average and that there was a range (higher
at the beginning, and lower at the end).
Salient changes in neoplastic incidences are summarized in Table 3.3.1-1.
The incidence of pituitary gland adenomas in the male rats demonstrated a positive trend with
incidences in the low and high-dose groups greater than that of the controls. Adenoma and
hyperplasia in the pituitary gland represent different stages of progression of the same lesion and
the histologic distinction between adenoma and hyperplasia was reported to be difficult to
distinguish. The study authors combined these lesions when compound-related effects were
analyzed. The incidences of hyperplasia or adenomas (combined) in treated and control male rats
Council for Responsible Nutrition
December 19, 2000
43
did not differ significantly. It was reported that the overall control rate of 10% in this study was
somewhat lower relative to the historical control rate for pituitary gland adenomas in males
(range 5 to 52%).
The incidence of adrenal gland pheochromocytomas in low-dose male rats was significantly
greater than the incidence in controls by the life table test but not by the incidental tumor test. It
was reported that the incidence in high-dose males was similar to the control incidence and
comparable to the mean historical control incidence of 20%. Nonmalignant pheochromocytoma
was not associated with any early deaths and was not considered to be compound-related based
on the findings that the increased incidence was only observed in low-dose males and that this
marginal increase was not significant in an incidental tumor test. Other adrenal gland
observations included angiectasis of the adrenal cortex observed at an increased incidence in
high-dose male rats.
The incidence of mammary gland fibroadenomas in female rats occurred with a significant
negative trend, and the incidence in the high-dose group was significantly lower than that in
controls. This decreased incidence has been observed in other studies and postulated to be
associated with reduced weight gain (Haseman, 1983). It was reported that the decreased
incidence of mammary gland fibroadenomas parallels a reduction in weight gain in both low- and
high-dose groups.
The incidences of endometrial gland cysts were greater in treated female rats than in control
animals; however, the incidence of endometrial stromal polyps was not significantly different
from the control incidence.
In the small intestine, a leiomyoma was observed in 1 out of 46 high-dose female rats, and a
leiomysarcoma was observed in another high-dose female rat. In the circulatory system,
lymphangiectasis was observed at increased incidences in treated female rats.
Testicular atrophy was initially observed at increased incidences in treated male rats (control,
19/50; low-dose 34/50; high-dose 33/50). However, an independent blind review of all available
sections of the testis from male rats, resulted in the observations of the following incidences of
testicular atrophy: control 42/50; low-dose 44/50; high-dose 45/50. The presence of testicular
atrophy was associated with the presence of testicular interstitial cell tumors.
Council for Responsible Nutrition
December 19, 2000
44
Table 3.3.1-1
Treatment Related Increases in Neoplasms in Rats
Tissue - Microscopic Lesion
Pituitary Gland - Adenoma
Adrenal Medulla Pheochromocytoma
Testis - interstitial cell tumor
Uterus - Endometrial stromal polyp
Small Intestine - Leiomyoma
Small Intestine - Leiomyosarcoma
Sex
M
M
M
F
F
F
Group
1
2
3
Dose
ephedrine sulfate
(ppm)
0
(control)
125
250
No. Examined
49
49
48
No. Affected
4
13
13
No. Examined
50
50
49
No. Affected
10
19
11
No. Examined
50
50
50
No. Affected
45
47
46
No. Examined
49
50
50
No. Affected
11
14
17
No. Examined
48
48
46
No. Affected
0
0
1
No. Examined
48
48
46
No. Affected
0
0
1
Overall, the study showed no evidence of a tumorigenic effect of ephedrine sulfate up to doses of
250 ppm. Rather, treatment was associated with increased survival in female rats but not in
males. In addition, a significant decrease in the incidence of mammary gland fibroadenomas was
observed. Positive, but not statistically significant, trends were observed in the incidence of
pituitary gland adenoma in males and adrenal gland pheochromocytomas. It was first observed
that increased incidence of testicular atrophy occurred; however, upon blinded independent
review, subsequent results showed no change in incidence level for testicular atrophy.
The NOEL/NOAEL from this study were found to be as follows; the NOEL for tumorigenicity
was greater than 250 ppm. The NOAEL for this study is considered to be the high dose despite
the observation of reduced weight gain in both sexes at both doses. Typically, reduced weight
gain is considered to be an adverse consequence of a toxicological effect. For ephedrine, this is
an expected physiological response which should not be considered adverse. Moreover, the
reduced weight in the female rat appeared to lead to increased survival, which has been noted in
other studies that have linked calorie restriction to enhanced survival of rodents. Furthermore,
the average reduction in weight, for both sexes, both doses, and at different times during the
Council for Responsible Nutrition
December 19, 2000
45
study, was less than 10%. Therefore, the NOAEL value from this lifetime study was 250 ppm,
which corresponds to 9 mg/kg in the male and 11 mg/kg in the female.
3.3.2
103-Week Mouse Feeding Study
Ephedrine sulfate was administered in the diet to groups of 50 male and 50 female B6C3F1 mice
at dose levels of 0, 125, or 250 ppm (maintained through monitoring of food consumption and
body weight values) for a period of 2 years. All mice were conditioned to the receiving
laboratory, cages and diet for 3 weeks. Thereafter, a complete necropsy was performed on 5
animals of each sex to assess their health status. The mice were placed on study at 8 to 9 weeks
of age. Prior to the conditioning period, mice were approximately 5 to 6 weeks old. Male mice
were housed individually (due to fighting observed in the previous 13-week study) and female
mice housed in groups of 5 per cage. Feed and water were available ad libitum. The highest
dose tested was selected on the basis of the results of the 3-month subchronic toxicity study (see
Section 3.2.2.2). Salient changes in neoplastic incidences are summarized in Table 3.3.2-1.
Endpoints monitored included: twice daily observations for viability; weekly observations for
clinical signs of overt toxicity once per week for the first 13 weeks and monthly thereafter during
the first year of the study. During the second year of the study, clinical signs were recorded
weekly. Body weights were measured once per week for the first 13 weeks and monthly
thereafter throughout the study. Food consumption was measured once monthly. At necropsy,
gross pathology findings were recorded for all major organs and tissues for all decedent and
sacrificed animals. Following necropsy, histopathological (microscopic) evaluations were
performed on all major tissues from all treated and control animals and on all lesions identified
in the gross pathological examinations. In particular, the following tissues were examined: gross
lesions, skin, mandibular lymph node, gallbladder, mammary gland, salivary gland, thigh muscle,
sciatic nerve, sternebrae, vertebrae or femur including marrow, costochondral junction (rib), oral
cavity, thymus, larynx and pharymx, trachea, lungs and bronchi, heart and aorta, thyroid gland,
parathyroids, esophagus, stomach, duodenum, jejunum, tongue, regional lymph nodes, ileum,
colon, cecum, rectum, mesenteric lymph node, liver, pancreas, spleen, kidneys, adrenal glands,
seminal vesicles/prostate/testes/epididymis or ovaries/uterus, nasal cavity and nasal turbinates,
brain, pituitary gland, spinal cord, eyes, and preputial or clitoral gland. No hematological,
clinical chemistry, urinalysis, or organ weight analyses were performed, consistent with a study
designed to investigate carcinogenic potential rather than combined chronic
toxicity/carcinogenicity.
Council for Responsible Nutrition
December 19, 2000
46
There were no significant differences in survival between any groups of either sex. Mean body
weights of high-dose male mice were 9 to 18% lower than those of the controls after Week 9, and
those of low-dose male mice were 5 to 9% lower than those of the controls after Week 10. Mean
body weights of high-dose female mice were 10 to 23% lower than those of the controls after
Week 11, and those of low-dose female mice were 13 to 16% lower than those of the controls
after Week 22. The average daily feed consumption by both treated male mouse groups was
100% that of the controls and by low- and high-dose female mice, 97% and 94% that of the
controls. The average amount of ephedrine sulfate consumed per day was estimated to be 14
mg/kg and 29 mg/kg for low- and high-dose male mice respectively, and 12 mg/kg and 25 mg/kg
for low- and high-dose female mice, respectively. It is important to note that the mg/kg/day are
an average which represents a range (higher at the beginning and lower at the end of the study).
Follicular cell hyperplasia of the thyroid gland occurred at increased incidences in treated female
mice; however, the incidence of follicular cell adenomas was marginally lower in treated animals
than in control animals. Hyperplasia and adenoma of the thyroid and follicle are generally
considered to be different stage of progression of the same lesion, and the lack of correlation
between the increase in the incidence of hyperplasia and the incidence of adenomas indicates that
these lesions are probably not compound related in the present study (NTP, 1986).
Granulosa cell tumors were found in 2 high-dose female mice. Histopathologically, the
neoplasm in 1 of the animals was small and contained numerous mitotic figures. It was reported
that the cells within this mass were not arranged in any particular pattern or structure. In the
other animal, the neoplasm was significantly larger and exhibited distinct patterns of cellular
organization. A luteoma was found in 1 low-dose and 1 high-dose female mouse. These tumors
were composed of a uniform population of large polyhedral cells with eosinophilic vacuolated
cytoplasm, round to oval vesicular nuclei, and prominent nucleoli. Teratomas were observed in
1 out of 41 control and 1/42 low-dose female mice. Although ovarian tumors are reportedly rare
in female B6C3F1 mice, the low incidence of these tumors in the present study, the marked
histologic differences among individual tumors, and their benign status make it unlikely that their
presence is associated with exposure to ephedrine sulfate.
In the adrenal gland, cortical adenomas in male mice occurred with a negative trend, and the
incidence in the high-dose group was significantly lower than that in controls. One low-dose and
1 high-dose male mouse had adenomas that appeared to arise from the subscapular cells.
Council for Responsible Nutrition
December 19, 2000
47
Overall, the study showed no evidence of a tumorigenic effect of ephedrine sulfate up to doses of
250 ppm. Treatment was not associated with any changes in survival rates between treated and
untreated animals. No evidence of carcinogenicity was observed in these mice.
The NOEL/NOAEL values from this study were found to be as follows: The NOEL for
tumorigenicity was greater than 250 ppm. As previously discussed for the rat study, the
reductions in weight gains observed in the mice were not considered adverse effects, since they
are expected physiological responses. Therefore, the NOAEL in mice was 250 ppm, or 29 mg/kg
in the male and 25 mg/kg in the female.
Table 3.3.2-1
Treatment Related Increases in Neoplasms in Mice
Tissue - Microscopic Lesion
Ovary - Luteoma
Ovary - Granulosa cell tumor
Ovary - Teratoma
Adrenal - Cortical Adenoma
Sex
F
F
F
M
F
Adrenal - Adenoma
M
F
Thyroid Gland - Follicular Cell
Adenoma
F
Group
1
2
3
Dose
ephedrine sulfate
(ppm)
0
(control)
125
250
No. Examined
41
42
43
No. Affected
0
1
1
No. Examined
41
42
43
No. Affected
0
0
2
No. Examined
41
42
43
No. Affected
1
1
No. Examined
50
50
48
No. Affected
7
3
1
No. Examined
48
49
49
No. Affected
0
0
1
No. Examined
50
50
48
No. Affected
0
1
1
No. Examined
48
49
49
No. Affected
1
0
1
No. Examined
48
49
49
No. Affected
2
1
0
Summary of Carcinogenicity Studies
In both rodent carcinogenicity studies, mean body weights of each sex were lower than those of
controls. These results are consistent with results of the 13-week and the 14-day studies, which
Council for Responsible Nutrition
December 19, 2000
48
suggests that the ingestion of ephedrine sulfate was associated with reduced weight gain over the
entire period of the 2-year studies. The NOEL for tumorigenicity was greater than 250 ppm in
both rats and mice, which was reported by NTP to correspond to an average daily consumption of
approximately 9 to 11 mg/kg body weight/day and 25 to 29 mg/kg body weight/day, respectively.
Limited dosing regimen was tested in this study and a full battery of clinical chemistry and
hematological endpoints were not assessed. The lifetime NOAEL was determined to be 250 ppm
which was reported by NTP to correspond to approximately 9 mg/kg body weight/day in male
rats and approximately 25 mg/kg body weight in female mouse. The use of male rat data and
female mouse data provides the most conservative estimation of the NOAEL value, since they
are the lowest value between the sexes which was obtained. No LOEL was determined based on
decreases in body weight gains at both low and high doses. It should be noted that the decreases
in body weight gain had no effect on survival nor did it increase the incidence of toxic findings in
these animals and were not considered adverse. These observations support the mild nature of
the body weight findings.
3.4
Reproductive and Teratogenicity Studies
Matsuoka et al. (1985) performed a detailed anatomicropathologic examination on an aborted
human embryo whose mother had taken 4 tablets of Tedral® for an upper respiratory tract
infection when the embryo was at approximately 30 days of development. This formulation of
Tedral® contained 130 mg theophylline, 25 mg ephedrine, and 8 mg phenobarbital. On the same
day, the mother developed acute chest pain and a fast, irregular heart beat. The spontaneous
abortion occurred at approximately 80 days of gestation. The main finding was the heart of the
fetus showed truncus arteriosus and overall abnormal development. Relevant medical history of
the mother included smoking 1 to 3 packs of cigarettes per day. The authors attributed the
abnormal development to the sizeable amount of theophylline contained in the Tedral® dose
taken by the mother based on the acute chest pain and arrhythmia developed shortly after
ingestion of a sizeable amount of Tedral®, and the known pharmacological activity of
theophylline on precordial pain, tachycardia, and arrhythmic in humans. The mother was a heavy
smoker, and the authors reported that this could have caused the fetal underdevelopment.
In an earlier evaluation, a comparative study of the effects of Tedral® and theophylline on
development of chick embryos was investigated (Gilbert et al., 1981). The test article was
applied to the surface of the chorioallantoic membrane of 250 chick embryos at 2 to 5 days of
incubation. The test compounds evaluated were Tedral®, and its single constituents alone theophylline, ephedrine and phenobarbital. The commonest cardiovascular anomalies induced by
Council for Responsible Nutrition
December 19, 2000
49
Tedral® were double outlet right ventricle with ventricular septal defect. Aneurysms were larger
in size and cardiovascular malformations were far more complex in embryos exposed to Tedral®
than in those injected with theophylline alone. Slitlike small ventricular septal defects were
found in 9.5% of the ephedrine-treated chicken embryo group, 8.7% in the phenobarbital group,
and 9.1% in the control group, which were not statistically different from each other. Together,
these data show that theophylline, which is a major component of Tedral® produces
cardiovascular anomalies in embryonic chick hearts. In addition, these results are consistent with
a synergistic effect of all 3 components in Tedral® in the development of chick embryos.
The cardiovascular teratogenicity and embryotoxicity of ephedrine were studied in chick embryos
treated after 2.5 to 6 days of incubation (Nishikawa et al., 1985). On incubation Day 3 of White
Leghorn eggs, observation windows were made in the shell and l-ephedrine hydrochloride was
topically administered to the chick embryos at doses of 0.5 to 20 mol in 0.9% sodium chloride
(saline) solution at 4 days of incubation. The optimal dose was defined as the dose that provided
the highest anomaly rate with a concomitant reasonable high survival rate. The optimal dose of
14 mol was applied to 2.5- to 6-day old chick embryos as, above. Eggs were then returned to
the incubator immediately after treatment and were left undisturbed until 14 days of incubation.
The surviving embryos were killed, and hearts were infused with Carnoy fixative for
examination. Embryos were examined for anomalies of cardiovascular morphology.
Cardiovascular malformations were observed in 29% (29/101) of treated embryos. Anomalies,
such as double-outlet right ventricle, truncus arteriosus communis or overriding aorta with
ventricular septal defect, were seen frequently in embryos exposed to the agent on Day 3 of
incubation. Malformations were induced by ephedrine at a dose as low as 1 mol/egg. The
present study showed that administration of ephedrine was capable of resulting in cardiovascular
malformations in the embryonic chick.
Kanai et al. (1986a,b) investigated the cardiovascular teratogenicity of ephedrine in pregnant rats.
Pregnant Wistar-Imamichi rats were injected intraperitoneally on Day 9, 10, or 11 of gestation
with single doses of 0.1, 1, 10, or 50 mg/kg of ephedrine. Sacrifice of the animals was carried
out on Day 20 of gestation with the removal of fetuses. No control groups were reported.
Cardiovascular anomalies were observed in 107 out of 523 fetuses or, 20.5%. The frequency of
embryos with anomalies was dose-dependent, and was 8.1 to 26.9% with the administration of
0.1 to 50 mg/kg ephedrine. There was no significant difference in the malformation rate among
fetuses dosed on Day 9, 10, or 11 of gestation. All of the cardiovascular malformations were
ventricular septal defect, 2 of which were associated with overriding aorta (2/107). Extracardiac
malformations were not observed in these fetuses. In a second experiment, ephedrine
Council for Responsible Nutrition
December 19, 2000
50
concentrations in the serum of dams and the whole body of fetuses was quantitatively analyzed
by gas chromatography in 10-day pregnant rats after injection with 50 mg/kg ephedrine.
Concentrations of ephedrine in rat dam serum were 19.2, 7.2, 1.9, and 0 g/ml at 1, 3, 6, and 12
hours after injection, respectively, and those in the fetus were 34.9, 9.5, 2.7, and 0 g/g body
weight at 1, 3, 6, and 12 hours after injection, respectively. The authors concluded that these
results indicated that ephedrine administration to rats during early stages of pregnancy affected
their fetuses and resulted in the cardiovascular malformations.
In the World Health Organization (WHO) monograph on Herba Ephedra, it was reported that
Ephedra sinica did not have any teratogenic effects in vivo, although it is unclear what this
conclusion is based upon. Furthermore, Ephedra sinica was not an abortifacient in rats (Lee,
1982).
The association of sympathomimetic drugs with malformations was studied in New Zealand
White rabbits based on case report findings by the authors (Gilbert-Barness and Drut, 2000).
After observation of malformations in 2 children following maternal ingestion of
sympathomimetic drugs during pregnancy, experiments in the pregnant rabbit were conducted to
ascertain whether these drugs may have teratogenic effects in a mammalian species.
Experimental studies were performed with pregnant rabbits using Primatene administered in high
and low dosage. Three groups were used: Group 1- 10 pregnant rabbits given a low dose of
Primatene containing 2 mg/kg/day ephedrine. Group 2- 9 pregnant rabbits given a high dose of
Primatene containing 4 mg/kg/day ephedrine. Control group – 6 pregnant rabbits given water by
gavage. All females were allowed to reach parturition without interference. Immediately upon
birth, all pups (dead or alive) were examined.
No toxicity of Primatene was noted in any of the rabbits during this experiment. With respect to
the offspring, a reduction in fertility and fetal loss in the treated groups was observed. In
addition, 2 offspring had cardiovascular defects (single atrium and single ventricle) and 2 had
exencephaly. Shortening of the extremities in 7/68 viable offspring in the treated groups who also
had extraskeletal malformations were observed. Measurements of limb length indicated a
significantly disproportionate development in both treated groups. Excluding the limb reduction
defects, malformations occurred in 7/68 viable offspring born alive in the treated groups.
Malformations included 3 with midline abdominal wall defects, 1 with pentalogy of Cantrell with
ectopia cordis; a second had chest abdominal wall defect with gastroschisis; and a third with
gastroschisis. The study authors concluded that these results substantiate the teratogenic effect of
Council for Responsible Nutrition
December 19, 2000
51
sympathomimetic drugs and therefore should be used with great caution or avoidance during the
first trimester of pregnancy.
Summary of Reproduction and Teratology Studies
The reproductive and teratogenic potential of ephedrine or ephedra has not been studied in a
methodical manner. Placental transfer of ephedrine occurs at 70% of the maternal blood levels.
Ephedrine is also excreted in breast milk. No clinical studies have been conducted with
ephedrine in pregnant or nursing mothers. In the clinical literature, fetal tachycardia has been
associated with maternal use of a related alkaloid, pseudoephedrine and the administration of
intramuscular ephedrine to treat maternal hypotension associated with increases in fetal heart rate
and beat-to-beat variability (Anastario and Haston, 1992). Gilbert-Barness and Drut, 2000
reported 2 cases with limb malformations associated with ingestion of products containing
sympathomimetics. Ephedrine intake during pregnancy and lactation is not recommended.
3.5
Mutagenicity Studies
The mutagenicity/genotoxicity potential of ephedrine in several in vitro studies has been
investigated. A summary of the findings is presented in Table 3.5-1
Table 3.5-1
Summary of Mutagenicity Studies on Ephedrine or Ephedra
Study Type
Concentration/Dose
Results
Reference
Ames/ Salmonella
typhimurium stand plate
incorporation assay (strains
TA98 and TA100)
-metabolic activation
obtained from the livers
of Aroclor 1254induced rats
-negative results were obtained
both with and without metabolic
activation and were confirmed in
triplicate assays.
Xue-jun et al.,
1991
-concentration/dose not
specified
Bone marrow micronucleus
assay using TAI mice (5
mice/sex)
stated that the tested
doses were 1, 5, 10, 20
or 40 times the dosage
used in traditional
medical
-Ephedra extract did not induce
any changes in the ratio of
polychromatic erythrocytes to
total erythrocytes, or in the
frequency of micronucleated
polychromatic erythrocytes, in
this assay system.
Xue-jun et al.,
1991
Ames/ Salmonella
typhimurium standard plate
incorporation assay (strains
TA 100, TA 1535, TA97, or
TA98)
-metabolic activation
from the livers of
Aroclor 1254-induced
rats
-0, 100, 333, 1,000,
3,333, 10,000 g/plate
-Not mutagenic in the presence
or absence of S9.
NTP, 1986
Council for Responsible Nutrition
December 19, 2000
52
Table 3.5-1
Summary of Mutagenicity Studies on Ephedrine or Ephedra
Study Type
Concentration/Dose
Results
Reference
Chromosome aberration
assay in Chinese hamster
ovary cells
-1,000, 1,250 and 1,490
g/ml without S9
activation
-6,500, 7,000, 8,000
g/ml with S9
activation
-Results of tests detected an
increased frequency of sister
chromatid exchange which was
considered equivocal, since a
positive response was observed
only at a dose at which toxicity
was observed
-The slight, consistent elevation
in SCE’s at all doses in the
presence of S9 was not
statistically significant.
NTP, 1986
Rec-assay with Bacillus
subtilis
5, 10, 20, 50, and 100
mg/ml
No mutagenic activity.
Morimoto et al.,
1982
Ames/ Salmonella
typhimurium standard plate
incorporation assay (strains
TA98 and TA100)
5, 10, 20, 50, and 100
mg/ml with and without
S9 (metabolic
activation obtained
from the livers of
polychlorobiphenylinduced rats)
No mutagenic activity.
Morimoto et al.,
1982
Xue-jun et al. (1991) studied the mutagenicity of 102 raw pharmaceuticals used in Chinese
traditional medicine. The mutagenic potential of Ephedrae sinica Staph. was evaluated after
extraction of dried herb with boiling water and frozen vacuum drying. The test article was then
tested using the Ames test, and the micronucleus and chromosomal aberration assays in mice in
vivo. Ephedrine sulfate was not mutagenic in 2 strains of Salmonella typhimurium (TA98 and
TA100) in the presence or absence of S9 from Aroclor 1254-induced male Sprague-Dawley rat
livers at doses up to 40 mg/plate. Aflatoxin B1 (0.1 g/plate) was used as positive control.
In the mouse bone marrow micronucleus assay, doses equivalent to 1, 5, 10, and 20 or 40 times
the dosage used in traditional medical uses were tested in 4 groups of 5 male and 5 female TAI
mice. The extract was administered by intraperitoneal injection in a volume of 0.2 to 0.3 ml.
Colchicine at 1 mg/kg was given 4 hours before sacrifice. For each group, 200 metaphases were
analyzed. Micronuclei in 10,000 polychromatic erythrocytes on the smear stained with acridine
orange were counted. For the observation of systemic toxicity to the bone marrow, smears were
stained with May-Grunwal-Giemsa and the incidence of polychromatic and normchromatic
erythrocytes and nucleated cells (including erthyrocytes) were scored. Treatment with ephedra
extract did not induce any changes in the ratio of polychromatic erythrocytes to total erythrocytes,
or in the frequency of micronucleated polychromatic erythrocytes, in this assay system.
Council for Responsible Nutrition
December 19, 2000
53
Mitomycin C at 0.001 g/kg body weight, used as a positive control which produced the expected
increases in micronucleated cells.
NTP investigated the genetic toxicology of ephedrine. Ephedrine sulfate was not mutagenic in
Salmonella typhimurium strains TA100, TA 1535, TA97, or TA98 in the presence or absence of
S9 prepared from the livers of Aroclor 1254-induced male Sprague-Dawley rats. The negative
results obtained were confirmed by repeating the experiment. The concentrations of ephedrine
sulfate that were used ranged up to 10,000 g/plate without producing cytotoxicity. The highest
concentration used in this assay exceeded the concentration of 5,000 g/plate recommended by
ICH and OECD guidelines for the Ames assay, supporting the negative finding.
Results of tests to detect an increased frequency of sister-chromatid exchanges (SCEs) in Chinese
hamster ovary (CHO) cells in culture were considered equivocal, since a positive response was
observed only at a dose at which slight toxicity of ephedrine sulfate was observed (indicated by
the necessity for delayed harvest before evaluation of cells). The slight, consistent elevations in
SCEs at all doses in the presence of S9 was not statistically significant. Results of tests to detect
an increased frequency of chromosomal aberrations in CHO cells were also considered
equivocal. No significant responses were observed in the absence of metabolic activation; the 2
significantly-elevated responses in the presence of S9 from Aroclor 1254-induced SpragueDawley rat livers occurred in the mid-range of a series of extremely high doses (5,600 to 8,000
g/ml).
Ephedrae herba was screened for mutagenic activity by the rec-assay with Bacillus subtilis as
well as the reversion assay with Ames strains TA98 and TA100 of Salmonella typhimurium
(Morimoto et al., 1982). The rec-assays showed that the ephedra extract was negative. The
Ames assays with or without metabolic activation showed that the ephedra extract was not
mutagenic. The highest concentration tested was 100 mg/ml.
Summary of Mutagenicity Studies
In summary, all in vitro and in vivo genotoxicity/mutagenicity tests performed on ephedrine
sulfate/ephedra extract produced negative responses and used concentrations or dose levels
which were sufficiently high to detect any changes, particularly in the NTP studies. Also,
negative and positive controls were used in the assay systems, with the appropriate responses
observed with each treatment. Based on the findings of Xue-Jun et al. (1991), Morimoto et al.
(1982), and most importantly the NTP studies, it is concluded that ephedrine was not mutagenic.
Council for Responsible Nutrition
December 19, 2000
54
In the NTP studies, ephedrine sulfate was not mutagenic in 4 strains of Salmonella typhimurium
(TA100, TA 1535, TA97, or TA98) in the presence or absence of S9 from Aroclor 1254-induced
male Sprague-Dawley rat livers or Syrian hamster liver S9 activation. Ephedrine sulfate did not
induce sister-chromatid exchanges or chromosomal aberrations in cultured Chinese hamster
ovary cells. Ephedrae herba was screened for mutagenic activity by the rec-assay with Bacillus
subtilis as well as the reversion assay with Ames strains TA98 and TA100 of Salmonella
typhimurium (Morimoto et al., 1982), and no evidence of mutagenic activity was observed.
3.6
Other Studies
An evaluation of l-ephedrine neurotoxicity with respect to its potential to damage dopaminergic
terminals in the caudate/putamen (CPu) was recently investigated (Bowyer et al., 2000). This
investigation used in vivo brain microdialysis experiments to determine the systemic doses and
extracellular brain levels of l-ephedrine necessary to produce similar increases in CPu
extracellular dopamine and marked hyperthermia that were previously shown necessary for
amphetamine-induced neurotoxicity in male Sprague-Dawley rats.
A single 40 mg/kg intraperitoneal dose of l-ephedrine produced marked hyperthermia with peak
microdialysate ephedrine levels of 7.3 ± 1.2M and a 20-fold increase in microdialysate
dopamine levels. At a lower concentration of 25 mg/kg, a lesser degree of hyperthermia, was
observed with peak ephedrine levels of 2.6 ± 0.4M, and a 10-fold increase in dopamine levels.
Multiple doses of either ephedrine and amphetamine were assessed. Multiple doses of either
ephedrine or amphetamine caused severe hyperthermia, but striatal tissue levels of dopamine 7
days after dosing were reduced only 25% or less by ephedrine compared to 75% reductions
produced by amphetamine. Levels of serotonin and glutamate in the CPu microdialysate did not
differ significantly between ephedrine versus amphetamine treatment, but elevation of dopamine
levels of d-amphetamine were over 2-fold those caused by l-ephedrine. It was concluded that lephedrine was not as neurotoxic to dopaminergic terminals as d-amphetamine, because nonlethal doses of l-ephedrine did not sufficiently increase the CPu dopamine levels within nerve
terminals or the extracellular space to those necessary for a more pronounced long-term
depletion.
3.7
Discussion/Summary of Animal Data
The nonclinical toxicology of ephedrine and ephedra was reviewed to assess its consistency with
data obtained from clinical studies. The chemical characteristics of ephedra are dependent upon
Council for Responsible Nutrition
December 19, 2000
55
its chemical composition. Since the dominant ephedrine alkaloid isomer of most Ephedra
species is ephedrine, the characteristics of ephedrine would provide a good indicator of the
expected chemistry, pharmacology, and toxicology. As with any mixture, the characteristics of
only one, albeit major, component cannot define all of the characteristics of ephedra. However,
in the case of ephedra, understanding the effects of ephedrine provides insight into the biological
activities of the herb itself. The studies evaluated addressed the acute, subchronic and chronic
safety, carcinogenicity, reproductive toxicity and mutagenicity of ephedrine. Where available,
data related to ephedra are discussed; however, there are only limited data, so information
available related to the safety of ephedrine must be relied upon.
In the determination of the probable safe dose of ephedrine to which humans can safely be
exposed, animal toxicology data are relied on to support the findings in clinical studies. In the
absence of clinical data, a 100- to 300-fold uncertainty factor would typically be applied to
animal data; however in the case of ephedrine, there is an extensive clinical database and also
clinical experience with its use. Because of this, the animal data become more supportive than
definitive in the assessment of safety in humans. Valid human data are considered superior to
data derived from animals when assessing the potential risks to humans from exposure to
chemicals; however, unlike animal experiments, where the conditions of the study (e.g., doses,
duration of treatment, etc.) can be controlled and defined, observations in human subjects can
suffer from bias and the lack of objective assessments.
Twelve published studies are available in which the effects were examined of acute
administration of ephedrine or ephedra extracts via several different routes of administration and
under different experimental conditions. Particular emphasis is placed on studies conducted in
rodents by NTP. LD50 values of 812 mg/kg body and 1,072 mg/kg were obtained for male and
female mice respectively. No rat LD50 was reported by NTP.
It is interesting to note that one study in the nonclinical literature compared the acute toxicity of
ephedrine to that of botanical ephedra extract. The LD50 of the extract was 5.30 g/kg body
weight/day whereas the LD50 of ephedrine was 841 mg/kg. Furthermore, the general symptoms
observed with the extract were milder in nature and time to death was longer than that of with
ephedrine. Although only one study was located in the literature which compared the effects of
ephedra versus ephedrine, these results support the conservative assumption that ephedrine can
be used in a safety assessment as a surrogate for ephedra, since the potency of ephedrine
overestimates the potential potency of ephedra itself.
Council for Responsible Nutrition
December 19, 2000
56
Subchronic studies conducted by NTP in rodents showed that there were no deaths attributed to
ephedrine sulfate toxicity. The most commonly reported clinical observations were hyperactivity
and excitability with the greatest incidence in animals treated at 1,000 ppm. Compound-related
reduced weight gain was observed in both sexes in both species during the 13-week studies. Like
the findings in the 14-day studies, feed consumption by treated and control animals were
comparable in the 13-week studies. These findings indicate that the reduced weight gain that
occurred in treated animals was associated with ephedrine sulfate. The reduction in body weight
gain was also observed in shorter-duration studies in obese monkeys and mice receiving
ephedrine (Massoudi and Miller, 1977; Yen et al., 1981; Ramsey et al., 1998).
Carcinogenicity studies were conducted by NTP for ephedrine sulfate in rats and mice for 103
weeks. Ephedrine sulfate was administered in the diet at dose levels of 0, 125, or 250 ppm for a
period of 2 years. In both rodent carcinogenicity studies, mean body weights of each sex were
lower than those of controls and no treatment-related tumors were observed. These results are
consistent with results of the 13-week studies and the 14-day studies.
In vitro and in vivo genotoxicity/mutagenicity tests performed on ephedrine sulfate or ephedra
extract produced negative responses and used concentrations or dose levels which were
sufficiently high to detect any changes, particularly in the NTP studies.
The NTP studies, given the quality of the investigations, are used as support for the analysis of a
UL based on the clinical data. Rat data were used, since mice were less sensitive to the effects of
ephedrine. Thus, the use of the rat species conservatively estimates the NOAEL values. It was
determined from the rat data that a NOEL could not be determined given the limited doses tested
in the longer-term studies and the fact that the carcinogenicity study did not incorporate full
hematological or clinical chemistry evaluations. A NOAEL value was obtained in male rats, at
an average daily consumption of approximately 9 mg/kg body weight/day. Decreased body
weight gains were observed at both doses in both sexes which did not affect survival or increase
the frequency of adverse events. Moreover, the decreases in body weight gain were likely the
effect of the ephedrine sulfate ingestion, as decreased food consumption did not adequately
account for the observed decreases. In addition, the higher dose of approximately 9 mg/kg did
not result in any additional effects; no additional pathology and no changes in frequency of
neoplastic or non-neoplastic lesions were observed. A dose of 9 mg/kg body weight/day from
the rat data extrapolated to a 60 kg person would be 540 mg/day.
Council for Responsible Nutrition
December 19, 2000
57
4.0
HUMAN STUDIES RELATED TO THE SAFETY OF EPHEDRA AND
EPHEDRINE ALKALOIDS
The analysis of the clinical database involves a review of published case reports and of clinical
trials and investigations involving normal healthy individuals and special populations (e.g.,
obese, asthmatic, etc.). Spontaneous adverse events captured by SN/AEMS on dietary
supplements containing ephedrine alkaloids are analyzed in Appendix A. Examination of
clinical trials involving the use of ephedrine was limited to studies which investigated safety
parameters. Pharmacological efficacy and therapeutic benefit of treatment were not assessed.
While valid human data are considered superior to data derived from animals when assessing the
potential risks to humans from exposure to chemicals, there are factors that must be seriously
considered when reviewing and interpreting information derived from human studies. Unlike
animal experiments, where the conditions of the study (e.g., doses, duration of treatment, etc.)
can be controlled and defined, this is difficult in human studies. Furthermore, observational
studies in human subjects often suffer from bias and the lack of objective assessments. Any such
weaknesses in a study make interpretation of the results difficult.
In terms of assessing the health effects of chemicals in humans, controlled, prospective clinical
investigations provide the most reliable source of information. For example, it is from studies of
this type that information related to the efficacy and safety of new pharmaceuticals is derived
(after appropriate animal testing has defined potential risks). For most chemicals to which
humans are exposed, prospective studies are unavailable, and as a result, relevant information
related to their health effects must be obtained retrospectively through the use of epidemiological
methods, using standard principles in an attempt to establish causation and dose-response
relationships. Another source of information regarding adverse effects of agents in humans are
case reports. These are typically based upon observations in individuals or small groups and they
serve the very important function of alerting the medical/scientific community to possible
adverse events. Individual case reports typically cannot be relied upon to establish a cause-effect
relationship, but the confidence in the reported findings of individual reports increases when
there is consistency in the observations among reports published by different authors. As with all
scientific investigations, case-reports must be carefully reviewed for limitations in methodology
and the findings interpreted in the light of the weight-of-evidence.
Before considering the observational data and the clinical trial data, a number of factors must be
recognized that may influence the likelihood and severity of adverse effects that occur secondary
to consumption of ephedrine alkaloids. These factors include concurrent use of medications and
Council for Responsible Nutrition
December 19, 2000
58
other products (such as caffeine, monoamine oxidase inhibitors, methydopa, beta-receptor
blocking agents) or pre-existing conditions (autonomic dysfunction) that influence the sensitivity
to sympathomimetics. Persons with pre-existing renal disease, ischemic heart disease, coronary
thrombosis, diabetes, glaucoma, impaired cerebral circulation, pheochromocytoma, hypertension,
thyrotoxicosis, and prostatic hypertrophy are considered to be at increased risk for adverse effects
from the use of ephedrine, and in many groups, use of ephedrine alkaloids is medically
contraindicated (Dollery, 1991a,b,c; Hoffman and Lefkowitz, 1996). Other risk groups may
include neonates and breast-fed infants secondary to maternal exposure, pregnant women,
children and the elderly. These groups are potentially at risk because of their known increased
sensitivity to the effects of sympathomimetic stimulation and because the potential effects of
ephedrine and related compounds in these populations have not been well-studied.
Co-administration of ephedrine-containing preparations with monomine oxidase inhibitors is
contraindicated, as the combination may cause severe, possibly fatal, hypertension (Hoffman and
Lefkowitz, 1996). The action of ephedrine is known to be affected by antacids and agents which
alter the pH of urine. Of course, the cumulative dose contraindicates use of multiple products
containing ephedrine alkaloids.
4.1
Adverse Event Reports from CFSAN SN/AEMS/Published Case Reports
4.1.1
Adverse Event Reports for Dietary Supplements Containing Ephedrine
Alkaloids Reported to FDA SN/AEMS
The available reported adverse experiences that were compiled through the Food and Drug
Administration’s (FDA) Special Nutritional Adverse Event Monitoring System (SN/AEMS) for
dietary supplements containing ephedrine alkaloids were evaluated as an integral component of
the safety assessment of ephedra. The AERs were compiled into a database and qualitatively
analyzed to examine any trends in the AERs (see Appendix A for detailed report).
After extensive examination of the database, it was not possible to determine conclusively if
there were any unexpected toxicological effects due to ephedrine alkaloids contained in the
dietary supplements based solely on the information presented in the AERs. Rather, only a
qualitative evaluation of trends in the database of AERs could be conducted.
Council for Responsible Nutrition
December 19, 2000
59
4.1.1.1
Data Deficiency
An assessment of the 1,173 AERs reported to the SN/AEMS at the FDA revealed that 98% of the
AERs did not contain complete critical information. The total daily intake of ephedra, was not
reported for 80.7% of individuals. Often, the specific product that was used and its constituents
were unknown, and many of these products contained other herbal ingredients. Age was not
reported in ~25% of the AERs. Potential contributing factors such as pre-existing conditions and
concomitant product use were not known for 44.0% and 44.7% of individuals, respectively.
Other issues that were identified were elapsed time between the date of the adverse event and
date reported, and contraindications within several AERs.
4.1.1.2
Basis for Selected AERs Dataset
Due to the large number of AERs with missing information, 121 AERs were selected based on
quantity of critical information provided. These cases were chosen based on criteria that they
included information regarding age, dose frequency, amount consumed daily, duration of use,
pre-existing conditions and concomitant products. These AERs were considered to contain a
sufficient quantity of information to warrant detailed examination.
4.1.1.3
Demographic Characteristics
The age characteristics of the 121 selected cases revealed that approximately 70% of the
individuals reporting adverse events were between 21 and 50 years old, with 15% being older
than 50 and 15% being younger than 20. Approximately 73% of the individuals reported to have
adverse events following use of dietary supplements containing ephedra were female and
approximately 27% were male. For the majority of adverse events, the race of the individual was
not reported (41%) or the individual was Caucasian (55%). The demographics for the selected
cases were comparable to those of the total original database (containing 1,173 individuals).
4.1.1.4
Dose and Duration Characteristics
In the 121 selected cases, the majority of individuals who reported adverse events (~84%)
consumed doses that included less than 150 mg ephedrine alkaloids. The majority of events were
reported following use of products containing ephedrine alkaloids for longer than 1 week
(~70%), and 48% had used the product for durations longer than 1 month.
Council for Responsible Nutrition
December 19, 2000
60
4.1.1.5
Date of Adverse Event Report
It is interesting to note that there were few adverse events reported through the SN/AEMS
passive surveillance reporting system following use of dietary supplements containing ephedrine
alkaloids prior to 1993, and the majority of the AERs were received in 1996. Of the 121 selected
cases, approximately 90% of the adverse events were reported after 1996. At approximately this
time, FDA launched a media campaign that included radio and television advertisements warning
the public about ephedra and its possible side effects, which may have influenced the report of
adverse events.
4.1.1.6
Adverse Event Profile
The types of adverse events that were reported following the use of dietary supplements
containing ephedrine alkaloids were classified according to the COSTART event terms
(COSTART 5TH EDITION) for both the overall database and the 121 individual cases. When
classified according to the COSTART body system, the reported adverse effects following use of
ephedrine alkaloids are consistent with both its promoted health benefits and its expected
pharmacological actions such as central nervous system stimulant effects and cardiovascularadrenergic effects. Approximately 36 and 30% of the AERs contained nervous system and
cardiovascular system effects, respectively. Of the 121 selected cases, 39% (47 of 121 cases)
were considered to contain serious adverse events, including 15 cases of strokes and stroke-like
symptoms, 13 cases of seizures, 15 cases of cardiac arrest, and 2 individuals who collapsed.
However, this percentage is considered to contain an artificially large proportion of serious cases
because the 121 cases were selected based on the quantity of information that they included and
only serious cases were followed-up by the FDA. None of these serious adverse events could be
attributed solely to the ephedrine alkaloid contained in the dietary supplement. None of the
consumed dietary supplements contained pure ephedra, and it is likely that some were not
manufactured under the good manufacturing practices regulations that would be applicable for
OTC products. Some products contained more than 9 different herbal ingredients.
Of the selected 121 cases, less than 30% of individuals reported taking no other medications or
concomitant products. The primary types of other products that were consumed by the
individuals who reported adverse events included drugs affecting the central nervous system
(~30%), such as antidepressants, caffeine, and nicotine, as well as other dietary supplements
(~32%), such as other herbal products and vitamins. Due to the potential pharmacological
actions of ephedrine alkaloids, it would be expected that concomitant use of sympathomimetic
agents (including heart and asthma medications) and stimulants (including caffeine) could lead to
Council for Responsible Nutrition
December 19, 2000
61
additive effects. While the percentage of individuals reporting adverse events following use of
dietary supplements containing ephedrine alkaloids who were treated concomitantly with these
types of medications was comparable to the percentage of those who did not take any
concomitant products, it is difficult to draw conclusions regarding the potential sensitivities of
these populations from these data. Again, a limitation of the analysis of AERs is that it does not
allow for a control population who took similar types of concomitant products to compare if they
experienced similar adverse events.
Of the 121 cases that were chosen for evaluation based on the availability of detailed information
there were 8 deaths (5.8%). Of the 8 deaths that were a part of the 121 selected cases, 1 occurred
in an automobile accident, 6 were cardiovascular in origin, and 1 spontaneous abortion. Of the 6
cardiovascular deaths, 5 were in males and 1 was in a female. All 5 males were using dietary
supplements containing ephedra as an athletic performance enhancement. Autopsies revealed
that 1 patient had atherosclerotic cardiovascular disease and another had myocardial disease due
to chronic catecholamine use. Neither of these deaths can therefore be directly related to ephedra
use as their pre-existing conditions made them at high risk for a cardiovascular event. Of the 5
male deaths in this group who consumed dietary supplements containing ephedrine alkaloids to
increase athletic performance, 4 of the 5 individuals were using other performance enhancing
products, such as caffeine, and so their deaths cannot be directly attributed to the use of ephedra.
The remaining individual who did not report using other supplements suffered from asthma,
which is a contraindication for the use of ephedra in OTC products due to potential additive beta
adrenergic effects. In addition, there was 1 death of a female that also was reported in this group.
However, this individual had been taking Phen-fen during the last year prior to her death. In
addition to being obese, she also had suffered blood clots during the birth of her child 5 months
prior to the death. While the cause of death was unreported, she would have been at high risk for
cardiovascular complications, and there is no evidence that the death was caused by ephedra use.
There was spontaneous abortion that occurred at 13 weeks of gestation. This mother had been
taking a dietary supplement containing ephedra throughout the pregnancy. However, she also
reported consuming other herbal products for which any ingredient lists were not provided.
Given the lack of data in this AER, it is not possible to draw conclusions from this event and
relate them to the safety of the ephedra contained within the product.
While there have been several deaths that have been reported after the use of dietary supplements
containing ephedrine alkaloids, these have been complicated by the concomitant use of products,
which may have an effect, as well as pre-existing conditions that had a high risk attributed to
Council for Responsible Nutrition
December 19, 2000
62
them. In none of these cases can the conclusions be drawn that the use of ephedra contributed to
the cause of death.
There were 8 serious AERs that were reported for individuals who had used dietary supplements
containing ephedrine alkaloids with no pre-existing conditions or concomitant products. This
value represents 6.7% of the 121 AERs that were considered to contain sufficient quantity of
information for scientific analysis of trends. Despite this, there is not enough information to do a
detailed analysis of each of these individuals (i.e., complete hospital records), and therefore,
specific conclusions can not be drawn as to the role of ephedra in these reactions.
An examination of group characteristics among individuals using the products to increase weight
loss and those who for enhancement of athletic performance was evaluated. The majority of
individuals reporting adverse events after using an ephedra containing product for weight loss
were females, whereas males accounted for the majority of events reported in the enhancement of
athletic performance group. This would reflect the demographics of those members of the
general population that would be using the ephedra supplements. Within the population using
ephedra for weight loss, 51.1% of the adverse events reported were related to the nervous system
and 48.9% were related to the cardiovascular system. The symptoms recorded in these reports
are consistent with the known effects of ephedra and the promoted health benefits. In the
population who were ingesting ephedra for the enhancement of athletic performance, 66.7% of
the adverse events were found in the nervous system and 33.3% were attributed to the
cardiovascular system. As individuals using dietary supplements containing ephedrine alkaloids
to enhance athletic performance would be expected to be more concerned about cardiovascular
and aerobic health than individuals using dietary supplements containing ephedrine alkaloids to
increase weight loss, this may, in part, explain the differences in the incidences of cardiovascular
versus nervous system adverse events that were reported by these 2 groups. As with the weight
loss group, the symptoms recorded in these reports are consistent with the known effects of
ephedra. While the individuals related these effects as adverse, in most cases they were well
described pharmacological effects of ephedra that have been published in the scientific literature
that the general public may not be aware of and hence reported them.
4.1.1.7
Summary of AERs Reported to FDA SN/AEMS
While passive AER surveillance systems are generally regarded as a conservative estimate of the
incidence of adverse experiences with marketed products, the small number of reports for
ephedra in comparison to its wide availability indicates that it has a good margin of safety in the
general population. Surveys indicate that approximately half of the citizens in the U.S. use
Council for Responsible Nutrition
December 19, 2000
63
dietary supplements, and approximately 2 to 3 billion doses of dietary supplements containing
ephedrine alkaloids are consumed per year (GAO, 1999; AHPA, 2000). A total of 1,173 AERs
for over 2 to 3 billion doses indicates that there is good margin of safety for dietary supplements
containing ephedrine alkaloids in the general healthy population, when taken as recommended.
The non-life threatening adverse effects that were reported were attributable to the
pharmacological actions of ephedra, and none of the serious adverse events could be directly
(causally) related to the use of ephedra containing products. However, it is logical that specific
factors such as pre-existing medical conditions (e.g., cardiovascular problems) or concomitant
use of sympathomimetic agents (e.g., caffeine) could lead to serious adverse effects and the use
of these types of products (including dietary supplements containing ephedra or other stimulants)
should be avoided.
4.1.2
Published Case Reports
Knowledge about an adverse effect typically starts out as a signal of a possible problem, usually
identified through spontaneous reports of a suspected adverse reaction. These signals serve an
important function in alerting the medical/scientific community to possible adverse events.
These signals are subject to verification in an iterative fashion either through further reports or
studies of its biological plausibility, which could be quantitated with epidemiological or
experimental clinical studies. In the determination of a cause-effect relationship between the
purported adverse event and the agent, one must consider that the clinical event may be
associated with a number of factors, such as concomitant intake of other agents, diseases, diet,
genetics and the environment, which might contribute to the adverse event. The criteria for the
development of causality are summarized in Table 4.1.2-1. Individual case reports typically
cannot be relied upon to establish a cause-effect relationship, but the confidence in the reported
findings of individual reports increases when there is consistency in the observations among
reports published by different authors. As with all scientific investigations, case-reports must be
carefully reviewed for limitations in methodology and the findings interpreted in the light of the
weight-of-evidence.
Table 4.1.2-1
Criteria for Development of Concepts of
Causality
Criteria for Development of Concepts of Causality 1
Consistency of an association
Strength of an association
Council for Responsible Nutrition
December 19, 2000
64
Table 4.1.2-1
Criteria for Development of Concepts of
Causality
Criteria for Development of Concepts of Causality 1
Specificity of an association
Appropriate temporal relationship of an association
Biological plausibility of an association
Evidence of prior experience, analogous to the consistency of an association
Effect of dechallenge and rechallenge relative to disappearance and reappearance,
respectively, of a suspected event, implicitly testing the strength of the association in
character and time
Consideration of confounding or other causal factors, roughly similar to a converse
specificity criterion
1
Adapted from Jones, 1992
The published case reports were divided into two groups, 1) case reports related to abuse/misuse
and 2) spontaneous case reports which were not related to misuse/abuse. Criteria to classify an
abuse/misuse situation included use of very large doses, chronic exposure to relatively large
dosages of ephedrine, and/or abuse intent. The therapeutic dose for ephedrine is 15 to 60 mg
given 3 times daily (Dollery, 1991a). Case reports are briefly summarized by reaction displayed.
Full case report summaries are located in Appendix B.
4.1.2.1
Psychiatric Reactions
Psychosis has been reported following abuse of ephedrine and has been known since 1968 by
Herridge and A’Brook, who described ephedrine-induced psychosis. Later reports of ephedrineinduced psychosis and mania were also reported (Roxanas and Spalding, 1977; Whitehouse and
Duncan, 1987; Loosmore and Armstrong, 1990). The psychosis is similar to the psychosis
induced by amphetamines characterized by paranoia with delusions of persecution and auditory
and visual hallucinations which is generally time limited for ephedrine use (Jacobs and Hirsch,
2000). The relevance of this adverse event to a typical dietary supplement user is low, since
these events were usually related to very significant overdose and prolonged use. Capwell (1995)
and Doyle and Kargin (1996) reported psychiatric illness in two patients with no history of
mental illness. The duration of exposure was limited to 10 days and 1 month, where the exact
dose of ephedrine was unknown in both cases. Upon discontinuation of the product, the patients
recovered without sequellae. In cases involving asthmatic individuals, many of the psychosis
cases were the result of individuals taking products containing ephedrine initially for relief of
Council for Responsible Nutrition
December 19, 2000
65
asthma or other respiratory conditions. Chronic administration of ephedrine results in down
regulation of -receptors and decreased bronchial responsiveness, which has reduced and limited
its utility for this indication (Neve and Molinoff, 1986). As the recommended dose (15 to 60 mg,
3 times/day) becomes less efficacious, there is a tendency to increase the dose, and either
psychosis results from the acute increase, or psychosis occurs from the long-term abuse of
ephedrine due to the stimulant effects experienced at the higher dose levels. The extremely
elevated daily dose level was between 2.6 g to 6.6 g/day in this subset of case reports.
Psychiatric disorders have more frequently been attributed to other ephedrine class alkaloids,
which have important differences in pharmacology, such as pseudoephedrine (Dalton, 1990),
phenylpropanolamine (Puar, 1984; Lake et al., 1990a,b; Dewsnap and Libby, 1992; Mendez,
1992; Clovis, 1993).
4.1.2.2
Cerebrovascular Effects
Bruno et al. (1993) reported 3 case reports of ephedrine related stroke. In all 3 case reports,
certain risk factors were identified which may have contributed to the stroke, such has excessive
quantities of ephedrine (150 mg/daily greater than manufacturer recommended maximum), and
history of drug abuse. The authors reported that use of excessive quantities of ephedrine may be
an important stroke determinant; however, the use of ephedrine according to manufacturer’s
recommended dosages (exact dosage not indicated) was not a risk for stroke. Furthermore,
Matthews et al., 1997 reported a case of stroke in a 19-year old female from intentional overdose
of ephedrine in an attempted suicide attempt. Stroke has not been reported in the peer-reviewed
literature at recommended doses. Many cerebrovascular events have been attributed to
ephedrine; however, it would be more accurate to attribute these events to other ephedrine class
alkaloids, which have important differences in pharmacology, such as pseudoephedrine (Loizou
et al., 1982), phenylpropanolamine (Bale et al., 1984; Kizer, 1984; Edwards et al., 1987; Glick et
al., 1987; Maertens et al., 1987; Lake et al., 1990a,b) and even methylephedrine in BRON®,
which is intentionally used as a psychostimulant for its hallucinatory paranoid state which occurs
after short-term usage of relatively small amounts of this preparation in Japan (Ishigooka et al.,
1991). There has been one published case of intoxication involving BRON® in North American
even though BRON® is not available (Levine et al., 1993).
4.1.2.3
Renal Effects
Nephrolithiasis (kidney stones) has been associated with chronic ephedrine intake and/or abuse.
Blau (1998) reported a case of a 24-year old man who had taken 1,000 to 3,000 mg/day of
ephedrine for several years. The stone passed and analysis revealed ephedrine. Nephrolithiasis
Council for Responsible Nutrition
December 19, 2000
66
was reported in a patient using an energy supplement containing ma huang extract (Powell et al.,
1998). A 27-year old white man was evaluated for his nephrolithiasis. Kidney stones were
removed and evaluated for content. Three compounds, namely ephedrine, norephedrine and
pseudoephedrine were observed in each of the kidney stone extracts. The energy supplement
contained ma huang extract (170 mg/tablet), which was 6% ephedrine (10.2 mg
ephedrine/tablet), and the patient admitted to taking between 4 and 12 tablets a day (total
ephedrine intake 41 to 122 mg/day). Subsequent to this case report, an evaluation was initiated
by the authors to study kidney stones with a similar ephedrine composition. Two hundred survey
kidney stones were characterized by ephedrine metabolite, from a total of 166,466 stones which
were archived at a laboratory for future reference purposes. The incidence of ephedrine
metabolites was calculated at an incidence of approximately 0.064%. Deficiencies include the
finding that the analytical technique could not differentiate ephedrine from pseudoephedrine. In
addition, a survey was sent to these 200 individuals; however, only 15 returned questionnaires
were received which have significant impact on the findings and conclusions. Six of 15 surveys
reported some use of ephedrine, and 7 of 15 surveys admitted to abuse, often greater than 25
tablets of the various available preparations daily. One patient admitted to consuming up to 500
mini-thin tablets (60 mg pseudoephedrine each) daily for several years. It is not known how
many of these stones were associated with the use of herbal ephedrine-containing products.
One case report on urinary retention was presented and reviewed (Glidden and DiBona, 1977). A
12-year old boy had taken an oral combination drug containing 25 mg ephedrine, 130
theophylline and 10 mg hydroxyzine 2 to 3 times/day (50 to 75 mg/day of ephedrine) for
treatment of bronchial asthma and allergic rhinitis. Following a few weeks on treatment, urinary
retention was experienced. The patient discontinued the treatment and was asymptomatic.
Urinary retention is a pharmacodynamic effect of ephedrine and has been further documented
(Beck et al., 1992).
4.1.2.4
Cardiovascular Effects
Cardiomyopathy from cocaine and methamphetamine occurs from chronic exposure to
abnormally high levels of circulating catecholamines which can cause damage to the heart (Karch
et al., 1995). Ephedrine related cardiomyopathy also has been reported; however, these cases
have been reported in individuals who have taken significant doses above the recommended
dosages for prolonged durations of time (Van Miegham et al., 1978; To et al., 1980; Gualtieri
and Harris, 1996). In the 3 cases reviewed, a 35-year old asthmatic had taken progressively
increased amounts of ephedrine for 20 years up to doses of 400 mg/day, 1 woman had taken up to
540 mg/day of ephedrine for 10 years, and the third case involved a 28-year old obese women
Council for Responsible Nutrition
December 19, 2000
67
smoker, who took 2,000 mg/day for 8 years. In all cases, angiography was not performed.
Amelioration after cessation of ephedrine treatment was reported. Myocardial infarction was
reported in a 25-year old man subsequent to injecting himself intravenously with a solution he
thought to be amphetamine (Cockings and Brown, 1997). The concentration of ephedrine he
used and injected was not quantitated. He was symptom free 1 month after the episode.
Weesner et al. (1982), Snook et al. (1992), and Burkhart (1992) all report on cases of intentional
overdose. The intake described in these case reports involved doses between 450 mg and 17.5 g
of ephedrine which resulted in tachydysrrhythmias. Recovery was reported for all cases.
Zahn et al. (1999) reported cardiovascular toxicity after ingestion of herbal ecstasy in a 21-year
old male. Four capsules reported to contain ephedrine, ginseng, kola nut, and nutmeg, were
taken together with a glass of alcohol and a marijuana cigarette. The urine screen was positive
for ephedrine or pseudoephedrine, cannabinoid, traces of opiate and caffeine. The authors
suggested the possibility of effects contributed by caffeine toxicity should be considered, and
reported that the combination of caffeine in combination with ephedrine may show additive
effects. Herbal ecstasy is a product whose name implies a misuse intention. Furthermore, the
concomitant use of alcohol together with marijuana confounds the analysis of the safety of
ephedrine use.
A case of hypersensitivity myocarditis was associated with ephedra use (Zaacks et al., 1999). A
review of the literature determined that this was the first case associated with ephedrine and
myocarditis. The patient improved subsequent to clinical treatment of myocarditis and
withdrawal of the herbal supplement which was reported to contain 7 mg/tablet of ephedrine
(total per day was 21 mg). The patient was diagnosed 2 years previously with hypertension
which is a known contraindication and likely contributed to the hypersensitivity myocarditis
experienced in this patient.
Haller and Benowitz (2000) have recently published an evaluation of the AERs that FDA
released in March 2000. This evaluation is essentially the same as their review released by FDA
along with the newer AERs. Their conclusion that a significant number of the AERs for vascular
events were causally related to consumption of ephedra includes a strong emphasis on biological
plausibility, as necessitated by the insufficient information available on the dose response
relationships.
Council for Responsible Nutrition
December 19, 2000
68
4.1.2.5
Fatality
In 1997, a body building college student died suddenly (Theoharides, 1997). Autopsy revealed
myocardial necrosis and cellular infiltration. It was reported that the student took ephedrinecontaining tablets. His medical history did not include any known risk factors. Analysis of
blood and urine revealed no ephedrine in blood, but small amounts (16 g/dl ephedrine) in the
urine were suggested to be representative of about 5% of the original blood level (ephedrine is
excreted mostly unchanged in the urine with a half life of about 7 hours). The original blood
level was estimated by “back calculation” at 3 mg/L, reported to be within the range associated
with some ephedrine-associated fatalities. This case report has been the subject of much
speculation, but ephedrine intake at quantities which are unknown is thought by some to have
some part in the death of this otherwise healthy college student; however, the extent of ephedrine
involvement is uncertain and is still debated in the published literature.
Garriott et al. (1985) reported 5 cases of fatal overdose from caffeine-containing “look-alike”
drugs. “Look-alikes” is a term used to describe widely available non-prescription drugs sold as
appetite suppressants or stimulants. Three of the cases had taken caffeine/ephedrine
combinations, and 2 had taken caffeine only. All 5 cases had lethal concentrations of caffeine
detected in the blood (130 to 344 mg/L) and also 3 had high ephedrine concentrations from 3.5 to
20.5 mg/L. Caffeine and ephedrine were detected in overdose quantities in the blood and other
organs tested in 3 cases, and the other 2 had caffeine in overdose quantities in the blood along
with ethanol in 1 and diazepam and ethanol in the other case. Blood concentrations of 79 to 181
mg/L have previously been reported in caffeine fatalities (Baselt, 1982b). Caffeine
concentrations in blood resulting from coffee or caffeine-containing beverages, are usually less
than 10 mg/L. After oral ingestion of 120 mg of caffeine, peak plasma concentrations range from
2.0 to 4.0 mg/L (Baselt, 1982b). The ephedrine concentrations in the 3 fatalities with
caffeine/ephedrine combinations were 3.49, 7.85, and 20.5 mg/L, respectively. In only 1 of the
cases, a dose form was available for quantitative analysis. In this tablet, 113 mg of caffeine and
25 mg of ephedrine were found. Dosages could not be ascertained in any of the fatalities;
however, all involved large overdoses. Four of the cases were ruled as suicides as manner of
death, and the fifth case was considered to have been an accidental death due to drug abuse.
4.1.2.6
Interactions
Dawson et al. (1995) reported on a 28-year old woman following ingestion of a tablet which was
reported to contain 18.31 mg of ephedrine, 30 mg of caffeine and 100 mg of theophylline. The
patient had taken the product for a wheezy cough; however, only a day earlier she discontinued a
Council for Responsible Nutrition
December 19, 2000
69
monoamine oxidase inhibitor (MAOI) treatment for atypical depression. She developed
encephalopathy, neuromuscular irritability, hypotension, sinus tachycardia, rhabdomyloysis, and
hyperthermia. The interaction between ephedrine and MAOI was concluded to be the cause of
the effects.
4.1.2.7
Other Effects
Lustik et al. (1997) reported a case of ephedrine-induced coronary artery vasospasm in a patient
with prior cocaine use. The use of intravenous ephedrine for anesthesia resulted in ventricular
tachycardia which was thought to be related to the chronic cocaine. Intravenous ephedrine is not
relevant for dietary supplement users who ingest ephedrine in a tablet form. In a related case
report, Hirabayashi et al. (1996) reported coronary artery vasospasm after ephedrine use in a
patient with high spinal anesthesia.
Nadir et al. (1996) reported a case of hepatitis in a 33-year old woman taking a Chinese medicine
product containing ma huang. No composition information on the product was available. The
hepatitis was associated with ingestion of the product, due to the temporal relationship, and the
worsening following re-challenge with the product. It was reported that the authors performed a
literature search and communicated with FDA to find whether any other reports of liver injury
were available. No such information was found. The authors proposed that the ma huang
product the patient used may have contained some other ingredient or contaminant or was
misidentified. This is an important possibility, which should not be overlooked. Mistaking
poisonous plants for beneficial herbs has resulted in deaths (Fugh-Berman, 1997).
Martinez et al. (1993) reported generalized dermatitis in a 64-year old woman with recurrent
generalized maculpapular eruption following the intake of a nasal decongestant. The nasal
decongestant was reported to contain ephedrine, pseudoephedrine, and phenylpropanolamine
(concentrations not specified). Lesions cleared within 1 week of discontinuation of treatment.
The authors concluded that the administration provoked her cutaneous lesion; however, a
negative patch test was found with ephedrine.
4.1.2.8
Summary of Published Case Reports
The adverse effects reported in these cases of abuse/misuse are not surprising, given the
pharmacological activity of ephedrine at these chronic, extremely high doses, which are many
times the anticipated dose levels, even for prescription ephedrine intake. Ephedrine is expected
to stimulate heart rate, as well as cardiac output. Analysis of the published literature revealed
Council for Responsible Nutrition
December 19, 2000
70
that the following adverse events were reported in abuse situations; psychosis, cardiopathy,
stroke, and nephrolithiasis. The relevance of these adverse events to typical dietary supplement
users is low, since these events usually occurred at very high doses and prolonged use. In
chronic abuse cases, the duration of abuse was up to 30 years. In the majority of the abuse cases,
the usual dosage was approximately 240 to 450 mg/day. In case reports involving asthmatic
individuals, the usual daily dose level was between 2.6 g to 6.6 g/day. In abuse situations
involving intended suicide attempts and drug addiction/experimentation, dosages up to 17.5 g of
ephedrine intake have been reported.
In the literature, statements regarding ephedrine alkaloids sometimes consider them to be
synonymous, which implies that the pharmacological activity of a particular alkaloid is
equipotent with one another and that the toxicity of all optical isomers is equivalent, which is not
the case. In general, all the ephedrine alkaloids contained in ephedra show significant
stereoselective differences with regard to pharmacokinetic and pharmacodynamic effects. All
have effects on the cardiovascular and respiratory system, but not to the same degree. It is
important to note that the pharmacokinetic and toxicokinetic behavior of any isomer cannot be
used to predict that of any other ephedrine alkaloid isomer. Adverse events reported for a
particular ephedrine alkaloid isomer are used to demonstrate that ephedrine could also have the
same adverse reaction despite the absence of specific data with ephedrine.
Review of the case reports classified as spontaneous (i.e., not related to abuse/misuse of
ephedrine) revealed that many of the adverse events were known responses to the
pharmacological activity of ephedrine, together with a number of factors, such as pre-existing
health condition and concomitant use of other drugs. In some case reports, causal relationships
could not be established due to limitations such as product identification and characterization
(e.g., dosage levels). Urinary analysis of ephedrine was not consistently conducted in subjects to
confirm ephedrine intake. In the majority of the spontaneous case reports, no irreversible
damage was reported, and all subjects recovered. The published fatalities have been the subject
of much debate.
4.2
Clinical Studies
In the data evaluation process, high quality human data are usually considered superior to data
derived from animals when assessing the potential risks to humans from exposure to chemicals.
The clinical database included two sets of data, observational case reports and clinical
investigations involving ephedrine intake. Observational data in the form of case reports were
Council for Responsible Nutrition
December 19, 2000
71
evaluated for their usefulness in developing hypotheses/relationships between exposure and
effect. The clinical studies provided an opportunity to assess the safety and tolerability of
ephedrine intake in fairly diverse populations; however, the focus of these studies was typically
efficacy. Taken collectively, they are of sufficient quality and consistency to draw certain
conclusions regarding the safety of ephedrine. Only those clinical studies in the literature with
adequate evaluation of safety/tolerability parameters were used. Clinical studies in healthy
human subjects and obese subjects who are healthy are included. Table 4.2-1 is an index of all
clinical studies reviewed. Section 4.2.1 reviews the literature pertaining to healthy individuals.
Section 4.2.2 reviews the literature pertaining to healthy individuals given ephedrine and tested
under exercise/physical parameter conditions. Section 4.2.3 reviews the literature pertaining to
individuals classified as obese but determined to be healthy otherwise. Section 4.2.4 reviews
literature pertaining to ephedra or ephedrine use in asthmatics, Section 4.2.5 reviews a study
conducted in hypertensive patient population, and Section 4.2.6 reviews a study conducted in a
smoking population. These studies provided an opportunity to assess the safety and tolerability
associated with ephedrine use in fairly diverse populations. Randomized, double-blind, placebocontrolled studies are considered the least likely to result in bias.
Council for Responsible Nutrition
December 19, 2000
72
Table 4.2-1
Frequency and
Total Dose
(mg/day)
Index of All Clinical Studies Reviewed
Duration
Number of Subjects
(Gender)
Reported Results
Reference
Acute Normal Healthy Studies
3 times/day: 150
mg
24 hours
-10 healthy subjects
(6 male and 4
female)
-double-blind, randomized, placebo-control, 2-period crossover study
-all subjects underwent a thorough clinical examination, ECG, admission
urinalysis and blood work
-7 subjects taking ephedrine reported the following reactions: difficulty sleeping
(n=5);increased/stronger heart beat (n=4);decreased appetite (n=3)
-all subjects completed study, and no serious adverse effects reported
Shannon et
al., 1999
Once/day; 25 mg
24 hours
-10 healthy subjects
(5 male and 5
female)
-double-blind, randomized, crossover study with 4 phases
-eligibility determined by results of a medical history, brief physical examination,
medication history, and a pregnancy test for females
-candidates who were in good health, not pregnant, and not taking continuous
medications were selected
-all subjects experienced minor side effects such as tachycardia, anxiety,
headache, irritability, insomnia and loss of appetite (frequency was not reported)
-all subjects completed study with no major side effects reported
Gurley et al.,
1998a
Council for Responsible Nutrition
December 19, 2000
73
Table 4.2-1
Frequency and
Total Dose
(mg/day)
Index of All Clinical Studies Reviewed
Duration
Number of Subjects
(Gender)
Reported Results
Reference
Twice/day: 38.8 mg
24 hours
-12 healthy
nonsmoking subjects
(6 male/6 female)
-test article and meals were administered by study investigators
-caffeine intake was monitored
-no adverse effects were noted by any of the 12 participants during both
monitoring phases with respect to cardiovascular effects
-6 of 12 participants demonstrated a statistically significant increase in mean 12hour heart rate after receiving ma huang
-3 participants had a slight increase in heart rate which was not statistically
significant and 3 remained unchanged from baseline.
-4 participants experienced statistically significant increases in systolic blood
pressure which was not associated with clinical signs
- heart rate increased in 6 participants during the first 3 hours of administration
interval from approximately 72 bpm to 81 bpm; although statistical significance
was met, no participant described symptoms or tachycardia or palpitations
-the cardiovascular findings in this study indicate moderate pharmacodynamic
effects observed, but the dosage of 19.4 mg was not large enough to elicit
significant cardiovascular changes in all participants
White et al.,
1997
Once/day : 30 mg
24 hours
-9 health male
volunteers
-heart rate and blood pressure showed a progressive small increase resulting in a
mean increase of 5 beats/min
-systolic blood pressure was shown to increase significantly in all treatments of
14 mm Hg, but taking into account changes in placebo group, showed only 99
mm Hg different
-diastolic blood pressure was not significantly changed following ephedrine
administration
-no adverse effects were reported in this study
Liu et al.,
1995
Council for Responsible Nutrition
December 19, 2000
74
Table 4.2-1
Frequency and
Total Dose
(mg/day)
Once/day:
10, 20, 40 mg
ephedrine
Index of All Clinical Studies Reviewed
Duration
24 hours
Number of Subjects
(Gender)
-12 healthy subjects
(6 male and 6
female)
100, 200, 400 mg
caffeine
Reported Results
-diastolic blood pressure did not change after ephedrine intake
-at 40 mg there was an increase of 5 mm Hg in systolic pressure
-heart rate increased dose-dependently after ephedrine intake
-effects were not more frequent following the ephedrine doses than after placebo
administration (data not shown)
Reference
Astrup and
Toubro,
1993
-caffeine at doses up to 200 mg/day had only modest and clinically irrelevant
effects on blood pressure and heart rate
-no adverse effects were reported in the subjects
-caffeine at 400 mg/day had some clinical effect; however, details were not
provided.
Ephedrine +
caffeine :
-10 mg:100 mg
-20 mg:100 mg
-20 mg:200 mg
-ephedrine and caffeine mixtures resulted in an average 5 to 7 mm Hg increase
compared to placebo, which was greater than the predicted additive value
-E+C 20mg:100 mg and 20 mg:200 mg increased heart rate slightly more than
placebo, while 10 mg:200 mg was without significant effect
-no information on adverse effects were reported for this group.
Once/day:
-10 mg, 20 mg
ephedrine
24 hours
-6 lean healthy
subjects (3 male and
3 female)
-at both ephedrine doses, increased in heart rate more than placebo
-systolic blood pressure was minimally changed with no statistical significance
-adverse effects were assessed, and none were reported
-mixtures (10 mg ephedrine/200 caffeine; 20 mg ephedrine/100 caffeine and 20
mg ephedrine/200 caffeine) resulted in statistical changes in systolic blood
pressure. Diastolic diastolic blood pressure increased in 20/200 and 10/200.
Astrup et al.,
1991
24 hours
-43 healthy subjects;
22 females and 21
males
-ephedrine significantly increased systolic blood pressure and heart rate
-information on adverse effects was not reported
Kuitunen et
al., 1984
-combinations
(eph/caff)
-10 mg:200 mg
-20 mg:100 mg
-20 mg:200mg
Once/day:
-30 mg, 40 mg
ephedrine
Council for Responsible Nutrition
December 19, 2000
75
Table 4.2-1
Frequency and
Total Dose
(mg/day)
Index of All Clinical Studies Reviewed
Duration
Number of Subjects
(Gender)
Reported Results
Reference
Once/day:
-60 mg, 90 mg
ephedrine
-4 healthy subjects
-ephedrine increased diastolic blood pressure at 60 or 90 mg/day
-not enough statistical power to continue this study
Drew et al.,
1978
Once/day:
-50 mg
ephedrine
-12 healthy subjects
-no changes in diastolic blood pressure at doses up to 50 mg/day
Bye et al.,
1974
Initial enrollment:
Active = 83;
Placebo=84
ACUTE PHASE
Boozer et
al., 2000
Obese Subjects
Three/day: 90
mg/day ephedrine
alkaloids in ephedra
+ 192 mg/day
caffeine
Obese healthy
individuals: sex not
specified.
Acute
Phase 1-4
Weeks
Chronic
Phase 6
months
- systolic blood pressure was greater at week 4 in the Active group
-initial heart rate in the Active group was significantly less than Placebo, while at
week 4 Active showed statistically significant increase in heart rate
-no significant change for ventricular events, or tachycardia
Active = 69;
Placebo=68
-Active Group:46
CHRONIC PHASE
-Placebo Group: 38
-self-reported symptoms in Active consisted of dry mouth, heart burn, insomnia
and diarrhea
Boozer et
al., 2000
-symptoms such as chest pain, palpitation, irritability, nausea and constipation
were similar among Active and Placebo group.
-it was reported that blood pressure was transiently increased and heart rate
persistently increased; however, cardiac arrhythmias were not increased.
Abstract findings, full study details and findings are pending publication
Council for Responsible Nutrition
December 19, 2000
76
Table 4.2-1
Frequency and
Total Dose
(mg/day)
Three/day: 36
mg/day ephedrine +
120 mg/day
caffeine
Index of All Clinical Studies Reviewed
Duration
6 weeks
Three/day: 72
mg/day ephedrine +
240 mg/day
caffeine
Number of Subjects
(Gender)
Obese, healthy
individuals, sex not
specified
26 enrolled: 15
continued
Reported Results
-no serious adverse events occurred
Reference
Huber, 2000
-general symptoms such as cardiovascular, skin, urinary tract, musculoskeletal,
sexual function, nervous system, endocrine/metabolic, gastrointestinal and
respiratory system were assessed for adverse events
-a thorough metabolic check list was also evaluated
-it was reported that there were no significant increases in blood pressure or heart
rate, or other cardiovascular changes
Placebo
26 enrolled: 19
continued
Huber, 2000
Three/day: 36 mg
ephedrine
21 enrolled: 14
continued
Huber, 2000
Three/day: 72
mg/day ephedrine +
300 mg/day
caffeine
21 enrolled: 14
continued
Council for Responsible Nutrition
December 19, 2000
26 enrolled;19
continued
77
Table 4.2-1
Frequency and
Total Dose
(mg/day)
Three/day: 30 mg
ephedrine + 300 mg
caffeine (given to
individuals <80 kg)
Index of All Clinical Studies Reviewed
Duration
20 weeks
Number of Subjects
(Gender)
Obese adolescents.
Placebo: 13
Active: 16 (not
specified which
group, low or high
given)
Three/day:60 mg
ephedrine + 600 mg
caffeine (given to
individuals >80 kg)
Reported Results
-side effects were negligible and did not differ between ephedrine/caffeine
mixture and placebo
Reference
Molnár et
al., 2000
-hemoglobin, hematocrit, white blood cell and platelet count, ASAT, LDH,
bilirubin, ALP, serum albumin and creatinine were in the normal range in all
patients at baseline and remained there at weeks 8 and 20.
-blood pressure and heart rate values showed no significant changes during the
trial in either group.
-withdrawal symptoms following termination of dosing were monitored and were
reported as mild, and transient, and their frequencies were not different between
ephedrine/caffeine mixture and placebo
6 months
Twice/day: 48
mg/day ephedra
Twice/day: 24
mg/day ephedra
Twice/day: 72
mg/day
ephedra+200 mg
caffeine
Council for Responsible Nutrition
December 19, 2000
Obese healthy
individuals, sex not
specified
N=20
-adverse symptoms reported during the course of study were stated to be at an
extremely low frequency
Huber, 1999
-neither systolic nor diastolic blood pressure increased while the subjects were on
ephedra-containing or caffeine-containing dietary supplements
N=44
N=58
78
Table 4.2-1
Frequency and
Total Dose
(mg/day)
Index of All Clinical Studies Reviewed
Duration
Number of Subjects
(Gender)
Reported Results
Reference
Once/day: 72mg
ephedrine + 240 mg
caffeine
-8 weeks
-67 obese subjects
(sex not specified)
-in subjects who completed the study, the treatment vs. placebo resulted in;
-dry mouth (5 vs. 1)
-heart palpitations (2 vs. 2)
-blood pressure (>20 treatment)
-systolic (2 vs. 0)
-diastolic (1 vs. 1)
-insomnia (9 vs. 2)
-constipation (1 vs. 4)
-extra menstrual bleeding (1 vs. 2)
-drop-outs reported included heart palpitations, irritability, increased systolic
blood pressure
Nasser et al.,
1999
Once/day:
Group I: placebo
-10 days
-27 obese women
otherwise healthy,
n=9 per group.
-no cardiac
disturbances or
arterial hypertension
before test
-no change in systolic pressure, cardiac load or peripheral resistance
-diastolic pressure and heart rate were increased in group III compared to control
-information on adverse effects was not reported in the study
Waluga et
al., 1998
Group II: 50 mg
ephedrine +
400 caffeine
Group III: 50 mg
ephedrine + 400 mg
caffeine +10 mg
yohimbine
Council for Responsible Nutrition
December 19, 2000
79
Table 4.2-1
Frequency and
Total Dose
(mg/day)
Index of All Clinical Studies Reviewed
Duration
Number of Subjects
(Gender)
Reported Results
Once/day:
5 treatment groups:
-ephedrine (50 mg)
-ephedrine (50
mg)+ caffeine (150
mg
-ephedrine (50 mg)
+ ASA (330 mg)
-ephedrine (50 mg)
+ caffeine (150 mg)
+ ASA (330 mg)
-placebo
-12 weeks
-163 healthy
premenopausal obese
women
-placebo-controlled, double blind design
-heart rate, blood pressure, clinical signs were assessed
-energy expenditure, blood glucose, triglycerides, total cholesterol, HDL, DLL
evaluated
-Exclusion criteria: hypertension, heart disease, gastric ulcer or other serious
medical conditions
-cholesterol, DLL and glucose were decreased in all groups but were increased in
the placebo group
-the authors concluded that treatment with ephedrine, caffeine and ASA improved
fat loss and health risk factors in obese women
-study design stated that symptoms were evaluated and monitored; however, no
information on adverse effects was reported
Moheb et
al., 1998
3/day:
60 mg ephedrine +
600 mg caffeine
-15 week
study
n=50 in ephedrine/
caffeine group
n=38 who completed
trial
-effects were reported in 54% of the treatment group
-central nervous system side-effects, especially agitation
-effects were most prevalent during the first month of treatment but subsided
markedly as study progressed
-rapid decline in events after first week of treatment
-drop outs complained of vomiting, abdominal pain, tremor, palpitations and
syncope, vertigo, nausea and insomnia. All symptoms disappeared after cessation
of trial
-no serious adverse effects were reported during the study
Breum et al.,
1994
-15 week
follow-up
period
-85 patients were
included in follow up
-9 in the ephedrine/caffeine group complained of transient ADRs
-no serious side-effects were observed during the follow-up study
Breum et al.,
1994
Council for Responsible Nutrition
December 19, 2000
Reference
80
Table 4.2-1
Frequency and
Total Dose
(mg/day)
Index of All Clinical Studies Reviewed
Duration
Number of Subjects
(Gender)
Reported Results
Reference
Herbal formulation
(dose information
not specified and
limited report due
to abstract)
-4 week
-100 patients
-double-blind, placebo, crossover protocol
-100 subjects randomly assigned to placebo or treatment
-body composition tests, blood chemistry, resting heart rates and blood pressures
were obtained weekly with self reports of energy
-it was reported that there were no significant changes in blood pressure or
resting heart rates
Kaats and
Adelman,
1994
3/day:
60 mg
ephedrine:600 mg
caffeine
-8 week
-41 obese but
otherwise healthy
women
-placebo-control, double blind design
-effect of caffeine and ephedrine treatment on a low calorie diet
-plasma total and HDL cholesterol and triglyceride concentrations were assessed
basally on the day before the start of the diet period and on the 4 th and 8th weeks
during dieting
Buemann et
al., 1994
Twice/day: 100 mg
ephedrine
-1 week
-27 obese
adolescents
-screened for endocrine disorders, medication, smoking status, drinking status
and exercise fitness
-the thermogencic effect of ephedrine was investigated
-it was reported by the study authors that side effects were not observed
Molnár,
1993
3/day:
Phase I Study:
75 mg ephedrine +
150 mg caffeine +
330 mg ASA (for
first 4 weeks)
-8 weeks
-11 subjects in
ephedrine, caffeine,
ASA group
-effects reported in 3/11 subjects were transient jitteriness, dry mouth and
constipation
-the study reported that there was no significant difference in frequency in any
adverse effects, which did not persist
-no significant changes were observed in systolic blood pressure, diastolic blood
pressure, mean arterial blood pressure or heart rate
Daly et al.,
1993
Council for Responsible Nutrition
December 19, 2000
81
Table 4.2-1
Frequency and
Total Dose
(mg/day)
3/day:
Phase I Study:
75 mg ephedrine +
150 mg caffeine +
330 mg ASA (for
first week)
Index of All Clinical Studies Reviewed
Duration
Number of Subjects
(Gender)
Reported Results
Reference
-8 weeks
-8 women and 1 man
in ephedrine,
caffeine and ASA
group
-8 women completed the study, but the man was unable to tolerate the higher
dose of ephedrine after week 1 due to jitteriness and mild hypertension. He had
an undisclosed history of borderline hypertension.
-effects reported were transient dry mouth
-no significant difference in the frequency of any adverse effects and in these 8
subjects.
-no adverse effect persisted throughout the study
Daly et al.,
1993
-7 to 26
months
-6 patients from
Phase II study
continued
-6 of 8 subjects who completed Phase II, agreed to continued on treatment to
assess longer term efficacy and safety and were monitored for 7 to 26 months
-all subjects reported effects such as dry mouth or constipation.
-blood pressure and heart rate remained normal
-it was concluded by study authors that the treatment was well tolerated
-no significant adverse effects were found in study subjects
Daly et al.,
1993
-2 weeks
-10 obese subjects
-it was reported that tolerance was good and no adverse effects were observed
throughout the study
Pasquali et
al., 1992
3/day
Phase II
150 mg ephedrine +
150 mg caffeine +
330 mg ASA (for
weeks 2 - 8)
3/day:
Phase III: patients
who completed
Phase II
volunteered to
continue the 150
mg ephedrine + 150
mg caffeine + 330
mg ASA dose for 726 months.
3/day:150 mg
ephedrine
Council for Responsible Nutrition
December 19, 2000
82
Table 4.2-1
Frequency and
Total Dose
(mg/day)
3/day: 60 mg
ephedrine + 600 mg
caffeine
Index of All Clinical Studies Reviewed
Duration
Number of Subjects
(Gender)
-24 weeks
-180 obese patients
were randomized to
3 groups and
maintained on a low
energy diet
-n=45 in E+C group
-n=45 in E group
-blood pressure, heart rate and adverse effects were monitored
-ECG, fasting blood glucose, total cholesterol, triglyceride, hematology,
biochemical screening, analysis of urine were evaluated at weeks 12 and 24
-systolic and diastolic blood pressure decreased significantly in all treatment
groups
-at week 24, significant decreases in blood glucose, triglyceride and total
cholesterol were found in all groups without group differences
-all other measured variables, such as hematology, sodium, potassium, bilirubin,
liver enzymes, creatinine, uric acid and urine analyses were without any
significant differences.
-study results showed that at week 4, significantly more patients in the treatment
group 60% ephedrine/caffeine mixture vs. 44 in ephedrine mixture reported at
least 1 adverse effect
-by week 8, there was no statistically significant differences between symptom
reporting among all groups and adverse effects greatly diminished
Astrup et al.,
1992;
Toubro et
al., 1993a
-24 week
follow up
-127 patients from
original study: all
patients received
same treatment
-n=30 in E+C group
-n=31 in E group
-reactions were experienced by 102 patients during the study from week 26 to 50
-distribution showed that the majority of the symptoms (75%) occurred during the
first 4 weeks: most frequently reported central nervous symptoms were tremor,
agitation, insomnia, increased sweating and nervousness; palpitations and
tachycardia were also reported
-the authors reported that these effects were temporary and did not persist
Toubro et
al., 1993b
n=11 obese
volunteers in the
ephedrine, caffeine
and ASA group (sex
not specified)
-transient jitteriness and transient dry mouth reported but no statistical
significance between placebo group
Krieger et
al., 1990
3/day:
60 mg ephedrine
3/day:
60 mg ephedrine +
600 mg caffeine
3/day:
75 mg ephedrine
(first 4 weeks) then
150 mg ephedrine
next 4 weeks
-8 weeks
Reported Results
Reference
n=13 placebo
Council for Responsible Nutrition
December 19, 2000
83
Table 4.2-1
Index of All Clinical Studies Reviewed
Frequency and
Total Dose
(mg/day)
Duration
Number of Subjects
(Gender)
Reported Results
Reference
3/day:60 mg
ephedrine
-3 months
-5 obese women
-it was reported that effects were few
-only 2 subjects reported transient hand tremor the first 2-5 days
-blood pressure was increased but not significantly (blood pressure only
measured during treatment week 4)
-all subjects completed the study
Astrup et al.,
1985
3/day:
Group I: placebo
Group II: 75 mg
ephedrine
Group III: 150 mg
ephedrine
-3 months
Group I: n-16
Group II: n=13
Group III:n=17
-effects such as agitation, insomnia, headache, weakness, palpitation, giddiness,
tremor and constipation were present in the group treated with 150 mg/day but
disappeared with time, and was reported to be well tolerated
-a statistically significant difference between incidence of effects was reported for
the 150 mg/day group compared to placebo; increase in pulse rate
-no significance was reported in subjects treated with 75 mg/day compared to
placebo with respect to adverse effects
-no significant compound-related effects were present on arterial blood pressure
in any treatment group
Pasquali et
al., 1985
3/day: 150 mg
ephedrine
-1 month
-10 low-energy
adapted obese
women
-it was reported that the incidence of effects was very rare and only a few women
during the first month presented mild forms of agitation, insomnia, palpitation or
giddiness while taking ephedrine
-no significant changes in arterial blood pressure pulse rate were found
Pasquali et
al., 1987
-16 male youths with
asthma
-effects for ephedrine were lowest on own, than together with any agent
-ephedrine taken together with theophylline resulted in adverse effects which
made treatment unacceptable to 50% of participants
Bierman et
al., 1975
Asthmatic Volunteers
Once/day:
25 mg ephedrine
-24 hours
25 mg ephedrine +
130 theophylline
25 mg ephedrine +
10 mg hydroxyzine
HCl
Council for Responsible Nutrition
December 19, 2000
84
Table 4.2-1
Frequency and
Total Dose
(mg/day)
Index of All Clinical Studies Reviewed
Duration
Number of Subjects
(Gender)
Reported Results
Reference
3/day:
75 mg ephedrine +
15 mg of terbutaline
-3 to 12
months
-41 chronic asthmatic
patients
-heart rate, blood pressure, electrocardiograph, hematocrit, red and white cell
counts, urinalysis and plasma chemistries were evaluated
-effects were evaluated by daily patient diary
-cardiovascular changes following onset of treatment therapy were of relatively
small magnitude
-heart rate and blood pressure were not adversely effected
-urinalysis, blood counts and chemistries, electrocardiograms, and physical and
ophthalmologic examinations remained within normal limits or demonstrated no
new abnormalities for ephedrine treatment
-initial study duration was 3 to 6 months; however, the good tolerability
experienced in this study extended the duration of study to 12 months
-22 patients completed 12 months of study
Wilson et
al., 1976
3/day:
60 mg ephedrine +
600 mg caffeine
-6 weeks
-136 obese patients
-112 patients
completed trial
-hypertensive patient + betablocker therapy+ (ephedrine/caffeine) = 25 subjects
-hypertensive patient + hypertensive therapy + (ephedrine/caffeine) = 28 subjects
-normotensive patient + (ephedrine/caffeine) = 28
-hypertensive patient + placebo = 28
-normotensive patient + placebo = 25
-systolic blood pressure was reduced significantly in the hypertensive group
treated with antihypertensive agents plus the E+C (no change in other groups)
-in the normotensive group tested with E+C, both systolic and diastolic blood
pressure were reduced significantly
-heart rate increased significantly only in normotensive patients receiving E+C
-with respect to effects, E+C group, 41 out of 81 patients reported:, nausea
(12%), palpitations (10%), increased perspiration (6%), and tremor (5%)
-6 patients (7%) with withdrew from the E+C group due to side-effects
-in the placebo group, 21% had effects
-the authors reported that no serious events occurred
-E+C did not increase blood pressure in either normotensive or hypertensive
patients during short term treatment
-a significant increase in heart rate was demonstrated in the normotensive group
which was attributed to the pharmacological effect of E+C
-the study did not support the assumption that E+C would cause significant blood
Ingerslev et
al., 1997
Council for Responsible Nutrition
December 19, 2000
85
Table 4.2-1
Frequency and
Total Dose
(mg/day)
Index of All Clinical Studies Reviewed
Duration
Number of Subjects
(Gender)
Reported Results
Reference
pressure rises in normotensive, or well-treated hypertensive, obese patients,
either at the beginning of the treatment or after 6 weeks of treatment.
-the antihypertensive effect of betablockers was not impaired by E+C
3/day:
60 mg ephedrine +
600 mg caffeine
1 year
Council for Responsible Nutrition
December 19, 2000
-225 heavy smokers:
randomized 2/3 to
treatment and 1/3 to
placebo
n=152 (ephedrine/
caffeine)
n=73 placebo
-subjects in the treatment group reported significantly more palpitations,
sweating, dizziness, and nausea during the first week
-differences between treatment and placebo group leveled off during the
following weeks
-difficulty falling asleep at weeks 1 and 3 was reported but not later
-6 subjects in the treatment group withdrew due to effects which subsided the day
after cessation of treatment
-the study reported good tolerability of 60 mg/day of ephedrine together with 600
mg of caffeine in a heavy smoking population wanting to quit smoking.
Norregaard
et al., 1996
86
4.2.1
Clinical Trials and Investigations in Normal Healthy Individuals
Nine studies in normal healthy individuals investigated the effects of ephedrine intake (Bye et al.,
1974; Drew et al., 1978; Kuitunen et al., 1984; Astrup et al., 1991; Astrup and Toubro, 1993;
Liu et al., 1995; White et al., 1997; Gurley et al., 1998a; Shannon et al., 1999). Ephedrine
exposures involved oral administration over a short duration such as 24 hours. No long-term
studies were identified in a population of generally healthy individuals. The range of total doses
within these 9 studies was from 10 to 150 mg/day, given at a frequency of 1 to 3 times/day to
achieve the daily maximum specified. Table 4.2.1-1 tabulates the acute human data in a healthy
population by reverse chronology.
Council for Responsible Nutrition
December 19, 2000
Table 4.2.1-1
Total Dose
(mg/day)
Summary of Ephedrine Intake in Humans and Safety
Duration
Number of Subjects
(Gender)
Reported Results
Reference
Acute Normal Healthy Studies
3/day:
150 mg
ephedrine
24 hours
-10 healthy subjects (6
male and 4 female)
-double-blind, randomized, placebo-control, 2-period crossover study
-all subjects underwent a thorough clinical examination, ECG, admission
urinalysis and blood work
-7 subjects taking ephedrine reported the following reactions: difficulty sleeping
(n=5);increased/stronger heart beat (n=4);decreased appetite (n=3)
-all subjects completed study, and no serious adverse effects reported
Shannon et
al., 1999
once/day:25 mg
ephedrine
24 hours
-10 healthy subjects (5
male and 5 female)
-double-blind, randomized, crossover study with 4 phases
-eligibility determined by results of a medical history, brief physical examination,
medication history, and a pregnancy test for females
-candidates who were in good health, not pregnant, and not taking continuous
medications were selected
-all subjects experienced minor side effects such as tachycardia, anxiety,
headache, irritability, insomnia and loss of appetite (frequency was not reported)
-all subjects completed study with no major side effects reported
Gurley et al.,
1998a
Council for Responsible Nutrition
December 19, 2000
88
Table 4.2.1-1
Total Dose
(mg/day)
Summary of Ephedrine Intake in Humans and Safety
Duration
Number of Subjects
(Gender)
Reported Results
Reference
twice/day: 38.8
mg ephedrine
alkaloids in ma
huang
24 hours
-12 healthy
nonsmoking subjects
(6 male/6 female)
-test article and meals were administered by study investigators
-caffeine intake was monitored
-no adverse effects were noted by any of the 12 participants during both
monitoring phases with respect to cardiovascular effects
-6 of 12 participants demonstrated a statistically significant increase in mean 12hour heart rate after receiving ma huang
-3 participants had a slight increase in heart rate which was not statistically
significant and 3 remained unchanged from baseline.
-4 participants experienced statistically significant increases in systolic blood
pressure which was not associated with clinical signs
- heart rate increased in 6 participants during the first 3 hours of administration
from approximately 72 bpm to 81 bpm; although statistical significance was met,
no participant described symptoms or tachycardia or palpitations
-the cardiovascular findings in this study indicate moderate pharmacodynamic
effects observed, but the dosage of 19.4 mg was not large enough to elicit
significant cardiovascular changes in all participants
White et al.,
1997
once/day: 30 mg
ephedrine
24 hours
-9 health male
volunteers
-heart rate and blood pressure showed a progressive small increase resulting in a
mean increase of 5 beats/min
-systolic blood pressure was shown to increase significantly in all treatments of
14 mm Hg, but taking into account changes in placebo group, showed only 99
mm Hg different
-diastolic blood pressure was not significantly changed following ephedrine
administration
-no adverse effects were reported in this study
Liu et al.,
1995
Council for Responsible Nutrition
December 19, 2000
89
Table 4.2.1-1
Total Dose
(mg/day)
once/day:
-10, 20, 40 mg
ephedrine
Summary of Ephedrine Intake in Humans and Safety
Duration
24 hours
Number of Subjects
(Gender)
-12 healthy subjects (6
male and 6 female)
100, 200, 400
mg caffeine
Reported Results
-diastolic blood pressure did not change after ephedrine intake
-at 40 mg there was an increase of 5 mm Hg in systolic pressure
-heart rate increased dose-dependently after ephedrine intake
-adverse effects were not more frequent following the ephedrine doses than after
placebo administration (data not shown)
Reference
Astrup and
Toubro,
1993
-caffeine at doses up to 200 mg/day had only modest and clinically irrelevant
effects on blood pressure and heart rate
-no adverse effects were reported in the subjects
-caffeine at 400 mg/day had some clinical effect; however, details were not
provided.
ephedrine +
caffeine :
-10 mg:100 mg
-20 mg:100 mg
-20 mg:200 mg
-ephedrine and caffeine mixtures resulted in an average 5 to 7 mm Hg increase
compared to placebo, which was greater than the predicted additive value
-E+C 20mg:100 mg and 20 mg:200 mg increased heart rate slightly more than
placebo, while 10 mg:200 mg was without significant effect
-no information on adverse effects was reported for this group.
once/day:
-10 mg, 20 mg
ephedrine
24 hours
-6 lean healthy subjects
(3 male and 3 female)
-at both ephedrine doses, increased in heart rate more than placebo
-systolic blood pressure was minimally changed with no statistical significance
-adverse effects were assessed, and none was reported
-mixtures (10 mg ephedrine:200 caffeine; 20 mg ephedrine:100 caffeine and 20
mg ephedrine:200 caffeine) resulted in statistical changes in systolic blood
pressure. Diastolic blood pressure increased in 20/200 and 10/200.
Astrup et al.,
1991
24 hours
-43 healthy subjects;
22 females and 21
males
-ephedrine significantly increased systolic blood pressure and heart rate
-information on adverse effects was not reported
Kuitunen et
al., 1984
-combinations
(eph/caff)
-10 mg:200 mg
-20 mg:100 mg
-20 mg:200mg
once/day:
-30 mg, 40 mg
ephedrine
Council for Responsible Nutrition
December 19, 2000
90
Table 4.2.1-1
Total Dose
(mg/day)
Summary of Ephedrine Intake in Humans and Safety
Duration
Number of Subjects
(Gender)
Reported Results
Reference
once/day:
-60 mg, 90 mg
ephedrine
24 hours
-4 healthy subjects
-ephedrine increased diastolic blood pressure at 60 or 90 mg/day
-not enough statistical power to continue this study
Drew et al.,
1978
once/day:
-50 mg
ephedrine
24 hours
-12 healthy subjects
-no changes in diastolic blood pressure at doses up to 50 mg/day
Bye et al.,
1974
Council for Responsible Nutrition
December 19, 2000
91
Shannon et al. (1999) studied the acute effects of ephedrine on 24-hour energy balance,
mechanical work and urinary catecholamines in a double-blind, randomized, placebo-controlled,
2-period crossover study. Ten healthy volunteers (6 male and 4 female) were given 50 mg
ephedrine tablet or placebo 3 times during each of two 24-hour periods. Subjects were nonsmokers and were not taking any medication. The study lasted a total of 21 days, consisting of a
7-day baseline period, sequence 1 to Day 14, and sequence 2 to Day 21, with tablet
administration on Day 14 and 21. All subjects underwent a thorough clinical examination, ECG,
admission urinalysis and blood work. Measurements were taken of 24-hour energy expenditure,
mechanical work, urinary catecholamines and binding of ephedrine in vitro to human 1-, 2- and
3- adrenoreceptors. With ephedrine treatment, 7 subjects reported difficulty sleeping (n=5),
increased or stronger heart beat (n=4) or decreased appetite (n=3). Less frequently reported
effects were skin tingling, coldness of hands and feet, and mouth dryness. With placebo, 1
subject reported heart pounding and difficulty sleeping; another reported a brief period of
palpitations and decreased appetite. All subjects completed the study, and there were no serious
adverse events reported. With result to energy expenditure, acute ephedrine treatment at
relatively high doses (50 mg, 3 times/day) was associated with increased 24-hour energy
expenditure by 3.5%. The increase in energy expenditure could not be explained by any increase
in physical activity.
Originally reviewed in the pharmacokinetic section (Section 2.4.1), the information related to
safety is reviewed, and details of study design are reiterated. Gurley et al. (1998a) examined the
pharmacokinetics in 10 subjects (5 male and 5 female) subsequent to the ingestion of a dietary
supplement containing Ephedra sinica. The study was a randomized, crossover study with 4
phases which characterized the pharmacokinetics of ephedrine after the ingestion of 3
commercially available ma huang products compared with a 25 mg ephedrine capsule.
Eligibility was determined by the results of a medical history, brief physical examination,
medication history, and a pregnancy test for female subjects. Those candidates who were in good
health, not pregnant, and not taking continuous medications were selected. Subjects agreed not
to consume any medication or alcohol for the duration of the study. The nutritional supplements
contained 1 or more of the following ingredients; astragalus, bee pollen, caffeine, Camellia
sinensis, Centella asiatica, Cola nitida, d-alpha tocopherol, Ginkgo biloba, Glycyrrhiza glabra,
Panx ginseng, Paullinia cupana, Spirulina pratensis, and Triticum aestivum. On Day 1, after an
8-hour fast, an oral dose of medication and 8 oz of water were administered at 7 am. Subjects
were then asked to refrain from eating for an additional 4 hours. A 1-week washout phase
occurred between ingestion of each of the 4 products. It was reported that all subjects
experienced minor effects typical of ephedrine alkaloids. These effects included tachycardia,
anxiety, headache, irritability, insomnia, and loss of appetite (frequency not reported).
Council for Responsible Nutrition
December 19, 2000
92
Originally reviewed in the pharmacokinetic section (Section 2.3.1), the information (White et al.,
1997) related to safety is reviewed and details of study design are reiterated concerning the
pharmacokinetics and cardiovascular effects of ma huang in normotensive adults. The primary
stated goal of this study was to determine if ingestion, of the manufacturer’s recommended doses
of an herbal product containing ma huang, induced changes in blood pressure and heart rate in
normotensive participants. In addition, the study authors measured the variability of ephedrine
and pseudoephedrine content among capsules of the same lot to determine the agreement among
stated doses. Lastly, the study authors determined the pharmacokinetic parameters of ephedrine
and pseudoephedrine in participants who ingested ma huang at doses recommended by package
labeling. Twelve normotensive volunteers, 6 women and 6 men participated in the study. All
participants were nonsmokers and were classified as normotensive based on mean systolic and
diastolic blood pressures. Participants were not taking any other medications known to cause
changes in blood pressure or heart rate. In Phase I (control phase), all participants underwent
ambulatory blood pressure monitoring every 15 minutes from 7 am until 8 pm In Phase II
(treatment phase), the participants again wore the ambulatory blood pressure monitor for the
same time period. At 8 hours, each participant ingested 4 capsules of a powdered ma huang
product. At 17 hours, participants ingested another 4 capsules with their evening meals. The
ephedrine alkaloid content of each 4-capsule dose (labeled 375 mg E. sinica ) was determined by
HPLC to be 19.4 mg ephedrine, 4.9 mg pseudoephedrine and 1.2 mg methylephedrine (38.8 mg
ephedrine total/day).
The study investigators administered the supplement product and all meals during the study.
Caffeine intake was also monitored to ensure that it remained consistent from Phase I to Phase II.
Study participants were moderately mobile but stayed on site during the study. Pharmacokinetic
parameters of ephedrine were determined from plasma concentration-time profiles.
Blood pressure and heart rate data from the first hour were excluded from the analysis due to the
known transient increases from ambulatory blood pressure monitors. No adverse effects were
noted by any of the 12 participants during both monitoring phases with respect to cardiovascular
effects. Six of 12 participants demonstrated a statistically significant increase in mean 12-hour
heart rate after receiving ma huang. Three participants had a slight increase in heart rate which
was not statistically significant and 3 remained unchanged from baseline. With respect to blood
pressure, 4 participants experienced statistically significant increases in systolic blood pressure,
but 2 had a significant decrease in diastolic blood pressure. It was reported that none of the
changes was associated with symptoms, nor were they considered to be clinically significant.
Heart rate increased in 6 participants during the first 3 hours of administration interval from
Council for Responsible Nutrition
December 19, 2000
93
approximately 72 bpm to 81 bpm; although statistical significance was met, no participant
described symptoms of tachycardia or palpitations. The cardiovascular findings in this study
indicate moderate pharmacodynamic effects observed, which may be due to the relatively low
dose of ephedrine contained within this product (~4.84 mg/tablet; 19.4 mg/dose; 38.8 mg
total/day), which was not large enough to elicit significant cardiovascular changes in all
participants.
Liu et al. (1995) investigated ephedrine-induced thermogenesis in healthy young male
volunteers. The study enrolled 9 healthy male volunteers, mean age of 24 years old, with no
history of asthma, cardiac dysarrhythmia, hypertension, diabetes, or thyroid disease. All subjects
were non-smokers and all were not taking any concurrent medications. Oral doses of placebo or
30 mg of ephedrine chloride were given in a single-blind crossover design with 5 days between
testing. Blood was drawn at (15 minutes prior to ingestion), 0, 20, 40, 60, 90, 120, 150, and 180
min relative to the intake of either ephedrine or placebo. Heart rate and blood pressure were
measured every 30 minutes. Ephedrine produced significant increases in energy expenditure
(thermogenesis), heart rate, systolic blood pressure, and plasma glucose. More specifically,
ephedrine intake resulted in a small, progressive increase in heart rate throughout the 3-hour
period, resulting in a mean increase of 5 beats/min compared to basal values (P<0.05). Systolic
blood pressure was shown to increase significantly in all treatments including placebo. The
increase in systolic blood pressure in the ephedrine-treated group was 14 mm Hg (P<0.001);
however, when taking into account the changes in the placebo group, there was a mean increase
of only 9 mm Hg after ephedrine intake. Diastolic blood pressure was not significantly changed
following ephedrine administration. Ephedrine treatment induced a significant increase in
plasma glucose with the peak increase seen at 40 minutes after the intake of ephedrine.
Astrup and Toubro (1993) reported on the acute thermogenic, metabolic, and cardiovascular
effects of different doses of caffeine and ephedrine given separately, and in combination, to
normal subjects. Twelve healthy subjects (6 male and 6 female) with normal body weights
underwent a series of evaluations following administration of ephedrine at 10, 20, and 40 mg;
caffeine at 100, 200, and 400 mg and 2 placebo treatments, in a double-blind, placebo-controlled
fashion. At least 3 days elapsed between 2 consecutive tests. In addition to testing the
compounds alone as an extension of the first trial, 3 different combinations of ephedrine and
caffeine were evaluated. Results from the ephedrine group showed that diastolic blood pressure
did not change after ephedrine intake, and only after 40 mg of ephedrine was a 5 mm Hg increase
in systolic pressure observed. Heart rate increased dose-dependently after ephedrine intake. It
was reported that adverse effects were not more frequent following the ephedrine doses than after
placebo administration (data not shown). All 3 dose levels of ephedrine increased energy
Council for Responsible Nutrition
December 19, 2000
94
expenditure, but no linear dose relationship was observed. Dose-dependent, slight increases were
found in plasma glucose and lactate concentration. Ephedrine had no effect on lipid metabolism.
Caffeine intake was related to a linear relationship between dose and thermogenic response, at
100 and 400 mg compared to placebo. It was reported that caffeine at doses up to 200 mg/day
had only modest and clinically irrelevant effects on blood pressure and heart rate, and resulted in
no reported subjective adverse effects in the subjects. Caffeine at 400 mg/day reportedly had
some clinical effect; however, details were not provided.
Combination intake of ephedrine and caffeine (E+C) was compared with their components given
separately. The thermogenic effect after E+C (20 mg:200 mg) was larger than that of the 2 other
combinations, and in this mixture E and C exerted a supra-additive thermogenic synergism,
while the responses of the other 2 mixtures at 10 mg:200 mg and 20 mg:100 mg were only
additive. The effect on glucose and lipid metabolism was generally an additive synergism as
predicted from responses observed after the components were given separately. The post-intake
increase in blood pressure after all 3 mixtures averaged 5 to 7 mm Hg more than placebo. The
E+C 20mg:100 mg and 20 mg:200 mg increased heart rate slightly more than placebo, while 10
mg:200 mg was without significant effect.
In a related study, Astrup et al. (1991) reported the effects of caffeine on thermogenic, metabolic
and cardiovascular effects in healthy volunteers. The study tested doses of 100, 200, and 400
mg/day on 6 experimental subjects administered via gelatin capsules. Small, but not statistically
significant, changes in systolic and diastolic blood pressure after 100 and 200 mg caffeine were
observed. In contrast, 400 mg caffeine increased systolic blood pressure, and similarly increased
diastolic blood pressure. It was reported that at the highest dose of caffeine tested, an increase in
heart rate significantly above the baseline was observed.
Few effects were reported after 100 mg, 200 mg or placebo treatment; however, at 400 mg
caffeine, significantly more subjects reported effects compared with placebo (p<0.01); 4 reported
palpitation; 3 anxiety; 3 headache; 2 restlessness, and 1 dizziness. The cardiovascular effects of
caffeine are known in detail because of the studies by Robertson et al. (1978) and Whitsett et al.
(1978). When 250 mg oral caffeine was given to people who do not drink coffee, systolic blood
pressure increased by 10 mm Hg, whereas heart rate showed a biphasic decrease after the first
hour followed by an increase above baseline after 2 hours. In a subsequent study Robertson et al.
(1978) found that during chronic caffeine intake, an essentially complete tolerance developed to
these effects after 1 to 4 days of consumption of 750 mg caffeine/day.
Council for Responsible Nutrition
December 19, 2000
95
In a later study, the thermogenic synergism of ephedrine and caffeine in 6 healthy volunteers (3
male and 3 female) was evaluated by Astrup et al. (1991). Single oral doses of placebo,
ephedrine (10 mg, 20 mg), or caffeine (100 mg or 200 mg) were compared with the effects of 3
different combinations of ephedrine + caffeine (E+C) (10 mg:200 mg, 20 mg:100 mg, and 20
mg:200 mg) in 6 healthy, lean subjects. The study was designed as a placebo-controlled, doubleblind test. Six normal-weight healthy subjects were recruited. None of the individuals was
engaged in regular exercise or taking medicine during the study. One subject smoked
occasionally on weekends. The experimental subjects abstained from food, coffee, tea, cola
beverages, cocoa, chocolate, and smoking overnight (>12 hours) before each test was started in
the morning. Two consecutive tests were separated by at least 3 days. Arterial blood pressure
and heart rate were evaluated. Subjective feelings of adverse effects were assessed by
questioning the experimental subjects after each test substance.
Ephedrine at doses of 10 and 20 mg increased the heart rate over placebo (P<0.05), whereas
caffeine had no effect. In contrast, the combinations ephedrine and caffeine at 20 mg:100 mg
and 20 mg:200 mg increased heart rate more than placebo (P<0.01), whereas ephedrine +
caffeine at 10 mg:200 mg had no effect. Systolic blood pressure was only minimally changed
with no statistical significance with ephedrine or caffeine alone. An increase in systolic blood
pressure of 8 to 10 mm Hg was found after all 3 combinations (P<0.01). Diastolic blood
pressure did not change after most of the doses, except after ephedrine + caffeine 20 mg:100 mg
and 10 mg:200 mg, which increased diastolic blood pressure by about 4 mm Hg more than
placebo which was not statistically different from placebo. All combinations increased plasma
glucose, insulin and C-peptide. It was concluded that the combination of ephedrine and caffeine
at 20 mg and 200 mg, respectively had a favorable thermogenic effect with no marked effect on
mean blood pressure and heart rate.
Kuitunen et al. (1984) studied the acute physical and mental effects of a single oral dose of
ephedrine hydrochloride at 30 or 40 mg in a double-blind placebo-controlled study against other
agents. The participants fasted for 3 hours before administration of the test article and until all
the recordings were taken at 1.5 and 2.5 hours after test article administration. The agents were
given in a double-blind manner. The placebo group consisted of 16 subjects (7 females and 9
males), and the groups receiving ephedrine consisted of 21 females and 21 males. Ephedrine
hydrochloride was given in 30 mg or 40 mg tablets. Each subject received 1 capsule, and the
smaller dose was given to subjects weighing less than 60 kg. The physical parameters that were
measured were arterial pressure, heart rate and tapping rate. Mental activity was evaluated with a
self-rating check list consisting of various adjectives describing mental state in a random order.
The subjects were asked to grade those modalities according to their first impression. Tests for
Council for Responsible Nutrition
December 19, 2000
96
memory, learning and concentration ability were evaluated with a single recording test and a digit
span test. The subjects were instructed to transcribe numbers 0 to 9 to various symbols as fast as
possible for 3 minutes. The score was the number of correctly transcribed symbols at 1.5 and 3
minutes. In the digit span test the subjects were asked to repeat aloud sets of numbers in a given
order and in the reverse order.
Ephedrine significantly increased systolic blood pressure and heart rate compared to placebo. No
significant diastolic pressure changes were observed, and no change in tapping rate was
observed. No changes in mental activity or effects on memory, learning and concentration ability
were observed.
Drew et al. (1978) compared the effects of ephedrine and pseudoephedrine on the cardiovascular
and respiratory systems in 4 healthy volunteers. In a preliminary double blind trial, the effects of
ephedrine and pseudoephedrine on the blood pressure and heart rate of resting healthy volunteers
were compared. Doses of 30, 60 and 90 mg ephedrine hydrochloride and 60, 90, 120, 150, 180,
210, and 240 mg pseudoephedrine hydrochloride were administered in a random double-blind
manner. All the subjects took all the dose levels of each treatment and placebo. Ephedrine at 60
or 90 mg was required to raise the diastolic blood pressure above 90 mm Hg, whereas 210 or 240
mg pseudoephedrine were required to produce the same effect. Changes in heart rate were small,
particularly after pseudoephedrine. No changes in the electrocardiogram other than those from
increased rate were found in any subject receiving any dose of the treatments. Since the number
of subjects studied was too small, an extensive statistical analysis was not applied.
Bye et al. (1974) studied the effects of ephedrine in healthy volunteers on heart rate, and blood
pressure. Twelve healthy volunteers were used in 2 separate trials to study the effect of D(-)
ephedrine and pseudoephedrine separately. D(-)ephedrine was determined to be 4 times as
potent as L(+) pseudoephedrine in producing both tachycardia and a rise in systolic blood
pressure. No changes in diastolic blood pressure occurred in 12 subjects with doses of up to D(-)
ephedrine (50 mg) and L(+)pseudoephedrine (180 mg).
4.2.1.1
Summary of Clinical Trials and Investigations in Normal Healthy Individuals
Typically, studies in healthy populations consisted of small numbers of patients, were not
designed to examine safety and were of limited duration (24 hours). Furthermore, progressive
doses were not assessed, which does not permit analysis of dose-responsiveness of any effects.
Other limitations specific to the studies evaluated include the selective report of incidence and
Council for Responsible Nutrition
December 19, 2000
97
severity of any effects and any withdrawals. Information on possible adverse events was not
reported in several studies due in part to the focus on efficacy.
Nine studies in normal healthy individuals investigated the effect of ephedrine over a range of
doses from 10 to 150 mg/day (Bye et al., 1974; Drew et al., 1978; Kuitunen et al., 1984; Astrup
et al., 1991; Astrup and Toubro, 1993; Liu et al., 1995; White et al., 1997; Gurley et al., 1998a;
Shannon et al., 1999). Although ephedrine exposures involved oral administration over a short
duration such as 24 hours, no adverse effects at doses up to 150 mg/day were identified. In many
of these studies, intake of concomitant drugs/therapies, smoking and caffeine intake was
controlled. Taken altogether, the studies conducted in healthy (normal weight) individuals
support the safety and tolerability profile of ephedrine, albeit these studies were conducted only
for short durations. Furthermore, the investigations on the combination of ephedrine together
with caffeine provide some information in healthy human populations, given that many of the
studies in the obese clinical database have been tested with combination products, and this
combination product is characteristic of many dietary supplements.
4.2.2
Clinical Trials and Investigations of Ephedrine Together with Physical
Exercise/Temperature in Normal Healthy Individuals
It has been reported that among athletes, ephedrine may be used as an ergogenic, or performanceenhancing agent. Athletic competition normally exerts extra demands on the cardiovascular
system, but ephedrine can potentiate those demands even further (Sprague et al., 1998). The
toxicity of sympathomimetic agents can be exacerbated by physical exercise, dehydration and
increases in body temperature (Insel and Motulsky, 1987); hence, the use of sympathomimetics
by recreational and competitive athletes attempting to improve performance, decrease body fat
and increase lean body mass has been suggested to be of particular concern (Catlin and Hatton,
1991). In particular, there have been reports of ephedrine abuse among professional weightlifters
(Gruber and Pope, 1998). Five studies in healthy normal individuals investigated the effects of
exercise/physical parameters together with ephedrine use (Sidney and Lefcoe, 1977; Strömberg et
al., 1992; Vanakoski et al., 1993; Bell et al., 1998; Bell and Jacobs, 1999). Table 4.2.2-1
tabulates these data.
Council for Responsible Nutrition
December 19, 2000
98
Table 4.2.2-1
Total Dose
(mg/day)
Summary of Ephedrine Intake Together with Physical Parameters in Healthy Normal Individuals
Duration
Number of Subjects
(Gender)
Reported Results
Reference
Normal Healthy Individuals with Ephedrine Intake and Exercise/Physical Parameters
once/day:
-81 mg
ephedrine
-405 mg caffeine
24 hours
-8 healthy male
subjects
-repeated measures, double-blind design
-studied the effects of caffeine, ephedrine and their combination on time to
exhaustion during high-intensity exercise
-studied in control session (exercise without treatment) or exercise ergometer
with treatment
-heart rate during exercise was significantly increased for C+E and C trials
compared to placebo
-no increase in heart rate was reported for ephedrine singly
-subjective ratings of perceived exertion during exercise were significantly lower
after C+E compared to placebo
-C+E treatment significantly prolonged exercise time to exhaustion compared to
placebo, while neither C or E alone significantly changed this parameter
-four of the original 12 stopped exercising during the C+E trial because of
nausea, which was reported to be stimulated by exercise. These subjects did not
experience nausea with the other treatments
Bell et al.,
1998
24 hours
-9 healthy male
subjects
-double-blind design
-studied effects of combination on run times in a warrior test
-studied control session (exercise without treatment) or exercise warrior test
session (with treatment)
-run times in the warrior test were significantly improved after C+E treatment
-lower subjective ratings of perceived exertion were observed
-faster running velocity for the warrior test was associated with a higher heart rate
during the C+E trial
-nausea or vomiting was not reported in this trial with treatment
Bell and
Jacobs, 1999
combination
(ephedrine 81
mg + caffeine
405 mg)
-once/day:
375 mg caffeine
and 75 mg of
ephedrine
Council for Responsible Nutrition
December 19, 2000
99
Table 4.2.2-1
Summary of Ephedrine Intake Together with Physical Parameters in Healthy Normal Individuals
Total Dose
(mg/day)
Duration
Number of Subjects
(Gender)
Reported Results
Reference
once/day:
50 mg ephedrine
24 hours
-6 healthy 21-year old
women
-double-blind, placebo controlled, cross over
-subjects were ascertained to be healthy based on a physical examination, ECG
-all subjects except one took no medication during the trial
-all were non-smokers
-subjects received a single dose of 50 mg ephedrine in a control session and in a
sauna session
-ephedrine was absorbed more rapidly and the maximum plasma concentration
occurred earlier than in the control sessions; however, no differences were found
between the elimination half-lives and AUC values.
- systolic blood pressure was significantly higher in the sauna than in the control
session (p<0.01).
-subjectively, ephedrine induced alertness and nervousness (0.001 < p<0.05 vs.
placebo) in both conditions. Ephedrine abolished the sauna-induced calmness.
Vanakoski et
al., 1993
once/day:
-50 mg
ephedrine
24 hours
-6 lean healthy women
-double-blind, placebo controlled, cross over design
-subjects received single doses of 50 mg ephedrine in control session and in an
exercise session
-subjects were ascertained to be healthy by a clinical examination, including ECG
and maximal exercise test on treadmill
-heart rate, blood pressure, critical flicker fusion test, Maddox wing test, and
visual analog scales relating to mood and feelings of tiredness were included
-kinetics of ephedrine were not affected by exercise
-exercise did enhance the tachycardic response to ephedrine and abolished its
blood pressure effects.
Strömberg et
al., 1992
Council for Responsible Nutrition
December 19, 2000
100
Table 4.2.2-1
Summary of Ephedrine Intake Together with Physical Parameters in Healthy Normal Individuals
Total Dose
(mg/day)
Duration
Number of Subjects
(Gender)
Reported Results
Reference
once/day:
-24 mg
ephedrine
hydrochloride
24 hours
-21 healthy males
-double-blind crossover design
-first day of testing, baseline data were collected; second and third day of test, a
pill containing either 24 mg of ephedrine or a lactose placebo was administered
orally approximately 60 minutes before testing
-effects at rest show that a minimal effect on pulse rate and indirect systemic
blood pressure were observed with ephedrine treatment; only diastolic blood
pressure was statistically different
-psychomotor performance was improved compared with placebo data when
based on average scores but not best scores
-ephedrine administration did not affect perception of physical exertion
Sidney and
Lefcoe,
1977
Council for Responsible Nutrition
December 19, 2000
101
Bell et al. (1998) studied the effects of caffeine, ephedrine and their combination on time to
exhaustion during high-intensity exercise. Using a repeated-measures, double-blind design, eight
male subjects exercised on a cycle ergometer at a level which led to exhaustion after 12 minutes
during a placebo control trial. Then they repeated the exercise 1.5 hours after ingesting either
caffeine (5 mg/kg; 405 mg total dose) or ephedrine (1 mg/kg; 81 mg total dose), or both (C+E) or
placebo (P). Trials were separated by 1 week. Heart rate during exercise was significantly
increased for C+E and C trials compared to P. Subjective ratings of perceived exertion during
exercise were significantly lower after C+E compared to P in the 8/12 people who did not stop
due to nausea. The combination of C+E treatment significantly prolonged exercise time to
exhaustion compared to P, while neither C nor E treatments alone significantly changed time to
exhaustion. The improved performance was attributed to increased central nervous system
stimulation. Four of the original 12 subjects stopped exercising during the C+E trial because of
nausea. It was reported that their nausea was stimulated by the exercise and was not reported by
the subjects prior to commencing the exercise. The authors presumed that it was the interaction
of the high-intensity exercise with the caffeine and ephedrine which resulted in the nausea, since
these subjects were able to complete all the other trials uneventfully. In particular, the ephedrine
trial was uneventful. The scope of the experiment did not identify the cause. It was remarked by
the authors that the interaction of ephedrine with caffeine should be investigated systematically
before any application of the ergogenic findings is pursued.
In a subsequent study published by Bell and Jacobs (1999), the ingestion of caffeine and
ephedrine on run times of a Canadian Forces Warrior Test was evaluated. Nine healthy male
recreational runners completed six balanced and double-blind trials of the Canadian Forces
Warrior Test (WT). The trials were performed in sets of two runs, and separated by a minimum
of 7 days. Heart rates were recorded. The subjects were instructed to refrain from consuming
substances containing caffeine the night before the treatment trials. The dose given was 375 mg
of caffeine and 75 mg ephedrine. Plasma from the venous blood samples was assayed for both
caffeine and ephedrine concentration. The main finding in this study was that run time was
significantly improved after C+E treatment. These results extend the previous findings by the
same investigators. From an earlier investigation, it was concluded that the increased ergometer
results were attributed to increased central nervous system stimulation as evidenced by lower
subjective ratings of perceived exertion which were also found in the follow-up study.
Faster running velocity for the WT trial was associated with a higher heart rate during the C+E
trial. Bell and Jacob (1999) reported that no nausea or vomiting occurred during any of the trials
in the investigation.
Council for Responsible Nutrition
December 19, 2000
102
Originally reviewed in the pharmacokinetic section (Section 2.3.1), the information related to
safety is reviewed and details of study design are reiterated. The pharmacokinetics of ephedrine
were investigated in 6 healthy, 21-year old female volunteers before and after exercise
(Strömberg et al., 1992). Before entering the study, the subjects were ascertained to be healthy
by a clinical examination, including resting ECG and maximal exercise test on a treadmill. All
subjects were regularly engaged in physical activity, but none of them participated in competitive
sports. Six healthy volunteers received single doses of 50 mg ephedrine, 15 mg midazolam or
placebo. All treatments were given twice; before exercise (control session) and during exercise.
Relevant safety/tolerability assessments included heart rate, blood pressure, critical flicker fusion
frequency which measures sedative effects of psychotropic drugs, Maddox wing test used to
measure external eye muscle balance, visual analog scales relating to mood and feelings of
tiredness. The pharmacokinetics of ephedrine were not altered by exercise. Ephedrine increased
heart rate and systolic blood pressure 2 hours after administration. It was reported that the heart
rate response was even higher after the exercise, whereas exercise abolished the blood pressure
response.
In a related study, the effects of a sauna on the pharmacokinetics and pharmacodynamics of
ephedrine in healthy young women were investigated (Vanakoski et al., 1993). Six, healthy 21year old women of normal weight volunteered for the study. Before entering the trial, they
underwent a physical examination and a 12-lead ECG. With the exception of one subject, who
used oral contraceptives, the subjects took no medication during the trial and all of them were
non-smokers. Blood samples were taken for clinical laboratory tests. Each subject received in a
double-blind and cross-over fashion single oral doses of 50 mg ephedrine and placebo for control
and sauna sessions. Relevant safety/tolerability assessments included heart rate, blood pressure,
critical flicker fusion frequency and binocular flicker fusion frequency which measures sedative
effects of psychotropic drugs, Maddox wing test used to measure external eye muscle balance,
visual analog scales relating to mood and feelings of tiredness were included in the sessions as
pharmacodynamic measures. The sauna modified the pharmacokinetics of ephedrine. Ephedrine
was absorbed more rapidly and the maximum plasma concentration occurred earlier than in the
control sessions; however, no differences were found between the elimination half-lives and
AUC values. Ephedrine did not significantly modify the results of the critical flicker fusion or
Maddox wing tests in test sauna condition or placebo. Increased systolic blood pressure was
observed in both conditions. Systolic blood pressure was significantly higher in the sauna than in
the control session (p<0.01). Subjectively, ephedrine induced alertness and nervousness (0.001 <
p<0.05 vs. placebo) in both conditions. Ephedrine abolished the sauna-induced calmness. The
authors proposed that the greater systolic blood pressure and heart rate in the sauna due to
ephedrine can better be explained by additional sympathetic activity triggered by greater heat
Council for Responsible Nutrition
December 19, 2000
103
stress than by increased ephedrine concentration. Increased effects on cardiovascular parameters
suggest a pharmacodynamic interaction and also that the effects and adverse-effects of
sympathomimetics may be more marked in a sauna.
Sidney and Lefcoe (1977) studied the effects of ephedrine on the physiological and psychological
responses to submaximal and maximal exercise in man. Twenty-one healthy males, aged 19- to
30-years old, were tested on 3 occasions within 3 weeks with a minimum of 1-day rest between
test sessions. A modified double-blind crossover design was used. On the first day of testing,
baseline data were collected. On the second and third days of test, a pill containing either 24 mg
of ephedrine hydrochloride or a lactose placebo was administered orally, approximately 60
minutes before testing. The effects of ephedrine were determined by comparing the difference
scores for drug versus control to the difference scores for placebo versus control. Effects at rest
showed that ephedrine had only a minimal effect upon pulse rate and indirect systemic blood
pressures. There was apparently a 7 mm Hg increase in pulse pressure when ephedrine was
given; 3 mm Hg rise in systolic pressure and a 4mm Hg decrease in diastolic pressure; only the
diastolic blood pressure change was statistically significant. Effects at submaximal effort
indicated that when ephedrine was administered, the average changes in cardiac frequency were
consistently (but not statistically) less than those seen under placebo conditions. Ephedrine had
no significant effect on either grip strength, endurance, anaerobic capacity, or muscle power.
Psychomotor performance was statistically improved compared with placebo data when based on
average scores but not best scores. Ephedrine administration did not affect perception of
physical exertion during submaximal exercise and during all-out maximal exercise, subjects did
not exert themselves any more when given ephedrine. In summary, it was concluded that
ephedrine did not affect physical performance; however, some physiological changes relative to
placebo were noted which included a widening of resting pulse pressure, minor increases in
exercise heart rates, and a slowing of the rate of recovery following muscular effort.
4.2.2.1
Summary/Discussion of Clinical Trials and Investigations of Ephedrine Together
with Physical Exercise/Temperature in Normal Healthy Individuals
The findings from studies conducted by Sidney and Lefcoe, 1977; Strömberg et al., 1992;
Vanakoski et al., 1993; Bell et al., 1998; Bell and Jacobs, 1999 support the known effects of
physical exercise and of physical parameters, such as increases in body temperature, may have in
combination with sympathomimetic agents. These factors did not result in toxicity from
ephedrine use. No adverse effects were reported in these studies at doses up to 81 mg of
ephedrine/day (duration 24 hours). Results from Bell et al. (1998) indicated a possible
interaction caffeine and ephedrine together with exercise; however, in a subsequent investigation
Council for Responsible Nutrition
December 19, 2000
104
these findings were not confirmed (Bell and Jacobs, 1999). The degree of performance
improvement associated with ephedrine ingestion has not been established (Sidney and Lefcoe,
1977; Smith and Perry, 1992; Gruber and Pope, 1998). Products for performance enhancement
are generally compounded with other ingredients such as vitamins, minerals, and amino acids
(Clarkson and Thompson, 1997).
4.2.3
Obesity Clinical Trials
Clinical trials using ephedrine in the treatment of obesity were used to evaluate the safety of
ephedrine. The clinical studies summarized below primarily examined the effects of ephedrine,
either singly or combined with caffeine or ASA on weight loss in the treatment of obesity. The
studies also provided information on the tolerability and safety of ephedrine-containing
preparations in humans. Given that many dietary supplements containing ephedrine alkaloids are
marketed for weight loss or energy purposes, these data provide useful information on the safe
use of these products in this population. The range of total doses tested in these studies was from
50 to 150 mg/day, involving durations of 10 days to 26 months. These studies are summarized in
Table 4.2.3-1.
The majority of the randomized trials conducted in clinical studies have been investigated in
obese subjects. However, before considering this database, one must consider the possibility that
there may be differences in the sensitivity and/or pharmacokinetic handling of ephedrine in obese
vs. non-obese individuals. Given the known chemical and metabolic characteristics of ephedrine,
differences are unlikely in the sensitivity and/or pharmacokinetic profile of ephedrine in obese
individuals. Review of literature pertaining to issues dealing with sensitivity of adverse events in
lean and obese subjects has revealed conflicting findings. Horton and Geissler (1991) reported
on the effect of ephedrine (30 mg) and ASA (300 mg) on the acute thermogenic response to a
liquid meal in lean and obese women. Analysis of subjective response to treatment showed that
fewer side effects were noted with the treatments in the obese subjects compared to the lean
group. In 2 later studies from the same authors (Geissler, 1993; Horton and Geissler, 1996),
these findings were not confirmed and no such difference in sensitivity was observed. No
significant correlations were found in either the lean or the obese with respect to the number of
side effects. Based on the more recent studies obtained from the same investigators, there is no
compelling evidence that any differences in sensitivities to ephedrine would be expected in lean
vs. obese individuals.
Council for Responsible Nutrition
December 19, 2000
105
Table 4.2.3-1
Total Dose (mg/day)
Summary of Clinical Trials with Obese Subjects Taking Ephedrine
Duration
Three/day: 90 mg/day
ephedrine in ephedra +
192 mg/day caffeine
Acute Phase
1-4 Weeks
Number of Subjects
(sex)
Reported Results
Reference
Initial enrollment:
Active = 83;
Placebo=84
ACUTE PHASE
Boozer et al.,
2000
Obese healthy
individuals: sex not
specified.
- systolic blood pressure was greater at week 4 in the Active group
-initial heart rate in the Active group was significantly less than
Placebo, while at week 4 Active showed statistically significant
increase in heart rate
-no significant change for ventricular events, or tachycardia
-Active Group: 69
Placebo Group: 68
Chronic
Phase 6
months
-Active Group:46
CHRONIC PHASE
-Placebo Group: 38
-self-reported symptoms in Active consisted of dry mouth, heart
burn, insomnia and diarrhea
Boozer et al.,
2000
-symptoms such as chest pain, palpitation, irritability, nausea and
constipation were similar among Active and Placebo group.
-it was reported that blood pressure was transiently increased and
heart rate persistently increased; however, cardiac arrhythmias
were not increased.
Council for Responsible Nutrition
December 19, 2000
106
Table 4.2.3-1
Summary of Clinical Trials with Obese Subjects Taking Ephedrine
Total Dose (mg/day)
Duration
Number of Subjects
(sex)
Reported Results
Reference
Three/day: 36 mg/day
ephedrine + 120 mg/day
caffeine
6 weeks
Obese, healthy
individuals, sex not
specified
-no serious adverse events occurred
Huber, 2000
Three/day: 72 mg/day
ephedrine + 240 mg/day
caffeine
Placebo
Three/day: 36 mg
ephedrine
Three/day: 72 mg/day
ephedrine + 300 mg/day
caffeine
26 enrolled: 15
continued
-general symptoms such as cardiovascular, skin, urinary tract,
musculoskeletal, sexual function, nervous system,
endocrine/metabolic, gastrointestinal and respiratory system were
assessed for adverse events
-a thorough metabolic check list was also evaluated
26 enrolled: 19
continued
-it was reported that there were no significant increases in blood
pressure or heart rate, or other cardiovascular changes
21 enrolled: 14
continued
21 enrolled: 14
continued
26 enrolled;19
continued
Council for Responsible Nutrition
December 19, 2000
107
Table 4.2.3-1
Summary of Clinical Trials with Obese Subjects Taking Ephedrine
Total Dose (mg/day)
Duration
Number of Subjects
(sex)
Reported Results
Reference
Three/day: 30 mg
ephedrine + 300 mg
caffeine (given to
individuals <80 kg)
20 weeks
Obese adolescents.
-side effects were negligible and did not differ between
ephedrine/caffeine mixture and placebo
Molnár et al.,
2000
Placebo: 13
Active: 16 (not
specified which
group, low or high
given)
Three/day:60 mg
ephedrine + 600 mg
caffeine (given to
individuals >80 kg)
-hemoglobin, hematocrit, white blood cell and platelet count,
ASAT, LDH, bilirubin, ALP, serum albumin and creatinine were
in the normal range in all patients at baseline and remained there at
weeks 8 and 20.
-blood pressure and heart rate values showed no significant
changes during the trial in either group.
-withdrawal symptoms were monitored and were reported mild,
transient and their frequency were not different between
ephedrine/caffeine mixture and placebo
6 months
Twice/day: 48 mg/day
ephedra
Twice/day: 24 mg/day
ephedra
Twice/day: 72 mg/day
ephedra+200 mg caffeine
Council for Responsible Nutrition
December 19, 2000
Obese healthy
individuals, sex not
specified
N=20
-adverse symptoms reported during the course of study were stated
to be at an extremely low frequency
Huber, 1999
-neither systolic nor diastolic blood pressure increased while the
subjects were on ephedra-containing or caffeine-containing dietary
supplements
N=44
N=58
108
Table 4.2.3-1
Summary of Clinical Trials with Obese Subjects Taking Ephedrine
Total Dose (mg/day)
Duration
Number of Subjects
(sex)
Reported Results
Reference
once/day:
72mg ephedrine + 240 mg
caffeine
-8 weeks
-67 obese subjects
(sex not specified)
-Exclusion criteria: nursing, pregnancy, continuous medications,
cancer, asthma, enlarged prostate, glaucoma, seizures, migraine
headaches, hypertension, diabetes or major organ illness
-in subjects who completed the study, the treatment vs. placebo
resulted in;
-dry mouth (5 vs. 1)
-heart palpitations (2 vs. 2)
-blood pressure (>20 treatment vs. placebo not reported)
-systolic (2 vs. 0)
-diastolic (1 vs. 1)
-insomnia (9 vs. 2)
-constipation (1 vs. 4)
-extra menstrual bleeding (1 vs. 2)
-drop-outs reported included heart palpitations, irritability,
increased systolic blood pressure
Nasser et al.,
1999
once/day:
Group I: placebo
-10 days
-27 obese women
otherwise healthy,
n=9 per group.
-subjects were judged to be in normal health on the basis of history
and physical examination as well as laboratory tests, X-ray
examination of the chest, ECG, ultrasound of the gastrointestinal
system and kidneys
-all subjects were without cardiovascular disturbances or arterial
hypertension
-no medication was allowed 2 weeks prior to the study and
participants were asked to abstain from smoking and drinking
beverages with caffeine for at least 24 hours before the study
-no change in systolic pressure, cardiac load or peripheral
resistance
-diastolic pressure and heart rate were increased in group III
compared to control
-information on adverse effects was not reported in the study
Waluga et al.,
1998
Group II: 50 mg
ephedrine +
400 caffeine
Group III: 50 mg
ephedrine + 400 mg
caffeine +10 mg
yohimbine
Council for Responsible Nutrition
December 19, 2000
109
Table 4.2.3-1
Summary of Clinical Trials with Obese Subjects Taking Ephedrine
Total Dose (mg/day)
Duration
Number of Subjects
(sex)
Reported Results
Reference
once/day:
5 treatment groups:
-ephedrine (50 mg)
-ephedrine (50 mg)+
caffeine (150 mg
-ephedrine (50 mg) +
ASA (330 mg)
-ephedrine (50 mg) +
caffeine (150 mg) + ASA
(330 mg)
-placebo
-12 weeks
-163 healthy
premenopausal obese
women
-placebo-controlled, double blind design
-heart rate, blood pressure, clinical signs were assessed
-energy expenditure, blood glucose, triglycerides, total cholesterol,
HDL, DLL evaluated
-Exclusion criteria: hypertension, heart disease, gastric ulcer or
other serious medical conditions
-cholesterol, DLL and glucose was decreased in all groups but was
increased in the placebo group
-the authors concluded that treatment with ephedrine, caffeine and
ASA improved fat loss and health risk factors in obese women
-study design stated that symptoms were evaluated and monitored;
however, no information on adverse effects was reported
Moheb et al.,
1998
3/day:
60 mg ephedrine + 600
mg caffeine
-15-week
study
n=50 in ephedrine/
caffeine group (39
female/11 male)
n=38 who completed
trial
-effects were reported in 54% of the treatment group
-central nervous system side-effects, especially agitation
-effects were most prevalent during the first month of treatment but
subsided markedly as study progressed
-rapid decline in events after first week of treatment
-drop outs complained of vomiting, abdominal pain, tremor,
palpitations and syncope, vertigo, nausea and insomnia. All
symptoms disappeared after cessation of trial
-no serious adverse effects were reported during the study
Breum et al.,
1994
-15-week
follow-up
period
-85 patients were
included in follow up
with the E+C
combination
-57 completed the
follow-up period
-9 in the ephedrine/caffeine group complained of transient side
effects
-29 in the dexfenfluramine group complained of transient side
effects
-no serious side-effects were observed during the follow-up study
Breum et al.,
1994
2/day:
15 mg dexfenfluramine
Council for Responsible Nutrition
December 19, 2000
110
Table 4.2.3-1
Summary of Clinical Trials with Obese Subjects Taking Ephedrine
Total Dose (mg/day)
Duration
Number of Subjects
(sex)
Reported Results
Reference
Herbal formulation (dose
information not specified
and limited report due to
abstract)
-4 week
-100 patients
-double-blind, placebo, crossover protocol
-100 subjects randomly assigned to placebo or treatment
-body composition tests, blood chemistry, resting heart rates and
blood pressures were obtained weekly with self reports of energy
-it was reported that there were no significant changes in blood
pressure or resting heart rates
Kaats and
Adelman, 1994
3/day:60 mg ephedrine +
600 mg caffeine
-8 week
-41 obese but
otherwise healthy
women
-placebo-control, double blind design
-effect of caffeine and ephedrine treatment on a low calorie diet
-plasma total and HDL cholesterol and triglyceride concentrations
were assessed basally on the day before the start of the diet period
and on the 4th and 8th weeks during dieting
Buemann et al.,
1994
2/day:100 mg ephedrine
-1 week
-27 obese adolescents
-screened for endocrine disorders, medication, smoking status,
drinking status and exercise fitness
-the thermogenic effect of ephedrine was investigated
-it was reported by the study authors that side effects were not
observed
Molnár, 1993
3/day:Phase I Study:75
mg ephedrine + 150 mg
caffeine + 330 mg ASA
(for first 4 weeks)
-8 weeks
-11 subjects in
ephedrine, caffeine,
ASA group
-effects reported in 3/11 subjects were transient jitteriness, dry
mouth and constipation
-the study reported that there was no significant difference in
frequency in any effects, and did not persist
-no significant changes were observed effects in systolic blood
pressure, diastolic blood pressure, mean arterial blood pressure or
heart rate
Daly et al., 1993
Council for Responsible Nutrition
December 19, 2000
111
Table 4.2.3-1
Summary of Clinical Trials with Obese Subjects Taking Ephedrine
Total Dose (mg/day)
Duration
Number of Subjects
(sex)
Reported Results
Reference
3/day:Phase I Study:75
mg ephedrine + 150 mg
caffeine + 330 mg ASA
(for first week)
Phase II
150 mg ephedrine + 150
mg caffeine + 330 mg
ASA (for weeks 2 - 8)
-8 weeks
-8 women and 1 man
in ephedrine, caffeine
and ASA group
-8 women completed the study, the man was unable to tolerate the
higher dose of ephedrine after week 1 due to jitteriness and mild
hypertension. He had an undisclosed history of borderline
hypertension.
-effects reported were transient dry mouth
-no significant difference in the frequency of any effects and in
these 8 subjects.
-no adverse effect persisted throughout the study
Daly et al., 1993
3/day:Phase III: patients
who completed Phase II
volunteered to continue
the 150 mg ephedrine +
150 mg caffeine + 330 mg
ASA dose for 7-26
months.
-7 to 26
months
-6 patients from
Phase II study
continued
-6 of 8 subjects who completed Phase II, agreed to continue on
treatment to assess longer term efficacy and safety and were
monitored for 7 to 26 months
-all subjects reported effects such as dry mouth or constipation.
-blood pressure and heart rate remained normal
-it was concluded by study authors that the treatment was well
tolerated
-no significant adverse effects were found in study subjects
Daly et al., 1993
3/day:
150 mg ephedrine
-2 weeks
-10 obese subjects
-it was reported that tolerance was good and no adverse effects
were observed throughout the study
Pasquali et al.,
1992
Council for Responsible Nutrition
December 19, 2000
112
Table 4.2.3-1
Summary of Clinical Trials with Obese Subjects Taking Ephedrine
Total Dose (mg/day)
Duration
Number of Subjects
(sex)
Reported Results
Reference
3/day:60 mg ephedrine +
600 mg caffeine
-24 weeks
-180 obese patients
were randomized to 3
groups and
maintained on a low
energy diet
-n=45 in E+C group
-n=45 in E group
-blood pressure, heart rate and adverse effects were monitored
-ECG, fasting blood glucose, total cholesterol, triglyceride,
hematology, biochemical screening, analysis of urine were
evaluated at weeks 12 and 24
-systolic and diastolic blood pressure decreased significantly in all
treatment groups
-at Week 24, significant decreases in blood glucose, triglyceride
and total cholesterol were found in all groups without group
differences
-all other measured variables, such as hematology, sodium,
potassium, bilirubin, liver enzymes, creatinine, uric acid and urine
analyses were without any significant differences.
-study results showed that at Week 4, significantly more patients in
the treatment group 60% ephedrine/caffeine mixture vs. 44 %in
ephedrine mixture reported at least 1 adverse effect
-by Week 8, there were no statistically significant differences
between symptom reporting among all groups and effects greatly
diminished
Astrup et al.,
1992; Toubro et
al., 1993a
-24-week
follow up
-127 patients from
original study: all
patients received
same treatment
-n=30 in E+C group
-n=31 in E group
-reactions were experienced by 102 patients during the study from
week 26 to 50
-distribution showed that the majority of the symptoms (75%)
occurred during the first 4 weeks
-most frequently reported central nervous symptoms were tremor,
agitation, insomnia, increased sweating and nervousness
-palpitations and tachycardia were also reported
-the authors reported that these adverse effects were temporary and
did not persist
Astrup et al.,1992
3/day:60 mg ephedrine
3/day:60 mg ephedrine +
600 mg caffeine
Council for Responsible Nutrition
December 19, 2000
113
Table 4.2.3-1
Total Dose (mg/day)
3/day:75 mg ephedrine
(first 4 weeks) then 150
mg ephedrine next 4
weeks
Summary of Clinical Trials with Obese Subjects Taking Ephedrine
Duration
- 8 weeks
Number of Subjects
(sex)
Reported Results
Reference
n=11 obese
volunteers in the
ephedrine, caffeine
and ASA group (sex
not specified)
n=13 placebo
-transient jitteriness and transient dry mouth reported but no
statistical significance between placebo group
Krieger et al.,
1990
3/day:60 mg
-3 months
-5 obese women
-it was reported that effects were few
-only 2 subjects reported transient hand tremor the first 2-5 days
-blood pressure was increased but not significantly (blood pressure
only measured during treatment week 4)
-all subjects completed the study
Astrup et al.,
1985
3/day:Group I: placebo
Group II: 75 mg
ephedrine
Group III: 150 mg
ephedrine
-3 months
Group I: n=16
Group II: n=13
Group III: n=17
-effects such as agitation, insomnia, headache, weakness,
palpitation, giddiness, tremor and constipation were present in the
group treated with 150 mg/day but disappeared with time, and
were reported to be well tolerated
-a statistically significant difference between incidence of effects
was reported for the 150 mg/day group compared to placebo;
increase in pulse rate
-no significance was reported in subjects treated with 75 mg/day
compared to placebo with respect to effects
-no significant compound-related effects were present on arterial
blood pressure in any treatment group
Pasquali et al.,
1985
3/day:150 mg ephedrine
-1 month
-10 low-energy
adapted obese women
-it was reported that the incidence of adverse effects was very rare
and only a few women during the first month presented mild forms
of agitation, insomnia, palpitation or giddiness while taking
ephedrine
-no significant changes in arterial blood pressure pulse rate were
found
Pasquali et al.,
1987
Council for Responsible Nutrition
December 19, 2000
114
In a pivotal study recently released, the safety and efficacy of naturally occurring ephedrine
alkaloids found in an herbal ephedra/caffeine supplement were assessed with a clinical protocol
(Boozer et al., 2000). The abstract was presented at the North America Association for the Study
of Obesity Annual Meeting, November 1, 2000. The abstract and data on ephedrine alkaloid and
caffeine analyses, and the methods used are presented in Appendix C. The study was conducted
jointly at the New York Obesity Research Center, at St. Luke’s-Roosevelt Hospital, Columbia
University and Beth Israel-Deaconess Medical Center, Harvard Medical School. Information
about the study is available from the abstract and from statements presented by the principal
investigators at the Office on Women’s Health, U.S. Department of Health and Human Services
(HHS) public meeting on the safety of dietary supplements containing ephedrine alkaloids, in
Washington, D.C., on August 8-9, 2000.
In a multi-center, randomized, double-blind, placebo-controlled trial, the long-term safety and
efficacy for weight loss of an herbal supplement containing ma huang (90 mg/day ephedrine) and
koala nut (192 mg/day caffeine) were assessed. Ephedrine and pseudoephedrine occurred in a
2:1 ratio, and together accounted for 86 to 98 percent of the ephedrine alkaloids. One hundred
sixty seven weight-stable men and women were randomized to an Active (A, n=83) or Placebo
(P, n=84) group. Subject characteristics among the groups were similar for age, weight and basal
metabolic index. Subjects with serious medical conditions were excluded from participation. In
a statement presented at the HHS meeting, Dr. Daly reported that some dropouts were related to
unwillingness or inconvenience of wearing Holter monitors with the blood pressure monitor on
the arm. Dr. Daly explained that these devices take blood pressures every 15 minutes during the
day, and every half-hour at night for the full 24 hours. In addition, these subjects wear
simultaneously a cardiac monitor with ECG leads over their entire chest which become itchy
during monitoring. During this 24-hour period they are unable to shower.
Two phases were investigated, an acute phase of 1 to 4 weeks, and a chronic phase of 6 months.
In the acute phase, 69 subjects were given the herbal supplement, and 68 were placebo subjects.
From statements presented at the HHS meeting, Dr. Daly described the protocol for this
investigation. Baseline evaluations of the subjects included 24-hour blood pressure and Holter
monitors, ECGs, routine lab tests, and urinary screening. Holter and 24-hour ambulatory blood
pressure monitors were worn 5 times a day in the initial and acute phases. Evaluations were
performed at 1, 2, and 4 weeks after randomization for compliance, symptom questionnaires, and
physical examination (which included 24-hour blood pressure and Holter monitors). After the
first 4 weeks, which was referred to as the acute phase, subjects who continued with the study
returned on a monthly basis. Blood testing was also done on a monthly basis for examination of
Council for Responsible Nutrition
December 19, 2000
115
possible deleterious effects on kidney and liver. Dr. Daly stated that the protocol evaluated
cardiovascular endpoints most stringently during the first 4 weeks of the study.
It was reported that these evaluations showed significant time and group interactions for systolic
and diastolic blood pressures, and heart rate. Systolic blood pressure was greater at Week 4 in
the Active group. Initial heart rate in the Active group was significantly less than Placebo, while
at Week 4 Active showed statistically significant increase in heart rate. Time and group
interactions for ventricular events/hour, runs of ventricular events, multifocal ventricular events
and tachycardia were not significant. Significant interactions for bradycardia and ventricular
couplets were due to declining rates in Active, but not Placebo group.
In the 6-month chronic phase, there were 46 Active subjects with 38 subjects in Placebo.
Significant time and group interactions were body weight (significantly decreased), basal
metabolic index (significantly decreased), and percentage fat (significantly decreased). Selfreported symptoms in Active consisted of dry mouth, heartburn, insomnia and diarrhea.
Symptoms such as chest pain, palpitation, irritability, nausea and constipation were similar
among supplement and placebo groups.
The authors reported that herbal ephedra/caffeine lowered body weight, fat and BMI. Blood
pressure was transiently increased and heart rate persistently increased; however, most
importantly, cardiac arrhythmias were not increased. Self-reported symptoms were similar to
those known for synthetic ephedrine/caffeine mixtures. Full study details and findings are not
available and are pending publication.
In another study, a prospective clinical investigation was conducted on overweight or obese
individuals who voluntarily sought medical assistance for weight management in an outpatient,
nonprofit bariatric clinic based in a community hospital (Huber, 1999). The study results were
presented at the American Society of Bariatric Physicians (ASBP) in Las Vegas October 16,
1999 and at the North American Society for the Study of Obesity (NAASO) on November 16,
1999 and represent work not currently published.
Subjects meeting the strict inclusion criteria for participation in this study were assigned on a
random basis to one of three nutraceutical adjunctive weight-loss preparations for 6 months. The
three products, Nutra 1 (“Lean-R-Gy”) (n=20), Nutra 2 (“Trim-4-Life”) (n=44) and Nutra 3
(“ProTrim”) (n=58) were given. There was no control group in this study, and participants and
investigators were not blinded to the nutraceutical products evaluated. The exact amounts of the
constituents were not identified; however, manufactures did indicate that Nutra 1 contained
Council for Responsible Nutrition
December 19, 2000
116
approximately 24 mg of ephedra for a maximum total of 48 mg/day of ephedra when used as
directed. Nutra 2 contained approximately 12 mg of ephedra-equivalent per thermogenic tablet,
for a maximum total of 24 mg/day of ephedra-equivalent when used as directed. Nutra 3
contained approximately 12 mg of ephedra and slightly more than 33 mg of caffeine per
thermogenic caplet, for a maximum total of 72 mg/day of ephedra and 200 mg/day of caffeine
daily, when used as recommended. The ephedra delivered by Nutra 1 and Nutra 3 was derived
primarily from ma huang; the ephedra in Nutra 2 was derived from other sources. Safety
parameters monitored included adverse events, blood pressure, heart rate, complete blood count,
lipid profile, urinalysis, thyroid panel, and thyroid stimulating hormone.
Subjects were provided with a 1-month supply, and upon monitoring they were provided with a
subsequent month’s supply when determined to be a “responder” (i.e., weight loss) to the
supplement given. Symptoms reported during the course of this study were stated to be at an
extremely low frequency. Neither systolic nor diastolic blood pressure increased while the
subjects were on ephedra-containing or caffeine-containing dietary supplements. After an initial
transient rise in apical pulse rates, this increase did not significantly change in any group. Based
on the study design, the authors state that the results should be viewed more as the descriptive
findings of compiled individual cases evaluated through a strictly monitored clinical research
protocol.
In a subsequent report, a randomized, placebo-controlled, double-blind study was conducted on
ephedra-containing dietary supplements for 6 weeks (Huber, 2000 – unpublished). The groups
were randomly assigned and are summarized in Table 4.2.3-2. A medical evaluation and
physical examination were performed by a bariatric physician prior to enrollment with strict
inclusion criteria for admission to the study. Following an observational period of 9 to 10 weeks
before supplement initiation, subjects were evaluated at approximately 2 weeks and at 6 weeks
after initiation of the dietary supplement.
Council for Responsible Nutrition
December 19, 2000
117
Table 4.2.3-2
Group
Group Assignments for Huber, 2000
Ephedrine (total
mg/day): Caffeine (total
mg/day)
Initial Subjects Enrolled
Subjects Actively
Followed
Metabolize and Save (1
tablet 3x/day)
36:120
26
15
Metabolize and Save (2
tablets 3x/day)
72:240
26
19
Placebo (1 or 2 tablets
3x/day)
0:0
21
14
Metabolite (1 tablet
3x/day)
36:0
21
14
72:300
26
19
Product D
Huber (2000) reported that no serious adverse events occurred. General symptoms,
cardiovascular, skin, urinary tract, musculoskeletal, sexual function, nervous system,
endocrine/metabolic, gastrointestinal and respiratory system were effects. A metabolic study
checklist included measurements of glycohemoglobin, 24-hour urine collection/creatinine/
protein, fasting insulin, basal metabolic rate, hydrostatic weighing, fitness assessment,
psychometric, memory test, trail making, digit span and digit symbol. Adverse effects were
expressed as relative ratios for the supplement group relative to the observational period.
Specifically, there were no significant increases in blood pressure or heart rate, or other
cardiovascular changes. Blood pressure was monitored on each visit. It was measured in the
supine and upright position, and apical pulse rates were checked by oscillation over a 2-minute
period of time. The average duration of observation with the higher dosage of Metabolize and
Save was about 1.5 weeks less than the lower dosage group due to the withdrawal of 3 subjects
for reasons stated as “too jittery”. An explanation for the drop-outs in the study was not reported.
Molnár et al. (2000) investigated the effects of ephedrine and caffeine on safety and efficacy in
obese adolescents for 20 weeks. In a randomized, double-blind, placebo-controlled study, 32
obese adolescents were assessed. Thirteen adolescents were randomized to the placebo group
and 16 were randomized to 1 of 2 ephedrine/caffeine groups based on weight. Adolescents <80
kg were given tablets of 100 mg caffeine/10 mg ephedrine – 3 times/day (total 300 mg
caffeine/30 mg ephedrine), while adolescents >80 kg were given two tablets of 100 mg
caffine/10 mg ephedrine – 3 times/day (total 600 mg caffeine/60 mg ephedrine). The average age
of the adolescents was 16 years. Strict exclusion criteria included any metabolic or endocrine
disease, psychiatric or somatic disease; any drug treatment; evidence of alcohol or drug abuse;
Council for Responsible Nutrition
December 19, 2000
118
treatment with methylxanthines less than 1 month prior to the start; and any contraindications to
the trial medication.
The caffeine/ephedrine tablets were gradually introduced starting with 1tablet per day and
increasing the dose to 1 tablet 3 times daily. The maximal dose was reached by the end of the
second or third week in the case of the low and high dose, respectively. After the 20th week the
patients were weaned gradually (2x1 or 2 tablets daily for 3 days, then 1x1 or 2 tablets daily for
another 3 days, then the caffeine/ephedrine tablets were terminated. The adolescents were
evaluated before the start, at Weeks 2, 8, 12, 16, 20, and at the follow-up visit (5 days to 2 weeks
after the termination of treatment). Safety parameters monitored included detailed physical
assessment, blood pressure and heart rate measurement and monitoring of side effects,
withdrawal symptoms, blood glucose, plasma insulin, thyrotrophin, free thyroxine,
triiodothyronine, total cholesterol, high-density lipoprotein, apolipoprotein A1 and B. In
addition, screening for hemoglobin, hematocrit, white blood cell and platelet count, aspartate
aminotransferase, lactate dehydrogenase, bilirubin, alkaline phosphatase, serum albumin, and
creatinine concentrations were measured from fasting blood samples. Urine was checked for
glucose and protein at the start and at Week 8 and 20. Physical fitness testing was performed
before the start and on Week 20 to check cardiovascular side effects.
Blood glucose, plasma insulin, total cholesterol, HDL-cholesterol, ApoA1 levels and thyroid
hormone plasma concentrations did not change during the trial period in either group. The
plasma triglyceride and ApoB plasma concentrations of the active group were significantly lower
than those of the placebo group which became significant at Week 20. Hemoglobin, hematocrit,
white blood cell and platelet count, ASAT, LDH, bilirubin, ALP, serum albumin, and creatinine
were in the normal range in all adolescents at baseline and remained there at Weeks 8 and 20.
Urine was negative for glucose and albumin at all time points. Blood pressure and heart rate
values showed no significant changes during the trial in either group. With respect to side effects
11 and 10 patients reported some kind of side effects from the placebo and caffeine/ephedrine
groups, respectively. The side effects were more frequent at the beginning of the treatment in the
active group than in the placebo group and more frequent during the follow-up period as
compared to the beginning of the treatment in the placebo group; however, the side effects were
transient, graded as mild to moderate in the majority of all cases. Side effects were graded as
severe on six occasions (placebo,5: caffeine/ephedrine,1). It was reported that no serious adverse
reactions were encountered in the trial. The number of reported withdrawal symptoms such as
sweating, palpitation, tremor, nervousness, vomiting, diarrhea, insomnia and poor general state of
health were checked on the 1st, 3rd, and 5th day of the weaning period and were not different in
the placebo and caffeine/ephedrine groups, respectively.
Council for Responsible Nutrition
December 19, 2000
119
The authors concluded that based on the study findings the ephedrine/ephedrine mixture at doses
up to 600 mg caffeine and 60 mg ephedrine can be a safety and effective compound for the
treatment of obesity in adolescents.
In a meeting abstract, Nasser et al. (1999) reported on the safety and efficacy of an herbal
supplement containing ma huang and guarana in a clinical study conducted. Additional
information is summarized from statements by the principal investigators presented at the Office
on Women’s Health, U.S. Department of Health and Human Services (HHS) public meeting on
the safety of dietary supplements containing ephedrine alkaloids, in Washington, D.C., on
August 8-9, 2000.
The double-blind, placebo-controlled, 8-week trial was conducted on a supplement containing 72
mg/day of ephedrine in ma huang, and 240 mg of caffeine from guarauna in 67 participants.
Exclusions included nursing, pregnancy, taking concurrent medications, cancer, asthma, enlarged
prostate, glaucoma, seizures, migraine headaches, hypertension, diabetes, or major organ illness.
Of the 67 randomized subjects, 7 dropped out before the first follow-up (5 supplement subjects
and 2 placebo subjects). Of the 5 drop-outs for the herbal supplement, 4 reported heart
palpitations and 1 developed high blood pressure. Of the 60 remaining subjects who returned for
at least 1 follow-up visit, 12 dropped out before Week 8 of the study. These drop-outs consisted
of 6 participants in the supplement group and 6 in the placebo group. Of the supplement group
drop-outs, 2 reported heart palpitations, 1 irritability, and 1 had increased systolic blood pressure.
Those subjects who withdrew for self-reported palpitations, underwent follow-up ECGs that
showed no abnormalities.
In the subjects who completed the study, the ratio of self-reported symptoms in supplement vs.
placebo were: dry mouth (5 vs. 1); heart palpitations (2 vs. 2); blood pressure (>20 individuals treatment vs. placebo not reported); systolic (2 vs. 0); diastolic (1 vs. 1); insomnia (9 vs. 2);
constipation (1 vs. 4), and extra menstrual bleeding (1 vs. 2). Supplements resulted in greater
changes in body weight, body fat and serum triglycerides compared to placebo. In details
presented at the HHS meeting, heart rate was significantly increased over baseline in the
supplement group with an increase of 6.9 bpm versus a decrease of 1.7 bpm in placebo. Mean
blood pressure systolic and diastolic did not differ between groups at any time point nor were
they different from baseline in either group at study termination. When the rise over baseline for
all subjects was compared at each time point, mean systolic blood pressure was significant only
at Week 6 for supplement subjects versus placebo. Repeated measures analysis of variance
showed that the variability of the change in blood pressure was constant within subjects over
Council for Responsible Nutrition
December 19, 2000
120
groups. A between-group effect was not significant unless weight loss was used as a covariant.
In addition, Dr. Boozer continued to summarize the study as follows; among the subjects who
completed the study, there were no statistically significant differences in self-reported symptoms.
There were however differences with increased reporting of dry mouth and insomnia. No
subjects had any serious or long-lasting adverse event in this 8-week trial.
The authors concluded that the herbal supplement promoted weight loss, but was accompanied
by undesirable effects in some subjects at 72 mg/day of ephedrine. Full study details and
findings are not available and are pending publication.
A prospective clinical investigation was conducted on overweight or obese individuals who
voluntarily sought medical assistance for weight management in an outpatient, nonprofit bariatric
clinic based in a community hospital (Huber, 1999). The study results were presented at the
American Society of Bariatric Physicians (ASBP) in Las Vegas October 16, 1999 and at the
North American Society for the Study of Obesity (NAASO) on November 16, 1999 and
represents work not currently published.
Subjects meeting the strict inclusion criteria for participation in this study were assigned on a
random basis to one of three nutraceutical adjunctive weight-loss preparations for 6 months. The
three products, Nutra 1 (“Lean-R-Gy”) (n=20), Nutra 2 (“Trim-4-Life”) (n=44)and Nutra 3
(“ProTrim”) (n=58) were given. There was no control group in this study, and participants and
investigators were not blinded to the nutraceutical products evaluated. The exact amount of the
constituents were not identified; however, manufactures did indicate that Nutra 1 contained
approximately 24 mg of ephedra for a maximum total of 48 mg/day of ephedra when used as
directed. Nutra 2 contained approximately 12 mg of ephedra-equivalent per thermogenic tablet,
for a maximum total of 24 mg/day of ephedra-equivalent when used as directed. Nutra 3
contains approximately 12 mg of ephedra and slightly more than 33 mg of caffeine per
thermogenic caplet, for a maximum total of 72 mg/day of ephedra and 200 mg/day of caffeine
daily, when used as recommended. The ephedra delivered by Nutra 1 and Nutra 3 was derived
primarily from ma huang; the ephedra in Nutra 2 was derived from other sources. Safety
parameters monitored included adverse events, blood pressure, heart rate, complete blood count,
lipid profile, urinalysis, thyroid panel and thyroid stimulating hormone.
Subjects were provided with a 1-month supply, and upon monitoring they were provided with a
subsequent month’s supply when determined to be a “responder” (i.e., weight loss) to the
supplement given. Symptoms reported during the course of this study were stated to be at an
extremely low frequency of side effects. Neither systolic nor diastolic blood pressure increased
Council for Responsible Nutrition
December 19, 2000
121
while the subjects were on ephedra-containing or caffeine-containing dietary supplements. After
an initial transient rise in apical pulse rates, this increase did not significantly increase in any
group. Based on the study design, the authors state that the results should be viewed more as the
descriptive findings of compiled individual cases evaluated through a strictly monitored clinical
research protocol.
The cardiovascular effects of ephedrine were reported in obese women by Waluga et al. (1998).
Twenty-seven obese, but healthy, women were divided into 3 equal groups. The subjects were
judged to be in normal health on the basis of history and physical examination as well as
laboratory tests, X-ray examination of the chest, ECG, ultrasound of the gastrointestinal system
and kidneys. They had no cardiovascular disturbances or arterial hypertension. No other
medication was allowed 2 weeks prior to the study. The participants were asked to abstain from
smoking and from drinking beverages containing caffeine for at least 24 hours before the study.
Group 1 received a standard low caloric diet and placebo; Group II received the same diet with
ephedrine (2 x 25 mg) with caffeine (2 x 200 mg); Group III received the same diet and
ephedrine (2 x 25 mg) with caffeine (2 x 200 mg) and yohimbine (2 x 5 mg). The study was
performed in a double-blind, placebo fashion for 10 days. The cardiovascular state was
evaluated by thoracic electrical bioimpedance, automatic sphygmomanometer, and continuous
ECG recording. In each patient, the hemodynamic study was performed twice, once before
pharmacological treatment and after 10 days of diet or diet plus treatment. Systolic pressure,
cardiac load and peripheral resistance were not statistically changed during measurements at rest.
Diastolic pressure and heart rate were statistically increased in Group 3 (ephedrine, caffeine, and
yohimbe) compared to control during measurements at rest. The reported aim of the study was to
determine if the combinations used were safe for the cardiovascular system. Ten days of
observation were deemed adequate by the study authors to detect some cardiovascular reactions.
The authors concluded that they did not observe any significant changes in most hemodynamic
parameters after 10 days of dietary administration; however, they did find that the ejection
fraction was decreased. It was concluded that chronic administration, as demonstrated in this
study, showed no undesirable effects on cardiovascular state in obese patients.
Moheb et al. (1998) studied the effect of ephedrine, caffeine and ASA in combinations on weight
loss in obese women. The experiment was a placebo-controlled, double-blind trial on weight
loss, and adverse effects when taken with a calorie restricted diet. Subjects were 163
premenopausal female volunteers aged 20 to 49 years. They were sequentially assigned to 5
treatment groups for 12 weeks: E, E+C; E+A, E+C+A; and placebo. Doses of ephedrine were 50
mg (25 mg, for the first 2 weeks), caffeine 50 mg and ASA 110 mg, given 3 times per day.
Exclusion criteria included hypertension, heart disease, gastric ulcer or other serious medical
Council for Responsible Nutrition
December 19, 2000
122
conditions. Subjects were seen before treatment, weekly for 1 month, then every 2 weeks.
Relevant safety parameters which were measured included blood pressure, heart rate and clinical
signs. Subsamples of 10 subjects from each group were randomly selected for additional
measurements pre- and post-treatment of: energy expenditure, fasting and post meal and
thermogenic effects, urinary catecholamines; occult blood in stools; and blood glucose,
triglyceride, total cholesterol, HDL, DLL, free fatty acids, free thyroxine and insulin.
Cholesterol, DLL and glucose were decreased in all groups, but were increased in the placebo
group. Although the authors stated that clinical signs were evaluated and monitored, no
information on possible adverse effects was reported by the authors.
Breum et al. (1994) compared the effects of an ephedrine/caffeine combination compared to
dexfenfluramine in the treatment of obesity in a double-blind multi-center trial in general practice
(i.e., not in a controlled clinical setting). One hundred and three patients, who were
approximately 20 to 80% overweight, were included in this 15-week study. Patients were
randomized to 2 treatment regimens: 15 mg of dexfenfluramine twice daily (n=53), or 20 mg:200
mg ephedrine:caffeine 3 times a day (n=50 - 39 female/11 male). Measurements of body weight,
heart rate, blood pressure and side effects were taken at the end of Week 1 and every 3 weeks
thereafter. After 15 weeks of treatment, 10 patients dropped out in the dexfenfluramine group
and 12 dropped out from the ephedrine:caffeine group. In particular, 6 patients from the
ephedrine:caffeine group were withdrawn due to vomiting and abdominal pain, 1 had tremor,
palpitations and syncope, and the last 3 patients experienced vertigo, nausea, and insomnia. All
symptoms disappeared after cessation of treatment. Effects were reported in 43% of patients in
the dexfenfluramine and 54% in the ephedrine + caffeine group. Statistically significant central
nervous system effects, especially agitation and insomnia, were more pronounced in the
ephedrine + caffeine group, whereas gastrointestinal symptoms were more frequent in the
dexfenfluramine group. Effects were most prevalent during the first month of treatment, and
subsided markedly as the study progressed. A rapid decline in events was found in the
ephedrine/caffeine group after the first week of treatment. Evaluation of mean systolic and
diastolic blood pressures showed a statistically significant reduction in the EC group. It was
reported that mean heart rate increased significantly compared to baseline in the EC group;
however, the change was only 1.1 ±11.6 bpm. No placebo group was included in this study
which reduces the utility of this study.
Eighty-five patients were included in an open 15-week follow-up period, and 29 patients
complained of transient effects; 9 from the ephedrine and caffeine group and 20 from the
dexfenfluramine group. It was reported that no serious side-effects were observed during the
follow-up study period or during the study period, and after cessation of trial treatment, all
Council for Responsible Nutrition
December 19, 2000
123
symptoms remitted. Blood pressure was unchanged during the follow-up period. One patient
(57 year old man) from the ephedrine + caffeine group died during the study. Careful
examination of his medical history found he had a history of alcohol abuse (not reported during
patient recruitment). He was hospitalized 3 weeks after the start of the study with severe alcohol
intoxication and died shortly afterwards from fatal gastro-intestinal bleeding. The authors
reported that the death was unrelated to ephedrine+caffeine treatment, but was due to fatal gastric
bleeding in combination with alcohol intoxication.
Effects of a multiple herbal formulation on body composition, blood chemistry, vital signs, and
self-reported energy levels and appetite control were reported in an abstract by Kaats and
Adelman (1994). Using a double-blind, placebo, crossover protocol, 100 subjects were randomly
assigned to a group consuming an inactive placebo while following a self-directed behavior
modification program; or to a group following the same program, but consuming a proprietary
herbal formulation (dose not specified) that included ma huang. The test period consisted of two
4-week phases. Body composition tests, blood chemistry, resting heart rates and blood pressures
were obtained weekly with self-reports of energy levels. It was reported that there were no
significant changes in blood pressure or resting heart rates. Dose information was not specified,
and the findings of this study were determined to be limited. A literature search for the full
publication did not locate a published version of this study.
Buemann et al. (1994) investigated the effect of ephedrine together with caffeine on plasma
lipids and lipoproteins on a calorie-restricted diet. Forty-one obese but healthy women were
referred by general practitioners for treatment of obesity. They were randomly assigned by a
third party to a diet + ephedrine+caffeine (EC) group or a diet + placebo group. The experiment
was conducted as a double blind design. Due to drop-outs and incomplete blood analyses, only
16 subjects from each group were included in this investigation. The study duration was 8
weeks, and the diet was supplemented by ephedrine 20 mg plus caffeine 200 mg, 3 times per day.
Both groups were supervised by clinical dietitians weekly. Total plasma cholesterol, HDLcholesterol and triglyceride concentrations were assessed on the day before the start of the diet
period and during Weeks 4 and 8 of dieting. Heart rate and blood pressure measurements were
not mentioned.
Molnár (1993) investigated the effects of ephedrine and aminophylline on resting energy
expenditure in obese adolescents for 1 week. Fifty seven obese adolescents attending an obesity
clinic were assessed. These adolescents were screened for endocrine disorder, medication,
smoking, alcohol consumption and not engaged in regular exercise. The thermogenic effect of
ephedrine was investigated in 27 obese adolescents at 50 mg 2 times per day. Ten adolescents
Council for Responsible Nutrition
December 19, 2000
124
served as controls. It was reported by the study authors that side effects were not observed.
Heart rate and blood pressure measurements were not mentioned.
Daly et al.(1993) investigated the safety and efficacy of a combination of ephedrine, caffeine, and
ASA in obese subjects. The initial phase of the study was an 8 week, randomized double-blind
trial of the ephedrine, caffeine, and ASA (ECA) mixture vs. placebo. The placebo group then
returned for an unblinded crossover for 8 weeks. Twenty-nine subjects were recruited to enroll
in part I, but 5 defaulted due to difficulty in keeping appointments. Of the 24 who completed
part I of the study, 11 (10 female/1 male) were in the ECA group and 13 (12 female/ 1 male) in
the placebo group. In study Phase I, subjects were assigned to receive either placebo or treatment
for 8 weeks. Both placebo and treatment were administered 3 times daily. For the first 4 weeks,
a total of 75 mg ephedrine, 150 mg caffeine and 330 mg ASA, or placebo were given per day.
After the fourth week, the ephedrine dose was increased to a total of 150 mg per day. In Phase I,
subjects returned for evaluations at Weeks 1, 4, 6, and 8.
In study Phase II, placebo group subjects were asked to return for an 8-week, nonblinded
crossover of ECA, and the ephedrine dose was doubled after the first week. Willing subjects
from Phase II then continued for 7 to 26 months to assess possible longer-term effects of the
ephedrine, caffeine, and ASA mixture (Phase III). In Phase II, each subject returned at Weeks 2,
4, 6, and 8 and in part III, subjects returned at monthly intervals.
In all phases, consumption of coffee and other caffeinated beverages was limited to 2 cups daily.
At each visit, weight, blood pressure, heart rate were measured, and subjects were asked about
adverse effects.
In study Phase I, effects were reported in 3 of 11 ECA subjects who reported transient jitteriness,
2 reported dry mouth and 2 reported constipation, while 1 of 13 placebo subjects reported
jitteriness, 2 reported dry mouth, and 1 of constipation. The study reported that there was no
significant difference in frequency of any of these effects, and in both ECA and placebo groups,
effects tended not to persist. Furthermore, average blood pressure and heart rates showed no
significant differences within groups or between ECA and placebo, in systolic blood pressure,
diastolic blood pressure, mean arterial blood pressure, and heart rate as well as glucose, insulin,
and total or HDL cholesterol.
In study Phase II, 8 women and 1 man enrolled, and the 8 women completed the study. The man
was unable to tolerate the higher dose of ephedrine due to jitteriness and mild hypertension. On
further questioning, he acknowledged a medical history of undisclosed borderline hypertension.
Council for Responsible Nutrition
December 19, 2000
125
With respect to effects, 3 of 8 subjects complained of transient dry mouth with ECA, while none
did with placebo; however there was no significant difference in the frequency of any effects and
in these 8 subjects no effect from either the placebo or ECA persisted throughout the study. No
significant differences were found between ECA and placebo in systolic, diastolic, or mean
arterial blood pressure, heart rate, glucose, insulin, and total or HDL cholesterol.
In study Phase III, 6 of 8 subjects who completed Phase II of the study agreed to continue on
ECA in an open study design to assess possible longer-term efficacy and safety, and were
followed at monthly intervals for 7 to 26 months. Weight, blood pressure, heart rate,
compliance, appetite and adverse effects were assessed at monthly intervals. All subjects (n=6
females) reported effects such as dry mouth or constipation. The study reported that blood
pressure and heart rate remained normal, and concluded that ECA combination continued to be
well tolerated. No significant adverse effects were found in study subjects over periods ranging
from 5 months to 2 years during treatment with this 3-way combination of ephedrine, ASA, and
caffeine. The authors suggested that the good tolerability displayed by the ECA combination
may be due in part to the time period allowed on a lower dose of ephedrine before the full dose
was given.
Pasquali et al. (1992) studied the effects of chronic administration of ephedrine during very lowcalorie diets on energy expenditure, protein metabolism, and hormone levels in obese subjects.
Ephedrine hydrochloride was administered at a dose of 50 mg 3 times a day orally or placebo
during 2-week periods in a randomized, double-blind, cross-over design. Five subjects started
with ephedrine and 5 subjects with placebo. The results were analyzed separately in the 2
groups. Relevant safety information in this study reported that tolerance of the pharmacological
therapy was good in all subjects with no adverse effects observed throughout the study; however,
the study did not report how tolerance was assessed.
Astrup et al. (1992), Quaade et al. (1992), and Toubro et al. (1993a) reported the effects of an
ephedrine/caffeine compound compared to ephedrine, caffeine and placebo agents alone in obese
subjects on an energy-restricted diet. These 3 publications describes a single clinical trial by a
group of Danish researchers, one of the few published trials which enrolled a large number of
subjects. Subjects were between 20 to 65 years of age and were 20 to 80% overweight.
Exclusion criteria included screening for history of psychiatric/somatic disease, GI
malabsorption, cardiovascular disease, thyroid disease, and any concomitant treatments with
drugs. In a randomized, placebo-controlled, double-blind study, 180 obese patients were
randomized to an ephedrine+caffeine (EC) combination (20 mg:200 mg), ephedrine (E) (20 mg),
caffeine (C) (200 mg) or placebo, 3 times a day for 24 weeks and maintained on a low energy
Council for Responsible Nutrition
December 19, 2000
126
diet (45 subjects per group). The subject profile of the treatment groups consisted of 39 female/6
male in the E+C group; 40 female/5 male in E group; 42 female/3 male in C group and 34
female/11 male in placebo group. Prior to the study, the bioavailability and absorption of
ephedrine and caffeine were found to be identical when they were given separately and in
combination. Patients were seen every 2 weeks and weight, waist and hip circumference, resting
heart rate, blood pressure and adverse effects were monitored. The following parameters were
recorded before the study and at Weeks 12 and 24: ECG, fasting blood glucose, total cholesterol,
triglyceride, hematology, biochemical screening, analysis of urine, and the total caffeine
consumption during the previous week.
Of the 180 patients, 141 completed the 24-week treatment period. Thirty-nine patients withdrew
from the study and it was reported that they were equally distributed among the 4 groups, with no
statistically significant differences between the groups (see Table 4.2.3-3). In particular, 6
patients withdrew due to side effects, 3 in the ephedrine/caffeine group: 1 had vertigo,
tachycardia and syncope; the second was withdrawn due to hypertension, and; the third patient
experienced euphoria, neurotic behavior and increased sweating. One patient who received
ephedrine was withdrawn due to a depressed mood, insomnia, tremor and tachycardia. One
patient in the caffeine group had neurotic symptoms, and another had brachycardia, tiredness and
dizziness.
Table 4.2.3-3
Reasons for Patient Withdrawal (Astrup et al., 1992; Quaade et al.,
1992; Toubro et al., 1993a)
Cause for Withdrawal
Ephedrine
and Caffeine
Ephedrine
Caffeine
Placebo
lack of weight loss
0
0
1
0
side effects
3
1
2
0
complications to obesity
1
1
1
0
Pregnancy
2
2
1
4
non-compliance
1
0
1
3
not willing to continue
3
6
2
2
Other
0
0
1
1
Total
10
10
9
10
number of subjects originally in group
45
45
45
45
Council for Responsible Nutrition
December 19, 2000
127
Study results showed that at week 4, significantly more patients in the treatment groups (60% of
the ephedrine and caffeine), (44% of ephedrine), and (36% of caffeine) than in the placebo group
(24%) reported at least 1 side effect (P<0.05), whereas the differences between the non-placebo
groups were not significant. By Week 8, there was no statistically significant difference between
symptom reporting among all groups, and side effects reported were greatly diminished (see
Table 4.2.3-4). Typical effects of treatment and frequency are reported in Table 4.2.3-5 which
were generally minor. In addition to these findings, this study showed that there was a possibility
of withdrawal symptoms. Two weeks after cessation of treatment, more symptoms were reported
from the groups receiving ephedrine and caffeine, and ephedrine singly than in the placebo
group. In particular, in the ephedrine and caffeine group, headache and tiredness were more
frequently reported, whereas more patients of the ephedrine group reported hunger. In the
caffeine group only, headache was reported more frequently than in the placebo group following
cessation of treatment.
Table 4.2.3-4
Time Course of Effects
Time of Report (Week)
Ephedrine + Caffeine
Ephedrine
Caffeine
Placebo
4
27
25
22
5
8
3
2
2
3
12
5
5
1
1
16
3
1
1
1
20
2
4
1
1
24
4
3
5
2
Council for Responsible Nutrition
December 19, 2000
128
Table 4.2.3-5
Adverse Effect
Frequency of Effects in All Patients
Ephedrine and Caffeine
Ephedrine
Caffeine
Placebo
Dizziness
5
2
5
1
Headache
2
2
3
0
Tremor
5
4
1
0
Depressed mood
1
2
2
0
Euphoria
2
1
2
0
Insomnia
9
8
3
3
Dry mouth
0
3
0
0
Postural hypotension
2
2
1
1
Palpitation
2
1
0
0
Tachycardia
2
2
0
0
Constipation
0
1
0
2
Number of Subjects
Originally in Group
35
35
34
35
Systolic and diastolic blood pressure decreased significantly in all treatment groups, without any
significant differences among the 4 groups. Mean heart rate decreased 4 to 6 beats/min only in
the caffeine and placebo group. At Week 24, significant decreases in blood glucose, triglyceride
and total cholesterol were found in all groups without group differences. These decreases were
maintained in all groups at Week 50. All other measured variables, such as hematology, sodium,
potassium, bilirubin, liver enzymes, creatinine, uric acid, and urine analyses were without any
significant group differences.
In a follow-up trial, Toubro et al. (1993b) enrolled 127 patients from the above studies to further
analyze the acute and chronic effects of ephedrine/caffeine mixtures. The study comprised a 24week follow-up with an open-labeled design where all patients received the same treatment (diet
and medication). This study was a continuation of a 24-week double-blind randomized parallel
study originally with 4 treatment groups. All medication was stopped from Week 24 to 26 in
order to monitor any withdrawal symptoms. Subsequently, all remaining patients were offered a
further 24 weeks of treatment with a low calorie diet in combination with the ephedrine/caffeine
combination (20 mg:200 mg) 3 times a day.
Council for Responsible Nutrition
December 19, 2000
129
From Weeks 26 to 50, 28 patients withdrew from the study (see Table 4.2.2-6). Two patients
from the former ephedrine group withdrew, 1 due to insomnia, sweating and finger anesthesia,
and 1 due to depression, tremor, nervousness, and irritability. Three from the caffeine group
withdrew, 1 due to tachycardia, nausea and vertigo, 1 with nausea, tachycardia, vomiting, and
headache, and 1 with irritability and insomnia. Six patients were recorded as having intercurrent
diseases unrelated to the treatment.
Side effects were experienced by 102 patients during the study from Week 26 to 50. This
distribution showed that the majority of the symptoms (75%) started during the first 4 weeks of
treatment (Week 26 to 30). The most frequently reported central nervous system symptoms were
tremor, agitation, insomnia, increased sweating and nervousness. Significant decreases in blood
glucose, triglyceride, and total cholesterol levels were found in all groups. All other measured
variables such as hematology, sodium, potassium, bilirubin, liver enzymes, creatinine, uric acid,
and urine analyses were without any significant differences. It was reported that effects such as
tremor, tachycardia, and insomnia were temporary, and no serious withdrawal symptoms were
noted. The frequency and severity of individual signs and symptoms were not stated.
Table 4.2.2-6
Reasons for Patient Withdrawal during Week 26 to 50 (Toubro et
al., 1993b)
Cause of Withdrawal
Ephedrine and
Caffeine
Ephedrine
Caffeine
Placebo
Side effects
0
2
3
0
Pregnancy or desire for pregnancy
2
0
0
0
Non-compliance
0
0
1
0
Discontinuation
2
3
1
7
Not showing up for visits
0
0
1
0
Intercurrent disease
2
2
2
0
Total
6
7
8
7
Number of subjects enrolled in
Week 26-50
30
31
34
32
Number of completers at Week 50
24
24
26
25
Krieger et al. (1990) investigated the weight loss effects of ephedrine+caffeine+ASA in obese
subjects. Twenty-nine subjects enrolled in the study and 5 defaulted due to difficulty in keeping
follow-up appointments. Of the 24 subjects who completed the study, 11 were in the ephedrine+
Council for Responsible Nutrition
December 19, 2000
130
ASA+caffeine treatment group and 13 in the placebo group. Volunteers were screened for
eligibility by medical history, physical examination, and laboratory studies (complete blood
count, fasting blood glucose, electrolytes, renal, hepatic function tests, ECG and stool) to exclude
those with cardiovascular, psychiatric, gastrointestinal, hematologic, and metabolic disorders.
The treatment was administered as follows: for the first 4 weeks the ephedrine dose was 25 mg, 3
times per day (75 mg of ephedrine/day), and after the follow-up visit at Week 4, the ephedrine
dose was increased to 50 mg, 3 times per day (150 mg of ephedrine/day). The caffeine (50 mg, 3
tablets/day) and ASA (100 mg, 3 tablets/day) were administered in a single tablet, and the dose
remained fixed throughout the study, i.e.,150 mg of ephedrine + 150 mg of caffeine + 300 mg of
ASA/day. At each follow-up visit (Weeks 1, 4, 6, and 8), blood pressure and heart rate were
measured, and subjects were questioned about side effects and compliance with the pills and
asked to rate their appetite. Subjects were instructed to restrict caffeinated beverage
consumption to 2 cups/day. At Weeks 0, 4, and 6, fasting blood samples were obtained for
analysis of glucose, insulin and total and HDL-cholesterol. No differences between treatment
and placebo were observed in resting heart rate, blood pressure, fasting plasma glucose, insulin
or total or HDL cholesterol concentrations. Treatment subjects tended to report transient
jitteriness (3/11), transient dry mouth (2/11), and constipation (2/11); however, there were no
differences in the frequency of these side effects between treatment and placebo by Fisher’s exact
test. This clinical study is different from many of the obesity clinical trials, in that the study
design involved a stepped dose of ephedrine. Due to the novel combination at the time of the
study of ephedrine with caffeine and ASA, ephedrine was administered at a lower dose, and once
cardiovascular evaluations showed no effect, the dosage of ephedrine was doubled. This higher
dose level of ephedrine together with caffeine and ASA showed no treatment-related differences
compared to placebo treatment.
The effects of chronic administration of ephedrine were evaluated in 5 women characterized by
the author as obese (Astrup et al., 1985). Subjects were between 18 to 49 years old and were 10
to 17% overweight. An initial clinical examination with measurement of blood pressure and
pulse rate was performed. Subjects were given 20 mg of ephedrine 1 hour before meals 3
times/day for 3 months. Various parameters were measured, in particular, plasma sodium,
potassium, glucose, serum thyroxine and tri-iodothyronine, TSH, and determination of
catecholamines. It was reported that side effects were few. Two subjects reported transient hand
tremor during the first 2 to 5 days during the 3-month study. Blood pressure and heart rate were
only evaluated during treatment Week 4. There was an increase in mean blood pressure which
was not statistically significant. No change in pulse rate could be detected. After 4 weeks, no
significant difference in mean arterial blood pressure or heart rate was observed. Plasma levels
Council for Responsible Nutrition
December 19, 2000
131
of K and Na were measured. Plasma K decreased from the initial value (4.1 to 3.7 mmol/L);
however, no alterations were observed in Na levels. All 5 patients completed the study.
Pasquali et al. (1985) reported the effects of ephedrine in the treatment of obesity. A doubleblind controlled study was performed on 62 consecutive, unselected obese patients (i.e., strict
exclusion criteria were not applied). Patients were treated for 3 months with placebo (Group I),
25 mg 3 times a day or 50 mg or ephedrine 3 times a day (Group II and Group III, respectively).
The group composition: Group I (16 subjects - 12 female/4 male); Group II (13 subjects - 9
female/4 male); Group III (17 subjects - 11 female/6 male). During the first month of treatment,
5 patients were excluded for non-compliance with the protocol study; moreover, 10 other
subjects stopped the therapy spontaneously due to the presence of undesirable effects and 1
female patient was removed from the study due to pregnancy. Of these patients, 5 belonged to
the Placebo group, 6 belonged to Group II and 5 belonged to Group III. The final subject sample
that was considered in the analysis of the results by the authors, included only those subjects who
had completed at least 1-month’s treatment which consisted of 46 subjects (32 females/14
males). Forty participants completed the second month, and 31 completed third month of the
trial. Four subjects were excluded during the second month and 9 during the third month for
non-compliance with the treatment regimen.
During follow-up appointments, pulse rate, arterial blood pressure and incidence of adverse
effects were recorded. Effects such as agitation, insomnia, headache, weakness, palpitation,
giddiness, tremor, and constipation were present in the group treated with 150 mg/day but
disappeared with time, and treatment was reported to be well tolerated. A statistically significant
difference between incidence of effects was reported for the 150 mg/day group compared to
placebo; however, no significance was reported in subjects treated with 75 mg/day compared to
placebo. No significant compound-related effects on arterial blood pressure were present in any
treatment group. Patients treated with 150 mg/day of ephedrine had a small but significant
increase in pulse rate, when compared to placebo. It is interesting to note that strict exclusion
criteria were not applied in this study which would be representative of a general population of
fairly diverse individuals.
In a later study, Pasquali et al. (1987) studied the effects of ephedrine in low-energy adapted
obese women. A double-blind cross-over randomized study was performed in 10 selected adult
overweight or obese women. Treatment consisted of 50 mg of ephedrine 3 times a day (150 mg
ephedrine/day) or placebo, after a period of stabilization with a low diet for 1 month. Each
treatment lasted for a duration of 2 months. It was reported that the incidence of side effects was
very rare and only a few women during the first month presented mild forms of agitation (2),
Council for Responsible Nutrition
December 19, 2000
132
insomnia (3), palpitation (2), or giddiness (2), while taking ephedrine. No significant changes in
arterial blood pressure or pulse rate were found.
4.2.3.1
Summary/Discussion of Obesity Clinical Trials
Twenty studies in obese, but otherwise reportedly healthy individuals, investigated the effects of
ephedrine intake (Astrup et al., 1985, 1992; Pasquali et al., 1985, 1987, 1992; Krieger et al.,
1990; Daly et al., 1993; Molnár, 1993; Toubro et al., 1993a,b; Breum et al., 1994; Buemann et
al., 1994; Kaats and Adelman, 1994; Moheb et al., 1998; Waluga et al., 1998; Huber, 1999,
2000; Nasser et al., 1999; Boozer et al., 2000; Molnár et al., 2000). Ephedrine exposures
involved oral administration over durations from 10 days to 26 months. The range of total doses
within these studies was from 50 to 150 mg/day, given at frequencies of 1 to 3 times/day to
achieve the daily maximum specified. Information on possible side effects was not reported in
several studies due in part to the focus on efficacy; however, the recent Boozer et al. (2000)
reported the long-term safety of an herbal ephedra supplement and provides strong evidence to
support the safety of ephedra use.
Based on the strengths of the study design, duration of study, number of subjects enrolled and
endpoints evaluated, studies conducted in obese individuals were determined to be of sufficient
quality and consistency for inclusion as the critical dataset for the determination of a UL (see
Section 6.0). It is expected that obese subjects would not be more or less sensitive than nonobese subjects using ephedrine-containing dietary supplements. Review of the literature
pertaining to issues dealing with sensitivity of adverse events in lean and obese subjects has
revealed conflicting findings.
Clinical trials examined the effects of ephedrine, either singly or combined with caffeine or ASA
on weight loss in the treatment of obesity. Given that many dietary supplements containing
ephedrine also contain other ingredients, these evaluations provide useful information on the
safety and tolerability in fairly diverse populations.
In general, the treatment and placebo groups were comparable with respect to age and weight of
individuals. There were however differences within and among groups with respect to gender.
For many of the studies, females were more often enrolled compared to males, although both
genders are represented in the database used to derive the UL.
Nine studies were determined to be of sufficient quality and are given the greatest weight.
Studies by Pasquali et al. (1985), Krieger et al. (1990), Astrup et al. (1992), Quaade et al. (1992),
Council for Responsible Nutrition
December 19, 2000
133
Daly et al. (1993), Toubro et al. (1993a,b), Nasser et al. (1999), Boozer et al. (2000), and Molnár
et al. (2000) were conducted using a randomized, double-blind, placebo-controlled design.
Ephedrine was taken daily for at least 8 weeks. Heart rate, blood pressure, adverse effects,
frequency of adverse effects and related tolerability parameters were monitored. Doses of up to
90 mg/day were well-tolerated in all studies. Any effects which were reported were minor and
disappeared over time. Astrup et al. (1992), Quaade et al. (1992), and Toubro et al. (1993a)
reported a statistically significant increase in frequency of events at 60 mg/day only up to Week
4. These effects did not persist, even at durations of exposure of 24 weeks and 50 weeks in the
follow-up study. In Molnár et al., 2000, treatment up to 60 mg/day in adolescents (18 years
old) showed no change in frequency of side effects, heart rate or blood pressure and clinical
chemistry measurements such as hemoglobin, hematocrit, white blood cell and platelet count,
ASAT, LDH etc; however, these results support the selection of 90 mg/day as the NOAEL for an
adult population and are not intended to support use in person aged 18 years old or younger. The
selection of 90 mg/day is a conservative value for a NOAEL in light of the evidence of no
significant increases in frequency of effects or changes in heart rate or blood pressure at or below
that level that resulted in arrhythmia. It is important to note that the effects which were reported
were expected, anticipated physiological responses to ephedrine. No studies reported any
serious, unanticipated toxicities.
4.2.4
Asthmatic Patients
Oral ephedrine was previously used as a bronchodilator in mildly asthmatic individuals in which
there is a long history of safe use; however, ephedrine is no longer the compound of choice since
more selective beta2 - agonists are available. Asthmatic patients are included for completeness;
however, use of this population for any generalization to a healthy population is not intended
since asthma is a condition, which typically requires the use of other concomitant drugs to
manage the disease. Of the literature, only 4 studies are highlighted.
Blanc et al. (1997) studied the effects of alternative therapies and their impact on health
outcomes in adult asthma patients. The objective of this study was to study the prevalence and
morbidity of asthma self-treatment with herbal products, coffee, black tea, and over-the-counter
medications containing ephedrine or epinephrine. A cross-sectional analysis of interview data
for 601 adults with asthma was recruited from a random sample of pulmonary and allergy
specialists. The reported prevalence of ephedrine or epinephrine OTC self-medication was 6%.
Taking into account several covariant parameters, such as age, sex, education, marital status,
annual income, severity of asthma score, quality of life score, asthma control score, general
health score, onset in childhood and atopic history, the use of ephedrine or epinephrine OTC
Council for Responsible Nutrition
December 19, 2000
134
products was not associated with either emergency room use or hospitalization. Ingestion of
coffee or black tea was strongly associated with increased risk of emergency department visits
and hospitalization and herbal product ingestion was strongly associated with hospitalization
only. The subgroup of ephedrine herbal users did not have an increased hospitalization risk.
The relative effectiveness and safety of ephedrine, theophylline, and hydroxyzine hydrochloride
and their combinations was studied in a 2-part investigation of 16 youths who had asthma and
exercise-induced asthma (Bierman et al., 1975). The beneficial and adverse effects of the drugs
in the control of asthma were studied. The study employed a double-blind, double orthogonal
Latin square design. The 16 subjects were assigned to each of 8 randomly sequenced drug
periods. Drug sequences involving ephedrine sulfate were: capsule administration of ephedrine
sulfate (25 mg) alone; ephedrine sulfate (25 mg) together with theophylline (130 mg); ephedrine
sulfate 25 mg + hydroxyzine hydrochloride (10 mg); ephedrine sulfate (25 mg) + theophylline
(130 mg) + hydroxyzine hydrochloride (10 mg). There was a 24-hour wash-out period between
drug trials. Safety parameters evaluated included measurements of pulse rates and adverse
effects in addition to measurements of asthmatic parameters. Ephedrine treatment together with
theophylline resulted in increased undesirable side effects, which made the treatment
unacceptable to 50% of the participants. Ephedrine treatment singly resulted in the lowest
frequency of effects reported in this study but was not efficacious in the treatment of the asthma.
The addition of hydroxyzine diminished the side effects appreciably and was the most efficacious
in the treatment of exercise-induced bronchoconstriction.
Comparative effects of ephedrine on adrenergic responsiveness was assessed in normal and
asthmatic subjects. Six normal subjects and 10 mildly asthmatic subjects were treated with equal
amounts of ephedrine at 25 mg 4 times daily for 7 to 10 days. During the control and placebo
periods, the measurements of cyclic adenosine monophosphate in leukocytes of asthmatic
subjects were similar to those of normal subjects. Baseline measurements were taken of plasma
glucose, plasma cortisol, and leukocyte cyclic AMP, and pulmonary function. It was reported
that the majority of the subjects in both groups experienced nervousness and insomnia during
treatment with ephedrine. No difference in sensitivity with respect to side effects was noted
between asthmatic and normal individuals.
The cardiopulmonary effects of long-term bronchodilator administration were investigated in
patients suffering from chronic asthma (Wilson et al., 1976). Patients suffering from chronic
asthma and requiring more continuous treatment were enrolled in this study. To avoid effects of
previous medications, bronchodilator drugs were not taken for the period of their effective action
prior to study. The patients were randomly assigned, and double-blinded for the ephedrine and
Council for Responsible Nutrition
December 19, 2000
135
terbutaline administration. The investigation was initially designed for 3 to 6 months duration;
however, good therapeutic success was achieved, and patients were permitted to remain in the
study for up to 1 year. Study participants took 25 mg of ephedrine 3 times daily (75 mg/day) and
5 mg (15 mg) of terbutaline 3 times per day. Among asthma/respiratory parameters evaluated,
heart rate was calculated from an electrocardiographic rhythm strip and blood pressure was
measured. Physical examinations included electrocardiograph, hematocrit, red and white cell
counts, and differential, urinalysis. Plasma chemistries (Na, K, Ca, Cl, HC02), blood urea
nitrogen (BUN), creatinine, uric acid, serum glutamic oxaloacetic transaminase (SGOT), serum
glutamic pyruvic transaminase (SGPT), lactic dehydrogenase (LDH), creatine phosphokinase
activity (CPK), alkaline phosphatase, glucose, cholesterol, bilirubin, total protein, and albumin,
were performed at monthly intervals. Chest films and ophthalmologic examinations were
obtained every 6 months. Side effects were evaluated by daily patient diary and monthly
historical review with a physician.
It was reported that all cardiovascular changes following onset of treatment were of relatively
small magnitude. Over the year of investigation both baseline systolic pressure and diastolic
pressure progressively fell, particularly during the last 6 months. Baseline heart rate changed
little in the ephedrine group. Urinalysis, blood counts and chemistries, electrocardiograms, and
physical and ophthalmologic examinations either remained within normal limits or demonstrated
no new abnormalities for ephedrine treatment at 75 mg/day.
4.2.5
Hypertensive Patients
Persons with hypertension should be aware that some of the nonprescription drugs and other
agents available may affect blood pressure control. In a review by Bradley (1991), it was
published that approximately 300,000 medications containing 700 active ingredients are
available over-the-counter. Some, but not all of these products bear warning labels regarding use
in persons with hypertension. Since this publication, it is certain that these numbers have
increased. In general, adrenergic agents such as phenylpropanolamine, ephedrine,
pseudoephedrine and phenylephrine should be used with caution or avoided by hypertensive
patients (Insel, 1991).
Ingerslev et al. (1997) studied the effects of ephedrine and caffeine combination on blood
pressure in normotensive and hypertensive patients treated with adrenergic beta-receptor
blocking drugs and/or other antihypertensive agents for a period of 6 weeks. The study was
conducted in a double-blind, randomized, placebo-controlled manner, with a study of 5 parallel
groups of overweight patients from general practices. Treatment consisted of ephedrine 20 mg
Council for Responsible Nutrition
December 19, 2000
136
and caffeine 200 mg per tablet (E+C). The dosage regimen included 1 tablet on Day 1, 2 tablets
on Day 2, and 3 tablets a day for the remainder of the 6 weeks. This study was designed with a
rapid increase of E+C dose over 3 days. The purpose of this study was to evaluate the possible
risks of developing hypertension or tachycardia in normotensive patients, or of reducing the
effect of an antihypertensive treatment administered to well-regulated hypertensive patients with
or without betablockers. One hundred and thirty-six patients were randomized into 5 groups.
The composition of these patient groups is summarized in Table 4.2.5-1.
Table 4.2.5-1
Summary of Study Design of Ingerslev et al. (1997)
Group
No. of Subjects (Gender)
Patient Description and Study Medication
Group I
25 (7 male/28 female)
Hypertensive + betablocker + E+C
Group II
28 (14 male/14 female)
Hypertensive + antihypertensive but not betablocker + E+C
Group III
28 (9 male/19 female)
Normotensive + E+C
Group IV
28 (14 male/14 female)
Hypertensive + placebo
Group V
25 (3 male/22 female)
Normotensive + placebo
The study schedule involved monitoring blood pressure and heart rate 2 to 3 times daily at home
during the week prior to onset of treatment and during the first week of treatment. This close
monitoring at home during the first week of treatment was used to provide data on very acute
effects of treatment. Blood pressure, heart rate, and weight were measured weekly and on Day 1
after discontinuation of treatment. At each weekly visit to the study site, all patients were asked
if any side effects were experienced.
Test article administration consisted of E+C tablets consisting of 20 mg of ephedrine and 200 mg
of caffeine. Anorexia drugs or monamine oxidase inhibitors were not permitted during the trial
while other chronic therapy including antihypertensives continued unchanged. In the physician’s
office, blood pressure and heart rate were measured. At each visit, the patient was asked if the
treatment had resulted in any discomfort. The nature, duration and intensity were recorded.
Patients were withdrawn from the study if the diastolic blood pressure rose to 115 mm Hg, and in
the case of unacceptable adverse reactions.
One hundred and thirty-six patients were included in the study. Two patients were withdrawn at
the second visit before the study medication was delivered. Within the first week of treatment, a
further 7 patients were withdrawn. Fifteen patients were treated for less than 5 weeks. The
population included in the full protocol therefore comprised 112 patients. A total of 124 patients
Council for Responsible Nutrition
December 19, 2000
137
were included in the primary analysis of side effects. Six patients treated with E+C and no
placebo-treated patients were withdrawn due to undesirable effects.
Systolic blood pressure was reduced significantly in the hypertensive group treated with
antihypertensive agents other than betablockers, plus E+C. In the other hypertensive groups,
blood pressure did not change significantly. In the normotensive group tested with E+C, both
systolic and diastolic blood pressure were reduced significantly. Blood pressure values taken
before treatment and during treatment were not statistically different. Heart rate increased
significantly (an average of 4.9 bpm) only in normotensive patients receiving E+C.
With respect to effects, in the E+C treated groups 45 of the 81 patients had effects which
included nausea (12%), palpitations (10%), increased perspiration (6%), and tremor (5%). Six
patients (7%) from the E+C group were withdrawn from the study due to such effects. In the
placebo group, 21% reported undesirable effects, mainly palpitations (6%) and nausea (4%). The
difference between the E+C and the placebo group was significant. The authors reported that no
serious adverse events occurred. Any possible difference between effects reported with E+C
treatment in normotensive vs. hypertensive individuals was not reported. Based on these
findings, E+C did not increase blood pressure in either normotensive or hypertensive patients
during short-term treatment. During the first week of treatment no significant differences
between the groups were detected in home measured heart rate. During the 6-week study, a
significant increase in heart rate (4.9 beats per minute) was demonstrated in the normotensive
group treated with E+C which was attributed by the study authors to be due to the
pharmacological effect of E+C. In long-term studies of E+C combination, Astrup et al. (1992)
and Breum et al. (1994) studied the effects of combination products on the cardiovascular
system. They found declining diastolic and systolic blood pressure and unchanged or slightly
increased heart rate during a period of 24 weeks and 15 weeks respectively. The authors
concluded that the study did not support the assumption that E+C would cause significant blood
pressure rises in normotensive, or well-treated hypertensive, obese patients, either at the
beginning of the treatment or after 6 weeks of treatment. The anti-hypertensive effect of
betablockers was not impaired by E+C.
4.2.5.1
Summary/Discussion of Hypertensive Patient Study
Although the study conducted by Ingerslev et al. (1997) showed that ephedrine/caffeine
combination at 60/600 mg/day did not increase blood pressure in normotensive, or well-treated
hypertensive, obese patients, either at the beginning of the treatment or after 6 weeks of
treatment. The hypertensive subjects investigated in this study were treated with other
Council for Responsible Nutrition
December 19, 2000
138
pharmacological agents which were well monitored by their original physicians. Even though it
is recommended that ephedrine not be used in hypertensive individuals these data demonstrate
that serious adverse events do not arise from intake of 60 mg ephedrine together with 600 mg
caffeine/day in hypertensive individuals with or without pharmacological treatment.
Unfortunately, the frequency and characterization of effects for normotensive versus hypertensive
individuals were not reported; however, the authors reported no serious adverse events occurred.
4.2.6
Smoking Population
Norregaard et al. (1996) studied the effects of a combination of ephedrine and caffeine on a
population of 225 heavy smokers who wanted to quit smoking without gaining weight. The
study was conducted in a randomized double-blind placebo-controlled manner with a 1-year
follow-up period. The approximate ages of the smokers were between 25 to 65 years of age, who
smoked at least 10 cigarettes a day for a minimum of 3 years. Exclusion criteria were the
presence of cardiovascular disease, previous myocardial infarction or heart failure,
hyperthyroidism, gastric or duodenal ulcers within the past 3 months, pregnancy or breastfeeding, daily use of psychotropic drugs (including anxiolytics), daily alcohol consumption of
more than 3 drinks a day, acute medical disease, hypertension, competition sports, low body
weight, and intake of other ephedrine-caffeine combinations during the last 2 years.
Eight visits of approximately 60 minutes were scheduled during the 52-week study period (at the
beginning of the study and after Weeks 1, 3, 6, 12, 26, 39, and 52). The subjects were advised to
stop smoking completely from the start of the study. All the subjects were randomized to
treatment with the ephedrine plus caffeine combination or placebo tablet. Two-thirds of the
subjects were randomized to receive 20 mg ephedrine plus 200 mg caffeine 3 times a day; onethird of the subjects received placebo treatment. On the first day of treatment the participants
were instructed to take only 1 tablet, on the second day subjects were instructed to take 2 tablets,
and then 1 tablet 3 times per day for the next 3 months. After this time the dosage was reduced
to 1 tablet 2 times per day for months 4 though 6, followed by 1 tablet daily for another 3
months. During the last 3 months they took no trial medication. If patients were troubled by
effects of treatment, they were instructed to reduced dosage by themselves or dosage was reduced
by the physician at the clinical visits. At each visit subjects were interviewed about smoking
during the last period. Measurements of carbon monoxide were made to confirm consistency
with participants. At the initial visit and after 6 and 52 weeks venous blood samples were taken.
Serum cholesterol and high density lipoprotein (HDL) cholesterol, bilirubin, lactate
dehydrogenase, alkaline phosphatase, and aspartate aminotransferase were also determined for
Council for Responsible Nutrition
December 19, 2000
139
the purpose of establishing the tolerability of the treatment. Occurrence of palpitations, increased
perspiration, nausea, dizziness, and other possible adverse effects were scored.
The subjects in the ephedrine plus caffeine treated group reported significantly more palpitations,
sweating, dizziness, and nausea during the first week. The differences leveled off during the
following weeks. Problems falling asleep and poor sleep scored higher in the ephedrine plus
caffeine-treated subjects at Weeks 1 and 3, but not later. Six subjects in the treatment group
withdrew due to troubling effects. In all these subjects, the symptoms subsided the day after
cessation of treatment. There were no differences in smoking withdrawal symptoms among
treatment groups. Blood biochemistry of lactate dehydrogenase and alkaline phosphatase did not
change after the start of the study but aspartate aminotransferase showed a significant median
increase of 2 mmol/L (no significant differences between the treatment groups). This study
reported good tolerability of doses up to 60 mg/day of ephedrine and 600 mg/day caffeine for up
39 weeks.
4.2.6.1
Summary/Discussion of Smoking Population Data
Group characteristics have important implications for the interpretation of clinical trial studies.
As such, the possible contribution of tobacco use (smoking) could by addressed by analysis of
the study conducted by Norregaard et al. (1996) on the effects of ephedrine and caffeine on a
population of 225 heavy smokers who wanted to quit smoking. This was the only published
report identified in the literature that evaluated the effects of ephedrine in a population of
smokers, albeit these smokers were trying to quit. Most clinical trials applied strict exclusion
criteria which included exclusion of smokers. Review of published case reports revealed some
subjects who had adverse effects and were reported to be smokers, but a causal association
between these individuals and ephedrine intake could not be made.
The study conducted by Norregaard et al. (1996) studied subjects for 1 year who smoked at least
10 cigarettes a day for a minimum of 3 years, in a randomized double-blind placebo-controlled
manner. Other than the smoking, these individuals were otherwise reportedly healthy. The
subjects in the ephedrine plus caffeine treated group reported significantly more palpitations,
sweating, dizziness, and nausea during the first week. It was reported that the differences leveled
off during the following weeks. Problems falling asleep and poor sleep scored higher in the
ephedrine plus caffeine-treated subjects at Weeks 1 and 3, but not later. Six subjects in the
treatment group withdrew due to adverse effects. In all these subjects, the symptoms subsided
the day after cessation of treatment. This study reported good tolerability of ephedrine at doses
up to 60 mg/day of ephedrine and 600 mg/day caffeine for up to 39 weeks.
Council for Responsible Nutrition
December 19, 2000
140
5.0
EVALUATION OF UNCERTAINTIES
5.1
Are Results with Ephedrine Applicable for Extrapolation to
Ephedra/Ephedrine Alkaloids?
In most Ephedra species used commercially, the dominant alkaloid is ephedrine, which usually
comprises between 40 to 90% of total alkaloids in the plant, depending on the species. Other
related alkaloids are also isolated such as pseudoephedrine, N-methylephedrine, Nmethylpseudoephedrine, norpseudoephedrine, and norephedrine (phenylpropanolamine). These
alkaloids have been collectively termed ephedrine-type alkaloids, or simply ephedrine alkaloids.
Proportions and total levels can vary from one species to another, time of year of harvest,
weather conditions, and altitude. Pseudoephedrine is present at only 20 to 25% the levels of
ephedrine, but may be as high as 50 percent of the amount of ephedrine.
The physiological characteristics of ephedra are dependent upon its chemical composition. In
general, all the ephedrine alkaloids contained in ephedra show significant diastereoselective
differences with regard to pharmacokinetic and pharmacodynamic effects. All have effects on
the cardiovascular and respiratory system, but not to the same degree. It is important to note that
the pharmacokinetic and toxicokinetic behavior of any isomer cannot be used to predict that of
any other ephedrine alkaloid isomers.
In the literature, statements regarding ephedrine alkaloids sometimes consider them to be
synonymous, which implies that the pharmacological activity and toxicity of all optical
isomersenantiomers are equivalent, which is not the case. Nevertheless, since the dominant
ephedrine alkaloid isomer in most Ephedra species is ephedrine, the characteristics of ephedrine
would provide a good indicator of the expected chemistry, physiology and toxicology. As with
any mixture, the characteristics of only one, albeit major, component cannot define all of the
characteristics of ephedra. However, in the case of ephedra, understanding the effects of
ephedrine provides insight into the biological activities of the herb itself. Furthermore, Lee et al.
(1999; 2000) recently reported that the potency of adrenergic activity and cytotoxicity of ma
huang extracts correlated with the ephedrine content; however, the cytotoxicity of all ma huang
extracts could not be totally accounted for by their ephedrine contents.
With regard to pseudoephedrine, since its effects are similar to ephedrine but are somewhat
weaker with respect to the hypertensive effects and stimulation of the central nervous system,
this assessment using ephedrine as a surrogate for ephedra will provide a conservative
Council for Responsible Nutrition
December 19, 2000
141
evaluation. Where available, data related to ephedra are discussed, but data on ephedrine are
considered because they contribute to the total evidence relevant to ephedra.
The acute toxicity of the ephedra herb was assessed in one study; subcutaneous and oral LD50
was 1 to 1.4 g/kg (Ueng et al., 1997), whereas oral administration was 5.30 g herb extract/kg and
24 g crude herb/kg (Minamatsu et al., 1991). Furthermore, in a comparative study between
ephedra and ephedrine, there was an indication that there may be a difference in toxicity. For
ephedra extract, the LD50 value was higher (i.e., less toxic) than ephedrine when normalized
based on ephedrine content, the general symptoms observed were milder in nature, and time to
death was longer than that of ephedrine. These results highlight the conservative assumption that
ephedrine content be used to characterize the effects of ephedra, since the toxicity assessment of
ephedrine shows that this approach overestimates the potential toxicity of ephedra itself.
5.2
Conservatism Built into the Risk Assessment
As stated above and throughout the report, the chemical/physiological characteristics of ephedra
are dependent upon its chemical composition. Since ephedrine is the dominant ephedrine
alkaloid isomer of most Ephedra species, the characteristics of ephedrine would provide a good
indicator of the expected chemistry, pharmacology, and toxicology. As with any mixture, the
characteristics of only one, albeit major, component cannot account for all the constituents of
ephedra, but ephedrine represents a significant portion of ephedra’s activity. This assumption
has not been confirmed in clinical studies.
Furthermore, the use of ephedrine as a surrogate for ephedra is appropriate given recent findings
(Lee et al., 1999, 2000) that the potency of adrenergic activity and of cytotoxicity of ma huang
extracts correlates with the ephedrine content. It was noted that the cytotoxicity of all ma huang
extracts tested could not be totally accounted for by their ephedrine contents. If there are
differences between the effects of ephedrine and the ephedrine alkaloids in ephedra, the use of
ephedrine data will overestimate the risk from ephedra.
5.3
Individual Risk Factors
It has been reported recently that the dietary supplement industry estimates that as many as 2 to 3
billion doses of dietary supplements containing ephedrine alkaloids are consumed each year in
the United States (GAO, 1999; AHPA, 2000). Despite the high usage levels of ephedrinecontaining supplements, adverse events reported to FDA SN/AEMS together with the published
case reports are numbered in the hundreds. If, in fact, these adverse events are in part due to
Council for Responsible Nutrition
December 19, 2000
142
ephedrine intake, it is possible that the very small proportion of reported adverse events arises
from substantial differences in individual susceptibility.
Ephedrine and related agents should not be administered, for example, to individuals with
coronary thrombosis, diabetes, glaucoma, heart disease, hypertension, thyroid disease, impaired
circulation of the cerebrum, autonomic insufficiency, pheochromocytoma, chronic
anxiety/psychiatric disorders or enlarged prostate (Dollery, 1991a; Hoffman and Lefkowitz,
1996). Patients with renal impairment may be at special risk for toxicity. Co-administration of
ephedrine-containing preparations with monomine oxidase inhibitors is contraindicated as the
combination may cause severe, possibly fatal, hypertension (Hoffman and Lefkowitz, 1996).
Other risk groups may include neonates and breast-fed infants secondary to maternal exposure,
pregnant women, children, and the elderly. These groups are potentially at risk because of their
known sensitivity to the effects of sympathomimetic stimulation and because the potential effects
of ephedrine and related compounds in these populations have not been well studied.
5.4
Uncertainties Pertaining to Study Findings
Clinical studies in healthy human subjects, obese subjects, asthmatic subjects, smokers, and
hypertensive individuals were reviewed. These studies provided an opportunity to assess the
safety and tolerability associated with ephedrine use. There are a number of recognized
limitations in clinical investigations associated with study design, methods and conduct, limited
number of subjects enrolled, and publication of certain information but not other (gaps).
Furthermore, unlike animal experiments where the conditions of the study (e.g., doses, duration
of treatment) can be controlled and defined, observations in human subjects often suffer from
bias and the lack of objective assessments. Randomized, double-blind, placebo-controlled
studies are considered the least likely to result in bias.
Typically, studies in the healthy population consisted of small numbers of patients, were not
designed to examine safety and were of limited duration (24 hours or less). The clinical studies
in obese subjects examined the effects of ephedrine or ephedra up to 26 months. It should be
noted that taken collectively, clinical studies have assessed the potential
pharmacological/toxicological effects of ephedrine/ephedra long term.
Studies in obese individuals were principally designed to test the efficacy of ephedrine/ephedra in
the treatment of obesity, rather than the safety of use in this population. Furthermore,
progressive doses were not assessed, not permitting analysis of dose-responsiveness of any
effects. Other limitations specific to the studies evaluated in the ephedrine/ephedra database
Council for Responsible Nutrition
December 19, 2000
143
include the selective reporting of incidence and severity of any effects, discussion of withdrawals
and publication of multiple studies using same subjects/data. In the ephedrine database, only
those clinical studies were reviewed with adequate measurements of safety/tolerability
parameters rather than just efficacy.
For many of the studies, the clinical trials used strict exclusion criteria to eliminate potential
confounding factors which may prevent interpretation of the study results (i.e., concurrent
medication usage, determination of underlying diseases, conditions or other risk factors). The
use of exclusion criteria does not reduce the utility of these findings, since the exclusion criteria
were based on known contraindications which would also apply to a typical dietary supplement
user taking a product containing ephedra. Furthermore, the majority of the studies employed an
open-label type setting, which was not necessarily a carefully controlled, physician-monitored
clinical trial. In particular, due to the duration of the trials (typically 13 weeks, but sometimes up
to 26 months), the conditions of use in these trials would mimic the conditions found under
normal use settings, even though regular maintenance visits to study monitors took place.
Although taken together, obesity trials have evaluated a significant number of individuals with
ephedrine intake, these studies do not have adequate numbers of subjects to detect uncommon
adverse effects that may be related to individual susceptibility. This deficiency is also
characteristic of all clinical trials with pharmaceuticals and not limited to these obesity trials.
5.5
Uncertainties Pertaining to Group Characteristics
Group characteristics have important implications for the interpretation of clinical trial studies
and are summarized below.
The majority of the randomized trials conducted in clinical studies have been investigated in
obese subjects. Given the known chemical and metabolic characteristics of ephedrine,
differences are unlikely in the sensitivity and/or pharmacokinetic handling of ephedrine in obese
vs. non-obese individuals. Review of literature pertaining to issues dealing with sensitivity of
adverse events in lean and obese subjects has revealed conflicting findings. Horton and Geissler,
(1991) reported on the effect of ephedrine (30 mg) and ASA (300 mg) on the acute thermogenic
response to a liquid meal in lean and obese women. Analysis of subjective response to treatment
showed that fewer adverse effects were noted for the drug treatments in the obese subjects
compared to the lean group. In 2 later studies from the same authors (Geissler, 1993; Horton and
Geissler, 1996), these findings were not confirmed and no such difference in sensitivity was
observed. No significant correlations were found in either the lean or the obese with respect to
Council for Responsible Nutrition
December 19, 2000
144
the number of effects. Based on the more recent studies from the same investigators, there is no
compelling evidence that any differences in sensitivities to ephedrine would be expected in lean
vs. obese individuals.
It has also been reported that among athletes, ephedrine used as an ergogenic, or performanceenhancing agent. Athletic competition normally exerts extra demands on the cardiovascular
system. The toxicity of sympathomimetic agents can be exacerbated by physical exercise,
dehydration and increases in body temperature. The use of sympathomimetic drugs by
recreational and competitive athletes attempting to improve performance, decrease body fat and
increase lean body mass may be of concern (Catlin and Hatton, 1991). Products for performance
enhancement are generally compounded with other ingredients such as vitamins, minerals, and
amino acids, to increase muscle mass and enhance endurance (Clarkson and Thompson, 1997).
There have been reports of ephedrine abuse among professional weightlifters (Gruber and Pope,
1998).
Five studies in healthy normal individuals investigated the effects of exercise/physical
parameters together with ephedrine use (Sidney and Lefcoe, 1977; Strömberg et al., 1992;
Vanakoski et al., 1993; Bell et al., 1998; Bell and Jacobs, 1999). The range of total doses within
these 5 studies was from 24 to 81 mg/day together with exercise, or some physical exertion over
a short duration of exposure (typically 24 hours). Nausea was reported by Bell et al. (1998)
subsequent to caffeine+ephedrine intake with exercise; however, in a subsequent study by the
same investigators, nausea was not reported and no clinical signs were attributable to
caffeine+ephedrine intake together with exercise. Higher heart rate was reported from ephedrine
treatment (either singly or combined with caffeine intake) in all studies which tested the
concomitant effects of intake with exercise/physical exertion. In all studies, no adverse effects
were reported. Taken together, these studies demonstrated the known effects physical exercise
and increases in body temperature may have in connection with sympathomimetic agents. These
physical factors did not result in toxicity from ephedrine use.
The possible contribution of tobacco use (smoking) in the analysis of the safety of ephedrine
could be addressed by analysis of the study conducted by Norregaard et al. (1996) on the effects
of ephedrine and caffeine on a population of 225 heavy smokers who wanted to quit smoking.
This was the only published report identified in the literature that evaluated the effects of
ephedrine in a population of smokers (smoked at least 10 cigarettes a day for a minimum of 3
years), albeit these smokers were trying to quit. Most clinical trials applied strict exclusion
criteria which included exclusion of smokers. Review of published case reports revealed some
subjects who had adverse effects and were reported to be smokers, but a causal association
Council for Responsible Nutrition
December 19, 2000
145
between these individuals and ephedrine intake could not be made. This study reported good
tolerability at 60 mg/day of ephedrine and 600 mg/day caffeine for up to12 weeks.
Oral ephedrine was previously used as a bronchodilator in mild asthmatic individuals in which
there is a long history of safe use; however, ephedrine is no longer the drug of choice since more
selective 2 - agonists are available. Studies with asthmatic patients are reviewed for
completeness; however, use of this population for any generalization to a healthy population is
not intended, since asthma is a condition which typically requires the use of other concomitant
drugs to manage the disease.
Ingerslev et al. (1997) investigated the effect of an ephedrine+caffeine combination at 60 mg:600
mg/day on blood pressure in normotensive and well-treated hypertensive, obese patients after 6
weeks of treatment. Even though it is recommended that ephedrine not be used in hypertensive
individuals and the subjects investigated in this study were treated with other pharmacological
agents which were well monitored by their original physicians, these data demonstrate that
serious adverse events did not arise from the intake of 60 mg ephedrine together with 600 mg
caffeine/day in this study of hypertensive individuals, with or without pharmacological treatment.
5.6
Uncertainties in Ephedrine Content in Botanically-Derived Supplements
Most ma huang product labels indicate how much ephedra herb is contained in each dosage form;
however, few make a claim of ephedrine or ephedrine alkaloid content. For consumers, this can
be misleading because Ephedra species vary widely in their ephedrine alkaloid content. This is
determined by where the plant is grown, the type of growing conditions, and the time of harvest
(Sagara et al., 1983; Zhang et al., 1993). It was recently reported that ephedrine alkaloid content
varied by as much as 5-fold between commercially available ma huang products, with brands
exhibiting lot-to-lot differences of 44 to 260% (Gurley et al., 1997b, 2000). This natural
inconsistency gives rise to commercial products with significant interproduct and intraproduct
variability (Betz et al., 1997; Gurley et al., 1997a,b, 1998b, 2000).
5.7
Uncertainties in Related Ephedrine Alkaloid Content in Botanically-Derived
Supplements
Phenylpropanolamine, also called norephedrine is a minor constituent found in ephedra and is a
metabolite of ephedrine. PPA represents between 1.6 to 8.1% of total alkaloids measured in
Ephedra species used to obtain ephedrine (Hu, 2000). In a recent evaluation of ephedrine
alkaloids found in 20 ephedra supplements, PPA represented 0.16 – 0.25 mg per dosage unit in 6
Council for Responsible Nutrition
December 19, 2000
146
supplements (Gurley et al., 2000). It was reported that norephedrine/PPA was the least prevalent
alkaloid measured in this analysis. Most supplements screened (14/20) were below the limit of
quantitation for norephedrine/PPA. The dose level of PPA is expected to be minimal, based on
minor and sometimes trace amounts of PPA found in ephedra supplements.
For completeness, the recent findings from the Hemorrhagic Stroke Project are presented which
suggest an association between consumption of PPA and hemorrhagic stroke. It is important to
note that dose levels of PPA, which is a minor alkaloid in ephedra, would not approach the
median dose level of PPA (75 mg) examined in this investigation, or the dose levels of PPA
found in recent over-the-counter preparations.
Responding to ongoing concerns about PPA and the risk for hemorrhagic stroke, but the very
recent findings are the subject of vigorous debate. in 1992 the FDA joined with manufacturers of
products containing PPA to recommend the conduct of an epidemiological study of the possible
association (HSP, 2000; Kernan et al., 2000). The research team was called the Hemorrhagic
Stroke Project. To examine this association, a case-control study involving men and women ages
18 to 49 years who were hospitalized with a subarachnoid hemorrhage (SAH) or intracerebral
hemorrhage (ICH). The research was designed and implemented with three co-equal specific
aims:
(1)
(2)
(3)
among men and women ages 18 to 49 years, to estimate the association between PPA
and hemorrhagic stroke;
among the same target group, to estimate the association between PPA and
hemorrhagic stroke by type of PPA exposure (cough-cold remedy or appetite
suppression); and
among women ages 18 to 49 years, to estimate; a) the association between first use of
PPA and hemorrhagic stroke and b) the association between PPA in appetite
suppressants and hemorrhagic stroke.
Case subjects were recruited from hospitals in 4 geographic regions of the United States. Study
recruitment involved 2 control subjects for each case subject, matched on age, gender, race and
telephone exchange. Cases and control subjects were interviewed to determine their medical
history, health behaviors and medication usage. A subject was classified as exposed to PPA if
they reported use within 3 days of the stroke event for case subjects or a corresponding date for
control subjects. The exposure was verified through use of a structured questionnaire developed
for this study which assisted subjects recalling details of their medication use, then through
Council for Responsible Nutrition
December 19, 2000
147
identification of product consumed and finally subjects were asked to produce the actual
container of medication reported.
The first co-equal specified aim was to determine whether PPA users, compared to non-users had
an increased risk of hemorrhagic stroke. The odds ratio calculated from conditional logistic
models for matched sets; revealed for any use of PPA within T3 days (either for cough-cold
remedy or appetite suppression), the unadjusted odds ratio was 1.67 (p=0.040) and the adjusted
odds ratio was 1.49 (lower limit of the 1-sided 95% confidence interval (LCL)=0.93, p=0.084).
The second co-equal specific aim was to estimate the association between use of PPA and
hemorrhagic stroke according to type of PPA exposure. For the association between PPA use in
cough-cold remedies within the 3-day exposure window, the unadjusted odds ratio was 1.38
(p=0.163). The adjusted odds ratio was 1.23 (LCL=0.75, p=0.245). For the association between
PPA use in appetite suppressants within the 3-day exposure window, the unadjusted odds ratio
was 11.98 (p=0.007) and the adjusted odds ratio was 15.92 (LCL=2.04, p=0.013).
The third co-equal specific aim was to estimate the association between PPA and risk for
hemorrhagic stroke among women for 2 exposure definitions: appetite suppressant use within 3
days and first dose use. For the association between PPA in appetite suppressants and risk for
hemorrhagic stroke among women, the unadjusted odds ratio was 12.19 (p=0.006) and the
adjusted odds ratio was 16.58 (LCL=2.22, p=0.011). Among stroke victims, all appetite
suppressant use within the 3-day exposure window occurred among women. Evaluation of first
dose PPA use, 11 of 13 exposures were among women (7 cases compared with 4 controls). The
unadjusted odds ratio was 3.50 (p=0.039) and the adjusted odds ratio was 3.13 (LCL=1.05,
p=0.042). All first dose PPA use involved cough-cold remedies.
Additional analysis investigated the association between current PPA dose and risk for
hemorrhagic stroke. Analysis for dose showed that the odds ratio was higher for current doses
above the median (>75 mg PPA) (AOR=2.31, LCL=1.10, p=0.031) than for lower doses
(AOR=1.01, LCL=0.43, p=0.490). Potential exposure to PPA through ephedra intake would be
far less than the apparent threshold of 75 mg.
These results, taken together suggest that PPA may increase the risk for hemorrhagic stroke.
Some limitations of the study were noted, which were related to the exclusion of dead or noncommunicative patients. A second limitation noted was the number of case and control subjects
who were exposed to PPA (n=60). Due to the small number of exposure subjects, subgroup
Council for Responsible Nutrition
December 19, 2000
148
analysis could not be undertaken. And lastly, the HSP interviewers were not blinded to the casecontrol status of subjects and some were aware of the study purpose.
There is no evidence that the PPA content of ephedra causes risk of hemorrhagic stroke. In the
Yale study (HSP, 2000; Kernan et al., 2000), significant risk occurred only with PPA intakes
above 75 mg/day. The PPA content of the 90 mg of ephedrine alkaloids in the clinical trial was
less than 1.8 mg/day. Even with a maximum (20 percent) metabolic conversion of the
approximately 60 mg/day of ephedrine in the ephedra given in clinical trial by Boozer and
colleagues, the total PPA exposure would be less than 14 mg/day (60 mg x 0.2 for metabolic
production, plus 1.8 mg preformed), a value far below the apparent threshold of 75 mg/day.
Thus even if hemorrhagic strokes can be related to PPA consumption, no significant effect would
be expected from 90 mg of ephedrine alkaloids in ephedra.
5.8
Uncertainties of Combination Herbal Products or Concomitant Use of Other
Products
Products containing ephedrine, alone or in combination with other ingredients, are marketed as
dietary supplements in the United States. In these products, kola nut, guarauna, and other
botanicals are used as natural caffeine sources. Willow bark is used as a natural source of
salicylates. The pharmacology of most of the individual ephedrine-type alkaloids has been well
characterized, but the effects of combinations of these other compounds are less well known. In
addition, interactions between ephedrine-type alkaloids and xanthine alkaloids, as well as
biologically active compounds in other plant species that are constituents of many dietary
supplements, have yet to be fully examined.
The clinical database that has been considered has involved administration of ephedrine/ephedra
singly, or together with other components such as caffeine or ASA. In addition, studies with
concomitant use of prescription and OTC medications, exposure to caffeine and related
compounds, diet, and use of tobacco are summarized when available and are reviewed insofar as
they contributed to the analysis of ephedrine itself. In particular, literature pertaining to
concomitant use with hypertensive drug therapy and tobacco use has been included (Norregaard
et al., 1996; Ingerslev et al., 1997).
It is known that co-administration of ephedrine-containing preparations with monomine oxidase
inhibitors is contraindicated as the combination may cause severe, possibly fatal, hypertension
(Hoffman and Lefkowitz, 1996). Furthermore, the use of antacids and agents which alter the pH
of urine may affect the duration and magnitude of ephedrine activity, thus affecting absorption
Council for Responsible Nutrition
December 19, 2000
149
and excretion, respectively. Ephedrine is also known to interact with corticosteroids and
theophylline (Upton, 1991). Alcohol may be expected to antagonize the central stimulant effects
of ephedrine (Dollery, 1991a).
Investigators have found that concomitant ingestion of other botanicals and stimulants can affect
the pharmacokinetic profile of ephedrine (Shenfield, 1982; Upton, 1991; Kanfer et al., 1993).
Adverse reactions to ephedrine-type alkaloid have been reported (Lake et al., 1990a,b). The
assumption is that a combination product (i.e., ephedrine/ephedra together with caffeine) would
be no more or less active than an equivalent dose of ephedrine singly. Since combination
products were given in many of the clinical studies, this assessment evaluated the
contribution/interaction of other ingredients typically contained in ephedra preparations, insofar
as they contributed to the analysis of ephedrine itself. The assessment of ephedrine together with
other ingredients is expected to provide a more conservative assessment of the safety of
ephedrine/ephedra.
Council for Responsible Nutrition
December 19, 2000
150
6.0
DOSE RESPONSE ASSESSMENT/CONCLUSIONS FOR THE GENERAL
POPULATION
The framework for developing an Upper Limit (UL) for ephedrine/ephedra intake involves the
use of the Tolerable Upper Intake Level risk assessment model. The UL is established for
ephedrine/ephedra on the basis that the chemical, pharmacological and toxicological
characteristics of ephedra are dependent upon its chemical composition. Since the dominant
ephedrine alkaloid isomer of most Ephedra species is ephedrine, the chemical characteristics of
ephedrine would provide a good indicator of the expected chemistry, pharmacology, and
toxicology. As with any mixture, the characteristics of only one, albeit major, component cannot
account for all the constituents of ephedra, but ephedrine represents a significant portion of
ephedra’s activity. Furthermore, since the effects of pseudoephedrine are similar to ephedrine
but are somewhat weaker with respect to the hypertensive effects and stimulation of the central
nervous system, this assessment will provide a more conservative evaluation based on the
activity of ephedrine, in terms of total ephedrine alkaloid content.
The term Tolerable Upper Intake Level is defined as the maximum level of total chronic daily
intake of a substance judged unlikely to pose a risk of adverse health effects to the most sensitive
members of the healthy population developed by applying uncertainty factors. Although the
model was intended to be used for nutrients, nutrients are like all chemical agents which can
produce adverse health effects if intakes are excessive.
The data evaluation process results in the selection of the most appropriate or critical dataset(s)
for deriving the UL. In the data evaluation process of nutrients, human data are generally
preferable to animal data; however, in the absence of appropriate human data, information from
an animal species whose biological responses are most like those of humans is used. The
available human data provide the most relevant kind of information for hazard identification of
ephedrine/ephedra. Although the focus of these clinical studies was typically efficacy, taken
collectively, they are of sufficient quality and quantity to comment and make conclusions on its
safety. Because adequate human data are available, animal data were not used to derive a UL,
although these data do provide support to the clinical data. Observational data in the form of
case reports were evaluated for their usefulness in developing hypotheses/ relationships between
exposure and effect. A large number of the published observational case reports reviewed in this
assessment represented adverse reactions from situations of long-term abuse/misuse situations
and do not accurately represent the typical adverse event profile from typical ephedrine/ephedra
use. Adverse events reported to FDA are also considered in the evaluation of a UL; however, for
Council for Responsible Nutrition
December 19, 2000
151
a large number of AERs, the frequency, duration of exposure and dose were not reported, which
limits the utility of these data.
Following the assessment of the most appropriate or critical dataset(s), a dose or intake level with
no observable adverse effect (i.e., NOAEL) is chosen. In the absence of a determination of a
NOAEL, a LOAEL is chosen. In principle, the primary aim of safety studies is to recognize the
potential hazards associated with a particular chemical and identify a NOAEL or LOAEL from
the dose-response data. Following characterization of these values, safety factors or uncertainty
factors (UFs)are typically applied. Judgments are made regarding uncertainties associated with
extrapolating from the observed data to the healthy population. A UF is applied to a NOAEL or
LOAEL to derive the UL, which generally represents a lower estimate of the threshold above
which the risk of adverse effects may increase.
6.1
Data Selection
The data on frequency of adverse effects following ephedrine/ephedra intake in obese individuals
were used to derive a UL for the general population. While the data on frequency of adverse
effects reported in these studies were used for the quantitative portion of the risk assessment, the
UL derived below is intended to be protective against individual adverse effects. Furthermore,
although an obese population was assessed for the critical dataset, these obese individuals were
healthy. Based on the quality and completeness of the database in obese individuals; e.g., the
study designs which encompassed randomized, double-blind, placebo-controlled methods;
duration, and number of subjects enrolled, etc., these studies were judged to be superior to data
obtained from healthy (normal weight) individuals. Data from healthy normal humans were used
to support the findings in obese subjects; however, due to their short-term nature (typically 24hour duration), these studies were not used to derive a UL.
Basis for Data Selection
The majority of the randomized trials conducted as clinical studies have been investigations
using obese subjects. It is expected that obese subjects would not be more or less sensitive than
non-obese subjects to ephedrine-containing dietary supplements. Horton and Geissler (1991)
reported on the effect of ephedrine (30 mg) and ASA (300 mg) on the acute thermogenic
response to a liquid meal in lean and obese women. Analysis of subjective response to treatment
showed that fewer adverse effects to the drug treatments were noted in the obese subjects
compared to the lean group. In a later study from the same authors (Geissler, 1993; Horton and
Geissler, 1996), these findings were not confirmed and no such difference in sensitivity was
Council for Responsible Nutrition
December 19, 2000
152
observed. No significant correlations were found in either the lean or obese individuals with
respect to the number of adverse effects. Based on the more recent studies from the same
investigators, there is no compelling evidence that any differences in sensitivity to ephedrine
would be expected in obese individuals vs. the general population. With respect to the animal
literature, Chappel et al. (1959) investigated the cardiotoxic actions of certain sympathomimetic
agents into rats. Sublethal doses of sympathomimetic agents were injected into the rats, and in
the course of study, a difference was noted among older, heavier rats. The authors of this study
speculated that the effects of isoproterenol were correlated with weight and stated that they
believed that more severe cardiac lesions in their animal model were more common in older,
heavier rats. This study design in the animal did not assess the effects of weight on sensitivity to
stimulants.
Normal Healthy Individuals
Nine studies investigated the effects of ephedrine intake in normal healthy individuals (Bye et al.,
1974; Drew et al., 1978; Kuitunen et al., 1984; Astrup et al., 1992; Astrup and Toubro, 1993;
Liu et al., 1995; White et al., 1997; Gurley et al., 1998a; Shannon et al., 1999). Ephedrine
exposures involved oral administration over a short duration such as 24 hours. No long-term
studies were identified in a population of generally healthy (normal weight) individuals. The
range of total doses within these 9 studies was from 10 to 150 mg/day, given at a frequency of 1
to 3 times/day to achieve a daily maximum specified. Table 6.2-1 further classifies the studies
according to the strengths and weaknesses of the study design, which allow for assessment of the
utility of these studies in the determination of a UL.
Based on the strengths and weaknesses of the study design and findings in a healthy population,
it was concluded that limitations due to study duration (<24 hours) precluded this population in
the assessment of the UL. Nevertheless, these data are used to support the database in obese but
healthy subjects.
Normal Healthy Individuals Under Conditions of Physiological Stress
Five studies in healthy normal individuals investigated the effects of exercise/physical
parameters together with ephedrine use (Sidney and Lefcoe, 1977; Strömberg et al., 1992;
Vanakoski et al., 1993; Bell et al., 1998; Bell and Jacobs, 1999). The range of total doses within
these 5 studies was from 24 to 81 mg/day together with exercise, or some physical parameters,
over a short duration of exposure (typically 24 hours). Table 6.2-2 further classifies the studies
Council for Responsible Nutrition
December 19, 2000
153
according to the strengths and weaknesses of the study design, which allow for assessment of the
utility of these studies in the determination of a UL.
Based on the strengths and weaknesses of the study design and findings in a physically-fit healthy
population tested with ephedrine and exercise/physical exertion, it was concluded that limitations
due to study duration (<24 hours) precluded this population in the assessment of the UL.
Nevertheless, these data are used to support the safety of ephedrine/ephedra use in physically-fit
individuals together with physical exertion such as exercise. Furthermore, these data are used to
support the database in obese but healthy subjects.
Obese Individuals
Twenty studies in obese, but reportedly healthy individuals, investigated the effects of
ephedrine/ephedra intake (Astrup et al., 1985, 1992; Pasquali et al., 1985, 1987; Krieger et al.,
1990; Pasquali et al., 1992; Daly et al., 1993; Molnár, 1993; Toubro et al., 1993a,b; Breum et al.,
1994; Buemann et al., 1994; Kaats and Adelman, 1994; Moheb et al., 1998; Waluga et al., 1998;
Huber, 1999, 2000; Nasser et al., 1999; Boozer et al., 2000; Molnár et al., 2000). Ephedrine/
ephedra exposures involved oral administration over durations from 10 days to 26 months. The
range of total doses within these studies was from 50 to 150 mg/day, given at frequencies of 1 to
3 times/day to achieve the daily maximum specified. Table 6.2-3 further classifies the studies
according to strengths and weaknesses of the study design, which allow for assessment of the
utility of these studies in the determination of a UL.
Based on the strengths of the study design, duration of study, number of subjects enrolled and
endpoints evaluated, studies conducted in obese individuals were determined to be of sufficient
quality and quantity for inclusion as the critical dataset for the determination of the UL.
Asthmatic Individuals
Oral ephedrine was previously used as a bronchodilator in mild asthmatic individuals in which
there is a long history of safe use; however, ephedrine is no longer the drug of choice since more
selective 2 - agonists are available. Of the literature, only 4 studies are highlighted on asthmatic
patients which are included for completeness; however, use of this population for any
generalization to a healthy population is not intended since asthma is a condition which typically
requires the use of other concomitant drugs to manage the disease.
Council for Responsible Nutrition
December 19, 2000
154
Hypertensive Individuals
Ingerslev et al. (1997) investigated the effect of an ephedrine+caffeine combination at 60/600
mg/day on blood pressure in normotensive and treated hypertensive, obese patients after 6 weeks
of treatment. The hypertensive subjects investigated in this study were treated with
pharmacological agents which were well monitored by their original physicians. Even though it
is recommended that ephedrine/ephedra not be used in hypertensive individuals, these data
demonstrate that serious adverse events do not arise from intake of 60 mg ephedrine together
with 600 mg caffeine/day in hypertensive individuals, with or without pharmacological
treatment.
Smoking Population
Group characteristics have important implications for the interpretation of clinical trial studies.
As such, smoking status was evaluated in a study conducted by Norregaard et al. (1996) on the
effects of ephedrine and caffeine on a population of 225 heavy smokers who wanted to quit
smoking. This was the only published report identified in the literature that evaluated the effects
of ephedrine in a population of smokers, albeit these smokers were trying to quit. Most clinical
trials applied strict exclusion criteria which included exclusion of smokers.
Adverse Event Reports
The available reported adverse experiences that were compiled through the FDA SN/AEMS for
dietary supplements containing ephedrine alkaloids were evaluated as an integral component of
the safety assessment of ephedrine and ephedrine alkaloids. Of the 1,173 AERs reported, 98% of
the AERs did not contain complete information and only 10% (121 selected cases) were
considered to contain sufficient information (such as, quantity of ephedrine alkaloids consumed,
pre-existing conditions or concomitant products) for qualitative scientific analysis. These 121
represent anecdotal case reports that suggested an association but not causality. Nervous system
and cardiovascular effects were the principal reported events which consisted of 35% and 28% of
these AERs, respectively and were anticipated pharmacological/physiological effects to
ephedrine intake. After extensive examination of the database, it was not possible to
conclusively determine if there were any unexpected toxicological effects due to the ephedrine
alkaloids contained in the dietary supplements based solely on the information presented in the
AERs. Rather, only a qualitative evaluation of trends in the database of AERs could be
conducted. These data were not included in the critical dataset that was used to establish the UL.
Council for Responsible Nutrition
December 19, 2000
155
6.2
Identification of a NOAEL and a LOAEL
Identification of a NOAEL and a LOAEL. Based on the available scientific data, a NOAEL of
90 mg/day of ephedrine alkaloids in ephedra and a LOAEL of 150 mg/day were identified based
on a critical evaluation of clinical studies in obese individuals, in particular 8 clinical studies
(Pasquali et al., 1985; Krieger et al., 1990; Astrup et al., 1992; Quaade et al., 1992; Daly et al.,
1993; Toubro et al., 1993a,b; Nasser et al., 1999; Boozer et al., 2000; Molnár et al., 2000).
These studies reported no statistically significant increase in frequency of events up to 90
mg/day. In the investigation by Astrup et al. (1992), a statistical difference between frequency of
events was observed only at Week 4 (duration of study was 24 weeks) with 60 mg ephedrine/day.
The effects which were reported in any of these studies were not serious and did not persist, even
at durations of study of 8 weeks up to 26 months. No statistically significant differences between
75 mg ephedrine/day and placebo were observed in heart rate or blood pressure in these studies.
In the recent Columbia/Harvard study by Boozer et al. (2000), blood pressure was transiently
increased and heart rate persistently increased; however, cardiac arrhythmias were not reported to
occur in groups given 90 mg ephedrine alkaloids/day versus placebo. Self-reported symptoms
were similar among supplement and placebo groups. Because these studies meet all the predetermined criteria specified in Data Selection and are consistent with evidence from the other 11
clinical studies, they were used to identify the NOAEL of 90 mg/day for ephedrine alkaloids.
Basis for the Identification of a NOAEL
Twenty studies in obese, but otherwise reportedly healthy individuals, investigated the effects of
ephedrine/ephedra intake (Astrup et al., 1985, 1992; Pasquali et al., 1985, 1987, 1992; Krieger et
al., 1990; Daly et al., 1993; Molnár, 1993; Toubro et al., 1993a,b; Breum et al., 1994; Buemann
et al., 1994; Kaats and Adelman, 1994; Moheb et al., 1998; Waluga et al., 1998; Huber, 1999,
2000; Nasser et al., 1999; Boozer et al., 2000; Molnár et al., 2000). Ephedrine/ ephedra
exposures involved oral administration over durations from 10 days to 26 months. The range of
total daily doses within these studies was from 50 to 150 mg/day, given at frequencies of 1 to 3
times/day to achieve the daily maximum specified. These studies were considered in the
identification of a NOAEL, and taken together they collectively contribute to the determination
of the UL.
Based on the strength of study design, however, only 9 of these studies were determined to be of
sufficient quality and extent and are given the greatest weight. These studies by Pasquali et al.
(1985), Krieger et al. (1990), Astrup et al. (1992), Quaade et al. (1992), Daly et al. (1993),
Toubro et al. (1993a,b), Nasser et al. (1999), Boozer et al. (2000), and Molnár et al. (2000) were
Council for Responsible Nutrition
December 19, 2000
156
conducted using a randomized, double-blind, placebo-controlled design. Ephedrine/ephedra was
taken daily for at least 8 weeks. Heart rate, blood pressure, adverse effects, frequency of adverse
effects and related tolerability parameters were monitored. Pasquali et al. (1985), Krieger et al.
(1990), Daly et al. (1993), and Nasser et al. (1999) reported no statistically significant increase in
frequency of events at 75 mg/day. Astrup et al. (1992), Quaade et al. (1992), and Toubro et al.
(1993a) reported a statistically significant increase in frequency of events at 60 mg/day only up to
Week 4. These events did not persist, even at durations of exposure of 24 weeks and 50 weeks in
the follow-up study. In Molnár et al. (2000), treatment up to 60 mg/day in adolescents (18
years old) showed no change in frequency of side effects, heart rate or blood pressure and clinical
chemistry measurements such as hemoglobin, hematocrit, white blood cell and platelet count,
ASAT, LDH etc; these results support the selection of 90 mg/day as the NOAEL for an adult
population but are not intended in this risk assessment to support use in persons aged 18 years
old or younger. In all studies, no statistically significant differences at doses up to 75 mg/day and
placebo were observed in heart rate or blood pressure in these studies. In the recent
Columbia/Harvard study on ephedra by Boozer et al. (2000), blood pressure was transiently
increased and heart rate persistently increased; however, cardiac arrhythmias were not reported to
occur in subjects given 90 mg ephedrine alkaloids/day versus placebo. Self-reported symptoms
were similar among supplement and placebo groups.
The selection of 90 mg/day is an appropriate value for a NOAEL for ephedra in light of the
evidence of no significant increases in frequency of adverse effects or changes in heart rate or
blood pressure at or below this level leading to cardiac arrhythmias. The NOAEL is based on
strong scientific findings reported by the Columbia/Harvard study by Boozer et al. (2000) and
supported by the findings on ephedrine from Pasquali et al. (1985), Krieger et al. (1990), Astrup
et al. (1992), Quaade et al. (1992), Daly et al. (1993), Toubro et al. (1993a,b), Nasser et al.
(1999) and Molnár et al. (2000). Given the quality of the long-term investigation of ephedrine
alkaloids in an herbal ephedra supplement by Boozer et al. (2000), this study represents the
pivotal clinical study in the safety evaluation of ephedra. The NOAEL does not encompass the
dose level 150 mg/day, which was used in several studies, even though one could argue that the
effects reported may not be much more serious than those reported at lower doses. However due
to study weaknesses (e.g., small numbers of subjects), and recognizing the dose response
principle with increases of effects, a NOAEL of 150 mg/day was not considered to be appropriate
(see next section on LOAEL).
Council for Responsible Nutrition
December 19, 2000
157
Basis for the Identification of a LOAEL
A LOAEL of 150 mg/day of ephedrine was identified based on a critical evaluation of clinical
studies in obese individuals, in particular the 9 clinical studies outlined above (Pasquali et al.,
1985; Krieger et al., 1990; Astrup et al., 1992; Quaade et al., 1992; Daly et al., 1993; Toubro et
al., 1993a,b; Nasser et al., 1999; Boozer et al., 2000; Molnár et al., 2000). The range of total
doses administered per day ranged up to 150 mg/day, given at frequencies of 1 to 3 times/day to
achieve the daily maximum specified. Of these studies, Pasquali et al.(1985), Daly et al. (1993),
and Krieger et al. (1990) investigated the effects of ephedrine at 150 mg/day. Krieger et al.
(1990) reported no statistically significant differences in the frequency of adverse effects between
treatment and placebo groups. Pasquali et al. (1985) reported that effects such as agitation,
insomnia, headache, weakness, palpitation, giddiness, tremor, and constipation were present in
the high-dose group compared to the lower dose (75 mg/day) or placebo group, which
disappeared with time. Daly et al. (1993) reported that with respect to effects, 3 of 8 subjects
complained of transient dry mouth, while none did with placebo; however, there was no
significant difference in the frequency of any effects and no adverse effect persisted throughout
the study. Although a relatively good safety profile was observed in these investigations, these
studies did show statistical differences in frequency of clinical signs between 150 mg/day and
placebo. It is important to note that the effects which were reported were expected, anticipated
physiological responses to ephedrine. No studies reported any serious, unanticipated toxicities.
Furthermore, the findings in studies conducted with 150 mg/day were considered in the
evaluation of the UF and support the value selected for the NOAEL.
6.3
Uncertainty Assessment
Uncertainty factors have been used for over 30 years for the determination of a safe level of
human exposure to chemicals based on the results of studies in experimental animals and/or
humans (Renwick, 1995). In principle, the primary aim of safety studies is to recognize the
potential hazards associated with a particular chemical and to identify a dose or intake that is
without any observable effect. Safety factors or uncertainty factors (UF) are applied to convert
the NOAEL in a group of animals into a level of human intake that is considered to be without
significant health risk when consumed daily over a lifetime. The UF allocated are dependent on
the nature and extent of the toxicity database. A UF of 100 to account for interspecies and
interindividual variation is typically used for most databases; however, a flexible approach using
alternate factors allows use of data in particular areas of uncertainty to address and contribute to a
relevant compound-specific UF. A UF of 100 is typical for extrapolation from animal data when
applying the Acceptable Daily Intake (ADI) method to food additives.
Council for Responsible Nutrition
December 19, 2000
158
The NOAEL from an animal study is usually divided by a UF of 10 to convert the group
threshold in animals to a group threshold in humans. In cases when adequate human data are
available, as is the case for ephedra/ephedrine alkaloids, animal data are not used to derive a UL,
thus eliminating the need for this 10-fold factor.
Another default UF of 10 is often applied to account for individual variability among humans.
This UF is to allow for the possibility that “sensitive” human subjects may be up to 10 times
more sensitive to the external dose than the population average. However, subdivision of this
10-fold UF is possible, and in practice any value between 1 and 10 could be selected with proper
justification.
Further consideration of subdivision of the 10-fold UF may involve separation of the variability
in response due to kinetics and that due to dynamics. The kinetic factor is to allow for individual
differences between the external dose and the concentration delivered. The greatest
interindividual variability in area under the curve (AUC) is shown by compounds which have
low oral bioavailabilities (Hellriegel et al., 1996; Lindahl et al., 1996). For well-absorbed
compounds with low oral bioavailability, variability arises from differences in intestinal and
hepatic first-pass metabolism. Ephedrine has high oral bioavailability and also is well-absorbed,
minimizing the need to consider a kinetic factor.
Renwick and Lazarus (1998) performed an analysis of the default UF for possible interindividual
differences among humans with reference to the fate of the chemical in the body and target organ
sensitivity. This analysis considered an extensive database of literature which identified data on
in vivo concentration-effect relationships. Literature giving kinetic data was selected on the basis
of the quality and/or size of the study, and the physiological/metabolic process(es) determining
the kinetic parameters. Reports with dynamic data were selected on the basis of the adequate
separation of variability due to kinetics and dynamics. In analysis of these studies, some of the
studies contained small numbers of subjects (n<10). The standard deviation in these studies was
reported to be comparable to that for a larger group providing that the subjects studied were
representative of the population (Renwick and Lazarus, 1998).
Unfortunately, in the ephedrine database, no investigations of multiple dose pharmacokinetics
were available for review. Data from single-dose studies do not provide an adequate
understanding of human variability; however, a default UF of 10 would be unjustified based on
the known pharmacokinetic properties of ephedrine. Ephedrine is rapidly and completely
absorbed (100%) after oral administration within 2 to 2.5 hours (Wilkinson and Beckett,
Council for Responsible Nutrition
December 19, 2000
159
1968a,b; Welling et al., 1971). Up to 95% of an oral dose may be excreted in the urine within 24
hours, 55 to 75% as unchanged drug and the rest as metabolites (Dollery, 1991a). The mean T1/2
life is 6 hours, with a range of 3 to 11 hours. Ephedrine is rapidly and extensively distributed
throughout the body, with distribution to the liver, lungs, kidneys, spleen, and brain giving a
consistent apparent volume of distribution of 122 to 320 litres. A single 22 mg dose of ephedrine
hydrochloride has been reported to give a maximum plasma concentration in the range of 45 to
140 g/L for which bronchodilation has been observed with plasma concentrations from 20 to 80
g/L (Dollery, 1991a). Ingestion of 375 mg of ma huang containing 19.4 mg of ephedrine
resulted in blood concentrations of 81 ng/ml, which were similar to peak ephedrine levels
observed after the administration of an equivalent amount of pure ephedrine (White et al., 1997).
Vanakoski et al. (1993) gave 50 mg of ephedrine orally to 6 healthy, 21-year old women. The
mean peak plasma concentration was measured at 168 ng/ml at 127 minutes after ingestion.
These findings collectively are consistent with pharmacokinetic studies originally conducted by
Wilkinson and Beckett in 1968. No change in disposition kinetics after repeated dosing has been
observed, (Hughes et al., 1985).
In addition to a good understanding of the pharmacokinetic profile of ephedrine, further
consideration of the uncertainty factors may be appropriate in light of the intended users and use
patterns. This assessment recognizes that ephedra is not intended for use in infants, children,
adolescents less than 18 years of age, pregnant or lactating women. Rather, this assessment
provides an exposure level for a generally healthy adult population for which a daily level is
unlikely to pose a risk of adverse health effects. For individuals who are susceptible to the
adverse effects of excess ephedrine intake, ephedra intake is contraindicated, such as patients
with coronary thrombosis, diabetes, glaucoma, heart disease, hypertension, thyroid disease,
impaired circulation of the cerebrum, pheochromocytoma, or enlarged prostate (Dollery, 1991a;
Hoffman and Lefkowitz, 1996) and patients with renal impairment. The importance of these
contraindicated individuals has been recognized by the exclusion criteria used in all the clinical
studies, including the pivotal ephedra study by Boozer et al. (2000). In addition, the critical
dataset involved durations of exposure of 8 weeks up to 26 months and represents clinical studies
with chronic exposure. Although a UL is determined for chronic daily exposure, it is expected
that ingestion of ephedra/ephedrine alkaloids will not be for the duration of a lifetime. With
periods of actual intake of limited duration appropriate uncertainty factors may be considered,
that are based on intended uses for less than lifetime exposure.
Based on the quality of the database of clinical studies, notably the recent study on ephedra by
Boozer et al. (2000), and on the justifications above relating to pharmacokinetics, intended users,
and duration of use, the factor for individual variability of 1 is an appropriate UF for ephedrine in
Council for Responsible Nutrition
December 19, 2000
160
ephedra preparations, and this factor is supported further by consideration of the database in
experimental animals. Labeling instructions should include: (1) consumers to check with their
healthcare provider about taking the product; (2) contraindicated populations; (3) directions that
include splitting the daily dose; (4) inclusion of a statement that the product is intended for shortterm use only; (5) use in persons aged 18 years or older; (6) preganant or lactating women; (7)
strong warnings; (8) post-market monitoring; and, (9) industry educational materials. These
contraindications and exclusions support the scientific rationale leading to the selection of the UF
of 1.
Because adequate human data are available, animal data were not used directly to derive a UL;
however, animal data are supportive of the findings in clinical studies. Consideration of animal
data shows that daily chronic exposure in male rats for 2 years at 9 mg/kg body weight/day
produced no adverse effects. The only finding at this dose was decreased body weight gain,
which did not reduce survival. Moreover, the decreases in body weight were likely the
physiological response to the intended pharmacological effect of ephedrine sulfate ingestion, as
decreased food consumption did not adequately account for the decrease in body weight. No
additional pathology and no changes in frequency of neoplastic or non-neoplastic lesions were
observed. A dose of 9 mg/kg/day is equivalent to a dose of 540 mg/day in a 60 kg adult. In
addition, these lifetime rodent studies showed that there were no long-term, cumulative effects
that may not be detected in clinical studies.
The animal studies also provide important information about relative potency between ephedrine
itself and ephedrine in ephedra. In 2 comparative studies between ephedra and ephedrine, extract
and herb, the LD50 value for ephedra extract was higher (i.e., less toxic) than ephedrine when
normalized based on ephedrine content, and the general symptoms observed were milder in
nature and time to death was longer compared to ephedrine. Similarly, the LD50 value for
ephedra herb was greater than the ephedra extract. These results highlight the conservative
assumption that ephedrine content can be used to characterize effects of ephedra since the
toxicity assessment of ephedrine shows that this approach overestimates the potential toxicity of
ephedra itself. Furthermore, since the effects of other ephedrine alkaloids are similar to
ephedrine but are somewhat weaker, use of ephedrine as a surrogate for ephedrine alkaloids
contributes to a conservative assessment. These considerations strengthen confidence in the
results on ephedra in the clinical study by Boozer et al. (2000), and are consistent with and
supportive of a UF of 1.
Therefore, based on the above considerations of the clinical database, pharmacokinetics of
ephedrine, use patterns, duration of expected use, and supportive animal studies, a UF of 1 is
Council for Responsible Nutrition
December 19, 2000
161
judged to be appropriate for ephedrine in ephedra. The UF of 1 is further supported through the
use of ephedra label instructions which would include statements that (1) consumers should
check with their healthcare provider about taking the product; (2) identify contraindicated
populations; (3) direct the consumer to split the daily dose into at least three parts, so that no
dose exceeds 30 mg; (4) the product is intended for use of not more than 6 months; (5) persons
younger than 18 years should not use the product; (6) pregnant and lactating women should not
use the product; and (7) provide information to facilitate post-market monitoring.
6.4
Upper Limit (UL)
According to the methodology used in the Upper Limit (UL) Model of the National Academy of
Sciences, and using the NOAEL of 90 mg/day from the clinical study on ephedra by Boozer et al.
(2000) and the UF of 1 as discussed above, the UL for the ephedrine alkaloids in ephedra is
calculated as:
UL=NOAEL=90 mg/day=90 mg/day
UF
1
The UL level for ephedrine alkaloids in ephedra, therefore, based on this risk assessment
approach, current data, and inclusion of strong label instructions is 90 mg/day for a generally
healthy population.
Council for Responsible Nutrition
December 19, 2000
162
Table 6.2-1
Frequency
Summary of Strengths and Weaknesses in Healthy Human Population Study Design
Total Dose
(mg/day)
Duration
Number of
Subjects (Gender)
Strengths in Study Design
Weaknesses in Study
Design
Reference
24 hours
-6 lean healthy
subjects (3 male and
3 female)
-double-blind, placebo-controlled
-heart rate and blood pressure were
assessed
-side effects were assessed
-evaluated effect of combination
products
-both genders were tested
-limited number of subjects
tested
-limited duration of study
Astrup et al.,
1991
24 hours
-12 healthy subjects
(6 male and 6
female)
-double-blind, placebo-controlled
-blood pressure and heart rate were
assessed
-side effects were assessed
-effect of combination products was
assessed
-adequate number of subjects tested
-both genders were tested
-limited duration of study
Astrup and
Toubro, 1993
Acute Human Studies
once/day
10 mg, 20 mg
ephedrine
once/day
combinations
(eph/caff)
-10 mg:200 mg
-20 mg:100 mg
-20 mg:200 mg
once/day
10, 20 and 40
mg ephedrine
once/day
100, 200, 400
mg caffeine
once/day
ephedrine +
caffeine :
10 mg:100 mg,
20 mg:100 mg,
20 mg:200 mg
Council for Responsible Nutrition
December 19, 2000
163
Table 6.2-1
Summary of Strengths and Weaknesses in Healthy Human Population Study Design
Frequency
Total Dose
(mg/day)
Duration
Number of
Subjects (Gender)
Strengths in Study Design
Weaknesses in Study
Design
Reference
once/day
25 mg
24 hours
-10 healthy subjects
(5 male and 5
female)
-double-blind, randomized, crossover
study with 4 phases
-baseline health status evaluated
-both genders tested
-4 different ephedrine preparations were
evaluated
-pharmacokinetic information provided
-side effects were assessed
-limited duration of study
Gurley et al.,
1998a
once/day
30 mg
24 hours
-9 health male
volunteers
-single-blind, cross-over design
-blood pressure and heart rate were
assessed
-information on side effects
not reported
-only males were evaluated
-limited duration of study
Liu et al.,
1995
once/day
30, 40 mg
24 hours
-43 healthy subjects;
22 females and 21
males
-double-blind, placebo-controlled
-blood pressure and heart rate were
assessed
-number of subjects tested was adequate
-both genders tested
-information on side effects
not reported
-limited duration of study
Kuitunen et
al., 1984
twice daily:
8 hours
apart
38.8 mg
24 hours
-12 healthy
nonsmoking
subjects (6 male/6
female)
-cross-over design
-blood pressure and heart rate assessed
-side effects were assessed
-both genders tested
-adequate number of subjects tested
-test article administration was
confirmed
-baseline cardiovascular studies
conducted
-study controlled for smoking, caffeine
intake, etc.
-not placebo-controlled
-not blinded
-limited duration of study
White et al.,
1997
Council for Responsible Nutrition
December 19, 2000
164
Table 6.2-1
Summary of Strengths and Weaknesses in Healthy Human Population Study Design
Frequency
Total Dose
(mg/day)
Duration
Number of
Subjects (Gender)
Strengths in Study Design
Weaknesses in Study
Design
Reference
once/day
50 mg
24 hours
-12 healthy subjects
(7 male/5 female)
-double blind
-blood pressure and heart rate assessed
-information on side effects
not reported
-limited duration of study
Bye et al.,
1974
once/day
60, 90 mg
24 hours
-4 healthy subjects
-double-blind, randomized, placebocontrol, 2-period crossover
-blood pressure assessed
-limited number of subjects
studied
-limited information
-limited duration of study
Drew et al.,
1978
3 times/
day
150 mg
24 hours
-10 healthy subjects
(6 male and 4
female)
-blood pressure and heart rate assessed
-side effects were assessed
-all subjects underwent a thorough
clinical examination, ECG, admission
urinalysis and blood work
-adequate number of subjects studied
-both genders were studied
-limited duration of study
Shannon et
al., 1999
Council for Responsible Nutrition
December 19, 2000
165
Table 6.2-2
Frequency
Summary of Strengths and Weaknesses Ephedrine Intake Together with Physical Parameters in
Healthy Normal Individuals
Total Dose
(mg/day)
Duration
Number of
Subjects (Gender)
Strengths in Study Design
Weaknesses in Study
Design
Reference
Normal Healthy Individuals with Ephedrine Intake and Exercise/Physical Parameters
single
administration
- ephedrine
(81 mg)
-caffeine (405
mg)
-combination
(ephedrine 81
mg + caffeine
405 mg)
24 hours
-8 healthy male
subjects
-repeated measures, double-blind
design
-studied the effects of caffeine,
ephedrine and their combination on
time to exhaustion during highintensity exercise
-heart rate was assessed
-subjective exertion was assessed
-clinical signs assessed
-limited duration
Bell et al., 1998
-single
administration
-combination:
375 mg
caffeine and
75 mg of
ephedrine
24 hours
-9 healthy male
subjects
-double-blind design
-studied effects of combination on
run times in a warrior test
-runners were recruited: exclusion
criteria not reported
-heart rate assessed
-subjective exertion assessed
-clinical signs assessed
-limited duration
Bell and Jacobs,
1999
Council for Responsible Nutrition
December 19, 2000
166
Table 6.2-2
Summary of Strengths and Weaknesses Ephedrine Intake Together with Physical Parameters in
Healthy Normal Individuals
Frequency
Total Dose
(mg/day)
Duration
Number of
Subjects (Gender)
Strengths in Study Design
Weaknesses in Study
Design
Reference
single
administration
-50 mg
ephedrine
24 hours
-6 healthy 21 year
old women
-double-blind, placebo- controlled,
cross over
-subjects were ascertained to be
healthy based on a physical
examination, ECG
-all subjects except one took no
medication during the trial
-all were non-smokers
-heart rate, blood pressure, critical
flicker fusion test, Maddox wing test,
and visual analog scales relating to
mood and feelings of tiredness were
assessed
-limited duration
Vanakoski et al.,
1993
-single
administration
-50 mg
ephedrine
24 hours
-6 lean healthy
women
-double-blind, placebo- controlled,
cross over design
-subjects received single doses of 50
mg ephedrine in control session and
in an exercise session
-subjects were ascertained to be
healthy by a clinical examination,
including ECG and maximal exercise
test on treadmill
-heart rate, blood pressure, critical
flicker fusion test, Maddox wing test,
and visual analog scales relating to
mood and feelings of tiredness were
included
-limited duration
Strömberg et al.,
1992
Council for Responsible Nutrition
December 19, 2000
167
Table 6.2-2
Summary of Strengths and Weaknesses Ephedrine Intake Together with Physical Parameters in
Healthy Normal Individuals
Frequency
Total Dose
(mg/day)
Duration
Number of
Subjects (Gender)
Strengths in Study Design
Weaknesses in Study
Design
Reference
-single
administration
- 24 mg
ephedrine HCl
24 hours
-21 healthy males
-double-blind crossover design
-first day of testing, baseline data
were collected; second and third day
of test, a pill containing either 24 mg
of ephedrine or a lactose placebo was
administered orally approximately 60
minutes before testing
-heart rate was assessed
-blood pressure was assessed
-grip strength, endurance, anaerobic
capacity and muscle power were
assessed
-clinical signs assessed
-limited duration
-exclusion criteria not
reported
Sidney and
Lefcoe, 1977
Council for Responsible Nutrition
December 19, 2000
168
Table 6.2-3
Frequency
Summary of Strengths and Weaknesses in Study Design in Obese Individuals Taking Ephedrine
Total Dose
(mg/day)
Duration
Number of
Subjects (gender)
Strengths in Study Design
Weaknesses in Study
Design
Reference
6 months
Weeks 1-4: n=69
treated, n=68
control
-multi-center, randomized, doubleblind, placebo-controlled
-tested long-term safety of herbal
ephedra supplement containing
ephedrine
-subjects were assessed for health
-monitored for heart rate, blood
pressure, adverse effects, ECG, routine
lab tests, urinary screening, blood
testing for examination of possible
effects on kidney/liver
-published abstract
only, pending full
publication of findings:
however, information
obtained from
statements made at the
HHS meeting and the
NAASO meeting
provided additional
details on the rigor of
the study
Boozer et al.,
2000
-randomized, placebo-controlled,
double-blind study
tested safety of herbal ephedra
supplement containing ephedrine
-subjects were assessed for health
-monitored for heart rate, blood
pressure, adverse effects, metabolic
measurements
-nonpublished report
-not yet peer-reviewed
Huber et al.,
2000
Obese Subjects
three/day
90 mg ephedrine
+ 192 mg
caffeine
6 Month: n=46
treated, n=38
control
three/day
36 mg ephedrine
+ 120 mg
caffeine
72 mg ephedrine
+ 240 caffeine
6 weeks
26 enrolled: 15
completed
26 enrolled; 15
completed
21 enrolled: 14
Placebo
36 mg ephedrine
72 mg ephedrine
+ 300 mg
caffeine
Council for Responsible Nutrition
December 19, 2000
21 enrolled: 14
26 enrolled: 19
169
Table 6.2-3
Summary of Strengths and Weaknesses in Study Design in Obese Individuals Taking Ephedrine
Frequency
Total Dose
(mg/day)
Duration
Number of
Subjects (gender)
Strengths in Study Design
Weaknesses in Study
Design
Reference
three/day
30 mg
ephedrine/300
mg caffeine
60 mg
ephedrine/600
mg caffeine
20 weeks
Placebo:13
Mixture: 16 (low
/high dose group
not specified)
-graduated dose
-side effects monitored during
study and during withdrawal of
mixture
-heart rate and blood pressure
monitored
Dose assignments were
not indicated
Molnar et al.,
2000
-no control group
-prospective
clinical evaluation
-subjects and
investigators were
not blinded
Huber et al.,
1999
-hemoglobin, hematocrit, white blood
cell and platelet count, ASAT, LDH,
bilirubin, ALP, serum albumin and
creatinine evaluated
twice/day
48 mg/day
ephedra
24 mg ephedra
72 mg ephedra +
20 mg caffeine
6 months
N=20
N=44
N=58
-provide descriptive findings of
compiled individual cases evaluated
through a strictly monitored clinical
research protocol.
-exact amount of
ephedrine in the
ephedra products was
not reported
once/day
Group 1: placebo
Group II: 72 mg
ephedrine +240
caffeine
Council for Responsible Nutrition
December 19, 2000
8 weeks
67 obese subjects
(sex not specified)
-double-blind, placebo-controlled
-subjects were assessed for health
-monitored heart rate, blood pressure
and adverse effects
-abstract only: limited
information since full
publication not
available
Nasser et al.,
1999
170
Table 6.2-3
Summary of Strengths and Weaknesses in Study Design in Obese Individuals Taking Ephedrine
Frequency
Total Dose
(mg/day)
Duration
Number of
Subjects (gender)
Strengths in Study Design
Weaknesses in Study
Design
Reference
once/day
5 treatment
groups:
-ephedrine (50
mg)
-ephedrine (50
mg)+ caffeine
(150 mg
-ephedrine (50
mg) + ASA (330
mg)
-ephedrine (50
mg) + caffeine
(150 mg) + ASA
(330 mg)
-placebo
-12 weeks
-163 healthy
premenopausal
obese women
-placebo-controlled, double blind
design
-heart rate, blood pressure, clinical
signs were assessed
-energy expenditure, blood glucose,
triglycerides, total cholesterol, HDL,
DLL evaluated
-Exclusion criteria: hypertension, heart
disease, gastric ulcer or other serious
medical conditions
-study design stated
that symptoms were
evaluated and
monitored; however,
no information on
effects was reported
Moheb et al.,
1998
once/day
Group I: placebo
-10 days
Waluga et al.
1998
Group II: 50 mg
ephedrine +
400 caffeine
-randomized, double-blind, placebocontrolled
-subjects were assessed for health:
history and physical examination ,
laboratory tests, X-ray examination of
the chest, ECG, ultrasound of the
gastrointestinal system and kidneys
-monitored blood pressure, heart rate,
cardiac load, peripheral resistance
-no medication was allowed 2 weeks
prior to the study and participants were
asked to abstain from smoking and
drinking beverages with caffeine for at
least 24 hours before the study
-information on side
effects was not
reported in the study
once/day
-27 obese women
otherwise healthy,
n=9 per group.
-no cardiac
disturbances or
arterial
hypertension
before test
once/day
Group III: 50 mg
ephedrine + 400
mg caffeine +10
mg yohimbine
Council for Responsible Nutrition
December 19, 2000
171
Table 6.2-3
Summary of Strengths and Weaknesses in Study Design in Obese Individuals Taking Ephedrine
Frequency
Total Dose
(mg/day)
Duration
Number of
Subjects (gender)
Strengths in Study Design
Weaknesses in Study
Design
Reference
3/day
60 mg
ephedrine/600
mg caffeine
-15-week
study
-randomized, double-blind
-long duration
-monitored body weight, heart rate,
blood pressure, adverse effects
-enrolled sufficient number of subjects
-uneven sex
distribution
-general practice
setting (not controlled
clinical trial)
Breum et al.,
1994
2/day
30 mg
dexfenfluramine
n=50 in ephedrine/
caffeine group (39
female/11 male)
n=38 who
completed trial
n=53 in dexfen
group
3/day
60 mg
ephedrine/600
mg caffeine
-15-week
follow-up
period
-85 patients were
included in follow
up with the E+C
combination
-57 completed the
follow-up period
-frequency of side effects
-monitored body weight, heart rate,
blood pressure, adverse effects
frequency
not specified
dose information
not specified:
Herbal
formulation
-4-week
-placebo: 50
-treatment: 50
-randomized, double-blind, placebo,
crossover protocol
-dose information not
specified
-sex not specified
-limited information
reported
Kaats and
Adelman,
1994:abstract
Phase I:
3/day for
Week 1 Week 4
Phase I Study:
75 mg ephedrine
+ 150 mg
caffeine + 330
mg ASA
-4 weeks
-11 subjects (10
women/ 1man) in
ephedrine, caffeine,
ASA group
-randomized, double-blind, placebocontrolled
-frequency of side effects monitored
-consumption of coffee and other
caffeinated beverages were limited
-monitored weight, blood pressure,
heart rate
-uneven sex
distribution
Daly et al., 1993
Phase I:
3/day for
Week 5 Week 8
Phase I Study:
150 mg
ephedrine + 150
mg caffeine
+330 mg ASA
-4 weeks
-11 subjects 910
women/1 man) in
ephedrine, caffeine,
ASA group
Council for Responsible Nutrition
December 19, 2000
172
Table 6.2-3
Summary of Strengths and Weaknesses in Study Design in Obese Individuals Taking Ephedrine
Frequency
Total Dose
(mg/day)
Duration
Number of
Subjects (gender)
Strengths in Study Design
Weaknesses in Study
Design
Reference
Phase II:
3/day for 8
weeks
Phase II Study
Week 1: 75
ephedrine +150
caffeine+330
caffeine
Week 2-8:
150
ephedrine+150
caffeine + 330
ASA
-8 weeks
-8 women and 1
man in ephedrine,
caffeine and ASA
group
-cross-over design
-side effects were monitored
-uneven sex
distribution
-nonblinded
Daly et al., 1993
Phase III:
once/day
Phase III Study:
150 mg
ephedrine + 150
mg caffeine +
330 mg ASA
-7 to 26
months
-6 patients from
Phase II study
continued
-6 of 8 subjects who completed Phase
II, agreed to continued on treatment to
assess longer-term efficacy and safety
and were monitored for 7 to 26 months
-all subjects reported side effects such
as dry mouth or constipation.
-blood pressure and heart rate
remained normal
-it was concluded by study authors that
the treatment was well tolerated
-no significant adverse effects were
found in study subjects
3/day
150 mg
-2 weeks
-10 obese subjects
-randomized, double-blind, cross-over
design with placebo
-tolerability reported
Council for Responsible Nutrition
December 19, 2000
Daly et al. 1993
-sex not reported
Pasquali et al.,
1992
173
Table 6.2-3
Summary of Strengths and Weaknesses in Study Design in Obese Individuals Taking Ephedrine
Frequency
Total Dose
(mg/day)
Duration
Number of
Subjects (gender)
Strengths in Study Design
Weaknesses in Study
Design
Reference
3/day
EC: 60 mg
ephedrine + 600
mg caffeine
-24 weeks
-180 obese patients
were randomized
to 4 groups and
maintained on a
low energy diet
-randomized, double-blind, placebocontrolled
-enrolled large number of subjects
-monitored blood pressure, heart rate
and side effects
-ECG, fasting blood glucose, total
cholesterol, triglyceride, hematology,
biochemical screening, analysis of
urine were evaluated at Weeks 12 and
24
-measured hematology, sodium,
potassium, bilirubin, liver enzymes,
creatinine, uric acid and urine analyses
were without any significant
differences.
-uneven sex
distribution
Astrup et al.,
1992; Quaade et
al., 1992
-monitored blood pressure, heart rate
and side effects
-nonblinded, not
placebo-controlled;
however, a follow-up
study
Toubro et al.,
1993b
E:60 mg
ephedrine
EC: 45(39 female/6
male)
E:45 (40 female/5
male)
C:45 (42 female/3
male)
Placebo: 45 (34/11
male)
C:600 mg
caffeine
Placebo
3/day
60 mg ephedrine
+ 600 mg
caffeine
Council for Responsible Nutrition
December 19, 2000
-24-week
follow up
-127 patients from
original study: all
patients received
same treatment
-n=30 in E+C
group
-n=31 in E group
-sex not specified
174
Table 6.2-3
Summary of Strengths and Weaknesses in Study Design in Obese Individuals Taking Ephedrine
Frequency
Total Dose
(mg/day)
Duration
Number of
Subjects (gender)
Strengths in Study Design
3/day
75 mg ephedrine
+150 caffeine
+300 ASA
Week 1-4
(75 mg
ephedrine)
Week 5-8
(150 mg
ephedrine)
n=11 obese
volunteers in the
ephedrine, caffeine
and ASA group
(sex not specified)
-randomized, double-blind, placebocontrolled
-screened for history, physical
examination, laboratory studies
-frequency of side effects monitored
-heart rate, blood pressure,
fasting plasma glucose, insulin, total or
HDL cholesterol concentration
measured
150 mg
ephedrine +150
caffeine +300
ASA
n=13 placebo
3/day
60 mg
-3 months
-5 obese women
-monitored side effects, blood pressure
and heart rate
-monitored plasma sodium, glucose,
serum thyroxine, tri-iodothyronine,
TSH and levels of catecholamines
3/day
Group I: placebo
-3 months
Group I: 16 (12
women/4 men)
Group II: 13 (9
women/4 men)
Group III: 17 (11
women/6 men)
-double-blind, placebo-controlled
-monitored side effects, heart rate, and
blood pressure
-consecutive patients which were not
pre-screened
-1 month
-10 low-energy
adapted obese
women
-randomized, double-blind, cross-over
-monitored side effects, heart rate and
blood pressure
Group II: 75 mg
Group III: 150
mg
3/day
150 mg
Council for Responsible Nutrition
December 19, 2000
Weaknesses in Study
Design
Reference
Krieger et al.,
1990
-nonblinded
-not placebo-controlled
-one sex tested
Astrup et al.,
1985
Pasquali et al.,
1985
-one sex tested
Pasquali et al.,
1987
175
7.0
REFERENCES
AHPA, 2000. Ephedra Survey Results: 1995-1999. Survey Administered & Results Compiled
by: Arthur Andersen LLP prepared for The American Herbal Products Association. April
28, 2000.
Anastario, G.D., and Haston, P. 1992. Fetal tachycardia associated with maternal use of
pseudoephedrine and OTC oral decongestant. J Am Board Fam Pract 5:527-528.
Assismos, D.G., Langenstroer, P., Leinbach, R.F., Mandel, N.S., Stern, J. M., and Holmes, R.P.
1999. Guaifenesin- and ephedrine-induced stones. J Endourol 13(9):665-667.
Astrup, A., and Tubro, S. 1993. Thermogenic, metabolic, and cardiovascular responses to
ephedrine and caffeine in man. Int J Obesity Related Metabol Disord 17(Suppl. 1):S41S43.
Astrup, A., Breum, L., Tubro, S., Hein, P., and Quaade, F. 1992. The effect and safety of an
ephedrine/caffeine compound compared to ephedrine, caffeine and placebo in obese
subjects on an energy restricted diet. A double blind trial. Int J Obesity Related Metabol
Disord 16(4):269-277.
Astrup, A., Lundsgaard, C., Madsen, J., and Christensen, N.J. 1985. Enhanced thermogenic
responsiveness during chronic ephedrine treatment in man. Am J Clin Nutr 42(1):83-94.
Astrup, A., Toubro, S., Cannon, S., Hein, P., and Madsen, J. 1991. Thermogenic synergism
between ephedrine and caffeine in healthy volunteers: A double-blind, placebocontrolled study. Metab Clin Exper 40(3):323-329.
Aswal, B.S., Bhakuni, D.S., Goel, A.K., Kar, K., and Mehrotra, B.N. 1984. Screening of Indian
plants for biological activity. Part XI. Indian J Exper Biol 22:487-504.
Axelrod, J. 1953. Studies on sympathomimetic amines: I. The biotransformation and
physiological disposition of l-ephedrine and l-norephedrine. J Pharmacol Exper
Therapeut 109(1):62-73.
Backer, R., Tautman, D., Lowry, S., Harvey, C.M., and Poklis, A. 1997. Fatal ephedrine
intoxication. J Forensic Sci 42(1):157-159.
Bale, J.F., Fountain, M.T., and Shaddy, R. 1984. Phenylpropanolamine-associated CNS
complications in children and adolescents. Am J Dis Child 138(7):683-685.
Baselt, R.C. 1982a. Ephedra. In: Baselt, R.C. (Ed.). Disposition of Toxic Drugs and
Chemicals in Man (2nd Ed.). Chemical Toxicology Institute, Foster City, CA.
Council for Responsible Nutrition
December 19, 2000
176
Baselt, R.C. 1982b. Caffeine. In: Baselt, R.C. (Ed.). Drugs and Chemicals in Man (2nd Ed.).
Chemical Toxicology Institute, Foster City, CA, pp. 108-111.
Battig, K. 1993. Acute and chronic cardiovascular and behavioural effects of caffeine, aspirin
and ephedrine. Int J Obesity Related Metabol Disord 17(Suppl. 1):S61-S64.
Beck, R.A., Mercado, D.L., Seguin, S.M., Andrade, W.P., and Cushner, H.M. 1992.
Cardiovascular effects of pseudephedrine in medically controlled hypertensive patients.
Arch Intern Med 152(6):1242-1245.
Bell, D.G., and Jacob, I. 1999. Combined caffeine and ephedrine ingestion improves run times
of Canadian Forces warrior test. Aviat Space Environ Med 70(4):325-329.
Bell, D.G., Jacobs, I., and Zamecnik, J. 1998. Effects of caffeine, ephedrine and their
combination on time to exhaustion during high-intensity exercise. Eur J Appl Physiol
Occup Physiol 77(5):427-433.
Betz, J.M., Gay, M.L., Mossoba, M.M., Adams, S., and Portz, B.S. 1997. Chiral gas
chromatographic determination of ephedrine-type alkaloids in dietary supplements
containing Ma Huang. J AOAC Int 80(2):303-315.
Bierman, C.W., Pierson, W.E., and Shapiro, G.G. 1975. Exercise-induced asthma
pharmacological assessment of single drugs and drug combinations. J Am Med Assoc
234(3):295-298.
Blanc, P.D., Kuschner, W.G., Katz, P.P., Smith, S., and Yelin, E.H. 1997. Use of herbal
products, coffee or black tea, and over-the-counter medications as self-treatments among
adults with asthma. J Allergy Clin Immunol 100(6, Prt. 1):789-791.
Blau, J.J. 1998. Ephedrine nephrolithiasis associated with chronic ephedrine abuse. J Urol
160(3, Prt. 1):825.
Blumenthal, M., and Busse, W.R., (Eds.) 1998. Ephedra. In: Blumenthal, M., and Busse, W.R.,
(Eds.). (Translated by) Klein, S., and Rister, R.S. Complete German Commission E
Monographs: Therapeutic Guide to Herbal Medicines. American Botanical Council,
Austin, TX / Integrative Medicine Communications, Boston, MA, pp. 125-126, 414-416,
475-476.
Boozer, C.N., Daly, P.A., Blanchard, D., Nasser, J.A., Solomon, J.L., and Homel, P. 2000.
Herbal ephedra/caffeine for weight loss: A 6-month safety and efficacy trial. Abstract
presented at NAASO – North American Association for the Study of Obesity Annual
Meeting, October 29-November 2, 2000.
Boston, L.N. 1928. Dysuria following ephedrine therapy. Med Times 56:94-95.
Council for Responsible Nutrition
December 19, 2000
177
Bowyer, J.F., Newport, G.D., Slikker, W.Jr., Gough, B., Gerguson, S.A., and Tor-Agbidye, J.
2000. An evaluation of l-ephedrine neutortoxicity with respect to hyperthermia and
caudate/putamen microdialysate levels of ephedrine, dopamine, serotonine, and
glutamate. Toxicol Sci 55(1):133-142.
Bradley, J.G. 1991. Nonprescription drugs and hypertension: Which ones affect blood
pressure? Postgrad Med 89(6):195-197&201-202.
Breum, L., Pedersen, J.K., Ahlstrom, F., and Frimodt-Moller, J. 1994. Comparison of an
ephedrine/caffeine combination and dexfenfluramine in the treatment of obesity: A
double-blind, multi-centre trial in general practice. Int J Obesity Related Metabol Disord
18:99-103.
Brown, J.M., Ryder, D., and Branch, R.A. 1991. A pharmacodynamic interaction between
caffeine and phenylpropanolamine. Clin Pharmacol Therapeut 50(4):363-371.
Bruneton, J. 1996. Phenethylamines. In: Bruneton, J. Pharmacognosy, Phytochemistry,
Medicinal Plants. Lavoisier Pub., Paris, France, Secaucus, NY, pp. 711-715.
Bruno, A., Nolte, K.B., and Chapin, J. 1993. Stroke associated with ephedrine use. Neurology
43(7):1313-1316.
Buemann, B., Markmann, P., Christensen, J.J., and Astrup, A. 1994. The effect of ephedrine
plus caffeine on plasma lipids and lipoproteins during a 4.2 MJ/day diet. Int J Obesity
Related Metabol Disord 18(5):329-332.
Burkhart, K.K. 1992. Intravenous propranolol reverses hypertension after sympathomimetic
overdose: Two case reports. J Toxicol (Clin Toxicol) 30(1):109-114.
Bye, C., Dewsbury, D., and Peck, A.W. 1974. Effects on the human central nervous system of
the two isomers of ephedrine and triprolidine and their interaction. Br J Clin Pharmacol
1(1):71-78.
Capwell, R.R. 1995. Ephedrine-induced mania from an herbal diet supplement. Am J Psychiat
152(4):647.
Catlin, D.H., and Hatton, C.K. 1991. Use and abuse of anabolic and other drugs for athletic
enhancement. Adv Int Med 36:399-424.
Cetaruk, E.W., and Aaron, C.K. 1994. Hazards of nonprescription medications. Emerg Med
Clin N Am 12(2):483-510.
Chance, M.R.A. 1946. Aggregation as a factor influencing the toxicity of sympathomimetic
amines in mice. J Pharmacol Exper Therapeut 87:214-219.
Council for Responsible Nutrition
December 19, 2000
178
Chappel, C.I., Rona, G., Balazs, T., and, Gaudry, R. 1959. Comparison of cardiotoxic actions of
certain sympathomimetic amines. Cdn J Biochem Physiol 37:35-42.
Chau, S.S., and Benrimoj, S.I. 1988. Non-prescription sympathomimetic agents and
hypertension. Med Toxicol 3:387-417.
Chen, K.K. 1925a. The acute toxicity of ephedrine. Proc Soc Exper Biol Med 22(7):404-405.
Chen, K.K. 1925b. The effect of repeated administration of ephedrine. Proc Soc Exper Biol
Med 22(8):568-570.
Chen, K.K. 1926a. The acute toxicity of ephedrine. J Pharmacol Exper Therapeut 27:61-76.
Chen, K.K. 1926b. The effect of repeated administration of ephedrine. J Pharmacol Exper
Therapeut 27:77-86.
Chen, K.K., and Schmidt, C.F. 1930. Ephedrine and related substances. Medicine Vol. 9:1117.
Chen, K.K., Wu, C., , and Henriksen, E. 1929a. Relationship between the pharmacological
action and the chemical constitution and configuration of the optical isomers of ephedrine
and related compounds. J Pharmacol Exper Therapeut 36:363-400.
Chen, K.K., Wu, C.-K., and Henriksen, E. 1929b. Ephedrine homologs and isomers:
Relationship between their pharmacological action and their chemical constitution and
stereoisomerism. Proc Soc Exper Biol Med 26(4):348.
Clarkson, P.M., and Thompson H.S. 1997. Drugs and sport. Research findings and limitations.
Sports Med (Auckland) 24(6):366-384.
Clovis,W.L. 1993. Mania and cough syrup. J Clin Psychiat 54(5):200.
Cockings, J.G., and Brown, M. 1997. Ephedrine abuse causing acute myocardial infarction.
Med J Austral 167(4):199-200.
Costello, J.F., May, C.S., Paterson, J.W., and Pickup, M.E. 1975. Pharmacokinetics of
ephedrine in asthmatics receiving acute and chronic treatment. Br J Clin Pharmacol
2(2):180-181.
Cupp, M.J. 1999. Herbal remedies: Adverse effects and drug interactions. Am Family
Physician 59(5):1239-1245.
Dalton, R. 1990. Mixed bipolar disorder precipitated by pseudoephedrine hydrochloride. South
Med J 38(1):64-65.
Council for Responsible Nutrition
December 19, 2000
179
Daly, P.A., Drieger, D.R., Dulloo, A.G., Young, J.B., and Landsberg, L. 1993. Ephedrine,
caffeine and aspirin: Safety and efficacy for the treatment of human obesity. Int J
Obesity Related Metabol Disord 17(Suppl. 1):S73-S78.
Dawson, J.K., Earnshaw, S.M., and Graham, C.S. 1995. Dangerous monoamine oxidase
inhibitor interactions are still occurring in the 1990s. J Accid Emerg Med 12:49-51.
Derreza, H., Fine, M.D., and Sadaniantz, A. 1997. Acute myocardial infarction after use of
pseudoephedrine for sinus congestion. J Am Board Fam Pract. 10(6):436-438.
Dewsnap, P., and Libby, G. 1992. A case of affective psychosis after routine use of proprietary
cold remedy containing phenylpropanolamine. Hum Exper Toxicol 11(4):295-296.
Dollery, C. (Ed.) 1991a. Ephedrine (hydrochloride) In: Dollery, C. (Ed.) Therapeutic Drugs.
Churchill Livingstone, New York, NY, Vol. 1:E26-E29.
Dollery, C. (Ed.) 1991b. Pseudoephedrine hydrochloride. In: Dollery, C. (Ed.) Therapeutic
Drugs. Churchill Livingstone, New York, NY, Vol. 2:P297-P299.
Dollery, C. (Ed.) 1991c. Caffeine. In: Dollery, C. (Ed.) Therapeutic Drugs. Churchill
Livingstone, New York, Vol. 1:C3-C6.
Dollery, C. (Ed.) 1991d. Phenylpropanolamine (hydrochloride) In: Dollery, C. (Ed.)
Therapeutic Drugs. Churchill Livingstone, New York, NY, Vol. 2:P91-P93.
Doyle, H., and Kargin, M. 1996. Herbal stimulant containing ephedrine has also caused
psychosis. BMJ (Br Med J) 313(7059):756.
Drew, C.D., Knight, G.T., Hughes, D.T., and Bush, M. 1978. Comparison of the effects of D-()ephedirine and L-(+)-pseudoephedrine on the cardiovascular and respiratory systems in
man. Br J Clin Pharmacol 6(3):221-225.
Edwards, M., Russo, L., and Harwood-Nuss, A. 1987. Cerebral infarction with a single oral
dose of phenylpropanolamine. Am J Emerg Med 5(2):163-164.
Eldor, J. 1991. Ephedrine in the initial treatment of haemorrhagic shock. Med Hypotheses
35(3):250-252.
Ellenhorn, M.J., and Barcelous, D.G. 1988. Over-the-counter products. In: Ellenhorn, M.H.,
and Barceloux, D.G. Medical Toxicology: Diagnosis and Treatment of Human
Poisoning. Elsevier, New York, NY. Pp. 501-559.
Fairchild, M.D., and Alles, G.A. 1967. The central locomotor stimulatory activity and acute
toxicity of the ephedrine and norephedrine isomers in mice. J Pharmacol Exper
Therapeut 158(1):135-139.
Council for Responsible Nutrition
December 19, 2000
180
FDA. 2000. Assessment of Public Health Risks Associated with the Use of Ephedrine AlkaloidContaining Dietary Supplements. Food and Drug Administration, U.S. (FDA), Center for
Food Safety and Applied Nutrition (CFSAN). FDA Docket No. 00N-1200, Vol. 40,
March 31.
Feller, D., and Malspeis, L. 1977. Biotransformation of D(-) ephedrine and L(+) ephedrine in
the rabbit, in vivo and in vitro. Drug Metab Dispos 5(1):37-46.
Fugh-Berman, A. 1997. Clinical trials of herbs. Primary Care - Clinics Office Pract 24(4):889903.
GAO. 1999. Dietary Supplements: Uncertainties in Analyses Underlying FDA's proposed Rule
on Ephedrine Alkaloids. United States General Accounting Office (GAO), Washington,
DC.
Garriott, J.C., Simmons, L.M., Poklis, A., and MacKell, M.S. 1985. Five cases of fatal overdose
from caffeine-containing "look-alike" drugs. J Anal Toxicol 9(3):141-143.
Geissler, C. 1993. Effects of weight loss, ephedrine and aspirin on energy expenditure in obese
women. Int J Obesity Related Metabol Disord 17(Suppl. 1):S45-S48.
Gilbert, E.F., Matsuoka, R., Bruyere, H., and, Optiz, J.M. 1981. Teratogenic effect of Tedral
(theophylline, ephedrine and phenobarbital) on cardiac development in chick embryos.
Circulation 64(Suppl. 4):233 (Abstract No. 885).
Gilbert-Barness, E., and Drut, R.M. 2000. Association of sympathomimetic drugs with
malformations. Vet Human Toxicol 42(3):168-171.
Glick, R., Hoying, J., Cerullo, L., and Perlman, S. 1987. Phenylpropanolamine: An over-thecounter drug causing central nervous system vasculitis and intracerebral hemorrhage:
Case report and review. Neurosurgery 20(6):969-974.
Glidden, R.S., and DiBona, F.J. 1977. Urinary retention associated with ephedrine. J Pediatr
90(6):1013-1014.
Goldfrank, L.R., and Hoffman, R.S. 1991. The cardiovascular effects of cocaine. Ann Emerg
Med 20:165-175.
Gruber, A.J., and Pope, H.G. (Jr.) 1998. Ephedrine abuse among 36 female weightlifters. Am J
Addict 7(4):256-261.
Grunberg, E., Randall, L.O., and Schnitzer, R.J. 1949. The chemotherapeutic and
pharmacological properties of the l-ephedrine salt of penicillin G (Tersavin) J Pharmacol
Exper Therapeut 95:336-346.
Council for Responsible Nutrition
December 19, 2000
181
Gualtieri, J., and Harris, C. 1996. Dilated cardiomyopathy in a heavy ephedrine abuser. J
Toxicol (Clin Toxicol) 34(5):581-582 (Abstract No. 76).
Gurley, B.J., Gardner, S.F., White, L.M., and Wang, P. 1997a. Pharmacokinetics of ephedrine
following the ingestion of commercially available herbal preparations of ephedra sinica
(Ma-huang) Pharmaceut Res 14(11 Suppl.):S519 (Abstract No. 3160).
Gurley, B.J., Gardner, S.F., White, L.M., and Wang, P.L. 1998a. Ephedrine pharmacokinetics
after the ingestion of nutritional supplements containing Ephedra sinica (ma huang)
Therapeut Drug Monit 20(4):439-445.
Gurley, B.J., Wang, P., and Gardner, S.F. 1998b. Ephedrine-type alkaloid content of nutritional
supplements containing Ephedra sinica (Ma huang) as determined by high performance
liquid chromatography. J Pharmaceut Sci 87(12):1547-1553.
Gurley, B.J., Wang, P., and Gardner, S.F. 1997b. Ephedrine alkaloid content of five
commercially available herbal products containing ephedra sinica (Ma-huang)
Pharmaceut Res 14(11 Suppl. 1):S582-S583 (Abstract No. 3357).
Gurley, B.J., Gardner, S.F and Hubbard, M.A. 2000. Content versus label claims in ephedracontaining dietary supplements. Am J Healthy Syst Pharm Vol 57, May 15, 2000.
Haller, C.A., and Benowitz, N.L. 2000. Adverse cardiovascular and central nervous system
events associated with dietary supplements containing ephedra alkaloids. NEJM,
December 21, 2000.
Haseman, J.K. 1983. Patterns of tumor incidence in two-year cancer bioassay feeding studies in
Fischer 344 rats. Fundam Appl Toxicol 3(1):1-9.
Hellriegel, E.T., Bjornsson, R.D., and, Hauck, W.W. 1996. Interpatient variability in
bioavailability is related to the extent of absorption. Implication for bioavailability and
bioequivalence studies. Clin Pharmacol Therapeut 60:601-607.
Henney, J.E. 1999. Statement by Jane E. Henney, M.D., Commissioner, Food and Drug
Administration, Department of Health and Human Services Before the Committee on
Government Reform, March 25, 1999. U.S. House of Representatives, Washington, DC.
[http://www.fda.gov/ola/1999/dietary.html].
Herridge, C.F., and A’Brook, M.F. 1968. Ephedrine psychosis. BMJ (Br Med J) 2:160.
Hirabayashi, Y., Saitoh, K., Fukuda, H., Mitsuhata, H., and Shimizu, R. 1996. Coronary artery
spasm after ephedrine in a patient with high spinal anesthesia. Anesthesiology 84(1):221224.
Hoffman, B.B., and Lefkowitz, R.J. 1996. Catecholamines, sympathomimetic drugs, and
adrenergic receptors antagonists. In: Hardman, J.G., Limbird, L.E., Molinoff, P.B.,
Council for Responsible Nutrition
December 19, 2000
182
Ruddon, R.W., and Goodman Gilman, A. (Eds.) Goodman and Gilman's The
Pharmacological Basis of Therapeutics (9th Ed.) McGraw Hill., New York, NY, Toronto,
ON, pp. 199-248.
Horton, T.J., and Geissler, C.A. 1996. Post-prandial thermogenesis with ephedrine, caffeine and
aspirin in lean, pre-disposed obese and obese women. Int J Obesity Related Metabol
Disord 20:91-97.
Horton, T.J., and Geissler, C.A. 1991. Aspirin potentiates the effect of ephedrine on the
thermogenic response to a meal in obese but not lean women. Int J Obesity 15(5):359366.
HSP, 2000. Yale Hemorrhagic Stroke Project: Final Study Report. The safety of
phenylpropanolamine hydrochloride (PPA) used in OTC weight control and nasal
decongestant drug products.
Hu, S. 2000. Botanical, Agricultural, Production and Supply Aspects of Ephedra. Unpublished.
Huber, G.L. 1999. The benefits and risks of dietary supplements in the practice of bariatric
medicine and weight management. Presented at the Ephedra International Symposium,
American Herbal Products Association, Pentagon City- Arlington, VA. December 9-10,
1999. Unpublished.
Huber, G.L. 2000. Study on Dietary Supplements for Weight Loss. Presented at the Office on
Women’s Health, U.S. Department of Health and Human Services (HHS) public meeting
on the safety of dietary supplements containing ephedrine alkaloids, in Washington, D.C.,
on August 8-9, 2000. Unpublished.
Hughes, S.C., Ward, M.G., Levinson, G., Shnider, S.M., Wright, R.G., Grunenke, L.D., and,
Craig, J.D. 1985. Placental transfer of ephedrine does not affect neonatal outcome.
Anesthesiology 63:217-219.
Huxtable, R.J. 1992. The myth of beneficent nature: The risks of herbal preparations. Ann
Intern Med 117:165-166.
ICH Steering Committee. 1996. Guideline for Good Clinical Practice (ICH Harmonised
Tripartite Guideline). International Conference on Harmonisation of Technical
Requirements for Registration of Pharmaceutical for Human Use (ICH), No. E6.
Ingerslev, J., Svendsen, T.L., and Mørk, A. 1997. Is an ephedrine caffeine treatment
contraindicated in hypertension? Int J Obesity Related Metabol Disord 21(8):666-673.
Insel, P.A., and Motuksky, H.J. 1987. Physiologic and pharmacologic regulation of adrenergic
receptors. In: Insel, P.A. (Ed.). Adrenergic Receptors in Man. Dekker, New York, NY.
Receptors and Ligands in Intercellular Communication, Vol. 8:201-236.
Council for Responsible Nutrition
December 19, 2000
183
Insel, P.A. 1991. Beta-adrenergic receptors in pathophysiologic states and in clinical medicine.
In: Perkins, J.P. (Ed). The Beta-Adrenergic Receptors. Humana Press, Clifton, NJ (The
Receptors) pp. 295-343.
Ishigooka, J., Yoshida, Y., and Muraski, M. 1991. Abuse of "BRON": A Japanese OTC cough
suppressant solution containing methylephedrine, codeine, caffeine and
chlorpheniramine. Progr Neuro-Psychopharmacol Biol Psychiat 15(4):513-521.
Jacobs, K.M., and Hirsch, K.A. 2000. Psychiatric complications of ma-huang. Psychosomatics
41(1):58-62.
[Japanese]. 1978. [Ephedra herba]. Kiso to Rinsho (Clin Rep) 12:2125-2131.
Jones, J.K. 1992. Approaches to evaluation causation of suspected drug reactions. In: Strom,
B.L., and Velo, G. (Eds.). Drug Epidemiology and Post-Marketing Surveillance.
Plenum Press, New York, NY. NATO ASI Series A (Life Sciences), Vol. 224:103-113.
Kaats, G.R., and Aldeman, J.A. 1994. Effects of multiple herbal formulation on body
composition, blood chemistry, vital signs and self-reported energy levels and appetite
control. Int J Obesity Related Metabol Disord 18(Suppl. 2):145 (Abstract No. P550).
Kalman, D.S., Colker, C.M., Shi, Q., and Swain, M.A. 2000. Effects of a weight-loss aid in
healthy overweight adults: Double-blind, placebo-controlled clinical trial. Curr
Therapeut Res 61(4):199-205.
Kanai, T., Nishikawa, T., Satoh, A., and Kajita, A. 1986a. Cardiovascular teratogenicity of
ephedrine in rats. Senten Ijo (Cong Anom) 26(3):246.
Kanai, T., Nishikawa, T., Satoh, A., and Kajita, A. 1986b. Cardiovascular teratogenicity of
ephedrine in rats. Teratology 34(3):469 (Abstract).
Kanfer, I., Dowse, R., and Vuma, V. 1993. Pharmacokinetics of oral decongestants.
Pharmacotherapy 13(6, Prt. 2):116S-128S, discussion 143S-146S.
Karch, S.B. 1993. Synthetic stimulants <Phenylpropanolamine> In: Karch, S.B. The Pathology
of Drug Abuse. CRC Press, Boca Raton, FL, pp. 165, 177-198.
Karch, S.B. 1993. Synthetic stimulants <Fenfluramine, mescaline analogs> In: Karch, S.B.
The Pathology of Drug Abuse. CRC Press, Boca Raton, FL, pp. 199-218.
Karch, S.B., Green, G. and Young, S. 1995. Myocardial hypertrophy and coronary artery
disease in male cocaine users. J Forensic Sci 40(4):591-595.
Karch, S.B. 2000. Ma huang and the Ephedra alkaloids. In: Cupp, M.J. (Ed.) Toxicology and
Clinical Pharmacology of Herbal Products. Humana Press, Inc., Totowa, NJ, pp. 11-30.
Council for Responsible Nutrition
December 19, 2000
184
Kernan, W.N., Viscoli, C.M., Brass, L.M., Broderick, J.P., Brott, T., Feldmann, E., Morgenstern,
L.B., Wilterdink, J.L., and Horwitz, R.I. 2000. Phenylpropanolamine and the Risk of
Hemorrhagic stroke. NEJM, December 21, 2000.
Kizer, K.W. 1984. Intracranial hemorrhage associated with overdose of decogenstant containing
phenylpropanolamine. Am J Emerg Med 2(2):180-181.
Krieger, D.R., Daly, P.A., Dulloo, A.G., Ransil, B.J., Young, J.B., and Landsberg, L. 1990.
Ephedrine, caffeine and aspirin promote weight loss in obese subjects. Trans Assoc Am
Physicians 103:307-312.
Kuitunen, T., Kärkkäinen, S., and Ylitalo, P. 1984. Comparison of the acute physical and
mental effects of ephedrine, fenfluramine, phentermine and prolintane. Methods Find
Exper Clin Pharmacol 6(5):265-270.
Laitinen, L.A., Empey, D.W., Bye, C., Britton, M.G., McDonnell, K., and Hughes, D.T.D. 1982.
A comparison of the bronchodilator action of pseudoephedrine and ephedrine in patients
with reversible airway obstruction. Eur J Clin Pharmacol 23:107-109.
Lake, C.R., Gallant, S., Masson, E., and Miller, P. 1990a. Adverse drug effects attributed to
phenylpropanolamine: A review of 142 case reports. Am J Med 89:195-208.
Lake, C.R., Rosenberg, D.B., Gallant, S., Zaloga, G., and Chernow, B. 1990b.
Phenylpropanolamine increases plasma caffeine levels. Clin Pharmacol Therapeut
47(6):675-685.
Lake, C.R., Tenglin, R., Chernow, B., and Holloway, H.C. 1983. Psychomotor stimulatantinduced mania in a genetically predisposed patient: A review of the literature and report
of a case. J Clin Psychopharmacol 3(2):97-100.
Law, M.Y., Pedersen, G.H., Hennen, W.J., McCausland, C.W., and Sidwell, R.W. 1996. Subacute toxicity study of ma-huang in mice. Fundam Appl Toxicol 30(1-Prt. 2):111
(Abstract No. 566).
Lee, E.B. 1982. Teratogenicity of the extracts of crude drugs. Saengyak Hakhoe Chi (Korean J
Pharmacognosy) 13:116-121.
Lee, M.K., Wong, Y.K., Che, C.T., and Hsieh, D.P.H. 1999. Adrenergic agonists effects and
cyto-toxicity of Chinese ephedra (ma-huang) used for weight reduction. Toxicologist
48(1S):58 (Abstract No. 272).
Lee, M.K., Cheung, B.W.H., Che, C.T., and Hsieh, D.P.H. 2000. Cytotoxicity assessment of
ma-huang (ephedra) under different conditions of preparation. Tox Sci 56:424-430.
Lefkowitz, R.J., Hoffman, B.B., and Taylor, P. 1990. Neurohumoral transmission: The
autonomic and somatic motor nervous systems. In: Gilman, A.G., Rall, T.W., Nies,
Council for Responsible Nutrition
December 19, 2000
185
A.S., and Taylor, P. (Eds.). Goodman and Gilman's The Pharmacological Basis of
Therapeutics (8th Ed.). Pergamon Press Ltd., New York, NY, Toronto, ON, pp. 89-90.
Leung, A.Y., and Foster, S. 1996. Ephedra. In: Leung, A.Y., and Foster, S. Encyclopedia of
Common Natural Ingredients Used in Foods, Drugs and Cosmetics. John Wiley, New
York, NY, pp. 227.
Levine, B., Jones, R., Klette, K., Smith, M.L., and Kilbane, E. 1993. An intoxication involving
BRON™ and Verapamil. J Anal Toxicol 17(6):381-383.
Lindahl, A., Sandström, R., Ungell, A.-L., Abrahamsson, B., Knutson, T.W., Knutson, L., and
Lennernäs, H. 1996. Jejunal permability and hepatic extraction of fluvastatin in humans.
Clin Pharmacol Therapeut 60:493-503.
Liu, Y.L., Toubro, S., Astrup, A., and Stock, M.J. 1995. Contribution of ß3-adrenoceptor
activation to ephedrine-induced thermogenesis in humans. Int J Obesity Related Metabol
Disord 19(9):678-685.
Loizou, L.A., Hamilton, J.G., and Tsementzis, S.A. 1982. Intracranial haemorrhage in
association with pseudoephedrine overdose. J Neurol Neurosurg Psychiat 45(5):471-472.
Loosmore, S., and Armstrong, D. 1990. Do-Do abuse. Br J Psychiat 157:278-281.
LSRO. 1998. Alternative and Traditional Models for Safety Evaluation of Food Ingredients.
Prepared for: Center for Food Safety and Applied Nutrition Food and Drug
Administration Department of Health and Human Services, Washington, DC 20204,
under FDA Contract No. 223-92-2195, Task Order #9. Life Sciences Research Office,
American Society for Nutritional Sciences, Bethesda, MD.
Lustik, S.J., Chhibber, A.K., Van Vliet, M., and Pomerantz, R.M. 1997. Ephedrine-induced
coronary artery vasospasm in a patient with prior cocaine use. Anesthesia Analgesia
84(4):931-933.
Maertens, P., Lum, G., Williams, J.P., and White, J. 1987. Intracranial hemorrhage and cerebral
angiopathic changes in a suicidal phenylpropanolamine poisoning. South Med J
80(12):1584-1586.
Martinez, F.V., Badas, A.J., Goitia, J.F.G., and Aguirre, I. 1993. Generalized dermatitis due to
oral ephedrine. Contact Dermatit 29(4):215-216.
Marvola, M. 1976. Effect of acetylated derivatives of some symphathomimetic amines on the
acute toxicity, locomotor activity and barbiturate anaesthesia time in mice. Acta
Pharmacologica et Toxicologica 38:474-489.
Marvola, M., and Kivirinta, R. 1978. Pharmacokinetics and locomotor activity increasing effect
of ephedrine in mice. Acta Pharmacologica et Toxicologica 43:381-386.
Council for Responsible Nutrition
December 19, 2000
186
Massoudi, M., and Miller, D. 1977. Ephedrine, a thermogenic and potential slimming drug.
Proc Nutr Soc 36:135A.
Matsuoka, R., Gilbert, E.F., Bruyers, H.(Jr.), and Optiz, J.M. 1985. An aborted human fetus
with truncus arteriosus communis. Possible teratogenic effect of tedral. Heart Vessels
1(3):176-178.
Matthews, G., Smolinske, S., and White, S. 1997. Ephedrine-related stroke in a teenager. J
Toxicol (Clin Toxicol) 35(5):555 (Abstract No. 178).
May, C.S., Paterson, J.W., Spiro, S.G., and Johnson, A.J. 1975. Intravenous infusion of
salbutamol in the treatment of asthma. Br J Clin Pharmacol 2:503-508.
McLaurin, J.W., Shipman, W.F., and Rosedale, R. 1961. Oral decongestants. A double blind
comparison study of the effectiveness of four sympthomimetic drugs: Objective and
subjective. Laryngoscope 71:54-67.
Mendez, M.F. 1992. Mania self-induced with cough syrup. J Clin Psychiat 53(5):173-174.
Midha, K.K., Cooper, J.K., and, McGilveray, I.J. 1979. Simple and specific electron-capture
GLC assay for plasma and urine ephedrine concentrations following single doses. J
Pharmaceut Sci 68:557-560.
Miller, D.K., Mcmahon, L.R., Green, T.A., Nation, J.R., and Wellman, P.J. 1998. Repeated
administration of ephedrine induces behavioral sensitization in rats.
Psychopharmacology 140(1):52-56.
Minamatsu, S., Kobayashi, Y., Kobayashi, N., Juhii, Y., Aburada, M., and Yamashita, M. 1991.
Acute ephedra herba and ephedrine poisoning in mice. Chudoku Kenkyu (Jpn J Toxicol)
4:143-149.
Moheb, M.A., Geissler, C.A., and Lancer, K. 1998. Effect of ephedrine, caffeine, and aspirin, in
combinations of weight loss in obese women. Int J Obesity Related Metabol Disord
22(Suppl. 3):S264 (Abstract No. P636).
Molnár, D. 1993. Effects of ephedrine and aminophylline on resting energy expendure in obese
adolescents. Int J Obesity Related Metabol Disord 17(Suppl. 1):S49-S52.
Molnár, D., Torok, K., Erhardt, E., and Jeges, S. 2000. Safety and efficacy of treatment with an
ephedrine/caffeine mixture. The first double-blind placebo-controlled pilot study in
adolescents. Int J Obesity 24:1573-1578.
Morgan, J.P. 1986. Phenylpropanolamine: A Critical Analysis of Reported Adverse Reactions
and Overdosage. Jack K. Burgess, Inc., Fort Lee, NJ.
Council for Responsible Nutrition
December 19, 2000
187
Morimoto, L., Watanabe, F., Osawa, T., Okitsu, T., and Kada, T. 1982. Mutagenicity screening
of crude drugs with Bacillus subtilis rec- assay and Salmonella/microsome reversion
assay. Mutat Res 97(2):81-102.
Mortimer, E.A. (Jr.) 1977. Drug toxicity from breast milk? Pediatrics 60:780-781.
Nadir, A., Agrawal, S., King, P.D., and Marshall, J.B. 1996. Acute hepatitis associated with the
use of a chinese herbal product, Ma- huang. Am J Gastroenterol 91(7):1436-1438.
Namba, T., Kubo, M., Kanai, Y., Namba, K., Nishimura, H., and, Qazilbash, N.A. 1976.
Pharmacological studies of ephedra plants. Part 1. The comparative histological studies
on ephedra rhizomes from Pakistan and Afghanistan and Chinese crude drugs "Ma-HungGen". Planta Medica 29:216-225.
Nasser, J.A., Wang, V., Chen, G.C., Solomon, J.L., Heymsfield, S.B., and Boozer, C.N. 1999.
Efficacy trial for weight loss of an herbal supplement of Ma huang and guarana. FASEB
J 13(5, Prt. 2):A874 (Abstract No. 660.8).
National Academy of Sciences (NAS), 1998. National Academy of Sciences Model: Dietary
Reference Intakes: A Risk Assessment Model for Establishing Upper Intake Levels for
Nutrients. Institute of Medicine, National Academy Press (NAP), Washington, DC, pp.
71.
Neve, K.A., and Molinoff, P.B. 1986. Effects of chronic administration of agonists and
antagonists on the density of beta-adrenergic receptors. Am J Cardiol 57:17F-22F.
Nishikawa, T.H.J., Bruyere, H.J. (Jr.), Takagi, Y., Gilbert, E.F., and Uno, H. 1985.
Cardiovascular teratogenicity of ephedrine in chick embryos. Toxicol Lett 29(1):59-63.
NIOSH, 1997. Registry of Toxic Effects of Chemical Substances, Centers for Disease Control
and Prevention. Ephedrine.
Norregaard, J., Jorgensen, S., Mikkelsen, K.L., Tonnesen, P., Iversen, E., Sorensen, T., Soeberg,
B., and Jakobsen, H.B. 1996. The effect of ephedrine plus caffeine on smoking cessation
and postcessation weight gain. Clin Pharmacol Therapeut 60(6):679-686.
NTP. 1986. Toxicology and Carcinogenesis Studies of Ephedrine Sulfate (CAS No. 134-72-5)
in F344/N Rats and B6C3F1 Mice (Feed Studies) National Toxicology Program (NTP),
Research Triangle Park, NC, (NTP Technical Report Series) No. 307.
Nuotto, E. 1983. Psychomotor, physiological and cognitive effects of scopalamine and
ephedrine in healthy man. Eur J Clin Pharmacol 24:603-609.
Oosterbaan, R., and Burns, M.J. 2000. Myocardial infarction associated with
phenylpropanolamine. J Emerg Med. 18(1):55-59.
Council for Responsible Nutrition
December 19, 2000
188
Pace, S. 1996. Ma huang food supplement toxicity in two adolescents. J Toxicol (Clin Toxicol)
34(5):598 (Abstract No. 120).
Pasquali, R., and Casimirri, F. 1993. Clinical aspects of ephedrine in the treatment of obesity.
Int J Obesity Related Metabol Disord 17(Suppl.1):S65-S68.
Pasquali, R., Baralsi, G., Cesari, M.P., Melchionda, N., Zamboni, M., Stefanini, C., and Raitano,
A. 1985. A controlled trial using ephedrine in the treatment of obesity. Int J Obesity
9(2):93-98.
Pasquali, R., Casimirri, F., Melchionda, N., Grossi, G., Bortoluzzi, L., Morsellilabate, A.M.,
Stefanini, C., and Raitano, A. 1992. Effects of chronic administration of ephedrine
during very-low-calorie diets on energy expenditure, protein metabolism and hormone
levels in obese subjects. Clin Sci 82(1):85-92.
Pasquali, R., Cesari, M.P., Melchionda, N., Stefanini, C., Raitano, A., and Labo, G. 1987. Dose
ephedrine promote weight loss in low-energy-adapted obese women. Int J Obesity
11(2):163-168.
Perrotta, D.M., Coody, G., and Culmo, C. 1996. Adverse events associated with ephedrinecontaining products: Texas, December 1993-September 1995. J Am Med Assoc
276(21):1711-1712.
Peterson, D., and Hardings, M. 1967. The effect of various environmental factors on cocaine
and ephedrine toxicity. J Pharm Pharmacol 19:810-814.
Pickup, M.E., May, C.S., Senadagire, R.S., and Paterson, J.W. 1976. The pharmacokinetics of
ephedrine after oral dosage in asthmatics receiving acute and chronic treatment. Br J Clin
Pharmacol 3(1):123-134.
Pomerantz, B., and O'Rouke, R. 1969. The Stokes-Adams Syndrome. Am J Med 46:941-960.
Powell, T., Hsu, F.F., Turk, J., and Hruska, K. 1998. Ma-huang strikes again: Ephedrine
nephrolithiasis. Am J Kidney Dis 32(1):153-159.
Puar, H.S. 1984. Acute memory loss and nominal aphasia caused by phenylpropanolamine.
South Med J 77(12):1604-1605.
Quaade, F., Astrup, A., Breum, L., Toubro, S., and Hein, P. 1992. The effect of an
ephedrine/caffeine combination as a supplement to a weight-reducing diet. A randomized
placebo-controlled double-blind trial = Effekten af en efedrin/koffein-kombination som
understottelse af en affedningsdiaet: En randomisert, placbokontrolleret, dobbelblind
undersogelse. Ugeskrift for Laeger 154(18):1258-1263.
Council for Responsible Nutrition
December 19, 2000
189
Ramsey, J.J., Colman, R.J., Swick, A.G., and Kemnitz, J.W. 1998. Energy expenditure, body
composition, and glucose metabolism in lean and obese rhesus monkeys treated with
ephedrine and caffeine. Am J Clin Nutr 68(1):42-51.
Rang, H.P., and Dale, M.M. 1995. Pharmacology. Churchill Livingstone Inc., New York, NY.
Renwick, A.G. 1995. The use of an additional safety or uncertainty factor for nature of toxicity in
the estimation of acceptable daily intake and tolerable daily intake values. Regul Toxicol
Pharmacol 22(3):250-261
Renwick, A.G., and Lazarus, N.R. 1998. Human variability and noncancer risk assessment - An
analysis of the default uncertainty factor. Regul Toxicol Pharmacol 27(1):3-20.
Robertson, D., Frolich, J.C., Carr, R.K., Watson, J.T., Hollifield, J.W., Shand, D.G., and Oates,
J.A. 1978. Effects of caffeine on plasma renin activity, catecholamines, and blood
pressure. N Eng J Med 298(4):181-186.
Roxanas, M.G., and Spalding, J. 1977. Ephedrine abuse psychosis. Med J Austral 64(5):639640.
Sagara, K., Oshima, T., and, Misaki, T. 1983. A simultaneous determination of norephedrine,
pseudoephedrine, ephedrine and methylephedrine in ephedrae herba and oriental
pharmaceutical preparations by ion-pair high-performance liquid chromatography. Chem
Pharmaceut Bull 31:2359-2365.
Sever, P.S., Dring, L.G., and Williams, R.T. 1975. The metabolism of (-)-ephedrine in man.
Eur J Clin Pharmacol 9(2/3):193-198.
Shannon, J.R., Gottesdiener, K., Jordan, J., Chen, K., Flattery, S., Larson, P.J., Candelore, M.R.,
Gertz, B., Robertson, D., and Sun, M. 1999. Acute effect of ephedrine on 24-h energy
balance. Clin Sci 96(5):483-491.
Sharma, A.N., Cinci, P.M., and Hoffman, R.S. 2000. Ma huang-induced myocardial infarction
with normal coronary arteries. J Toxicol (Clin Toxicol) 38(5):521 (Abstract No. 24)
Shenfield, G.M. 1982. Combination bronchodilator therapy. Drugs 24(5):414-439.
Sheu, S.-J. 1997. Identification by chemical analysis of the botanical sources of commercial
samples of Chinese herbal drugs. Yao Wu Shih P'in Fen Hsi (J Food Drug Anal)
5(4):285-294.
Sidney, K., and Lefcoe, N.M. 1977. The effects of ephedrine on the physiological and
psychological responses to submaximal and maximal exercise in man. Med Sci Sports
9:95-99.
Council for Responsible Nutrition
December 19, 2000
190
Sinsheimer, J.E., Dring, L.G., and Williams, R.T. 1973. Species differences in the metabolism
of norephedrine in man, rabbit and rat. Biochem J 136:763-771.
Smith, D., and Perry, P. 1992. The efficacy of ergogenic agents in athletic competition. Part II:
Other performance-enhancing agents. Ann Pharmacother 26(5):653-659.
Snook, C., Otten, M., and Hassan, M. 1992. Massive ephedrine overdose: Case report and
toxicokinetic analysis. Vet Hum Toxicol 34(4):335 (Abstract No. 75).
Sprague, J.E., Harrod, A.D., and Teconchuk, A.L. 1998. Pharmacology and abuse potential of
ephedrine. Pharm Times 64(May):72-80.
Strömberg, C., Vanakoski, J., Olkkola, K.T., Lindquist, A., Seppälä, T., and Laitinen, L.A. 1992.
Exercise alters the pharmacokinetics of midazolam. Clin Pharmacol Therapeut
51(5):527-532.
Tang, D.H. 1996. Ephedra ('Ma huang') Clin Toxicol Rev 18(10).
Tashkin, D.P., Meth, R., Simmons, D.H., and, Lee, Y.E. 1975. Double-blind comparison of
acute bronchial and cardiovascular effects of oral terbutaline and ephedrine. Chest
68(2):155-161.
Theoharides, T.C. 1997. Sudden death of a healthy college student related to ephedrine toxicity
from a Ma Huang-containing drink. J Clin Psychopharmacol 17(5):437-439.
To, L.B., Sangster, J.F., Rampling, D., and Cammens, I. 1980. Ephedrine-induced
cardiomyopathy. Med J Austral 2(1):35-36.
Toubro, S., Astrup, A., Breum, L., and Quaade, F. 1993b. The acute and chronic effects of
ephedrine/caffeine mixtures on energy expenditure and glucose metabolism in humans.
Int J Obesity Related Metabol Disord 17(Suppl. 3):S73-S77.
Toubro, S., Astrup, A.V., Breum, L., and Quaade, F. 1993a. Safety and efficacy of long-term
treatment with ephedrine, caffeine and an ephedrine/caffeine mixture. Int J Obesity
Related Metabol Disord 17(Suppl. 1):S69-S72
Turner, J.E., and Cravey, R.H. 1977. A fatal ingestion of caffeine. Clin Toxicol 10:341-344.
Tyler, V.E. 1993. Ephedra (Ma huang) In: Tyler, V.E. The Honest Herbal: A Sensible Guide
to the Use of Herbs and Related Remedies (3rd Ed.) Pharmaceutical Products Press
(PPP), New York, NY, pp. 119-121.
Ueng, T.-H., Kang, J.-J., Wang, H.-W., and Lin, P.-C. 1997. An overview of the toxicology of
commonly used traditional Chinese medicine. Yao Wu Shih P'in Fen Hsi (J Food Drug
Anal) 5(4):241-264.
Council for Responsible Nutrition
December 19, 2000
191
Upton, R.A. 1991. Pharmacokinetic interactions between theophylline and other medication
(Part I) Clin Pharmacokinet 20(1):66-80.
Vahedi, K., Domigo, V., Amarenco, P., and Bousser, M.-G. 2000. Ischaemic stroke in a
sportsman who consumed MaHuang extract and creatin monohydrate for body building.
J Neurol Neurosurg Psychiat 68(1):112-113.
Van Mieghem, W., Stevens, E., and Cosemans, J. 1978. Ephedrine-induced cardiopathy. BMJ
(Br Med J) 1(6116):816.
Van Mil, E., and Molnar, D. 2000. Drug treatment in obese adolescents. Int J Obesity
24(Suppl. 1):S184 (Abstract No. 621).
Vanakoski, J., Strömberg, C., and Seppälä, T. 1993. Effects of a sauna on the pharmacokinetics
of midazolam and ephedrine in healthy young women. Eur J Clin Pharmacol 45(4):377381.
Waluga, M., Janusz, M., Karpel, E., Hartleb, M., and Nowak, A. 1998. Cardiovascular effects
of ephedrine, caffeine and yohimbine measured by thoracic electrical bioimpedance in
obese women. Clin Physiol 18(1):69-76.
Warot, D., Berlin, I., Aymard, G., Acquaviva, E., Legrand, M., Labarthe, B., Diquet, B., and
Lechat, P.H. 2000. Comparative pharmacodynamics and pharmacokinetics of oral and
intranasal ephedrine. Fun & Clin Pharma: Abstract 237-297.
Warren, M.R., and Werner, H.W. 1945c. Effect of temperature on the toxicity of some
vasopressor amines. Fed Proc (FASEB) 4:139 (Abstract).
Warren, M.R., and Werner, H.W. 1945a. Acute toxicity of vasopressor amines: II.
Comparative data. J Pharmacol Exper Therapeut 86:284-286.
Warren, M.R., and Werner, H.W. 1945b. The central stimulant action of some vasopressor
amines. J Pharmacol Exper Therapeut 85:119-121.
Wahl, M., Grant, C., and Jesperson, R. 2000. Acute psychosis from a dietary weight control
supplement. J Toxicol (Clin Toxicol) 38(5):522-523 (Abstract No. 48).
Weesner, K.M., Denison, M., and Roberts, R.J. 1982. Cardiac arrhythmias in an adolescent
following ingestion of an over-the- counter stimulant. Clin Pediatr 21(11):700-701.
Welling, P.G., Lee, K.P., Patel, J.A., Walker, J.E., and Wagner, J.G. 1971. Urinary excretion of
ephedrine in man without pH control following oral administration of three commercial
ephedrine sulfate preparations. J Pharmaceut Sci 60(11):1629-1634.
Council for Responsible Nutrition
December 19, 2000
192
White, L.M., Gardner, S.F., Gurley, B.J., Marx, M.A., Wang, P.L., and Estes, M. 1997.
Pharmacokinetics and cardiovascular effects of Ma-Huang (Ephedra sinica) in
normotensive adults. J Clin Pharmacol 37(2):116-122.
Whitehouse, A.M., and Duncan, J.M. 1987. Ephedrine psychosis rediscovered. Br J Psychiat
150:258-261.
WHO. 1987. Principles For The Safety Assessment Of Food Additives and Contaminants In
Food. World Health Organization (WHO), International Programme on Chemical Safety
(IPCS), Geneva, Switz. Environmental Health Criteria No. 70.
Wilkinson, G., and Beckett, A. 1968b. Absorption metabolism and excretion of the ephedrine in
man: II. Pharmacokinetics. J Pharmaceut Sci 57:1933-1938.
Wilkinson, G.R., and Beckett, A.H. 1968a. Absorption, metabolism, and excretion of the
ephedrine in man: I. The influence of urinary pH and urine volume output. J Pharmacol
Exper Therapeut 162(1):139-147.
Williams, R., Caldwell, J., and Dring, L. 1973. Comparative metabolism of some amphetamines
in various species. In: Usdin, E, and Snyder, S. (Eds.). Frontiers in Catecholamine
Research (3rd Ed.). Pergamon Press, New York, NY, pp. 927-932.
Wilson, A.F., Novey, H.S., Cloninger, P., Davis, J., and White, D. 1976. Cardiopulmonary
effects of long-term bronchodilator administration. J Allergy Clin Immunol 58(1, Prt.
2):204-212.
Wolf, H.H., Schuster, M.A., and Lanciault, G. 1964. 'Aggregation' phenomenon and some
ephedrine isomers. J Pharmaceut Sci 53:987-988.
Xue-Jun, Y., De-xiang, L., Hechuan, W., and Yu, Z. 1991. A study on the mutagenicity of 102
raw pharmaceuticals used in Chinese traditional medicine. Mutat Res 260(1):73-82.
Yates, K.M., O’Connor, A., and Horsley, C.A. 2000. ‘Herbal ecstasy’: A case series of adverse
reactions. N Zeal Med J 113 (1114):315-517.
Yen, T., McKee, M., and Bemis, K. 1981. Ephedrine reduces weight of viable yellow obese
mice. Life Sci 28:119-128.
Yoovathaworn, K.C., Sriwatanakul, K., and Tithapandha, A. 1986. Influence of caffeine on
aspirin pharmacokinetics. Eur J Drug Metab Pharmacokinet 11(1):71-74.
Zaacks, S.M., Klein, L., Tan, C.D., Rodriguez, E.R., and Leikin, J.B. 1999. Hypersensitivity
myocarditis associated with ephedra use. J Toxicol (Clin Toxicol) 37(4):485-489.
Zahn, K.A., Li, R.L., and Purssell, R.A. 1999. Cardiovascular toxicity after ingestion of "herbal
ecstacy" J Emerg Med 17(2):289-291.
Council for Responsible Nutrition
December 19, 2000
193
Zhang, J.S., Tian, Z., and Lou, Z.C. 1993. Quality evaluation of twelve species of Chinese
Ephedra (ma-huang) Chung Kuo Yao Li Hsueh Pao (Acta Pharmacologica Sinica)
22:419-425.
Council for Responsible Nutrition
December 19, 2000
194
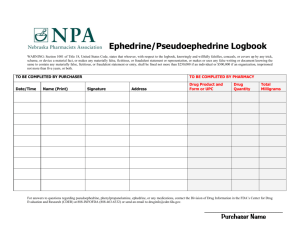
![[Versie 7, 08/2005] - Veterinary Medicines Directorate](http://s3.studylib.net/store/data/007507353_1-cc599c357de08cb27b9b1b1b0f78ebbf-300x300.png)
![[Versie 7, 08/2005] - Veterinary Medicines Directorate](http://s3.studylib.net/store/data/007257580_1-71667165b07d5e46a056ee9957328321-300x300.png)