OHSU Posters - Oregon Association of Hospitals and Health Systems
advertisement
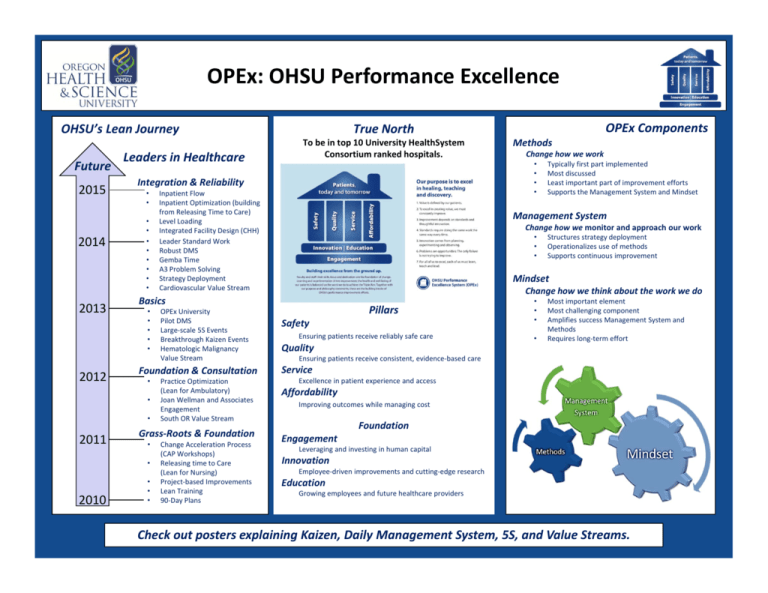
OPEx: OHSU Performance Excellence OHSU’s Lean Journey Future 2015 2014 2013 2012 Leaders in Healthcare • • • • • • • • • • Practice Optimization (Lean for Ambulatory) Joan Wellman and Associates Engagement South OR Value Stream Grass‐Roots & Foundation • • 2010 OPEx University Pilot DMS Large‐scale 5S Events Breakthrough Kaizen Events Hematologic Malignancy Value Stream Foundation & Consultation • 2011 Inpatient Flow Inpatient Optimization (building from Releasing Time to Care) Level Loading Integrated Facility Design (CHH) Leader Standard Work Robust DMS Gemba Time A3 Problem Solving Strategy Deployment Cardiovascular Value Stream • • • Change Acceleration Process (CAP Workshops) Releasing time to Care (Lean for Nursing) Project‐based Improvements Lean Training 90‐Day Plans Change how we work Typically first part implemented Most discussed Least important part of improvement efforts Supports the Management System and Mindset Management System Change how we monitor and approach our work • • • Structures strategy deployment Operationalizes use of methods Supports continuous improvement Mindset Change how we think about the work we do Basics • • • • • Methods • • • • Integration & Reliability • • OPEx Components True North To be in top 10 University HealthSystem Consortium ranked hospitals. Pillars Safety Ensuring patients receive reliably safe care • • • • Most important element Most challenging component Amplifies success Management System and Methods Requires long‐term effort Quality Ensuring patients receive consistent, evidence‐based care Service Excellence in patient experience and access Affordability Improving outcomes while managing cost Foundation Engagement Leveraging and investing in human capital Innovation Employee‐driven improvements and cutting‐edge research Education Growing employees and future healthcare providers Check out posters explaining Kaizen, Daily Management System, 5S, and Value Streams. Value Streams What is a Value Stream? Value Stream Process From the patient’s perspective, the path by which they travel (physically or virtually) to receive the product(s) or service(s) they need. Timeline of a Value Stream: Selection: Traditional Organizations: Launch: Each step of a patient’s visit is operated, analyzed, and optimized in a silo ED ICU IP Unit Home Education: Project Work: Pharmacy Value Stream Thinking: All activities involved in a patient’s visit, including their return to the community, are viewed together to better consider patient progression, care coordination, and improve visibility for quality and safety opportunities ICU 2‐3 month period clarifies the scope of the Value Stream, maps processes at a high level, and identifies areas of opportunity Key team members participate in OPEx Leader Training sessions and study visits to other leading organizations Lab ED The Value Stream is identified by the OPEx Steering Committee IP Unit Lab Pharmacy Home 18‐30 month period of Breakthrough Kaizen Events (about once a month) and other Kaizen and 5S Events Sustainability: Output from every event includes components of Daily Management Systems to ensure that improvements are maintained and improved further Transformation: It is the objective of the value stream to transform the operation’s performance as well as its methods, management system, and mindset Why Value Streams? • Act as a learning laboratory for the organization • Are tested and stressed to drive the system to transform • Accomplish breakthrough results • Surface opportunities in connected areas and teach those areas through their Daily Management Systems OHSU Value Streams South OR: • Launched December 2012 • Visibility Boards at KPV 5th Floor Hematologic Malignancies: • Launched Fall 2013 • Visibility Boards in CHM Clinic (MNP) and 14K Knight Cardiovascular Institute: • Launched Summer 2014 Inpatient Flow • Launched Fall 2014 • https://bridge.ohsu.edu/health/opex/IFV S/SitePages/Home.aspx) Check out posters explaining OPEx, Kaizen, Daily Management System, 5S, & Leader Standard Work. Hematologic Malignancies Value Stream Cindy Grueber Ann Raish Peggy Appel Executive Sponsor Sponsor Value Stream Manager 14K Key Improvements CHM Key Improvements HMVS in 2015 Scheduled Rounding The Inpatient Rounding event focused on including staff nurses and pharmacy on rounds, facilitated by following a rounding “schedule.” Also, afternoon Lightning Rounds help establish the rounding schedule and improve discharge planning. Percentage of Time Nurse Is Present When Team Rounds on Patient Level‐Loading CHM has made considerable progress towards an ideal level‐loaded system. Major changes include staggered patient arrival times for both clinic and infusion to alleviate bottlenecks around check‐in and patient preparation. Maximum Number of Patients Scheduled to Arrive for Check‐In at One Time (2 PAS Staff) Hematologic Malignancies patients are cared for as inpatients primarily on 14K and as outpatients at the CHM Clinic/Infusion Center. However, the average daily census for inpatients exceeds the total capacity on 14K, leading to HM patients on multiple other nursing units. In addition, CHM operates beyond scheduled “capacity” on a near daily basis. Improving the current state on 14K and at CHM will be measured by two metrics in 2015. <10% → >80% Discharge Zone The Inpatient Discharge Kaizen established a “Discharge Zone” for patients within 2‐3 days of expected discharge to help structure the work required for a smooth process without delays. A Milestone Board in the patient’s room helps improve communication with patients and caregivers about progression towards discharge. Average Time from Clinically Ready for Discharge to Actual Discharge 147 min → 102 min Epic Rounding Report The Inpatient Provider Documentation project identified wastes associated with collecting data and information before and during rounds. An Epic Rounding Report was designed to display multiple key data elements in a single location and reduce time spent “chart surfing.” 10 → 4 Just‐in‐Time Nurse Assignments CHM Infusion developed a Complexity Scale to quantify the nursing time required for a variety of treatments. This scale is then used to assign nurses as patients arrive and evenly distribute workload across the staff. Nurse Subjective Assessment of Workload Scale of 1 (Low) to 3 (High) with a Target of 2 2.6 → 2.0 Treatment Location Committee The Inpatient to Outpatient Shift Kaizen developed a process to systematically analyze treatments from clinical, social, financial, and other perspectives to determine if the setting of care should be shifted from inpatient to outpatient. Four regimens have been evaluated; two approved for pilots; and one pilot approved for full implementation in January 2015. Shift Setting of Care from Inpatient to Outpatient One strategy to reduce our number of inpatient days is to, when possible and appropriate, shift the setting of care for a treatment or service from inpatient to outpatient. Increasing CHM Capacity To accommodate the increasing demand on outpatient services, outpatient capacity must improve. Through waste reduction and process improvement, this capacity increase will be achieved ideally with minimal cost increases. Inpatient Flow Value Stream Megan Boyle, Hue Chiang Problem Statement Areas of Opportunity Results Hospital capacity is not meeting patient demand, leading to boarding patients, postponed/cancelled surgeries, and patients staying in their own communities longer than providers would like them to. Inputs: No standards around level loading, communications, patient placement prioritization Outputs: Discharges are not prioritized and unnecessarily complex Management systems: No standards around capacity management (Diverts, Andon, Communication) • Work gets pushed to the evening when there is less staff • Planning for home starts too late (no upfront mobility plans, milestone markers, education) • No standard for interdisciplinary communication November: The value stream improvement team mapped the value stream and identified the problems December: The value stream improvement team prioritized and sequenced the work January: The Inpatient Flow Value Stream bridge site and dashboard was created (https://bridge.ohsu.edu/health/opex/IFVS/Site Pages/Home.aspx) Discharges are batched and done late in the day when there are less resources and patients waiting to get admitted. Patients stay in the hospital longer than medically necessary. Target State Safety: No increase in readmissions Quality: 80% accuracy on discharge predictions Service: Decreased ED Boarding time and batching of discharges Affordability: LOS from 6.1 days to 5.15 days, increased number of admissions Improvement Projects Next Steps February: The first 2 events will be kicked off Knight Cardiovascular Value Stream Sanjiv Kaul, Chuck Kilo, Joaquin Cigarroa, Greg Lampros, Judi Workman, Miranda Fraundorfer, Kristi Hanson Problem Statement KCVI currently functions within 8 different subspecialties, 3 clinics, and 2 inpatient care areas that are very procedure focused. Patients come into the system through a variety of entry points, and due to a lack of standards, they receive different care, which leads to silos and fragmentation. Target State To operationalize a comprehensive disease state approach when caring for patients that is driven by standardized clinical pathways, and ensures transitions of care maintain a seamless flow. This will include transitions back to the community, thereby building trust and enhancing relationships with referring providers. Initial areas of focus are: • Complex Heart Valve • Aortic • Heart Failure • Arrhythmia Success will be indicated by the following: • Improve Overall Patient Satisfaction • Increase Market Share • Increase Access • Improve Safety and Quality of Care • Be in the top 10% of hospitals for all publicly reported quality and patient safety metrics • Reduce Cost of Care by 10% Improvement Projects May‐14 ‐ KCVI Value Stream Assessment/ Mapping/ Aug‐14 Alignment Complex Heart Valve (CHV) ‐ Standardize Referral Requirements / Communication Sep‐14 CVICU ‐ Standardize Provider Documentation CHV ‐ Improve Follow‐Up Care Aortic ‐ Alignment Oct‐14 CHV ‐ Identify One Location for Evaluation Activities Nov‐14 CHV ‐ Improve Clinic / Evaluation Flow Aortic – Build Standards for Capturing Registry Data Dec‐14 CHV ‐ Standardize the Medical Review Process Jan‐15 CHV ‐ Standardize Inpatient Pathways CHV ‐ Standardize Patient / Family Feb‐15 Education Aortic ‐ Build Aortic Center Leadership & Mar‐15 Support Struture CHV ‐ Improve Pre‐Op Flow Aortic ‐ Define Aortic Inpatient Apr‐15 Management Aortic ‐ Standardize Inpatient Pathways May‐15 Aortic ‐ Standardize Referral & Surgery Scheduling Aortic ‐ Standardize the Medical Review Jun‐15 Process Jul‐15 Level Loading the KCVI Clinics Aug‐15 ‐ Complete Remaining Aortic Work Dec‐15 Initial Results South OR Value Stream (since 2012) Rayna Tuski and Randy O’Donnell Problem Target State continued… Results The patient moving through the value stream is delayed and fragmented. This is the result of non‐standard work and poor communication. 4. Standards require doing the same work the same way every time 5. Innovation comes from planning, experimenting and observing Management System Barriers surfaced & resolved, standard work confirmed, metrics reviewed, staff engaging. • • • 6. • the OPEx House) 1. Value is defined by our patients • • • 2. • Leaders facilitate learning and engaging everyone in continuous improvement Our management system fosters an environment of self accountability and self regulation Metrics Areas of Opportunity & Improvement Projects To excel at creating value, we must constantly improve • • • • 3. There is only one customer, our patient Minimal patient waiting Right patient at the right OR site We view problems as treasures and opportunities We have transparency of data and feedback, visually managed We remove barriers to performing standard work (it’s easier to do the standard than to not) For all of us to excel, each of us must learn, teach, and lead • Target State (South OR’s explanation of Work facilitated by visual cues Clear systems and standards to achieve benchmark patient experience and surgical quality Problems are opportunities: The only failure is not trying to improve • • 7. Standard work is defined and followed Timely and accurate information regarding surgical procedure, instruments, supplies, duration, special requirements; and the patient’s medical information (components of pre op check list, H&P) Efficient operations through just‐in‐time flow of personnel, materials, supplies, and equipment Level loaded Cycle times / standard work Improvement depends on standards and thoughtful innovation • • Standard work is the basis for improvement Safety of staff and patients ensured Next Steps 1. Standardize intra‐op work 2. Level Load the OR operations 3. Continue to strengthen the Daily Management System 4. Surface and address barriers Act Plan Study Do Ambulatory Services Strategic A3 Judy Carlson, Kevin O’Boyle, Stephanie Winchester Jared Davis, Gretchen Landgraf, Travis Wilds Problem Statement Areas of Opportunity OHSU Ambulatory Services consists of over 70 independent practices that strive to provide a consistent, high quality experience for our patients. Ambulatory practices suffer from a lack of standardization, alignment, and resources/tools necessary to meet the Ambulatory Strategic A3 goals. Results Practice Variation in pt flow/mgmt Press Ganey Rank Scores (Q1 FY 14‐Q2 FY 15) 0.8 Lack of training and incentives for staff 0.7 Part‐time providers Variable perspectives on practice mgmt RVU‐based reward system Managers aren't trained in PI Target State Lack of consequences for poor performers (except MIP) Hospital’s True North Goals Variation in Mgmt structures 0.4 Patients informed of wait time/delays 0.3 Practices not achieving Ambulatory A3 Breakthrough Goals FY 14‐15 Improvements Check‐in standard work Rooming Standard Work Communication of Provider wait Time Team communication of patient progression 0.2 FY14 FY14 FY14 FY14 FY15 FY15 Q1 Q2 Q3 Q4 Q1 Q2 Poor access to data/measurement systems Lack of tracking external referrals Goals Overall patient experience 0.5 Incentives through SOM Variation in readiness for change Goal = 60% 0.6 Quality support under‐resourced Two/Four Day Referral Metrics (Q1 FY14‐Q2 FY 15) Improvement work is an unfunded mandate Goal = 80% Evaluated only by budget numbers, not PI, etc 0.8 FY 14‐15 Improvements Referral Scheduling Standard Work Referral Queue Fix‐It Team Ambulatory Goals % of patients contacted by the 2nd day 0.7 0.6 % of patients appointed by the 4th day 0.5 Means to achieve the goals Practice’s Goals FY14 FY14 FY14 FY14 FY15 FY15 Q1 Q2 Q3 Q4 Q1 Q2 Improvement Projects Focus on patient experience, access, and consistent service delivery Appointment Lag (Q1, FY14‐Q2 FY15) 30 FY 14‐15 Improvements Improved Access Plan (planned) Referral Scheduling Standard Work Level Loading (planned) 25 1 Engagement • Level Loading Kaizen Rollout Strategy for FY 14‐15 • 100% practice leaders enroll in OPEx education • 100% of leaders practice Leader Standard Work 0 FY14 Q1 4 Hold Level Loading Events FY14 Q2 FY14 Q3 FY14 Q4 FY15 Q1 FY15 Q2 Next Steps 5 Roll out Referral Standard Work and SW confirmation 6 Design future state ambulatory leader plan February 7 Rollout enhanced Leader Standard Work 8 Create ED & Hospitalization Follow Up Standard Work 9 Standardize Care Management processes 10 Standardize ED, Urgent Care avoidance practices 11 GIM template improvement (Dr. Bonazzola's team) TBD Metrics Oct‐15 Dec‐15 Jun‐15 Feb‐15 Target Dates Apr‐15 Major Tasks Major Tasks Aug‐15 Safety Service Affordability Engagement Affordability • Exam Room Utilization (ex. visits per 1/2 day session or unbooked exam room) – Goal TBD • Resource Consumption – Goal TBD Goal = 14.8 Days 5 2 Develop resource consumption metric 15 10 Develop safe staffing requirement 3 Determine Level loading event calendar Access • Median Appointment Lag Time ‐ new vs. return <14 days for all practices • Practices achieve the referral metric goals at least 80% of the time: • Patient Contact (w/in 2 days of referral) • Patient Appointment (w/in 4 days of referral) Project Completed By Major Tasks Days Objectives Major Tasks Ambulatory Services A3 Goals Service • Practices consistently achieve 60% on Press Ganey Rank Scores in: • Overall Satisfaction Measure • Communication About Delays 20 Level Loading Pilot April – Diabetes and Level Loading Pilot June Endocrinology Evaluation and Center Level Loading Rollout Planning Rollout Continued Referral Ambulatory Scheduling Leader Standard Practice A3 Goal Standard Work Work Point Enhancement Define Improvement Continued Affordability and Projects Safety A3 metrics Leader Standard Roll out FY 16 Ambulatory Work Strategic A3 Enhancement August Level Loading Rollout Continued Ambulatory Practice A3 Goal Point Improvement Project TBD A3: Venous Thromboembolism (VTE) Core Measures Deborah Eldredge, PhD, RN; Dio Sumagaysay, MS, RN; Tashina Sharp, MS, RN; Cheryl Wyborny, MPH, RN Problem Statement Areas of Opportunity OHSU is performing below target (100%) on venous thromboembolism (VTE) Core Measures Results Goal – 100%, Current rate – 96% Target State To achieve 100 % on all process measures: • Pharmacologic and/or mechanical prophylaxis on patients >18 on acute & critical care nursing units • Pharmacologic overlap therapy for 5 days in patients with confirmed VTE and/or pulmonary embolism (PE) • Written instructions provided to patients with confirmed VTE at discharge including: compliance, dietary advice, follow‐up monitoring and drug ‐ drug interactions To sustain 0% on outcome measure: • Preventative pharmacologic and/or mechanical prophylaxis was administered to patients prior to incurring VTE /PE during hospitalization VTE Composite 100% 90% 80% 70% 60% 50% Improvement Projects • Nursing and clinical technology to collaborate to reduce sequential compression device (SCD) breakage. • Nursing and Operational Effectiveness to ensure all RNs and CNAs complete Compass training of VTE prevention. • Epic workflow analyst to partner with workgroup to identify, build and implement decision support. • Nursing Informatics to modify VTE prevention dropdown menu options in Epic to support timely and effective documentation of applying SCDs. Next Steps Provide education on VTE prevention to all staff and physicians involved in the care and treatment of patients >18. Leverage Epic to support VTE prevention documentation. Make sure adequate numbers of properly functioning SCDs are available on the nursing units. Continue to monitor performance and provide feedback to staff and physicians when evidence based practice is not followed. Surgical Site Infection Prevention Dr. Renee Edwards, Dr. Daniel Herzig Brenda Quint‐Gaebel, Gretchen Landgraf Problem Statement Areas of Opportunity OHSU’s number one goal in the Clinical Enterprise Strategic Plan is to achieve a top 10 ranking in the University HealthSystem Consortium (UHC). Currently, it is ranked 27/73 with respect to Surgical Site Infection (SSI) rates for colon and abdominal hysterectomy surgeries with a Standardized Infection Ratio (SIR)* of 0.75. Variation in pt. prep (PMC) Batched SSI data from lab Standard bowel prep Pre‐op and Intra‐op skin prep Antibiotic selection, dosing, and discontinuation Colon & Abd Hyst SSI rate higher than UHC top 10 goal Nursing variability in practice High BMI *Standardized Infection Ratio = Observed SSIs Expected SSIs # of SSIs 2 1 1.82 0 Q1‐2013 2.22 1.82 0 0 1 2 Q2‐2013 Q3‐2013 Q4‐2013 # of SSIs 1.89 1 Q1‐2014 10.0 9.0 8.0 7.0 6.0 5.0 4.0 3.0 2.0 1.0 0.0 S S I R A T E OHSU Adult & Peds Colon SSIs (Q1, 2013 ‐ Q2, 2014) 10 10.00 8.65 9 9.00 8 8.00 6.48 # of SSIs 7 6 5.56 7.00 5.45 6.00 4.65 5 5.00 3.41 4 3 3.00 2 1 4.00 2.00 7 7 6 4 9 3 Q1‐2013 Q2‐2013 Q3‐2013 Q4‐2013 Q1‐2014 Q2‐2014 0 S S I R A T E 1.00 0.00 # of SSIs Focus on standardizing best practices in pre‐, intra‐, and post‐op phases of care Improvement Projects Pre-Op (PMC or Surgery Clinic or Inpatient Unit) Q2‐2014 SSI Rate • Pt. skin cleansing • Glycemic Management • Standard Bowel Prep (13y.o.+) Pre-Op (6A, day of surgery) • Pt. Skin Cleansing • Glycemic Management • Patient Warming • Antibiotic prophylaxis prep Intra-Op • Standard wound care • Glycemic Management -TBD • Patient Warming • Standard Antibiotic prophylaxis • Clean/Dirty Instrument Separation SSI Rate Target State • SSI SIR < 0.37 for patients undergoing colon and abdominal hysterectomy surgeries • Be among the top 10 UHC institutions • Standardize community best practices for SSI prevention Standardize: Patient Skin Cleansing with CHG Bowel Prep Periop Glycemic Management Antibiotic Prophylaxis Wound Care Patient Warming SSI Surveillance and Case Review • Surgeons received individual SSI rates • Case reviews & learnings shared with surgeons, Anesthesiology and nursing staff. • Surgeons, nursing, anesthesia providers support establishing an SSI prevention bundle Q3‐Q4, 2014 SSI rates to be reported in early 2015 Variable pt. flow to OR OHSU Abd Hyst SSIs (Q1, 2013‐Q2, 2014) 3 Results Post-Op (PACU + Ward+ Surgery Clinic) • Standard wound care • Glycemic Management - TBD • Patient Warming • SSI Surveillance and Case Review Next Steps 1. Concurrent monitoring of bundle compliance 2. Earlier identification of SSI cases 3. Home wound care – Case Management 4. Periop Glycemic management implementation (see graphic below) Iatrogenic Pneumothorax Strategic A3 Project Nancy McCully, MSN, MBA, RN, CCRN; Erin Reback, RN Hai Molinaro, Brenda Quint‐Gaebel and Matthias Merkel, MD PhD Problem Statement Improvement Projects Results (continued…) University Healthcare Consortium (UHC) data demonstrated that our patients were exhibiting a higher rate of Iatrogenic Pneumothorax (I‐ PTX) as compared to our Top 10 UHC peers. We recognize that I‐PTX will increase length of stay, increase tests/interventions, can lead to more complications, and decrease patient satisfaction. • Assure compliance with new Central Venous Catheter Placement and Follow‐up Policy • Standardize documentation for central venous catheter (CVC) placement and Dobhoff tube (DHT) placement • Require CVC training for new LIPs and for LIPs with low CVC placements • Standardize DHT placement • Implement algorithm for care escalation for difficult DHT placement • Standardized access approach in EP lab • Proactively identify preventive measures for surgical procedures Implemented hospital‐wide standards and expectations for staff training in central venous catheter (CVC) placement and Dobhoff tube (DHT) placement • Simulation training for central line placement expanded to include APP and faculty • Algorithm for site selection of CVC insertion reducing subclavian vein catheterization • Algorithm for escalation of difficult feeding tube placement • Standard documentation of CVC placement to promote standard workflow and improved data tracking Results Next Steps Target State To achieve UHC Top 10 status, we must have a less than 0.1 incidence rate of reportable I‐PTX. Areas of Opportunity A drilldown of the UHC reportable cases of Iatrogenic Pneumothorax for FY12, FY13, and FY14 YTD show the following causes: 1. Central Venous Catheter (CVC) placement: the number subclavian lines placed were one‐tenth the number of internal jugular lines placed with double the incidence rate, poor documentation of placement 2. Dobhoff tube (DHT) placement: poor documentation of placement and number of attempts, multiple placement attempts, escalation process unclear for multiple failed attempts. 3. Pacemaker / ICD Placement: lack of standardization in training of fellows, multiple placement attempts 4. Surgical procedures: entering the pleural space during surgery due to increased complexity or unanticipated complication Implemented standard for training fellows in pacemaker placement 0.1 Implemented Central Venous Catheter Policy • Roll out Risk Stratification Tool and Consultation Protocol for DHT placement • Continue to refine standards for CVC placement and DHT placement as these standards become more widely adopted at OHSU • Epic Documentation of OG/NG/NJ Procedure note for DHT placement and DHT LDA • Establish training program for US‐guided SC vein cannulation • Continue to work with surgical teams on rare surgery‐specific I‐PTX • Ongoing monitoring of reportable UHC I‐PTX cases • Monitor staff compliance with policies and protocols A3: Perioperative Hemorrhage & Hematoma Paul Flint, Ericka Mitchell, Karoly Crawford, Dan Kenron Problem Statement Improvement Projects To achieve UHC Top 10 performance in the AHRQ Patient Safety Indicator – Perioperative Hemorrhage & Hematoma (PSI‐09). Documentation & Coding ‐ Disconnect between documentation and coding: define what constitutes a “hemorrhage” or “hematoma” Target State To reach the UHC target, OHSU must have 5 or fewer Hemorrhage/Hematoma events per month (15/quarter) to achieve the quarterly target of 7.4 per 1000. To achieve UHC Top 10 standing, OHSU must have less than 1.6/1000 events per month (4.8/quarter) to achieve a O/E ratio of 0.60 Areas of Opportunity Root cause analysis led to focusing on three areas of opportunity: • Documentation and coding • Early vs. Delayed Hemorrhages • Postoperative pain control ‐ Documenting planned re‐ operations for bleeding and clear relation to primary procedure Results Next Steps Revision of Univ. of Michigan Health System’s Guidelines for Coding Postoperative Complications (2011). Used with permission. Postoperative pain control ‐ Establish pain control for Otolaryngology patients ‐ hypertension due to uncontrolled pain increases chance for hemorrhage • Continue to track instances of Peri‐op hemorrhage/ hematoma • Establish workflows for prospective (before UHC submission) of Peri‐op hemorrhage/ hematoma cases • Understand emerging trend in hysterectomy surgeries and hemorrhage/hematoma A3: Postoperative Respiratory Failure Matthias Merkel, Christopher Dodgion, Dan Kenron, Jennifer Watters, Karoly Crawford, Michelle Dedeo, Paul Lopinski, Stephanie Nonas Problem Statement Areas of Opportunity To achieve UHC Top 10 performance in the AHRQ Patient Safety Indicator ‐ Postoperative Respiratory Failure measure (PS‐‐11). Intraoperative Ventilation ‐ Tidal volume per body weight settings not <=8mL/kg ‐ PEEP settings ≤ 5 ‐ Ideal body weight documentation Target State Ventilation wean ‐ Spontaneous Breathing Trial not performed To reach the UHC Target, OHSU must have fewer than 6 Respiratory Failure events per month (18/quarter) to achieve the quarterly target of 16 per 1000. Documentation & Coding ‐ Disconnect between documentation and coding ‐ copy forward of progress notes ‐ definition of diagnoses ‐ Smartphrase in Epic does not have correct language ‐ Lack of education: proper documentation for proper coding To achieve UHC Top 10 standing, OHSU must have fewer than 2.5 events per month to achieve a O/E ratio of 0.49; quarterly, this target is 9 per 1000. Sedation used ‐ Intra‐operative ‐ Post‐operative ‐ Daily sedation hold not occurring Improvement Projects • Validation work queue for proactive Quality Specialist review • MD review team for case review • Spontaneous Breathing Trails (SBT) & Epic improvements • Understand & Track reasons for failure • Documentation handbook to define “respiratory failure” • Collaboration with Coding on PSI‐09 measure Results Clinical review of Occurrences Next Steps 1. 2. 3. 4. 5. 6. Present to All‐Hill ICU M&M on Jan 21st Continue to work with RT to improve SBT trials Improve data integration in Epic with ICU Navigator Be perfect: no patient outside of 90% O2 Case review by ICU Fellows and vent patients discussed at huddles Reporting on continued success at M&Ms Kaizen [ kahy‐ZEN ] What is a Kaizen? Kaizen is a Japanese word meaning “good change” and often used to communicate “continuous improvement.” A Kaizen Event is a performance improvement event lasting anywhere from several hours to several days to continuously improve processes. It requires involvement from all levels of workers. No matter the size, the same problem solving steps are completed Phases of Kaizen Events Assessment Planning Refine Refine Assessment Planning Act Plan Act Plan Study Do Study Do Evaluate Sustain Kaizen Event Evaluate Sustain Kaizen Event The Improvement Process Encountered Current State Improved State Obstacle Perfection Understand and overcome Assess, Plan Discovery, Design, Implement Kaizen Event Leading up to the Kaizen Event, there is an assessment of the current state and planning of the event. The yellow signifies that we go slow with assessing the current state so that we can go fast with the improvement. How is OHSU using Kaizen Events? • OHSU has been using and learning about Kaizen Events as an improvement method since 2011 • Kaizen Events are conducted: o 1/mo per value stream ( 48/ year) o Across ambulatory care o On hospital units (HAI Reduction, Patient Experience Improvement, Lunches & Breaks, Documentation & Coding, Supply Outdates, Clinical Alarm Safety) o Unit/Department-specific (Mother Baby Unit Length of Stay, Interventional Recovery Unit Scheduling, Labor & Delivery C-section improvement, GI Patient Flow o Various 5S events Check out posters explaining OPEx, Daily Management System, 5S, Leader Standard Work & Value Streams. Looking With New Eyes… At Things That Can’t Be Seen Preventing Healthcare Acquired Infections at OHSU HAI KAIZEN UNITS Problem Statement Areas of Opportunity Healthcare Associated Infections 4th Leading Cause of Death “There is no more vulnerable population than the hospital patient, who is terrified of acquiring a hospital infection, yet powerless to avoid it. Making us aware of your concerns, and letting us know that you follow clear, consistent hygiene procedures, shows us you care. It helps make us a part of the team. It lets us know you acknowledge there is a serious issue, and you are working to fix it.” ~OHSU Patient Target State: • Achieve or maintain ZERO Healthcare Associated Infections • Create a Culture of Safety • Improve Team Communication & Collaboration Improvement Projects Results: HAI Kaizen Units: “You can feel the culture and engagement of the team members in protecting our vulnerable patients by improving processes.” Infection Preventionist, after rounding @ OHSU Weekly Interdisciplinary Improvement Huddles • Celebrating successes with implementing standard work that prevents infections • Identifying variations in practices that put vulnerable patients at risk • Planning rapid cycle improvement steps Healthcare Infection Prevention Champions leading team members in early identification of patients who have gotten an HAI , thus facilitating early treatment “I’ve Got Your Back” Team members speaking up to keep each other safe:… Ask a question Make a Request Express Concern Chain of Resolution Over 60 Interdisciplinary Case Reviews have identified issues for focused improvement: • Inconsistent bathing & perineal care • Inconsistent documentation raises concerns about consistency of care Next Steps • HAI Kaizen Spread to all inpatient units • More units being transparent in acknowledging to patients when an HAI occurs and committing to them to continue to fix any issue. Daily Management Systems Tiered Huddle Structure Standardize and Improve Ongoing Improvement Efforts Principles • Design work to surface problems as they occur • Develop problem‐solving capabilities • Create and follow leader standard work 1. 1. Escalation Process a. Introduced blue dot to distinguish between issues that need to be escalated and those that do not b. Added tracking to Big Issues that are escalated in order to ensure closed‐loop feedback Leader Standard Work (LSW) a. Empowering the leadership structure to support DMS b. Helping better utilize time, set priorities, and align goals Key Elements 1. Run the Operation 2. Standardize and Improve 3. Leader Standard Work c. See LSW poster for more details 2. 2. Expanding MESS to include Patient Experience and Safety a. Identification of patient experience risks and determination of appropriate countermeasures b. Shifting safety focus from occurrences to risks in order to help prevent occurrences before they happen Pre‐DMS Culture Maturing DMS Culture Problems described as vague issues A problem described as a specific gap from standard No trigger to indicate a problem Signal occurs when an obstacle will keep standard work from being completed Staff reluctant to say there’s a problem Workarounds common Poor Staff readily surface problems without fear of blame Rapid PDSA cycles resolve problems Excellent 3. Addition of Metric Tracking and Review a. Adding review of previous day’s performance to daily huddles b. Introducing weekly metric reviews to drive improvement Expansion of Metric Reviews a. Continuing to develop reviews of key performance metrics b. Linking daily activities and improvement efforts to overall institutional goals 3. Problem Solving a. Utilizing a structured problem solving methodology to tackle big problems b. Driving to real root cause in order to ensure problems do no reoccur Leader Standard Work Hue Chiang & Evan Durant Problem Statement Areas of Opportunity Creating a lean culture requires a management system to sustain it and ensure continuous improvement. Lean leaders must understand and support the work at gemba (Japanese for “the real place” – where the work is done). • • • • • Reduce number of meetings Improve meeting effectiveness Use gemba time more efficiently Increase visibility of priorities Facilitate communication among all levels Results • Visual leader standard work tools created and in use • Regular reviews and discussions about priorities and barriers • Identification of opportunities to improve However, there are many obstacles to providing effective, gemba‐based leadership – including external demands on leaders’ time, competing priorities, and firefighting. Target State • • • • • Clear expectations and follow‐up by leaders Alignment of goals at all levels Prioritization of competing activities Leadership at gemba Continuous improvement Improvement Projects • Scheduled and on‐demand leader standard work classes and workshops • Leaders trained at all levels • Supervisors • Managers • Directors • Executives • Leader standard work rounding to ensure effectiveness and alignment Next Steps • Broader deployment throughout the institution • Training classes scheduled every month throughout 2015 • Continued learning and refinement of practices GME Optimization Patrick Brunett, MD, FACEP, Kim Irish, MS, CPHQ, Alison Lord, Hai Molinaro, Traci Rieckmann, PhD Target State Root Cause Analysis OHSU's Graduate Medical Education Division (GME) strives to continuously improve the clinical learning environment and the training provided to all residents and fellows, and to surpass accreditation standards of the ACGME while fulfilling the current and future healthcare needs of Oregon and beyond. To accomplish this mission , OHSU GME and Quality Management teams joined in an optimization process aligned with quality improvement and OHSU OPEx methodology. Lack of Data • Correlating post‐OHSU training placement and geographic needs in Oregon • Employer satisfaction with residents’ competency post‐graduation • Aggregate data from ACGME not utilized or available to programs; insufficient flow of data from GME to programs and programs back to GME; poor capacity to aggregate data and reflect back to individual programs • Lack of IT infrastructure and personnel Areas of Opportunity Lack of Standard Process At our first session in October 2014, GME Program • No standard process or timeline for providing Directors identified nine areas of opportunity: resident and faculty feedback after assignments Outcomes: Lack of Resources and Incentives 1) Providers matched to geographic and specialty • Educational activity not valued/rewarded by needs of Oregon’s communities OHSU post‐training OHSU 2)Employer survey demonstrating competency and • Resources for faculty development are not satisfaction with graduates available or readily accessible Resident Experience: Above National Mean or 4.0 (whichever is higher) for the following ACGME Improvement Projects Resident AND correlating Faculty Survey questions: 3) Resident satisfied with post‐assignment feedback At our second session in January 2015, the / Faculty satisfied with personal performance following projects were prioritized to work on over feedback the next six months: 4) Information (not) lost during shift changes and patient transfers #1: Improving faculty development opportunities, Resident Progression Performance: including enhanced skills for providing feedback to 5) Milestones Assessment and Achievement residents. 6) Individual Academic Advancement Plan Tracking Program Director/Faculty Development: #2: Employer and graduate surveys demonstrating 7) Participation in faculty development graduate competency and satisfaction with training 8) Collaboration and spread of best practices and assuring providers are matched with the needs 9) Collaboration and spread of innovation of Oregon communities. Rationale for Current Year’s Activities • To improve resident experience and outcomes, we will need to standardize and improve resident/faculty feedback after assignments and provide faculty development opportunities, including feedback given to residents. • We will also need to standardize the way that employers and graduates are surveyed regarding competency and satisfaction with their training across GME programs. This will help us determine if graduates are being hired into practice environments that are aligned with the needs of Oregon communities. Next Steps Faculty Development and Resident/Faculty Feedback • Conduct needs assessments for faculty development in resident feedback skills • Compile and validate best practices in feedback for both learner and faculty • Design faculty development tools and training plan for providing feedback Graduate and Employer Survey • Develop, implement and track both graduate and employer surveys • Establish a process for utilization of survey results in sustained program improvement This innovative work provides an opportunity for medical education and quality management to both develop efficacious partnership models and disseminate those findings nationally. UHC Quality and Accountability Scorecard Goal 1 of OHSU’s Clinical Enterprise Strategic Plan is to be a national leader in clinical quality, patient safety, and patient experience. Our 2014 Scorecard showed improvement with our overall ranking going from #41 in 2013 to #27 in 2014. Safety Success will be measured by scoring in the Top 10 of the University HealthSystem Consortium’s Quality and Accountability Scorecard Patient Centeredness Our 2014 Domain Rankings Mortality Effectiveness Safety Equity Pt. Centeredness Efficiency 39 23 25 1 46 67 We focused our 2014 improvement work in three domains (Effectiveness, Safety, and Patient Centeredness) and saw significant gains. Effectiveness Our Work for 2015 • We will continue our work to get into the Top 10 ranking for Effectiveness, Safety, and Patient Centeredness. • In 2014, we saw our rankings slip in Mortality and Efficiency. • For Mortality, areas of opportunity include transfers, sepsis, and coding/documentation. • For Efficiency, we will look at improvement opportunities related to length of stay and cost.