Axillary Intra-aortic Balloon Pump Placement as a Means for Safe
advertisement

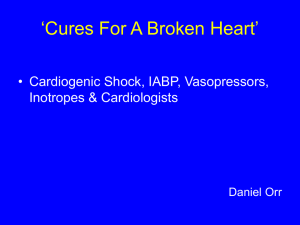
CASE REPORT Axillary Intra-aortic Balloon Pump Placement as a Means for Safe Mobility in a Patient Awaiting Left Ventricular Assist Device Implantation: A Case Report Kara Marie Shumock, PT, DPT; Jessica Appel, PT, DPT; Amy Toonstra PT, DPT Department of Physical Medicine and Rehabilitation, The Johns Hopkins Hospital, Baltimore, MD Introduction: Although there is no cure for heart failure, placement of an intra-aortic balloon pump (IABP) can act as temporary treatment. Historically, IABPs are inserted through the femoral artery and patients are placed on bed rest. The purpose of this case report was to demonstrate the physical therapy management of a patient with IABP catheter placement through axillary artery, including safe ambulation. Case Presentation: A 54-yearold South Asian man presented with profound cardiogenic shock. He had prolonged hospital course complicated by several femoral IABP placements, extracorporeal membrane oxygenation, and mechanical ventilation. He eventually received axillary IABP placement to allow for increased mobility. The patient was able to ambulate up to 182.88 m with a rolling walker while the axillary IABP was in place before left ventricular assist device placement, which occurred on hospital day 40. Conclusions: Physical therapy interventions, including functional mobility and gait training, were safely performed in a patient with axillary IABP access. However, additional studies are needed to support mobility as standard practice for this patient population. (Cardiopulm Phys Ther J. 2015;26:53–57) Key Words: intra-aortic balloon pump, physical therapy, mobility INTRODUCTION Heart failure (HF) is a common medical condition that affects approximately 5.1 million people in the United States.1 There is no cure for HF; however, a variety of treatment options exist including medication, lifestyle adjustments, surgical intervention, and heart transplantation.1 Advanced HF may require patients to remain hospitalized for medical management or while awaiting further treatment options such as surgery. Due to the deconditioning effects of HF, physical therapists (PTs) in the acute care setting are likely to encounter these patients at various stages of the disease. Copyright © 2015 Cardiovascular and Pulmonary Section, APTA Correspondence: Kara Marie Shumock, PT, DPT, Department of Physical Medicine and Rehabilitation, The Johns Hopkins Hospital, 1800 Orleans Street, Meyer-2 109, Baltimore, MD 21287 (kara.shumock@gmail.com). The authors declare no conflict of interest. DOI: 10.1097/CPT.0000000000000010 Cardiopulmonary Physical Therapy Journal One temporary treatment for HF is placement of an intraaortic balloon pump (IABP).2 An IABP provides cardiovascular support in 2 ways: it maximizes coronary perfusion and increases cardiac output by reducing left ventricular afterload.3,4 This device is traditionally inserted through the femoral artery and is positioned in the aorta; however, this approach greatly restricts mobility.2,4 If the patient does not tolerate weaning of the IABP, the patient must often remain on bed rest while awaiting a more definitive intervention, such as left ventricular assist device (LVAD) placement or cardiac transplant. In addition to decreased mobility, femoral IABP placement carries other limitations including risk of infection.5 An alternative placement of the IABP in the axillary artery allows the patient to mobilize out of bed and continue working with physical therapy while supported by the IABP.5 Current literature suggests that axillary placement of an IABP provides excellent support to patients while awaiting transplant with few adverse effects.5 In a patient population predisposed to physical deconditioning, strict bed rest, such as that associated Axillary Intra-aortic Balloon Pump Placement 53 Copyright Ó 2015 by the Cardiovascular and Pulmonary Section, APTA. Unauthorized reproduction of this article is prohibited. with femoral IABP placement, is detrimental to the musculoskeletal system.6 Immobility associated with bed rest has been linked to intensive care unit (ICU) acquired weakness.7 Bed rest has also been associated with other complications such as hypotension, dehydration, decreased lung functioning, and increased risk of deep vein thrombosis.8 Physical therapists play an important role in preventing these negative consequences through early assessment and development of an individualized patient plan of care to meet functional goals.9 Early mobility has been shown to decrease ICU and hospital length of stay and improve functional outcomes at discharge.10,11 To optimize function and reduce complications, PTs are a vital part of mobilization. Physical therapists typically play a smaller role in patients with femoral IABP providing limited bed-level exercises. However, in patients with axillary IABP, the role of PTs expands to include creation of individualized plans of care based on patient impairment and goals. Skilled care also includes continual assessment of response to interventions and progression of safe mobility. Despite the benefits of axillary IABP, this alternative placement is underused in cardiac ICUs. To the authors’ knowledge, there is no current literature surrounding the development, initiation, and management of a physical therapy plan of care with patients who have axillary IABPs. We are reporting on this patient’s case study to highlight the benefits of axillary IABP placement in a patient with complex end-stage HF. Given the limited research available, our aim was to focus on the management and feasibility for participation in mobility with physical therapy and nursing in a complex critically ill patient with an IABP through axillary artery. supine in bed with the head of bed elevated no more than 30° and the involved limb extended. An occupational therapist evaluated the patient on HD 21 and issued him a bed-level exercise program. A physical therapy evaluation was performed on HD 23 after axillary IABP placement. The patient was hemodynamically stable at this time (Table 1). Upon observation, the patient had right axillary IABP access with continuous monitoring, telemetry, a peripheral intravenous line, and a Foley catheter. He was alert and oriented to person, place, and time, and was also able to follow 3-step commands. The patient had 4/5 strength grossly in his bilateral lower extremities and left upper extremity. Formal manual muscle testing with resistance was not provided to the right upper extremity due to the sensitivity of the IABP access point. The patient’s range of motion, sensation, and pulmonary status were within normal limits. Moderate (21) edema was found in his bilateral upper and lower extremities. The patient was taking opioid medication to control tenderness and radiating right shoulder pain. Additional notable medications include angiotensinconverting enzyme inhibitor, P2Y12 platelet inhibitor, statin, loop diuretic, anticoagulant, antihypertensive, insulin, nitrate vasodilator, magnesium sulfate, potassium chloride, phenothiazine, and selective serotonin reuptake inhibitor. Relevant laboratory values included point of care glucose 156 to 176 mg/dL, blood urea nitrogen 30 mg/dL, creatinine 1.7 mg/dL, red blood cells 3.19 M/mm3, hemoglobin 8.8 g/dL, hematocrit 28.3%, international normalized ratio 1.2, and activated partial thromboplastin time 48.3 to 59.3 seconds. CLINICAL IMPRESSION CASE PRESENTATION A 54-year-old South Asian man with a history of diabetes, hypertension, peripheral venous insufficiency, peripheral neuropathy, and cardiac arrhythmias presented with profound cardiogenic shock. He was admitted to a 12-bed ICU in a large tertiary hospital and was found to have ST elevated myocardial infarction with peak troponin at .102.00 ng/mL. Echocardiography revealed an ejection fraction of 5% to 10%. Due to multivessel disease and the inability to revascularize the left anterior descending coronary artery, the patient was considered for an emergent coronary artery bypass graft; however, he was not medically stable enough to tolerate surgery, so a femoral IABP was placed. The patient developed respiratory and circulatory failure resulting in intubation, extracorporeal membrane oxygenation, percutaneous coronary intervention, and multiple reinsertions of a femoral IABP throughout his ICU stay. On hospital day (HD) 22, the femoral IABP was removed and reinserted through axillary artery to permit mobility. INITIAL EXAMINATION (HOSPITAL DAY 23) At this hospital, patients with femoral access IABP are not eligible for out-of-bed mobility. Patients must remain 54 Shumock et al In light of the patient’s recent axillary IABP line placement and deconditioned state, the interdisciplinary team set a mobility goal of transferring to the chair for the initial physical therapy session/evaluation. Goals for physical therapy were developed based on his functional baseline and personal goals, which included independence for all transfers, ambulation, and stair navigation. Physical therapy interventions focused on preventing deconditioning and weakness in anticipation of a prolonged hospital course. Given the patient’s hemodynamic stability and tolerance to upright posturing in the chair, the interdisciplinary team cleared the patient for ambulation on HD 26. Nursing assisted in ambulation by managing the wheeled IABP monitor and IV pole, whereas the PT provided guarding and assistance to the patient who was using a rolling walker (Fig. 1). Both nursing and the PT monitored the patient’s vitals with particular focus on mean arterial pressure (MAP) and heart rate (HR) as read on the IABP monitor, as well as physical appearance for signs of exercise intolerance, such as shortness of breath, during all mobility activities. Eventually, to progress the patient’s endurance and functional mobility, he was encouraged to ambulate once with the PT and once with nursing daily. Cardiopulmonary Physical Therapy Journal Copyright Ó 2015 by the Cardiovascular and Pulmonary Section, APTA. Unauthorized reproduction of this article is prohibited. TABLE 1 Cardiopulmonary Response to Physical Therapy Interventions and Associated Percentage of Disability HD Ambulation Distance and Assistance Required 23 OOB to chair with min A 25 26 27 28 29 30 33 Preintervention Vital Signs Postintervention Vital Signs AM-PAC (% Disability) BP: 87/55 mm Hg HR: 123 beats per minute SpO2: 93% OOB to chair with min A BP: 85/43 mm Hg MAP: 79 mm Hg HR: 116 beats per minute RR: 35 breaths per minute SpO2: 98% 2.44 m with min A/HHA BP: 91/55 mm Hg HR: 108 beats per minute SpO2: 93% 12.19 m with min A BP: 94/64 mm Hg HR: 109 beats per minute RR: 27 breaths per minute SpO2: 100% 27.43 m with min A using rolling walker BP: 80/53 mm Hg MAP: 77 mm Hg HR: 104 beats per minute RR: 22 breaths per minute 60.96 m with min A using rolling walker BP: 93/63 mm Hg MAP: 93 mm Hg HR: 103 beats per minute RR: 29 breaths per minute SpO2: 100% 60.96 m with CGA using rolling walker BP: 85/51 mm Hg MAP: 74 mm Hg HR: 104 beats per minute 182.88 m with S/SBA using rolling BP: 91/54 mm Hg walker MAP: 88 mm Hg HR: 103 beats per minute SpO2: 100% BP: 86/53 mm Hg HR: 127 beats per minute SpO2: 94% BP: 100/62 mm Hg MAP: 93 mm Hg HR: 113 beats per minute RR: 35 breaths per minute SpO2: 96% BP: 89/52 mm Hg HR: 110 beats per minute SpO2: 94% BP: 98/61 mm Hg HR: 104 beats per minute RR: 32 breaths per minute SpO2: 100% BP: 83/50 mm Hg MAP: 81 mm Hg HR: 97 beats per minute RR: 26 breaths per minute BP: 92/56 mm Hg MAP: 88 mm Hg HR: 103 beats per minute RR: 26 breaths per minute SpO2: 95% BP: 84/51 mm Hg MAP: 76 mm Hg HR: 104 beats per minute BP: 100/68 mm Hg 57.70% 54.16% 50.57% 50.57% 50.57% 50.57% 50.57% 50.57% MAP: 95 mm Hg HR: 106 beats per minute SpO2: 100% The patient’s vital signs were stable throughout all treatments, including when the patient was symptomatic. The patient was on room air during all physical therapist sessions. Vitals not listed in the table were not reported in the patient’s medical chart. Abbreviations: AM-PAC, Activity Measure for Post-Acute Care; BP, blood pressure; CGA, contact guard assist; HD, hospital day; HHA, handheld assist; HR, heart rate; MAP, mean arterial pressure; min A, minimal assistance; OOB, out of bed; RR, respiratory rate; S, supervision; SBA, stand by assist; SpO2, saturation of peripheral oxygen. Activity Measure for Post-Acute Care (AM-PAC) 6-Clicks basic mobility scale was used to measure function during each physical therapy session. This instrument includes 6 questions regarding patient’s functional mobility in the hospital.12 The therapist scores each activity from 1 (unable or total assist) to 4 (no assistance needed), and the sum of these scores creates the raw score, which can then be standardized to a T-score.12 The intraclass correlation coefficient is 0.849 (95% confidence interval) for the overall interrater reliability of the basic mobility scale.12 Evidence regarding the validity of this scale has Cardiopulmonary Physical Therapy Journal also been discussed by Jette et al.13 Table 1 displays the patient’s AM-PAC 6-Clicks basic mobility scale as a percentage of disability throughout the hospital stay. A higher percentage indicates a higher level of disability. INTERVENTION The PTs incorporated the following therapeutic interventions into the plan of care: transfer training, gait training, balance training, endurance training, and therapeutic exercises. The patient’s cardiopulmonary response Axillary Intra-aortic Balloon Pump Placement 55 Copyright Ó 2015 by the Cardiovascular and Pulmonary Section, APTA. Unauthorized reproduction of this article is prohibited. vitals during all physical therapy sessions. Given that the patient was on numerous medications affecting hemodynamics and was critically ill, hemodynamic parameters were established with the medical team to ensure patient safety during physical therapy interventions. These included MAP .65 mm Hg, HR ,130 beats per minute, orthostatic hypotension as evidenced by drop in systolic blood pressure (BP) of .20 mm Hg and drop in diastolic BP of .10 mm Hg, symptomatic dizziness or light-headedness, and clinical signs of decreased cardiac output. In the instance of any of these events, physical therapy would have stopped or been modified until hemodynamic stability returned. Measures were taken by the PTs to prevent any of these potential physiological abnormalities and included review of laboratory values and vital signs before start of physical therapy and continuous hemodynamic monitoring, including MAP measurements with position changes. PATIENT OUTCOMES Fig. 1. Patient ambulating with rolling walker while attached to multiple lines, including intra-aortic balloon pump monitor, with assistance from the physical therapist. This figure is available in color in the article on the journal website (journals.lww.com/cptj). to physical therapy interventions can be seen in Table 1. On HD 23, the patient was able to perform supine to/from sit, sit to/from stand, and bed-to-chair transfers with minimal assistance and standing for 2 minutes. The patient’s vital signs were only notable for a resting HR in the 120s, which remained stable throughout the therapy session. A personalized exercise program was initiated for further progression of strength outside of physical therapy sessions. On HD 25, mobility was limited by symptoms of light-headedness and nausea. Light-headedness was not position dependent, and vital signs remained stable during bed-to-chair transfer, which required minimal assistance. On HD 26, the patient required supervision for supine to sit, minimal assistance for sit to/from stand transfers, and was able to progress his exercise program further. The patient ambulated 2.44 m to a chair with minimal assistance at hips and handheld assistance on the left from the PT. On HD 27, the patient ambulated 12.19 m and continued to progress his exercise program to address strength and endurance deficits. On HD 28 to 30, the patient was able to progress ambulation distance from 27.43 m with minimal assistance to 60.96 m with contact guard assistance while using a rolling walker. During this time, balance activities were also initiated. On HD 33, he ambulated 182.88 m with supervision using a rolling walker. The patient had stable 56 Shumock et al The patient had LVAD placement as destination therapy on HD 40. Physical therapy continued after LVAD placement and included interventions such as transfer training, gait training, therapeutic exercises, more advanced balance activities, endurance, and LVAD management training. The patient’s AM-PAC score decreased from 68.66% disability on HD 41 to 46.58% disability on HD 58. The patient was discharged to home on HD 59 with a recommendation for home physical therapy as a bridge to phase II cardiac rehabilitation. DISCUSSION The benefits of early mobility over bed rest are widely known. Prolonged bed rest leads to muscle wasting, weakness, and ICU-acquired myopathy.7 In a healthy individual, bed rest can lead to a 4% to 5% decrease in maximum voluntary force in knee extensor muscles per week.14 At this hospital, patients with femoral IABP insertion are on flat bed rest until removal of the device. They are permitted to partake in bed-level exercise involving uninvolved limbs, which nursing primarily performs with the patient. The patient in this case study had axillary IABP access for 18 days, which allowed him greater freedom to participate in higher level mobility, including ambulation, during a time where he would have been bed bound, thus avoiding the deleterious effects of prolonged bed rest. To mobilize the patient safely, nursing was involved in treatment sessions to assist with equipment management and monitoring of vital signs. The PT was available to guard the patient and provide skilled feedback, as well as develop and modify a treatment plan to address the patient’s functional impairments while nursing managed the portable IABP monitor, which continuously reported BP, MAP, and HR. Physical therapists play a specific role in evaluation of body systems, development of individualized plans of care, management of lines/equipment for mobility, and use of clinical judgment surrounding safe exercise parameters with Cardiopulmonary Physical Therapy Journal Copyright Ó 2015 by the Cardiovascular and Pulmonary Section, APTA. Unauthorized reproduction of this article is prohibited. critically ill patients to maximize functional strength and endurance during hospitalization.9,15 The interventions chosen for this patient were aimed to improve mobility, balance, and endurance to prevent deconditioning and work toward maintaining functional strength for discharge home. The AM-PAC was used as an outcome measure to track percentage of disability throughout the hospital stay. Walking distance was also recorded to track objective improvements in endurance. CONCLUSIONS Axillary IABP placement has few adverse effects, decreases the risk of infection, and allows for patient mobility, thus preventing secondary complications from bed rest.5 This case study demonstrates safe and feasible mobility for a patient with axillary IABP placement. This was the first patient mobilized with axillary IABP placement at this hospital. Further research should focus on comparing functional outcomes of patients awaiting destination therapy who are on bed rest with femoral access IABP and those patients who are able to mobilize with axillary access IABP. ACKNOWLEDGMENTS The authors would like to thank our patient for allowing us to use his hospital course for the basis of this case report. They would also like to recognize Gabrielle Steinhorn, PT, DPT, NCS, and Paul Ricard, PT, DPT, CCS, for their guidance and critical review of this case report. Written patient consent was received for publication of this case report. REFERENCES 1. What is Heart Failure? NIH: National Heart, Lung and Blood Institute Website. 2014. http://www.nhlbi.nih.gov/health/health-topics/topics/hf/. Accessed October 21, 2014. Cardiopulmonary Physical Therapy Journal 2. Estep JD, Cordero-Reyes AM, Bhimaraj A, et al. Percutaneous placement of an intra-aortic balloon pump in the left axillary/ subclavian position provides safe, ambulatory long-term support as bridge to heart transplantation. JACC Heart Fail. 2013;1(5):382–388. 3. Peura JL, Colvin-Adams M, Francis GS, et al. Recommendations for the use of mechanical circulatory support: Device strategies and patient selection: A scientific statement from the American Heart Association. Circulation. 2012;126:2648–2667. 4. Macauley K. Physical therapy management of two patients with stage D heart failure in the cardiac medical intensive care unit. Cardiopulm Phys Ther J. 2012;23(3):37–45. 5. Umakanthan R, Hoff SJ, Solenkova N, et al. Benefits of ambulatory axillary intra-aortic balloon pump for circulatory support as bridge to heart transplant. J Thorac Cardiovasc Surg. 2012;143(5):1193–1197. 6. Burtin C, Clerckx B, Robbeets C, et al. Early exercise in critically ill patients enhances short-term functional recovery. Crit Care Med. 2009; 37:2499–2505. 7. Scheweickert WD, Hall J. ICU-acquired weakness. Chest. 2007;131(5): 1541–1549. 8. Knight J, Nigam Y, Jones A. Effects of bedrest 1: cardiovascular, respiratory and haematological systems. Nurs Times. 2009;105(21): 16–20. 9. Perme C, Chandrashekar R. Early mobility and walking program for patients in ICU units: Creating a standard of care. Am J Crit Care. 2009; 18(3):212–221. 10. Morris PE, Goad A, Thompson C, et al. Early intensive care unit mobility therapy in the treatment of acute respiratory failure. Crit Care Med. 2008;36(8):2238–2243. 11. Schweickert WD, Pohlman MC, Pohlman AS, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: A randomised controlled trial. Lancet. 2009;373(9678):1874–1882. 12. Jette DU, Stilphen M, Ranganathan VK, et al. Interrater reliability of “AM-PAC 6-Clicks” basic mobility and daily activity short forms. Phys Ther. 2014;95:1–26. 13. Jette DU, Stilphen M, Ranganathan VK, et al. Validity of the AM-PAC “6-Clicks” inpatient daily activity and basic mobility short forms. Phys Ther. 2014;94(3):379–391, 1252–1261. 14. Berg HE, Larsson I, Tesch PA. Lower limb skeletal muscle function after 6 wk of bed rest. J Appl Physiol (1985). 1997;82(1):182–188. 15. Masud F, Zainab A, Ratnani I, et al. Updates on critical care management of cardiovascular patients. Methodist Debakey Cardiovasc J. 2011;7(4): 28–32. Axillary Intra-aortic Balloon Pump Placement 57 Copyright Ó 2015 by the Cardiovascular and Pulmonary Section, APTA. Unauthorized reproduction of this article is prohibited.