Pathobiology Program - Johns Hopkins Medicine
advertisement
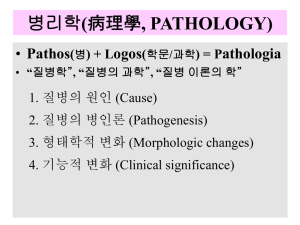
Pathobiology Program Cellular Injury and Cell Death Angelo M. De Marzo MD PhD Aug. 25, 2014 Pathology Study of structural, biochemical, and functional changes in cells, tissues and organs that underlie disease. Use of molecular, microbiologic, immunologic, and morphologic techniques to explain the signs and symptoms of disease and provide a basis for treatment. Serves as bridge between basic sciences and clinical medicine (scientific foundation for medicine) Robbins and Cotran, Pathological Basis of Disease, 9th Edition Case 50 year old male with sudden left sided paralysis Questions: •How is this manifested at the cellular and molecular level? •Can help with developing new Rx to reduce impact of injury and inform us about new cancer Rx approaches Robbins and Cotran, Pathological Basis of Disease, 7th Edition Introduction to Pathology Etiology or Cause of Disease The inciting agent (i.e. HIV virus infection) Pathogenesis (How it happens) Sequence of events in response of cells or tissues to the etiologic agent, from the initial stimulus to the ultimate expression of the disease (i.e. HIV infection CD4+ T cell death opportunistic infection of lung leading to pulmonary failure leading to cardiac failure death) Pathology Anatomic pathology: study changes in structure, or appearance of organs, tissues and cells as related to changes in function Morgagni's Seats and causes of disease ( 1761): symptoms explained in terms of anatomical changes observed at post-mortem Functional Derangements and Clinical Manifestations Organ injury starts with molecular or structural alterations in cells (nineteenth century by Rudolf Virchow) The nature of the morphologic changes and their distribution in different organs or tissues alter function and determine the clinical features (symptoms and signs), course, and prognosis of the disease Morphologic Changes Structural alterations in cells or tissues that are either characteristic of the disease or diagnostic of the process Diagnostic pathology is devoted to identifying the nature and progression of disease by studying morphologic changes in tissues Modern Diagnostic Pathology Molecular analyses augment anatomical approaches: Mutational analysis FISH gene expression microarrays Immunohistochemistry Uncovering changes or “signatures” that bear on the behavior of the disease Molecular Pathology Her-2-neu amplification in breast cancer Robbins and Cotran, Pathological Basis of Disease, 9th Edition Robbins and Cotran, Pathological Basis of Disease, 9th Edition Robbins and Cotran, Pathological Basis of Disease, 9th Edition Hypertrophy Robbins and Cotran, Pathological Basis of Disease, 7th Edition Atrophy Shrinkage in the size of the cell by loss of cell substance A form of adaptive response When many cells are involved, the entire tissue or organ diminishes in size, or becomes “atrophic” Can be physiologic or pathologic The uterus decreases in size shortly after parturition Pathologic atrophy depends on the underlying cause and can be local or generalized Robbins and Cotran, Pathological Basis of Disease, 9th Edition Causes of Atrophy Decreased workload (atrophy of disuse) Loss of innervation (denervation atrophy) Diminished blood supply Inadequate nutrition Loss of endocrine stimulation Aging (senile atrophy) Pressure Normal Breast Tissue Non Lactating Lactating Metaplasia a reversible change in which one adult cell type (epithelial or mesenchymal) is replaced by another adult cell type Commonly seen prior to cancer development – e.g. cervix, esophagus, stomach Robbins and Cotran, Pathological Basis of Disease, 7th Edition Causes of Cell Injury/Death Hypoxia/Ischemia – most common cause (e.g. myocardial infarction) Physical agents Trauma, temperature extremes, radiation, electric shock Chemical agents – (e.g. acid damage to esophagus) Infectious agents Immunological reactions (e.g. autoantibodies) Genetic derangements (e.g. Duchenne muscular dystrophy or sickle cell disease) Nutritional imbalances – too little or too much Mechanisms of Cell Injury/Death Plasma membrane damage Mitochondrial damage Ribosomal damage Nuclear damage Oxidative Stress Induced Damage Free radicals can produce profound cellular injury Produced by Powerful external energy source – e.g. ionizing radiation Oxidative-reductive reactions Inflammation Unpaired electrons are free to participate in chemical bond formation oxidative DNA damage – Sugar damage leading to strand breaks Base damage Lipid peroxidation – creating chain reaction Protein Oxidation Nitrosative Damage is also important Downloaded from: Robbins & Cotran Pathologic Basis of Disease (on 12 September 2006 07:47 PM) © 2005 Elsevier Reversible Cell Injury: e.g. Fatty Liver Fatty Liver Normal Liver Reversible Injury - Kidney Robbins and Cotran, Pathological Basis of Disease, 9th Edition Cell Death Plays a central role in multi-cellular organisms during their early development in sculpting body parts and in adult life by controlling cell numbers Further protects the organism overall by removal of cells damaged by disease, aging, infection, genetic mutation and exposure to toxic agents Traditionally broken down into Necrosis Apoptosis Necrosis Results from a variety of accidental and lethal actions by toxins or physical stimuli or in association with pathological conditions such as ischemia. Characterized by cellular swelling, dissolution of nuclear chromatin, disruption of the plasma membrane, and release of intracellular contents into the extracellular space, resulting in inflammation. Traditionally considered to be a passive process However, it is now known to be a genetically controlled process, at least at times (Peter, ME, Nature 471:310-,2011) Downloaded from: Robbins & Cotran Pathologic Basis of Disease (on 12 September 2006 04:49 PM) © 2005 Elsevier Time Course of Cell Injury and Necrosis Robbins and Cotran, Pathological Basis of Disease, 7th Edition Necrosis Necrosis: from “accidental” death of cells and living tissue Less orderly than apoptosis Lack cell signals which tell nearby phagocytes to engulf the dying cell The release of intracellular content after cellular membrane damage is the cause of inflammation in necrosis Emerging evidence that specific proteins may mediate this (e.g. HMGB1 and HDGF) Examples of “necrosis” at the gross level Robbins and Cotran, Pathological Basis of Disease, 7th Edition More Examples of Grossly Apparent “Necrosis” Necrosis at the Light Microscopic Level Coagulative Necrosis – Renal Infarct Normal Tubules Necrotic Tubules In Coagulative necrosis, the outline of the original cells remain intact, but nuceli are essentially dissolved Coagulative Necrosis – Myocardial Infarct Normal Myocardium Necrotic Myocardium Another “type” of Necrosis: Liquifactive Necrosis – Abscess – Microscopic Appearance In liquifactive necrosis, the outline of the original cells does not remain intact, all local tissue is dissolved Other Types of Necrosis Distinctly Visible Grossly and Microscopically Fat Necrosis In some tissues (i.e. pancreas), when cells die, lipases are released lysis of fat in adipocytes in surrounding tissues into free fatty acids Ca+ salts of these form “soap” deposits, which are chalky white Caseous Necrosis A specific type of liquifactive necrosis occurring in “granulomatous” inflammation (i.e. tuberculosis) http://www.sciencephoto.com/media/260971/enlarge http://quizlet.com/3021100/pathology-slides-flash-cards/ Casesous Necrosis – Microscopic Appearance (Lung) Fibrinoid necrosis Apoptosis (first recognized form of programmed cell death) First evidence of a genetic program that orchestrates physiological cell death came from developmental studies of the nematode Caenorhabditis elegans. Knowledge increased dramatically in last 3 decades with discovery of several death genes in C. elegans and counterparts in mammals. Dysregulation of apoptosis occurs in a wide variety of diseases including cancer, autoimmune diseases, neurodegenerative diseases, ischemic disease and viral infections. Apoptosis Coined by Kerr, Wyllie, and Currie (Brit J. Cancer 26:239) in 1972 a morphologically distinctive form of cell death that can be associated with normal physiology distinguished from necrosis characterized by nuclear chromatin condensation, cytoplasmic shrinking, dilated endoplasmic reticulum, and membrane blebbing. http://www.nih.gov/sigs/aig/Aboutapo.html Apoptosis Triggered by a wide variety of stimuli and occurs normally in some organs during development DNA damage (by irradiation or drugs) Some hormones such as corticosteroids lead to death in particular cells (e.g., thymocytes) Sometime triggered by removal of survival factors (i.e. androgens and prostate) Apoptosis – Scanning EM http://fig.cox.miami.edu/~cmallery/255/255hist/mcb1.19.apoptosis.jpg Apoptosis – Transmission EM Downloaded from: Robbins & Cotran Pathologic Basis of Disease (on 13 September 2006 04:51 AM) © 2005 Elsevier Apoptosis – Transmission EM http://www.msu.ac.th/bio-dept/Apoptosis.htm Nature Reviews Mol Cell Bio; 9:231-, 2008 Apoptosis – Hematoxylin & Eosin – in human tonsil tissue Apoptotic germinal center B cells are found within the cytoplasm of macrophages= “tingible body macrophages” http://library.med.utah.edu/WebPath/HEMEHTML/HEME121.html Classical Forms of Cell Death Necrosis Stimuli include toxins, severe hypoxia, massive insult, and conditions of ATP depletion. There is no energy requirement. It usually affects large numbers of contiguous cells such as death of patches of tissue. Cell swells; organelles swell; disruption of organelles occurs. DNA breakdown pattern gives randomly sized fragments. See smear pattern in gel electrophoresis. Plasma membrane is lysed. Inflammation occurs. Chemotactic factors stimulate neutrophil infiltration to degrade dead cells. Until recently was assumed to be entirely passive! http://www.msu.ac.th/bio-dept/Apoptosis.htm Apoptosis Stimuli include physiological and pathological conditions without ATP depletion. It is ATP dependent. It usually affects scattered individual cells such as death of single isolated cells. Cell contracts; chromatin condenses; apoptotic bodies form. DNA breakdown pattern gives DNA fragments in multiples of about 200 base pair units. See ladder pattern in gel. Plasma membrane remains intact and blebbed. No inflammation occurs. Apoptotic bodies are phagocytized and intact; generally no neutrophil infiltration occurs. Nature Reviews Mol Cell Bio; 9:231-, 2008 T cells to directly kill infected cells Death receptor agonists (e.g. to kill self reactive T cells in thymus) DISC= death-inducing Signaling complex • • • DNA Damage, Lack of growth factor signaling Protein misfolding Nature Reviews Mol Cell Bio; 9:231-, 2008 Nature Reviews Molecular Cell Biology 9, 378390 (May 2008) Classical DNA Ladder of Apoptosis Downloaded from: Robbins & Cotran Pathologic Basis of Disease (on 13 September 2006 04:51 AM) © 2005 Elsevier Nature Reviews Mol Cell Bio; 9:231-, 2008 Nature Reviews Mol Cell Bio; 9:231-, 2008 Nature Reviews Mol Cell Bio; 9:231-, 2008 Nature Reviews Mol Cell Bio; 9:231-, 2008 Apoptosis Movie Why Apoptosis vs Necrosis? Necrosis -> rapid loss of membrane integrity and release of cellular contents that trigger inflammation > danger signals! Danger Associated Molecular Patterns stimulate pattern recognition receptors on innate inflammatory cells that then can activate adaptive immunity This makes sense since pathogens can provoke necrosis, and, trauma which causes necrosis promotes pathogen growth… Yet, this can also result in “autoimmune” recognition if not controlled Potential Problems Solved by Apoptosis The membrane changes (i.e. flip phosphatidyl serine) facilitate removal of the cells by phagocytes before contents spill Many cellular contents are protected from immune system recognition Apoptosis “shreds the evidence” so these contents (i.e. chromatin, nuclear proteins like fibrillarin) cannot elicit immune response => prevents the “unmasking of hidden self” Autophagy Sequestration of cytoplasm and organelles by double or multi-membrane structures called autophagic vacuoles, followed by degradation of the contents of the vacuoles by fusing to lysosomes Long regarded as a cell survival mechanism: e.g. may help cancer cell survive under nutrient-limiting conditions If carried to exhaustion, digestion of own components results in cell death Autophagy Electron microscopy observations of the appearance of double membrane–enclosed structures termed autophagosomes Microtubule-associated protein 1 light chain 3 (LC3) is the homolog of yeast Atg8, an autophagy-related protein Autophagy Detection in Cell Culture Programmed Necrosis/Necroptosis Support as “non-passive” process came from studies of death receptors Activate FAS or TNFR, prototypic extrinsic apoptosis induction (recruit FADD and upstream caspase 8) But… in certain cell types same stimulation in a “apoptosis deficient condition”, produces cell death with morphology of necrosis “The fact that the activation of Fas/TNFa receptors may lead to cell death with features of either apoptosis or necrosis argues strongly for the existence of a regulated cellular necrosis mechanism, discrete from apoptosis, which we termed ‘necroptosis’’ Hitomi, et al., 2008, Cell 135, 1311-1323 Necroptosis RIP1 = kinase associated with death receptors but kinase activity not needed for apoptosis Block apoptosis and RIP1 kinase activity is needed for activation of necroptosis by death receptor agonists Nec-1 = necrostatin, a small molecule inhibitor of necroptosis, is allosteric inhibitor of RIP1 Kinase (tool to determine if necroptosis is involved) Apoptosis FAS + L929 Cells + Z.VAD.fmk (caspase inhibitor) Necroptosis +Z.VAD.fmk + Nec-1 Little cell death 432 genes involved in necroptosis, 32 are downstream or regulators of RIP1, 7 genes involved in both necroptosis and apposes, including Bmf (BH3-only protein) Hitomi, et al., 2008, Cell 135, 1311-1323 Mitochondrial Permeability Transition Pore Non-selective pore for which the precise structural identity is not well defined Nonselective water and solutepassing protein channel spanning the inner and outer mito membranes Closed in unstressed cells, and open upon oxidative stress, causing massive ion influx that dissipates the membrane potential and shuts down ATP production Regulated by cyclophilin D (a propyl isomerase) CypD-/- mice are resistant to ischemia induced necrosis in MI and stroke and CypD deficient mito and cells are resistant to Ca2+ and H202 induced cell death, but are sensitive to Bcl-2 family driven apoptosis Cell Death and Differentiation (2009) 16, 1419–1425 Programmed Necrosis Molecular Players Mediated by the opening of mitochondrial permeability transition pores (MPTP), which disrupts mitochondrial respiratory function Depends on RIP1 and RIP3 Kinases (Cho et al., Cell, 137:11121123, 2009) Cyclophilin D (CypD) (Halestrap, Biochemical Society Transactions 34, 232–237 2006) Newer data implicating p53 (Vaseva A, Cell,149:1536-1548, 2012) as well as ALKBH7 (Genes Dev. 27: 1089-1100, 2013) Regulates disease pathologies in animal models of hypoxic/ischemic injury acute pancreatitis and septic shock Why Programmed Necrosis May act as a second line of defense in viral infections. Viruses may encode caspase inhibitors to block apoptosis Viral inhibitor of RIP1 has been founds (M45) RIP3 -/- cells are protected against viral induced cell death Thus, necroptosis may function to stimulate the immune system in response to infection Cross talk between Apoptosis and Necroptosis In development, activation of apoptotic pathways results in repression of necrotic pathway Nature 471: 311-, 2911. Crosstalk between Autophagy and Necroptosis Treatment of RCC with PI3K inhibitors results in induction of autophagy and suppression of necroptosis by a reduction in RIPKs. Simultaneous treatment of RCC with PI3K inhibitor and autophagy inhibitor results in induction of RIPK and ROS-mediated necroptosis Thus, autophagy is a survival mechanism to RIPK-dependent necroptosis in the setting of cancer therapy PLoS ONE: 7:7, e41831, 2012 There Can Be Too Much and Too Little Programmed Cell Death Too much: AIDS ischemia and cardiac and stroke pathology neurodegenerative diseases Parkinson’s, Huntingtons, ALS Too little: Many cancers P53 is activated in response to DNA damage Cells having excessive DNA damage can develop mutations and should die, but tumor cells can develop blocks in apoptotic pathways (i.e. by mutating p53) or perhaps programmed necrosis Questions?