Presentation
advertisement

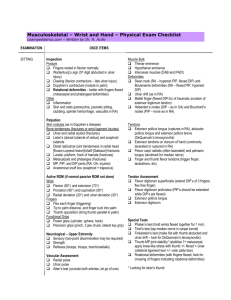
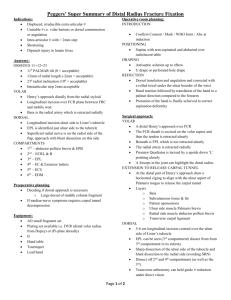
Evaluation and Treatment of Common Sports Injuries to the Wrist and Hand Mary L. Mundrane-Zweiacher, MPT, ATC, CHT Most often – You are the Expert!! First CMC Joint Extrinsic Hand Muscles: Volar Aspect Palmaris longus Flexor carpi radialis Flexor carpi ulnaris Flexor Pollicis Longus Flexor Digitorum Profundus (FDP) Flexor Digitorum Superficialis (FDS) The Extrinsic Hand Muscles: Volar Aspect Flexor Digitorum Profundus (FDP) Flexor Digitorum Superficialis (FDS) Extrinsic Hand Muscles: Dorsal Aspect Extensor Pollicis Longus (EPL) Extensor Pollicis Brevis (EPB) Abductor Pollicis Longus (APL) Extensor indicis Extensor Digitorum Communis (EDC) Visible Extensor Mechanism Extrinsic Hand Muscles: Dorsal Aspect Extensor carpi radialis longus ( ECRL) Extensor carpi radialis brevis (ECRB) Extensor carpi ulnaris Extensor digiti minimi The Intrinsic Hand Muscles Lumbricales Dorsal Interossei Palmar (Volar) Interossei Thenar Muscles Hypothenar Muscles Adductor Pollicis Intrinsic Hand Muscles Lumbricales Dorsal Interossei Palmar (Volar) Interossei Thenar Muscles Hypothenar Muscles Adductor Pollicis Intrinsic Hand Muscles Lumbricales Dorsal Interossei Palmar (Volar) Interossei Thenar Muscles Hypothenar Muscles Adductor Pollicis Volar Plate Phases of Connective Tissue Healing Inflammatory Phase Fibroplastic Phase Remodeling Phase Inflammatory Phase vasodilation hyperemia increased cell permeability increased vascularity cell migration debris removal Fibroplastic Phase re-epithelialization causing wound closure (skin) fibroplasia – fibroblasts are activated and move along the fibrin meshwork to generate new collagen, elastin, GAG’s, proteoglycans, and glycoproteins neovascularization – regeneration of small blood vessels wound contraction collagen with random alignment Remodeling Phase consolidation phase increased wound strength realignment of collagen reduction of abnormal cross links maturation phase – the scar links change from weak hydrogen bonds to strong covalent bonds AROM/PROM/AAROM Most reliable method for measuring finger/wrist flexion and extension is the volar/dorsal technique Bilateral comparison Strength/Grip testing Submax effort can be ruled out with use of rapid-exchange grip testing and bell curve with five position grip testing with a Jamar Five position grip testing can also assist with your tendon function assessment Sensibility Examination/Sensation Testing Done to screen for nerve compression Semmes Weinstein light touch threshold is the most sensitive clinical test for detecting nerve compression X-Ray Studies Variance (assessed on X-Ray with the forearm in neutral rotation) Neutral ulnar variance – the head of the distal ulna is even with the distal end of the radius Positive ulnar variance – the head of the ulna extends distally beyond the distal radius Negative ulnar variance – the head of the ulna is more proximal than the distal radius Common Finger/Hand Injuries Mallet Finger – is a disruption of the terminal aspect of the extensor tendon either because of laceration, rupture, or avulsion 1. Mechanism – forceful flexion of the dip joint when the finger is being actively extended Mallet finger Conservative Treatment for acute mallet finger (less than 3 weeks old) Acute Mallet Finger Treatment a. 0-6 weeks – continual splinting of the dip joint in 10-15deg hyperextension (volar splints work best) - the splint may be removed once a day to prevent skin breakdown or maceration but the hyperextension must be maintained - if the dip joint bends, the splint wearing time must be started over Splint choices Acute Mallet Finger Treatment after 6 weeks – active AROM at the dip joint is allowed in a limited range and for limited sessions each day. The mallet finger splint is worn outside of exercise. If an extensor lag develops, AROM sessions are decreased or put on hold and continual splinting resumed. Acute Mallet Finger Treatment at 8 weeks – if no extensor lag, the mallet splint is discontinued during the day but still worn at night. Gentle strengthening with putty, hand exerciser, etc can be added at 9 weeks – the mallet splint is discontinued if no lag no PROM to the dip joint is done with mallet finger, only active Chronic Mallet Finger Treatment 0-8 weeks – continual splinting of the dip joint in 10-15deg hyperextension (sometimes the dip joint may be pinned) - the splint may be removed once a day to prevent skin breakdown or maceration but the hyperextension must be maintained -if not pinned and if the dip joint bends, the splint wearing time must be started over Chronic Mallet Finger Treatment after 8 weeks – active AROM at the dip joint is allowed in a limited range and for limited sessions each day. The mallet finger splint is worn outside of exercise. If an extensor lag develops, AROM sessions are decreased or put on hold and continual splinting resumed. c. at 9 weeks – if no extensor lag, the mallet splint is gradually discontinued during the day but still worn at night. Decreased 1 hour per day is typical. PROM may be added if the dip extensor lag is < 10deg. Surgical Treatment for Mallet Finger (greater than 3 weeks old) is indicated when the avulsed distal fragment is 50% or greater of the articular surface of the distal phalanx surgical procedure – an incision is made along the area of the distal phalanx and dip joint. The displaced bone fragment is re-approximated along the distal phalanx. A k-wire is used to position the dip joint in extension. Surgical Candidate for Mallet Finger Surgical Treatment for Mallet Finger 3 days post-up – Dressing is removed and edema control is begun. A splint is made to protect the distal tip and pin and worn continually. Pin is cleaned daily with hydrogen peroxide (depending on physician) at 6 weeks – the pin is removed by the physician with continual splinting of the dip joint except during exercise sessions AROM exercises are initiated to the dip joint (6 times a day for 5-10min) Surgical Treatment for Mallet Finger at 7 weeks – active AROM at the dip joint is allowed in a limited range and for limited sessions each day. Gentle ROM exercises may be initiated to the dip joint as long as and extensor lag is not present at the dip joint. at 9 weeks – splint wearing time is steadily decreased usually 1 hour per day at 10 weeks – discontinue splint during the day at 12 weeks – discontinue splint at night Flexor Digitorum Profundus Injury versus Flexor Digitorum Superficialis Injury FDS FDP Flexor Digitorum Profundus Rupture or Avulsion • Mechanism – a forceful eccentric load on the FDP can cause an avulsion off the distal phalanx • Called Jersey Finger because this frequently occurs as a player grabs another player and the finger becomes caught in their jersey Forceful extension of the 4th dip joint Rupture of the FDP Flexor Digitorum Profundus Rupture or Avulsion Flexor Digitorum Profundus Rupture or Avulsion Signs and Symptoms: swelling and discomfort at the DIP joint Patient will not be able to flex the DIP joint actively Treatment: -RECOGNITION – often missed if FDS function is intact -Referral to MD (surgery to re-attach tendon) Flexor Digitorum Superficialis Injury (to 3rd through 5th fingers) Uncommon in athletics Mechanism – mostly lacerations from sharp objects Sign: patient will not be able to flex PIP joint of fingers with the other two fingers held in full extension Treatment: -referral to MD Boutonniere Deformity versus Volar Plate Contracture Boutonniere Deformity Boutonniere Deformity – Extensor tendon injury at Zone 3 and the lateral bands move volar to the axis of the PIP joint . Mechanism – volar dislocation or subluxation of the PIP joint. -because the lateral bands are volar to the axis, when the extensor contracts, instead of extending the joint, they flex the PIP joint. -over time, the extensor force is concentrated on the DIP joint, causing DIP hyperextension and loss of DIP flexion. -in early stages, there is full passive extension of the PIP joint. Boutonniere Deformity Treatment KEY – recognition of the injury Treatment: possible surgical repair consult with a hand therapist continuous splinting in extension, buddy taping is not sufficient finger splints are generally accepted by officials if they are covered with tape. Splinting for Boutonniere Deformity Good Bad Boutonniere Deformity Treatment when appropriate healing has occurred, early short-arc motion exercise where the PIP joint is held in extension and the DIP is flexed night splinting may be required for 2 to 3 months, and protective splinting for the remainder of the season Volar Plate Contracture Mechanism - commonly injured with dorsal dislocation of the PIP joint (hyperextension injury). the volar plate is a fibrocartilaginous structure on the volar aspect of the PIP joint. In response to injury it can become fibrotic and immobile, thus limiting PIP joint extension. PIP joint extension will be limited actively and passively Treatment for the Dorsal PIP Dislocation for a grade I– splinted in slight flexion until acute pain subsides. b. for a grade II - a dorsal splint with 20deg to 30deg of PIP joint flexion for approximately 7 to 14 days. After immobilization, the finger can be taped to an adjacent finger for protection. Patient needs to be watched for a missed Boutonniere. c. for a grade III - as per grade unless reduction is not maintained, then surgery is appropriate Treatment for the Volar Plate Contracture Modalities to increase mobility of the volar plate Volar plate mobilization PIP ext stretches, with cuing to avoid hyperextension of the DIP joint Possible night time static splinting in progressive extension Possible day time dynamic splinting Gamekeeper’s Thumb/Skier’s Thumb sprain of the Ulnar collateral ligament of the thumb MP joint (more common than injury to the radial collateral ligament) Gamekeeper’s Thumb/Skier’s Thumb Gamekeeper’s Thumb/Skier’s Thumb Mechanism Forced radial deviation of the thumb For radial collateral ligament injury, forced ulnar deviation Signs and Symptoms pain and swelling over the collateral ligament tenderness laxity and pain noted with passive stress test to the respective ligament pinch is often painful and weak Gamekeeper’s Thumb/Skier’s Thumb Treatment- non surgical conservative 0-4 weeks - thumb short opponens splint – motion at the mcp joint must be restricted splint will need to be remolded as swelling decreases anti-inflammatory modalities maintain ROM/function of wrist and fingers while maintaining thumb stability Short Opponens Splint Gamekeeper’s Thumb/Skier’s Thumb Treatment- non surgical conservative 4-6 weeks – if the pain is resolving, gentle AROM to the thumb Not uncommon for this to be painful and immobilized for 6 weeks before AROM fluido/MHP/etc when no longer acute swelling 6 weeks – if the patient is asymptomatic, unrestricted AROM to the thumb The short opponens splint can be worn for comfort and protection when not exercising Gamekeeper’s Thumb/Skier’s Thumb Treatment- non surgical conservative 8 weeks – if the patient is not tender along the collateral ligament Splint can be discontinued except for activities requiring heavy use of the hand Strengthening of the hand/wrist but tight, sustained pinch or gripping with the hand/thumb must be avoided for 10-12 weeks Gamekeeper’s Thumb/Skier’s Thumb Treatment – surgical Surgery is indicated to repair the UCL or RCL if the tear is complete and there is instability of the joint. A Stener’s lesion involves complete rupture of the UCL and the adductor apponeurosis displaces distal to the rupture causing the ligament to move away from the insertion. The UCL will not heal properly, and thus restore joint stability unless it is surgically restored. Stener’s Lesion Gamekeeper’s Thumb/Skier’s Thumb Treatment – surgical 10-14 days postop Edema control Forearm based thumb splint with the ip joint free, worn continually (splint should be molded to support the mcp joint well 4 weeks postop Pin is removed Thumb Spica Splint Gamekeeper’s Thumb/Skier’s Thumb Treatment – surgical 6 weeks postop AROM/AAROM to emphasize thumb/wrist flexion and extension, and thumb adduction/abduction/circumduction 7 weeks postop Splint revised to a short opponens splint PROM exercises begun to the thumb Dynamic splints are sometimes used to restore mcp and ip thumb motion but care needs to be taken to avoid stressing collaterals Gamekeeper’s Thumb/Skier’s Thumb Treatment – surgical 8 weeks postop Splint-wearing may be decreased to only times of heavy lifting and activities requiring a right, sustained pinch Dexterity and Progressive strengthening exercise as tolerated (putty and hand exerciser) 10-12 weeks postop General unrestricted use of the hand in most activities except for weighted resistance or sustained power pinching (that can be resumed at >er 14 weeks) Radial Collateral Ligament Injury Adductor Pollicis makes this injury significant Colles/Distal Radius Fracture Barton’s Fracture Zone Examination of the Wrist Radial dorsal zone Central dorsal zone Ulnar dorsal zone Radial volar zone Ulnar volar zone Radial Dorsal Zone Structures to palpate: Radial styloid Scaphoid Scaphotrapezial joint Trapezium Base of the first met 1st MCP joint The Extrinsic Hand Muscles: Dorsal Aspect Extensor Pollicis Longus (EPL) Extensor Pollicis Brevis (EPB) Abductor Pollicis Longus (APL) Extensor indicis Extensor Digitorum Communis (EDC) Radial styloid tenderness may indicate: Contusion Fracture If tenderness is accentuated with radial deviation (RD) – radioscaphoid arthritis Scaphoid tenderness in the snuffbox may indicate: scaphoid fracture scaphoid non-union scaphoid instability Scaphoid Non-Union Scaphoid and trapezium tenderness may indicate: scaphoid instability ST arthritis if accompanied by central dorsal complaints, see section III B4 First CMC joint tenderness may indicate: with a (+) Grind test (pain with axial compression of the 1st met with rotation) – 1st CMC joint degenerative arthritis with a (+) instability/laxity test (more laxity is present when the 1st met is distracted and moved side to side or RU direction while the trapezium is stabilized versus on the uninjured side) – 1st CMC joint instability or laxity Instability/Laxity Test st 1 CMC Splint Extensor pollicis brevis (EPB) and abductor pollicis longus (APL) tenderness may indicate: with a (+) Finkelstein’s test (pain localized to the radial aspect of the wrist when thumb flexion is combined with UD of the wrist) – de Quervain’s tenosynovitis st 1 1st CMC DJD versus deQuervain’s CMC DJD can be confused with deQuervain’s tenosynovitis so a Grind test should also be done deQuervain’s Tenosynovitis • • Stenosing tenosynovitis of the APL and EPB tendons in the sheath Anatomy – the APL and EPB tendons pass through the first dorsal compartment of the extensor retinaculum. There is a synovial sheath under the retinaculum encasing the tendons deQuervain’s Tenosynovitis Etiology – Microtrauma – forceful, sustained, or repetitive thumb abduction and simultaneous wrist UD. Some MD’s feel that RD with pinch is the most stressful because the APL and EPB tendons are taut and sharply angulated at the wrist and trapeziometacarpal joint Acute trauma – sudden wrenching of the wrist and thumb while trying to restrain an object or person or a fall deQuervain’s Tenosynovitis Signs and Symptoms radial-sided wrist pain over the 1st dorsal compartment pain can radiate to the thumb increased pain with increased tensile load on the EPB or APL (+) Finkelstein’s test wrist flexion will intensify the pain and extension should relieve it deQuervain’s Tenosynovitis Signs and Symptoms cont’d painful thumb extension MRI may show increased fluid in the 1st extensor compartment rarely pseudotriggering can co-exist with or be confused with trapeziometacarpal arthritis, scaphoid fractures, scapholunate instability, intersection syndrome, radial neuritis, and radioscaphoid/scaphotrapezoid joint problems deQuervain’s Tenosynovitis Treatment splint to minimize UD at wrist and substitutes power grip for pinch anti-inflamatory modalities gentle gliding of tendons and gentle AROM possible injection into sheath after failed conservative management, surgical release of the 1st dorsal compartment Make sure 1st CMC was assessed EPB and APL muscle belly tenderness or crepitus may indicate: with active thumb movement or friction and crepitus palpated 4 to 5 cm proximal to the radial styloid during wrist flexion and extension with radial deviation -intersection syndrome Intersection Point Intersection Syndrome stenosing tenosynovitis of the second dorsal compartment Anatomy – the intersection where the radial wrist extensor tendons pass underneath the muscle bellies of the APL and EPB approximately 4 cm proximally to Lister’s tubercle Intersection Syndrome Etiology repetitive wrist and/or thumb activities frequently seen in weight lifters and rowers possible bursal inflammation Signs and Symptoms pain and swelling of the overlying muscle bellies of the APL and EPB muscles possible redness possible painful crepitus with thumb and wrist movements grip and pinch are often painful and weak Intersection Syndrome Treatment forearm or thumb spica splint anti-inflammatory modalities gentle gliding of tendons and gentle AROM possible injection/possible surgical release Numbness, tingling, burning, and pain over the dorsal radial aspect of the hand may indicate: (+) Tinel’s with percussion along the course of the nerve produces tingling and pain which may radiate distally – Wartenberg’s Syndrome or Neuralgia (irritation of the Dorsal Radial Sensory Nerve) with more proximal complaints – CN root irritation????? Tinel’s Test Wartenberg’s Syndrome Anatomy – the dorsal radial sensory nerve (DRSN) travels along the dorsal radial aspect of the wrist (very superficial) between the tendons of the brachioradialis and the ECRL. Wartenberg’s Syndrome Etiology – because of the superficial location, the DRSN is susceptible to compressive forces (ex. from tight wrist straps). Repetitive pronation, flexion, and UD (pronation causes the ECRL tendon to cross under the brachioradialis tendon and compress the DRSN). Wartenberg’s Syndrome Signs and Symptoms flexion and UD puts the nerve on stretch which increases pain numbness, tingling, burning and pain over the dorsal radial aspect of the hand (+) Tinel’s possible decreased sensation over the dorsal web and thumb dorsum Wartenberg’s Syndrome Treatment anti-inflammatory modalities (phonophoresis) heat modalities (not cold) gentle stretching desensitization Central Dorsal Zone Structures to palpate: Distal radius (dorsal rim) Lister’s tubercle Lunate Scapholunate interval Capitate 2nd and 3rd metacarpal bases 2nd – 4th extensor tendons Posterior interosseus nerve (PIN) The Extrinsic Hand Muscles: Dorsal Aspect Extensor Pollicis Longus (EPL) Extensor Pollicis Brevis (EPB) Abductor Pollicis Longus (APL) Extensor indicis Extensor Digitorum Communis (EDC) Distal radius dorsal rim tenderness may indicate: (-) X-Ray changes – Impingement of the scaphoid on the radius (+) X-Ray changes and pain with pressure or with hyperextension and radial deviation of the wrist – osteophyte Lunate tenderness only, may indicate: (+) X-Ray changes – Kienbock’s disease (avascular necrosis of the lunate) Scapholunate interval tenderness may indicate: patient history of recurrent nodular swelling in the wrist dorsum and complaints of pain with deep palpation that may not be detected by clinical exam – dorsal wrist ganglion (***tenderness may be present with wrist flexion or extension secondary to compression of the ganglion) with localized non- nodular swelling – scapholunate ligament injury Scapholunate interval tenderness may indicate: with localized non-nodular swelling and a (+) finger extension test (pain in the scapholunate region with resisted finger extension with the wrist in flexion) – dorsal wrist syndrome or scapholunate synovitis Finger Extension Test Scaphoid (in the snuffbox) and scaphotrapezial-trapezoid joint tenderness with synovitis may indicate: and dorsal scapholunate synovitis, and (+) finger extension test, and a positive Watson/scaphoid shift test (reproduction of the patient’s symptoms and usually a painful clunk when the examiner applies pressure over the volar prominence of the scaphoid as the wrist is moved from UD to RD with slight flexion)– scaphoid rotary subluxation Watson/Scaphoid Shift Test Watson Shift Test Moving into RD and Flexion Terry Thomas Sign SLAC Wrist – ScaphoLunate Advanced Collapse 2nd and 3rd metacarpal base and CMC tenderness may indicate: with a bony prominence at the 2nd and 3rd metacarpal bases – carpal boss and/or a (+) Linscheid test (pain localized to the CMC joint area when the metacarpal heads are moved in a palmar and dorsal direction on one another) – 2nd and/or 3rd CMC ligament injury or instability and/or a (+) metacarpal stress test (pain at the CMC joint when the MCP joint is fully flexed and the metacarpal is pronated and supinated) – CMC joint injury Linscheid’s Test Metacarpal Stress Test Ulnar Dorsal Zone Structures to palpate: Ulnar styloid Ulnar head DRUJ (distal radial ulnar joint) TFCC (triangular fibrocartilage complex) Hamate Triquetrum Lunotriquetral interval (LT interval) Fourth and fifth CMC joints Extensor carpi ulnaris (ECU) The Extrinsic Hand Muscles: Dorsal Aspect Extensor Pollicis Longus (EPL) Extensor Pollicis Brevis (EPB) Abductor Pollicis Longus (APL) Extensor indicis Extensor Digitorum Communis (EDC) Ulnar Dorsal Joint Ulnar styloid tenderness may indicate: ulnar styloid fracture ulnar fracture nonunion Ulnar Compression Test Fovea tenderness may indicate: with (+) TFCC load test (pain, clicking, or crepitus and reproduction of the patient’s symptoms when the wrist is ulnarly deviated and axial loaded, and then moved volarly and dorsally , or the forearm is rotated)- Ulnocarpal abutment (ulnar impaction syndrome) or TFCC tear with (+) TFCC load test and a (+) relocation test (pain reduction when the subluxed ulnar carpus is relocated. The combined movement of pronation, and anterior to posterior glide of the carpus on the ulna relocates the carpus into normal alignment– TFCC tear/ulnocarpal instability TFCC Load Test Relocation Test Triangular Fibrocartilage Complex Tear Triangular Fibrocartilage Complex Tear Anatomy consists of articular disc (triangular fibrocartilage), meniscus homologue (lunocarpal), ulnocarpal ligament, dorsal & volar radioulnar ligament, and ECU sheath only the peripheral 15-20% of the TFCC has a blood supply Triangular Fibrocartilage Complex Tear Function TFCC is main stabilizer of distal radioulnar joint, in addition to contributing to ulnocarpal stability volar TFC prevents dorsal displacement of ulna and is tight in pronation dorsal TFC prevents volar displacement of ulna and is tight in supination Triangular Fibrocartilage Complex Tear Function during axial loading, the radius carries the majority of load (82%), and the ulna a smaller load (18%) increasing the ulnar variance to a positive 2.5 mm increases the load transmission across the TFCC to 42% with the TFCC excised, the radial load increases to 94%; Triangular Fibrocartilage Complex Tear Mechanism Peripheryl tears are almost always secondary to ulnar deviation and forearm rotation with compressive load on the TFCC Central tears are associated with degenerative processes or trauma A positive ulnar variance is a predisposing factor Triangular Fibrocartilage Complex Tear Signs and Symptoms pain with forearm rotation (especially pronation), ulnar deviation, and gripping a painful “click” tenderness between the ulna and triquetrum (+) TFCC load test X-Rays may show an avulsion of the ulnar styloid or a tilt to the lunate and triquetrum. Ulnar variance will also be assessed. Triangular Fibrocartilage Complex Tear Signs and Symptoms – diagnostic tests Triple Injustion Arthrography – study of choice with tears being revealed as the contrast dye passes thru the radiocarpal joint and DRUJ MRI – a complete tear would show a full thickness disruption which would extend thru the disc Triangular Fibrocartilage Complex Tear Treatment (depends on location of tear) Non-surgical: Application of a Sugartong or Muenster splint that immobilizes the forearm in neutral because this is the best position to allow the TFCC to heal Activity modification Steroid injections Anti-inflammatory modalities Stabilization exercises Triangular Fibrocartilage Complex Tear Treatment (depends on location of tear) Surgical: Central tears are debrided while peripheryl tears are repaired. Ulnar shortening if there is a positive ulnar variance Wafer procedure Radial Volar Zone Structures to palpate: Radial styloid Scaphoid tuberosity STT joint Trapezial ridge Flexor carpi radialis (FCR) Palmaris longus (if present) Flexor tendons to the fingers Medial nerve Radial artery The Extrinsic Hand Muscles: Volar Aspect Palmaris longus Flexor carpi radialis Flexor carpi ulnaris Flexor Pollicis Longus Flexor Digitorum Profundus (FDP) Flexor Digitorum Superficialis (FDS) Radial styloid tenderness may indicate: distal radius fracture with increased pain upon wrist extension and radial deviation – radiocarpal ligament injury Volar scaphoid tenderness may indicate: scaphoid disease Complaints of numbness, pain, or tingling from the distal wrist into the fingers in the median nerve distribution may indicate: with a (+) Tinel’s sign/test (pain and tingling radiates to the fingers in the median nerve distribution when the median nerve is gently percussed at the wrist level – carpel tunnel syndrome and/or a (+) Phalen’s test (numbness and tingling in the distribution of the median nerve with passive flexion of the wrist for 15 to 60 seconds) – carpel tunnel syndrome with a (+) Lumbicale pinch test (reproduction of the signs and symptoms when the patient is asked to hold a sheet of paper in a lumbricale pinch – carpel tunnel caused by a more proximal origin of the lumbricales Phalen’s Test Lumbricale Pinch Test Carpal Tunnel Syndrome CRPS CRPS Ulnar volar zone Structures to palpate: Pisiform TFCC (triangular fibrocartilage complex) Hook of the hamate Flexor carpi ulnaris (FCU) Ulnar nerve Ulnar artery Hook of the hamate tenderness may indicate: with pain accentuated with resisted flexion of the 4th and 5th finger with the wrist in UD – hamate fracture Complaints of ulnar-sided pain and coldness and a (+) Allen’s test for the ulnar artery may indicate: ulnar hammer/hypothenar hammer syndrome Complaints of numbness and paresthesias in the 4th and 5th fingers and possibly a (+) Tinel’s sign cyclist’s palsy (ulnar nerve compression within Guyon’s Canal) Case Study Mid Range Strengthening Thank you to my family and Staff at Bayhealth Rehab Services Thank You!