Brain Tumors - SRL Diagnostics
advertisement

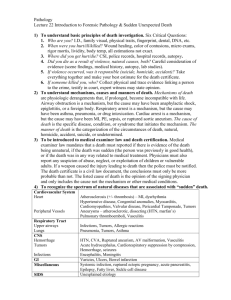
Innersense 155 May 2014 Brain Tumors: From Pathological to Molecular Classification Primary brain tumor results when a tumor originates in the brain itself. When cancer metastasizes or spreads from other areas, such as the lungs or the breasts to the brain, a secondary (or metastatic) brain tumor results. 2007 WHO Classification of Primary Brain Tumors (1) Primary brain tumors are classified by the type of tissue in which they begin. A. Gliomas - One of the most common types of brain tumor - Grows from glial cell (supportive cell in the brain) - Types of glial cells: astrocytes and oligodendrocytes Types of Gliomas: 1. Astrocytoma - Most common type of glioma - Begins in cells called astrocytes in the cerebrum or cerebellum a. Grade I or Pilocytic Astrocytoma - Slow-growing, most often benign - Accounts for about 2% of all brain tumors b. Grade II or Low-grade Diffuse Astrocytoma - Slow-growing, often spreads to nearby tissue and become a higher grade - Makes up about 3% of all brain tumors c. Grade III or Anaplastic Astrocytoma - Cancerous, grows quickly and spread to nearby tissues - Accounts for about 2% of all brain tumors d. Grade IV or Glioblastoma Multiforme (GBM) Brain Tumors: From Pathological to Molecular Classification 1 Innersense 155 May 2014 - Very aggressive form - Makes up about 16% of all brain tumors 2. Oligodendroglioma - Develop from oligodendrocytes, makes myelin - Make up about 2% of primary brain tumors - Subclassified as oligodendrogliomas (considered low grade) or anaplastic oligodendroglioma 3. Mixed Glioma is made up of more than one glial cell types. a. Ependymomas - Begin in the ependyma (passageways in the brain where CSF is made and stored) - Make up about 2% of primary brain tumors b. Brain Stem Glioma - Begins in the glial cells in the brain stem B. Non-gliomas 1. Meningioma - Most common type of non-gliomas - Begins in meninges, most often noncancerous - Can cause serious symptoms if it grows and presses on the brain or spinal cord or grows into the brain tissue 2. Pineal Gland and Pituitary Gland Tumors - Account for about 14% of all brain tumors 3. Primary CNS Lymphoma - Starts in brain and can spread to the spinal fluid and eyes - Makes up about 2% of all brain tumors 4. Medulloblastoma - Begins in granular cells in the cerebellum - Most common in children - Usually cancerous, often spreading throughout the CNS - Makes up about 2% of all brain tumors 5. Craniopharyngioma - Benign tumor - Begins near the pituitary gland - Rare, make up less than 1% of all brain tumors 6. Acoustic Schwannoma (Vestibular/ Acoustic Neuroma) - Rare, typically noncancerous - Begins in the vestibular nerve Epidemiology Worldwide, every year around 445,000 people are diagnosed with tumors that start in the brain or elsewhere in the CNS. (Cancer Research UK) Worldwide Incidence of Brain Tumors (IARC 2012) Brain Tumors: From Pathological to Molecular Classification 2 Innersense 155 May 2014 Brain Tumors in India (IARC 2012) Metrics Count ASR/P Incidence-Male 11,855 2.1 Incidence-Female 6,976 1.2 Mortality-Male 9,574 1.7 Mortality-Female 5,578 1.0 Prevalence-Male 17,251 3.8 Prevalence-Female 10,157 2.4 ASR: Age-standardized rate Molecular Evaluation of Brain Tumors (2, 3, 4, 5, 6) Gliomas are the most common primary brain tumors of adults and include a variety of histologic types and morphologies. Histologic evaluation remains the gold standard for glioma diagnosis; however, diagnostic difficulty may arise from tumor heterogeneity, overlapping morphologic features, and tumor sampling. SRL offers a distinctive and cost-effective customized IHC panel which helps the pathologist to take informed on-site decision with a range of IHC markers for tumors of various types. Advances in neurosurgery, radiation, and chemotherapy during the past decade have provided only small improvements in clinical outcome. As with many other tumors, the development of new molecular markers is expected to lead to improved diagnosis Tumors are heterogeneous and prognosis and to aid in the clinical Morphologic features are overlapping management of gliomas. Recently, our WHO classification is subjective and not reproducible knowledge about the genetics of these Molecular biology adds to morphologic examination tumors has expanded, and new molecular Pathology & molecular diagnostics are complementary markers have been developed. Some of these markers can be used diagnostically to help the neuropathologist in glioma classification and grading, especially for tumors with ambiguous histologic features. Alternatively, some of them can be used to estimate prognosis for patients and to predict response to certain therapies. Figure 1: Molecular pathways and common genetic alterations in astrocytic, oligodendroglial, and oligoastrocytic neoplasms Abbreviations: ampl., amplification; BRAF, v-raf murine sarcoma viral oncogene homolog B1 gene; CDKN2A/B, cyclin-dependent kinase inhibitors 2A and 2B genes; EGFR, epidermal growth factor receptor gene; GBM, glioblastoma multiforme; IDH, isocitrate dehydrogenase gene; mut., mutation; MGMT, O(6)-methylguanine-DNA methyltransferase; PTEN, phosphatase and tensin homolog gene; TP53, tumor protein p53 gene; WHO, World Health Organization. Brain Tumors: From Pathological to Molecular Classification 3 Innersense 155 May 2014 1p AND 19q CODELETION Loss of the short arm of chromosome 1 (1p), along with the long arm of chromosome 19 (19q), is an established genetic marker of oligodendroglial tumors. The frequency of 1p and 19q codeletion has been given (Table 1). Tumor Type PA O AO DA AA SGBM PGBM Clinical utility WHO Grade I II III II III IV IV BRAF % 60-80 1p/19q % 80-90 50-70 Diagnostic MGMT % 20 60-93 50-75 40-45 50 40-60 40 EGFR % ~40 Diagnostic Prognostic Diagnostic Prognostic Predictive Predictive Predictive Table 1: Average Prevalence of Genetic Abnormalities in Gliomas & their Clinical Utility PA, pilocytic astrocytoma; O, oligodedroglioma; AO, anaplastic oligodendroglioma; DA, diffuse astrocytoma; AA, anaplastic astrocytoma; SGBM & PGBM, secondary & primary glioblastoma multiforme There is a strong association between 1p/19q codeletion and the classic histologic features of an oligodendroglioma. However, not all oligodendroglial tumors reveal such correlation, and morphology alone cannot predict the 1p/19q status. The 1p and 19q codeletion is found to be a useful marker for prognostication about patient survival and chemosensitivity. In 1998, Cairncross and colleagues reported that loss of 1p (and combined loss of 1p and 19q) predicts a better response to procarbazine-lomustinevincristine chemotherapy and a longer survival in patients with anaplastic oligodendroglioma. Moreover, oligodendroglial tumors with loss of 1p/19q showed a response to treatment with the alkylating drug temozolomide and radiotherapy, indicating its predictive value for a broader spectrum of therapeutic regimens. MGMT METHYLATION The MGMT gene is located at chromosome 10q26 and encodes for a DNA repair protein. Epigenetic silencing of this gene by promoter hypermethylation leads to reduced expression of the MGMT protein. In 2005, Hegi et al reported that MGMT gene silencing improves survival in patients with glioblastoma who are treated concurrently with alkylating drug temozolomide and radiation therapy. Temozolomide adds a methyl group to the O6-position of nucleotide guanine, which results in DNA damage and cell death. Active MGMT is ensuring repair of damaged DNA by irreversibly transferring a methyl group from the O6-position of a modified guanine to its own cysteine residue and, therefore, decreasing the cytotoxic effects of temozolomide. However, inactivation of MGMT by promoter hypermethylation leads to decreased MGMT protein expression, which inhibits the cell’s ability to repair alkylated DNA and thus allows alkylating drugs to work more effectively. MGMT promoter methylation is found among different grades of glioma (Table 1) and is considered to be a prognostic and predictive marker. Correlation with prognosis was also reported in pediatric glioblastomas, low-grade gliomas, and more recently, in anaplastic gliomas (WHO grade III). In addition to prognostic benefit, several studies have demonstrated the predictive value of methylated MGMT in response to temozolomide chemotherapy in patients with glioblastoma. However, for anaplastic gliomas only the Brain Tumors: From Pathological to Molecular Classification 4 Innersense 155 May 2014 prognostic benefit, and not the predictive value of MGMT methylation, was reported. Interestingly, Rivera and colleagues found that methylated MGMT may predict response to radiotherapy alone even in the absence of adjuvant alkylating chemotherapy. MGMT Methylation by IHC Assessment of MGMT methylation by IHC failed to correlate with disease outcome likely due to interobserver variability, heterogeneity of the glioma sample, contamination with non-neoplastic cells that express MGMT, and differences in tumor immunoreactivity. Therefore, at present, IHC is not the method of choice for the detection of MGMT methylation. BRAF/KIAA1549 FUSION BRAF is usually activated by the point mutation BRAF V600E. In gliomas, BRAF activation by gene duplication, which leads to fusion between the KIAA1549 and BRAF genes, or by point mutation has been identified in 60% to 80% of pilocytic astrocytomas. These genetic abnormalities are rare in diffuse astrocytic gliomas and, therefore, may allow the differentiation of pilocytic astrocytomas from low-grade astrocytomas (Table 1). A Case: BRAF in Pediatric Low-Grade Gliomas (Clark K et al. Am J Clin Pathol 2013; 139:275-288) 14-year-old boy with a thalamic tumor featured with “low-grade glioma, not otherwise specified.” Despite its location, the patient has been completely recurrence-free for the past 26 years, never requiring any adjuvant therapy or re-resection. Recent BRAF FISH analysis revealed an abnormal signal pattern in nearly 50% of the cells, consisting of a small orange signal near one of the larger orange BRAF signals. From diagnostic and prognostic perspectives, the presence of a BRAF fusion suggests either a pilocytic or pilomyxoid astrocytoma, whereas the differential for a V600E-mutant tumor is broader. In this case, histologic examination could not resolve the diagnosis beyond “low-grade glioma, not otherwise specified,” but the BRAF fusion signal is consistent with the indolent nature of the tumor. Indeed, the fusion tends to be a favorable prognostic marker, whereas V600E may be slightly unfavorable. EGFR ALTERATIONS Detection of EGFR amplification is indicative of high-grade glioma and can be used diagnostically (Table 1). In neuropathology practice, identification of EGFR amplification in neoplastic astrocytes strongly supports diagnosis of GBM even if the histologic criteria are not met. EGFR amplification can also predict responsiveness to tyrosine kinase inhibitors. Brain Tumors: From Pathological to Molecular Classification 5 Innersense 155 May 2014 Conclusion The classification of malignant gliomas is moving from a morphology-based guide to a system built on molecular criteria. Changing Landscape of Glioma Diagnostics (2) Recent years have been characterized by a rapid expansion of our knowledge about the biology and genetics of gliomas and by the development of new molecular markers. Some of these markers have shown diagnostic value, whereas others are useful for patient prognostication and predicting response to therapies. Genetic testing of gliomas is increasingly used in routine clinical practice and requires neuropathologists to be familiar with all aspects of molecular analysis. References 1. Louis DN et al. Acta Neuropathol 114:97–109 (2007) 2. Jansen M. et al. Lancet Neurol. 9(7): 717–726 July (2010) 3. Riemenschneider MJ et al. Acta Neuropathol 120:567–584 (2010) 4. Nikiforova MN, Hamilton RL. Arch Pathol Lab Med Vol 135, May (2011) 5. Masui K et al. Neuropathology and Applied Neurobiology, 38, 271–291 (2012) 6. McNamara MG et al. Cancers. 5, 1103-1119 (2013) Brain Tumors: From Pathological to Molecular Classification 6 Innersense 155 May 2014 Tests Offered at SRL Test Name Method Test Code Histopathology 1500/ 1511 Immunohistochemistry 1519 Immunohistochemistry Z009K FISH 6027F ARMS PCR RD1317 EGFR Gene Amplification FISH 6016F EGFR Mutation Detection PCR Sequencing RD1405 MGMT Methylation Pyrosequencing Coming Soon Small/ Medium Tissue Biopsy Biopsy-Brain Biopsy with Special Stains (PTAH & Reticulin) Complete Diagnosis with Special Stains & IHC (Customized IHC Panel) 1p/19q Deletions BRAF V600E Mutation Register yourself at www.srlknowledgeforum.com to get Updates on Recent Trends in Medical Diagnostics Brain Tumors: From Pathological to Molecular Classification 7