From www.bloodjournal.org by guest on March 6, 2016. For personal use only.
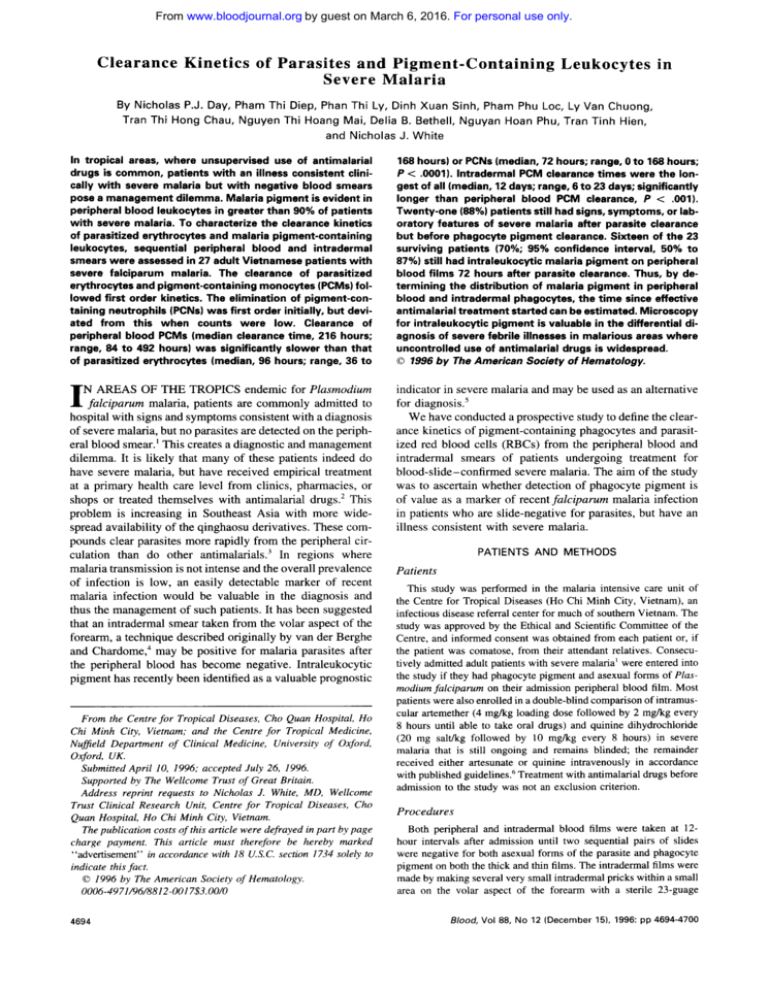
Clearance Kinetics of Parasites and Pigment-Containing Leukocytes in
Severe Malaria
By Nicholas P.J. Day, Pharn Thi Diep, Phan Thi Ly, Dinh Xuan Sinh, Pham Phu LOC,Ly Van Chuong,
Tran Thi Hong Chau, Nguyen Thi Hoang Mai, Delia B. Bethell, Nguyan Hoan Phu, Tran Tinh Hien,
and Nicholas J. White
In tropical areas, where unsupervised use of antimalarial
drugs is common, patients with an illness consistent clinically with severe malaria but with negative blood smears
pose a management dilemma. Malaria pigment isevident in
peripheral blood leukocytes in greater than 90% of patients
with severe malaria. To characterize the clearance kinetics
of parasitized erythrocytes and malaria pigment-containing
leukocytes, sequentialperipheral bloodand intradermal
smears were assessed in 27 adult Vietnamese patients with
severe falciparum malaria. The clearance ofparasitized
erythrocytes and pigment-containingmonocytes (PCMs)followed first order kinetics. The elimination of pigment-containing neutrophils (PCNs) was first order initially, but deviatedfromthiswhen
counts werelow.
Clearance of
peripheral blood PCMs (median clearance time, 216 hours;
range, 84 t o 492 hours) was significantly slower than that
of parasitized erythrocytes (median, 96 hours; range, 36 t o
168 hours) or PCNs (median, 72 hours; range, 0 t o 168 hours;
P < .0001). Intradermal PCM clearance times were the longest of all (median, 12 days; range, 6 t o 23 days; significantly
longer than peripheral blood PCM clearance, P < .001).
Twenty-one (88%) patients still had signs, symptoms, or laboratory features of severe malaria after parasite clearance
but before phagocyte pigment clearance. Sixteen of the 23
surviving patients (70%; 95% confidence interval, 50% t o
87%) still hadintraleukocytic malaria pigment onperipheral
blood films 72 hours after parasite clearance. Thus, by determining the distributionof malaria pigment in peripheral
blood and intradermal phagocytes, the time since effective
antimalarial treatment startedcan be estimated. Microscopy
for intraleukocytic pigment isvaluable in the differential diagnosis of severe febrile illnesses in malarious areas where
uncontrolled use of antimalarial drugs is widespread.
0 1996 by The American Society of Hematology.
I
indicator in severe malaria and may be usedas an alternative
for diagno~is.~
We have conducted a prospective study todefine the clearance kinetics of pigment-containing phagocytes and parasitized red blood cells (RBCs) from the peripheral blood and
intradermal smears of patients undergoing treatment for
blood-slide-confirmed severe malaria. The aim of the study
was to ascertain whether detection of phagocyte pigment is
of value as a marker of recent falciparum malaria infection
in patients who are slide-negative for parasites, but have an
illness consistent with severe malaria.
N AREAS OF THE TROPICS endemic for Plasmodium
fakiparum malaria, patients are commonly admitted to
hospital with signs and symptoms consistent with a diagnosis
of severe malaria, but no parasites are detected on the peripheral blood smear.’ This creates a diagnostic and management
dilemma. It is likely that many of these patients indeed do
have severe malaria, but have received empirical treatment
at a primary health care level from clinics, pharmacies, or
shops or treated themselves with antimalarial drugs.’ This
problem is increasing in Southeast Asiawithmorewidespread availability of the qinghaosu derivatives. These compounds clear parasites more rapidly from the peripheral circulation than do other antimalarials.3 In regions where
malaria transmission is not intense and the overall prevalence
of infection is low, an easily detectable marker of recent
malaria infection would be valuable in the diagnosis and
thus the management of such patients. It has been suggested
that an intradermal smear taken from the volar aspect of the
forearm, a technique described originally by van der Berghe
and Chardome: may be positive for malaria parasites after
the peripheral blood has become negative. Intraleukocytic
pigment has recently been identified as a valuable prognostic
From the Centre for Tropical Diseases, Cho Quan Hospital, H 0
Chi Minh City, Vietnam: and the Centre for Tropical Medicine,
Nufield Department of Clinical Medicine,University of Oxford,
Oxford, UK.
Submitted April 10, 1996: accepted July 26, 1996.
Supported by The Wellcome Trust of Great Britain.
Address reprint requests to Nicholas J. White, MD, Wellcome
Trust Clinical Research Unit, Centre for Tropical Diseases, Cho
guan Hospital, H0 Chi Minh City, Vietnam.
The publication costsof this article were defrayedin part by page
charge payment. This article must therefore be hereby marked
“advertisement” in accordance with 18 U.S.C. section 1734 solely to
indicate this fact.
0 I996 by The American Society of Hematology.
0006-497//96/8812-00I7$3.00/0
4694
PATIENTSANDMETHODS
Patients
This study was performed in the malaria intensive care unit of
the Centre for Tropical Diseases (Ho Chi Minh City, Vietnam), an
infectious disease referral center for much of southern Vietnam. The
study was approved by the Ethical and Scientific Committee of the
Centre, and informed consent was obtained from each patient or, if
the patient was comatose, from their attendant relatives. Consecutively admitted adult patients with severe malaria’ were entered into
the study if they had phagocyte pigment and asexual forms of Plasmodium falciparum on their admission peripheral blood film. Most
patients were also enrolled in a double-blind comparison of intramuscular artemether (4 mgkg loading dose followed by 2 mgkg every
8 hours until able to take oral drugs) and quinine dihydrochloride
(20 mg saltikg followed by I O mgkg every 8 hours) in severe
malaria that is still ongoing and remains blinded; the remainder
received either artesunate or quinine intravenously in accordance
with published guidelines? Treatment with antimalarial drugs before
admission to the study was not an exclusion criterion.
Procedures
Both peripheral and intradermal blood films were taken at 12hour intervals after admission until two sequential pairs of slides
were negative for both asexual forms of the parasite and phagocyte
pigment on both the thick and thin films. The intradermal films were
made by making several very small intradermal pricks within a small
area on the volar aspect of the forearm with a sterile 23-guage
Blood, Vol88, No 12 (December 15). 1996: pp 4694-4700
From www.bloodjournal.org by guest on March 6, 2016. For personal use only.
4695
MALARIAPIGMENT AND PARASITECLEARANCE
needle, gently squeezing the area, and applying the sero-sanguinous
fluid produced to a slide. The thin films were stained with reverse
Field’s stain,’ and the thick films were stained with Giemsa. Parasite
counts were reported from thin films as parasitized RBCs per 1,000
RBCs and converted to quantitative counts by correcting for the
RBC count. Thick films counts were reported as parasites per 400
leukocytes. Thick film counts per microliter of blood were obtained
by assuming a white blood cell (WBC) count of 8,0oO/pL, and thin
film counts were obtained by adjusting for the number of RBCs per
microliter. The diameter of each thick film was approximately 10
mm. Phagocyte pigment was reported as pigment-containing neutrophils (PCNs) per 1 0 0 neutrophils and pigment-containing monocytes
(PCMs) per 30 monocytes, as described previously? Malaria pigment is easily seen and is characteristic in appearance. Once the
pigment count had fallen below 1 pigment-containing cell per 100
neutrophils or per 30 monocytes or the parasite count had fallen
below one parasite per 400 WBCs, slides were reported qualitatively
as either positive or negative; however, slides were only reported as
negative for either parasites or phagocyte pigment after the entire
thick film had been scanned. The last positive slide for each parameter on each type of smear (6 slides per patient) was carefully counted
in its entirety (ie, numerator = total parameter count on the slide;
denominator = total number of WBCs on the slide) to allow an
empirical estimate of the level of detection possible using light microscopy of the thick film. Slides were read by two expert technicians
who were blinded as to the identity and clinical details of the patients.
Patients remained on the ward until either death or complete clearance of both parasites and phagocyte pigment.
Statistical Analysis and Modelling of Clearance Curves
Statisrics. Continuous variables were assessed for normality by
visual inspection of histograms and the Shapiro-Wilks W test (using
Stata; Stata Corp, College Station, TX). Data were expressed as
means or medians as appropriate with t-distribution or binomialbased 95% confidence intervals (CI), respectively. 95% exact C1 for
proportions (such as sensitivities) were calculated according to the
method of Miettinen.’Clearance times (which were normally distributed) were compared using repeated measurements analysis of variance (SuperANOVA; Abacus Concepts, Berkeley, CA) with smear
type and marker type as within patient factors. The Bonferroni correction was applied to the significance levels obtained from multiple
contrasts between means.
Kinetics. For each patient and for each combination of slide type
and clearance marker, an exponential decay equation of the form y
= Ae-”‘ was fitted to the sequential 12-hour counts, where “t” is
time in hours, “A” the count at t = 0, and “o“ the first order rate
constant. This gave a better curve fitthan a double exponential
equation of the form y = Ae-”‘ + Be-4‘ based on residuals assessed
by the Aikake Information Criterion.’ Data series in which the initial
counts were less than 5 (or < 100/pL in the case of parasite counts)
were excluded from the curve fitting, as were the increasing data
points of those series in which the counts increased before declining
(in all cases, only the first point in such series). A and “a” were
derived for each data series for each patient and then mean values
were calculated for all patients. The object was to model the exponential decay phase of each of the counted parameters. The curve
fitting was performed using the statisticallgraphing computer software packages CricketGraph (Computer Associates, New York, NY)
and the NonLin module of StatisticalMac (Statsoft, Tulsa, OK). The
decay phase half-lives were calculated using the equation Ln ( 2 ) h ,
and means were analyzed between slide type and clearance marker
by the same method as that used for clearance times. Estimated
limits of detection were obtained by dividing each patient’s parasite
clearance time minus 12 hours (the last time the parameter of interest
is seen on a smear) by the derived half-life and then applying this
Table 1. Admission Clinical Features
Clinical Feature
No. of Patients (n = 27)
Cerebral (Glasgow coma score <11)
Jaundice (total
bilirubin
>2.5 mg/dL)
Acute renal failure (creatinine >3 mg/dL)
Hyperparasitemia (>500,OOO/pL)
Generalized convulsions
Severe anemia (hematocrit 120%)
Pulmonary edema
Hypoglycemia (glucose <40 mg/dL)
19 (70%)
19 (70%)
10 (37%)
5 (19%)
4 (15%)
4 (15%)
1 (4%)
1 (4%)
number of half-lives before clearance to the original admission count
to obtain the estimated count just before clearance. Using the Wilcoxon matched-paired signed-rank test, this derived limit of detection was then compared for each parameter and smear type, with
the empirical limit of detection obtained from quantitation of the
last positive slide. The null hypothesis was that the clearance process
followed first order kinetics throughout, so there should be no significant difference between the two estimates.
RESULTS
Clinical Features
Of the 27 patients entered into the study, 22 (81%) were
male. This proportion is similar to the overall severe malaria
admissions to this hospital. The mean (standard deviation)
age was 30.1 (12.5) years. Twelve (44%) cases were known
to have taken antimalarial drugs for up to 2 days before
entry to the study. Seven patients (26%) reported having had
malaria one or more times in the past. The admission clinical
features of the patients are summarized in Table 1. More
than one complication of severe malaria was present in 20
of the 27 patients. Six (23%) developed gastrointestinal
bleeding, and 9 patients (35%) required one or more blood
transfusions for either bleeding or severe anemia. Seven
(70%) of the 10 patients with acute renal failure required
dialysis, and 2 of these died subsequently. Overall, 4 patients
(15%) died; the median time to death was 130 hours (range,
52 to 249 hours). This mortality rate is similar to the overall
mortality for strictly defined severe malaria cases at this
center.
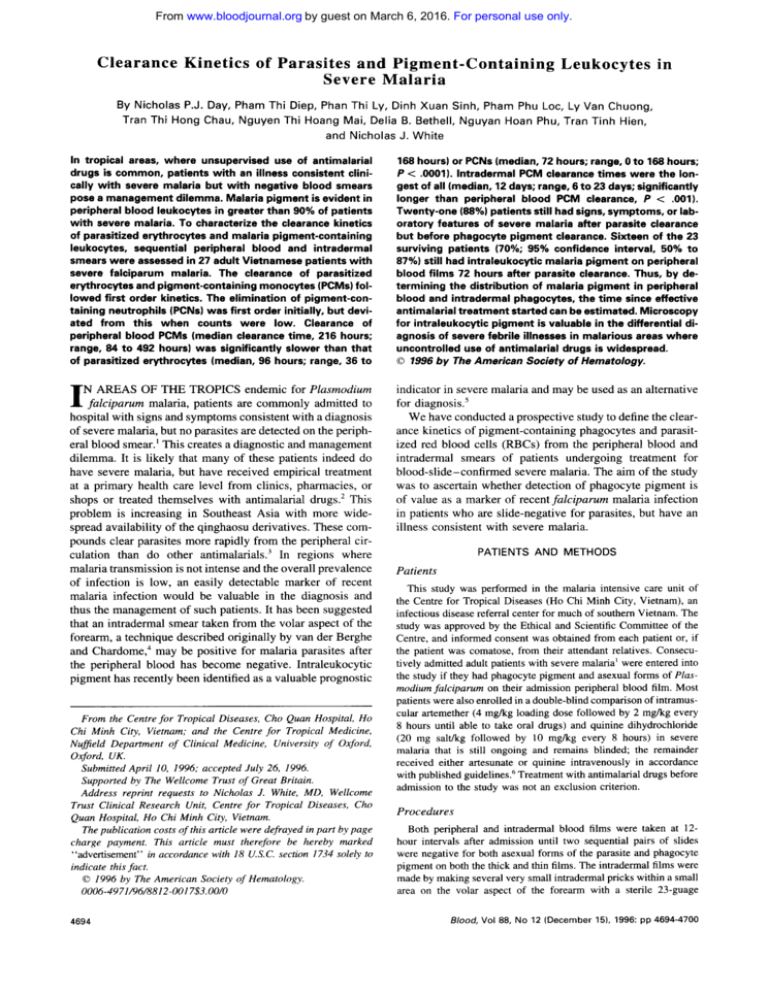
Clearance Times
The admission counts and clearance times for intradermal
and peripheral blood parasitized erythrocytes and phagocyte
pigment are summarized in Table 2, and the mean clearance
times with 95% C1 are shown in Fig 1. Three patients died
before parasite clearance. Clearance times using intradermal
smears were significantly longer than those using peripheral
blood smears for pigment-containing phagocytes ( P <
.OOOS), but were similar for parasitized erythrocytes ( P =
.99). PCNs cleared significantly more slowly than parasites
on the intradermal films ( P < .Ol), but rates were similar
on peripheral blood films ( P = .99). Both intradermal and
peripheral bloodPCMs cleared considerably more slowly
than either parasites or PCNs ( P < .OOl). In all patients, the
PCM clearance time waslonger than the PCN and parasitized
erythrocyte clearance times, regardless of which type of film
From www.bloodjournal.org by guest on March 6, 2016. For personal use only.
DAY ET AL
4696
Table 2. Parasite and Pigment-Containing Leukocyte Clearance
Parasite Count
n
(h)
=
Peripheral
27
Pigment-Containing Neutrophils*
Intradermal
Admission
count
90,500 (32,000
to 250,000,
80-1,100,000) pL”
82.000 (21,200
Clearance
time
Empirical limit
of detection
96 (78 to 113,
(80
96
36-168)
5.9 (3.5 to
7.9. 0.18-18.6) pL”
to 158,000,
40-910.000) pL
to72108,
36-204)
2.3 11.4 to
4.7, 0.35-22) pL
l1
Pigment-Containing Monocytest
Peripheral
Intradermal
Peripheral
Intradermal
to 6.1)/100
neutrophils
165 (55 to 337,
0-1.540) pL
(49 to 95,
0-168)
5.5* (2.1 to 8.3,
0.21-221 pL”
0.1 10.04 to 0.15,
0.004-0.41/
100 neutrophils
6 (2 to 9.9)/100
neutrophils
330 (110 to 544,
0-1.430) pL”
120 (75 to 144,
0-408)
3.91 12.0 to 7.2,
0.35-22)
0.071 (0.037 to
0.13, 0.007-0.431/
100 neutrophils
6 (3.9 to 9.1)/30
15 110 to 18)/30
monocytes
250 (168 to 300,
67-400) pL
288 (229 to 347,
144-552)
6.1 (4.7 to 9.3,
0.24-17.91pL
0.36 (0.28to
0.56, 0.015-1.1)/
30 monocytes
3
’
monocytes
100 (66to 151,
0-3161 pL
216 (180 to 240,
84-492)
4.0 (3.4 to 7.0,
1.3-13.5) pL”
0.14 (0.08to
0.28,0.02-1.3)/
30 monocytes
‘
Median values are shown, with the 95% Cl range in parentheses.
Conversion of pigment-containing cells per 100 neutrophils to pigment-containing neutrophils per microliter of blood based on assumed neutrophil count of 5,500
pL”.
t Conversion of pigment-containing cells per 30 monocytes to pigment-containing monocytes per microliter of blood based on assumed monocyte count of 500
pL”.
Significantly lower than model-derived median limit of detection, P < .02.
5 Significantly lower than model-derived median limit of detection, P < ,005.
$
was examined. Intradermal PCM clearance times were the
longest of all, with a mean of 12.6 days (95% Cl, 10.6% to
14.7%; range, 6 to 23 days), and were significantly longer
than peripheral bloodPCM clearance times (mean difference, 75 hours; 95% CI, 44 to 106 hours; P < .001). In
every patient, peripheral blood phagocyte pigment clearance
was slower than parasite clearance; pigment in peripheral
blood phagocytes was still detectable for a median period
of 4.8 days (95% CI, 2.6% to 6.8%; range, 1.5 to 19 days)
after peripheral parasite clearance. After parasite clearance,
but before phagocyte pigment clearance, 21 of 24 patients
(88%) still had signs, symptoms, or laboratory features of
severe disease: 12 patients (50%)were severely anemic (hematocrit level, <20%); 11 were still clinically jaundiced; 15
(63%) had residual renal impairment (serum creatinine level,
>1.5 mg/dL), of whom 2 were still undergoing dialysis; 9
of the 19 cerebral cases (47%) had a Glasgow coma score
(GCS) of less than 15; and 3 still had unrouseable coma
(GCS < I 1). One patient with cerebral malaria, jaundice,
severe anemia, and renal failure requiring dialysis cleared
parasites from the peripheral blood after 5 days and died 5
days later, when his peripheral and intradermal smears were
both still positive for neutrophil and monocyte pigment.
In this series of selected cases in which peripheral blood
phagocyte pigment was present on admission, pigment was
present for greater than 3 days after parasite clearance in 16
of 23 surviving patients, giving a sensitivity for the diagnosis
of malaria infection of 70% (exact 95% Cl, 50% to 87%).
Because 92% (95% CI, 88% to 95%) of smear-positive severe malaria patients in our center have phagocyte pigment
evident on admission (279 of 303 consecutive patients with
severe malaria), assuming conservatively that patients nega-
Intradermal pigment-containing
monocyte clearance time
Peripheral pigrnent-containing
monocyte clearance time
Intradermal pigment-containing
neutrophil clearance time
Peripheral pigment-containing
neutrophil clearance time
Intradermal parasite
clearance time
Peripheral parasite
clearance time
0
50
loo
*O0
250
Mean (95%Confidence
Intervals)
hours
time
ance
in
Fig 1. Mean parasiteand pig
ment-containing leukocyte dear-
times.
From www.bloodjournal.org by guest on March 6, 2016. For personal use only.
T
)
MALARIA
4697
Table 3. Parasite and Pigment-Containing Leukocyte Fitted Clearance Curves (n = 27)
Parasites
Curve Fit (y = Ae-“‘)
A
a (h“)
Peripheral
87,500
(9,400
to
220,000)
pL” @L”
Pigment-Containing Neutrophils*
Intradermal
82,000 (20.800to
pL” 333,000) pL”
(0.094
0.126
to
0.141)
No. of curves fitted
27 (100%)
r2 (mean
(0.124)
[SDI)
0.828
(0.146)
0.805
10.0756)
0.861
10.0926)
0.883
(0.0605)
0.892
(0.0889)
0.906
Half-life (hr)
5.5 15.1 to(5.2
7.1
7.5,
10.6-47.0)
3.5-21.2)
2.7-16.7)
No. of half-lives before
14.2
(11.6
to 16.7)
13.1
(10.5
clearance
Model-derived limitof
2.3
(1.4 to 7.8,
detection*
0.0005-20) pL”
Peripheral
Intradermal
526 (300 to 948)
483 (388 to 895)
9.6 (5.4 to 17.W
100 neutrophils
8.8(7.1 to 16.3)l
0.098 (0.068to
0.039 10.033 to
21 (78%)
13 (48%)
Pigment-Containing Monocytest
Peripheral
Intradermal
165 (115 to292
200)
pL”
9.9
(6.9
to 12V30
monocytes
(252 to 345)
pLC
17.5 (15.1 to
20.6)/30
monocytes
0.038 10.029 f
0.016 (0.013 to 0.02)
(0.00127
0.013
13 (48%)
22 (81%)
24 (89%)
100 neutrophils
to
0.138)
to 10.7,
18.5
(16.3 to 21.1,
18.5
to 15.6)
5.0
13.5
4.2 (1.3 to 12.2,
30.85
(5.1
0.12-18.9) pL”
to 6.6)
to 43,
0.34-59) pL”
0.56
(0.093-0.78,
0.12
0.006-1.1)/
100 neutrophils
(11.4 to 25.7,
44.7
(4.8
7.2
to 9.7)
(4.2
5.9
15.8¶
(10.4 to 25,
0.58-185) pL”
(0.017 to
o.oo1-1.1)/
0.40,
100 neutrophils
(35.4 to 54.4,
52.8
(45.5
to 7.7)
2.0 (1.4 to 10.1,
(3.2
4.8
0.001-1.1) pL”
0.12 (0.08to 0.61, 8
X
to 7)/
30 monocytes
to 60.2,
(5.0
5.7
to 6.2)
to 7.6,
0.18-56) pL”
0.29(0.19 to 0.45.
0.01-3.4)1
30 monocytes
Median values are shown, with the 95% Cl in parentheses.
Conversion of pigment-containing cells per 100 neutrophils to pigment-containing neutrophils per microliter of blood based on assumed neutrophil concentration
of 5,500 pL”.
t Conversion of pigment-containing cells per 30 monocytes to pigment-containing monocytes per microliter of blood based on assumed monocyte concentration of
500 @L”.
Admission Count
*Calculated from: Derived Limit of Detection =
2(ClearanceTime/Derived Half-Life)’
5 Significantly higher than empirically derived median limit of detection, P < .OZ.
Significantly higher than empirically derived median limit of detection, P < ,005.
tive for phagocyte pigment on admission remain negative,
then the estimated diagnostic sensitivity for malaria of peripheral blood phagocyte pigment greater than 3 days after
parasite clearance is 64% (95% CI, 45% to 82%). After 5
days, the sensitivity of such a test decreases rapidly, although
peripheral blood phagocyte pigment was detected for up to
17 days after parasite clearance.
Clearance Kinetics
Curves were fitted successfully to 110 of the 162 data
series (6 series for each of 27 patients), and the results are
shown in Table 3. The lowest success rate was in the peripheral and intradermal PCN series because of low initial
counts. Figure 2A and B shows the raw counts pooled across
patients and plotted against time. This does not take into
account the shape of each individual clearance curve. The
curves shown in Fig 2C and D are derived from the means
of (Y for each clearance marker. These curves give a better
representation of the average clearance curve, because each
value of (Y used in calculating the mean describes the shape
of an individual patient’s clearance curve.
Parasite and pigment-containing phagocyte elimination
rates, or elimination half lives, were not significantly different between peripheral and intradermal smears ( P = SS).
However, both PCM and PCN half lives were significantly
longer than parasitized erythrocyte half lives ( P < .0001 and
P < .05, respectively), and PCM half lives were longer than
PCN half lives ( P < .0005). Model-derived and empirical
limits of detection for all the markers on both peripheral
and intradermal smears are all between 2 and 35 parasitized
erythrocytes or pigment-containing phagocytes per microliter. Derived limits of detection of peripheral and intradermal
parasites and PCMs were not significantly different from the
empirical limits, suggesting that the clearance processes for
these two parameters followed first order kinetics throughout. However, for PCNs, the actual counts atthe limit of
detection on both peripheral and intradermal smears were
significantly lower than those predicted by thefirst order
model derived from the earlier higher counts ( P < .02 and
P < .005, respectively). This suggests that in the early stages
PCN clearance follows first order kinetics, but at low counts
the clearance of PCNs is faster than this model predicts.
DISCUSSION
Malaria pigment, or hemozoin, is produced by parasites
during intraerythrocytic development as the end product of
hemoglobin digestion. It consists of a polymer of heme
groups linked by iron carboxylate bonds and is readily seen
by light microscopy as a refractile brown-black intraparasitic
aggregate (resembling coal) in older trophozoites and meronts (schizonts). At merogony (schizogony), the parasitized
erythrocyte bursts, releasing a number of daughter merozoites and some of this pigment into the blood stream, leaving
behind anRBC ghost and exposed parasite remnants, including residual malaria pigment. In the case of P falciparum,
the RBC ghosts and pigment remain adherent to vascular
endotheli~m.~
The free particulate pigment and eventually
these cytoadherent RBC ghosts are phagocytosed by scavenger monocytes and neutrophils. If the parasite burden has
been large enough, then intraleukocytic pigment is easily
seen on light microscopy of the peripheral blood film. The
proportion of peripheral blood neutrophils and monocytes
containing pigment is related to the size and synchronicity
of the parasite burden undergoing schizogony and has been
shown recently to be related to the clinical severity of the
malaria infe~tion.~
In this referral center in Southern Viet-
From www.bloodjournal.org by guest on March 6, 2016. For personal use only.
4698
DAY ET AL
smearsPeripheral
Intradermal
blood smears
15
- Mean peripheral parasite count
-
Mean peripheral pigmentcontaining neutrophilcount
Mean peripheral pigment-containingmonocyte count
E m baa am 95%
nemb
125
-
E
g
--m
-:c
Mean unradennal parasite count
Mean intrademat plgment-mntaining
neutrophil
count
intradermal
Mean
pigment-containing
monocyte
count
1
E m barn are 95%mnMPnce ntervab
0.75
0
2 0.5
5
g 0.25
0
The
..........
In
hours
Peripheralparasite dearance curve
Peripheralpigment-containingneutrophilclearancecurve
Peripheral pigment-mntalnlng monocyte dearanm curve
nrne in houn
-
Intradermal parasiteClearance CUNB
lntradennal pgment-containingneutophilclearancecurve
lntradennal plgment-uxltaining monocyte dearanm curve
........ ..............._,..
...e
nm
In houn
Tlme in hours
Fig 2. Plots of mean raw counts against time (graphsA and B) and of the derived functions describingthe decay phase only (graphsC and
to each patient data series.
D).The latter were calculated using the means of the constant CY derived from exponential functions fmed
nam, 92% (95% CI, 88% to 95%) of patients with slidelimits of detection and were compared with the actual observed
positive severe and complicated malaria have intraleukocytic
limits of detection deduced from exhaustive counting
of the last
pigment on the admission peripheral blood film.
positive blood slide. For parasitized erythrocytes and PCMs, the
Changes in parasitemia infalcipmm malaria result from the derived and observed values were not significantly different,
net balance between parasite production (asexual multiplicationprovidingstrongevidencethattheelimination
ofthese two
rate), sequestration, and elimination." Changes in the numbers markers followed first order kinetics throughout. For PCNs, the
ofpigment-containing phagocytesderivefromsimilarprovalues wereof similar magnitude but differed significantly; the
cesses (ie, production rates, vascular ingress and egress, and
derived value was higher than the observed value.
This suggests
cell lie-span), although each with different time constants. In
that, as the densityof PCNs decreased, the processesthat detersevere malaria, leukocytosis may occur in the most seriously
mined their numbers in the peripheral blood departedfrom first
ill patients,but, in general, W C countsremainconstant
order kinetics and their rate of disappearance increased. Becauseof the high production rates and short half-life of the
throughout the disease provided that there are no bacterialsuneutrophils, the balance of factors dictating clearance is likely to
perinfections.' As patients are treated, the numbers of parasitized erythrocytes and pigment-containing phagocytes decrease be different from those involved
in parasite and PCM clearance,
becausetheerythrocyteandmonocytehaveasubstantially
and eventually disappear, although until recently the kinetics
longer clearance time.
of this process have been poorly defined, evenfor parasites. In
Clearance times estimated from peripheral blood films are
the early stagesof parasite and pigment clearancein this study,
dependent on the limit of detection by light microscopy and
when absolute counts were high, first order elimination kinetics
the experience, skill, and diligence of the microscopist. In
fitted thedata well for allthree measurements (parasites, PCNs,
routine practice, the limit of parasite detection is usually
and PCMs); ie, the rate of decrease in the density (or concentraconsidered to be 20 to 50 parasites per microliter. The metion) of cells containing the marker at a given time was propordian lowest parasite count detectable on thick blood smears
tional to the density of those cells at that time." It is difficult
in this detailed study was just less than YpL, which is marto followthis process accurately once the density
of the marker
ginally lower than the values of between 5 and 40 parasited
decreases to levels near the limit of detection. To determine
pL derived by other investigator^.'^.'^ The estimated limits
whether this one compartment open model remained valid at
of detection of PCNs and PCMs were similar. Given that
low concentrations, the half times derived from the early part
pigment particles are approximately the same size as a ringof the clearance curves were used to derive estimates for the
From www.bloodjournal.org by guest on March 6, 2016. For personal use only.
MALARIA PIGMENT AND
PARASITE CLEARANCE
stage P falciparum parasite, we conclude that the factors
influencing parasite and pigment detection (ease of recognition, confusion with artefacts, and smear quality) are similar.
Li et all4 have suggested that the counts made on intradermal smears are representative of the sequestered parasite
biomass and that intradermal smears can be used as an alternative to bone marrow smears in patients suspected of having
malaria but having a negative peripheral blood smear. The
usefulness of this approach is limited by the low level of
sequestration in dermal microvasculature'5 and the problem
of variable contamination of the smear with capillary and
arteriolar blood from subdermal structures. In the current
study, parasite clearance times from intradermal smears were
similar to peripheral blood estimates. This lack of difference
in parasite clearance despite a relative increase in the proportion of mature parasite stages in the intradermal smear may
be explained by the effects on different stages of parasite
development of most antimalarial drugs and different clearance processes involved for circulating and sequestered infected erythrocytes.*After treatment and later on in the parasite clearance process, it is likely that only a few viable
mature sequestered parasites will remain, because most antimalarial drugs act preferentially on these more mature trophozoites rather than on the young circulating ring forms.
The fate of the dead cytoadherent parasites is not known,
although this study indicates they are cleared rapidly, presumably by phagocytosis, because there is no evidence that
they are released intact into the circulation. However, RBCs
containing dying or dead parasites are more likely to be
cleared by the spleen, so it remains possible that these dying
trophozoites are released into the circulation and are cleared
so rapidly that they never reach the level of microscopic
detection. This is unlikely, because ultrastructural studies
show that even residual RBC membranes remain cytoadherent after schi~ogony.~
The more mature schizonts will have
undergone merogony (even after antimalarial drug exposure
as they are relatively drug-resistant16), and the new young
ring forms will be circulating in the peripheral blood. These
young rings are relatively drug-resistant, particularly to quinine. The processes of phagocytosis of dead cytoadherent
parasitized erythrocytes and peripheral ring clearance and
sequestration presumably occur at approximately the same
rates.
The opportunities for phagocytic cells to ingest pigment
include the clearance of particulate material released into the
circulation at merogony, the phagocytosis of either mature
parasitized RBCs or RBC ghosts produced as a byproduct of
merogony, and the phagocytosis of living or dead pigmentcontaining phagocytes. The first and second of these depend
on the existence of an actively reproducing malaria infection,
although it is unclear how rapidly RBC ghosts are phagocytosed. Because the half-life of a neutrophil is short (about 9
hours) and there is little difference between parasite and
PCN clearance times, it is likely that pigment phagocytosis
occurs rapidly after merogony (or before) and that neutrophil
phagocytosis of other pigment-containing phagocytes is uncommon. The long PCM clearance time may result from a
combination of factors: the long life of the PCMs themselves
and the ingestion by scavenger monocytes of PCN remnants
4699
long after resolution of the infection. PCMs may also be
moreefficient at scavenging cytoadherent material than
PCNs.
The clearance times of pigment-containing phagocytes
from intradermal smears are considerably longer than from
peripheral blood smears. This difference may reflect margination or vascular egress from the dermal microvasculature
of scavenger leukocytes after phagocytosis of the pigment
present in local cytoadherent RBC ghosts, as suggested previously.2 The long clearance time of PCMs makes this the
most useful late marker of malaria infection, although, when
present, PCNs have greater prognostic ~ignificance.~
In the
absence of parasitized erythrocytes, PCNs are an accurate
marker of recent infection, because their short half-life provides a limited time window in which parasite clearance can
have occurred. Furthermore, they indicate that a large parasite burden must have been present, whereas the finding of
monocyte or macrophage pigment does not necessarily imply
such a large burden, because the lower clearance of PCM
pigment will allow a higher steady state to be acheived for
any given input (ie, number of parasitized RBCs undergoing
schizont rupture or phagocytosis). We predict that PCMs but
not PCNs would be observed relatively commonly in areas
of high transmission where malaria infections are frequent
or continuous. In this epidemiologic context, severe malaria
is largely confined to childhood. In areas of very high transmission (eg, more than20 infections per year), severe anemia
is the predominant clinical presentation of severe falciparum
malaria, whereas at lower levels of transmission, cerebral
malaria and metabolic acidosis predominate. The finding of
PCNs should still indicate a recent heavy parasite burden,
but PCMs could reflect either a recent severe infection, a
protracted infection, or a series of repeated infections.
Is phagocyte pigment useful clinically as a marker of recent malaria infection? We have studied adult patients
known to have severe malaria and obtained estimates for
sensitivity at different times after parasite clearance. Approximately two thirds of the patients admitted with severe malaria had detectable phagocyte pigment on their peripheral
smears 3 days after parasite clearance, which suggests that
phagocyte pigment would have useful sensitivity as a test for
malaria in pretreated, parasite-negative, severely ill patients.
However, several questions remain regarding specificity and
practicality. In areas of relatively low malaria transmission
such as Vietnam, the chance of finding pigment produced
by a coexisting relatively asymptomatic malaria infection in
a patient severely ill from another cause is very low. This
may not be so in holoendemic areas where the population
level of malaria immunity and the prevalence of parasitemia
are high. This clearly needs further study. Whether other
species of Plasmodium produce similar levels of circulating
pigment-containing phagocytes is unknown, although our
preliminary observations with P v i v a suggest this will not
be a confounding factor. Other biologic structures and film
artefacts may be misidentified as pigment. In our experience,
technicians and doctors adept at examining blood films for
parasites require little extra training to become competent at
pigment recognition. Whether use of buffy coat smears or the
use of birefringence to increase the sensitivity of hemozoin
From www.bloodjournal.org by guest on March 6, 2016. For personal use only.
4700
DAY ET AL
7. White NJ, Silamut K: Rapid diagnosis of malaria. Lancet
detection will improve the sensitivity of pigment detection
I :435, 1989
remains to be established.
8. Miettinen OS: Estimation of relative riskfromindividually
In conclusion, the clearance of parasitized erythrocytes
matched series. Biometrics 26:75, 1970
and PCMs follows first order elimination kinetics up to the
9. Chatfield C (ed): The Analysis of Time Series (ed 4). London,
limit of microscopic detection.
PCN clearance follows the
UK, Chapman and Hall, 1989
same kinetics in the early stages of the process, but deviates
I O . White NJ, Chapman D, Watt G: The effects of multiplication
from it when counts are low. Phagocyte pigment can be usedand synchronicity on the vascular distribution of parasites in falcipato diagnose severe malaria after clearance of parasites from
rum malaria. Trans R Soc Trop Med Hyg 86590, 1992
the peripheral blood.
1 I . Pasvol G, Newton CR, Winstanley PA, Watkins WM, Peshu
NM, Were JB, Marsh K, Warrell DA: Quinine treatment of severe
ACKNOWLEDGMENT
fakiparum malaria in African children: A randomized comparison
of three regimens. Am J Trop Med Hyg 45:702, 1991
We thank the medical and nursing staff
of the severe malaria ward
12. Payne D: Use and limitations of light microscopy for diagnosat the Centre for Tropical Diseases for their help with this study.
ing malaria attheprimaryhealth
care level. WHOBull 66:6214,
REFERENCES
1988
13.WorldHealth
Organization: Biologyof malaria parasites.
I . World Health Organization: Control of tropical diseases. SeTechnical report series 743. Geneva, Switzerland, World Health Orvere and complicated malaria. Trans R Soc Trop Med Hyg 80: I ,
ganization, 1987
1990 (suppl 2 )
14. Li QQ, Guo X, Jian H, Fan T, Huang W: Development state of
2. Silamut K, Hough R, Eggelte T, Pukrittayakamee S, White
Plusrnodiunl fakiparum in the intradermal, peripheral and medullary
NJ: Simple methods for assessing quinine pre-treatment in acute
blood of patients with cerebral malaria. Nat Med J China 63:692,
malaria. Trans R Soc Trop Med Hyg 89:665, 1995
1983
3. Hien TT, White NJ: Qinghaosu. Lancet 341:603, 1993
15. MacPherson GC, Warrell MJ, White NJ, Looareesuwan S,
4. van den Berghe L, Chardome M: An easier and more accurate
Warrell DA: Human cerebral malaria. A quantitative ultrastructural
diagnosis of malaria and filariasis through the use of the skin scarifianalysis of parasitized erythrocyte sequestration. Am J Pathol
cation smear. Ann J Trop Med Parasitol 3 1 :41I , 1951
I19:385, 1985
S . Phu NH, Day NPJ, Diep PT, Ferguson DJP, White NJ: Leuko16. ter Kuile F, White NJ, Holloway P, Pasvol G, Krishna S:
cyte malaria pigment and prognosis in severe malaria. Trans R Soc
Pla.rnzodium fulciparumt In-vitro studies of the pharmacodynamic
Trop Med Hyg 89: 197, 1994
properties of drugs used for the treatment of severe malaria. Exp
6. White NJ: The treatment of malaria. N Engl J Med 335:800,
Parasitol 76:86. 1993
1996
From www.bloodjournal.org by guest on March 6, 2016. For personal use only.
1996 88: 4694-4700
Clearance kinetics of parasites and pigment-containing leukocytes in
severe malaria
NP Day, TD Pham, TL Phan, XS Dinh, PL Pham, VC Ly, TH Tran, TH Nguyen, DB Bethell, HP
Nguyan, TH Tran and NJ White
Updated information and services can be found at:
http://www.bloodjournal.org/content/88/12/4694.full.html
Articles on similar topics can be found in the following Blood collections
Information about reproducing this article in parts or in its entirety may be found online at:
http://www.bloodjournal.org/site/misc/rights.xhtml#repub_requests
Information about ordering reprints may be found online at:
http://www.bloodjournal.org/site/misc/rights.xhtml#reprints
Information about subscriptions and ASH membership may be found online at:
http://www.bloodjournal.org/site/subscriptions/index.xhtml
Blood (print ISSN 0006-4971, online ISSN 1528-0020), is published weekly by the American
Society of Hematology, 2021 L St, NW, Suite 900, Washington DC 20036.
Copyright 2011 by The American Society of Hematology; all rights reserved.