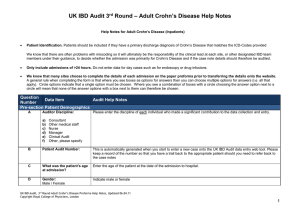
Integrated Pre-admission Assessment Form, Service Directory
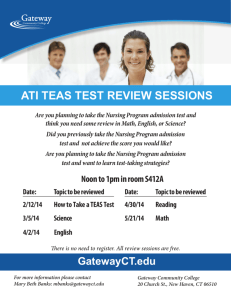
advertisement

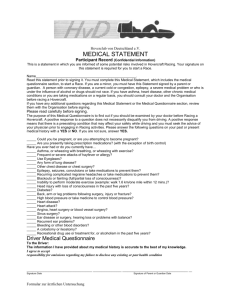
Integrated PREAC Form (Sample) The Royal Brisbane & Women’s Hospital PATIENT IDENTIFICATION LABEL: Health Service District INTEGRATED PRE-ADMISSION ASSESSMENT FORM UR No.: ___________________________________________ Name: ___________________________________________ Address: ___________________________________________ DOB: / / Male Female (or affix patient ID label here) TO THE PATIENT: Please fill in all the shaded areas on pages 1 & 2. Circle ‘Y’ or ‘N’ as appropriate or place a cross in the appropriate box. You can attend your GP to assist in completion of this form is necessary. Do you have any religious/cultural needs? Interpreter needed? No No Yes Home: Yes Language spoken: Do you have difficulties with speech, hearing, touch or vision? Are these contact details correct? Telephone Details: No No Work: Yes Other: Yes LOCAL DOCTOR (GP): Dr’s Name: Telephone: Fax: Address: Postcode: REASON FOR ADMISSION/PROCEDURE Pre-admission Date: TCI Date: Consultant: Admission Time: am pm DAY OF ADMISSION (Nurse): (Instructions for SDCU or WARD) SAFETY ALERTS: AT RISK OF FALLS? Patient colonised/infected with multi-resistant organisms? Medications taken? No No No Yes Yes Yes Patient belongings labelled? No Yes QUESTIONS ABOUT YOUR GENERAL HEALTH Past Medical History Please list any major problems with your health or surgery in the past 10 years (including any complications) Illness or Surgery Type Date A) B) C) D) Do you smoke? No Yes Have you ever smoked? When did you cease? No Yes How many & for how long? INTEGRATED PRE ADMISSION ASSESSMENT FORM Procedure Date: -2ALLERGIES: _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ RELEVANT HISTORY (Medical, Surgical, Social, Family) _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ CURRENT MANAGEMENT PLAN: _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ Signature: ________________________ Print Name: ___________________________ Date: ____/____/____ Designation: ___________________________ Do you have or have you ever had any of the following? 1. Asthma No Yes When? 2. Chronic or productive cough (bronchitis or bronchiectasis) No Yes Describe duration, colour & amount: 3. Home oxygen or CPAP No Yes Explain: 4. Shortness of breath or difficulty breathing (including when you are lying flat) No Yes 5. High blood pressure No Yes How long? 6. Chest pain, angina or heart attack No Yes Which/when? 7. Heart disease, artificial valve or pacemaker No Yes Which/when? 8. Rheumatic fever, heart murmur, irregular pulse or palpitations No Yes When? 9. Swelling of ankles No Yes 10. Blood disorder (eg. leukaemia or anaemia) No Yes What type/when? 11. Blood transfusion No Yes When? 12. Blood clots in legs or lungs No Yes Which/when? 13. Bleeding tendency or easy bruising No Yes When? 14. Diabetes No Yes How is it controlled? 15. Hepatitis, jaundice or cirrhosis No Yes What type/when? 16. Kidney disorder No Yes What type/when? 17. Gastric reflux, hiatus hernia or heartburn No Yes Which/when? 18. Epilepsy or other fits No Yes When? 19. Stroke No Yes What is affected? 20. Organ transplant No Yes Which/when? 21. Do you have an artificial joint, hearing aid, contact lenses No Yes Please specify: 22. Significant neck or back injury No Yes Explain: 23. Other serious illness or disabling condition No Yes What/when? 24. Was your last menstrual period more than 3 weeks ago? No Yes How many weeks? 25. Are you currently breast feeding? No Yes 26. Do you suffer from anxiety, depression or emotional disorders? No Yes 27. Do you drink alcohol? No Yes How much a day? 28. Do you have any allergies (drugs/food/tapes)? No Yes To what? When? CURRENT MEDICATIONS TAKEN: Regular & prn. Include ALL medications including over the counter medications, inhalers, topical, eyedrops & painkillers. Please bring them to hospital with you. Name A) B) C) D) E) Strength How many tablets per day? (number at each time) YOUR ANAESTHETIC HISTORY (This point forward to be completed by Hospital Staff Only) 30. Have you had a cough/cold/sore throat in the past fortnight? No Yes 31. Have you had any problems with anaesthetics or surgery before (eg. nausea, temperature, and prolonged drowsiness)? No Yes 32. Do you have any blood relatives who have had problems with anaesthetics? No Yes 33. Do you have any capped, false or loose teeth? No Yes 34. Is there any limitation in the movement of your neck or jaw? (you should be able to open your mouth at least 2 finger widths & be able to tilt your head to look straight up) No Yes 35. Does any condition prevent you from undertaking normal daily activities? No Yes 36. Do you have any other chronic pain conditions? No Yes 37. Tick the box most applicable to you Comments: Give details: Give details: Give details: Give details: What/when? Give details: A) No limitation to activity B) Slight limitation to activity, can walk one flight of stairs without resting C) Marked limitation of normal activity, cannot walk one flight of stairs without resting D) Pain or short of breath at rest 38. Do you have any questions or concerns about the anaesthetic, operation or coming into hospital you would like to discuss? No Yes ANAESTHETIC REFERRAL BY NURSE Day Surgery Day of Surgery Adm. Refer to Anaesthetist Surgery deferred Reason / Management: PHYSIOTHERAPY ASSESSMENT (if required) Medical & nursing assessment noted Other notes/alerts: Auscultation: Muscle power/ROM: Other specific tests/findings: Exercise tolerance: History DVT/PE Instructions given: TED - Size: SEQUENTIAL COMPRESSION - Size: Deep breathing Supported Huff Circulation Exercises Specific Instructions: Physiotherapist Name: Signature: Date: PLANNING FOR YOUR CARE (refer to nursing guidelines if answer is Yes) Accommodation House/Unit Number of stairs/steps Nursing Home Hostel Front/back: Retirement Village Internal: A) Will the patient’s occupation affect their recovery? No Yes B) Will you be by yourself at home when you leave hospital? No Yes C) Do you have dependants living with you? No Yes C) If you have dependants, do you have any problems making arrangements to care for them? No Yes D) Do you receive any community support services such as domiciliary nursing, home help, and meals on wheels or ambulance? No Yes E) Do you have any difficulty managing day to day activities such as stairs, bathing, dressing, going to the toilet or performing home duties? No Yes F) Have you had any falls in the last few months? No Yes F) Do you use a walking aid such as a stick or frame? No Yes G) Do you have any swallowing/eating difficulties or special dietary needs? No Yes G) Have you had a recent change in your weight? No Yes H) Have you any problems with passing urine or with your bowels? No Yes I) Have any communication difficulties been identified? No Yes J) Have any chronic conditions been identified? No Yes Weight: OBSERVATIONS (guidelines 39 – 42) B/P: Temp: Boarding Resps: Height: Which? Which? BMI: Pulse: Oxygen Saturation: K) Skin/Integument: does the patient have any wounds, ulcers, cuts bruises or other problems? Circle affected areas and describe: Pressure area risk score: PRE-ADMISSION PLAN No Discharge problems identified? Yes Education sheet discussed with patient Patient care plan completed? No Yes Post op pain education performed Vital signs recorded Nursing assessment completed by: Nurse’s name: Patient’s signature: Signature/designation: Date: Expected Discharge Date: