Varicosities, Treatment Alternatives to Vein Stripping and Ligation
advertisement

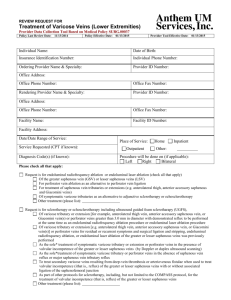
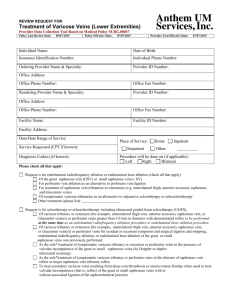
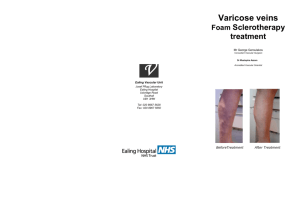
MEDICAL POLICY SUBJECT: VARICOSITIES, TREATMENT ALTERNATIVES TO VEIN STRIPPING AND LIGATION EFFECTIVE DATE: 04/19/01 REVISED DATE: 04/17/02, 12/19/02, 07/17/03, 03/18/04, 05/19/04, 04/21/05, 04/20/06, 04/19/07, 03/20/08, 09/17/09, 10/28/10, 05/19/11, 05/24/12, 06/20/13, 05/22/14, 06/18/15 PAGE: 1 OF: 9 POLICY NUMBER: 7.01.47 CATEGORY: Technology Assessment If the member's subscriber contract excludes coverage for a specific service it is not covered under that contract. In such cases, medical policy criteria are not applied. Medical policies apply to commercial and Safety Net products only when a contract benefit for the specific service exists. Medical policies only apply to Medicare products when a contract benefit exists and where there is no national or local Medicare coverage decision for the specific service. ***Note: This policy does not address vein stripping and ligation. Please refer to the nationally recognized InterQual standards regarding vein stripping and ligation.*** POLICY STATEMENT: I. Based on our criteria and review of peer-reviewed literature, treatment of documented symptomatic* varicose veins with reflux is considered medically appropriate when treated with the following techniques and when the patient has failed a course of conservative therapy: A. Ambulatory phlebectomy, transilluminated powered phlebectomy (TPP/TIPP, TriVex) and stab phlebectomy; B. Endoluminal radiofrequency ablation (e.g., VNUS® ClosureFAST™, ClosurePlus™); C. Laser ablation of the saphenous vein, including endovenous laser ablation (EVLA) of the saphenous vein (ELAS) or endovenous laser treatment (EVLT); or D. Compressive sclerotherapy (liquid or foam, including microfoam [e.g. Varithena™]) as an adjunct to prior or concomitant surgical treatment of venous reflux disease. *A patient is considered to have symptomatic varicose veins if any of the following signs and symptoms of significantly diseased vessels of the lower extremities are documented: A. stasis ulcer of the lower leg, or B. significant symptoms (e.g., pain, heaviness) that are refractory to a 12 week course of conservative therapy (e.g., utilization of compressive hose, systematic anti-inflammatories/analgesics, or activity modification), or C. bleeding associated with the diseased vessels of the lower extremities, or D. recurrent episodes of superficial phlebitis, or E. stasis dermatitis. II. Based on our criteria and review of peer-reviewed literature, the following are considered not medically necessary: A. Compressive sclerotherapy when performed for dermal or subdermal cosmetic lesions, for star and/or flare lesions, spider nevi, and/or telangiectasia; B. Microsclerosis (injection of telangiectasia or spider veins); C. Non-compressive sclerotherapy; or D. Transcutaneous laser ablation of telangiectasia. III. Based upon our criteria and review of the peer-reviewed literature, the following are considered investigational as the treatments have not been medically proven to be effective: A. Endovascular embolization with a cyanoacrylate adhesive (e.g., VenaSeal™ Closure System); B. Intense pulsed light source (photothermal sclerosis) in the treatment of superficial veins; C. Mechanochemical endovenous ablation (MOCA) (e.g., ClariVein®); D. Sclerotherapy as the sole treatment of varicose tributaries with documented reflux of the saphenofemoral junction or reflux isolated to the perforator veins of the upper thigh; E. Sclerotherapy of the greater saphenous vein with or without associated ligation of the saphenofemoral junction; F. Transcutaneous laser ablation of small diameter veins. Proprietary Information of Excellus Health Plan, Inc. A nonprofit independent licensee of the BlueCross BlueShield Association SUBJECT: VARICOSITIES, TREATMENT ALTERNATIVES TO VEIN STRIPPING AND LIGATION POLICY NUMBER: 7.01.47 CATEGORY: Technology Assessment EFFECTIVE DATE: 04/19/01 REVISED DATE: 04/17/02, 12/19/02, 07/17/03, 03/18/04, 05/19/04, 04/21/05, 04/20/06, 04/19/07, 03/20/08, 09/17/09, 10/28/10, 05/19/11, 05/24/12, 06/20/13, 05/22/14, 06/18/15 PAGE: 2 OF: 9 POLICY GUIDELINES: I. Treatment of some varicose veins may be considered cosmetic in nature. Treatment of varicose veins for cosmetic purposes is not medically necessary. II. The Federal Employee Health Benefit Program (FEHBP/FEP) requires that procedures, devices or laboratory tests approved by the U.S. Food and Drug Administration (FDA) may not be considered investigational and thus these procedures, devices or laboratory tests may be assessed only on the basis of their medical necessity. DESCRIPTION: The venous system of the lower extremities consists of the superficial system (greater and lesser saphenous veins) and the deep system (popliteal and femoral veins). These two parallel systems are interconnected via perforator veins. One-way valves are present at the junctions between the bifurcation point of the deep and superficial system (e.g., saphenofemoral and the saphenopopliteal junction). Varicose veins of the superficial system are typically secondary to valve incompetence. While most are secondary to incompetent valves at the saphenofemoral or saphenopopliteal junctions, a minority may be secondary to incompetence of valves within the perforator veins. Varicose veins may be asymptomatic or symptomatic. Although many varicose veins are asymptomatic, when they are present symptoms include itching, heaviness, aching legs, tension, and pain. In addition, varicose veins may be complicated by peripheral edema due to venous insufficiency, hemorrhage, thrombophlebitis, venous ulceration, and chronic skin changes. Larger varicose veins may be tortuous protruding above the surface of the skin. Treatment options typically focus first on identifying and correcting the site of reflux, and second to redirecting venous flow through veins with intact valves. Thus surgical treatment of varicosities associated with valve incompetence is based on the following three principles: I. Control of the most proximal point of reflux, typically at the saphenofemoral junction, as identified by preoperative Doppler ultrasonography. Surgical ligation is the most common form of treatment of the site of reflux. II. Isolation of the refluxing greater saphenous from the circulation. The most typical strategy for isolation is vein stripping, which is always preceded by ligation. III. Removal of the varicose tributaries. Strategies for this removal may include procedures such as stab avulsion or injection sclerotherapy, either at the time of the initial treatment, or subsequently. Over the years various different minimally invasive alternatives to ligation and stripping have been investigated. For example, sclerotherapy of the saphenous vein (as opposed to sclerotherapy of the varicose tributaries) is designed to promote fibrosis of the saphenous vein and thus remove it from the circulation. The term “varicose veins” does not apply to telangiectatic dermal veins, which may be described as spider veins or broken blood vessels. While abnormal in appearance, these veins typically are not associated with any symptoms (such as pain or heaviness) and their treatment is typically considered cosmetic in nature. Ambulatory phlebectomy Ambulatory phlebectomy (also known as microphlebectomy or microincisional phlebectomy) is the removal of varicose veins through a series of tiny incisions along the path of an enlarged vein. Prior to surgery the degree of reflux in incompetent veins is evaluated and the location of the veins is determined by Doppler ultrasound. The vessels are marked with a surgical marker. The surgical procedure is done under local tumescent anesthesia. Small pinhole incisions are made adjacent to the varicose veins. A small stripper head is inserted, turns the vein inside out and peels it away from the soft tissues of the leg through a minimal skin opening. Afterward the leg is wrapped with a compression bandage. Stab phlebectomy is a type of ambulatory phlebectomy also known as the “crochet hook” method of stab avulsion. Transilluminated powered phlebectomy (TPP/TIPP), also known as the TriVex procedure, is a minimally invasive type of ambulatory phlebectomy offered as an alternative to standard surgery for symptomatic varicosities of the leg. It is a 3-part procedure performed under general, regional, or local anesthesia, beginning with tumescent anesthesia to enhance Proprietary Information of Excellus Health Plan, Inc. SUBJECT: VARICOSITIES, TREATMENT ALTERNATIVES TO VEIN STRIPPING AND LIGATION POLICY NUMBER: 7.01.47 CATEGORY: Technology Assessment EFFECTIVE DATE: 04/19/01 REVISED DATE: 04/17/02, 12/19/02, 07/17/03, 03/18/04, 05/19/04, 04/21/05, 04/20/06, 04/19/07, 03/20/08, 09/17/09, 10/28/10, 05/19/11, 05/24/12, 06/20/13, 05/22/14, 06/18/15 PAGE: 3 OF: 9 visualization surrounding the varicose veins and to reduce operative discomfort. Tumescence anesthesia involves infusion of large amounts of saline mixed with lidocaine to reduce hemorrhage and epinephrine to delay absorption of lidocaine. Once adequate tumescent infiltration is achieved, the resector and illuminator are inserted and positioned underneath the skin through small (2-3 cm) incisions on either end of the varicosity. The tip of the resector follows the veins slowly to chop the veins an aspirate fragments. Once removal of the affected vein(s) is complete, a second stage tumescent anesthesia is employed to minimize blood loss, to reduce bruising and hematoma formation, and to decrease postoperative pain. The incisions are then closed using surgical tape or similar closures, and the leg is wrapped. Endoluminal Radiofrequency Ablation of Varicose Veins (VNUS®) Endoluminal radiofrequency ablation is a minimally invasive alternative to vein ligation and stripping. The technique relies on radiofrequency energy to damage the intimal wall of the vessel resulting in fibrosis and ultimately obliteration of a long segment of the vein, thus eliminating reflux. The procedure is performed by means of a specifically designed catheter (VNUS® ClosureFASTTM catheter, VNUS Technologies) inserted through a small incision in the distal medical thigh to within 1-2 cm. of the sapheno-femoral junction. High frequency radiowaves (200-300 kHz) are delivered through the catheter electrode and cause direct heating of the adjacent tissues. The vein is heated to approximately 120o C for 20second intervals to sequentially heat and ablate the vein in seven cm increments. Intense Pulsed Light Source Intense pulsed light source or photothermal sclerosis (such as PhotoDerm® VasculiteTM). The light source is not a laser and involves no needles or incisions. Treatment consists of small pulses of light energy traveling through the skin, which is absorbed by the blood, changed to heat, and the vein is destroyed. It is used for smaller surface veins. LASER (Light Amplification by the Stimulated Emission of Radiation) Ablation Laser ablation of symptomatic varicose veins, such as but not limited to endovenous laser ablation (EVLA) of the saphenous vein (ELAS) or endovenous laser treatment (EVLT), consists of a bare-tipped or ceramic coated tip laser fiber being introduced through a small incision into the greater saphenous vein under ultrasound guidance. The laser is activated, with the resulting heat at the tip causing a reaction in the walls of the vein, and then being slowly removed along the course of the saphenous vein. Damage to the intimal wall of the vessel results in fibrosis and ultimately obliteration of a long segment of the vein. The varicosities associated with this vein then disappear and blood from the lower leg reroutes through deeper circulation. Transcutaneous laser ablation of small diameter veins. A small spot of laser travels through the skin and is absorbed by the blood within the vein. The resulting heat coagulates the blood and destroys the function of the vein. Over time the vein will be absorbed by the body and will disappear from sight. Laser Ablation of Telangiectasia (spider veins). Telangiectasis is a vascular lesion formed by dilation of a group of small blood vessels. Telangiectasia may appear as birthmarks or become apparent in young children. Acquired telangiectasia may also be caused by long-term sun exposure. Although the lesions may occur anywhere on the skin, they are seen most frequently on the face and thighs. Hereditary hemorrhagic telangiectasia is a disease transmitted by autosomal dominant inheritance marked by thinness of the walls of the blood vessels of the nose, skin, and digestive tract as well as a tendency to hemorrhage. Rendu-Osler Weber syndrome is a form of hereditary hemorrhagic telangiectasia. Mechanochemical endovenous ablation (MOCA) Mechanochemical endovenous ablation utilizes both sclerotherapy and mechanical damage to the lumen. Following ultrasound imaging, a disposable catheter with a motor drive is inserted into the distal end of the target vein and advanced to the saphenofemoral junction. As the catheter is pulled back, a wire rotates within the lumen of the vein, abrading the lumen. At the same time, a liquid sclerosant (sodium tetradecyl sulphate) is infused near the rotating wire. It is proposed that mechanical ablation allows for better efficacy of the sclerosant, without the need for the tumescent anesthesia used in radiofrequency ablation or endovenous laser ablation. The ClariVein® Infusion Catheter is utilized to perform MOCA and received 510(k) approval by the U.S. Food and Drug Administration (FDA) in February 2008. The system includes an infusion catheter, motor drive, stopcock and syringe and is intended for the infusion of physician-specified agents in the peripheral vasculature. Proprietary Information of Excellus Health Plan, Inc. SUBJECT: VARICOSITIES, TREATMENT ALTERNATIVES TO VEIN STRIPPING AND LIGATION POLICY NUMBER: 7.01.47 CATEGORY: Technology Assessment EFFECTIVE DATE: 04/19/01 REVISED DATE: 04/17/02, 12/19/02, 07/17/03, 03/18/04, 05/19/04, 04/21/05, 04/20/06, 04/19/07, 03/20/08, 09/17/09, 10/28/10, 05/19/11, 05/24/12, 06/20/13, 05/22/14, 06/18/15 PAGE: 4 OF: 9 Sclerotherapy (Sclerosing Injection/Compression Therapy) Sclerotherapy is a method of eliminating cutaneous varicose veins in which a sclerosing agent is injected into the veins. The principle of sclerotherapy is to cause irreversible endothelial injury in the desired location, while avoiding any damage to normal vessels that may be interconnected with the abnormal vessel being treated. Sclerotherapy usually requires no anesthesia and is performed in the outpatient setting or in the practitioner’s office setting. It is sometimes performed in situations that might otherwise require surgery. Since the saphenous vein is not visible with the naked eye, injection may be guided by ultrasonography, and the combined procedure may be referred to as echosclerotherapy. Technical improvements in sclerotherapy have included the routine use of Duplex ultrasound to target refluxing vessels, luminal compression of the vein with anesthetics, and a foam/sclerosant injectate in place of liquid sclerosant. Foam sclerosants are produced by forcibly mixing a gas (e.g., air or carbon dioxide) with a liquid sclerosant (e.g., polidocanol or sodium tetradecyl sulfate). In November 2013, the FDA approved Varithena™, a foam sclerosant that utilizes micro bubbles (microfoam) and is composed of polidocanol. Varithena™ is dispensed from a canister with a controlled density and a more consistent bubble size. Varithena™ is used for the treatment of incompetent great saphenous veins, accessory saphenous veins and visible varicosities of the great saphenous vein system above and below the knee. Compressive sclerotherapy involves injection of the sclerosant into an “empty” vein (elevated limb) followed by application of compressive dressings. This is the most commonly performed sclerotherapy procedure for varicose veins of the lower extremities. Non-compressive sclerotherapy implies injection of the sclerosant into veins when the patient is upright and the veins are “full”. Technically this is thrombotic therapy, not sclerotherapy. Other treatments On Feb 20, 2015, the FDA granted pre-market approval of the VenaSeal Closure System to treat superficial varicosities of the legs through endovascular embolization and is intended for adults with clinically symptomatic venous reflux diagnosed by duplex ultrasound. The VenaSeal system is a tumescentless technique that utilizes a cyanoacrylate- based adhesive that is injected into a diseased vein via a catheter inserted through the skin, while being monitored by ultrasound. Once the adhesive is injected the area is manually compressed and the adhesive changes into a solid to seal the varicose vein. Other proposed methods of treating varicose veins include steam injection (Steam Vein Sclerosis System [SVS™, VenoSteam™], CermaVEIN, France) and endovenous microwave ablation (Microwave Intracavitary Coagulation System, Shanghai Medical Electronics, China). Results of a small, preliminary study performed outside of the U.S., for each system, have been reported. Neither of these procedures have been approved or cleared for marketing by U.S. Food and Drug Administration (FDA). A search of the FDA website did not identify any information regarding either system. RATIONALE: Ambulatory phlebectomy, including but not limited to transilluminated powered phlebectomy (TPP/TIPP, TriVex) and stab phlebectomy, are variations of currently accepted surgical techniques for the treatment of varicose veins. In October 2003, the Trivex system, a device for transilluminated powered phlebectomy, was approved by the FDA. A variety of case series describe initial experience with transilluminated powered phlebectomy. In general, these studies demonstrate its technical feasibility and report that the technique is associated with decreased surgical time and decreased number of incisions compared to historical controls. A randomized study of 141 patients (188 limbs) compares removal of superficial varicosities with either stab avulsions or the TriVex system. Authors concluded that the TriVex system was a safe and effective method of excision of varicosities that compared well to standard stab avulsion. Proprietary Information of Excellus Health Plan, Inc. SUBJECT: VARICOSITIES, TREATMENT ALTERNATIVES TO VEIN STRIPPING AND LIGATION POLICY NUMBER: 7.01.47 CATEGORY: Technology Assessment EFFECTIVE DATE: 04/19/01 REVISED DATE: 04/17/02, 12/19/02, 07/17/03, 03/18/04, 05/19/04, 04/21/05, 04/20/06, 04/19/07, 03/20/08, 09/17/09, 10/28/10, 05/19/11, 05/24/12, 06/20/13, 05/22/14, 06/18/15 PAGE: 5 OF: 9 Endoluminal Radiofrequency Ablation. In 1999, the VNUS® ClosureTM System was approved by the FDA for endovascular coagulation of blood vessels in patients with superficial vein reflux. Clinical evidence supports the safety and efficacy of endoluminal radiofrequency ablation (such as VNUS®) of the greater saphenous vein as an alternative to saphenous vein ligation and stripping in patients with documented symptomatic saphenofemoral reflux. Although the studies have a short follow-up period, in one study of 301 limbs 89% of procedures were successful after five months with no evidence of recannulation. In a randomized controlled clinical trial of 28 patients, all cases were considered successful after a 50-day follow-up based on the absence of Duplex detected flow in the treated segments of the greater saphenous veins. In a clinical trial of 26 limbs in 26 patients the long saphenous vein was successfully occluded in 88% of patients. These studies suggest that endoluminal radiofrequency ablation of the greater saphenous vein is effective as a treatment option for symptomatic varicose veins and is associated with a faster postoperative recovery and less pain. Endovascular embolization (VenaSeal™ Closure System). In April 2015, the results of a multicenter, prospective, randomized study – the VeClose study - comparing cyanoacrylate embolization (CAE) with radiofrequency ablation (RFA) for the treatment of symptomatic, incompetent, great saphenous veins (GSV), was published. 222 subjects with symptomatic GSV incompetence were randomly assigned to receive either CAE (n = 108) with the VenaSeal™ Sapheon Closure System or RFA (n = 114) with the ClosureFast system. After discharge, subjects returned to the clinic on day 3 and again at months 1 and 3. The study’s primary endpoint was closure of the target vein at month 3 as assessed by duplex ultrasound and adjudicated by an independent vascular ultrasound core laboratory. Statistical testing focused on showing non-inferiority with a 10% delta conditionally followed by superiority testing. No adjunctive procedures were allowed until after the month 3 visit, and missing month 3 data were imputed by various methods. Secondary end points included patient-reported pain during vein treatment and extent of ecchymosis at day 3. Additional assessments included general and disease-specific quality of life surveys and adverse event rates. By use of the predictive method for imputing missing data, 3-month closure rates were 99% for CAE and 96% for RFA. All primary end point analyses, which used various methods to account for the missing data rate (14%), showed evidence to support the study’s non-inferiority hypothesis (all P < .01); some of the analyses supported a trend toward superiority (P = .07 in the predictive model). Pain experienced during the procedure was mild and similar between treatment groups (2.2 and 2.4 for CAE and RFA, respectively, on a 10-point scale; P = .11). At day 3, less ecchymosis in the treated region was present after CAE compared with RFA (P < .01). Other adverse events occurred at a similar rate between groups and were generally mild and well tolerated. The authors concluded CAE was proven to be non-inferior to RFA for the treatment of incompetent GSVs at month 3 after the procedure; both treatment methods showed good safety profiles; CAE does not require tumescent anesthesia; and is associated with less post-procedure ecchymosis. Study follow-up will continue for 3 years to obtain long term success rates, likelihood of recanalization, and chronic venous disorder (CVD) progression. (Morrison, et al, 2015). Endovenous Laser Ablation. In 2002, the Diomed 810 nm surgical laser and EVLT (endovenous laser therapy) procedure kit received FDA clearance for use in the endovascular coagulation of the greater saphenous vein of the thigh in patients with superficial vein reflux. There is little clinical evidence in the form of randomized prospective clinical trials to support endovenous laser ablation of the greater saphenous vein (ELAS, EVLT) or transcutaneous laser ablation of small diameter veins. Available studies are small with short-term follow-up. However, available studies support the safety and efficacy of ELAS and EVLT in patients with documented symptomatic saphenofemoral reflux. Mechanochemical Endovenous Ablation (MOCA). Very few peer-reviewed studies of have been published that address MOCA. Studies that have been published address the safety and efficacy of the ClariVein® system. One study (Elias and Raines, 2012), reported an industry-sponsored safety and efficacy study of the ClariVein® system. Thirty greater saphenous veins in 29 patients were treated with the device. Greater saphenous veins with diameters greater than 12 mm were excluded. 77% of veins were CEAP class 2 with 7% in class 3 (varicose veins and edema) and 16% in class 4a (varicose veins with skin changes). At 6-month follow-up 1 vein had recanalized, for a primary closure rate of 96.7%. No pain during the procedure or adverse events were reported. There is insufficient evidence to permit conclusions regarding the efficacy and safety of mechanochemical endovenous ablation and further controlled studies with longer follow-up are needed. Proprietary Information of Excellus Health Plan, Inc. SUBJECT: VARICOSITIES, TREATMENT ALTERNATIVES TO VEIN STRIPPING AND LIGATION POLICY NUMBER: 7.01.47 CATEGORY: Technology Assessment EFFECTIVE DATE: 04/19/01 REVISED DATE: 04/17/02, 12/19/02, 07/17/03, 03/18/04, 05/19/04, 04/21/05, 04/20/06, 04/19/07, 03/20/08, 09/17/09, 10/28/10, 05/19/11, 05/24/12, 06/20/13, 05/22/14, 06/18/15 PAGE: 6 OF: 9 The National Institute for Health and Clinical Evidence (United Kingdom) issued guidance on endovenous mechanochemical ablation in 2013, concluding that current evidence on the safety and efficacy of endovenous mechanochemical ablation for varicose veins is inadequate in quantity and quality and the procedure should only be used with special arrangements for clinical governance, consent, and audit or research. Sclerotherapy. Two sclerosants (sodium tetradecyl sulfate and sodium sulfate) have been approved by the U.S. Food and Drug Administration (FDA) for the treatment of varicose veins of the lower extremity. Published clinical trials support the safety and efficacy of conventional sclerotherapy for lower extremity varicose veins. Compressive sclerotherapy has been found to be as effective as surgery in relieving the symptoms associated with varicose veins with few complications. Studies consider sclerotherapy successful based on the absence of Duplex detected flow in the treated segments of the greater saphenous veins, and is associated with a faster postoperative recovery. Clinical evidence indicates that sclerotherapy of varicose tributaries alone is less effective than treatment that includes control of the underlying refluxing veins. However, since recurrence typically arises after 2 to 4 years, isolated sclerotherapy may be medically appropriate for patients in whom long-term control of venous reflux is not a treatment goal. Such patients may include older patients who experience recurrent bleeding form varicose blebs or older patients with recurrent thrombophlebitis in varicose tributaries. Sclerotherapy of the greater saphenous vein raises issues regarding appropriate volume and concentration of the sclerosant and the ability to provide adequate post-procedure compression, since the greater saphenous vein is larger and deeper than telangiectatic dermal veins. Also the use of sclerotherapy, as opposed to the physical removal of the vein with stripping, raises the issue of recurrence due to recanalization. Non-compressive sclerotherapy has not been shown to be effective in producing long-term obliteration of the incompetent veins. CODES: Number Description Eligibility for reimbursement is based upon the benefits set forth in the member’s subscriber contract. CODES MAY NOT BE COVERED UNDER ALL CIRCUMSTANCES. PLEASE READ THE POLICY AND GUIDELINES STATEMENTS CAREFULLY. Codes may not be all inclusive as the AMA and CMS code updates may occur more frequently than policy updates. Code Key: Experimental/Investigational = (E/I), Not medically necessary/ appropriate = (NMN) CPT: 36468 (NMN) Single or multiple injections of sclerosing solutions, spider veins (telangiectasia); limb or trunk 36470 Injection of sclerosing solution; single vein 36471 36475 36476 36478 36479 multiple veins, same leg Endovenous ablation therapy of incompetent vein, extremity, inclusive of all imaging guidance and monitoring, percutaneous, radiofrequency; first vein treated second and subsequent veins treated in a single extremity, each through separate access sites Endovenous ablation therapy of incompetent vein, extremity, inclusive of all imaging guidance and monitoring, percutaneous, laser; first vein treated second and subsequent veins treated in a single extremity, each through separate access sites Proprietary Information of Excellus Health Plan, Inc. SUBJECT: VARICOSITIES, TREATMENT ALTERNATIVES TO VEIN STRIPPING AND LIGATION POLICY NUMBER: 7.01.47 CATEGORY: Technology Assessment 37765 37766 37799 EFFECTIVE DATE: 04/19/01 REVISED DATE: 04/17/02, 12/19/02, 07/17/03, 03/18/04, 05/19/04, 04/21/05, 04/20/06, 04/19/07, 03/20/08, 09/17/09, 10/28/10, 05/19/11, 05/24/12, 06/20/13, 05/22/14, 06/18/15 PAGE: 7 OF: 9 Stab phlebectomy of varicose veins, one extremity; 10-20 stab incisions more than 20 incisions Unlisted procedure, vascular surgery Note: Used for stab phlebectomy of varicose veins; less than 10 incisions Copyright © 2015 American Medical Association, Chicago, IL HCPCS: S2202 Echosclerotherapy ICD-9: 448.1 (NMN) Spider nevus (telangiectasis) 454.0 - 454.2, 454.8 459.81 Varicose veins of the lower extremity (code range) I83.001-I83.229 Varicose veins of lower extremities with ulcer and/or inflammation (code range) I83.811-I83.899 Varicose veins of lower extremities with other complications (code range) I87.2 Venous insufficiency (chronic) (peripheral) I87.9 Disorder of vein, unspecified ICD10: Venous insufficiency, unspecified REFERENCES: Biemans AA, et al. Comparing endovenous laser ablation, foam sclerotherapy, and conventional surgery for great saphenous varicose veins. J Vasc Surg 2013 Sep;58(3):727-34.e1. BlueCross BlueShield Association. Treatment of varicose veins/venous insufficiency. Medical Policy Reference Manual Policy #7.01.124. 2014 Dec 11. Boersma D, et al. Mechanochemical endovenous ablation of small saphenous vein insufficiency using the ClariVein® device: one-year results of a prospective series. Eur J Vasc Endovasc Surg 2013 Mar;45(3):299-303. Brittenden J, et al. A randomized trial comparing treatments for varicose veins. N Engl J Med 2014 Sep 25;371(13):121827. Carradice D, et al. Clinical and technical outcomes from a randomized clinical trial of endovenous laser ablation compared with conventional surgery for great saphenous varicose veins. Br J Surg 2011 Aug;98(8):1117-23. Carroll C, et al. Systematic review, network meta-analysis and exploratory cost-effectiveness model of randomized trials of minimally invasive techniques versus surgery for varicose veins. Br J Surg 2014 Aug;101(9):1040-52. Creton D, et al. Radiofrequency-powered segmental thermal obliteration carried out with the ClosureFast procedure: results at 1 year. Ann Vasc Surg 2010 Apr;24(3):360-6. Cullum NA, et al. Therapeutic ultrasound for venous leg ulcers. Cochrane Database Syst Rev. 2010 Jun 16;6:CD001180. Disselhoff BC, et al. Five-year results of a randomized clinical trial comparing endovenous laser ablation with cryostripping for great saphenous varicose veins. Br J Surg 2011 Aug;98(8):1107-11. Elias S and Raines JK. Mechanochemical tumescentless endovenous ablation: final results of the initial clinical trial. Phlebology 2012;27(2):67-72. Gloviczki P, et al. The care of patients with varicose veins and associated chronic venous diseases: clinical practice guidelines of the Society for Vascular Surgery and the American Venous Forum. J Vasc Surg 2011 May;53(5 Suppl):2S48S. Guex JJ. Endovenous chemical (and physical) treatments for varices: what's new? Phlebology 2014 May 19;29(1 suppl):45-48 [Epub ahead of print]. Proprietary Information of Excellus Health Plan, Inc. SUBJECT: VARICOSITIES, TREATMENT ALTERNATIVES TO VEIN STRIPPING AND LIGATION POLICY NUMBER: 7.01.47 CATEGORY: Technology Assessment EFFECTIVE DATE: 04/19/01 REVISED DATE: 04/17/02, 12/19/02, 07/17/03, 03/18/04, 05/19/04, 04/21/05, 04/20/06, 04/19/07, 03/20/08, 09/17/09, 10/28/10, 05/19/11, 05/24/12, 06/20/13, 05/22/14, 06/18/15 PAGE: 8 OF: 9 *Labropoulos N, et al. Primary superficial vein reflux with competent saphenous trunk. Eur J Vasc Endovasc Surg 1999 Sep;18:201-6. Lattimer CR, et al. Interim results on abolishing reflux alongside a randomized clinical trial on laser ablation with phlebectomies versus foam sclerotherapy. Int Angiol 2013 Aug;32(4):394-403. Lawson J, et al. Sapheon: the solution? Phlebology 2013 Mar;28 Suppl 1:2-9. Milleret R, et al. Great saphenous vein ablation with steam injection: results of a multicentre study. Eur J Vasc Endovasc Surg 2013 Apr;45(4):391-6. Morrison N, et al. Randomized trial comparing cyanoacrylate embolization and radiofrequency ablation for incompetent great saphenous veins (VeClose). J Vasc Surg 2015 Apr;61(4):985-94. Mueller RL and Raines JK. ClariVein mechanochemical ablation: background and procedural details. Vasc Endovascular Surg 2013 Apr;47(3):195-206. Murad MH, et al. A systematic review and meta-analysis of the treatments of varicose veins. J Vasc Surg 2011 May;53(5 Suppl):49S-65S. National Institute for Health and Clinical Excellence. IPG435 Endovenous mechanochemical ablation for varicose veins: guidance. 2013 Jan [http://www.nice.org.uk/guidance/ipg435] accessed 4/14/15. Nesbitt C, et al. Endovenous ablation (radiofrequency and laser) and foam sclerotherapy versus conventional surgery for great saphenous vein varices. Cochrane Database Syst Rev 2014 Jul;(7):CD005624. Nordon IM, et al. A prospective double-blind randomized controlled trial of radiofrequency versus laser treatment of the great saphenous vein in patients with varicose veins. Ann Surg 2011 Dec;254(6):876-81. O'Donnell TF Jr, et al; Society for Vascular Surgery; American Venous Forum. Management of venous leg ulcers: clinical practice guidelines of the Society for Vascular Surgery ® and the American Venous Forum. J Vasc Surg 2014 Aug;60(2 Suppl):3S-59S. Pan Y, et al. Comparison of endovenous laser ablation and high ligation and stripping for varicose vein treatment: a metaanalysis. Phlebology 2014 Mar;29(2):109-19. Rasmussen LH, et al. Randomised clinical trial comparing endovenous laser ablation with stripping of the great saphenous vein: clinical outcome and recurrence after 2 years. Eur J Vasc Endovasc Surg 2010 May;39(5):630-5. Rasmussen L, et al. Randomized clinical trial comparing endovenous laser ablation and stripping of the great saphenous vein with clinical and duplex outcome after 5 years. J Vasc Surg 2013 Aug;58(2):421-6. Rasmussen LH, et al. Randomized clinical trial comparing endovenous laser ablation, radiofrequency ablation, foam sclerotherapy and surgical stripping for great saphenous varicose veins. Br J Surg 2011 Aug;98(8):1079-87. Rass K, et al. Comparable effectiveness of endovenous laser ablation and high ligation with stripping of the great saphenous vein: two-year results of a randomized clinical trial (RELACS study). Arch Dermatol 2012 Jan;148(1):49-58. Rathbun S, et al. Performance of endovenous foam sclerotherapy in the USA for the treatment of venous disorders: ACP/SVM/AVF/SIR quality improvement guidelines. Phlebology 2014 Mar;29(2):76-82. Samuel N, et al. Randomized clinical trial of endovenous laser ablation versus conventional surgery for small saphenous varicose veins. Ann Surg 2013 Mar;257(3):419-26. Sarvananthan T, et al. Neurological complications of sclerotherapy for varicose veins. J Vasc Surg 2012 Jan;55(1):24351. Sell H, et al. Compression therapy versus surgery in the treatment of patients with varicose veins: A RCT. Eur J Vasc Endovasc Surg 2014 Jun;47(6):670-7. Proprietary Information of Excellus Health Plan, Inc. SUBJECT: VARICOSITIES, TREATMENT ALTERNATIVES TO VEIN STRIPPING AND LIGATION POLICY NUMBER: 7.01.47 CATEGORY: Technology Assessment EFFECTIVE DATE: 04/19/01 REVISED DATE: 04/17/02, 12/19/02, 07/17/03, 03/18/04, 05/19/04, 04/21/05, 04/20/06, 04/19/07, 03/20/08, 09/17/09, 10/28/10, 05/19/11, 05/24/12, 06/20/13, 05/22/14, 06/18/15 PAGE: 9 OF: 9 Shepherd AC, et al. Randomized clinical trial of VNUS ClosureFAST radiofrequency ablation versus laser for varicose veins. Br J Surg 2010 Jun;97(6):810-8. Siribumrungwong B, et al. A systematic review and meta-analysis of randomised controlled trials comparing endovenous ablation and surgical intervention in patients with varicose vein. Eur J Vasc Endovasc Surg 2012 Aug;44(2):214-23. Stücker M, et al. Review of published information on foam sclerotherapy. Dermatol Surg 2010 Jun;36(Suppl 2):983-92. Tellings SS, et al. Surgery and endovenous techniques for the treatment of small saphenous varicose veins: a review of the literature. Phlebology 2011 Aug;26(5):179-84. *Tisi PV, et al. Injection sclerotherapy for varicose veins. Cochrane Database Syst Rev 2006(4):CD001732. Todd KL 3rd, et al; VANISH-2 Investigator Group. The VANISH-2 study: a randomized, blinded, multicenter study to evaluate the efficacy and safety of polidocanol endovenous microfoam 0.5% and 1.0% compared with placebo for the treatment of saphenofemoral junction incompetence. Phlebology 2014 Oct;29(9):608-18. U.S. Food and Drug Administration. Drug approval package. Varithena, (polidocanol) injectable foam. 2014 Jul 23 [http://www.accessdata.fda.gov/drugsatfda_docs/nda/2013/205098Orig1s000TOC.cfm] accessed 5/1/15. van den Bos RR, et al. Randomized clinical trial of endovenous laser ablation versus steam ablation (LAST trial) for great saphenous varicose veins. Br J Surg 2014 Aug;101(9):1077-83. Erratum in: Br J Surg 2014 Oct;101(11):1484. van Eekeren RR, et al. Postoperative pain and early quality of life after radiofrequency ablation and mechanochemical endovenous ablation of incompetent great saphenous veins. J Vasc Surg 2013 Feb;57(2):445-50. van Eekeren RR, et al. Endovenous mechanochemical ablation of great saphenous vein incompetence using the ClariVein device: a safety study. J Endovasc Ther 2011 Jun;18(3):328-34. Weiss MA, et al. Consensus for sclerotherapy. Dermatol Surg 2014 Dec;40(12):1309-18. Yang L, et al. Randomized clinical trial of endovenous microwave ablation combined with high ligation versus conventional surgery for varicose veins. Eur J Vasc Endovasc Surg 2013 Oct;46(4):473-9. KEY WORDS: Ambulatory phlebectomy, ClariVein®, Endoluminal radiofrequency ablation, Endovascular embolization, Endovenous laser ablation, Endovenous microwave ablation, Mechanochemical endovenous ablation (MOCA), Microfoam sclerotherapy, Pulse light source, Sclerotherapy, Stab phlebectomy, Steam Vein Sclerosis System, SVS™, Varithena™, VenaSeal™, VenoSteam™, Transilluminated powered phlebectomy, VNUS. CMS COVERAGE FOR MEDICARE PRODUCT MEMBERS There is currently a Local Coverage Determination (LCD) and a supplemental article addressing Treatment of Varicose Veins of the Lower Extremity. Please refer to the following LCD websites for Medicare Members: LCD: http://www.cms.gov/medicare-coverage-database/details/lcddetails.aspx?LCDId=25519&ContrId=298&ver=62&ContrVer=1&CoverageSelection=Both&ArticleType=All&PolicyT ype=Final&s=New+York++Entire+State&KeyWord=varicose&KeyWordLookUp=Title&KeyWordSearchType=And&bc=gAAAABAAAAAAAA %3d%3d& Article: http://www.cms.gov/medicare-coverage-database/details/articledetails.aspx?articleId=44614&ver=65&ContrId=298&ContrVer=1&LCDId=25519&CoverageSelection=Both&ArticleT ype=All&PolicyType=Final&s=New+York++Entire+State&KeyWord=varicose&KeyWordLookUp=Title&KeyWordSearchType=And&bc=gAAAABAAAAAAAA %3d%3d& Proprietary Information of Excellus Health Plan, Inc.