Echocardiographic Epicardial Fat: A Review of Research and

STATE OF THE ART REVIEW ARTICLE
Echocardiographic Epicardial Fat: A Review of
Research and Clinical Applications
Gianluca Iacobellis, MD, PhD and Howard J. Willens, MD, Hamilton, Ontario, Canada; Miami, Florida
Epicardial fat plays a role in cardiovascular diseases. Because of its anatomic and functional proximity to the myocardium and its intense metabolic activity, some interactions between the heart and its visceral fat depot have been suggested. Epicardial fat can be visualized and measured using standard two-dimensional echocardiography. Standard parasternal long-axis and short-axis views permit the most accurate measurement of epicardial fat thickness overlying the right ventricle. Epicardial fat thickness is generally identified as the echofree space between the outer wall of the myocardium and the visceral layer of pericardium and is measured perpendicularly on the free wall of the right ventricle at end-systole. Echocardiographic epicardial fat thickness ranges from a minimum of 1 mm to a maximum of almost 23 mm. Echocardiographic epicardial fat thickness clearly reflects visceral adiposity rather than general obesity. It correlates with metabolic syndrome, insulin resistance, coronary artery disease, and subclinical atherosclerosis, and therefore it might serve as a simple tool for cardiometabolic risk prediction. Substantial changes in echocardiographic epicardial fat thickness during weight-loss strategies may also suggest its use as a marker of therapeutic effect. Echocardiographic epicardial fat measurement in both clinical and research scenarios has several advantages, including its low cost, easy accessibility, rapid applicability, and good reproducibility. However, more evidence is necessary to evaluate whether echocardiographic epicardial fat thickness may become a routine way of assessing cardiovascular risk in a clinical setting. (J Am Soc Echocardiogr 2009;22:1311-9.)
Keywords: Epicardial adipose tissue, Epicardial fat, Echocardiography, Obesity, Metabolic syndrome
Accreditation Statement
The American Society of Echocardiography is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.
The American Society of Echocardiography designates this educational activity for a maximum of 1 AMA PRA Category 1 Credit Ô . Physicians should only claim credit commensurate with the extent of their participation in the activity.
ARDMS and CCI recognize ASE’s certificates and have agreed to honor the credit hours toward their registry requirements for sonographers.
The American Society of Echocardiography is committed to ensuring that its educational mission and all sponsored educational programs are not influenced by the special interests of any corporation or individual, and its mandate is to retain only those authors whose financial interests can be effectively resolved to maintain the goals and educational integrity of the activity. Although a monetary or professional affiliation with a corporation does not necessarily influence an author’s presentation, the Essential Areas and policies of the ACCME require that any relationships that could possibly conflict with the educational value of the activity be resolved prior to publication and disclosed to the audience. Disclosures of faculty and commercial support relationships, if any, have been indicated.
Target Audience
This activity is designed for all cardiovascular physicians and cardiac sonographers with a primary interest and knowledge base in the field of echocardiography; in addition, residents, researchers, clinicians, intensivists, and other medical professionals with a specific interest in cardiac ultrasound will find this activity beneficial.
Objectives
Upon completing the reading of this article, participants will better be able to:
1. Name the postulated roles that epicardial fat might play in cardiac disease.
2. Describe the location of epicardial fat deposits in relation to the coronary arteries and myocardium.
3. Define the 2-dimensional technique for the measurement of epicardial fat and appreciate characteristics that distinguish it from pericardial fat.
4. Recognize the limitations of echocardiography in the quantification of epicardial fat.
5. Identify the potential utility of echocardiographically-measured epicardial fat in the diagnosis, prognosis, and therapy of various cardiac diseases.
Author Disclosure
Dr. Iacobellis reported no actual or potential conflicts of interest in relation to this program. Dr. Willens reported that he receives research support from Actelion Pharmaceuticals (Allschwil, Switzerland), Abbott Laboratories (Abbott Park, IL), and GE Healthcare
(Milwaukee, WI).
Estimated Time to Complete This Activity: 1 hour
EPICARDIAL FAT
What Is Epicardial Fat and Where Is It Located?
Epicardial fat is the true visceral fat depot of the heart.
Epicardial and intra-abdominal fat evolve from brown adipose tissue during embryogenesis. In the adult human heart, epicardial fat is commonly found in the atrioventricular and interventricular grooves.
Minor foci of fat are also located subepicardially along the free walls of the atria and around the two appendages. As the amount of epicardial fat increases, it progressively fills the space between the ventricles, sometimes covering the entire epicardial surface.
A small amount of adipose tissue also extends from the epicardial surface into the myocardium, often following the adventitia of the coronary artery branches. No muscle fascia divides epicardial fat and myocardium; therefore, the two tissues share the same
Why Is Epicardial Fat Important?
A dichotomous role, both unfavorable and protective, has been attrib-
but its physiology in animals and humans is not
From the Department of Medicine, Division of Endocrinology, McMaster
University, Hamilton, Ontario, Canada (G.I.); and the Department of Medicine,
Division of Cardiology, University of Miami Miller School of Medicine, Miami,
Florida (H.J.W.).
Reprint requests: Gianluca Iacobellis, MD, PhD, St Joseph’s Hospital, Department of Medicine, 50 Charlton Avenue East, 5th Fontbonne Building, Hamilton, ON L8N
4A6, Canada (E-mail: gianluca@ccc.mcmaster.ca
).
0894-7317/$36.00
Copyright 2009 by the American Society of Echocardiography.
doi:10.1016/j.echo.2009.10.013
1311
1312 Iacobellis and H. J. Willens Journal of the American Society of Echocardiography
December 2009 completely clear. Epicardial adipose tissue has a smaller adipocyte size but higher rates of fatty acid uptake and secretion than other visceral
Under normal physiologic conditions, epicardial fat could therefore serve several distinct functions: as a buffer, absorbing fatty acids and protecting the heart against high fatty acids levels; as a local energy source at times of high demand, channeling fatty acids to the
; and perhaps as brown fat to defend the myocardium
against hypothermia.
Whereas epicardial fat may release factors that blunt the toxic effects of high fatty acid levels on the myocardium, it may also release factors that promote harmful coronary artery and
A body of evidence shows that epicardial fat is an extremely active organ that produces several bioactive adipokines.
It is a source of several proinflammatory and proatherogenic cytokines, as well as tumor necrosis factor– a , monocyte chemoattractant protein–1, interlukin-6, nerve growth factor, resistin, visfatin, omentin, leptin, plasminogen activator inhibitor–1, and angiotensino-
However, epicardial fat also produces anti-inflammatory, antiatherogenic adipokines, such as adiponectin and adrenomedullin.
Nevertheless, what could influence this equilibrium between harmful and possible protective effects is still unknown. Because of its anatomic proximity to the heart and the absence of fascial boundaries, epicardial adipose tissue may interact locally and modulate the coronary arteries through the paracrine or vasocrine secretion of proinflammatory adipokines.
It is reasonable to postulate that inflammatory signals from the epicardial fat could act reciprocally because of atherogenic inflammation in the underlying plaques. The regional ischemia could make the epicardial adipose tissue active toward oxidant-sensitive inflammatory signals in adjacent adipose stores.
The presence of inflammatory cells in epicardial adipose tissue could also reflect the response to plaque rupture and lead to the amplification of vascular inflammation and plaque instability.
It is also plausible that the paracrine release of cytokines from periadventitial epicardial fat could traverse the coronary wall by diffusion from outside to inside and interact with cells in each of its layers. Inflammatory adipokines might be released from epicardial tissue directly into vasa vasorum and be transported downstream into the arterial wall,
according to a ‘‘vasocrine signaling’’ mechanism.
The local secretion of proinflammatory cytokines from the epicardial fat could be predominant and therefore down-regulate the production of protective and anti-inflammatory cytokines, as well as adiponectin and adreno-
medullin in severe and unstable coronary artery disease (CAD).
Epicardial fat secretes adiponectin and adrenomedullin into the coro-
Adiponectin improves insulin sensitivity and has anti-inflammatory and antiatherogenic actions, whereas adrenomedullin is a potent vasodilator, anti-inflammatory, and angiogenic factor. Epicardial fat might exert a protective effect through adiponectin and adrenomedullin secretion in response to local or systemic metabolic or mechanical insults. Although epicardial fat is a source of bioactive molecules, it is not clear whether this activity is directly and simply related to the amount of fat accumulation, particularly when it is expressed as thickness. A mass-dependent mechanism could also be evoked to explain higher proinflammatory markers in combination with higher epicardial fat thickness.
How Is Epicardial Fat Distinguished From Pericardial Fat?
The heart is covered by more or less abundant adipose tissue, partic-
ularly on its right side, as astutely noted at the end of 19th century.
Two different fat depots were described, one located extrinsic to the
pericardium and another directly on the myocardium.
More recently, however, whether and how these two fat depots are really different has been questioned.
Autopsy and imaging studies seem be of help in defining and understanding the difference between epicardial and pericardial fat. Epicardial adipose tissue is the fat located between the myocardium and visceral pericardium, as detected by autopsy and imaging studies.
Pericardial adipose tissue is the fat depot outside the visceral pericardium and on the external surface of the parietal pericardium, as defined by autopsy and imaging studies.
Pericardial fat volume is also defined as any adipose tissue located within the pericardial sac, described as the border
between pericardial and intrathoracic fat.
Epicardial and pericardial fat have different embryologic origins.
Epicardial, mesenteric, and omental fat all share the same origin
from the splanchnopleuric mesoderm.
Pericardial fat originates from the primitive thoracic mesenchyme, which splits to form the pa-
rietal pericardium and the outer thoracic wall.
Local circulation is also different between the two fat depots. Epicardial fat is supplied by branches of the coronary arteries, whereas the pericardial fat is supplied by noncoronary sources, such as the pericardiacophrenic branch
of the internal mammary artery.
In addition, although the epicardial fat and the myocardium share the same microcirculation, this is not true for the pericardial fat. As result of this peculiarity and different anatomic location, the epicardial fat should be considered the true visceral fat depot of the heart. To simplify, the adipose tissue of the heart is divided into two layers: (1) epicardial fat, the visceral layer, and (2) pericardial fat, situated externally to the parietal layer of the pericardium. Under physiologic conditions, pericardial adipose tissue covers 80% of the heart and constitutes between 20% and 50% of its mass, whereas the epicardial adipose tissue weighs on average 50 g and represents approximately 20% of the heart’s mass.
It is seems that it is not just a matter of terminology, but that epicardial fat should be really distinguished from the pericardial fat, because they are two different cardiac visceral fat depots. However, recent reports from the Framingham Heart Study do not seem to make a differentiation between epicardial and pericardial fat, especially when the authors discuss the biomolecular properties of these two
The Multi-Ethnic Study of Atherosclerosis (MESA) more generally defined the pericardial fat as the fat around the
In these large and well-conducted population studies, pericardial fat volume has been measured using cardiac computed tomography (CT) or multidetector CT (MDCT) and then defined as any adipose tissue located within the pericardial sac.
A brief summary of the heart’s anatomy may be of help. The pericardial sac consists essentially of two sacs intimately connected with each other but totally different in structure. The outer sac, known as the fibrous pericardium, consists of fibrous tissue. The inner sac, the serous pericardium, is a closed sac that lines the fibrous pericardium and is invaginated by the heart; it therefore consists of a visceral and a parietal portion. The visceral portion, or epicardium, covers the heart and the great vessels and from the latter is continuous with the parietal layer, which lines the fibrous pericardium. It could be therefore assumed that the term pericardial fat is intended to include both epicardial and pericardial adipose tissues,
which are actually different fat depots. Conversely, if these large epidemiologic studies really intended to distinguish between the two fat depots, pericardial fat
should be considered differently, as paracardial fat.
Reports from
the Framingham Heart Study and others
all agree that the volume of pericardial fat, as determined on cardiac CT, is significantly associated with the risk for coronary heart disease, coronary artery calcification, metabolic syndrome, diabetes mellitus, and left ventricular (LV) morphology, independently of traditional anthropometric indicators such as body mass index and waist circumference. Hence, if it is
Journal of the American Society of Echocardiography
Volume 22 Number 12
Iacobellis and H. J. Willens 1313 unquestionable that pericardial fat volume, as measured using
MDCT, could be an important cardiovascular risk factor, it might be still questionable if these recent studies really made a differentiation between the pericardial fat, the outer fat accumulation, and the epicardial fat, the fat depot immediately adjacent to the heart wall.
In addition, it is worth emphasizing that although the physiologic, biochemical, and biomolecular properties of epicardial adipose tissue and its possible paracrine interactions with the heart have been described,
the function and pathophysiologic role of paracardial fat are still unknown. Conceptually, because its biochemical properties and anatomic proximity to the myocardium and coronary arteries, epicardial fat thickness might provide a more direct measure of the cardiac visceral adiposity. However, further studies will be necessary to clarify this issue.
MEASUREMENT OF EPICARDIAL FAT USING
ECHOCARDIOGRAPHY
Visceral fat deposition has been recognized as an important risk factor for cardiovascular disease.
The quantification of visceral fat is a helpful practical diagnostic tool for clinicians who are committed to managing patients at high risk for cardiovascular disease. In a clinical setting, visceral fat is typically measured by surrogate markers, such as waist circumference alone or the ratio of waist circumference to hip circumference. More direct measurements of visceral fat, including magnetic resonance imaging (MRI) and/or CT, are certainly precise, but they are expensive and cumbersome, especially if they are intended to be used in clinical practice. There is therefore a compelling need and growing interest in less expensive and more reliable imaging markers of visceral adiposity.
Although much attention has been focused on the measurement of intra-abdominal fat, interest in nontraditional visceral fat depots, such as epicardial fat, is relatively recent.
Methodology and Technical Tips
Epicardial fat thickness can be visualized and measured with two-dimensional (2D) echocardiography using commercially available equipment, as first proposed and validated by Iacobellis
Standard parasternal long-axis and short-axis views from
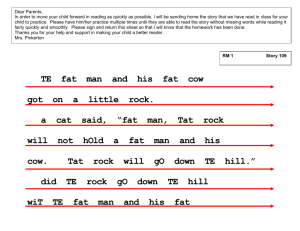
2D images permit the most accurate measurement of epicardial fat thickness on the right ventricle, with optimal cursor beam orientation in each view. Echocardiographically, epicardial fat is generally identified as the relatively echo-free space between the outer wall of the myocardium and the visceral layer of pericardium; its thickness is measured perpendicularly on the free wall of the right ventricle at
end-systole in 3 cardiac cycles ( Figure 1 ). Because it is compressed
during diastole, epicardial fat thickness is best measured at end-systole at the point on the free wall of the right ventricle at which the ultrasound beam is oriented in a perpendicular manner, using the aortic annulus as an anatomic landmark.
Epicardial fat thickness can be also appear as hyperechoic space, if in large amount (>15 mm). Maximum epicardial fat thickness is measured from 2D parasternal longaxis images at the point on the free wall of the right ventricle along the midline of the ultrasound beam, perpendicular to the aortic annulus, used as an anatomic landmark for this view. For midventricular parasternal short-axis assessment, maximum epicardial fat thickness is measured from 2D images on the right ventricular free wall along the midline of the ultrasound beam perpendicular to the interventricular septum at midchordal and tip of the papillary muscle level, as anatomic landmarks. The average value of 3 cardiac cycles from each
Figure 1 Echocardiographic epicardial fat thickness. Epicardial fat thickness (within red dashed shape) is identified as the echofree space between the outer wall of the myocardium and the visceral layer of pericardium in the parasternal long-axis view.
Epicardial fat thickness is measured during end-systole at the point on the free wall of the right ventricle along the midline of the ultrasound beam, with the best effort to be perpendicular to the aortic annulus, used as an anatomic landmark.
echocardiographic view is determined. The majority of populationbased clinical studies have reported excellent interobserver and intraobserver agreement for epicardial fat thickness measurement.
Intraclass correlation coefficients have ranged from 0.90 to 0.98 and from 0.93 to 0.98, respectively, indicating good reproducibility and reliability. Concordance of long-axis and short-axis average epicardial fat thickness measurement was also excellent at 0.98 (95% confi-
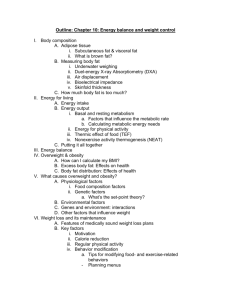
Echocardiographically, epicardial fat can be distinguished from pericardial fat. Pericardial fat thickness can be identified as the hypoechoic space anterior to the epicardial fat and parietal pericardium
). Pericardial fat usually does not deform substantially with cardiac cycles and does not appear hyperechoic. However, fat thickness deformation is not a good way of distinguishing between the two depots.
A normal upper-limit value for epicardial fat thickness has not been established yet. Echocardiographic epicardial fat thickness varies from a minimum of 1 mm to a maximum measured value of almost 23
The wide range of epicardial fat thicknesses likely reflects the substantial variation in abdominal visceral fat distribution. Iacobelfound median epicardial fat thicknesses of 7 mm in men and
6.5 mm in women in a large population of patients who underwent transthoracic echocardiography for standard clinical indications.
Jeong et al
reported a mean epicardial fat thickness of 6.3 mm in
>200 subjects who underwent coronary angiography. Natale et al
set the normal upper limit to 7 mm, on the basis of the mean value and distribution of epicardial fat thickness in 50 normal volunteers.
Advantages of Echocardiographic Epicardial Fat Thickness
Echocardiographic epicardial fat measurement may have some advantages as an index of high cardiometabolic risk: (1) It is a direct measure of visceral fat rather than an anthropometric measure, such as waist circumference, that includes muscle and skin layers. The echocardiographic measurement of epicardial fat provides a more sensitive and specific measure of true visceral fat content, avoiding the possible confounding effect of increased subcutaneous
1314 Iacobellis and H. J. Willens Journal of the American Society of Echocardiography
December 2009
Figure 2 fat (within yellow arrows and yellow dashed shape) tified as the hypoechoic space anterior to the epicardial fat
(within red arrows and red dashed shape) does not deform substantially with cardiac cycles and does not appear as hyperechoic space. Modified parasternal long-axis view.
Epicardial versus pericardial fat thickness. Pericardial can be iden-
. Pericardial fat usually abdominal fat. (2) It is an objective, noninvasive, readily available, and certainly less expensive measure of visceral fat than MRI or
CT. (3) Visceral cardiac fat can be quantified fairly precisely compared with ectopic fat deposition in organs such as the liver, which can be described only qualitatively unless expensive measurements are made, such as CT or MRI. (4) Echocardiographic epicardial fat is a direct measure of ectopic fat deposition, whereas anthropometric measures can be associated only with ectopic fat deposition. (5) It can be measured even from echocardiograms that were not specifically performed to optimize the measurement of epicardial fat. (6)
It can be quantified with other echocardiographic parameters, such
LV mass and ejection fraction, traditionally associated with cardiovascular risk. (7) Echocardiographic epicardial fat could be a more reliable quantitative therapeutic marker during interventions modulating and reducing visceral adiposity.
Limitations of Using Echocardiography to Measure Epicardial
Fat
Echocardiography may be not the optimal technique for the quantification of epicardial fat. Although the majority of studies have shown excellent coefficients of interobserver and intraobserver variability, a single study raised some concerns on the dispersion and
variability in the measurement of epicardial fat thickness.
A moderate concordance in echocardiographic epicardial fat measurement and a relatively poor agreement with measurement on MDCT were reported in this study. Given the small number of patients with interpretable results on MDCT (n = 55) and the use of end-diastolic epicardial fat thickness in the study, the actual variability of this measurement is still in question. However, if the echocardiographic quantification of epicardial fat is performed for cardiometabolic risk stratification, the reproducibility of this measurement is undoubtedly a critical issue.
Echocardiographic epicardial fat thickness is a linear measurement at a single location and therefore may not reflect the variability of fat thickness or total epicardial fat volume. Although the anterior layer of epicardial fat is the one commonly measured by echocardiography, this region may have the most variability in fat content as measured using MRI and MDCT. Epicardial fat thickness is usually smaller in the vicinity of the mid right ventricular free wall and greater in the distal portion of the right ventricular free wall.
Echocardiographic measurements of epicardial fat thickness in the atrioventricular groove or interventricular groove areas may give a more accurate assessment of epicardial fat amount. MDCT is more sensitive and specific than echocardiography for measuring fat thickness in deeper epicardial fat layers as well as the thickest
part of the epicardial fat in the atrioventricular grooves.
Epicardial fat has a conspicuous distribution around the heart, and 2D echocardiographic assessment may not be a completely accurate estimate of the total amount of fat. Three-dimensional echocardiography could provide a noninvasive and more accurate volumetric assessment of epicardial fat thickness. Epicardial fat volume, rather than its thickness, may in fact be the most consistent measure of risk, as recently suggested.
Future studies in this direction should be encouraged.
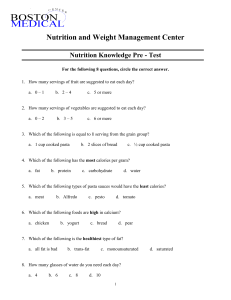
The variability of echocardiographic measurement techniques has also resulted in inconsistencies among studies. Epicardial fat thickness when measured just to the right of the aortic annular plane may increase in size abruptly compared with thickness measured either at or just to the left of the aortic annular plane (
crease in end-systolic epicardial fat thickness is due to the steep downward turn of the free wall of the right ventricle as it approaches the proximal ascending aorta. In such cases, we recommend measuring the largest epicardial fat thickness to the left of the annular plane.
When during the cardiac cycle echocardiographic epicardial fat should be measured has also been a subject of debate. Some echocardiographic studies have measured epicardial fat thickness at end-diastole rather than end-systole. Although there is no clear consensus yet, we strongly suggest that maximum epicardial fat thickness is better measured at end-systole, as highlighted before. When scrolling through the cardiac cycle, in some cases, the largest epicardial fat thickness may fail to correspond to true end-systole or end-diastole. In these cases, we recommend measuring epicardial fat thickness at end-systole.
Potential limitations of echocardiography also include difficulties in differentiating between epicardial fat thickness and pericardial fat, as well as changes in the velocity of sound in adipose tissue. Although there are no current data on how and whether the latter might affect the accuracy of epicardial fat thickness measurement using echocardiography, it would be of interest to evaluate whether it is necessary to correct for this confounding factor when determining the amount of epicardial fat.
POTENTIAL USES OF ECHOCARDIOGRAPHIC EPICARDIAL
FAT THICKNESS FOR DIAGNOSIS
The potential role of echocardiographic epicardial fat thickness as a marker and predictor of cardiometabolic risk has been evaluated.
Journal of the American Society of Echocardiography
Volume 22 Number 12
Iacobellis and H. J. Willens 1315
Figure 3 Large echocardiographic epicardial fat thickness.
Large epicardial fat thickness (within red arrows and red dashed shape) when measured just to the right of the aortic annular plane may abruptly increase in size. This abrupt increase in end-systolic epicardial fat thickness is due to the steep downward turn of the free wall of the right ventricle as it approaches the proximal ascending aorta. In these cases, it is recommended to measure the largest epicardial fat thickness to the left of the annular plane.
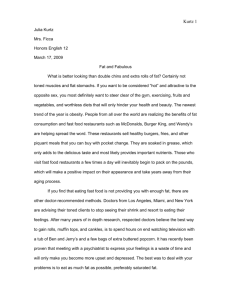
Different cutoff points of epicardial fat thickness for the prediction of metabolic syndrome, excess visceral fat accumulation, insulin resistance, subclinical atherosclerosis, and CAD have been proposed and are summarized in
Marker of Visceral Adiposity
It has been established that echocardiographic epicardial fat is a measure of visceral fat, as measured by gold-standard techniques. In fact, echocardiographic epicardial fat strongly reflects the intra-abdominal accumulation of visceral fat as measured on MRI and does so better than waist circumference.
Echocardiographic epicardial fat thickness is therefore an independent predictor of visceral adiposity and weakly reflects the degree of obesity as measured by body mass
Subjects with higher waist circumferences clearly show
higher epicardial fat thickness, as previously reported.
Whether echocardiographic epicardial fat can be associated with intramyocardial and intrahepatic fat accumulation, as measured using magnetic
is still unknown but is the object of current investigations.
Correlation With Cardiometabolic Risk Factors
Several clinical studies have shown the relationship of echocardiographic epicardial fat thickness and traditional and novel cardiovascular risk factors. Metabolic syndrome is a cluster of diseases with common pathogenic mechanisms, as well as increased visceral fat accumulation and insulin resistance. Epicardial fat thickness in subjects with metabolic syndrome is significantly higher than that observed in subjects without metabolic syndrome.
Receiveroperating characteristic curve analysis showed that epicardial fat thickness values of 9.5 and 7.5 mm maximize the sensitivity and specificity to predict the metabolic syndrome in men and women, respectively.
Epicardial fat thickness is inversely associated with insulin sensitivity, as assessed by euglycemic hyperinsulinemic clamp studies in obese subjects,
and directly related to surrogate markers of insulin resistance as well as fasting insulin and the homeostatic model
assessment of insulin resistance index in a general population.
An epicardial fat thickness of 9.5 mm is associated with clinical parameters of insulin resistance.
The highest values of epicardial fat were found in those categories with extremely high intra-abdominal fat
Although these cutoff values have shown good sensitivity and specificity for the prediction of metabolic syndrome, they have been obtained only in whites and thus may not be applicable in different ethnic groups.
When other cardiometabolic parameters are considered separately, epicardial fat is also independently associated with blood pressure,
low-density lipoprotein cholesterol,
fasting glucose,
and inflammatory markers.
In particular, echocardiographic epicardial fat thickness is higher in subjects with impaired fasting glucose, a prediabetes condition, than in normoglycemic individuals, suggesting its potential role as an additional tool for diabetes-related cardiac risk stratification.
Epicardial fat is an endocrine and paracrine source
and its echocardiographic thickness is correlated with several circulating adipokines levels. Epicardial fat thickness is associated with proatherogenic and proinflammatory adipokines, such as visfatin, plasminogen activator inhibitor–1, monocyte chemoattrac-
tant protein–1, and C-reactive protein.
These correlations remain significant even after adjusting for visceral adipose tissue, as detected
by CT, and waist-to-hip ratio.
However, epicardial fat thickness is inversely related to plasma adiponectin levels, an adipokine with specific anti-inflammatory and antiatherogenic properties.
Lower plasma adiponectin levels are associated with higher cardiovascular risk.
Additionally, a higher thickness of epicardial fat is also significantly associated with higher liver enzymes, surrogate markers of fatty liver.
This association seems to be independent of overall adiposity and rather a function of excess visceral adiposity.
Potential Relevance in CAD
Although its role is still unclear, echocardiographic epicardial fat has been associated with CAD. Epicardial fat thickness > 7 mm has been associated with subclinical atherosclerosis
and CAD, but only in women.
However, different and lower epicardial fat thickness cutoff values (>4.5 mm) have shown a good sensitivity and specificity to detect low coronary flow reserve in women.
The absence of men may prevent the generalization of these interesting results. Epicardial fat thickness values > 3.0 mm were independently associated with the presence of CAD in a Korean population of men and women.
Ethnic differences and therefore different regional fat distribution could explain, at least partially, this variability.
Epicardial fat thickness seems to be higher in patients with CAD and in those with unstable angina than in subjects without CAD and in
those with stable angina or atypical chest pain.
Interestingly, epicardial fat thickness was significantly correlated with the extent and severity of CAD, as assessed by the Gensini score.
Echocardiographic epicardial fat thickness has been shown to predict coronary flow reserve in women with angiographically normal coronary arteries.
Potential Relevance in Atherosclerotic Vascular Disease
The relationship of epicardial fat and atherosclerosis is also of great
Carotid intima-media thickness (C-IMT), as measured by ultrasound, is a well-recognized clinical predictor of subclinical atherosclerosis. Echocardiographic epicardial fat thickness was the best independent predictor of C-IMT in subjects infected with the human immunodeficiency virus with associated metabolic syndrome.
1316 Iacobellis and H. J. Willens Journal of the American Society of Echocardiography
December 2009
Table 1 Proposed echocardiographic epicardial fat thickness cutoff values
Outcome Men (mm) Women (mm) Ethnicity
Metabolic syndrome *
High abdominal fat
†
Extremely high abdominal fat
‡
Insulin resistance
§
High insulin resistance jj
CAD
{
CAD
{
CAD
{
Low coronary flow reserve
Subclinical atherosclerosis
#
**
$
$
$
$
$
$
$
9.5
9.5
13
9.5
11
7
$ 5.2
$ 3
—
7
$ 7.5
$ 7.5
$ 10
$ 9.5
$ 11
$ 7
$ 5.2
$ 3
$ 4.5
$ 7
*As defined by National Cholesterol Education Program Adult Treatment Panel III criteria.
†Waist circumference >88 cm in women and >102 cm in men.
‡Waist circumference >100 cm in women and >120 cm in men.
§Homeostasis model assessment of insulin resistance score of 2.7 to 7.
jj
Homeostasis model assessment of insulin resistance score $ 7.
{ Presence of $ 1 coronary arteries stenosis $ 50% on coronary angiography.
#
Echocardiographically defined as coronary flow reserve < 2.
**Defined by ultrasonographic C-IMT measurement.
European
European
European
European
European
Korean
European
Korean
European
European n
246
246
246
246
246
203
150
527
68
459
Study
Jeong et al (2007)
Eroglu et al (2009)
Ahn et al (2008)
Subjects with metabolic syndrome associated with human immunodeficiency virus infection commonly present with abnormal regional fat distribution and increased visceral adiposity. Hence, this finding suggests that the echocardiographic epicardial fat thickness may serve as independent predictor of subclinical atherosclerosis in subjects with excess visceral adiposity. Similar results have been recently reported in a more general high-risk population.
Interestingly, epicardial fat thickness was correlated with C-IMT and arterial stiffness better than waist circumference in hypertensive subjects.
ment.
exercise programs,
and hormone-replacement treat-
Echocardiographic epicardial fat thickness significantly decreased in all 3 studies that included body weight modulations and changes. In fact, epicardial fat decreased after very low calorie diet, bariatric surgery–induced weight loss, and moderate aerobic exercise.
Of great interest, the weight loss intervention study showed that the decrease in epicardial fat during weight loss was quicker and higher than the decreases in body mass index, waist circumference, and body weight, common indices of body fatness.
We may assume that epicardial fat reflects the more rapid and massive visceral fat loss after a very low calorie diet. This finding may open new perspectives in the management of patients with high cardiometabolic risk.
Echocardiographic epicardial fat could become a new target during
pharmaceutical treatments directly or indirectly targeting the fat.
Correlation With LV Mass and Function
Increased LV mass and LV hypertrophy are independent cardiovascular risk factors. Increased epicardial fat thickness has been associated with changes in LV mass and diastolic function, as detected by echo-
Echocardiographic findings seem to be in agreement with autopsy studies.
Although epicardial fat located over both ventricles normally accounted for about 20% of the total ventricular mass, left, right, and total epicardial fat weights are significantly greater in hypertrophied hearts.
LV hypertrophy seems to be associated with a proportional increase in epicardial fat mass. Echocardiographic LV mass is significantly correlated with the amount of epicardial fat thickness in subjects with a wide range of adiposity, independent of body mass index and age.
Because of the relationship between epicardial fat and blood pressure, vascular changes and the metabolic syndrome, the relationship to LV hypertrophy is in all likelihood multifactorial. An increase in epicardial fat thickness is also significantly correlated with enlarged atria and impaired right ventricular and LV diastolic filling in morbidly obese subjects.
However, metabolically healthy obesity can be independently associated with these abnormalities.
POTENTIAL USE OF ECHOCARDIOGRAPHIC EPICARDIAL
FAT FOR MONITORING THERAPY
On the basis of the evidence that epicardial fat reflects visceral adiposity, its echocardiographic measurement has been used as a therapeutic
target in subjects who undergo weight-loss interventions,
bariatric
FUTURE DIRECTIONS
Although several types of evidence have been provided, most published studies might not have large enough sample sizes to draw definitive conclusions to establish a strong association between echocardiographic epicardial fat thickness and cardiometabolic risk. The currently available data might not allow a precise estimate of the relationshipr, might not allow to fully explore the relationship within various subgroups, and might not allow the calculation of the diagnostic properties of epicardial fat with precision. A larger sample size would make all of these evaluations possible and therefore make the results applicable in a general population. Whether this echocardiographic measurement may provide incremental or superior information compared with other more commonly used anthropometric markers, such as waist circumference, is still not completely established but is currently under evaluation. Ethnic differences in echocar-
diographic epicardial fat thickness have also been reported recently.
Several lines of research pointed out the role of ethnicity in cardiovascular disease. Echocardiographic epicardial fat might be a helpful marker of visceral adiposity in multiethnic population studies. Threshold values of high-risk epicardial fat thickness may therefore vary among different populations and ethnic groups. It can be also
Journal of the American Society of Echocardiography
Volume 22 Number 12
Iacobellis and H. J. Willens 1317 postulated that the cutoff values could be different if they aimed to predict metabolic syndrome or CAD. Although the majority of the studies have found positive relationships between epicardial fat and cardiovascular risk, a few studies have questioned this association.
Subepicardial adipose tissue on the free wall of the right ventricle was measured at end-diastole, but it was not associated with the severity of CAD in that study.
It also has to be proven whether echocardiographic epicardial fat is associated with intramyocardial and intrahepatic fat accumulation, as measured by magnetic resonance spectroscopy.
Whether or not echocardiographic epicardial fat thickness may really have the diagnostic properties to serve as an indicator of cardiovascular risk should be analyzed in large, randomized, and well-studied multiethnic populations. Finally, the role of epicardial fat as a cardiometabolic risk marker might be stronger in association with other cardiovascular risk factors, considered singly or in combination.
CONCLUSIONS
Echocardiographic epicardial fat is an inexpensive, reproducible, and direct measure of visceral fat. It may have an important role in predicting and stratifying cardiovascular risk in both clinical care and the research setting. However, more robust and convincing evidence is necessary to evaluate whether echocardiographic epicardial fat thickness may have these diagnostic and predictive properties and really become a routine way of assessing cardiovascular risk in a clinical setting. Further investigations should be encouraged to confirm or refute a physiologic mechanism or explanation for a relationship between epicardial fat and cardiovascular risk. Future studies in these directions seem to be warranted.
REFERENCES
1. Iacobellis G, Corradi D, Sharma AM. Epicardial adipose tissue: anatomic, biomolecular and clinical relationships with the heart. Nat Clin Pract Cardiovasc Med 2005;2:536-43.
2. Sacks HS, Fain JN. Human epicardial adipose tissue: a review. Am Heart J
2007;153:907-17.
3. Rabkin RW. Epicardial fat: properties, function and relationship to obesity.
Obesity Rev 2007;8:253-61.
4. Reiner L, Mazzoleni A, Rodriguez FL. Statistical analysis of the epicardial fat weight in human hearts. AMA Arch Pathol 1955;60:369-73.
5. Schejbal V. Epicardial fatty tissue of the right ventricle: morphology, morphometry and functional significance. Pneumologie 1989;43:490-9.
6. Iacobellis G, Barbaro G. The double role of epicardial adipose tissue as proand anti-inflammatory organ. Horm Metab Res 2008;40:442-5.
7. Marchington JM, Pond CM. Site specific properties of pericardial and epicardial adipose tissue: the effects of insulin and high-fat feeding on lipogenesis and the incorporation of fatty acids in vivo. Int J Obesity 1990;14:
1013-22.
8. Sacks HS, Fain JN, Holman B, Cheema P, Chary A, Parks F, et al. Uncoupling protein-1 and related mRNAs in human epicardial and other adipose tissues: epicardial fat functioning as brown fat. J Clin Endocrinol Metab
2009;94:3611-5.
9. Mazurek T, Zhang L, Zalewski A, Mannion JD, Diehl JT, Arafat H, et al.
Human epicardial adipose tissue is a source of inflammatory mediators.
Circulation 2003;108:2460-6.
10. Baker AR, Silva NF, Quinn DW, Harte AL, Pagano D, Bonser RS, et al. Human epicardial adipose tissue expresses a pathogenic profile of adipocytokines in patients with cardiovascular disease. Cardiovasc Diabetol 2006;
13:1.
11. Chaldakov GN, Fiore M, Stankulov IS, Manni L, Hristova MG, Antonelli A, et al. Neurotrophin presence in human coronary atherosclerosis and metabolic syndrome: a role for NGF and BDNF in cardiovascular disease?
Prog Brain Res 2004;146:279-89.
12. Kremen J, Dolinkova M, Krajickova J, Blaha J, Anderlova K, Lacinova Z, et al. Increased subcutaneous and epicardial adipose tissue production of proinflammatory cytokines in cardiac surgery patients: possible role in postoperative insulin resistance. J Clin Endocrinol Metab 2006;91:
4620-7.
13. Cheng KH, Chu CS, Lee KT, Lin TH, Hsieh CC, Chiu CC, et al. Adipocytokines and proinflammatory mediators from abdominal and epicardial adipose tissue in patients with coronary artery disease. Int J Obes (Lond)
2008;32:268-74.
14. Fain JN, Sacks HS, Buehrer B, Bahouth SW, Garrett E, Wolf RY, et al. Identification of omentin mRNA in human epicardial adipose tissue: comparison to omentin in subcutaneous, internal mammary artery periadventitial and visceral abdominal depots. Int J Obes (Lond) 2008;32:810-5.
15. Iacobellis G, Pistilli D, Gucciardo M, Leonetti F, Miraldi F, Brancaccio G, et al. Adiponectin expression in human epicardial adipose tissue in vivo is lower in patients with coronary artery disease. Cytokine 2005;
29:251-5.
16. Iacobellis G, di Gioia CR, Cotesta D, Petramala L, Travaglini C, De
Santis V, et al. Epicardial adipose tissue adiponectin expression is related to intracoronary adiponectin levels. Horm Metab Res 2009;41:227-31.
17. Silaghi A, Achard V, Paulmyer-Lacroix O, Scridon T, Tassistro V, Duncea I, et al. Expression of adrenomedullin in human epicardial adipose tissue: role of coronary status. Am J Physiol Endocrinol Metab 2007;293:
E1443-50.
18. Iacobellis G, Gioia CR, Di Vito M, Petramala L, Cotesta D, De Santis V, et al. Epicardial adipose tissue and intracoronary adrenomedullin levels in coronary artery disease. Horm Metab Res. In press.
19. Clark A. Lectures on diseases of the heart: delivered at the college of physicians and surgeons. New York: Bermingham & Company; 1884.
142-149.
20. Iacobellis G. Epicardial and pericardial fat: close, but very different.
Obesity (Silver Spring) 2009;17:625.
21. Shirani J, Berezowski K, Roberts WC. Quantitative measurement of normal and excessive (cor adiposum) subepicardial adipose tissue, its clinical significance, and its effect on electrocardiographic QRS voltage. Am J
Cardiol 1995;76:414-8.
22. Schoenmackers J, Willmen HR. On lipomatosis cordis, its relations to the efficiency and insufficiency of the right ventricle [article in German]. Arch
Kreislaufforsch 1963;40:251-83.
23. Ho E, Shimada Y. Formation of the epicardium studied with the scanning electron microscope. Dev Biol 1978;66:579-85.
24. Sons HU, Hoffmann V. Epicardial fat cell size, fat distribution and fat infiltration of the right and left ventricle of the heart. Anat Anz 1986;161:
355-73.
25. Cle´ment K, Basdevant A, Dutour A. Weight of pericardial fat on coronaropathy. Arterioscler Thromb Vasc Biol 2009;29:615.
26. Nelson AJ, Worthley MI, Psaltis PJ, Carbone A, Dundon BK, Duncan RF, et al. Validation of cardiovascular magnetic resonance assessment of pericardial adipose tissue volume. J Cardiovasc Magn Reson 2009;11:
15-8.
27. Mahabadi AA, Massaro JM, Rosito GA, Levy D, Murabito JM, Wolf PA, et al. Association of pericardial fat, intrathoracic fat, and visceral abdominal fat with cardiovascular disease burden: the Framingham Heart Study. Eur
Heart J 2009;30:850-6.
28. Fox CS, Gona P, Hoffmann U, Porter SA, Salton CJ, Massaro JM, et al. Pericardial fat, intrathoracic fat, and measures of left ventricular structure and function: the Framingham Heart Study. Circulation 2009;119:1586-91.
29. Marchington JM, Mattacks CA, Pond CM. Adipose tissue in the mammalian heart and pericardium; structure, foetal development and biochemical properties. Comp Biochem Physiol 1989;94B:225-32.
30. Moore KL, Persaud TVN. The developing human. Clinically oriented embryology. 7th ed. Philadelphia, PA: Saunders; 2003: 189.
1318 Iacobellis and H. J. Willens Journal of the American Society of Echocardiography
December 2009
31. Corradi D, Maestri R, Callegari S, Pastori P, Goldoni M, Luong TV, et al.
The ventricular epicardial fat is related to the myocardial mass in normal, ischemic and hypertrophic hearts. Cardiovasc Pathol 2004;13:313-6.
32. Rosito GA, Massaro JM, Hoffmann U, Ruberg FL, Mahabadi AA,
Vasan RS, et al. Pericardial fat, visceral abdominal fat, cardiovascular disease risk factors, and vascular calcification in a community-based sample: the Framingham Heart Study. Circulation 2008;117:605-13.
33. Ding J, Hsu FC, Harris TB, Liu Y, Kritchevsky SB, Szklo M, et al. The association of pericardial fat with incident coronary heart disease: the Multi-
Ethnic Study of Atherosclerosis (MESA). Am J Clin Nutr 2009;90:
499-504.
34. Greif M, Becker A, von Ziegler F, Lebherz C, Lehrke M, Broedl UC, et al.
Pericardial adipose tissue determined by dual source CT is a risk factor for coronary atherosclerosis. Arterioscler Thromb Vasc Biol 2009;29:781-6.
35. Taguchi R, Takasu J, Itani Y, Yamamoto R, Yokoyama K, Watanabe S, et al.
Pericardial fat accumulation in men as a risk factor for coronary artery disease. Atherosclerosis 2001;157:203-9.
36. Wheeler GL, Shi R, Beck SR, Langefeld CD, Lenchik L, Wagenknecht LE, et al. Pericardial and visceral adipose tissues measured volumetrically with computed tomography are highly associated in type 2 diabetic families.
Invest Radiol 2005;40:97-101.
37. Silaghi A, Piercecchi-Marti MD, Grino M, Leonetti G, Alessi MC,
Clement K, et al. Epicardial adipose tissue extent: relationship with age, body fat distribution, and coronaropathy. Obesity (Silver Spring) 2008;
16:2424-30.
38. Gorter PM, de Vos AM, van der Graaf Y, Stella PR, Doevendans PA,
Meijs MF, et al. Relation of epicardial and pericoronary fat to coronary atherosclerosis and coronary artery calcium in patients undergoing coronary angiography. Am J Cardiol 2008;102:380-5.
39. de Vos AM, Prokop M, Roos CJ, Meijs MF, van der Schouw YT, Rutten A.
Peri-coronary epicardial adipose tissue is related to cardiovascular risk factors and coronary artery calcification in post-menopausal women. Eur
Heart J 2007;29:777-83.
40. Wang CP, Hsu HL, Hung WC, Yu TH, Chen YH, Chiu CA, et al. Increased epicardial adipose tissue (EAT) volume in type 2 diabetes mellitus and association with metabolic syndrome and severity of coronary atherosclerosis. Clin Endocrinol (Oxf) 2009;70:876-82.
41. Djaberi R, Schuijf JD, van Werkhoven JM, Nucifora G, Jukema JW, Bax JJ.
Relation of epicardial adipose tissue to coronary atherosclerosis. Am J
Cardiol 2008;102:1602.
42. Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, et al., INTER-
HEART Study Investigators. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 2004;364:937-52.
43. Fox CS, Massaro JM, Hoffmann U, Pou KM, Maurovich-Horvat P, Liu CY, et al. Abdominal visceral and subcutaneous adipose tissue compartments: association with metabolic risk factors in the Framingham Heart Study.
Circulation 2007;116:39-48.
44. Iacobellis G. Imaging of visceral adipose tissue: an emerging diagnostic tool and therapeutic target. Curr Drug Targets Cardiovasc Haematol Disord 2005;5:345-53.
45. Iacobellis G, Assael F, Ribaudo MC, Zappaterreno A, Alessi G, Di Mario U, et al. Epicardial fat from echocardiography: a new method for visceral adipose tissue prediction. Obes Res 2003;11:304-10.
46. Iacobellis G, Willens HJ, Barbaro G, Sharma AM. threshold values of highrisk echocardiographic epicardial fat thickness. Obesity (Silver Spring)
2008;16:887-92.
47. Sade LE, Eroglu S, Bozbas H, Ozbic¸er S, Hayran M, Haberal A, et al. Relation between epicardial fat thickness and coronary flow reserve in women with chest pain and angiographically normal coronary arteries. Atherosclerosis 2009;204:580-5.
48. Jeong JW, Jeong MH, Yun KH, Oh SK, Park EM, Kim YK. Echocardiographic epicardial fat thickness and coronary artery disease. Circ J 2007;
71:536-9.
49. Natale F, Tedesco MA, Mocerino R, de Simone V, Di Marco GM,
Aronne L, et al. Visceral adiposity and arterial stiffness: echocardiographic epicardial fat thickness reflects, better than waist circumference, carotid arterial stiffness in a large population of hypertensives. Eur J Echocardiogr
2009;10:549-55.
50. Saura D, Oliva MJ, Rodrı´guez D, Pascual-Figal DA, Hurtado JA, Pinar E, et al. Reproducibility of echocardiographic measurements of epicardial fat thickness. Int J Cardiol. In press.
51. Wang TD, Lee WJ, Shih FY, Huang CH, Chang YC, Chen WJ, et al. Relations of epicardial adipose tissue measured by multidetector computed tomography to components of the metabolic syndrome are region-specific and independent of anthropometric indexes and intraabdominal visceral fat. J Clin Endocrinol Metab 2009;94:662-9.
52. Sarin S, Wenger C, Marwaha A, Qureshi A, Go BD, Woomert CA, et al.
Clinical significance of epicardial fat measured using cardiac multislice computed tomography. J Cardiol 2008;102:767-71.
53. Abbara S, Desai JC, Cury RC, Butler J, Nieman K, Reddy V. Mapping epicardial fat with multi-detector computed tomography to facilitate percutaneous transepicardial arrhythmia ablation. Eur J Radiol 2006;57:417-22.
54. Iacobellis G, Sharma AM. Adiposity of the heart. Ann Intern Med 2006;
145:554-5.
55. Kankaanpaa M, Lehto HR, Parkka J Komu P, Viljanen A, Ferrannini E, et al. Myocardial triglyceride content and epicardial adipose mass in human obesity: relationship to left ventricular function and serum free fatty acid levels. J Clin Endocrinol Metab 2006;91:4689-95.
56. Iacobellis G, Ribaudo MC, Assael F, Vecci E, Tiberti C, Zappaterreno A, et al. Echocardiographic epicardial adipose tissue is related to anthropometric and clinical parameters of metabolic syndrome: a new indicator of cardiovascular risk. J Clin Endocrinol Metab 2003;88:5163-8.
57. Iacobellis G, Leonetti F. Epicardial adipose tissue and insulin resistance in obese subjects. J Clin Endocrinol Metab 2005;90:6300-2.
58. Iacobellis G, Barbaro G, Gerstein HC. Relationship of epicardial fat thickness and fasting glucose. Int J Cardiol 2008;128:424-6.
59. Malavazos AE, Ermetici F, Cereda E, Coman C, Locati M, Morricone L, et al. Epicardial fat thickness: relationship with plasma visfatin and plasminogen activator inhibitor-1 levels in visceral obesity. Nutr Metab Cardiovasc Dis 2008;18:523-30.
60. Ahn SG, Lim HS, Joe DY, Kang SJ, Choi BJ, Choi SY. Relationship of epicardial adipose tissue by echocardiography to coronary artery disease.
Heart 2008;94:e7.
61. Iacobellis G, Pellicelli AM, Grisorio B, Barbarini G, Leonetti F, Sharma AM, et al. Relation of epicardial fat and alanine aminotransferase in subjects with increased visceral fat. Obesity (Silver Spring) 2008;16:179-83.
62. Eroglu S, Sade LE, Yildirir A, Bal U, Ozbicer S, Ozgul AS, et al. Epicardial adipose tissue thickness by echocardiography is a marker for the presence and severity of coronary artery disease. Nutr Metab Cardiovasc Dis 2009;
19:211-7.
63. Iacobellis G, Gao YJ, Sharma AM. Do cardiac and perivascular adipose tissue play a role in atherosclerosis? Curr Diab Rep 2008;8:20-4.
64. Iacobellis G, Pellicelli AM, Sharma AM, Grisorio B, Barbarini G, Barbaro G.
Relation of subepicardial adipose tissue to carotid intima-media thickness in patients with human immunodeficiency virus. Am J Cardiol 2007;99:
1470-2.
65. Iacobellis G, Sharma AM, Pellicelli AM, Grisorio B, Barbarini G, Barbaro G.
Epicardial adipose tissue is related to carotid intima-media thickness and visceral adiposity in HIV-infected patients with highly active antiretroviral therapy-associated metabolic syndrome. Curr HIV Res 2007;5:
275-9.
66. Iacobellis G, Ribaudo MC, Zappaterreno A, Iannucci CV, Leonetti F. Relation between epicardial adipose tissue and left ventricular mass. Am J
Cardiol 2004;94:1084-7.
67. Iacobellis G, Pond CM, Sharma AM. Different ‘‘weight’’ of cardiac and general adiposity in predicting left ventricle morphology. Obesity (Silver
Spring) 2006;14:1679-84.
68. Iacobellis G, Leonetti F, Singh N, Sharma AM. Relationship of epicardial adipose tissue with atrial dimensions and diastolic function in morbidly obese subjects. Int J Cardiol 2007;115:272-3.
69. Iacobellis G, Ribaudo MC, Leto G, Zappaterreno A, Vecci E, Di Mario U, et al. Influence of excess fat on cardiac morphology and function: study in uncomplicated obesity. Obes Res 2002;10:767-73.
Journal of the American Society of Echocardiography
Volume 22 Number 12
Iacobellis and H. J. Willens 1319
70. Iacobellis G, Singh N, Wharton S, Sharma AM. Substantial changes in epicardial fat thickness after weight loss in severely obese subjects. Obesity
(Silver Spring) 2008;16:1693-7.
71. Willens HJ, Byers P, Chirinos JA, Labrador E, Hare JM, de Marchena E. Effects of weight loss after bariatric surgery on epicardial fat measured using echocardiography. Am J Cardiol 2007;99:1242-5.
72. Kim MK, Tomita T, Kim MJ, Sasai H, Maeda S, Tanaka K. Aerobic exercise training reduces epicardial fat in obese men. J Appl Physiol 2009;106:5-11.
73. Lanes R, Soros A, Flores K, Gunczler P, Carrillo E, Bandel J. Endothelial function, carotid artery intima-media thickness, epicardial adipose tissue, and left ventricular mass and function in growth hormone-deficient adolescents: apparent effects of growth hormone treatment on these parameters. J Clin Endocrinol Metab 2005;90:3978-82.
74. Iacobellis G, Sharma AM. Epicardial adipose tissue as new cardio-metabolic risk marker and potential therapeutic target in the metabolic syndrome. Curr Pharm Des 2007;13:2180-4.
75. Willens HJ, Go´mez-Marı´n O, Chirinos JA, Goldberg R, Lowery MH,
Iacobellis G. Comparison of epicardial and pericardial fat thickness assessed by echocardiography in African American and non-Hispanic white men: a pilot study. Ethn Dis 2008;18:311-6.
76. Chaowalit N, Somers VK, Pellikka PA, Rihal CS, Lopez-Jimenez F. Subepicardial adipose tissue and the presence and severity of coronary artery disease. Atherosclerosis 2006;186:354-9.
77. Perseghin G, Lattuada G, De Cobelli F, Esposito A, Belloni E, Natali G, et al.
Increased mediastinal fat and impaired left ventricular energy metabolism in young men with newly found fatty liver. Hepatology 2008;47:51-8.