In Vivo Determination of Condylar Lift-off and Screw
advertisement

The Journal of Arthroplasty Vol. 14 No. 3 1999
In Vivo D e t e r m i n a t i o n of Condylar Lift-off
a n d S c r e w - H o m e in a M o b i l e - B e a r i n g
Total K n e e A r t h r o p l a s t y
James
B. S t i e h l , M D , * D o u g l a s
A. D e n n i s ,
MD, t Richard
a n d H a l S. C r a n e ,
D. K o m i s t e k ,
PhD,-~
MDt
Abstract: Twenty subjects implanted with the low-contact stress (LCS) cruciatesacrificing, mobile-bearing total knee arthroplasty underwent dynamic videofluoroscopy during in vivo weight-bearing conditions using a 3-dimensional computer-aided
design (CAD) interactive modeling method. Ninety percent of the subjects demonstrated significant lift-off during stance phase of gait. Condylar lift-off was present at
both the medial and the lateral condyles. The maximal medial lift-off was 2.12 mm,
whereas the greatest lateral lift-off was 3.53 ram. The maximal positive screw-home
was 9.6 °, whereas the maximal negative or reverse screw-home was 6.2 ° . The
average screw-home rotation was positive 0.5 ° . In 50% of patients, medial condylar
translation was unexpectedly greater than lateral condylar motion. Condylar lift-off
and screw-home motion are significant kinematic functions in this rotationally
unconstrained total condylar knee arthroplasty. Key words: total knee arthroplasty,
kinematics, condylar lift-off, screw-home rotation.
In total k n e e arthroplasty (TKA), k n o w l e d g e of
k i n e m a t i c function is necessary if the in vivo weightbearing forces a n d shear stresses applied to the
bearing surfaces are to be determined. Posterior
cruciate-retaining designs t e n d to h a v e lower conformity to allow greater rotational freedom, believed to be necessary for n o r m a l function a n d
to lower stresses at the i m p l a n t - b o n e interface.
Posterior cruciate-sacrificing implants h a v e higher
conformity, w h i c h increases i m p l a n t stability a n d
i m p r o v e s w e a r characteristics. F r o m a r e v i e w of
the literature, w e could find no clear a d v a n t a g e
of one t e c h n i q u e or implant, a l t h o u g h certain posterior cruciate-retaining designs h a v e s h o w n a dis-
turbing incidence of osteolysis not recognized with
older posterior cruciate-sacrificing total condylar
designs [1-5]. Blunn et al. [6] d e m o n s t r a t e d p a t t e r n
w e a r a n d peripheral w e a r in designs with polyethylene delamination, k n o w n to result f r o m the m o s t
severe wear.
The potential for femoral-tibial separation or
condylar lift-off during weight-bearing has b e e n
postulated by several authors. Dennis eta]. [7] w e r e
able to d e m o n s t r a t e condylar lift-off in b o t h posterior c r u c i a t e - r e t a i n i n g a n d p o s t e r i o r c r u c i a t e sacrificing designs using in vivo d y n a m i c videofluoroscopy. Nilsson et al. [8] h a v e also s h o w n this
p h e n o m e n o n using stereoradiography. The clinical
implication of this finding is that edge loading at the
peripheral surface of the tibia] plateau m a y be
deleterious, particularly if a Jlat-on-flat condylar
design is used [9,10].
In vivo rotational m o v e m e n t in TKA has b e e n
investigated using several methods, including roentgen s t e r e o p h o t o g r a m m e t r y , videofluoroscopy, a n d
electromagnetic orthotic fixtures [8,11,I2]. These
From the *Midwest Orthopaedic Biomechanical Laboratory, St.
Luke's Hospital, Milwaukee, Wisconsin; and ~-Rose Musculoskeletal
Research Laboratory, Rose Medical Center, Denver, Colorado.
Submitted March 15, 1998; accepted September 1 l, 1998.
Reprint requests: James B. StiehI, MD, 2015 E. Newport, #703,
Milwaukee, WI 53211.
Copyright © 1999 by Churchill Livingstone®
0883-5403/99/1403-0006510.00/0
293
294
The Journal of Arthroplasty Vol, 14 No. 3 April 1999
studies have typically s h o w n screw-home or external
rotation of the tibia in extension with internal
rotation as the angle of flexion increases. Alterations
from the rotation of the n o r m a l knee m a y be related
to anterior cruciate deficiency, prosthetic geometry,
and differences in surgical technique in individual
patients. Knowledge of rotational m o v e m e n t is an
important consideration for understanding polyethylene wear patterns, in which exaggerated sliding
motion m a y produce detrimental delamination wear.
Dynamic videofluoroscopy has emerged as a valuable scientific tool for investigating in vivo kinematic
performance of TKA. Our initial experience with
the technique allowed the determination of 1-point
contact in the sagittal plane, such as the lateral
femoral condyle with the tibial plateau {13]. More
recently, we have used 3-dimensional model fitting
to determine kinematic relationships accurately.
With this method, determination of both medial
and lateral condylar position as well as condylar
lift-off and s c r e w - h o m e rotation can be m e a s u r e d in
gait [ 14].
The purpose of this paper is to use in vivo fluoroscopy with an interactive model-fitting technique to
examine coronal and transverse plane m o t i o n in a
mobile-bearing TKA during gait. The results are
compared with our prior experience with fixed
bearing designs and with information on n o r m a l
knees from literature review. The low-contact stress
(LCS) rotating platform prosthesis (Depuy, Inc, Warsaw, IN) is a posterior cruciate-sacrificing implant
that was designed to have u n c o n s t r a i n e d rotational
f r e e d o m and conforming coronal plane articulation
that allowed condylar lift-off.
Materials and Methods
Before inclusion in this study, each patient reviewed and signed an investigation review b o a r d approved consent form. We p e r f o r m e d dynamic
fluoroscopy u n d e r weight-bearing conditions in 20
patients with a c e m e n t e d posterior cruciate-sacrificing LCS mobile-bearing (rotating platform) TKA
(Deputy, Warsaw, IN). The patients were chosen on
the basis of an excellent clinical result (>90/90)
using the Knee Society scoring system. The time
from surgery to analysis was a m i n i m u m of 12
m o n t h s in all cases. The resultant femoral-tibial
alignment was n o r m a l in all (range, 5o-7 °) with
excellent stability in extension.
Each patient u n d e r w e n t 2-dimensional videofluoroscopy using a VJ Works fluoroscopy unit (VF
Works, Palm Harbor, FL), which produces images at
a rate of 30 Hz. The technique required the patient
to take 1 step while walking on an elevated platform. The radiology technician t h e n followed the
knee joint by attempting to keep the lateral side of
the knee centered on the x-ray machine's fluoroscopic image at all times. This was done to simulate
the walking gait cycle from heel-strike to toe-off.
Video Analysis
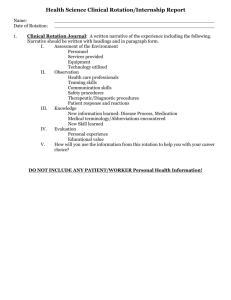
We have evolved our video analysis to an interactive model-fitting technique. This m e t h o d fits 3-dimensional computer-aided design (CAD) solid models of the femoral and tibial implants onto the
2-dimensional fluoroscopic silhouette images. The
fluoroscopic images had b e e n stored on videotapes
for subsequent redigitization using a frame grabber.
The videos were t h e n analyzed on a c o m p u t e r
workstation using the interactive c o m p u t e r algorithm (Fig. 1).
The femoral and tibial c o m p o n e n t s of the best-fit
overlay were rotated into the precise sagittal plane
to measure anteroposterior contact of the medial
and lateral condyles and screw-home rotation, which
is a function of these points. Four distinct positions
of the sagittal plane fluoroscopy images were analyzed during the n o r m a l gait cycle including i) at
heel-strike, ii) at 33% of stance phase, iii) at 66% of
stance phase, and 4) at toe-off. These positions were
confirmed using a second video camera to determine the exact frame of heel-strike and toe-off and
calculating 33 % and 66 % of the weight-bearing gait
cycle.
The overlay model was t h e n rotated into the
frontal plane to measure the distance from the
femoral condyle to the tibial plateau to determine
femoral-tibial lift-off. M e a s u r e m e n t of condylar liftoff is done by comparing the difference of the
medial and lateral condylar distances to the tibial
baseplate. It is assumed that the condyles are in a
similar plane of tibial contact, and there should be
little difference in plastic thickness.
Rotation was d e t e r m i n e d from an arbitrary reference line that was perpendicular to the sagittaltibial plane. Medial and lateral condylar translation
at each point in the gait cycle were used to calculate
rotation. Determination of the specific medial and
lateral condyle has b e e n easy for several reasons.
First, the leg involved is k n o w n , and therefore
medial and lateral overlay prosthetic condyles are
k n o w n . Second, most implants are asymmetric, and
condylar shapes become obvious. Third, for symmetric implants, the lateral condyle is always closer to
the x-ray tube and is larger.
For the anteroposterior reference, a positive reference is d e n o t e d as anterior and a negative posterior
to the sagittal plane midline of the tibial prosthesis.
Normal or positive s c r e w - h o m e m o t i o n was defined
as tibial internal rotation in relation to the distal
f e m u r with increasing flexion [15]. Femoral-tibial
Condylar Liftoff and Screw Home in Mobile-Bearing TKA
Fig. 1. Interactive 3-dimensional CAD modeling showing
(A) CAD model overlay superimposed on 2-dimensional
videofluoroscopy frame. (B)
Example of sagittal view of
solid model. (C) Example of
coronal view of solid model.
(D) Coronal view demonstrating condylar lift-off.
A
•
Stiehl et al.
295
B
C
contact of the medial a n d lateral condyles could
h a v e 3 patterns of translation to cause this motion:
i) Lateral condyle m o v e s m o r e posterior t h a n the
medial; ii) lateral condyle m o v e s posterior, w h e r e a s
the medial condyle m o v e s anterior; a n d iii) lateral
condyle m o v e s less anterior t h a n the medial condyle. Reverse or negative s c r e w - h o m e was defined
as tibial external rotation in relation to the f e m u r
w i t h increasing flexion. Femoral-tibial contact of
the medial a n d lateral condyles could h a v e 3 patterns of translation to cause the motion: i) medial
condyle m o v e s m o r e posterior t h a n the lateral; ii)
medial condyle m o v e s posterior, w h e r e a s the lateral
m o v e s anterior; a n d iii) medial condyle m o v e s less
anterior t h a n the lateral condyle.
Error Analysis
An error analysis was p e r f o r m e d to d e t e r m i n e the
reproducibility a n d accuracy of m e a s u r e m e n t of o u r
technique. This analysis was done b y fluoroscoping
i m p l a n t c o m p o n e n t s m o u n t e d on a 6 ° of f r e e d o m
apparatus. Accurate positioning of the c o m p o n e n t s
was achieved using rotational a n d translational
stages w i t h a n accuracy of 15 arc seconds a n d 0.01
m m . The c o m p o n e n t s w e r e set in an initial position,
t h e n rotated and translated to k n o w n values. Fluoroscopic images of the c o m p o n e n t s w e r e created at
each setting. The 3-dimensional model-fitting process was p e r f o r m e d for each setting of the rotational
D
a n d translational stages to d e t e r m i n e the relative
pose of the c o m p o n e n t s . A second d y n a m i c test was
p e r f o r m e d to d e t e r m i n e the effect of motion. The
c o m p o n e n t s w e r e pulled t h r o u g h the fluoroscopic
scene at a variable speed b e t w e e n 0.5 a n d 1.0 feet
per second. The translational and rotational 3-dim e n s i o n a l model-fitting technique was accurate to
0.5 m m and 0.5 ° [14]. A threshold of 0.75 m m and
0.75 ° (50% safety factor) was used to account for
u n k n o w n variables.
Results
Condylar Lift-off
Significant condylar lift-off was seen in 90% of
subjects at heel-strike a n d 66% of subjects at stance
phase a n d toe-off. In 50% of TKAs, we f o u n d b o t h
medial and lateral lift-off, w h e r e a s only 15% s h o w e d
nonsignificant lift-off (<0.75 m m ) . The greatest
medial lift-off was 2.12 m m , w h e r e a s the greatest
lateral was 3.53 m m (Table 1).
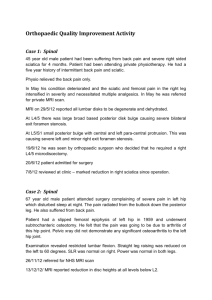
Screw-Home Rotation
Seven of 20 patients d e m o n s t r a t e d positive screwh o m e rotation w i t h tibial internal rotation o n flexion. In 5 subjects, the overall rotation was m i n i m a l
or insignificant ( < 0.75). Eight patients s h o w e d negative s c r e w - h o m e w i t h tibial external rotation on
296
The Journal of ArthroplastyVol. 14 No. 3April 1999
flexion. Six patients demonstrated greater t h a n 5 °
rotation with the maximal positive s c r e w - h o m e of
9.6 °, whereas the maximal negative s c r e w - h o m e
was negative 6.2 ° . The average s c r e w - h o m e for the
group was a positive 0.5 °. We could not find a
relationship b e t w e e n condylar lift-off and a specific
pattern of s c r e w - h o m e because condylar lik-off
was seen with all screw-home possibilities (Table 2;
Fig. 2).
Normal s c r e w - h o m e with medial condylar pivot
and the medial condyle moving less posterior t h a n
the lateral condyle with gait was seen in only 2
patients. Five patients demonstrated abnormal positive screw-home, with the medial condyle m o v i n g
more anterior t h a n the lateral in 4 and the medial
condyle m o v i n g anterior, whereas the lateral condyle m o v e d posterior in 1 (Table 3).
Reverse s c r e w - h o m e was seen in 13 patients. In 5
subjects, the medial condyle translated m o r e posterior t h a n the lateral. For 3 knees, the medial condyle
translated posterior, whereas the lateral m o v e d
anterior. In 5 cases, the medial condyle translated
less anterior t h a n the lateral.
Table 2. Screw-Home Results During 0%, 33%, 66%,
and 100% Stance Phase of Gait Cycle*
Subject
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
Average
0%-33%
33%-66%
66%-100%
0%-100%
2.46
-4.59
-2.92
9.37
4.04
1.04
-1.42
- 1.69
-1.01
0.57
-0.12
-2.72
0.10
0.27
7.22
4.75
-1.60
0.19
--0.96
--0.93
0.29
-2.22
-9.I4
-1.48
1.04
- 1.11
-0.26
1.73
0.21
-2.29
0.14
--2.03
2.33
-2.13
--2.48
3.14
0.91
--1.47
5.45
0.62
- 5.78
1.19
5.90
1.57
0.00
1.78
-0.94
-4.83
0.22
1.60
-0.78
4.39
3.90
4.93
-1.56
1.66
0.14
-0.04
-5.70
0.49
- 3.03
-5.62
-6.16
9.45
5.08
1.72
-2.62
-4.79
-1.03
-0.12
-0.76
-0.35
6.33
3.07
3.18
9.55
-0.55
-1.32
- 1.21
-0.81
0.60
- 0.44
0.34
0.50
*Positive = tibia i n t e r n a l r o t a t i o n ; n e g a t i v e = tibia e x t e r n a l
rotation.
Discussion
Dynamic fluoroscopy has p r o v e d to be invaluable
for investigating kinematic performance of TKA.
Using c o m p u t e r vector analysis, we have previously
identified abnormal anteroposterior translation, loss
Table 1. Lift-Off Results*
% of Gait
Subject
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
Average
0%
33 %
66%
100%
0.81
0.53
0.48
0.81
0.21
-1.41
1.60
-1.31
0.00
0.00
0.91
--0.47
1.01
0.42
1.78
0.66
0.00
1.56
0.40
-I.15
-1.93
0.54
-0.25
0.00
-1.50
2.29
-1.34
0.44
-0.42
-0.13
1.70
- 1.89
--0.22
0.02
-2.05
-0.06
1.19
-0.55
1.59
1.87
1.60
-1.35
-0.09
0.80
-0.55
-1.07
1.08
0.52
1.39
0.09
0.00
0.47
1.19
1.19
-0.43
0.47
-0.46
0.00
0.45
0.00
1.42
-0.16
0.65
2.06
0.19
1.60
1.15
-0.09
1.10
0.85
-0.27
2.12
-1.87
-1.87
-0.54
-0.25
-0.04
-1.70
-3.53
0.89
0.78
1.00
0.63
1.05
*Negative = medial condyle; positive = lateral condyle.
of posterior femoral rollback, and lateral condylar
lift-off in posterior cruciate-retaining TKAs [13].
Evolution of our technique led to an inverse perspective m e t h o d that required developing a library of
CAD implant models that could be m a t c h e d to each
isolated femoral and tibial implant on the video
frame [14]. More recently, we have used an interactive modeling system that allows us to manipulate
the 3-dimensional CAD model implant precisely
onto the video 2-dimensional image. This m e t h o d
does not require precise sagittal plane positioning of
the patient's knee because the video image can
accurately be superimposed e v e n with some degree
of malrotation. The reason for this is that the
complex g e o m e t r y of the implant image allows for
only 1 finite position of the CAD model in space.
The fluoroscopic image can t h e n be extracted leaving the CAD image from which kinematic calculations are possible.
We have b e e n able to demonstrate that condylar
lift-off occurs in all TKAs that we evaluated regardless of surgical technique, including posterior cruciate retention, sacrifice, or substitution. Most of the
mobile-bearing TKAs of this study showed both
medial and lateral condylar lilt-off using a posterior
cruciate-sacrificing technique. The largest a m o u n t
of lift-off was identified in the lateral compartment.
Dennis et al. [7] evaluated posterior cruciatesubstituting TKAs, finding that medial condylar
lift-off occurred about equal to lateral lift-off. In
Condylar Liftoff and Screw Home in Mobile-Bearing TKA
•
Stiehl et al.
297
14
Subject 1
12
¢
Subject 2
10
Subject 3
8
Subject 4
Subject 5
F i g . 2. Five r a n d o m l y s e l e c t e d
patients demonstrating diverse
4
2
d i s t r i b u t i o n of r o t a t i o n .
0
-2
/
-4
/
-6
Heel-strike
33%Stance
66%Stance
Toe-off
% of Stance Phase
posterior cruciate-retaining TKAs, condylar lift-off
was predominantly lateral. Using a different method,
roentgenographic stereophotogrammetry, Nilsson et
al. [8] were also able to demonstrate this p h e n o m enon, w h i c h they defined as tibial rotation (abduction/adduction) about the sagittal axis. In their
study, the LCS mensical-bearing implant revealed a
m e a n of 3 ° adduction at 50 ° flexion, similar to
normal knees. The fact that condylar lift-off occurs
is not surprising considering the adduction and
abduction m o m e n t s that have b e e n hypothesized
with gait {16].
Condylar lift-off becomes a significant issue for
TKA design w h e n one considers peripheral edge
loading that is likely with fiat-on-fiat total condylar
designs [9,10]. Wasielewski et al. [17] and Blunn et
al. [6] f o u n d peripheral wear and pattern wear with
severe polyethylene delamination in these designs.
Because abnormal medial c o m p a r t m e n t anteroposterior translation is c o m p o u n d e d with lateral condylar lift-off, the posterior medial wear patterns identi-
Table 3. Screw-Home Mechanism
Internal
Tibial
Rotation
+
+
+
Type
Normal
Reverse
Reverse
Normal
Normal
Reverse
Condylar M o t i o n
Med
Med
Med
Med
Med
Med
Post < Lat Post
Post > Lat Post
Post:Lat Ant
Ant:Lat Post
Ant:Lat Ant
Ant < Lat Ant
Med, medial; Post, posterior; Lat, lateral; Ant, anterior.
No.
Patients
2
5
3
1
4
5
fled in those studies are expected. The coronal
geometry of the LCS rotating platform implant used
in this study is Conforming in the coronal plane to
allow for congruity with lift-off. Retrievals of this
implant have revealed minimal wear of the polyethylene surface after e x t e n d e d clinical use [ 18].
High rotational constraint in TKA has been recognized as a p r e d o m i n a n t cause of failure in early
hinge designs. Rotational m o v e m e n t of the normal
knee was studied by LaFortune et al. [19] using
high-speed p h o t o g r a p h y and implanted Steinman
pins as skeletal markers in n o r m a l walking volunteers. Internal rotation at heel-strike and toe-off
m e a s u r e d slightly less than 5 °, whereas external
rotation increased to 9 ° during swing phase. Screwhome m o v e m e n t has been described as relative
external rotation of the tibia in relation to the f e m u r
near full extension [20]. Early investigators postulated that abnormalities of knee function are related
to disturbance of this mechanism. K a r r h o l m et
al. [21] demonstrated significant alterations in rota~
tion with anterior cruciate-deficient knees finding a
m o r e externally rotated tibia in extension followed
by decreased internal rotation in flexion. Nilsson et
al. [8] reported similar findings with several different posterior cruciate-retaining TKAs, noting less
terminal screw-home or terminal external tibial rotation, again relating to the m o r e externally rotated
tibia in extension and decreased internal rotation in
flexion.
Nilsson et al. [9] investigated the LCS meniscalbearing total knee implant, finding that initial extension started with a more externally rotated tibia
t h a n n o r m a l and had minimal internal rotation
298
The Journal ofArthroplasty Vol. 14 No. 3April 1999
(mean, 0.5 °) during flexion. Using the LCS rotating
platform implant, w h i c h sacrifices the posterior
cruciate ligament, our study f o u n d similar overall
internal rotation (mean, 0.5 ° ) during flexion, but
our patients d e m o n s t r a t e d m u c h greater variability
with rotation. For example, only 7 of our patients
d e m o n s t r a t e d internal tibial rotation with flexion.
Of that group, only 2 patients had n o r m a l screwh o m e with lateral femoral tibial contact m o v i n g
m o r e posterior t h a n medial contact on flexion. The
other 5 had significant anterior sliding of the medial
condyle to cause internal rotation. Reverse screwh o m e was seen in 13 of our patients, in w h o m there
was actually tibial external rotation in flexion. This
reverse s c r e w - h o m e resulted from exaggerated lateral condylar anterior translation in flexion or medial condylar posterior translation that exceeded
lateral translation. Two patients in our study d e m o n strated greater t h a n 9 ° of tibial internal rotation
with gait.
Other authors have been able to demonstrate
significant tibial rotation of u n c o n s t r a i n e d TKAs. E1
Nahass et al. [11] evaluated the kinematic condylar
posterior cruciate-retaining TKA using electrogoniometers, finding that tibial external rotation on
extension varied from 4.4 ° to 11.3% Markovich et
al. [121 used in vivo videofluoroscopy to evaluate
weight-bearing step-up activity finding 8 ° of tibial
external rotation from flexion to extension. This
rotation occurred from posterior translation of the
medial femoral condyle in extension (average, 6.3
mm), whereas lateral condylar translation was limited.
We have s h o w n that significant rotation and
condylar lift-off were present in a cohort of successfully performed TKAs. The results of our study
suggest that a complex rotational m o t i o n m a y exist
in m a n y with regard to femoral-tibial contact of the
condyles in TKA. Transverse plane rotations and
lift-off for each individual patient were highly variable, reflecting the inability to restore perfectly the
n o r m a l kinematics of the joint. We believe that
these kinematic abnormalities, w h e n exaggerated,
can be related to some of the current problems of
TKA, such as peripheral pattern and posterior medial condylar wear. Further studies are necessary to
investigate the complex relationship of biomechanical and biomaterial p e r f o r m a n c e in TKA. These
data suggest that designs such as the LCS mobilebearing platform, w h i c h a c c o m m o d a t e significant
rotation and lift-off while maintaining high articular
surface congruity, m a y importantly diminish contract surface stresses. This m a y represent an optimal
solution to these unresolved kinematic derangements.
References
1. Malkani AL, Rand JA, Bryan RS, Wallrichs SL: Total
knee arthroplasty with the kinematic condylar prosthesis. J Bone Joint Surg Am 77:423, 1995
2. Ranawat CS, Flynn WE Saddler S, et al: Long-term
results of the total condylar knee arthroplasty. Clin
Orthop 286:94, 1993
3. Stern SH, Insall JN: Posterior stabilized prosthesis:
results after follow-up of nine to twelve years. J Bone
Joint Surg Am 74:980, 1992
4. Kim YH, Oh JH, Oh SH: Osteolysis around cementless
porous-coated anatomic knee prosthesis. J Bone Joint
Surg Br 77:236, 1995
5. Becker M, Insall JN, Faris PM: Bilateral total knee
arthroplasty: one cruciate retaining and one cruciate
substituting. Clin Orthop 271:122, 1991
6. Blunn GW, Joshi AB, Minns RJ, et al: Wear in
retrieved condylar knee arthroplasties. J Arthroplasty
12:281, 1997
7. Dennis DA, Komistek RD, Cheal EJ, Stiehl JB: A
determination of condylar lift-off using fluoroscopy.
Proceedings 43rd Annual Orthopaedic Research Society Meeting, San Francisco, 1997, p 645
8. Nilsson KG, Karrholm J, Gadegaard P: Abnormal
kinematics of the artificial knee: roentgen stereophotogrammetric analysis of 10 Miller-Galante and five
New Jersey LCS knees. Acta Orthop Scand 62:440,
1991
9. Lewis P, Rorabeck CH, Bourne RB, Devane P: Posteromedial tibial polyethylene failure in total knee replacements. Clin Orthop 299:1 l, 1994
10. Feng EL, Stulberg DS, Wixson RS: Progressive subluxation and polyethylene wear in total knee replacements with flat articular surfaces. Clin Orthop 299:
60, 1993
I 1. E1Nahass E, Madson MM, Walker PS: Motion of knee
after condylar resurfacing. Proceedings 36th Orthopaedic Research Society Annual Meeting, New Orleans, 1990, p 476
12. Markovich GD, Banks SA, Hodge WA: Comparison of
passive and active knee replacement kinematics.
Proceedings 43rd Orthopaedic Research Annual Meeting, San Francisco, 1997, p 240
13. Stiehl JB, Komistek RD, Dennis DA, et al: Fluoroscopic analysis of kinematics after posterior-cruciateretaining total knee arthroplasty. J Bone Joint Surg Br
77:884, 1995
14. Dennis DA, Komistek RD, Hoff WA, Gabriel SM: In
vivo kinematics derived using an inverse perspective
technique. Clin Orthop 331:107, 1996
15. Muller W: The knee: form, function and ligament
reconstruction. Springer-Verlag, Berlin, 1983
16. Andriacchi TP, Galante JO: Retention of the posterior
cruciate in total knee arthroplasty. J Arthroplasty
(Suppl) 3:13, 1988
17. Wasielewski RC, Galante JO, Leighty RM, et al: Wear
patterns on retrieved polyethylene tibial inserts and
Condylar Liftoff and Screw Home in Mobile-Bearing TKA
their relationship to technical considerations during
total knee arthroplasty. Clin Orthop 299:31, 1993
18. Collier JP, Mayor MB, McNamara JL, et al: Analysis of
the failure of 122 polyethylene inserts from uncemented tibial knee components. Clin Orthop 273:
232, 1991
19. LaFortune MA, Cavanagh PR, Sommer HJ, Kalenak
•
Stiehl et al.
299
A: Three-dimensional kinematics of the h u m a n knee
during walking. J Biomech 25:347, 1992
20. Hallen LG, Kindahl O: The "screw-home" m o v e m e n t
in the knee joint. Acta Orthop Scand 37:97, 1966
21. Karrholm J, Selvik G, Elmlqvist LG, Hansson LI:
Active knee motion after cruciate ligament rupture:
stereoradiography. Acta Orthop Scand 59:158, 1988