Dissection 32
advertisement

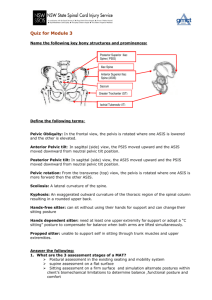
DISSECTION 32 The Pelvis References: M1 327-402; N240, 340-356, 380-383, 390-393, 481; N248, 352-371, 400-403, 410-413, 499; R 327-334, 338-347, 352-355, 419-424, 456-457 AT THE END OF THIS LABORATORY PERIOD YOU WILL BE RESPONSIBLE FOR THE IDENTIFICATION AND DEMONSTRATION OF THE STRUCTURES LISTED BELOW: 1. Bones and bony features: sacrum: (promontory, ala, anterior sacral foramina), coccyx, bony pelvis: (ilium, ischium, pubis, obturator foramen, iliac crest, anterior superior iliac spine, arcuate line, pubic symphysis, ischial tuberosity, ischial spine, greater sciatic notch, lesser sciatic notch). 2. Viscera: urinary bladder (trigone, ureteral orifice, urethral orifice), rectum, ureter, ovary, uterus, uterine tube. 3. Peritoneal folds and fossae: paravesical fossa, pararectal fossa, ureteral fold, rectovesical fold, rectovesical pouch, rectouterine fold, rectouterine pouch, vesicouterine pouch. 4. Mesenteries and ligaments: mesovarium, round ligament of uterus, ovarian ligament, broad ligament (and its subdivisions), suspensory ligament of the ovary, medial umbilical ligament. 5. Muscles: levator ani, coccygeus, arcus tendineus, obturator internus, piriformis. 6. Vessels: external iliac, inferior epigastric, deep circumflex iliac, abnormal obturator from inferior epigastric, common iliac, internal iliac, umbilical, superior vesical, internal pudendal, obturator, inferior gluteal, uterine, iliolumbar, lateral sacral, superior gluteal arteries, external and internal iliac veins. 7. Nerves: femoral, obturator, lumbosacral trunk. YOU SHOULD ALSO BE ABLE TO DO THE FOLLOWING THINGS: 1. Describe the peritoneal reflections in the male and female pelvis. 2. Discuss the lymphatic drainage of each of the pelvic organs. 3. Demonstrate the parts of the bony pelvis. 4. Relate the pelvic organs to the skeleton of the pelvis. 5. Explain the innervation of the pelvic organs and describe the fiber composition and distribution of the pelvic splanchnic nerves. List the results of sectioning the hypogastric plexus or the pelvic splanchnic nerves. 6. List the principal structures which support the uterus. 7. Name and identify the subdivisions of the broad ligament. 8. List 3 differences between the male bony pelvis and the female bony pelvis. 9. Name the subdivisions of the uterine tube. 10. Describe the pelvic diaphragm and its attachments. 11. Give the relationship of the uterine artery to the ureter. 12. Identify structures on cross-sectional drawings, C-T scans, or tissue sections through the pelvis. Dissection 32, The Pelvis Page 2 The Pelvic Skeleton Understanding the pelvic structures and perineum is facilitated by a familiarity with the pelvic skeleton. This consists of the SACRUM, the COCCYX, and the two hip bones (os coxae) which in turn consist of the ILIUM, the ISCHIUM, and the PUBIS (G3.2; N340, 341; N352, 353; A395, 398). Also the function and attachments of the pelvic diaphragm should be understood (G3.4, 5, Table 3.1; N343, 346; N356, 359; A365). Identify the OBTURATOR FORAMEN, the ILIAC CREST, the ANTERIOR SUPERIOR ILIAC SPINE, the ARCUATE LINE, the PUBIC SYMPHYSIS, the ISCHIAL TUBEROSITY, the ISCHIAL SPINE, the GREATER SCIATIC NOTCH, the LESSER SCIATIC NOTCH, and the SACRAL PROMONTORY, ALA OF THE SACRUM and ANTERIOR SACRAL FORAMINA (G4.16, 17, 3.2; N340, 341; N352, 353; A395398). Study the pelvic contents and the reflections of the peritoneum noting the following (G3.8A, 28; N340-341; N352-353; A353-354, 377-378): MALE rectovesical pouch rectovesical fold MALE & FEMALE urinary bladder rectum ureter (pelvic part) paravesical fossa pararectal fossa ureteral fold FEMALE ovary mesovarium round ligament (of uterus) ovarian ligament uterus uterine tube broad ligament rectouterine fold rectouterine pouch vesicouterine pouch suspensory ligament of the ovary In some bodies, especially when much fat is present external to the peritoneum, identification of folds and fossae may be difficult. You will then need to study them from an atlas or on another body and note where they should have appeared on your own specimen. Arteries of the Pelvis Remove the peritoneum from the pelvic organs and clear away the extraperitoneal fat. Clean the EXTERNAL ILIAC VESSELS, which traverse the brim of the pelvis, and note the origins of the INFERIOR EPIGASTRIC and DEEP CIRCUMFLEX ILIAC ARTERIES (N351; N364). Look for an unusual origin of the OBTURATOR ARTERY from the external iliac or inferior epigastric. Clean the COMMON ILIAC and the INTERNAL ILIAC (BNA, hypogastric) vessels and their branches, and trace them as far as may be practical in the intact pelvis (N328, 382, 383; N341, 402, 403). The internal iliac often has two major branches, an anterior branch and a posterior branch, with all of the visceral branches coming from the anterior branch along with the obturator and inferior gluteal. The first large branch is usually the UMBILICAL ARTERY, which in turn gives off one or more SUPERIOR VESICAL ARTERIES to the bladder. Beyond this point the umbilical artery is obliterated and continues to the umbilicus as the MEDIAL UMBILICAL LIGAMENT. The anterior division of the internal iliac also usually, but not always, gives rise to the following arteries: INTERNAL PUDENDAL, OBTURATOR, INFERIOR GLUTEAL, and UTERINE (female only). Using G3.19 or N382, 383; N402, 403 or A355, 364, identify as many of the above as you can. From the posterior branch of the internal iliac look for the ILIOLUMBAR, LATERAL SACRAL, and the SUPERIOR GLUTEAL ARTERIES. Note that the superior and inferior gluteal arteries pass out of the pelvis above and below the PIRIFORMIS MUSCLE respectively and the muscle can be identified on this basis. Considerable variation in the pattern of branching of the internal iliac artery is to be expected; hence, positive identification of a given vessel must be made according to what organ or region it supplies, rather than on its manner of origin. These vessels may be grouped into visceral and parietal arteries, of which the vesicals, middle rectal, deferential (male), UTERINE and vaginal (female) are typically visceral, and the remainder are classified as parietal. The INTERNAL PUDENDAL (predominantly parietal) has visceral branches. Any vessel that cannot be identified positively Dissection 32, The Pelvis while the pelvis is still intact should be reviewed and traced after the pelvis is divided (G3.19; N382, 383; N402, 403; A364). The Pelvic Diaphragm Identify the superior surface of the pelvic diaphragm. This is the internal layer of fascia that invests the LEVATOR ANI and the COCCYGEUS MUSCLES. Look for the ARCUS TENDINEUS where the lateral border of the levator ani crosses the upper part of the OBTURATOR INTERNUS MUSCLE. This arch is attached to the superior pubic ramus anteriorly and to the spine of the ischium posteriorly. Superiorly, its fascia is continuous with that of the iliacus muscle (G3.5; N343, 345, 351; N356, 358, 364; A359, 365). The Lumbar Plexus ON THE RIGHT SIDE ONLY, remove the veins, including the common iliac; free the arteries enough to give access to the anterior rami of lumbar and sacral nerves. Trace the sympathetic trunks into the pelvis. Remove the medial part of the psoas major muscle, but spare nerves that pierce it, the genitofemoral in particular. Identify by number, lumbar nerves 15; the lumbar part of the lumbosacral plexus which gives rise to the FEMORAL, lateral femoral cutaneous and OBTURATOR NERVES; then trace Page 3 these and the genitofemoral to their sites of exit from abdominal or pelvic cavities (N259, 327; N267, 340). Trace the LUMBOSACRAL TRUNK, formed by part of the 4th and most of the 5th lumbar nerves, to its junction with the lst sacral. Further dissection of the sacral portion of the plexus may be deferred until the pelvis is divided (G3.24A; N478-480; N496-498). Plexuses of autonomic nerves are well represented about the walls of organs and arteries of the pelvis. A satisfactory display of them is not ordinarily required in routine dissection, but their presence should not be forgotten. Sympathetic nerves from the caudal part of the sympathetic trunks and parasympathetic nerves (craniosacral division of the autonomic system) from S2, S3, and S4 (pelvic splanchnics) go to the pelvic autonomic plexuses. Their study from a textbook is recommended (M1 358-361, H752756). The pelvic splanchnic nerves can be seen better after the pelvis is divided. The interior of the bladder can be observed by cutting a window through the anterosuperior wall to observe the TRIGONE (G3.16; N353; N366; A356) and the URETERAL and URETHRAL ORIFICES. Dissection 32, The Pelvis Page 4 STUDY QUESTIONS 1. Name the bones that make up the bony pelvis. 1. The two hip bones, the sacrum, and the coccyx. Each hip bone, or os coxae, has three parts: the ilium, the ischium, and the pubis. 2. How are the bones which form the bony pelvis held together? 2. By ligaments and by two synovial joints, the sacroiliac joints, and by two symphyses, the symphysis pubis and the sacrococcygeal joint. 3. What is the pelvic brim? 3. The pelvic brim is a line or ridge that extends from the sacral promontory posteriorly around the lateral margin of the superior pelvic aperture to the top of the symphysis pubis anteriorly. 4. What are the three parts of the pelvic brim? 4. 1) the promontory and anterior border of the ala of the sacrum, 2) the arcuate line of the ilium, 3) the pecten and crest of the pubis. 5. Define the terms major pelvis, minor pelvis, true pelvis, false pelvis, greater pelvis, lesser pelvis, and obstetric pelvis. 5 The major pelvis (also greater or false pelvis) is that part of the bony pelvis above the pelvic brim. The minor (also true, lesser, or obstetric pelvis) is that part of the bony pelvis below the pelvic brim. 6. What is the pelvic inlet? Pelvic outlet? 6. The pelvic inlet, or superior pelvic aperture, is the opening surrounded by the pelvic brim. The pelvic outlet is the inferior pelvic aperture. 7. List major ways in which the female pelvis differs from the male pelvis. 7. 1) Females have a broader sacrum, and thus the hip bones are farther apart. 2) Females have a wider subpubic angle and thus the ischial tuberosities are farther apart. 3) Females have a less curved sacrum, which also increases the size of the inferior pelvic aperture. 8. List the muscles that cross the pelvic brim. 8. 9. List the muscles that line the walls of the true pelvis. 9. 10. Name the muscles that form the pelvic diaphragm. The piriformis and the obturator internus. 10. The levator ani and the coccygeus. Dissection 32, The Pelvis Page 5 11. What part of the levator ani muscle is important in maintaining the angle between the rectum and the anal canal? 11. The puborectalis. 12. Name the nerves that cross the pelvic brim. 12. The lumbosacral trunk, the obturator nerve and the sympathetic trunk on each side. 13. Name the arteries that cross the pelvic brim. 13. Internal iliac, median sacral, superior rectal, and ovarian. 14. What is the relationship of the uterine artery to the ureter? 14. The uterine artery passes anterior and superior to the ureter where they cross near the lateral fornix of the vagina. "Water runs under the bridge." 15. Describe the course of the internal pudendal artery. 15. After branching from the internal iliac artery, it passes inferiorly along the lateral wall of the minor pelvis to the cleft between the piriformis and the coccygeus where it passes through the wall. It then passes superficial to the ischial spine or the sacrospinous ligament and enters the pudendal canal in the lateral wall of the ischiorectal fossa. The pudendal canal is located in the fascia of the obturator internus muscle. 16. What are the terminal branches of the internal pudendal artery? 16. The deep artery of the penis (clitoris) and the dorsal artery of the penis (clitoris) 17. Name the pelvic venous plexuses: 17. a. in the male. a. external rectal plexus internal rectal plexus prostatic plexus vesical plexus b. in the female. b. external rectal plexus internal rectal plexus vesical plexus vaginal plexus uterine plexus 18. In general, what is the lymphatic drainage of the pelvic viscera? 18. Lymph from the pelvic organs drains either to internal iliac nodes, to external iliac nodes, or to sacral nodes. Efferents from the external and internal iliac nodes and from sacral nodes drain to common iliac nodes. The common iliac nodes drain to lumbar nodes. Dissection 32, The Pelvis Page 6 19. What is the main importance of the prostatic venous plexus? 19. The prostatic venous plexus drains into the vesical plexus and from it into the internal iliac veins. The internal iliac veins also receive blood from the lateral sacral veins which communicate with the external and internal vertebral venous plexuses. Since none of these veins is valved, any increase in intraabdominal pressure can force blood from the pelvic veins into the vertebral venous plexus. Valsalva maneuvers associated with straining, coughing, etc., can cause the spread of prostatic tumor cells through the blood to the vertebral column, the brain, and elsewhere by this route. By this means metastatic tumors from the prostate can reach distant sites without passing through the lungs. 20. For the bladder: what is its base, its apex, its neck? 20. The bladder has four surfaces: a superior surface, two inferolateral surfaces, and a posterior surface. The posterior surface is the base of the bladder, and it is this surface that is in contact with the seminal vesicles. The apex is opposite the base and is at the point of attachment of the median umbilical ligament (urachus). The neck of the bladder is the inferior narrowed portion just above the opening of the urethra. What is the fundus of the bladder? The term fundus is sometimes applied to the base of the bladder. The two terms are synonymous. 21. Discuss the nerve supply to the bladder. 21. 22. Locate the cell bodies of nerve fibers which: 22. The pelvic splanchnic nerves supply afferent fibers and preganglionic efferent fibers to the bladder. Postganglionic neurons (terminal ganglia) are located in the bladder wall. Cell bodies of afferent fibers are located in the dorsal root ganglia of the midsacral (S2, S3, S4) nerves. a. innervate smooth muscle which contracts the bladder; a. Ganglia of the outer and submucous coats of the bladder (parasympathetic terminal ganglia). b. innervate blood vessels in the wall of the bladder; b. Ganglia of the pelvic portion of the sympathetic trunk (lateral ganglia) or sympathetic ganglia of the pelvic plexus (collateral ganglia). c. are activated by stretch of bladder muscle (detrusor) fibers; c. Dorsal root ganglia at S2, S3, and S4. d. initiate and interrupt micturition. d. Anterior gray column of the second, third, and fourth sacral segments of the spinal cord. Dissection 32, The Pelvis Page 7 23. What deleterious effect on body functions is produced by enlargement of the prostate? 23. Obstruction of the flow of urine from the bladder (urinary retention). 24. List the structures supporting the uterus. 24. The broad ligament, the cardinal ligaments, the uterosacral ligaments, and the round ligaments; probably the most important structure supporting the uterus, however, is the pelvic diaphragm. 25. Name the subdivisions of the uterine tube. 25. The fimbriated end, the infundibulum, the ampulla, the isthmus, and the intramural or uterine part. What prevents peritoneal fluid from leaking out the vaginal orifice? The walls of the cervix usually remain in close opposition as do the walls of the vagina, preventing the cavity of the uterus from "opening" directly to the outside; in addition, the volume of peritoneal fluid is usually very small. How can a physician determine if at least one tube is patent? Both tubes? 26. Trace lymphatic drainage from the uterus. Why is this important? By instilling a small amount of air into the uterus. The air will ascend through a patent uterine tube and escape into the peritoneal cavity to collect beneath the diaphragm. By radiographic demonstration of bilateral leakage into the peritoneal cavity of radio-opaque material placed in the cavity of the uterus. (G3.33B) 26. Most efferent vessels from the cervix and lower body end in nodes of the pelvis: internal iliac, external iliac; and sacral. Most efferent vessels from the fundus and upper body drain to nodes of the lumbar chain, although a few drain along the round ligament to end in superficial inguinal nodes. The pattern of lymphatic drainage of the uterus is important because of the prevalence of cancer of the uterus and because of the tendency of these cancers to spread by way of the lymphatics. Dissection 32, The Pelvis 27. What is a cystocele? Page 8 27. A bulging of the bladder into the anterior wall of the vagina (and sometimes out the vestibule!) What types of trauma produce this defect? This results from tearing of the connective tissue fibers of the anterior vaginal wall when the vagina is stretched during childbirth. What deleterious effects on body functions result from a cystocele? Distortion of the shape of the bladder allows the bladder sphincter to leak, especially under stress such as sneezing, etc.; this is called urinary incontinence. Another problem frequently associated with a cystocele is failure to empty the bladder, i.e. residual urine, which favors the development of infection. What is prolapse of the uterus? Relaxation of the supports of the uterus, allowing the organ to descend into the vagina; in severe cases the cervix may appear through the vestibule and become chronically inflamed. 28. In what clinical situations are the venous anastomoses around the rectum important? 28. In cases of portal hypertension the connections of the superior rectal veins may serve as an important communication of the portal with the caval system to relieve, somewhat, the portal hypertension. What is the route of lymphatic drainage from the rectum? From upper rectum to inferior mesenteric nodes; from middle and lower rectum to internal iliac nodes. Abnormality of what embryonic structure results in imperforate anus? Cloacal membrane At what time in development does this defect occur? 7 or 8 weeks 29. What is the neural hypogastric plexus (presacral nerve)? 29. Preganglionic and postganglionic sympathetic fibers, small sympathetic ganglia (collateral), and a few afferent fibers. What are the results of presacral neurectomy? Loss of ability by the male to ejaculate; possibly relief of pain in dysmenorrhea (female). What types of fibers are contained in the pelvic plexus? Preganglionic and postganglionic sympathetic fibers, preganglionic and postganglionic parasympathetic fibers, and afferent fibers. What results from interruption of the nervi erigentes (pelvic splanchnic nerves)? Loss of muscle tone in the wall of the bladder (atonic bladder) reduced peristalsis in the rectum, loss of sensation (pain, fullness) from pelvic organs, and, in the male, loss of the ability to produce an erection. Dissection 32, The Pelvis Page 9 30. What is the relation of the ovarian artery to the ureter at the pelvic brim? 30. The artery is lateral to the ureter. 31. What remains of the umbilical artery after birth? 31. It remains patent as far as the superior vesical artery and becomes the medial umbilical ligament distal to this. 32. Where is the vagina in relation to the peritoneum? 32. Posterior fornix 33. What are the subdivisions of the broad ligament? 33. The mesovarium extending between the ovary and the major part of the broad ligament, the mesosalpinx between the attachment of the mesovarium and the uterine tube, and the mesometrium below the attachment of the mesovarium. LJ:bh revised 06/19/09