Assessment of the Role of Interstitial Glucagon in the
advertisement

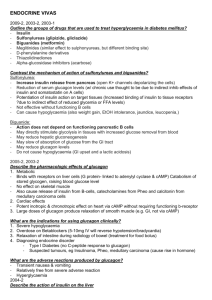
Assessment of the Role of Interstitial Glucagon in the Acute Glucose Secretory Responsiveness of In Situ Pancreatic -Cells Karen Moens,1 Veerle Berger,1 Jung-Mo Ahn,2 Chris Van Schravendijk,1 Victor J. Hruby,2 Daniel Pipeleers,1 and Frans Schuit1 Glucagon is a potent stimulator of insulin release in the presence of a permissive glucose concentration, activating -cells in vitro via both glucagon- and glucagon-like peptide-1 (GLP-1)–receptors. It is still unclear whether locally released glucagon amplifies the secretory responsiveness of neighboring -cells in the intact pancreas. The present study investigates this question in the perfused pancreas by examining the effects of antagonists for glucagon receptors ([des-His1,des-Phe6,Glu9]glucagon-NH2, 10 mol/l) and GLP-1–receptors [exendin-(9-39)-NH2, 1 mol/l] on the insulin secretory response to glucose. The specificity of both antagonists was demonstrated by their selective interaction with glucagon-receptor signaling in rat hepatocytes and GLP-1–receptor signaling in Chinese hamster lung (CHL) fibroblasts. In purified rat -cells, the glucagon-receptor antagonist (10 mol/l) inhibited the effect of 1 nmol/l glucagon upon glucose-induced insulin release by 78 ⴞ 6%. In the perfused rat pancreas, neither of these antagonists inhibited the potent secretory response to 20 mmol/l glucose, although they effectively suppressed the potentiating effect of, respectively, an infusion of glucagon (1 nmol/l) or GLP-1 (1 nmol/l) on insulin release. When endogenous glucagon release was enhanced by isoproterenol (100 nmol/l), no amplification was seen in the simultaneous or subsequent insulin secretory response to glucose. It is concluded that, at least under the present selected conditions, the glucose-induced insulin release by the perfused rat pancreas seems to occur independent of an amplifying glucagon signal from neighboring ␣-cells. Diabetes 51:669 – 675, 2002 W e have previously reported that the potent insulin secretory response to glucose is markedly diminished when pancreatic -cells are isolated from the islet structure. A number of previous in vitro observations using isolated islets or purified islet cells have supported the idea that the amplitude of glucose stimulation of insulin release is strongly influenced by the intracellular cAMP level, which From the 1Diabetes Research Center, Vrije Universiteit Brussel, Brussels, Belgium; and the 2Department of Chemistry, University of Arizona, Tucson, Arizona. Address correspondence and reprint requests to Dr. Frans Schuit, Molecular Pharmacology Unit, Diabetes Research Center, Faculty of Medicine, Vrije Universiteit Brussel, Laarbeeklaan 103, B-1090 Brussels, Belgium. E-mail: fschuit@minf.vub.ac.be. Received for publication 10 July 2001 and accepted in revised form 26 November 2001. AUC, area under the curve; CHL, Chinese hamster lung; GLP-1, glucagonlike peptide-1; IBMX, 3-isobutyl-1-methylxanthine; RIA, radioimmunoassay. DIABETES, VOL. 51, MARCH 2002 is regulated by various hormones and neurotransmitters (1–5). It remained unclear, however, which agents provide the amplifying cAMP signals in physiological conditions (6). There is sufficient evidence for a major role of glucagon in isolated islet preparations (1–3,7), which can potentiate glucose-induced insulin release via two different receptors (8). In vitro studies have indicated that separation of -cells from ␣-cells explains in part the lower secretory activity of purified -cells as compared with isolated islets (1,2). Locally released glucagon was indeed found to amplify glucose-induced insulin release in isolated islet cell preparations (1,7,8). This also explains the higher secretory responsiveness of ␣-cell– containing islets isolated from the dorsal pancreatic lobe when compared with that of ␣-cell poor islets from the ventral lobe (5,9). It is conceivable that circulating glucagon levels influence the cAMP levels in -cells in vivo. Other peptides, in particular glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic polypeptide, are likely candidates to contribute in this regulatory pathway through variations in their circulatory concentrations (3,10). In addition to this endocrine pathway, peptides such as glucagon may act via interstitial interactions. It is not yet possible to investigate such influences in the endocrine pancreas in vivo. Experiments have been undertaken in the isolated perfused pancreas to examine the possible role of ␣-cells on neighboring -cells. These studies have indicated that islet blood flows in the direction from the -cell core toward the non–-cell mantle (11,12). However, none of these data could provide final conclusions concerning interstitial glucagon interacting at sites where both ␣- and -cells are in close contact. As was suggested 10 years ago, specific glucagon-receptor antagonists would be required to assess the contribution of glucagon in the -cell response to glucose (13). Such antagonists would have the advantage over the previously used antibodies to glucagon in that they can penetrate into the interstitial space (14,15). In the present work, we examined the effect of a glucagon-receptor antagonist, [des-His1,des-Phe6,Glu9]glucagon-NH2 (16), to assess the role of interstitial glucagon in the acute responsiveness to glucose of in situ pancreatic -cells in the glucagon-rich dorsal part of the rat pancreas. Because high nanomolar glucagon concentrations were reported to activate GLP-1 receptors on -cells (8), we also used a GLP-1–receptor antagonist, exendin-(9-39)-NH2 (17). Our 669 INTERSTITIAL GLUCAGON AND THE SECRETORY STATE OF IN SITU -CELLS data show that, at least in the condition of rat pancreas perfusion, there is little or no contribution of locally secreted glucagon to the acute secretory response of islet -cells to glucose. RESEARCH DESIGN AND METHODS Materials. The glucagon-receptor antagonist [des-His1,des-Phe6,Glu9] glucagon-NH2 was prepared as described previously (16,18). Synthetic glucagon was purchased from Penninsula Laboratories Europe (Merseyside, U.K.). Dextran T70 was from Amersham Pharmacia Biotech AB (Uppsala, Sweden); HEPES was from Gibco BRL (Gaithersburg, MD); 3-isobutyl-1-methylxanthine (IBMX) was from Aldrich (Janssen Chimica, Beerse, Belgium), and BSA was from Roche Diagnostics (Mannheim, Germany). Exendin-(9-39)-NH2 was provided by Dr. J. Vandekerckhove (Department of Physiological Chemistry, State University of Ghent, Belgium). All other products were analytical grade and obtained from either Merck (Darmstadt, Germany) or Sigma (St. Louis, MO). All studies involving animals were carried out according to the Belgium regulation of animal welfare and after approval by the institution’s commission for animal experiments. Cells and cell culture. Rat hepatocytes were isolated from adult male Sprague-Dawley rats (200 –250 g) as described previously (19). Chinese hamster lung (CHL) fibroblasts stably transfected with the rat GLP-1 receptor cDNA (donated by Dr. B. Thorens, Department of Pharmacology and Toxicology, University of Lausanne, Switzerland [20]) were cultured in Dulbecco’s modified Eagle’s medium (Gibco BRL) with 10% FCS (Gibco BRL), 2 mmol/l glutamine, 25 mmol/l glucose, 100 mg/l streptomycin, 60 mg/l penicillin, and 500 mg/ml geneticin (Gibco BRL). Measurement of cAMP production in hepatocytes and transfected CHL cells. In rat hepatocytes, cAMP levels were measured as described previously (8). Cells (5 ⫻ 104 cells/condition) were incubated for 15 min at 37°C in Earle’s HEPES medium supplemented with 5 mmol/l glucose, 0.5% BSA, 250 mol/l IBMX, and different peptide hormones at the indicated concentrations. Cellular cAMP content was measured using a commercially available [125I]cAMP radioimmunoassay (RIA) kit (Amersham, Buckinghamshire, U.K.). Transfected CHL cells were grown in 24-well plates (2 ⫻ 104 cells/ condition) until 80% confluence (⬃24 h) in 1 ml of culture medium. Cells were washed three times with Earle’s HEPES containing 25 mmol/l glucose and 0.5% BSA and then incubated in a Steri-cult 200 incubator (Forma Scientific, Parker, CO) for 15 min at 37°C in 1 ml of this medium, supplemented with 250 mol/l IBMX, glucagon, and GLP-1, with or without receptor antagonists. After 15 min, the medium was aspirated, 500 l of trichloroacetic acid (8% [wt/vol] in water) was added, and each cup was sonicated. Of this sonicated sample, 400 l was collected in 5-ml plastic tubes (Falcon, Oxnard, CA) and centrifuged at 2000g for 15 min. The soluble fraction was extracted three times with 4 ml of water-saturated ether, lyophilized, redissolved in sodium acetate buffer (0.05 mol/l, pH 5.8), and assayed for cAMP content. Results were expressed as femtomoles per 103 initial cells at the beginning of cell culture. Pancreas perfusion. Insulin secretion by in situ -cells was investigated using the isolated perfused rat pancreas model (21). Male Wistar rats (250 –350 g) were anesthetized with 60 mg/kg Nembutal (Sanofi Santé Animale, Libourne Cedex, France). To ensure perfusion of only the dorsal part of the pancreas, we inserted a catheter (24 G; Neoflon, Ohmeda, Sweden) immediately into the celiac artery. The perfusate was collected via a 22-G Surflo intravenous catheter (Terumo Europe NV, Leuven, Belgium) inserted and tied into the portal vein. Anoxia time was kept to a minimum and was always ⬍3 min. The pancreas preparation was placed on a heated, moist surface (surrounded by basal medium) and covered with Parafilm M (American National Can Company, Chicago, IL), and the temperature was kept constant at 37°C. Flow rate was constant throughout the perfusion experiment (2.5 ml/min); perfusions in which flow rates dropped below 2.5 ml/min before the end of the experiment were excluded. The perfusion medium consisted of Earle’s HEPES buffer (pH 7.35) (22) continuously gassed with 95% O2/5% CO2, supplemented with 0.2% charcoal-treated BSA, 4% dextran T-70, and 1.4 mmol/l glucose (basal medium). At the time points indicated in the figures, 20 mmol/l glucose or glucose⫹peptides (glucagon/GLP-1 and/or receptor antagonists) was added to the medium. Perfusions were started with a 20-min/ equilibration period, followed by the experimental conditions, and ended with neutral red perfusion to control the completeness of tissue perfusion. The perfusate was collected every minute and analyzed for insulin and glucagon content using RIAs (1,23), the detection limits being 20 pg and 4 pg, respectively. To minimize degradation of peptides, fractions were collected in 50 l of 7.5% precooled EDTA and immediately kept on ice. Data were expressed as nanograms of hormone released per minute, taking into account the dead space of perfusion, i.e., the time for neutral red to stain the pancreas 670 (1 min). Areas under the curve (AUC) in response to 20 mmol/l glucose stimulations (min 11–20, 36 – 45, and 61–70), with or without GLP-1/glucagon receptor agonists/antagonists (AUC1, AUC2, and AUC3) or 100 nmol/l isoproterenol subtraction were calculated after basal insulin release at 1.4 mmol/l glucose. To adjust for the differences of the first glucose stimulation between different experiments, we expressed AUC2 and AUC3 as a percentage of AUC1. The potentiating effect of glucagon and GLP-1 and the effects of receptor antagonists were subsequently calculated by subtracting the response to glucose alone from the corresponding peak, in this way taking into account the memory effect of glucose alone. Statistical analysis. Data are expressed as mean values ⫾ SD of n independent experiments in the table and the text and as mean values ⫾ SE in the figures. Significance of differences between experimental conditions was assessed by the two-tailed Student’s t tests. In the pancreas perfusions, the magnitude of the secretory response after the first glucose stimulation (AUC1) was normally distributed for the 36 tested pancreata in our study (data not shown), validating the use of Student’s t tests for further analysis. RESULTS Characterization of the glucagon receptor antagonist [des-His1,des-Phe6,Glu9]glucagon-NH2. The specificity and potency of [des-His1,des-Phe6,Glu9]glucagon-NH2 as a glucagon receptor antagonist was tested on primary rat hepatocytes, a well-characterized reference system for glucagon receptor signaling (24), and on CHL cells stably transfected with the rat GLP-1–receptor gene (20). Significant antagonism of 1 nmol/l glucagon-induced cAMP production in hepatocytes was noted between 0.3 mol/l peptide (17 ⫾ 5% inhibition; P ⬍ 0.005) and 10 mol/l (80% inhibition; P ⬍ 0.001). At 10 mol/l [des-His1,des-Phe6,Glu9] glucagon-NH2, antagonism was almost complete at 0.1 nmol/l glucagon (97 ⫾ 1% inhibition; P ⬍ 0.005) but became nonsignificant at 10 nmol/l glucagon. The overall effect was a shift of the concentration response curve to the right (Fig. 1A), resulting in higher apparent EC50 for glucagon (12 ⫾ 4 nmol/l) than in control cells (EC50 ⫽ 0.9 ⫾ 0.4 nmol/l; P ⬍ 0.05). We previously reported that 1 mol/l exendin-(9-39)-NH2 had no effect on glucagoninduced cAMP production by rat hepatocytes (8). In CHL cells expressing rat GLP-1 receptors, cAMP content was elevated 4.5 ⫾ 0.3 times by 1 nmol/l glucagon (Fig. 1B), confirming the observation (8) that glucagon can activate GLP-1 receptors. Because these cells do not express glucagon receptors, no inhibition of glucagoninduced cAMP production was observed with 10 mol/l [des-His1,des-Phe6,Glu9]glucagon-NH2, whereas 1 mol/l exendin-(9-39)-NH2 could inhibit this effect by 99 ⫾ 2%. Likewise, 10 pmol/l GLP-1–induced cAMP production was decreased by exendin-(9-39)-NH2, with 90 ⫾ 4% (stimulation above basal cAMP production: 285 ⫾ 87 vs. 28 ⫾ 18 fmol 䡠 103 initial cells⫺1 䡠 15 min⫺1 in the absence or presence, respectively, of 1 mol/l exendin-(9-39)-NH2; n ⫽ 4; P ⬍ 0.01), whereas 10 mol/l [des-His1,desPhe6,Glu9]glucagon-NH2 had no effect (312 ⫾ 113 fmol 䡠 103 initial cells⫺1 䡠 15 min⫺1 in the presence of [desHis1,des-Phe6,Glu9]glucagon-NH2; n ⫽ 4; not significant). The effect of [des-His1,des-Phe6,Glu9]glucagon-NH2 was subsequently tested in fluorescence-activated cell sorter– purified -cells (expressing both glucagon- and GLP-1receptors [8]), which were perifused with 20 mmol/l glucose together with 1 nmol/l glucagon. This glucagon concentration was chosen because 1) it has previously been shown to potentiate significantly glucose-induced insulin release in -cells (1,8) and 2) 10 mol/l [desHis1,des-Phe6,Glu9]glucagon-NH2 could inhibit its stimulaDIABETES, VOL. 51, MARCH 2002 K. MOENS AND ASSOCIATES FIG. 1. Effect of [des-His1,des-Phe6,Glu9]Glucagon-NH2 and exendin-(9-39)-NH2 on glucagon-induced cAMP production. Glucagon-induced cAMP production in rat hepatocytes (A) or CHL cells transfected (20) with rat GLP-1 receptor cDNA (B), either in the absence of antagonists (E) or in the presence of 10 mol/l [des-His1,des-Phe6,Glu9]Glucagon-NH2 (f) or 1 mol/l exendin-(9-39)-NH2 (F) (B only). cAMP production was measured after 15 min of incubation in buffer containing 250 mol/l IBMX. Data are means ⴞ SE of four (A) or three (B) independent experiments. tory effect on cAMP production in rat hepatocytes by 80% (Fig. 1B). Administration of 10 mol/l [des-His1,desPhe6,Glu9]glucagon-NH2 counteracted the potentiating effect of 1 nmol/l glucagon on 20 mmol/l glucose-induced insulin secretion from perifused cells by 78 ⫾ 6% (glucagon-stimulated insulin release, without versus with antagonist: 476 ⫾ 218 vs. 110 ⫾ 69 pg 䡠 103 cells⫺1; n ⫽ 4; P ⬍ 0.02). As shown previously (8), this glucagon concentration was not affected by 1 mol/l exendin-(9-39)-NH2, whereas on the contrary, exendin-(9-39)-NH2 could inhibit the potentiating effect of 10 nmol/l glucagon by ⬎40% (8). Effect of [des-His1,des-Phe6,Glu9]glucagon-NH2 or exendin-(9-39)-NH2 on glucose-induced insulin release. Having characterized the molecular tools to block glucagon activation of glucagon- and GLP-1–receptors on -cells, we next assessed their effect on glucose-induced insulin release from the isolated perfused rat pancreas. As expected (25), 20 mmol/l glucose stimulation resulted in biphasic insulin secretory response (Fig. 2A), with a rapid return to basal values when glucose was lowered to 1.4 mmol/l. Using a protocol with three successive 10-min glucose stimulation periods alternated by 15-min intervals of basal glucose (Fig. 2), we observed that the second glucose stimulation resulted in a 1.5 ⫾ 0.2-fold larger insulin secretory response than the first stimulation (AUC1 561 ⫾ 191 ng vs. AUC2 819 ⫾ 275 ng; n ⫽ 4; P ⬍ 0.02). As is shown in Fig. 2A, the mean secretory response to the third glucose stimulation was again 30% higher than the second (AUC3 1,044 ⫾ 395 ng; P ⬍ 0.05). These results are compatible with a glucose memory effect described by Grill et al. (26,27). The potent insulin secretory response to glucose— on average 55 ⫾ 18 ng/min for the first glucose stimulation, 80 ⫾ 27 ng/min for the second, and 102 ⫾ 39 ng/min for the third— occurred in the presence of an undetectable pancreatic glucagon output before or during the 20 mmol/l glucose stimulation (⬍6 pmol/l). To investigate whether locally released glucagon may have influenced the observed secretory responsiveness, we added a second series of perfusions, the glucagon receptor antagDIABETES, VOL. 51, MARCH 2002 onist [des-His1,des-Phe6,Glu9]glucagon-NH2 (10 mol/l) to the perfusion medium 15 min before and until the end of the second period of glucose stimulation. This addition had no effect on the time kinetics and magnitude of glucose-stimulated insulin release (Fig. 2B) because AUC2 was again 1.3 ⫾ 0.2-fold higher (905 ⫾ 166 ng) than the AUC1 caused by the first stimulation (682 ⫾ 75 ng; P ⫽ 0.05). Furthermore, as in the control experiment, the third glucose stimulation, performed in the absence of the glucagon-receptor antagonist, resulted in 1.4 ⫾ 0.3-fold higher release (AUC3 1,290 ⫾ 319 ng) than the second glucose stimulation (mean ⫾ SD, n ⫽ 4; P ⫽ 0.056). The absence of an antagonizing effect of [des-His1,desPhe6,Glu9]glucagon-NH2 might be attributable to the presence of local glucagon levels above 10 nmol/l, in which range the antagonist was found to be ineffective. However, such local levels should have been detected in the effluent. Furthermore, at such high concentrations, glucagon is known to activate -cells via GLP-1 receptors (8), which would have resulted in exendin-(9-39)-NH2 antagonizing such effects, and this was not the case (Fig. 2C). Therefore, neither the presence of the glucagon-receptor antagonist [des-His1,des-Phe6,Glu9]glucagon-NH2 nor that of the GLP-1 receptor antagonist exendin-(9-39)-NH2 could affect the amplitude and time kinetics of glucose-induced insulin secretory response from the perfused glucagon-rich lobe of the rat pancreas. This could mean either that these antagonists do not block their respective receptors on -cells because they are degraded before binding occurs or that occupancy of glucagon- and/or GLP-1–receptors with endogenous glucagon is very low in the studied conditions. Effect of [des-His1,des-Phe6,Glu9]glucagon-NH2 and exendin-(9-39)-NH2 on glucagon and GLP-1 potentiation of glucose-induced insulin release. To exclude the possibility of antagonist degradation in the chosen experimental conditions (Fig. 2), we added in a new series of experiments with exogenous glucagon or GLP-1 in the presence or absence of antagonist (Table 1). Glucagon (1 671 INTERSTITIAL GLUCAGON AND THE SECRETORY STATE OF IN SITU -CELLS FIG. 2. Effect of [des-His1,des-Phe6,Glu9]glucagon-NH2 and exendin-(939)-NH2 on glucose-induced insulin secretion from the perfused pancreas. Changes in the glucose concentration of the perfusion medium are indicated in the top of each panel. A: Control pancreata stimulated three times with 20 mmol/l glucose. The receptor antagonists [desHis1,des-Phe6,Glu9]glucagon-NH2 (desHisdesPhe; B) and exendin-(939)-NH2 (Exendin; C) were added 15 min before and during the second glucose stimulation, as indicated by the bold line. Insulin secretion in response to 1.4 mmol/l glucose was below the detection limit of the RIA assay (20 pg). Data represent means ⴞ SE of four independent experiments. nmol/l) potentiated the second glucose stimulation more than twofold (AUC2 as % of AUC1: 1 nmol/l glucagon 300 ⫾ 4, n ⫽ 12, vs. control 146 ⫾ 16, n ⫽ 4; P ⬍ 0.001). Taking into account the memory effect of glucose alone, a second combined glucagon/glucose stimulation resulted in a 57% larger insulin output than the first glucagon/glucose stimulation (AUC3 as % of AUC1: 1 nmol/l glucagon 427 ⫾ 65, n ⫽ 4, vs. control 185 ⫾ 14, n ⫽ 4; P ⬍ 0.01). Presence of the glucagon-receptor antagonist [des-His1,des-Phe6,Glu9] glucagon-NH2 prevented 81 ⫾ 10% of this potentiating effect of glucagon on insulin release during the third stimulation with glucose (AUC3 as % of AUC1: 230 ⫾ 21 in the presence vs. 427 ⫾ 65 in the absence of antagonist, n ⫽ 4; P ⬍ 0.002). In contrast, we observed no antagonism of the glucagon-potentiation of glucose-induced insulin release using 1 mol/l exendin-(9-39)-NH2 (AUC3 as % of 672 AUC1: 389 ⫾ 61 in the presence vs. 427 ⫾ 65 in the absence of antagonist, n ⫽ 4; not significant). As expected (28), 1 nmol/l GLP-1 potentiated glucose-induced insulin release more than threefold (AUC2 as % of AUC1: 1 nmol/l GLP-1 500 ⫾ 66 ng, n ⫽ 8, vs. control 146 ⫾ 16, n ⫽ 4; P ⬍ 0.001). Similar to the gain in secretory response after repeated glucagon/glucose stimulation, the second GLP-1/glucose exposure of the pancreas resulted in a 58% more efficient amplification of the glucose-induced insulin release (AUC3 as % of AUC1: 1 nmol/l GLP-1 742 ⫾ 94, n ⫽ 4, vs. control 185 ⫾ 14, n ⫽ 4) than the first GLP-1 addition (P ⬍ 0.002). This second GLP-1 stimulation was antagonized by 89 ⫾ 9% (P ⬍ 0.0001) by simultaneous perfusion with exendin(9-39)-NH2. Therefore, the present data indicate that both [des-His1,des-Phe6,Glu9]glucagon-NH2 and exendin-(9-39)NH2 effectively antagonize the effect of, respectively, glucagon on glucagon receptors and GLP-1 on GLP-1– receptors. Together with the data in Fig. 2, these results suggest that the glucose-induced insulin release from the perfused pancreas can occur in the absence of significant activity of occupied glucagon- and/or GLP-1–receptors. Effect of ␣-cell stimulation on glucose-induced insulin release. To investigate the possible contribution of local glucagon to glucose-induced insulin secretion in a condition of elevated glucagon release, we performed a perfusion experiment in which the second glucose stimulation and the 15 min preceding this period were supplemented with 100 nmol/l isoproterenol (Fig. 3). This -adrenergic agonist has been shown to stimulate directly the glucagon release from rat ␣-cells, without affecting insulin secretion from -cells (4). Furthermore, in contrast to the effects observed in humans whereby the potentiation of glucose-induced insulin release by isoproterenol is strong (29), interaction between isoproterenol and glucose at the level of insulin release has been reported to be weak and both stimulatory and inhibitory in the rat perfused pancreas (30,31). As could be expected (4,32), perfusion with 100 nmol/l isoproterenol induced a strong glucagon secretory response at 1.4 mmol/l glucose, with a maximal release of 0.24 ng/min that was at least fivefold above basal and returned to levels below the detection limit at 40 min (Fig. 3). This resulted in an AUC of 1.7 ⫾ 0.4 ng glucagon and no detectable insulin during the 15-min perfusion with 1.4 mmol/l glucose and 100 nmol/l isoproterenol. Despite this previous elevated glucagon secretion, glucoseinduced insulin secretion was not augmented as compared with the control experiment without isoproterenol (AUC2 ⫽ 148 ⫾ 18% of AUC1 in the presence vs. 146 ⫾ 16% in the absence of isoproterenol, n ⫽ 4; not significant). Furthermore, glucagon remained elevated for 3 min more during the 20 mmol/l glucose stimulation, resulting in an average glucagon level of 0.09 ⫾ 0.02 ng/min (10 pmol/l). Because locally secreted glucagon is diluted into the islet blood flow, which represents in itself only 10% of the total pancreatic blood flow (33), we can assume that locally these glucagon concentrations may rise up to at least 100 pmol/l. We have previously shown that such glucagon concentration can significantly potentiate glucose-induced insulin secretion (1). However, during this period of elevated pancreatic glucagon output (min 37–39) (Fig. 3), glucose-induced insulin secretion was not significantly altered. In isoproterenol-stimulated pancreata, insulin reDIABETES, VOL. 51, MARCH 2002 K. MOENS AND ASSOCIATES TABLE 1 Glucagon and GLP-1 potentiation of 20 mmol/l glucose-induced insulin release from the isolated perfused rat pancreas: effect of the receptor antagonists [des-His1,des-Phe6,Glu9]glucagon-NH2 and exendin-(9-39)-NH2 Condition Released insulin (AUC) % of stimulation 1 (min 11–20) Stimulation 2 Stimulation 3 (min 36–45) (min 61–70) Control Glucagon (1 nmol/l) Glucagon (1 nmol/l) ⫹ [des-His1,des-Phe6,Glu9]Glucagon-NH2 (10 mol/l) Glucagon (1 nmol/l) ⫹ exendin-(9-39)-NH2 (1 mol/l) GLP-1 (1 nmol/l) GLP-1 (1 nmol/l) ⫹ exendin-(9-39)-NH2 (1 mol/l) 146 ⫾ 16 (4) 300 ⫾ 46 (12) NT NT 500 ⫾ 66 (8) NT 185 ⫾ 14 (4) 427 ⫾ 65 (4) 230 ⫾ 21 (4)* 389 ⫾ 61 (4) NS 742 ⫾ 94 (4) 242 ⫾ 44 (4)† Data represent the means ⫾ SD of insulin released (AUC after glucose stimulation 2 [min 36 – 45] or 3 [min 61–70] and expressed as % of AUC after glucose stimulation 1 [min 11–20]) from (n) individual pancreata. Statistical significance of difference between absence or presence of antagonists versus control (stimulation 2), glucagon, or GLP-1 (stimulation 3) was calculated via the two-tailed Student’s t test. *P ⬍ 0.02; †P ⬍ 0.001. NS, not significant; NT, not tested. lease during this period (298 ⫾ 115 ng) was 1.5 ⫾ 0.1-fold higher than release during the comparable period of the first glucose stimulation (193 ⫾ 76 ng). This memory effect was similar to control pancreata (Fig. 2A), from which release during min 37–39 (224 ⫾ 103 ng) was 1.4 ⫾ 0.3-fold higher than that observed during the first 3 min of the first glucose stimulation (158 ⫾ 59 ng). Together, our results indicate that an episode of stimulated glucagon release, before or during glucose stimulation, does not potentiate the insulin response from the pancreas, further supporting the idea that locally secreted glucagon may not play a role in the responsiveness of pancreatic -cells to glucose through interstitial interactions. DISCUSSION In rats and mice, -cells are located in the islet center, whereas the non–-cells are situated in the islet mantle (34). For the dorsal rat pancreas, which contains most glucagon cells of the gland, this means that the -cell core of the islet is surrounded by a mantle of glucagon-secreting and somatostatin-secreting cells (9,35). Because both glucagon and somatostatin exert powerful effects on the glucose response of isolated rat -cells (1,36), the possibility was proposed that local (paracrine) interactions of glucagon and somatostatin with islet -cells modulate the secretory response of the pancreas to elevated glucose (37). The data in the present study suggest that the strong insulin secretory response to glucose of the isolated perfused pancreas can occur in the absence of interstitial influences by locally secreted glucagon. A potent insulin secretory response of -cells to glucose was demonstrated in the isolated rat perfused pancreas in a condition of glucagon levels ⬍6 pmol/l in the pancreatic effluent. However, locally secreted glucagon is diluted first in the islet blood circulation and subsequently in the total pancreatic blood circulation. Furthermore, in vivo normal blood glucagon levels are reported to be between 1 and 100 pmol/l (38 – 40), whereas 1 pmol/l glucagon is enough to stimulate significantly insulin secretion from the perfused rat pancreas (41). The use of a specific glucagonand GLP-1–receptor antagonist, [des-His1,des-Phe6,Glu9] glucagon-NH2 and exendin-(9-39)-NH2 respectively, allowed us to assess interstitial influences of locally secreted glucagon, because these antagonists can enter the interstitial space (14,15). We demonstrate here that [des-His1,des-Phe6,Glu9] glucagon-NH2 inhibits specifically glucagon receptors, blocking 80% of 1 nmol/l glucagon activation of hepatocytes, and that it does not interfere with GLP-1–receptor activation by either glucagon or GLP-1. We acknowledge the problem of low potency of [des-His1,des-Phe6,Glu9] FIG. 3. Effect of isoproterenol on glucagon secretion and subsequent glucose-induced insulin secretion from the perfused pancreas. Insulin (E) and glucagon (F) secretion were assessed as outlined in RESEARCH DESIGN AND METHODS. Changes in the perfusion medium are indicated in the top. The -adrenergic agonist isoproterenol (100 nmol/l) was added 15 min before and during the second glucose stimulation, as indicated by the bold line. Insulin secretion in response to 1.4 mmol/l glucose was below the detection limit of the RIA assay (20 pg); glucagon secretion values below the detection limit of the RIA assay (4 pg) are not shown. Data represent the means ⴞ SE of four independent experiments. DIABETES, VOL. 51, MARCH 2002 673 INTERSTITIAL GLUCAGON AND THE SECRETORY STATE OF IN SITU -CELLS glucagon-NH2 for the glucagon receptors. In a concentration-response experiment performed with hepatocytes (data not shown), we observed concentration-dependent effects of the antagonist on 1 nmol/l glucagon-induced cAMP production. Because of solubility and pH effects on the buffers, we could not use concentrations ⬎10 mol/l. This concentration could significantly antagonize glucagon concentrations up to 1 nmol/l in hepatocytes (Fig. 1A). However, if higher glucagon levels exist locally, it could be expected that, in addition to glucagon receptors, GLP-1 receptors will be activated (8). Therefore, 1 mol/l exendin-(9-39)-NH2 was used in parallel (Fig. 2C). Because glucagon amplifies 20 mmol/l glucose-induced insulin release (1,8), perfusion of the pancreas with either [desHis1,des-Phe6,Glu9]glucagon-NH2 or exendin-(9-39)-NH2 should result in a lower glucose-induced insulin secretory response than in the control pancreas on the condition that local glucagon can activate -cells. That we did not observe any inhibition of the pancreatic glucose-induced insulin response by either antagonist indicates that if glucagon interacts with -cells, then it occurs after dilution in the general circulation (42,43), i.e., after at least one passage through the liver. Therefore, the lack of measurable glucagon levels in the pancreatic effluent may be explained by an extremely low glucagon secretion in the present experimental conditions. The observed effect of 1 nmol/l exogenous glucagon on insulin release (Table 1) further supports the absence of high glucagon concentrations influencing neighboring -cells. This argument was already used by Kawai et al. (42). It is unlikely that our negative results were caused by antagonist degradation before binding on their respective receptors. First, high concentrations were used, so degradation would have been extremely rapid. Second, [des-His1,des-Phe6,Glu9] glucagon-NH2 and exendin-(9-39)-NH2 could block ⬎80% of the insulin-stimulating effect of, respectively, 1 nmol/l glucagon and GLP-1 that was added to the perfusion medium. Positive controls for the action of these antagonists in the perfused pancreas were therefore obtained. The same degree of inhibition was also observed with hepatocytes stimulated with 1 nmol/l glucagon (Fig. 1A), further supporting the idea that in the present model the used exogenous glucagon is not diluted extensively by endogenous glucagon. The low rates of glucagon release under the chosen experimental conditions are a limitation of the present experimental system. We therefore induced glucagon release with the -adrenergic agonist isoproterenol, a condition that is known to stimulate ␣-cells (4,32), while at the same time this agonist is not expected to stimulate -cells directly (4). We observed that this condition did not potentiate the insulin secretory response of pancreatic -cells to 20 mmol/l glucose, despite a clearly elevated rate of glucagon release before and during the first minutes of glucose stimulation. These observations further support the idea that the secretory response of the intact pancreas is not dependent on locally released glucagon. It is extremely difficult to rule out the possibility that tight junctions between neighboring cells seal off intercellular compartments where locally released glucagon is allowed to interact with receptors on -cells. Considering our data (Fig. 3), the release of such glucagon pools should not be 674 isoproterenol-sensitive, which is very unlikely. It can thus be proposed that under the present conditions, local release of glucagon has no major effect on the magnitude of glucose-induced insulin release from the isolated rat pancreas. Extrapolation of these observations to in vivo conditions will require appropriate models to measure glucagon levels within the interstitial space, where it can potentiate insulin secretion. In summary, our data demonstrate that the potent glucose-induced insulin release from the isolated perfused rat pancreas is not dependent on the priming effect of locally released glucagon, at least under the chosen experimental conditions. This both supports the view that islet blood flow direction is not from ␣- to -cells (11) and indicates that glucagon in the islet interstitium is not in contact with glucagon- and GLP-1–receptors on -cells. If the present observations on isolated rat pancreas (where no evidence for interstitial glucagon is found) can be extrapolated to human pancreas, then these data can be relevant for the clinical development of glucagon-receptor antagonists (16), which aim to suppress glucagon-stimulated liver metabolism rather than glucose-induced insulin secretion. ACKNOWLEDGMENTS The work in this article has been supported by grants G.3127.93 and G.0376.97 from the Flemish Fund for Scientific Research (FWO Vlaanderen), the Ministerie van de Vlaamse Gemeenschap, departement Onderwijs (Geconcerteerde Onderzoeksactie 1807), the Services of the Belgian Prime Minister (Interuniversity Attraction Pole P4/ 21), and the U.S. Public Health Service (Grant DK-21085). We thank Dr. V. Rogiers, Sonia Beken, and Karen De Smet for isolating rat hepatocytes; Dr. B. Thorens (Institut de Pharmacologie, Université de Lausanne, Switzerland) for kindly donating CHL cells transfected with the GLP-1 receptor; and Dr. J. Vandekerckhove (Department of Physiological Chemistry, State University of Ghent, Belgium) for providing synthetic exendin-(9-39)-NH2. Dr. L. Kaufman is acknowledged for statistical advice. REFERENCES 1. Pipeleers DG, Schuit FC, in’t Veld P, Maes E, Hooghe-Peters EL, Van De Winkel M, Gepts W: Interplay of nutrients and hormones in the regulation of insulin release. Endocrinology 117:824 – 833, 1985 2. Schuit FC, Pipeleers DG: Regulation of adenosine 3⬘,5⬘-monophosphate levels in the pancreatic B cell. Endocrinology 117:834 – 840, 1985 3. Moens K, Heimberg H, Flamez D, Huypens P, Quartier E, Ling Z, Pipeleers D, Gremlich S, Thorens B, Schuit F: Expression and functional activity of glucagon, glucagon-like peptide I, and glucose-dependent insulinotropic peptide receptors in rat pancreatic islet cell. Diabetes 45:257–261, 1996 4. Schuit FC, Pipeleers DG: Differences in adrenergic recognition by pancreatic A and B cells. Science 232:875– 877, 1986 5. Trimble ER, Halban PA, Wollheim CB, Renold AE: Functional differences between rat islets of ventral and dorsal pancreatic origin. J Clin Invest 69:405– 413, 1982 6. Pipeleers D: Purified islet cells in diabetes research. Horm Res 23:225–234, 1986 7. Huypens P, Ling Z, Pipeleers D, Schuit, F: Glucagon receptors on human islet cells contribute to glucose competence of insulin release. Diabetologia 43:1012–1019, 2000 8. Moens K, Flamez D, Van Schravendijk C, Ling Z, Pipeleers D, Schuit F: Dual glucagon recognition by pancreatic -cells via glucagon and glucagon-like peptide 1 receptors. Diabetes 47:66 –72, 1998 9. Baetens D, Malaisse-Lagae F, Perrelet A, Orci L: Endocrine pancreas: three-dimensional reconstruction shows two types of islets of Langerhans. Science 206:1323–1324, 1979 DIABETES, VOL. 51, MARCH 2002 K. MOENS AND ASSOCIATES 10. Creutzfeldt W: The incretin concept today. Diabetologia 16:75– 85, 1979 11. Bonner-Weir S, Orci L: New perspectives on the microvasculature of the islets of Langerhans in the rat. Diabetes 31:883– 889, 1982 12. Samols E, Stagner JI: Intra-islet regulation. Am J Med 85:31–35, 1988 13. Weir GC, Bonner-Weir S: Islets of Langerhans: the puzzle of intraislet interactions and their relevance to diabetes. J Clin Invest 85:983–987, 1990 14. Kvietys PR, Perry MA, Granger DN: Permeability of pancreatic capillaries to small molecules. Am J Physiol 245:G519 –G524, 1983 15. Rippe B, Haraldsson B: Transport of macromolecules across microvascular walls: the two-pore theory. Physiol Rev 74:163–219, 1994 16. Van Tine BA, Azizeh BY, Trivedi D, Phelps JR, Houslay MD, Johnson DG, Hruby VJ: Low level cyclic adenosine 3⬘,5⬘-monophosphate accumulation analysis of [des-His1,des-Phe6,Glu9]glucagon-NH2 identifies glucagon antagonists from weak partial agonists/antagonists. Endocrinology 137: 3316 –3322, 1996 17. Göke R, Fehmann H-C, Linn T, Schmidt H, Krause M, Eng J, Göke B: Exendin-4 is a high potency agonist and truncated exendin-(9-39)-amide an antagonist at the glucagon-like peptide 1-(7-36)-amide receptor of insulinsecreting -cells. J Biol Chem 268:19650 –19655, 1993 18. Azizeh BY, Van Tine BA, Sturm NS, Hutzler AM, David C, Trivedi D, Hruby VJ: [des-His1,des-Phe6,Glu9]glucagon amide: a newly designed “pure” glucagon antagonist. Bioorg Med Chem Lett 5:1849 –1852, 1995 19. Rogiers V, Paeme G, Vercruysse A, Bouwens L: Procycline metabolism in isolated rat liver cells. In Pharmacological, Morphological and Physiological Aspects of Liver Ageing, Van Bezooyen CFA, Ed. Eurage, Rijswijk, Holland, 1984, p. 155–163 20. Widmann C, Bürki E, Dolci W, Thorens B: Signal transduction by the cloned glucagon-like peptide-1 receptor: comparison with signaling by the endogenous receptors of  cell lines. Mol Pharmacol 45:1029 –1035, 1994 21. Grodsky GM, Fanska R: The in vitro perfused pancreas. In Methods in Enzymology, Vol. 39: Hormone Action, Part D: Isolated Cells, Tissues, and Organ Systems. Hardman JG, O’Malley BW, Eds. New York, NY, Academic Press, 1975, p. 364 –372 22. Pipeleers DG, in’t Veld P, Van De Winkel M, Maes E, Schuit FC, Gepts W: A new in vitro model for the study of pancreatic A and B cells. Endocrinology 117:806 – 816, 1985 23. Pipeleers DG, Schuit FC, Van Schravendijk CFH, Van De Winkel M: Interplay of nutrients and hormones in the regulation of glucagon release. Endocrinology 117:817– 823, 1985 24. Fehlman M, Morin O, Kitagbi P, Freychet P: Insulin and glucagon receptors in isolated rat hepatocytes: comparison between hormone binding and amino acid transport stimulation. Endocrinology 109:253–261, 1981 25. Curry DL, Bennett LL, Grodsky GM: Dynamics of insulin secretion by the perfused rat pancreas. Endocrinology 83:572–584, 1968 26. Grill V, Adamson U, Cerasi E: Immediate and time dependent effects of glucose on insulin release from rat pancreatic tissue. J Clin Invest 61:1034 –1043, 1977 DIABETES, VOL. 51, MARCH 2002 27. Grill V: Time and dose dependencies for priming effect of glucose on insulin secretion. Am J Physiol 240:E24 –E31, 1981 28. Weir GC, Mojsov S, Hendrick GK, Habener JF: Glucagonlike peptide I (7-37) actions on endocrine pancreas. Diabetes 38:338 –342, 1989 29. Halter JB, Graf RJ, Porte D Jr: Potentiation of insulin secretory responses by plasma glucose levels in man: evidence that hyperglycemia in diabetes compensates for impaired glucose potentiation. J Clin Endocrinol Metab 48:946 –954, 1979 30. Loubatieres-Mariani MM, Chapa J, Puech R, Manteghetti M: A different action of hypothermia on insulin release from the isolated, perfused rat pancreas, depending on the stimulating agent. Diabetes 29:895– 898, 1980 31. Weir GC, Clore ET, Zmachinski CJ, Bonner-Weir S: Islet secretion in a new experimental model for non-insulin-dependent diabetes. Diabetes 30:590 – 595, 1981 32. Gerich JE, Lovinger R, Grodsky GM: Inhibition by somatostatin of glucagon and insulin release from the perfused rat pancreas in response to arginine, isoproterenol and theophylline: evidence for a preferential effect on glucagon secretion. Endocrinology 96:749 –754, 1975 33. Jansson L, Hellerström C: Stimulation by glucose of the blood flow to the pancreatic islets of the rat. Diabetologia 25:45–50, 1983 34. Orci L, Unger RH: Functional subdivision of islets of Langerhans and possible role of D cells. Lancet 2:1243–1244, 1975 35. Orci L, Baetens D, Ravazzola M, Stefan Y, Malaisse-Lagae F: Pancreatic polypeptide and glucagon: non-random distribution in pancreatic islets. Life Sci 19:1811–1816, 1976 36. Schuit FC, Derde MP, Pipeleers DG: Sensitivity of pancreatic A and B cells to somatostatin. Diabetologia 32:207–212, 1989 37. Unger RH, Orci L: Possible roles of the pancreatic D-cell in the normal and diabetic states. Diabetes 26:241–244, 1977 38. Yamamoto T, Raskin P, Aydin I, Unger R: Effects of insulin on the response of immunoreactive glucagon to an intravenous glucose load in human diabetes. Metabolism 28:568 –574, 1979 39. Hansen CB, Jen KC, Pek SB, Wolfe RA: Rapid oscillations in plasma insulin, glucagon, and glucose in obese and normal weight humans. J Clin Endocrinol Metab 54:785–792, 1982 40. Golay A, Swislocki ALM, Chen YI, Jaspan JB, Reaven GM: Effect of obesity on ambient plasma glucose, free fatty acid, insulin, growth hormone, and glucagon concentrations. J Clin Endocrinol Metab 63:481– 484, 1986 41. Kieffer TJ, Heller RS, Unson CG, Weir GC, Habener JF: Distribution of glucagon receptors on hormone-specific endocrine cells of rat pancreatic islets. Endocrinology 137:5119 –5125, 1996 42. Kawai K, Ipp E, Orci L, Perrelet A, Unger RH: Circulating somatostatin acts on the islets of Langerhans by way of a somatostatin-poor compartment. Science 218:477– 478, 1982 43. Bonner-Weir S: Morphological evidence for pancreatic polarity of -cell within islets of Langerhans. Diabetes 37:616 – 621, 1988 675