Smart living with
heart failureTM
Working Toward Stability
You know what it’s like to cope with serious heart disease
and the attention to detail it takes, such as weighing yourself,
watching your diet, and taking your medications. You’re also
familiar with the emotional ups and downs and how much it
means to have the support of others. Using the heart failure
program helps you meet the daily challenges you face with
the support of a team of professionals.
The most effective way to keep your heart condition stable
so you can stay out of the hospital is to monitor your weight
and symptoms. With the heart failure program, you are
less likely to forget to do these things. And if there are any
significant changes, your doctor will be notified.
In fact, you have quite a bit of control over your heart
condition. You have already taken control by using the heart
failure program. Are you also in control of other areas? Your
doctor prescribes your medications, but you’re the one who
decides to take them. You’re advised to eat a low-salt diet,
but it’s up to you whether you follow it. Within the limits
that your doctor sets, you can be as active or inactive as
you like. How well you manage your heart condition is very
much up to you.
Heart failure
is a common
condition with
an unfortunate
name. Most
people with
heart failure
have hearts that
function well
enough most
of the time. Of
course, living
with a heart
condition is
hard. But using
the heart failure
program may
help you with
the challenges.
Throughout your
guide, we’ll be
talking about
motivation, selfconfidence,
and having a
plan. These are
three essential
ingredients to
making any kind
of successful
change, whether
it’s taking your
medications
regularly, being
more active,
or dealing with
stress.
Know why you
want to change,
what is likely
to get in your
way, and what
you will do to
deal with your
barriers. Not
everything will
go smoothly. It
never does for
anybody. But by
managing your
heart condition,
you can start
envisioning a
better future.
What do you see?
Taking on the Challenge
Do you feel that you can handle it all? At first it may seem
kind of scary. You may feel confused as to where or how to
begin. But taking charge and managing your condition puts
you in control.
Wanting to be in charge is only the first step. Next, you need
information so you know what to do and why. But even that
isn’t enough. In addition to knowing what to do, you have to
have a plan for how to change.
We’ll give you the basics about heart failure and its
management. We’ll also get you started on developing a
plan for yourself. The topics we address are:
Description of heart failure
Heart medications
Other diseases you may have
Diet and fluids
Physical activity
Stress and depression
Lifestyle risk factors for heart failure
Other resources
Don’t try to do everything at once. Make each change
slowly. Learn from your mistakes. Reward yourself for
meeting your goals. And remember to keep using the
heart failure program to help you along the way.
What Does “Heart Failure” Mean?
Heart failure means that your heart can’t pump blood as
well as it used to. Heart failure usually develops because
the heart has been damaged by, for instance, diabetes, high
blood pressure that isn’t controlled, or a heart attack.
Heart failure does not mean your heart is about to stop
beating.
A damaged heart is not strong enough to pump blood to all
parts of your body, so the blood starts to back up in your
veins. This may cause fluid to build up in your lungs, feet,
ankles, or abdomen.
This is where the term congestive heart failure comes
from.
Common Symptoms of Heart Failure
The earliest and most common symptoms of heart failure
are:
Shortness of breath
Weight gain
Swelling in feet or ankles
Fatigue
Dry cough
Frequent urination
Abdominal swelling
Weakness
The more you
know about
your condition,
the better you’ll
be able to care
for yourself and
help others care
for you. We’ll
start by talking
about what heart
failure is—and
what it isn’t,
the symptoms
it causes, and
the importance
of monitoring
yourself.
There are a
lot of things
you can do for
yourself. That’s
what this guide
is all about. By
working with
your doctor
and the rest
of your health
care team,
you’ll be able to
take control of
your condition.
Keep reading
to learn about
diet, activity,
medications,
stress
management,
and more.
With progression of the disease, your symptoms may
change. As someone with moderate to severe heart failure,
you may be experiencing some of the following symptoms.
Cough
Shortness of breath at rest, while lying down, or
sleeping
Abdominal bloating
Cold hands and feet
Less frequent urination
Lightheadedness
Mental confusion
Passing out
Impotence
Monitoring your symptoms is the best way to prevent
sudden worsening of your heart condition. The heart failure
program not only keeps track for you but the program’s
nurses notify your doctor if there is a significant change.
Catching symptoms early may help keep you out of the
hospital. The heart failure program has been proven to
improve the quality of life for people like you. It has also
been proven to keep people with a heart condition out of
the hospital and the emergency room. But remember, the
only way the heart failure program can help you is if you
keep using it.
If It’s 6 A.M., It’s Time for the Blue Pill
First, it’s important to know what drugs you’re taking and
what they do. You also need to know how often to take them
and what doses you’re on. Finally, if you haven’t already,
speak with your doctor or pharmacist about common side
effects of your drugs.
The chart below describes the most common types of heart
failure medications. You may be taking other drugs for your
heart failure or other conditions. Talk with your doctor about
the specific drugs you are on.
Commonly Used Drugs in Heart Failure
TYPE OF DRUG
(with some examples)
ACTION OF DRUG
IN YOUR BODY
Eliminate water and sodium through your kidneys. Reduce swelling
& shortness of breath.
COMMON SIDE
EFFECTS
Dizziness, irregular pulse, nausea,
fatigue, leg cramps
ACE INHIBITORS
(Altace®, Capoten®,
Vasotec ®, Zestril®,
and others)
Widen your blood vessels to make it easier
for your heart to pump
Dizziness, dry cough,
headache, low blood
pressure, fatigue,
dizziness with abrupt
change in position,
loss of taste, swelling in lips or throat
BETA-BLOCKERS
(Coreg®, Zebeta®,
and others)
Increase the pumping
efficiency of your heart.
Decrease heart rate.
Lower risk of abnormal heart rhythm.
Fatigue, dizziness,
low blood pressure,
fluid retention, slow
pulse, diarrhea, headache, masks signs
of low blood sugar
DIGOXIN
(Lanoxin®)
Increase the strength
of your heart’s contractions. Slows heart rate.
Nausea, vomiting,
blurred or colored
vision, muscle weakness, headache, anorexia, diarrhea, sensitivity to bright light
DIURETICS or
WATER PILLS
(Lasix®, Bumex®,
and others)
You are
probably
aware of how
important your
medications
are to helping
your heart
function, but
if you’re like
many people,
you don’t
always take
your pills
exactly as your
doctor has
directed. We
understand
how hard it can
be. We’d like
to offer some
ideas on how to
stick with your
medication
plan.
Drugs and
Herbs to Avoid
There are some
drugs and herbs
that do not mix
well with drugs
for heart failure.
Some of them
are:
• Pain medications, such as
Motrin®, Aleve®,
ibuprofen,
Anaprox®, indocin, Relafen®,
Celebrex®, and
other NSAIDS
• Some blood
pressure drugs
• Some heart
rhythm drugs
• Nasal decongestants, such
as pseudoephedrine
• St. John’s wort
• Ephedra or ma
huang
• Ginseng
• Ginkgo
Staying on your medication schedule depends a lot on
why you want to do it and whether you feel that you can
do it. Reasons people take their medications include:
Feeling better
Not wanting to disappoint the doctor
If not taken, spouse might get mad
Living longer
Now, list your reasons. Decide which are most important
to you personally and write them down.
Next, think about how confident you are that you can take
your medications as directed. Rate yourself on a scale
from 1 to 10 with 1 being the lowest confidence and 10 the
highest.
Then think about what would keep you from following your
medication plan. Common barriers include forgetfulness,
cost, side effects, and taking lots of pills. What are your
barriers?
Finally, come up with ways to overcome your barriers.
Some ideas are: putting your medication at a place you’ll
be when you need to take it, using a pillbox, and asking
about cheaper generic drugs. Make a commitment to take
first-class care of yourself. You deserve it.
Speak with your
doctor about specific drugs and
herbs you should
avoid. And don’t
stop taking any
medication without first talking to
your doctor.
Other Conditions You May Also Have
It’s very common for people who have diabetes, coronary
heart disease, and high blood pressure to also have heart
failure.
Diabetes
If you have diabetes, you are probably used to managing your
illness. Managing your heart condition involves the same kind
of attention.
You already know that the heart failure program helps you
keep track of your health. If there is a major change, the
nurses will contact your physician.
Coronary Artery Disease (CAD)
Most people who have heart failure also have CAD. You may
have chest pain or a history of a heart attack. The best way to
protect your heart from more damage is to follow your diet, be
as active as you can, and take your medications as directed.
High Blood Pressure
High blood pressure makes it harder for your heart to pump
blood, so it tends to make heart failure worse. If you take your
blood pressure at home, you will have a record over time.
This is a good way for your doctor to see if your treatment is
working.
Fortunately, many of the treatments used for diabetes, CAD,
and high blood pressure are also good for heart failure, such
as ACE inhibitors and beta-blockers. Also, physical activity
and weight loss are good for all these conditions.
A diet low in salt with lots of fruit, vegetables, and low-fat
dairy products may lower blood pressure in some people.
Ask your doctor if this diet would be good for you.
Your Partners in Care
It can be hard and frustrating to take care of yourself when
you have more than one chronic condition. Some common
issues for people with two or more chronic illnesses are:
Drugs for one illness affect another health problem
Coordinating all the medications
Physical limitations of one condition may make it
hard to manage another
Cost of medications
Feeling a loss of control
Need for social support
Visits to many healthcare providers
Depression
People with more than one serious condition need a reliable
support system. This group may include your doctor,
nurse, pharmacist, social worker, home health aide, other
providers, family, and friends, as well as the heart failure
program. Your best strategy is to work with your doctor,
social worker, or other provider to help you come up with a
plan to improve your quality of life.
IMPORTANT IMMUNIZATIONS
Influenza Vaccine (The Flu Shot)—People who have
heart conditions are more likely than other people to
develop complications from the flu, such as pneumonia.
Getting a flu shot will help reduce that risk. The flu shot
you got last year won’t work this year because the virus
changes so rapidly. You need to get a shot every year
to stay protected.
Pneumonia Vaccine—There is also a vaccine to
protect you from getting many types of pneumonia. If
you’re 65 or older and have not had this vaccine before,
you just need to get it once. If you get the vaccine when
you’re younger than 65, you’ll need to get a booster
shot, but not until at least five years after you got your
first one.
Fresh foods are
always ideal, but
you can have
processed or
prepared foods.
Here are some
good choices:
• Air-popped
or salt-free
microwave
popcorn
• Applesauce
• Frozen or nosalt-added
canned green
beans
• Skinless
chicken breasts
• Low-sodium
canned tuna
• Low-sodium
vegetable broth
Shake the Salt Habit
Because you have a heart condition, it is important to watch
your salt intake. Eating too much salt will make your body
retain water and you’ll gain weight. The extra fluid puts a
strain on your heart and you might experience shortness of
breath, edema (swelling), or other symptoms. Cutting down
on the amount of salt you eat may prevent this. Aim for about
a teaspoon of salt or 2000 milligrams of sodium a day.
What About Flavor?
Your food will taste bland if you remove the salt all at once.
But if you cut down slowly, you will probably find that you
don’t miss salt. Most people adapt in two to three months.
How Can I Cut Down?
There are four basic steps to reducing salt:
Avoid adding salt to your food. Take the salt shaker
off the table and do not add salt while you are cooking
foods.
Adapt dishes you like to eat so that they have less
salt. Flavor your food with herbs, spices, onions,
lemon juice, and vinegar. (Avoid salt substitutes that
contain potassium. But Mrs. Dash® and Papa Dash®
are OK.)
Pick foods that are naturally low in sodium. Think
fresh—fresh foods (fruits, vegetables, meats, poultry,
fish, and fruit juice) are always a great choice.
Canned fruits, plain frozen vegetables, and dried
beans, peas, rice, and lentils are also a good lowsodium choice.
10
Learn to read food labels. Most of the salt in our diet
comes from processed food. Look for food labeled
low-sodium or salt-free. Low-sodium foods are
better than high-sodium foods, but they can still
have up to 140 milligrams of sodium per serving. A
few servings can put you over your limit. It’s better to
go with salt-free foods, which contain less than five
milligrams per serving.
It is not just what you eat. How much you eat is also very
important. Learn about serving sizes and use measuring
cups to serve your food.
Many patients with a heart condition are told to limit their
fluids to lower the risk of edema. For example, your doctor
may have limited your fluids to no more than two quarts
a day. To help you track your fluids, fill up a two-quart
container with water each morning. Every time you have
some fluid (water, soup, coffee, tea, or juice), empty that
same amount from the container. When the container is
empty, you have had your two quarts!
11
Table salt is
a combination
of the minerals
sodium and
chloride. Most
of our sodium
comes from
table salt, but it
shows up other
places as well.
Check food
labels for
sodium
additives and
preservatives.
Avoid foods
that have
an additive
with sodium
in the name.
Common ones
are:
• Sodium sulfite
• Sodium
benzoate
• Sodium
caseinate
• Disodium
phosphate
• Monosodium
glutamate or
MSG
Consult your
doctor before
starting any
exercise
program. You
should also
always talk with
your doctor
before doing any
kind of exercise
or any activity
that makes
your symptoms
worse.
You Mean Exercise Is Good for Me?
It sure is! If your doctor hasn’t already talked to you about an
exercise program, you need to bring it up. Even someone
with severe heart failure can do mild exercise.
Research has shown that exercise can ease symptoms,
increase strength, and improve quality of life for people in
all stages of heart failure.
Your doctor will want to make sure that your condition is
stable before recommending exercise training. If you get
the go-ahead, you will need to know what kinds of exercises
are safe for you to do. You should also find out how often
to do them, what it should feel like, and what you shouldn’t
do.
You may be referred to a training program to get a
personalized exercise plan. The goal is to gradually increase
your physical strength and emotional well-being.
You should stop exercising immediately if you experience
any of the following: increased fatigue, worsened shortness
of breath, chest pain, lightheadedness, or palpitations.
12
But I Have Trouble Climbing Stairs. How Can I
Exercise?
You may be thinking that you have enough to worry about
without figuring out how to exercise, too. But being more active
can help you feel better physically and mentally. Exercising
can be another way you do something for yourself in addition
to participating in the heart failure program.
It’s easy to come up with reasons not to exercise. Just a
few might be:
I’m too tired.
I don’t like to exercise.
I don’t have the willpower.
The list is endless, but the people who are the most
successful at sticking with exercise are the ones who do it
for reasons other than their doctor’s recommendation. For
instance:
I’d like to play with my grandchild.
I want to be able to get my own lunch.
I want to be able to visit with my friends.
What are the things you would like to
do if you felt stronger?
13
9
Besides feeling
motivated to be
more physically
active, you need
to have a plan
with a goal. Your
physician or
exercise trainer
should work with
you to create
a program that
gets you moving
and gradually
increases your
strength.
Many people
with serious
heart conditions
feel anxious
and stressed.
It’s not
surprising. You
have to deal
with physical
limitations,
your diet, and
medications.
Even daily
hassles can
seem bigger.
Emotional Strain and Your Heart
Taming Stress
One part of taming stress is knowing that you’ll always have
to deal with it. Another part is realizing that you have some
control over it.
Since you use the heart failure program, you know that taking
good care of yourself can affect how you feel physically and
mentally. This is important because emotional stress can
increase the risk of hospitalization for patients with heart
failure. There are lots of ways to manage stress, including:
Deep breathing
Worry control
Meditation or relaxation
Time management
Yoga, tai chi, or other meditative movement
These methods aren’t hard to learn, but they require
practice. Knowing that you have the skills to handle stress
will help, too.
In a study, patients with heart failure learned how to calm
themselves by taking slow, deep breaths, focusing their
attention around their heart, and remembering a positive
emotion. They practiced at least two to five times a day.
After 10 weeks, they had lower stress levels, better physical
fitness, and less emotional upset.
14
10
Not Feeling Like Yourself?
If you are having trouble sleeping, your appetite has changed,
or you don’t have as much energy as you used to, your
symptoms could be due to your heart condition. But there’s
also a good chance that they’re caused by depression.
The good news is that depression can be treated with
medications and counseling. Depression is a medical
condition; it’s not due to weak character. Let your doctor
know if you have had any of the following symptoms for
more than two weeks:
Sleeping too little or too much
Decreased pleasure in activities
Excessive guilt or feelings of worthlessness
Loss of energy or fatigue
Decreased concentration
Change in appetite
Mental slowness or agitation
Thoughts of death or suicide, or suicide attempt
If you have any of these symptoms, you don’t have to suffer.
Effective treatment is available.
15
Staying
Connected
People who don’t
have a chronic
illness might
have a hard time
understanding
the struggles
you have to
deal with. But
avoiding them
won’t help. If
you don’t have
the support
you need you
may feel more
stressed or
depressed.
It can make
your physical
condition worse.
If you need more
support, speak
with your doctor
or nurse. Find
out what types
of resources
are available for
you and your
family. Staying
connected to
loved ones can
be powerful
medicine.
You’re already
doing many
things for yourself to maintain
or improve your
quality of life,
such as
monitoring your
weight and
symptoms with
the heart failure
program. Here
are three more
suggestions that,
if they apply to
you, can ease
the burden on
your heart:
• Quit smoking
• Lose weight
• Limit alcohol
Risks You Can Control
If You Smoke, Quit
We know we’re not telling you anything new about the risks
of smoking, but a lot of people don’t really know how bad
it is for your heart. A smoker who quits reduces his or her
risk of a heart attack in the first 24 hours, and the risk keeps
going down. On top of that, quitting can help your heart
pump more effectively.
We’re not trying to make it sound as though quitting smoking
is easy. We know it’s not, but there are many different
medications available now that can help you through it. Talk
with your doctor about the resources available to help you
quit. It could do your heart a world of good.
16
If Needed, Lose Weight
You already know how excess fluid can put additional strain
on your heart. Carrying around excess fat can also make your
heart work harder. If you have diabetes or high blood pressure,
you can also improve those conditions by losing weight.
Losing a small amount of weight, combined with limiting
dietary salt, can result in a marked improvement in your
heart function. Losing more weight will result in even greater
benefits to your heart, and if your heart is working better,
you’re less likely to be hospitalized.
We know that it’s a lot easier to talk about losing weight
than to do it. But the same approach we discussed in the
exercise section applies here.
What are your reasons for losing weight?
Because your doctor says it’s a good idea, you want to
stay out of the hospital, or another reason?
What are your barriers to losing weight?
Snacking? Large portions? Inactivity?
What can you do to overcome your barriers?
Make a plan that will help you deal with your personal
problem situations, and find people who support your efforts.
Talk with your doctor or nutritionist and keep working at it.
Remember to use the heart failure program to track your
weight on a regular basis. Remind yourself of your goals at
least once a day, and reward yourself for reaching specific
goals, like eating an extra vegetable serving a day for one
week.
Build your confidence in your ability to take charge of your
health by turning small steps into the results you want.
17
Limit Alcohol
Alcohol use is
discouraged for
patients with
heart failure, or
saved for special
occasions. Many
years of heavy
drinking can
actually damage
your heart and
lead to heart
failure.
If you drink
heavily, quitting
drinking
completely
is your best
strategy.
Fortunately, if
you stop drinking
now, you can
limit, and possibly
reverse, some of
the damage to
your heart.
Even cutting
down may
keep your heart
condition from
getting worse.
Speak with your
doctor about
making a plan to
stop or limit your
alcohol use.
You’ve got
some quality
partners.
Because you are
using the heart
failure program,
you have nurses
monitoring your
health every
day. They keep
track of how you
are doing and
alert your doctor
when needed.
However, there
may be a time
when you will
need to contact
the doctor
yourself.
When to Get Help
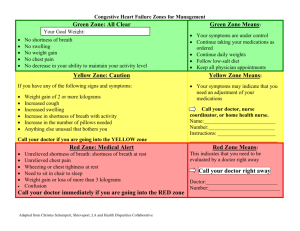
When to Call the Doctor:
Call your doctor if you have a sudden change in ANY heart
failure symptoms.
Other Reasons to Call Your Doctor:
Difficulty breathing during activities that did not
cause breathing problems before
Shortness of breath when you lie down
Waking up at night with shortness of breath
Dry, hacking cough, especially when you lie down
Rapid weight gain (2-3 lbs. in 6 days or less)
Increased fluid in your legs or elsewhere
When to Call 911:
Chest pain not relieved within 15-20 minutes by rest
or medication
Sudden onset of tingling, numbness, or weakness of a part of the body
Sudden dimmed or blurred vision
Difficulty speaking or understanding speech
Dizziness, vomiting, or seizures
Clumsiness
Loss of consciousness
Severe, localized headache
18
When to Seek Emergency Medical Care:
Onset of severe shortness of breath
Sudden episode of prolonged, irregular
or very rapid heartbeat associated
with dizziness, nausea, or fainting
Foamy, pink mucus with cough
Sense of impending doom associated
with heart or lung symptoms
Books for More Information:
American Heart
Association
www.americanheart.org
Heart Failure
Society of
America
www.abouthf.org
Success with Heart Failure: Help and Hope for Those with Congestive Heart Failure
Marc Silver, M.D.
American Heart Association Low Salt Cookbook American Heart Association
The No-Salt, Lowest Sodium Cookbook
Donald Gazzinga
The Living Heart Brand Name Shoppers’ Guide Michael DeBakey and Antonio Gotto, Jr.
The Relaxation & Stress Reduction Workbook – Martha Davis, Elizabeth Eshelman, and Matthew McKay
Next Steps: Speak with your doctor about any questions
you have. Make sure that you get the answers you need.
Also, remember to continue to use the heart failure program.
You don’t need to face the challenges of having a heart
condition alone. The heart failure program nurse team is
there for you.
Web Sites
for More
Information
19
Mind Body
Medical
Institute,
Harvard
University
www.mbmi.org
Aleve® is a registered trademark of Bayer Group. Altace® is a registered
trademark of King Pharmaceuticals Inc. Anaprox® and Bumex® are
registered trademarks of Roche Pharmaceuticals. Capoten® is a
registered trademark of Par Pharmaceutical, Inc. Celebrex® is a
registered trademark of Pfizer, Inc. Coreg®, Lanoxin®, and Relafen®
are registered trademarks of GlaxoSmithKline. Lasix® is a registered
trademark of Aventis Pharmaceuticals Inc. Motrin® is a registered
trademark of McNeil Consumer & Specialty Pharmaceuticals. Vasotec ®
is a registered trademark of Biovail Corporation. Zebeta® is a registered
trademark of Lederle Pharmaceuticals. Zestril® is a registered trademark
of AstraZeneca PLC. Mrs. Dash® and Papa Dash® are registered
trademarks of Alberto-Culver Company.
20
Notes
Copyright 2006. Alere Medical Incorporated. All rights reserved. Any mention of a particular
product is not an endorsement, but only mentioned for educational purposes.
E4
21
This booklet contains general
health information and is not
a substitute for professional
health care. You should consult
an appropriate health care
professional for your specific
needs. Some treatments
mentioned in this booklet may
not be covered by your health
plan. Please refer to your
benefit plan documents for
information about coverage.
Insurance coverage provided by or through United HealthCare Insurance Company or its affiliates. Administrative services
provided by United HealthCare Insurance Company, United HealthCare Services, Inc. or their affiliates.
©2007 UnitedHealthcare Services, Inc.
UHC 0445