Video Endoscopic Inguinal Lymphadenectomy: A New Minimally
advertisement

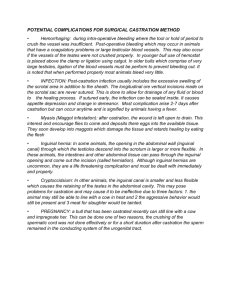
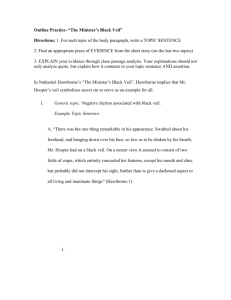
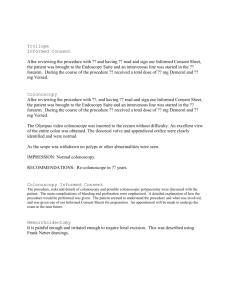
Video Endoscopic Inguinal Lymphadenectomy: A New Minimally Invasive Procedure for Radical Management of Inguinal Nodes in Patients With Penile Squamous Cell Carcinoma Marcos Tobias-Machado, Alessandro Tavares, Antônio Augusto Ornellas, Wilson Rica Molina, Jr., Roberto Vaz Juliano* and Eric Roger Wroclawski From the Section of Urologic Oncology, Discipline of Urology, ABC Medical School, São Paulo and Albert Einstein Jewish Hospital Research Institute, National Institute of Cancer (AAO), Rio de Janeiro, Brazil Purpose: Video endoscopic inguinal lymphadenectomy is a recently described lymphadenectomy with the same template of the open technique but performed with laparoscopic instruments under video guidance. It was developed to decrease procedure related morbidity while maintaining good oncological results. We report our initial results in a trial comparing video endoscopic inguinal lymphadenectomy with standard inguinal lymphadenectomy. Materials and Methods: From 2003 to 2005, 10 patients with penile carcinoma who were at high risk for inguinal metastases underwent bilateral inguinal lymphadenectomy. We performed standard lymphadenectomy in 1 limb and video endoscopic inguinal lymphadenectomy on the contralateral side. Perioperative results and followup data were compared. Results: No intraoperative complications occurred. Mean operative time was 92 and 126 minutes for open and endoscopic surgery, respectively (p ⫽ 0.00002). Despite the small number of patients we noted a decrease in cutaneous complications with video endoscopic inguinal lymphadenectomy (0% vs 50%, p ⫽ 0.017) and a trend toward decreased overall morbidity with this endoscopic technique (20% vs 70%, p ⫽ 0.059). The mean number of retrieved and positive lymph nodes were similar for the 2 techniques. At a mean followup of 18.7 months (range 12 to 31) no signs of recurrence or disease progression were noted. In the postoperative period 9 of the 10 patients identified video endoscopic inguinal lymphadenectomy as the preferred technique in terms of surgical morbidity. Conclusions: Video endoscopic inguinal lymphadenectomy is a safe and feasible technique in patients with penile carcinoma and nonpalpable nodes. These preliminary results suggest that video endoscopic inguinal lymphadenectomy may decrease postoperative morbidity without compromising oncological control. Future studies should include the bilateral procedure, longer term followup and a greater number of patients. Key Words: penis, penile neoplasms, lymph node excision, laparoscopy, urethral neoplasms standard open procedure. VEIL is an emerging technique recently reported in clinical settings, which was developed to decrease morbidity and improve patient outcomes without compromising oncological control.13 We report the initial results of a trial comparing VEIL and open conventional inguinal lymphadenectomy in terms of feasibility, surgical morbidity and preliminary cancer control in patients with penile cancer treated at our institution. enile carcinoma is a rare malignant disease with a significantly higher incidence in some areas of underdeveloped countries. Inguinal nodal involvement is found in 20% to 40% of cases at diagnosis and nodal metastasis is an important predictive factor for survival.1–3 Although recent data demonstrated a survival benefit with immediate resection of clinically occult lymph node metastases, surgical morbidity is still high.4,5 Contemporary series show that refinements of the technique during surgery associated with adequate postoperative care can decrease complication rates to approximately 50%.6,7 In recent years some alternatives were proposed targeting decreased surgical morbidity after inguinal lymphadenectomy based on templates with limited excision.8 –10 Although these options are potentially less invasive, they have some drawbacks concerning cancer control and inguinal recurrence during followup.11,12 Minimally invasive techniques for ablative procedures are accepted for a wide range of urological diseases because morbidity is decreased compared with the corresponding P PATIENTS AND METHODS From August 2003 to February 2005, 10 patients with penile squamous cell carcinoma were selected at our institution. They underwent penile amputation and 1 month after initial surgery they underwent the inguinal procedure based on specimen pathological features. They had no clinically palpable lymph nodes but they had high risk pathological factors for inguinal metastases, such as pathological stage greater than pT1, histological grade greater than 1, or microvascular or lymphatic embolization.2,14 After they provided informed consent for the study, which was approved by our Ethical Institutional Committee, they were included in our prospective protocol. Submitted for publication June 9, 2006. Study received Ethical Institutional Committee approval. * Financial interest and/or other relationship with Mentor. 0022-5347/07/1773-0953/0 THE JOURNAL OF UROLOGY® Copyright © 2007 by AMERICAN UROLOGICAL ASSOCIATION 953 Vol. 177, 953-958, March 2007 Printed in U.S.A. DOI:10.1016/j.juro.2006.10.075 954 VIDEO ENDOSCOPIC VERSUS STANDARD INGUINAL LYMPHADENECTOMY In each patient classic open inguinal lymphadenectomy was performed in 1 limb (standard procedure) and VEIL was performed in the other limb (study group). The choice of which side to use for each technique was randomized. A pathologist blinded to the technique used for each side and to patient outcomes examined the specimens. Parameters analyzed were operative time per side, number of dissected lymph nodes, intraoperative complications, incision aspect, drain output, postoperative patient outcomes, histologically positive lymph nodes and cancer control after at least 1 year of followup. Subjective pain evaluation was determined during postoperative days 1 to 3. Patient satisfaction was evaluated at discharge from the hospital. All patients with positive inguinal lymph nodes subsequently underwent extended pelvic laparoscopic lymphadenectomy and they received no further surgical treatment. A conventional radical procedure was performed using an oblique inguinal incision, as previously described.5 Briefly, superficial and deep lymph nodes were dissected at the femoral triangle medially to the femoral artery without saphenous vein preservation. At the end of resection the sartorius muscle was rotated to cover the artery and femoral vein.5 VEIL was performed with the patient supine with thigh abduction. The video system was placed at the opposite side next to the patient waist. A 2 cm incision was made 2 cm distal to the lower vertex of the femoral triangle. Scissors and digital maneuvers were used to develop a dissection plane deep to Scarpa’s fascia. After digital elevation of the skin through the first incision a second 1.0 cm incision was made 6 cm medial to the apex of the triangle to place a 10 mm trocar. The last 5 mm port was placed in an analogous manner 6 cm lateral to the apex of the triangle. A 10 mm Hassan trocar was inserted in the first incision. The first port accommodated 0-degree optics. The medial port accepted the harmonic scalpel or the clip applier and the lateral port accepted the grasper, scissors or a dissection device (fig. 1). The surgical team was positioned lateral to the patient leg, so that surgery could be performed ergonomically. The working space was insufflated with CO2 at 15 mm Hg. CO2 pressure was kept as low as 5 to 10 mm Hg during all procedures. Transillumination allowed good orientation and control of the progression of dissection toward the cavity (fig. 2). So that all superficial lymphatic tissue can be removed, it is imperative to perform dissection with a harmonic scalpel FIG. 1. Disposition of trocars in right thigh for VEIL. Pentagons represent 10 mm trocars. Circle represents 5 mm trocar. FIG. 2. Transillumination and external reference points to monitor working space development. in the plane just below Scarpa’s fascia (fig. 3). The main landmarks are the adductor longus muscle medial, the sartorius muscle lateral and the inguinal ligament superior. At this point we could identify the saphenous vein medial, and the spermatic cord and external inguinal ring superomedial. The femoral nerve branches, which could be preserved, were present laterally. Identification and dissection of the saphenous vein was made cranially up to the fossa ovalis. The femoral artery was identified at the femoral triangle at the lateral edge of the dissection limit. Distal lymphatic tissue was ligated at the femoral triangle vertex and dissected with a harmonic scalpel with final control achieved using clips (fig. 4). Lymphatic tissue dissection reached the femoral vessels above the femoral ring. Distal saphenous ligation was performed with metallic or polymeric clips. Control of the saphenous branches was performed and proximal ligation of the saphenous vein at the femoral vein was done with metallic or polymeric clips. At the end of dissection the specimen was freed after ligation of the proximal portion of the lymphatic tissue at the deep portion of the femoral channel (fig. 5). The specimen was removed through the first 20 mm incision after being placed in a plastic retrieval bag. A suction drain was inserted through the 5 mm port incision. Prophylactic intravenous cephalothin was done routinely. In the postoperative period patients were encouraged to FIG. 3. Dissection deep to Scarpa’s fascia with harmonic scalpel VIDEO ENDOSCOPIC VERSUS STANDARD INGUINAL LYMPHADENECTOMY 955 specimens using the endoscopic technique. Pathological examination of positive lymph nodes did not demonstrate any capsular rupture. These 3 patients underwent additional laparoscopic pelvic lymphadenectomy posteriorly, which showed no additional positive nodes. Based on patient subjective evaluation 9 patients preferred the endoscopic technique in terms of surgical morbidity and 1 could not identify which technique was best for him. DISCUSSION FIG. 4. Specimen after control of venous and lymphatic branches with clips. ambulate early and none received anticoagulants. Oral intake was started 12 hours after the procedure. The suction drain was removed with an output of 50 ml or less. All patients were followed with clinical evaluation on postoperative days 7, 14, 30 and 60, and every 3 months thereafter. Followup was 12 to 31 months (mean 18.7). Statistical analysis was performed using the chi-square t and Fisher’s exact tests for comparative parameters. The confidence level was 95%. RESULTS Patient age was 39 to 60 years (mean 47). Table 1 shows patient characteristics, including local pathological stage, histological grade and associated vascular or lymphatic invasion before bilateral lymphadenectomy. No intraoperative complications were observed and all procedures were performed successfully. Mean operative time was 92 minutes (range 80 to 110) for open surgery and 126 minutes (range 90 to 130) for VEIL (p ⫽ 0.00002). The mean number of nodes removed was 9.7 (range 6 to 14) and 10 (range 6 to 16) for open surgery and VEIL, respectively (p ⫽ 0.52). Regarding postoperative complications, we observed a 20% incidence of complications related to VEIL vs 70% for open surgery (p ⫽ 0.059). With VEIL the frequency of skin related events was 0%, while with the conventional technique the frequency was 50% (p ⫽ 0.017, tables 1 and 2). Complications in the open group were skin necrosis in a small area in 3 cases, wound infection in 1, an area of cellulitis in 1, chronic lymphedema in 1 and lymphocele with spontaneous regression 2 months after lymphadenectomy in 1. In the endoscopic group there was 1 case of local hematoma with clinical resolution 10 days after surgery and 1 of lymphorrhea through the drain orifice, which lasted for 12 days. Concerning pain evaluation during the first 3 postoperative days, 9 patients reported less pain in the limb that underwent the endoscopic procedure and 1 reported no difference regarding pain between the 2 limbs. Mean time to drain removal (output less than 50 ml) was 6.4 days for open surgery and 4.9 days for VEIL. Positive lymph nodes were found in 3 patients (30%) (table 2). One positive lymph node was found on a specimen obtained through the open technique and 2 were obtained in There are some controversial issues concerning prophylactic inguinal lymphadenectomy in patients with penile cancer. While some groups reported data justifying immediate lymphadenectomy because of survival advantages,3,4 others recommended a watchful waiting policy and salvage surgery when the inguinal lymph nodes become clinically positive.15 Although the survival benefits of lymphadenectomy in patients with impalpable lymph nodes have been demonstrated, surgical morbidity is still high.3,5,6,15 Conventional surgery is frequently performed with a large inguinal incision and it can result in skin complications, such as skin necrosis and wound infection. Depending on the extent of ganglionic resection chronic lymphedema, lymphorrhea and lymphocele can occur. More recent studies suggest that the application of some intraoperative and postoperative measures can decrease complication rates.7 During the last 2 decades treatment in patients with penile carcinoma and impalpable regional lymph nodes has improved, making the procedure considerably less morbid. There are some explanations for these improvements. 1) Patient selection has improved and surgery has been avoided in patients at low risk for lymphatic disease.2,14 2) Some surgeons perform limited dissection with preservation of the saphenous vein.8 –11 Although morbidity decreased, all of these techniques still did not achieve optimal oncological control. More recently d’Ancona et al reported fewer complications with simplified staged lymphadenectomy compared with radical dissection.9 On the other hand, 5.5% of patients with negative simplified dissection had inguinal metastatic disease during followup. Another strategy that is accepted worldwide is lymphoscintigraphy to detect the functional sentinel lymph node.10 FIG. 5. Inspection after lymphadenectomy confirmed complete removal of superficial and deep lymph nodes within dissection template. 956 VIDEO ENDOSCOPIC VERSUS STANDARD INGUINAL LYMPHADENECTOMY TABLE 1. Demographic data and surgical results in 10 patients with bilateral inguinal lymphadenectomy by open and VEIL techniques Pt No.—Age 1—40 2—52 3—43 4—50 5—39 6—60 7—45 8—55 9—41 10—45 Operative Time (mins) Local TNM Pathological Stage/Grade Vascular or Lymphatic Invasion Open Surgery T2/G3 T1/G2 T2/G2 T3/G3 T2/G2 T3/G2 T2/G2 T2/G2 T2/G3 T1/G2 No Yes No Yes No Yes No No Yes Yes 90 80 100 80 90 110 100 90 100 80 Complications Drainage (days)* VEIL Open Surgery VEIL Open Surgery VEIL Pt Preferred Technique 130 110 120 100 130 130 120 120 120 90 Cutaneous necrosis None Lymphedema Epidermolysis None Lymphocele Epidermolysis Cellulitis Incision infection None None None None Lymphorrhea None None Hematoma None None None 6 6 6 7 5 10 7 4 7 6 5 4 3 6 5 8 3 4 5 6 VEIL VEIL VEIL VEIL None VEIL VEIL VEIL VEIL VEIL * Less than 50 ml/24 hours. Although this produces excellent results in decreasing surgical morbidity, Kroon et al recently reported that this type of procedure resulted in a 15% incidence of late inguinal recurrence, which can possibly compromise patient prognosis.12 In 2003 Bishoff et al described endoscopic subcutaneous modified inguinal lymphadenectomy in 2 cadaveric models and in 1 patient with stage T3N1M0 penile carcinoma.16 They reported the feasibility of the approach in the models but dissection could not progress in the patient because of a large lymph node in close contact with the femoral vessels. Based on this initial report our initial protocol did not include patients with palpable inguinal lymph nodes. After some modifications to the procedure we reported the first successful experience in 3 patients.13 VEIL was also based on other endoscopic techniques for vascular and axillary lymph node dissection.17,18 Notably as we were finishing our report we found an electronic publication via Google™ that was not indexed in Medline®, which was our initial database, showing preliminary experience of a group in Lyon, France with endoscopic inguinal lymphadenectomy in 28 cases of vulvar or distal vaginal cancer.19 This technique (inguinoscopy) was similar to the VEIL technique except it is a gasless procedure and the group preserves the greater saphenous vein and some of its branches. They observed minimal procedure related morbidity with only 1 vascular lesion, which required opening of the skin for suturing, and 7 lymphoceles (25%), which required needle aspiration. No wound breakdowns or lymphedema were ob- TABLE 2. Pathology results and oncological followup in 10 patients with bilateral inguinal lymphadenectomy by open and VEIL techniques No. Nodes Retrieved No. Pos Nodes Pt No. Open Surgery VEIL Open Surgery VEIL Followup (mos) 1 2 3 4 5 6 7 8 9 10 7 6 8 14 12 10 6 8 12 14 8 6 10 16 10 10 7 9 10 14 0 0 1 0 0 0 0 0 0 0 0 1 0 0 0 0 0 0 1 0 31 26 21 20 18 17 15 14 13 12 No patients had recurrence. served. Although median followup was not stated, only 1 recurrence was noted. Concerning complications, our preliminary results are encouraging, suggesting that the VEIL technique has the potential to decrease postoperative morbidity. Cutaneous, lymphatic and overall morbidity was less frequent for the VEIL procedure. There was a statistically significant difference in cutaneous morbidity favoring VEIL and in cases of lymphatic and overall morbidity the difference approached significance. We speculate that if our sample was greater, we would also observe a decrease in lymphatic and overall morbidity. We believe that the decreased morbidity observed in these initial patients may be explained by the fulfillment of several principles. The procedure was performed using small incisions, allowing better preservation of the skin blood supply and lymphatic drainage with minimal use of electrocautery and mechanical retraction. Incisions were made away from the great vessels, making a sartorius muscle flap rotation unnecessary. Small lymphatic vessels were identified under magnification and controlled with a harmonic scalpel. Larger branches were controlled with clips, minimizing lymphatic leakage and lymphocele formation. If this is the surgeon preference, saphenous vein preservation, which is implied by some groups to lead to less postoperative edema, or simplified dissection with intraoperative frozen sections can be done via the endoscopic technique.8,19 We understand that if frozen sections are positive, extension of the limits of dissection leads to an important increase in morbidity when performed via an open approach.9 Since all anatomical landmarks must be perfectly identified so that oncological control can be optimal, we think that VEIL should only be performed by surgeons with relatively good expertise in laparoscopic techniques who are familiar with the open inguinal lymphadenectomy. Although operative time was longer in relation to the open procedure, we believe that it will decrease as we gain more experience.19 Hypercarbia can occur but it is easily managed by hyperventilation and hyperhydration without any clinical repercussions. Postoperative pain seemed to be less on the endoscopic side. Patient subjective preferences confirmed that VEIL is an attractive technique. The length of the larger VEIL incision was 2 cm compared to 10 cm for open surgery with improved cosmesis (fig. 6). The possible benefits regarding rapid hospital discharge were not assessed because of protocol design. The smaller drain output on the endoscopic side VIDEO ENDOSCOPIC VERSUS STANDARD INGUINAL LYMPHADENECTOMY 3. 4. 5. 6. 7. FIG. 6. Postoperative view of VEIL incisions in left limb and standard lymphadenectomy in right limb. 8. allows us to suppose that we would have removed the drain and discharged the patient home earlier if the endoscopic technique had been performed on the 2 limbs. This hypothesis can be confirmed in a future study. The similar number of nodes removed on the 2 sides of the same patient is an indirect sign that VEIL can be as effective as the open approach. The aerosol phenomenon related to CO2 in malignant lymph nodes in this operation must be observed with caution and its clinical significance in this type of procedure awaits future long-term results. Our followup is still short for evaluating oncological control but the lack of progression, recurrence or port implants after 12 months in patients with positive nodes is encouraging. CONCLUSIONS VEIL is a safe and feasible technique in patients with penile carcinoma. Preliminary results suggest that VEIL allows decreased postoperative morbidity without compromising oncological control. Based on our data VEIL could become the chosen minimally invasive procedure for prophylactic inguinal lymphadenectomy in patients with penile cancer. Its experimental application can be expanded to treat lymph nodes in urethral, vulvar or skin cancer. New studies with more patients and longer followup are necessary to obtain more consistent data, although our results seem promising. Abbreviations and Acronyms 9. 10. 11. 12. 13. 14. 15. 16. VEIL ⫽ video endoscopic inguinal lymphadenectomy 17. REFERENCES 1. Srinivas V, Morse MJ, Herr HW, Sogani PC and Whitmore WF Jr: Penile cancer: relation of extent of nodal metastasis to survival. J Urol 1987; 137: 880. 2. Ficarra V, Zattoni F, Cunico SC, Galetti TP, Luciani L, Fandella A et al: Lymphatic and vascular embolizations are independent predictive variables of inguinal lymph node involvement in patients with squamous cell carcinoma 18. 19. 957 of the penis: Gruppo Uro-Oncologico del Nord Est (Northeast Uro-Oncological Group) Penile Cancer data base. Cancer 2005; 103: 2507. Ornellas AA, Correia Seixas AL, Marota A, Wisnescky A, Campos F and de Moraes JR: Surgical treatment of invasive squamous cell carcinoma of the penis: retrospective analysis of 350 cases. J Urol 1994; 151: 1244. Kroon BK, Horenblas S, Lont AP, Tanis PJ, Gallee MP and Nieweg OE: Patients with penile carcinoma benefit from immediate resection of clinically occult lymph node metastases. J Urol 2005; 173: 816. Abi-Aad AS and deKernion JB: Controversies in ilioinguinal lymphadenectomy for cancer of the penis. Urol Clin North Am 1992; 19: 319. Bevan-Thomas R, Slaton JW and Pettaway CA: Contemporary morbidity from lymphadenectomy for penile squamous cell carcinoma: the M.D. Anderson Cancer Center experience. J Urol 2002; 167: 1638. Nelson BA, Cookson MS, Smith JA Jr and Chang SS: Complications of inguinal and pelvic lymphadenectomy for squamous cell carcinoma of the penis: a contemporary series. J Urol 2004; 172: 494. Catalona WJ: Modified inguinal lymphadenectomy for carcinoma of the penis with preservation of saphenous veins: technique and preliminary results. J Urol 1988; 140: 306. d’Ancona CA, de Lucena RG, Querne FA, Martins MH, Denardi F and Netto NR Jr: Long-term followup of penile carcinoma treated with penectomy and bilateral modified inguinal lymphadenectomy. J Urol 2004; 72: 498. Lont AP, Horenblas S, Tanis PJ, Gallee MPW, van Tinteren H and Nieweg O E: Management of clinically node negative penile carcinoma: improved survival after the introduction of dynamic sentinel node biopsy. J Urol 2003; 170: 783. Lopes A, Rossi BM, Fonseca FP and Morini S: Unreliability of modified inguinal lymphadenectomy for clinical staging of penile carcinoma. Cancer 1996; 77: 2099. Kroon BK, Lont AP, Valdes Olmos RA, Nieweg OE and Horenblas S: Morbidity of dynamic sentinel node biopsy in penile carcinoma. J Urol 2005; 173: 813. Machado MT, Molina WR Jr, Tavares A, Forseto PH Jr, Juliano RV and Wroclawski ER: Comparative study between videoendoscopic inguinal lymphadenectomy (VEIL) and standard open procedure for penile cancer: preliminary surgical and oncological results. J Urol, suppl., 2005; 173: 226, abstract 834. Slaton JW, Morgenstern N, Levy DA, Santos MW Jr, Tamboli P, Ro JY et al: Tumor stage, vascular invasion and the percentage of poorly differentiated cancer: independent prognosticators for inguinal lymph node metastasis in penile squamous cancer. J Urol 2001; 165: 1138. Theodorescu D, Russo P, Zhang ZF, Morash C and Fair WR: Outcomes of initial surveillance of invasive squamous cell carcinoma of the penis and negative nodes. J Urol 1996; 155: 1626. Bishoff JT, Lackland AFB, Basler JW, Teichman JM and Thompson IM: Endoscopic subcutaneous modified inguinal lymph node dissection (ESMIL) for squamous cell carcinoma of the penis. J Urol, suppl., 2003; 169: 78, abstract 301. Folliguet TA, Le Bret E, Moneta A, Musumeci S and Laborde F: Endoscopic saphenous vein harvesting versus ‘open’ technique. A prospective study. Eur J Cardiothorac Surg 1998; 13: 662. Avrahami R, Nudelman I, Watenberg S, Lando O, Hiss Y and Lelchuk S: Minimally invasive surgery for axillary dissection. Cadaveric feasibility study. Surg Endosc 1998; 12: 466. Mathevet P, Schettini S, Roy M and Dargent D: Inguinoscopy or video-endoscopic lymph node dissection. Available at www.thetrocar.net. Accessed November 2, 2002. 958 VIDEO ENDOSCOPIC VERSUS STANDARD INGUINAL LYMPHADENECTOMY EDITORIAL COMMENT REPLY BY AUTHORS These authors present a prospective analysis of a novel technique of inguinal lymph node dissection for penile carcinoma. They not only present their new technique, but also compare it to standard radical inguinal lymphadenectomy in the contralateral groin. This novel approach of VEIL may decrease the surgical morbidity that is often attributable to conventional open surgery, such as skin necrosis, wound infections and lymphedema. With any new procedure caution and judgment should be exercised but the authors provide evidence for the safety and feasibility of this technique. In addition, oncological principles appear to be maintained. As with many technological discoveries in the field of urology, this is also an adaptation from other fields. In this case endoscopic techniques described for vascular and axillary lymph nodes are applied to the VEIL technique. This reiterates the fact that we can continue to learn from our colleagues in other disciplines and we should keep an open mind that surgery is a multidisciplinary field. High risk penile cancer can result in high mortality due to inadequate lymph node treatment or serious morbidity due to lymph node dissection. This difficult situation requires creative solutions and may benefit from incorporation of new technologies. A promising new option to consider is magnetic resonance imaging with lymphotropic nanoparticles. This technique may help improve patient selection for inguinal lymphadenectomy, preventing unnecessary procedures or indicating earlier surgery when lymph nodes are not yet palpable.1 Use of minimally invasive techniques, respecting the oncological and anatomical principles outlined for the VEIL procedure, may further reduce complications and sequelae of surgical treatment. 1. Michael A. Palese Minimally Invasive Urologic Surgery Mount Sinai Medical Center New York, New York Tabatabaei S, Harisinghani M and McDougal WS: Regional lymph node staging using lymphotropic nanoparticle enhanced magnetic resonance imaging with ferumoxtran-10 in patients with penile cancer. J Urol 2005; 174: 923.