LABORATORY-1
Biosafety Issues and Basic Techniques in Microbiology
Manvika Sahgal
Objective: To familiarize with biosafety issues in Microbiology laboratory and
instruments
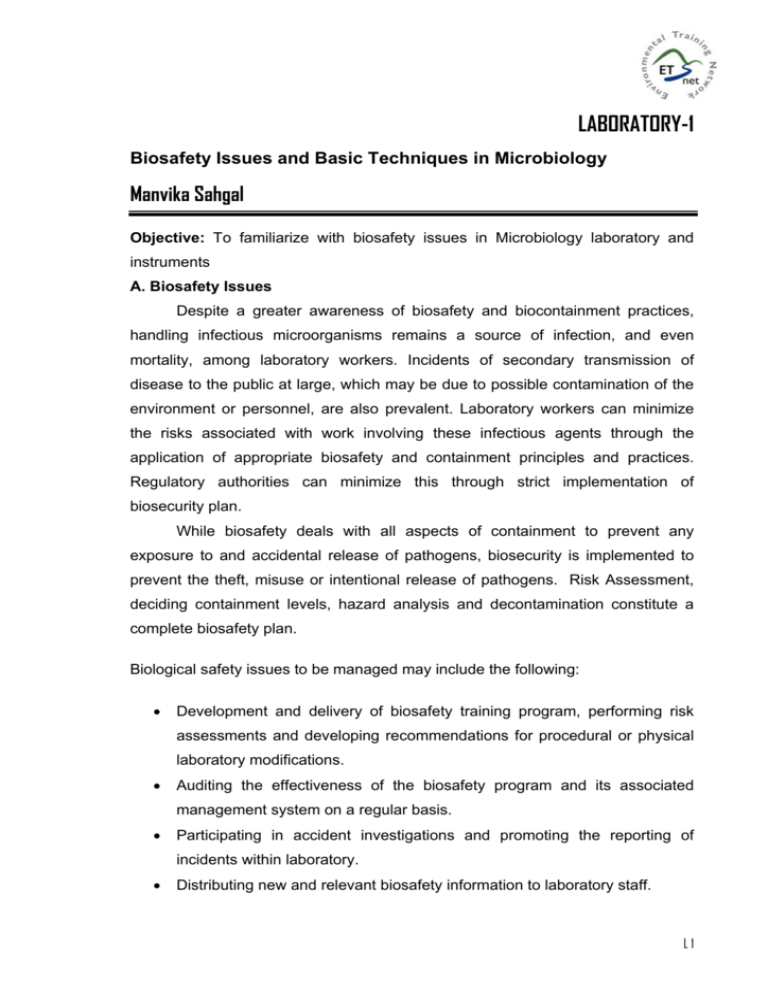
A. Biosafety Issues
Despite a greater awareness of biosafety and biocontainment practices,
handling infectious microorganisms remains a source of infection, and even
mortality, among laboratory workers. Incidents of secondary transmission of
disease to the public at large, which may be due to possible contamination of the
environment or personnel, are also prevalent. Laboratory workers can minimize
the risks associated with work involving these infectious agents through the
application of appropriate biosafety and containment principles and practices.
Regulatory authorities can minimize this through strict implementation of
biosecurity plan.
While biosafety deals with all aspects of containment to prevent any
exposure to and accidental release of pathogens, biosecurity is implemented to
prevent the theft, misuse or intentional release of pathogens. Risk Assessment,
deciding containment levels, hazard analysis and decontamination constitute a
complete biosafety plan.
Biological safety issues to be managed may include the following:
•
Development and delivery of biosafety training program, performing risk
assessments and developing recommendations for procedural or physical
laboratory modifications.
•
Auditing the effectiveness of the biosafety program and its associated
management system on a regular basis.
•
Participating in accident investigations and promoting the reporting of
incidents within laboratory.
•
Distributing new and relevant biosafety information to laboratory staff.
L1
•
Coordinating and monitoring the decontamination, disinfection and disposal
procedures for infectious materials.
•
Coordinating the receipt, shipment and transport within the facility of
infectious material.
•
Maintaining records and secure storage system for all infectious material
entering the facility.
•
Co-ordinating emergency response activities.
•
Maintaining liaison with support and housekeeping staff on matters related
to facility biosafety.
1.
Risk Assessment
A risk group to which an organism falls is based upon the characteristics of
the organism, such as pathogenicity, infectious dose, and mode of
transmission, host range, availability of effective preventive measures and
effective treatment. Four levels of risk have been defined as follows.
•
Risk Group 1 (low individual and community risk)
Any biological agent that is unlikely to cause disease in healthy
workers or animals.
•
Risk Group 2 (moderate individual risk, low community risk)
These pathogens cause human disease but are unlikely to be a
serious hazard to laboratory workers, the community, livestock or the
environment. Laboratory exposures rarely cause infection leading to
serious disease; effective treatment and preventive measures are
available, and the risk of spread is limited.
•
Risk Group 3 (high individual risk, low community risk)
Any pathogen that usually causes serious human disease, results in
serious economic consequences but does not spread by casual
contact from one individual to another. Disease is treatable by
antimicrobial agents.
•
Risk Group 4 (high individual risk, high community risk)
Any pathogen that usually causes very serious human disease, often
untreatable, and may be readily transmitted from one individual to
another, or from animal to human or vice-versa, directly or indirectly,
or by casual contact. In addition to the Risk Group classifications, the
L2
following factors associated with the laboratory operation should also
be examined:
potential for aerosol generation
quantity
concentration
agent stability in the environment
type of work (e.g., in vitro , in vivo , aerosol challenge studies)
use of recombinant organisms
2.
Containment Levels
Risk assessment is a critical step in the selection of an appropriate
containment level for the microbiological work to be carried out. The
containment level is based on the manipulations generally associated with
laboratory scale research and clinical procedures. If a particular procedure,
such as preliminary identification, poses a lower hazard than manipulation
of a live culture, then a lower containment level may be appropriate. An
increase in containment may be required once a facility begins large
scale production (manipulations in volume excess of 10L).The specific
safety procedures are available for large scale production and handling
facility. A hazard analysis may indicate that, because of high pathogenicity,
the route of transmission and the low infectious dose, a particular study
involving volumes of < 10 L may pose a greater hazard than research scale
quantities and therefore may require increased levels
of
physical
and
operational containment.
Four containment levels are described as follows:
Containment Level 1 (CL1) Biological safety cabinets (BSCs) are not
required. Work may be done on an open bench top, and containment is
achieved through the use of practices normally employed in a basic
microbiology laboratory.
Containment Level 2 (CL2) Biological safety cabinets (BSCs) and
centrifuges with sealed rotors or safety cups, appropriate personal
protective equipment (i.e., gloves, laboratory coat and protective
eyewear) must be used. An environmental contamination must be
minimized by the use of hand washing sinks and autoclaves.
L3
Containment Level 3 (CL3) Infectious agents transmitted by the
airborne route have a low infectious dose and can cause serious or lifethreatening disease. An appropriate respiratory protection, HEPA
filtration of exhausted laboratory air and strictly controlled laboratory
access are required.
Containment Level 4 (CL4) Infectious agents have the potential for
aerosol transmission, have a low infectious dose and produce very
serious and often fatal disease; there is generally no treatment or
vaccine available. CL4 emphasizes maximum containment of the
infectious agent by complete sealing of the facility perimeter with
confirmation by pressure decay testing; isolation of the researcher from
the pathogen by his or her containment in a positive pressure suit or
containment of the pathogen in a Class III BSC line; and
decontamination of air and other effluents produced in the facility.
3.
Decontamination
It is a basic biosafety principle that all contaminated materials be
decontaminated
prior
to
disposal.
Decontamination
includes
both
sterilization (the complete destruction of all microorganisms, including
bacterial spores) and disinfection (the destruction and removal of specific
types of micro-organisms). It is the responsibility of all laboratory workers to
ensure the effective use of products for decontamination of materials,
equipment, and samples from containment zones; of surfaces and rooms;
and of spills of infectious materials.
These procedures represent a critical containment barrier which in
case of failure results in occupational exposure to infectious agents and/or
the unintentional release of agents from a containment facility. Employee
infection with M. tuberculosis as a result of exposure to contaminated
waste has been documented. Employees should leave their laboratory
clothing for laundering in a designated area. Employees must be trained in
all decontamination procedures and factors influencing the effectiveness of
the treatment procedure, as discussed briefly below.
(i)
Autoclaves Infectious laboratory wastes (petri dishes, pipettes,
culture tubes, glassware, etc.) can be effectively decontaminated in
L4
autoclave.
The
effectiveness
of
decontamination
by
steam
autoclaving depends upon various loading factors that influence the
temperature to which the material is subjected and the contact time.
Tight-fitting containers do not permit steam penetration. Piling
containers above one another and overloading can result in
decontamination failure.
Monitoring : Ampoules of Bacillus sterothermophilus are sent to the
designated person in each laboratory biannually for validation of the
equipment. Instructions are provided for placement of ampoule in
the autoclave during the run. This ampoule is returned to the
Biological safety agency for incubation to determine if autoclave has
provided a proper microbiological kill. Results are sent back for
maintaining as long as machine is functional
(ii)
Chemical Disinfection. Chemical disinfectants are used for the
decontamination of surfaces and equipment that cannot be
autoclaved, such as specimen containers and clean up of spills of
infectious materials, rooms. The initial choice of a chemical
disinfectant depends upon the resistance of the microorganisms of
concern. The most susceptible are vegetative bacteria, fungi.
Mycobacteria and non-enveloped viruses are less susceptible;
bacterial spores and protozoan cysts are generally the most
resistant. Consideration should also be given to practicability,
stability, compatibility with materials and health hazards. Class of
chemicals (e.g., hypochlorites, quaternary ammonium compounds,
phenolics, iodines, alcohols) could be used as disinfectants.
(iii)
Gaseous Decontamination of Rooms Vaporized hydrogen peroxide
has
been
proposed
as
a
safer
alternative
to
gaseous
decontamination with formaldehyde. 30% liquid hydrogen peroxide
is vaporized to yield approximately 1200 ppm. The vapour breaks
down into nontoxic oxygen and water. Successful gaseous
decontamination requires an ambient temperature of at least 21o C
and a relative humidity of 70%. Biological indicators should be used
to monitor the effectiveness procedure.
L5
(iv)
Liquid Effluent Treatment Systems are used in containment level
4 laboratories for decontaminating liquid waste streams from sinks,
showers, autoclave chambers and other drains. This represents a
secondary treatment system, as no infectious micro-organisms are
disposed off directly into the drain without prior treatment.
Decontaminated liquids released from the treatment system must
meet
all
applicable
regulations
(e.g.
municipal
bylaws
for
temperature, chemical/metal content, suspended solids, oil/grease
and biochemical oxygen demand).
(v)
Irradiation Gamma irradiation (e.g., 60 Co) can be used for the
decontamination of heat-sensitive chemicals and solvents removed
from a containment facility.
(vi)
Incineration has traditionally been the chosen method for
processing anatomical biomedical waste and animal carcasses. In
most cases, wastes to be incinerated have to be packaged and
transported off-site in accordance with territorial legislation. Materials
removed from containment laboratories for off-site incineration
should initially be treated at the containment barrier, preferably by
autoclaving.
4.
Biosecurity Plan
A primary component to a biosecurity plan must be a detailed risk
assessment. The biosecurity risk assessment should review and list the
relevant assets, define the threats,
outline
the
vulnerabilities,
and
determine the counter measures or mitigation strategies specific for each
facility. The biosecurity plan should then address the following
factors:
physical protection; personnel suitability/reliability; pathogen accountability;
and related incident and emergency response.
L6
GENERAL LABORATORY QUALITY- CONTROL PRACTICES
General sterility and cleanliness
Sterility and cleanliness of the laboratory is necessary to ensure the
integrity of samples and analytical procedures
•
Traffic through the laboratory is restricted to those doing work in the
laboratory, especially when analytical work is being done.
•
The tabletops are wiped down with 70 percent ethanol, before and after use.
•
Antimicrobial soap is available at various laboratory sinks to facilitate hand
washing before and after laboratory work.
•
Clean and sterile glassware that is free of detergent residue is crucial to
ensure valid results in microbiology.
•
Dirty dishes are placed separately after use and are not to be stored on
tabletops. Dishes are washed with hot water and laboratory-grade
phosphate-free detergent.
Dishes are rinsed with tap water and then
deionized water.
Autoclaves
Sterilization is the process that eliminates living organisms from substances
or objects. Glasswares should be are wrapped in aluminum foil or paper and
placed in the autoclave for moist heat sterilization. Clean and sterile glassware
are stored in closed cupboards until use. The autoclaves are operated at 15 lb/in2
steam pressure, producing an inside temperature of 121 to 124oC. Do not
overload the autoclave. Autoclave time depends on the type and amount of
equipment as follows: Glassware and up to 250 ml of liquid—15 min
•
500 to 2,000 ml liquid - 30 min
•
Greater than 2,000 ml to 6,000 ml liquid - 15 min per 1,000 ml
•
Greater than 6,000 ml liquid - 90 min
•
Carbohydrate-containing media -15 min (250 ml)
•
Contaminated materials and discarded cultures - 45 to 90 min
Operating temperature and pressure are checked once a week. Heatsterilizing tape is used with each run to identify supplies that have been properly
sterilized and checks the performance of the autoclave. If the autoclave does not
reach the specified temperature, service the autoclave and re-sterilize all
L7
glassware and reagents that were insufficiently sterilized. The autoclaves are
operated using deionized water. At the end of the day, autoclaves are drained.
Twice a month, autoclaves are cleaned with mild soap, rinsed with water, and
drained. The condensate holding tank is drained daily or as needed.
Laboratory water
Aspirator bottles used to store single and triple distilled water are drained
completely and washed with soap solution every week.
Analytical balances
Analytical balances are used for accurate weighing of reagents and
media. They are checked and calibrated annually. Balances must rest on a firm,
level surface. Balance trays are wiped off daily with water or a surface
disinfectant such as 70 % ethanol.
A laminar-flow bench
•
Laminar flow hoods have magnehelic pressure gauges (MAG) that are
used to monitor operation of the hoods. When using, check that the
pressure gauge is
reading at a level approximately equal to the annually
recorded MAG level on the calibration sticker. A significant increase in
pressure indicates that the filters are dirty whereas decrease in pressure
indicates an electrical problem.
•
A laminar-flow bench must be free from contamination by live organisms.
•
The working surfaces of the laminar-flow bench are wiped with 70 %
ethanol before and after use.
•
The ultraviolet lights in the laminar flow bench are cleaned quarterly by
wiping with a soft cloth.
•
Biannually, nonselective agar plates are exposed to airflow in the laminarflow bench. The plates are incubated at 35oC for 24 h and examined for
contamination.
L8
pH meters
With each use of the specific conductance, pH, or turbidity meter, calibrate
the instrument according to the manufacturer’s instructions. Use a calibrated
solution that is within the range of the water sample to be measured. Label
specific conductance and pH buffer solutions with the date opened and discard
working solution weekly. Each piece of equipment has daily logbook; record all
calibrations in the appropriate logbook.
Micropipettors
Micropipettors are used for the accurate delivery of small volumes.
Pipettors are cleaned, calibrated and adjusted annually, if necessary.
Vacuum pump
The vacuum pump is mainly used for membrane filtration. The oil is
changed in the pump every 2 years.
Incubators, water baths, refrigerators, freezers, and thermometers
The temperatures of the laboratory incubators, water baths, refrigerators,
and freezers are checked quarterly with laboratory. During period of heavy use,
the temperatures are checked and recorded weekly. Deep freezers (-700 C) are
used to store samples and microbiological cultures. Its filter is cleaned and fans
behind the filter are checked. Water baths are filled with 50% deionized water and
50% tap water and are cleaned with mild soap quarterly, or more often as
needed.
Microscope
The microscope is used for general laboratory work. The microscope is
cleaned and the ocular micrometer is calibrated yearly.
Centrifuges
They
are
used
for
processing
bacterial
extractions,
purifications,
concentrations, and phase separations.
•
Each run of the centrifuge is recorded in the centrifuge log book.
•
The temperature is monitored quarterly with the digital thermometer
(acceptance criteria is 4+ 3ºC).
•
The buckets are cleaned with soap and water quarterly.
•
Rotors and adapters are checked for deterioration, as needed.
•
Lubrication is done annually, or as needed.
L9
Master Cycler
The Master Cycler is used to amplify bacterial DNA through a series of
temperatures changes. It detects enteric viruses in water by reverse-transcriptase
polymerase chain reaction (RT-PCR). It is also used in bacterial source tracking
methods.
•
The temperature is monitored twice a year.
L 10
LABORATORY-2
Media Preparation & PA Coliform Test
Mahejibin Khan
Part-I Preparation & Sterilization of Media
Objective: To prepare & sterilization the nutrient media for use in water analysis
Principle: A medium serves as a source of nutrient for in-vitro growth of various
types of microbes in the laboratory. Each medium has four basic constituents-C,
N, H, & O. Besides this, some other macro and microelements are also required
by fastidious organisms.
a)
Carbon source: Based on carbon requirement, microorganisms can be
divided into two categories
i)
Autotrophs-require CO2 as sole carbon source.
ii)
Heterotrophs-require organic form of carbon.
b)
Nitrogen: Required for synthesis of amino acids and proteins.
c)
Hydrogen & Oxygen: Forms part of many organic compound
d)
Sulphur: Biosynthesis of amino acids like cysteine, cystine, methionine.
e)
Phosphorous: Nucleic acids and ATP
f)
Mineral salts: Macroelements like Sodium & Ferrous help the enzyme while
microelements like Zinc, Manganese, Cobalt, Molybdenum, Copper are
required in trace quantity for activation of enzymes.
g)
Energy source: Light or chemical compounds.
Types of media
Media can be of two types:
a). Complex nutritional media: not defined quantitatively or qualitatively e.g.
nutrient agar
b). Chemically defined media: Media defined qualitatively as well as
quantitatively e.g. defined media.
On the basis of physical condition, media can be categorized into three categories as:
a). Solid media: Media having 2% agar-agar (solidifying agent)
L 11
b). Semi-solid media: Contains 0.75-1% agar-agar
c). Liquid media: Media not having solidifying agent i.e. agar-agar
Requirements:
Autoclave
250 ml. conical flasks
Weighing balance
Butter paper
Spatula
Laminar air flow bench
Petriplates
Measuring cylinder
Test tubes
Test tube stand
Cotton bundle
EMB Agar
Pepton
Lactose
Sucrose
K2HPO4
Eosin Y
Methylene blue
Agar
Distill water
g/l
10 g
5g
5g
2g
0.4
0.06
20.00
1000 ml
MacConkey Agar
Peptone
Lactose
Bill Salts
Sodium chloride
Neutral Red
pH
g/l
20.0
10.0
5.0
5.0
0.075
7.4
Alternatively, Hi-media supplies readymade EMB & MacConkey agar and
depending upon the grade, an amount of powder (as mentioned on the container)
is dissolved in 1 l of distilled water and autoclaved to get the specific agar medium
ready.
Methodology
Preparation of broth medium (test tubes)
1) Prepare the broth media as given above.
2) Transfer nutrient broth (liquid) to the test tubes before sterilization to
minimize chances of contamination while transferring after sterilization.
3) Test tubes are ready for sterilization after placing cotton plugs.
L 12
Preparation of agar slants (test tubes)
1) Add 2% agar-agar to the respective broth.
2) Homogenise the medium by heating it on hot plate or microwave oven.
3) Transfer 5-10 ml of Nutrient agar into test tubes for sterilization & put cotton
plugs.
4) Sterilize these by autoclaving. After autoclaving the tubes are placed at an
angle of 45ºC and allowed to solidity so that the slants are prepared.
Preparation of EMB or MacConkey agar for petriplates
1) Prepare respective media as given above.
2) Cover the conical flask with cotton plug and the flask is ready for
sterilization after covering the cotton plug with paper.
Note:
1) Sterilization in all three cases above is carried out at 15 lb pressure for
20-30 min.
2) Check the dye strip after sterilization to ensure proper sterilization of media.
Observations and result
(to be filled in by trainees)
QUESTIONS:
1. What is a complex medium?
2. Why are buffers added to the growth media for microbes?
3. How can the temperature in the autoclave go above boiling temperature of 212 F?
4. Why do you have boil the agar solution BEFORE dispensing it into tubes?
5. At what temperature does agar solidify?
L 13
Part-II PA Coliform Kit (HiMedia Laboratories)
A qualitative test to detect the presence or absence of coliform bacteria in water
for treatment plants or distribution systems.
Material Provided
1 sterile disposable bottle
= 100 ml capacity
Dehydrated Medium (PA broth)
= 3x Concentration
Ziplock bag
= 1 No.
Procedure:
Collect 100 ml water to be tested in ziplock bag and transfer to sterile disposable
bottle. Add entire quantity of dehydrated medium (PA broth) slowly to water by
swirling to dissolve the powder completely. After dissolution, incubate the bottle
for 24-48 hr. at 30-350C. Observe the colour change indicating the presence of
coliform bacteria.
L 14
LABORATORY-3
Microbiological Analysis of Water and Wastewater
Lakshmi Tewari
Objective: To test bacteriological quality of drinking water and microbial analysis
of wastewater
Principle:
With
increasing
industrialization,
water
sources
available
for
consumption and recreation have been adulterated with industrial as well as
animal and human wastes. As a result, water has become a formidable factor in
disease transmission. It may act as a potential common source of pathogenic and
non-pathogenic microorganisms. Water purification is, therefore, the most
important measure available for ensuring public health. In India more than 70% of
the epidemic emergencies are either water borne or are water related. Over 80
genera of bacteria that are non-pathogenic for humans have their natural habitat
in water. Several enteric bacteria, coliforms and several other pathogenic bacteria,
(Pseudomonas,
Streptomyces,
Serratia,
Vibrio
Aeromonas,
cholerae,
Enterobacter,
Cryptosporidium,
Escherichia
Yersinia
coli,
enterocolitica,
Campylobacter sp., streptococci etc.)
Water in relation to human consumption is classified as (i) the potable water
(drinking water) and (ii) the unpotable water or waste water (sewage). Potability
refers to the pollution level or drinking quality of water. It is therefore, highly
desirable that the water, before its wide circulation for consumption purposes,
should be undergone for proper bacteriological testing. Potable water can be
defined as any water that is clear, free from undesirable flavours, odors, of
reasonable temperature, neither corrosive nor scale forming, free from minerals
that could produce undesirable physiological effect and does not contain
pathogenic microorganisms capable of causing human diseases. World Health
Organization (WHO) has recommended following bacteriological standards for
treated water:
(i)
Coliform count in any sample of 100 ml should be zero or in 90%
samples examined throughout any year.
L 15
(ii)
Coliform organisms not more than 10/100 ml water samples shall be
present in any water and
(iii)
Coliform organisms should not be detectable in 100 ml of any two
consecutive samples or more than 50% of the samples collected for the
year.
Microbiological analysis of water:
The bacteriological analysis of water is done primarily to determine its potability
i.e. fitness for drinking and for waste-water to determine the most probable number
of bacteria in the sample.
The coliforms (E. coli & related organisms), Streptococcus faecalis and
Clostridium perfringens which are normal inhabitants of the large intestine of
animals and humans enter water supplies through faecal contamination. Presence
of any of these bacterial species in water is evidence of sewage or faecal
pollution. Techniques are available by which presence of these specific groups
can be easily identified. However, detection of specific pathogenic organisms in
water supply is much more difficult because of their small number. Therefore, E.
coli, which outnumbers the pathogens in faecal discharges of animals & human
beings, can serve as good indicator bacteria. Thus E. coli is used as an indicator
to assess contamination from sewage in case of drinking water; while
Enterobacter aerogenes, which originated from soil or plant materials, and
contaminate water can be easily distinguished from E. coli. Higher number of E.
coli may indicate high probability of pathogens presence.
The routine bacteriological examination of water involves three types of tests:
1) The standard plate count (total bacterial count) test.
2) Test for coliforms (the standard bacteriological test)
3) Membrane filter techniques
Requirements:
Lactose broth
Test tubes
Inoculating loop
Durham tubes
EMB agar (readymade, Hi-media)
L 16
IMViC Hi-media test kit
Water sample
Bacterial filters
Filtration assembly
Methodology:
I. The standard plate count method for total bacterial counts (ACC):
This test provides an estimate of the total number of bacteria in a water
sample which will grow and develop in a particular culture medium at 370C under
laboratory conditions.
I) Water sample is first diluted with sterile water and then plated on agar
medium (Cappuccino and Sherman, 1996).
II) The bacterial colonies developed on plates are counted to give the total
bacterial counts in the sample under test.
III) Total cfu counts/ml are calculated using the following formula:
cfu counts/ml = Dilution factor of original sample × No. of colonies
Water of good quality has low bacterial counts of less than 100/ml
II. Tests for Coliforms for assessing water safety (Drinking and Swimming
pool water):
Two procedures are commonly used to test for coliforms in water sample
I). The Most probable number (MPN) technique and
II). The Membrane filter (MF) technique.
The conventional test (used as standard analysis test) for the detection of faecal
contamination in water was given by Eijackman and is based on determination of
most probable number of coliforms.
Assessment of the microbiological load in different water samples viz. drinking
water (municipal water supply), surface water, waste water, ground water,
swimming pool water, mineral water etc. include
a). Total Aerobic Colony Counts (Heterotrophic Plate Count) (ACC/HPC),
b). Total Coliform Count (TCC),
c). Faecal Coliform Count (FCC) and
d). Faecal Streptococcal Counts (FSC).
L 17
These indicator parameters should be studied by standard methodologies
recommended by the American Public Health Association (APHA) or WHO.
In case of swimming pools, water is to be examined monthly for presence of
indicator microorganisms. Samples should be tested for aerobic colony counts
(ACC) or plate count, coliform (both FC & NFC), E. coli, Pseudomonas
aeruginosa. The aerobic colony count should normally be 10 or less cfu/ml of pool
water. Coliforms are sensitive to disinfectant and should be absent in 100 ml of
pool water. Pseudomonas aeruginosa can grow within untreated water and forms
biofilms. It can cause skin; ear and eye infections when present in large number
and outbreaks of skin infections have been linked to swimming pool and spa
pools. Well operated pools should usually not contain P. aeruginosa, if the count
is 10 cfu/100ml, repeat testing and filtration and disinfection processes should be
done and if counts exceed 50/100 ml (high contamination) the pool should be
closed to prevent illness in pool areas. Following should be considered as gross
contamination of swimming pool water:
a.
b.
> 10 E.coli cfu/100 ml in combination with one or both of the following:
1.
An unsatisfactory aerobic colony count (> 10 cfu/ml)
2.
An unsatisfactory P. aeruginosa count (> 10 cfu/100ml)
> 50 P. aeruginosa / 100 ml in combination with high aerobic colony count
(> 100/ml)
Additional microbiological testing in the event of an outbreak of illness
associated with a swimming pool may be considered necessary and tests should
be carried out quarterly for Legionella, Staphylococcus aureus, Cryptosporidium,
Giardia (Fig.3.2 a-b) and viruses.
I. Most Probable Number (MPN) Technique for Detection of Coliforms:
This test includes (a) presumptive test (b) confirmatory test and (c) completed
test. Schematic presentation of these tests is given in Fig-1.
A. Presumptive Test:
(i) Inoculate each of 3 test tubes containing 10.0 ml of double strength lactose
broth of a set aseptically with 10.0 ml of water sample.
(ii) Similarly inoculate 1.0 ml and 0.1 ml of water samples into each of three small
tubes of 2nd and 3rd sets respectively containing single-strength lactose broth
using aseptic conditions.
L 18
(iii) Incubate all tubes at 370C for 2 days.
(iv) Observe for gas production after 24 and 48 hours. The presence of gas in any
tube after 24 hr is a positive presumptive test. Find out number of tubes in each
set showing gas production and determine MPN counts /100 ml of the water
sample by comparing with Mac Greedy Chart (Annexure-IV) following the
standard methods for examination of water and waste water given by APHA.
The formation of gas during a second 24-hr period is a doubtful test. The absence
of gas formation after 48 hr incubation shows negative presumptive test indicating
that the water supply does not contain coliforms.
B. Confirmed Test: This test should be applied to all samples that give a positive
or doubtful presumptive test.
(i) From the lactose-broth tubes showing positive presumptive test with smallest
water sample, streak a plate of Eosine-methylene blue (EMB) agar
(ii) Incubates at 370C for two days.
(iii) If typical dark coloured colonies with metallic sheen develop on the plate within
this period, the confirmed test can be considered positive. The colonies of E.coli
are small and flat, and show a definite metallic green sheen. While Enterobacter
aerogenes also grows on EMB agar but it does not produce as much acid as E.
coli. Thus, E. aerogenes colonies are mucoid and slightly pink. Endo-agar is
another selective medium that can be used in the confirmatory test.
C. Completed Test:
i).
From the EMB-agar plates pick up one colony, which is most likely to be
organism of coliform group (E. coli), transfer half of the colony on agar-slant
and the other half to lactose-broth tube.
ii).
Incubate the tubes at 370C for two days.
iii).
From agar-slant, make a slide and perform gram staining and spore
staining.
iv).
Observe lactose broth tubes for gas production. Gram (-), non spore
forming, short rods in the agar culture constitute a positive test, showing
presence of coliform group of bacteria, and indicating that the water sample
was polluted.
L 19
II. Biochemical tests for Differentiation of Faecal (Escherichia coli) and NonFaecal (Enterobacter sp.) coliform present in water samples: IMViC Test:
Since, E. coli and E aerogenes bear a close resemblance to each other in their
morphological and cultural characteristics, four biochemical tests are performed to
differentiate them. These tests are collectively known as the IMViC tests. Each
letter of IMViC stands for a reaction/property or a product, which can be used for
both to characterize E. coli and to differentiate it from E. aerogenes (I - indole
production, M - methyl red test, Vi - Voges-Proskauer reaction, and C - citrate
utilization). Colonies from the nutrient agar slant of the completed test, described
above, are used to inoculate Hi Media IMViC test kit with 50 microlitre/loopful of
culture and the kit is incubated at 370C for 24-48 hours.
1. Indole test (I): E. coli produce/synthesize an enzyme, tryptophanase, which
forms indole, pyruvic acid and ammonia from tryptophan, whereas E. aerogenes
cannot catabolize tryptophan and do not produce indole.
2. Methyl red test (M): Methyl red is an acid-base indicator that turns red in a
slightly acid medium. Both the organisms produce acid from glucose, E. coli
produce large amount of acids thus a low pH, which turn the indicator (methyl red)
to red colour
whereas E. aerogenes cultures produce only small amounts of
organic acids and consequently do not produce the colour change.
3. Voges-Proskauer (Vi) test: It detects the presence of acetyl methyl carbinol.
E. coli do not produce acetyl-methyl-carbinol in glucose peptone medium but E.
aerogenes do.
4. Citrate utilization test (C): E. aerogenes is capable of utilizing sodium citrate
as its sole source of carbon, i.e. it will grow in a chemically defined medium in
which sodium citrate is the only source of carbon. E. coli does not grow under
these circumstances.
(ii) Membrane Filter Technique:
This technique has become common and is preferred. It involves the use of a
sterile filter disk having pores fine enough to retain bacteria (</= 0.22µ). The filter
disk is placed in filtration unit, and a measured volume of water is filtered through
it. The bacteria retained on the surface of the filter disk are removed and placed
upon the surface of Eosin Methylene Blue agar medium or on a sterile absorbent
pad that has been previously saturated with an appropriate broth culture medium
L 20
in Petri dish and incubated. The colonies develop on the surface of the membrane
wherever bacteria are entrapped. Eosin Methylene Blue culture medium, which is
both selective and differential medium for coliforms is used. The dark colour of
colonies is characteristics of coliform, which are counted and then from this value
the total number of coliforms in original water sample can be determined.
References:
A report of Department of Rural Development, Government of India on Executive
guidelines for imolementation of water quality testing laboratories. (1991)
Atlas, Ronald M. 1989. Microbiology Fundamentals and Applications. IInd Edition.
Macmillan Publishing Company, New York. Pp. 437-456.
Cappuccino, James, G. and Sherman, H. 1996. Microbiology: A laboratory
manual, IV ed. The Benjamin/cuming Publishing Inc., New York. pp 13.
CD Alert, Cholera: need for a constant and continuous vigil, 4, Directorate of
General Health Services, New Delhi, 2000, pp. 1-8.
Kamal, Rao, G. P., and Modi, D.R. 2005. Concepts of Microbiology. International
Book Distributing Co. pp. 289-314.
Madigan, Michael T. and Martinko, John M. 2006. Brock Biology of
Microorganisms. XI Edition. Pearson Prentice Hall, U.S.A. pp. 906-920.
May 1990
Sharma, S., Singh, I., and Virdi, J.S. 2003. Microbial contamination of various
water sources in Delhi. Current Science, Vol. 84 (11), pp. 1398-1399
Standard method for examination of water and waste water, American Public
Health Association (APHA), Washington DC, USA, 19th edn, 1995.
Szewzyk, U., Szewzyk, R., Manz, W. and Schleifer, K.-H., Annu. Rev. Micrabiol.,
2000, 54, 81-127.
The World Health Report. Fighting Diseases, Fostering Development, WHO,
Geneva, 1996.
L 21
Fig 3.1: Standard method for bacteriological water analysis
A
Fig.3.2.
B
C
Photograph
showing
microbial
contaminants:
A-Giardia;
B-Cryptosporidium oocysts; C-Coliform colonies growing on
membrane filter.
L 22
LABORATORY-4
Enumeration of Bacteria in Water Sample by Membrane Filtration
Technique
Manvika Sahgal & Mahejibin Khan
Objective: To determine the population of coliforms in the water sample
Materials required: Water sample, 0.45 µm bacteriological filter paper, filtration
assembly, prepared petriplates of specific medium
Principle: A measured amount of sample is filtered through a membrane with a
pore size of about 0.45 µm, which traps the bacteria on its surface. The
membrane is then placed on a thin absorbent pad that has been saturated with a
specific medium; a modified Endo medium for total coliforms, a modified
Enterococcus-agar medium (KF agar) containing azide for fecal streptococci, and
faecal colifrom medium (M-FC broth) with incubation at 44.5ºC for faecal
coliforms. After incubation in a small petri plate, the colonies are counted under
low magnification.
The success of this method depends on using effective differential or
selective media that will enable easy identification of colonies. This method has
advantages over the traditional water analysis procedure because it is more direct
and quicker (giving results in 18-24 h) and can easily test large volumes of water
(hence yielding more accurate results).
Procedure
Total Coliform Test
Attach the filter holder to the rubber stopper, insert into the vacuum flask, and
connect the flask to the vacuum line or aspirator.
1)
Using sterile forceps, transfer a sterile membrane filter to the platform
base of the filter unit. Place the filter with ruled side up.
2)
Place the matched funnel unit over the filter disc, making sure that it is
clamped in place firmly by the scissors-type clamp.
3)
Line up three small Petri dishes, labeled with the three sample volumes
to be used and your initials.
L 23
4)
Pour about 20 ml of sterile buffered water into the funnel before adding
your sample.
5)
Shake your bottle of sample vigorously.
6)
Measure out the volume of sample to be tested with a 10 ml pipette or a
graduated cylinder and introduce it into the funnel.
7)
Rinse the measuring vessel twice with an amount of sterile buffered
water that is equal in volume to the sample and add this water to the
funnel (this rinses cells from the measuring vessel).
8)
Turn on the vacuum motor or water aspirator and allow all the liquid to
pass through the filter into the flask.
9)
Leaving the vacuum on, rinse the funnel with a volume of sterile
buffered water that equals the total amount of liquid filtered; pour this
rinse water onto the inside wall of the funnel so that a swirling wash
results.
10) Allow the rinse water to pass entirely through the filter and then repeat
with a second equal rinse. After all the water has passed through the
filter, allow the vacuum to run for 1 min or until the filter appears dry.
11) If you are using the Millipore specialized 47 mm petri dishes and other
materials in the water testing kit, prepare one of the dishes as follows:
a).
Remove a presterilized pad from the package of pads and
filters with the aid of sterile forceps and place it in the perti
dish.
b).
Take an ampoule of sterile Endo medium and place it in an
ampoule breaker.
c).
Break the ampule and pour its contents onto the presterilized
pad.
12) Turn off the vacuum source and move the membrane filter with flamed
sterile forceps to the Endo medium in a small Petri dish.
13) Push the membrane against the far side of the petri dish and onto the
medium and roll it onto the medium to avoid trapping air bubbles under
the membrane. The medium will diffuse from the pad through the filter
to support the growth of bacteria on the upper surface of the filter.
14) Incubate at 37ºC for 22-24 h.
L 24
15) Examine the plates and note colonies that are pink or dark red with a
golden green metallic sheen. Count plates that contain 20-80 such
colonies of coliforms and no more than 200 colonies of all types.
16) Calculate the numbers of organisms per 100 ml using the formula:
indicator count per 100 ml = 100 ×
total number of colonies coutned
number of ml of the sample tested
Fecal Coliform Test
1)
Attach the filter holder to the rubber stopper, insert into the vacuum
flask, and connect the flask to the vacuum line or aspirator.
2)
Using sterile forceps, transfer a sterile membrane filter to the platform
base of the filter unit. Place the filter with ruled side up.
3)
Place the matched funnel unit over the filter disc, making sure that it is
clamped in place firmly by the scissors-type clamp.
4)
Line up three small Petri dishes, labeled with the three sample
volumes to be used and your initials.
5)
Pour about 20 ml of sterile buffered water into the funnel before
adding your sample.
6)
Shake your bottle of sample vigorously.
7)
Measure out the volume of sample to be tested with a 10 ml pipette or
a graduated cylinder and introduce it into the funnel.
8)
Rinse the measuring vessel twice with an amount of sterile buffered
water that is equal in volume to the sample and add this water to the
funnel (this rinses cells from the measuring vessel).
9)
Turn on the vacuum motor or water aspirator and allow all the liquid to
pass through the filter into the flask.
10) Leaving the vacuum on, rinse the funnel with a volume of sterile
buffered water that equals the total amount of liquid filtered; pour this
rinse water onto the inside wall of the funnel so that a swirling wash
results.
11) Allow the rinse water to pass entirely through the filter and then repeat
with a second equal rinse. After all the water has passed through the
filter, allow the vacuum to run 1 minute or until the filter appears dry.
L 25
12)
a) Remove a presterilized pad from the package of pads and
filters with the aid of sterile forceps and place it in the perti dish
b) Using a 10 ml pipet, add 2 ml M-FC broth to the surface of
each absorbent pad.
c) Aseptically transfer the membrane filter to the top of the
absorbent pad.
13) After snapping the Petri plates shut, seal them with waterproof tape,
insert them into a waterproof plastic bag, and incubate them in a
44.5ºC water bath for 22 h. Be sure to sink the bags beneath the
surface.
14) Count blue-colored colonies with characteristics resembling coliforms.
Use the plate containing 20-60 colonies.
Fecal Streptococcus Test
1)
Attach the filter holder to the rubber stopper, insert into the vacuum
flask, and connect the flask to the vacuum line or aspirator.
2)
Using sterile forceps, transfer a sterile membrane filter to the platform
base of the filter unit. Place the filter with ruled side up.
3)
Place the matched funnel unit over the filter disc, making sure that it is
clamped in place firmly by the scissors-type clamp.
4)
Line up three small Petri dishes, labeled with the three sample
volumes to be used and your initials.
5)
Pour about 20 ml of sterile buffered water into the funnel before
adding your sample.
6)
Shake your bottle of sample vigorously.
7)
Measure out the volume of sample to be tested with a 10 ml pipette or
a graduated cylinder and introduce it into the funnel.
8)
Rinse the measuring vessel twice with an amount of sterile buffered
water that is equal in volume to the sample and add this water to the
funnel (this rinses cells from the measuring vessel).
9)
Turn on the vacuum motor or water aspirator and allow all the liquid to
pass through the filter into the flask.
L 26
10) Leaving the vacuum on, rinse the funnel with a volume of sterile
buffered water that equals the total amount of liquid filtered; pour this
rinse water onto the inside wall of the funnel so that a swirling wash
results.
11) Allow the rinse water to pass entirely through the filter and then repeat
with a second equal rinse. After all the water has passed through the
filter, allow the vacuum to run 1 min or until the filter appears dry.
12) If you are using the Millipore specialized 47 mm petri dishes and other
materials in the water testing kit, prepare one of the dishes as follows:
a) Remove a presterilized pad from the package of pads and
filters with the aid of sterile forceps and place it in the perti
dish.
b) Take an ampule of sterile Endo medium and place it in an
ampoule breaker.
c) Break the ampoule and pour its contents onto the
preseterilized pad.
13) Aseptically transfer the three membrane filters to the top of the
absorbent pad of each plate.
14) Incubate the prepared plates for 48 hours at 37ºC.
15) Examine the plates for colonies that are light pink and flat and for
smooth, dark-red colonies with pink margins. Counts the plate that
has 20-100 colonies.
Collect the class data for fecal coliform (FC) and faecal streptococci (FS)
and calculate the ration FC/-FS:
number of fecal coliform per ml
number fecal streptococ ci per ml
An FC/FS greater than 4 shows strong evidence of pollution derived from
human waste. An FC/FS ratio less than 0.7 indicates pollution derived
predominantly or entirely from livestock or poultry waste. If the ratio is between
2 and 4, it suggests a predominance of human waste in mixed pollution. A ratio
of 1 to 2 cannot be interpreted; it is then suggested that a sample nearer the
point source of pollution be taken.
16) Record your results on the report sheet.
L 27
LABORATORY-5
Assessment of Quality of Potable Water
S.P. Singh
PART 1
Determination of Hardness of Water
Hardness of water is due to presence of bi-carbonates, chlorides and
sulphates of calcium and magnesium. Hardness is of two types.
1. Temporary:
This is due to presence of bi-carnontaes of calcium and magnesium and
can be removed by easy methods like boiling and addition of lime.
2. Permanent:
This is due to presence of chlorides and sulphates of calcium and
magnesium. It can be removed by adding of sodium carbonate and permuttit
process but can not be removed by boiling.
Total hardness is defined as the sum of the calcium and magnesium
concentrations, both expressed as calcium carbonate, in milligrams per litre.
The WHO in its publication “International Standards for drinking water
(1971) has recommended that hardness in water should be expressed in terms of
milli equivalents per liter (mEq/l) One m Eq/1 of hardness producing is equal to 50
mg CaCO3 (50 ppm) in one litre of water. The terms “Soft” and “Hard” may then
be used as follows.
Quantity
MEq/L
Ppm CaCO3
Soft
Less than 1 mEq/L
50
Moderately Hard
1 to 3 mEq/L
50-150
Hard
3 to 6 mEq/L
150-300
Very Hard
Over 6 mEq/L
Over 300
The drinking water should be moderately hard. The highest desirable level
of hardness of drinking water suggested by WHO in 2mE/L (100 ppm). The
question of softening of water arises if the hardness exceeds 3 m Eq/l.
L 28
Principle:
Ethylene diamine tetracetic acid (EDTA) or its sodium salts form a chelated
soluble complex whe added to a solution of certain metal cations. If a small
amount of a dye such as Eriochrome black T or Calmagite is added to an aqueous
solution containing Ca and Mg ions at pH of 10.0±0.1, the solution becomes wine
red. If EDTA is added as a titrant., the calcium and magnesium will be complexed.
The solution turns from wine red to blue, making the end point of the titration.
Magnesium ions must be present to yield a satisfactory end point to insure this, a
small amount of complex-matrically neutral magnesium salt of EDTA is added to
the buffer, this automatically introduces sufficient Mg.
The sharpness of endpoint increases with increasing pH. The specified pH
of 10.0±0.1 is quite satisfactory, a limit of 5 min is set for the duration of titration to
minimise CaCo3 percipitation.
Disadvantages of hardness of water are:
A. With industrial and economic point of view:
I. The hardness in water causes great wastage of soap while washing
of cloths
II. When hard water is heated, the carbonates are precipitated and
bring about furring in the boilers (scale formation). The life of boilers
is reduced and much more fuel is required to raise the steam.
B. From health point of view:
I. It causes stone formation in the vital organs e.g. gall stone and renal
calculi
II. Indigestion and constipation are other problems
III. Hard coat in horses
Material required
Burette, pipette, beaker, Total hardness indicator tablet (calmagite or
eriochrome black T), Ethylene di-amino tetra acetic acid (EDTA) N/50 and Amonia
buffer.
Method:
1. Take N/50 ethylene dia-amine tetra acetic acid in the burette
2. Transfer 100 ml of water in a beaker
3. Add 2 ml ammonia buffer
L 29
4. Dissolve 1 total hardness indicator tablet in the above water sample
5. Add drop by drop EDTA from the burette
6. The end point will be when colour of water becomes blue
Calculation
Degree of hardness (in ppm or mEq/l.) =
Volume of N/50 EDTA used x 1000
Volume of water taken
Interpretation:
Drinking water should be moderately hard i.e. 1-3 mEq/l.
L 30
PART 2
Chlorination of water and its detection
Chlorine treatment as a means of purification is applied to public water
supplies. Treatment with chlorine, whether in the form of gas or as sodium
hypochlorite solution, will destroy all forms of bacteria and sufficient to ensure an
excess of free or combined residual chlorine after the bacteria and organic matter
have been destroyed. In addition to its use for sterilizing drinking water,
chlorination also provides one of the most favoured methods for the treatment of
swimming water.
The residual chlorine to extent of between 0.2 and 0.5 parts per million in water is
considered to give adequate purification. For chlorination to be fully effective the
water must be maintained between pH of 7.2 and 7.6. If pH value is less than 7.0
sodium carbonate should be added and if it is higher than 8.0, hydrochloric acid
should be added.
To find out efficient chlorination the examintion of water should be made for
residual cholorine content. For this purpose, the BDH “Chlorotex” reagent
provides a simply performed but accurate test which could be easily conducted by
persons without chemical knowledge or experience.
Chlorinated water mixed with chlorotex reagent produces a colour which
varies in intensity and shade according to the proportion of residual chlorine
present in treated water. The following are the indications of various colour
shades developed with chlorotex reagent:
Parts of residual
chlorine per million of
water
White and milky with blue None
fluorescence
0.1
Faintly pink and slightly milky
Pink
0.2
Indication
Colour
Red
0.5
Water
insufficiently
chlorinated
Water
sterile
and
suitable for use, taste is
not altered
Purple
0.6
Too
Blue
1.0
present
much
chlorine
Taste of water becomes
objectionable
L 31
Chlorine demand and residual chlorine
When chlorine is added to a solution containing other forms of protein, it
will react with non living proteins just as readily as with the bacterial protein. The
quantities of chlorine thus combining with any substances in water with in arbitrary
time usually 5, 10 or 30 min are spoken as the chlorine demand. In the treatment
of water, sufficient quantity of chlorine is added to satisfy this demand and
additional amount sufficient to destroy undesirable organisms.
The chlorine left in water after satisfying the chlorine demand is spoken as
residual chlorine.
It has been found that after satisfying the chlorine demand, 0.1 to 0.2 ppm
of chlorine is adequate to accomplish the purification of water.
Formation of THM (Tri halo methanes)
Reaction of chlorine with certain organic compound such as humic
substances and alike to produce chloroforms and related chloro-organo
compounds (Carcinogen in nature).
To Control these, chlorine should be applied to water with lowest possible
organic content. Precholrination should be avoided. Chlorination is done after
coagulation sedimentation and filtration of water. In order to avoid THM
production, other disfinctants as ozone, chlorine-dioxide or chloramine are
preferred.
Material required:
Measuring cylinder, pippette, chlorotex reagent, colour chart.
Method:
1. Transfer 5 ml of the chlorotex reagent accurately measured by means
of a pipette to one of the graduated cylinders.
2. In another cylinder measure exactly 50 ml of water to be examined.
3. Pour this into the first cylinder on top of the reagent
4. After mixing with the glass stirring rod, allow to stand for exactly one
minute
5. Compare the colour produced with the tints on the chlorotex colour
charts.
L 32
Interpretation:
Colour
White and milky colour
Parts of residual chlorine per
million part of water
None
Faintly pink and slightly milky
0.1
Pink
0.2
Red
0.5
Purple
0.6
Blue
1.0
L 33
PART 3
Determination of pH of water
Measurement of pH is one of the most important and frequently used tests
in water chemistry. Practically every phase of water supply and waste water
treatment e.g. acid-base neutralization, water softening, precipitation, coagulation
and disinfection and corrosion control is pH dependent. pH is used in alkalinity
and CO2 measurements and many other acid-base equilibria. At a given temp.,
the intensity of the acidic or basic character of a solution is indicatedby pH or
hydrogen ion activity. Alkalinity and acidity are the acid and base neutralizing
capacities of water and usually are expressed as milligrams of CaCO3 per litre.
Buffer capacity is the amnoung of strong acid or base, usually expressed in moles
of a 12 sample by 1 unit.
pH is defined by Sorenson is – log (H) it is the intensity factor of acidity.
Use of the term pH assumes that the activity of the hydrogen ion aH+ is being
considered.
Natural waters usually have a pH values in the range of 4 to 9 and most are
slightly basic because of presence of bicarbonates and carbonates of the alkali
and alkaline earthy metals.
Material required:
Two buffer solutions of known pH, pH meter.
Method:
1. First standarize the pH meter with the buffer solution of known pH
2. Wash the electrodes and dry it’
3. Dip the electrodes in another buffer solution of known pH. The pH meter
should give exactly the same reading equivalent to the pH of the buffer
solution. This means that the pH meter has been standardized
4. After washing and drying the electrodes dip them in the water sample and
record the reading from pH meter.
Interpretation
According to BIS, the portable water should in pH range of 6.5-8.5.
L 34
LABORATORY-6
Microbiological Characterization of Coliform in Water Sample
M. Sahgal & Mahejibin Khan
Objective: To characterize the coliforms present in water sample using specific
media growth.
Procedure
(i)
From the lactose-broth tubes showing positive presumptive test with
smallest water sample, streak a plate of Eosine-methylene blue (EMB) agar
(ii)
Incubates at 370C for two days.
(iii) Growth of typical dark coloured colonies with metallic sheen confirms the
presence of E. coli. The colonies of E.coli are small and flat, and show a
definite metallic green sheen. While Enterobacter aerogenes also grows on
EMB agar and its colonies are mucoid and slightly pink. Step II Purification
of the bacterial culture isolated.
Material Required:
Water sample, EMB agar, Petri plates
Principle:
This test is applied to all the samples that give a positive test in PA coliform
test and is done to confirm the presence & characterize the coliform present in
water sample.
Selection of E. coli
EMB agar contains a dye methylene blue which inhibits the growth of grampositive organisms. In the presence of an acid environment, EMB forms a
complex that precipitates out onto the coliform colonies, producing dark centres
and a green metallic sheen. This reaction is characteristic for Escherichia coli, the
major indicator of fecal pollution. Other coliforms, Enterobacter aerogens produce
thick, mucoid, pink colonies on this medium. Enteric bacteria that do not ferment
lactose produce colourless colonies, which because of their transparency appear
to take on the purple colour of the medium.
L 35
LABORATORY-7
Biochemical Characterization of Microbial Flora of Water and
Wastewater
Anita Sharma
Drinking water should be aesthetically acceptable, being clear, odourless, without
disagreeable taste, free from chemical toxins and pathogenic micro-organisms.
Diseases like typhoid, cholera, diarrhea, poliomyelitis and viral hepatitis A and B
are water borne. Natural water sources usually contain some saprophytic bacteria
like Pseudomonas, Serratia, Flarobacterium, Chromobacterium, Acinetobacter
and Alcaligenes specis. Aerobie spore former bacilli, Enterobacter sps may also
be washed into natural waterbodies. These are harmless. Only pathogens
introduced into water by excremental or sewage pollution pose a risk to human
health.
The primary test employed as an indicator of fecal pollution of water is the
presence of coliform bacteria because they are present in feces of human beings
and other warm blooded animals in large numbers and can be detected in water,
even in high dilutions. Presence of thermotolerant E. coli provides definite proof of
fecal pollution.
Objective: To characterize water and wastewater microflora biochemically
Principle/Theory:
The challenge of waste water treatment is to remove (1) Compounds with high O2
demand (2) pathogenic organisms and viruses and (3) a multitude of human made
chemicals. Biochemical tests are one of the easiest and cheaper means for
identification. Here two different types of readymade biochemical test kits from Hi
Media labs will be used for the biochemical characterization. Besides this, given
below is identification of different groups of bacteria on the basis of media’s and
biochemical methods using conventional techniques
Conventional way to characterize water microbes:
Collection of Samples
The sample containers should be clean or sterilized. Sodium thiosulfate should be
added to samples of chlorinated water to inactivate residual chlorine which may
L 36
lower
bacterial
counts.
Samples
should
be
immediately
analyzed
for
microbiological testing.
Differential Coliform test
Eijkman test is usually employed to find out whether the coli forms of bacteria
detected in presumptive test are E.coli. After usual presumptive test, subcultures
are made from all the bottles showing acid and gas production to fresh tubes of
single strength MacConkey broth. They are incubated at 440C strictly.
Thermotolerant E. coli give definite proof of fecal pollution. Those showing gas in
Durham’s tubes, contain E.coli. Confirmation of E.coli can be done by testing for
indole production and citrate utilization.
IMViC Tests to differentiate enteric bacteria
Indole production: Tryptophan is an essential amino acid that can be
metabolized by tryptophanase produced by some bacteria. Ability to hydrolyze
tryptophan with the production of indole, a nitrogen compound is not a
characteristic of all microorganisms and therefore serves as a biochemical
marker. Indole can be detected chemically. Tryptone (digested protein) is used as
a substrate in this test.
Tryptophan ____________________ Indole + Pyruvic acid + Ammonia
Tryptophanase
Method: Inoculate two 1.0% tryptone broth tubes with test culture. Along with one
control; incubate tubes at 370C for 24-48 h. To about 6.0 ml of culture, add 0.3ml
Kovac’s reagent (p-dimethylaminobezaldehyde,5g, amyl alcohol, 75 ml and conc.
HCl ,25 ml). Mix well. Reddening of upper layer of broth within few min. indicates
a positive indole test.
Methyl Red (MR) Test: Sugars (hexose monosaccharide) are oxidized by all
enteric organisms for energy production but end products vary with the organisms
in use. Methyl red (a pH indicator) detects the presence of large concentrations of
acids. This test differentiates between E.coli and Enterobacter aerogens
particularly. Both organisms initially produce organic acids but at later stages
E.coli maintains acidic condition while Enterobacter aerogens converts these
acids to non acid products such as 2,3 butanediol and acetoin resulting in a rise in
pH.Methyl red at 4.0 ph turns red, indicating a positive test. At 6.0 ph indicator
remains yellow.
L 37
Glucose +H2O______Lactic, acetic and formic acids + CO2 + H2 (pH4.0) __Red color
MRVP broth contains glucose, 0.5, proteose peptone 0.5, K2HPO4 in 100 ml
water. Do not adjust pH.
Method: Inoculate 5 ml MRVP broth with bacterial culture and incubate for 48 h at
37 0C. Appearance of a distinct red colour on adding alc. methyl red solution
shows positive test.
Voges-Proskauer (VP) test: This test measures the production of neutral end
products such as acetylmethyl carbinol from organic acids from glucose by some
bacteria (Enterobacter aerogens)
Glucose + O2_________Acetic acid__________2, 3 dibutanediol, acetyl methyl
carbinol +CO2 +H2 (pH 6.0)
In the presence of Barritts reagent, acetyl methyl carbinol is oxidized to a diacetyl
compound, imparting red colour to the medium.Nonacidic compounds produced
from glucose fermentation by E.aerogens are detected .Barritts reagent consists
of a mixture of alcoholic alpha nephthol and 40 % KOH.
Citrate utilization: In the absence of fermentable sugars, some bacteria can
utilize citrate as a carbon source which depends on the presence of enzyme
citrate permease (positive test by Protease sps.)
Citric acid__________ Oxalacetic acid +acetic acid _________ Pyruvic acid
Citrase
Simmon citrate agar contains citrate as its only carbon and energy source. Colour
change from green to blue is a positive test of citrate utilization.
Detection of Salmonella
Salmonella typhi, the causative agent of typhoid and paratyphoid currently
comprise of more than 1000 serotypes or species and all of them are pathogenic.
Salmonellae are aerobic or facultative anaerobic and can grow at ph 6-8 at 15 –
41 0C.
On Mac Conkey Agar; Salmonella and Shigella (non lactose fermenter) form
colorless colonies and hence readily detectable. They are more translucent than
coliform colonies on Wilson and Blair bismuth sulphite medium; Jet black colonies
with metallic sheen are formed due to production of H2S. Paratyphii sps. does not
form H2S. They ferment glucose, mannitol and maltose with acid and gas
L 38
production. Lactose and sucrose are not fermented. Indole is not produced. They
are MR positive, VP negative and citrate positive.
Detection of Fecal Streptococci
Subcultures are made from all the positive bottles in presumptive coliform test with
the tubes containing 5.0 ml of glucose azide broth. It is an aerobe and a
facultative anaerobe, growing at 370C. Presence of Streptococci is indicated by
acid production after 18 h at 450C.Growth occurs only in media containing
fermentable carbohydrates or enriched with blood or serum. Growth can be
promoted by 10% CO2. Streptococci ferment several sugars producing acid but no
gas.
Examination of C. perfringens
This is tested by incubating varying quantities of the water in litmus milk medium
anaerobically at 370c for 5 days and looked for storming fermentation.
Detection of Vibrio Cholerae
The organism was first isolated by Koch (1883) from cholera patients in Egypt.
The cells are G-, curved rod and motile. They are asporogenous and
noncapsulated and are present in marine environment and surface waters
worldwide. They grow well in ordinary media in alkaline pH. On nutrient agar
colonies are moist, translucent with a bluish tinge in transmitted light. On
MacConkey agar, colonies are colorless at first but turn red on prolonged
incubation. Carbohydrate metabolism is fermentative, producing acid but no
gas.Indole is formed and nitrates are reduced to nitrites. These properties
contribute to the cholera reaction which is tested by adding a few drops of
concentrated sulfuric acid to a 24 h peptone water culture. With cholera vibrios, a
reddish pink colour is developed due to the formation of nitroso-indole. Catalase
and oxidase tests are positive. Methyl red and urease tests are negative. Gelatin
is liquefied.
Commercial Kits:
API systems (API laboratories product), Enterotube or oxifermtube, mintek and
Pathotec or Micro-ID systems are some examples of more comprehensive kits
which measure as many as 50 biochemical reactions. Variants of these products
have been developed for identifying anaerobes, Bacillus, enterobacteriaceae,
lactobacilli, pseudomonads, Staphylococcus, Streptococcus and yeasts.
L 39
Biolog plate uses dried substrate in 96 well microtitre trays which contain an
indicator of c-source metabolism, a triphenyltetrazolium salt indicating c utilization
rather than acid production in a fermentation reaction.
Media composition
Tryptone Broth: 1 g tryptone in 100 ml water
MRVP Broth: Glucose, 5g; Proteose peptone, 5g; K2HPO4 5g in 1000ml water
MacConkey Broth: (double strength pH 7.4):Peptone, 20g;lactose,10g; NaCl, 5g;
Bile salt, 5g; Neutral red soln.1%) 10ml in 1000ml water
Simmons
citrate
agar(pH
6.9):
ammonium
dihydrogen
phosphate,1g;
dipotessium hydrogen phosphate,1g; NaCl, 5g; Sodium citrate, 2g; Maganesium
sulphite, 0.2g; bromothymol blue 0.08;agar,15g and water 1000ml.
I) IMViC Test Kit (HiMedia)
Principle: Each HiMViC kit is a standardized colorimetric identification system
utilizing four conventional biochemical tests and eight carbohydrate utilization
tests. The tests are based on the principle of pH change and substrate utilization.
On incubation, organisms undergo metabolic changes which are indicated by
colour change in the media that can be either interpreted visually or after addition
of the reagent(s).
Requirements: HiIMViC Biochemical Test Kit (KB 001)
1.
Each kit contains sufficient material to perform 10 test
2.
Kovac’s reagent (R008) for indole test
3.
Methyl Red reagent (I007) for Methyl Red test
4.
Baritt reagent A (R029) for Voges-Proskauer’s test
5.
Baritt reagent B (R030) for Voges- Proskauer’s test
Procedure:
1)
Preparation of inoculum
KB001
cannot
be
used
directly
on
clinical
specimens.
The
organisms to be identified have to be first isolated and purified. Only pure
cultures should be used.
Isolate the organism to be identified on a common medium like Nutrient
Agar (M001/M1274) or Brain Heart Infusion Agar (M211). Pick up a single
well isolated colony and inoculate in 5 ml Brain Heart Infusion broth and
incubate at 37oC for 4-6 hours until the inoculum turbidity is ≥ 0.1 0D at 620
nm or 0.5 Mcfarland standard. Alternatively, a homogeneous suspension
L 40
made in 2-3 ml sterile saline can be used for inoculation. The density of the
suspension should be adjusted to 0.1 0D at 620 nm or 0.5 Mcfarland
standard.
Note
Erroneous false negative results may be obtained if the inoculum turbidity
is less than 0.1 OD
2)
Results are more prominent when enriched culture instead of suspension
Inoculation of the strip
Open the kit aseptically. Peel off the sealing tape
Inoculate each well with 50 µl of the above inoculum by surface inoculation
method
Alternatively the strip can be inoculated by stabbing each individual well
with a loopful of inoculum
Incubation : Temperature of incubation : 35-37oC, Duration of incubation :
3)
18-24 hours.
Observations & Result
Interpret results as per the standard given in the Result Interpretation
Chart. Addition of reagents in well nos 1, 2 and 3 should be done at the end
of incubation period that is after 18-24 hrs. Following reagents to be added
to the respective wells.
Indole Test : Well No. 1
Add 1-2 drops of Kovac’s reagent (R008). Development of reddish pink
colour with in 10 seconds indicates a positive reaction.
Reagent remains pale coloured if the test is negative.
Methyl Red Test : Well No. 2
Add 1-2 drops of Methyl Red reagent (I007).
Reagent remains red in colour if the test is positive.
Reagent decolourises and turns yellow if the test is negative.
Voges Proskaeur’s Test : Well No. 3
Add 2-3 drops of Baritt reagent A (R029) and 1-2 drops of Baritt reagent B (R030).
Pinkish red colour development within 5-10 minutes indicates a positive test.
No change in colour or a slight copper colour (due to reaction of Baritt
reagent A with Baritt reagent B) denotes a negative reaction.
L 41
Important points to be taken into consideration while interpreting the result
1) Allow the reagents to come to room temperature after removal from the
refrigerator.
2) In case of carbohydrate fermentation tests, some microorganisms show
weak reaction. In this case record the reaction as ± and incubate further
upto 48 hours. Orange colour after 48 hours of incubation should be
interpreted as a negative reaction.
3) In case of Lysine and Ornithine decarboxylation reaction, incubation upto
48 hours may be required.
4) At times organisms give contradictory result because of mutation or the
media used for isolation, cultivation and maintenance.
5) The identification index has been compiled from standard references and
results of tests have been obtained in the laboratory.
Precautions
Clinical samples and microbial cultures should be considered potentially
pathogenic and handled accordingly.
Aseptic conditions should be maintained during inoculation and handling of
the strips.
Reagents should not come in contact with skin, eyes or clothing.
Disposal of used material
After use, strips the instruments used for isolation and inoculation (pipettes, loops
etc.) must be disinfected using a suitable disinfectant and then discarded by
incineration or autoclaving in a disposable bag.
RESULT INTERPRETATION CHART
No.
Test
1
Indole
2
Methyl red
3
Voges
Proskauer’s
Reagents to
be added
after
incubation
1-2 drops of
Kovac’s
reagent
1-2 drops of
Methyl
reagent
1-2 drops of
Barrit
(reagent A
and 1-2
drops of
Baritt
reagent B
Principle
Detects
deamination of
tryptophan
Detects acid
production
Detects acetoin
production
Original
colour of
the
medium
Colourless
Positive
reaction
Negative
reaction
Reddish
pink
Colourless
Colourless
Red
Yellow
Colourless
Pinkish
red
Colourless/
slight
copper
L 42
4
Citrate
utilization
-
5
6
7
Glucose
Adonitol
Arabinose
-
8
9
10
11
Lactose
Sorbitol
Mannitol
Rhamnose
-
12
Sucrose
-
Detects capability
of organism to
utilize citrate as a
sole carbon
source
Glucose utilization
Adonitol utilization
Arabinose
utilization
Lactose utilization
Sorbitol utilization
Mannitol utilization
Rhamnose
utilization
Melibiose
utilization
Yellowish
green
Blue
Yellowish
green
Red
Red
Red
Yellow
Yellow
Yellow
Red
Red
Red
Red
Red
Red
Red
Yellow
Yellow
Yellow
Yellow
Red
Red
Red
Red
Red
Yellow
Red
RESULT ENTRY DATASHEET (to be filled in by trainees)
No.
Test
1
Indole
2
Methyl red
3
5
Voges
Proskauer’s
Citrate
utilization
Glucose
6
Adonitol
7
Arabinose
8
Lactose
9
Sorbitol
10
Mannitol
11
Rhamnose
12
Sucrose
4
1
2
3
4
5
6
7
8
9
10
Conclusion: (to be written in by trainees)
Books referred
1. Fergus Priest and Brian Austin (1993) Modern Bacterial Taxonomy 2nd
ed.Chapman and Hall, publishers, London.
2. Michael T. Madigan, John M. Matinko and Jack Parker (2000) Brock
Biology of Microorganisms 9th ed.Prentice hall International New Jersey.
3. Alexander N. Glazer and Hiroshi Nikaido (1998) Microbial Biotechnology:
fundamentals of applied Microbiology, W.H. freeman and Company, New
York.
L 43
LABORATORY-8
Preservation & Conservation of Bacterial Culture
Mahejibin Khan
Objective:
I) Preservation of pure cultures for short term and long term.
II) Reviving already stored cultures and checking for purity.
a. Preservation of pure cultures
Materials Required:
Pure cultures, inoculating loop, inoculating needle, Nutrient agar, nutrient broth
petri plates, test tubes, cryovials, glycerol, Micropipettes,
Principle: In nature, microbial population exists as a mixture of many cell types;
by simple visualization it is not possible to distinguish them from each other.
However, in laboratory these populations can be separated into pure cultures.
These pure cultures are suitable for study of cultural, morphological, physiological
and biochemical properties so that they may be exploited for commercial
biotechnological applications. The mixed cultures are separated by streak plate
and pour plate method on agar plates. Discrete colonies are restreaked twice on
agar plates. Cultures are preserved by the following methods.
1.
2.
Short-term preservation.
(a)
Agar slants.
(b)
Agar stabs.
Long-term preservation.
(a)
Glycerol stocks.
(b)
Lyophilization.
Procedure:
Preparation and Inoculation of Agar-slants:
a). Prepare nutrient agar tubes, by dispensing 8-10 ml of medium in
each tube and sterilize.
b). Allow them to solidify by placing in an inclined position (app. 450C
angle) so that an agar slope is formed.
c). When completely solidified inoculate the surface of each slant with
d). Individual bacterial cultures under aseptic conditions using an
inoculating loop.
L 44
e). During inoculation move the needle gently on the agar surface from
bottom to the top, taking care not to disturb the agar surface.
f). Incubate at appropriate temp. (28-300C) in an incubator and observe
for growth patterns.
Preparation and inoculation of agar-stabs:
a).
Prepare nutrient agar tubes containing 1% agar.
b).
Sterilize by autoclaving. Allow them to solidify by keeping in vertical
position.
c).
Inoculate the stabs by piercing in a vertical position using an inoculating
needle under aseptic conditions.
d).
Incubate the stab-tubes in an incubator at 28 ±2 0C for 24-48 h.
e).
Observe growth pattern.
During inoculation take care that the needle should go straight down the
agar
otherwise growth pattern would not be clear
Preservation as Glycerol stocks
Single colonies from pure culture is inoculated into 10ml half strength
nutrient broth and allowed to grow till log phase. Now in this tube add 4.5ml
solution of nutrient broth and glycerol mixed in the ratio 1:1.Mix the contents
thoroughly and dispense the mixtures in cry vials in an aliquot of 1ml.The cry vials
are preserved at –20oC/-80oC. In this way culture are preserved for several years.
Preservation as lyophilized powder
Log phase cultures are dispensed in 1.8ml ampoules and are allowed to
dry under freezing temperature. Moisture from the cultures evaporates and
cultures are preserved as dry powder. The ampoules are sealed under aseptic
conditions and stored at room temperature.
II) To revive cultures from
i) a) Agar slants, b) Agar stabs
Requirements: Nutrient agar plates, cultures preserved as agar slants and stabs.
Procedure: Cultures in agar slants have to revived and checked for purity after
every three months and those from stabs have to be revived every six months.
Prepare nutrient agar plates. Take loopful of cultures from slant stab and streak it
over already prepared nutrient agar plates. Incubate at 28-30oC in an incubator
and check the purity of cultures.
L 45
ii) (a) Glycerol stocks
Requirements: ½ strength nutrient broth (NB) in tubes, full strength NB tubes,
nutrient agar (NA) plates, glycerol stock of a cultures preserved for two years.
Procedure: 100 µl of culture from glycerol stock is aseptically transferred in 10 ml
½ strength NB and incubated at orbital shaker at 28oC and 120 rpm. After 24 hr
tubes are checked for growth and 100 µl culture is again transferred into full
strength nutrient broth tubes. After culture has attained growth, a loopful culture is
streaked on nutrient agar plates so as to obtain isolated colonies. Culture is
checked for purity.
(b) Lyophilized power
Requirements: Nutrient broth (flasks), nutrient agar plates, vials containing
bacterial culture as lyophilized powder.
Procedure: Seal of vial containing lyophilized powder is aseptically broken in front
of flame in laminar flow bench. Loopful of powder is transferred in nutrient broth in
50 ml flasks. It is incubated on shaker at 28oC, 120 rpm for 24 h. The flask is
checked for turbidity. If nutrient broth is turbid then loopful of culture is streaked on
nutrient agar plates and incubated at 28oC till discrete bacterial colonies are
observed. Purity of culture is checked.
L 46
LABORATORY-9
Detection of Salmonella in Drinking Water by PCR Techniques
Mumtesh Kumar Saxena
Objective: Identification of Salmonella in water
Introduction:
Salmonella is an important pathogenic organism of human and animals. It has
many serovars most of them are pathogenic. S. Typhi causes typhoid fever in
humans and apart from this some other serovars like S. Typhimurium, S.
Cholerasuis and S. Enteritides may cause serious health problem in human
beings. In India where hygienic conditions are not good. There is always a
possibility of contamination of water and food from Salmonella. To detect
Salmonella in water several methods has been used but the most rapid and
reliable technique is detection by PCR. In this technique Salmonella specific
primers has been used to target salmonella specific loci (his, inv ). This technique
can show lot number of sample in few hours. It is economic technique and does
not require any isolation procedure.
Principle:
Salmonella specific 496 b P region of his gene will be amplified using
specific primers.
Materials Required:
1.
Autoclave bottles
2.
Suspected water
3.
Positive control ( Salmonella culture )
4.
Filter holders, Sterilized water
5.
Sterilized syringe , boiling water bath and ice
6.
Luria bertanii broth
7.
Eppendorffs ,tips float , centrifuge
8.
PCR tubes
9.
Salmonella specific primers
10. Taq polymerase, dNTP(s) and PCR buffer
L 47
11. Thermal cycler
12. 10¯ TAE buffer, Agrose and Ethidium bromide
Method:
•
Take 200 ml of suspected water and filter it through ( 0.22 µ) filters.
•
Incubate filters in Luria broth at 370c for 6 to 18 hours in shaker cum
incubator
•
Inoculate one tube of Luria broth with salmonella cultures.
•
Take 1 ml of (6-18 hr grown) culture and centrifuge at6000rpm for 10
minute.
•
Discard supernatant and resuspend the pellet in 100µl sterilized water.
•
Keep tubes in boiling water for 10 minutes followed by immediate chilling
on ice.
•
Centrifuge tube at 6000 rpm for10 minute.
•
Take 5µl supernatant in PCR tube.
•
Make mix with following composition.
10¯buffer – 5.0µl (1.5mM)
primers
-1.0 +1.0µl (20 pmol each)
dNTP
- 2.0µl (200mm each)
lysate
- 5.0µl
Enzyme
- 1.0µl (3U)
Water
- 35 µl
Total
•
•
=
50µl
PCR programme will be as followed
940c
-5 minute
940c
-1minute
600c
-1 minute 30 cycles
720c
- 1 minute
720c
-5 minute
After completion of programme, take 5µl of PCR product mix it with 1µl of
loading dye.
•
Load it on 1% Agrose gel and run at 5V/cm
•
Visualise band under U.V. and save gel in gel documentation system.
L 48
Fig. 1 :
Amplicon of invA gene of
Salmonella specific PCR
Fig. 2:
Amplicon of hisA gene of
Salmonella specific PCR
L 49
LABORATORY-10
Rapid Detection of E. coli from Water Sample
Manvika Sahgal & Mahejibin Khan
Objective: Detection of E. coli, Citrobacter and Salmonella species in water
samples using kits from Himedia laboratories
Materials Required: Water sample, HiWater Test Kit (K015-1KT) & Rapid
Hicoliform Test Kit (K016-1KT)
Procedure:
HiWater Test Kit
For rapid and simultaneous detection of Salmonella species, E. coli, Citrobacter
species and Vibrio species. Kit contains two sterile 100 ml bottles with two
separate A and B media.
Direction: Collect 100 ml water to be tested in each sterile disposable bottles.
Add entire quantity of medium A powder slowly to water of one bottle by swirling
to dissolve the powder completely. Similarly add entire quantity of medium B
powder to another 100 ml bottle and repeat the same procedure for dissolution of
powder as specified for medium A. After dissolution incubate both the bottles for
24-48 h at 35-37ºC.
Medium A – for Salmonella, E. coli, Citrobater species
Colour change
H2S production
E. coli
Yellow
-
S. serotype Typhimurium
Black
+
C. treundii
Black
+
S. serotype Enteritidis
Black
+
Organism
Key: no colour change (purple
colour) Medium B- For Vibrio
species
Organism
Colour change
V. cholerae
Dark burgundy
V. parahaemolyticus
Red
L 50
Rapid Hicoliform Test Kit
For rapid detection and confirmation of Escherichia coli and total coliform on the
basis of enzyme substrate reaction from water samples. Kit contains 1 sterile
bottle – 100 ml capacity and dehydrated medium.
Direction:
Collect 100 ml water to be tested in sterile disposable bottle. Add entire quantity of
medium by swirling to dissolve the powder completely. After dissolution, incubate
the bottle for 24-48 h at 35-37ºC. Observe the colour change of the medium from
light yellow to blue green indicating the presence of coliforms and light yellow to
fluorescent blue green (under UV) indicating presence of Escherichia coli.
L 51