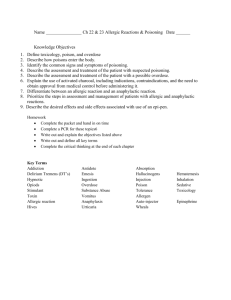
CPR Lesson 13-Sudden Illness Compatibility Mode
advertisement
Sudden Illness CPR/First Aid It is not that important to know the cause or type of sudden illness because the care you give will be the same with few exceptions. Lesson 13 Sudden Illness –Fainting –Diabetic Emergency –Seizure –Poisoning –Allergic Reaction 1 2 General Guidelines of Care for Sudden Illness Sudden IllnessesIllnesses-Key Points Some illnesses develop over time, while others can strike without a moment’s notice. By knowing the signals of sudden illness and paying careful attention to details at the emergency scene, you can determine how best to help a person with sudden illness. Do no further harm. Monitor breathing and consciousness. Help the person rest in a comfortable position. Keep the person from getting chilled or overheated. Reassure and provide care as needed. 3 4 Fainting--First Aid Fainting Fainting Check the airway and for breathing. If necessary begin rescue breathing/CPR, call 911. Loosen tight clothing from around the neck. (Pants/belt) Elevate the feet. Lay down for several minutes, or sit and place your head between your knees. Temporary loss of consciousness that could be a signal of a more serious condition. Caused by a reduction of blood flow to the brain. It is usually self-correcting, when the person collapses, normal circulation to the brain resumes. 5 7 1 Diabetic EmergencyEmergency-First Aid Diabetic Emergency If the person is unconscious, unable to swallow or a form of sugar is not available, call 911. If the person is conscious and able to swallow, give him/her sugar in the form of fruit juice, candy, non-diet soda or table sugar. (Dry or dissolved in water.) Diabetes is a condition where the body does not produce enough insulin or does not use insulin effectively. 8 9 Petit Mal Seizure Seizures Staring spell, most commonly called an “absence seizure”. It is a brief (usually less than 15 sec.) Most commonly in people under age 20, usually in children ages 6 to 12. They can occur as the only type of seizure but can also happen along with other types of seizures. When injury, disease, fever, poisoning or infection disrupts normal functions of the brain, the electrical activity of the brain could become irregular. This irregularity can cause a sudden loss of body control known as a seizure. 10 11 Seizure--First Aid Seizure Grand Mal Seizure Such seizures usually involve muscle rigidity, muscle contractions, and loss of consciousness. Grand Mal are the type of seizure that most people associate with the term "seizure," convulsion, or epilepsy. They may occur at any age, as a single episode, or as part of a chronic condition. 12 Protect the person’s head. Remove nearby objects that could cause injury. Call 911 for the following situations– Seizure lasts more than 5 minutes. Has repeated seizures, with out regaining consciousness. The person is injured. Fails to regain consciousness, is a diabetic or is pregnant. 13 2 Stroke (cont) Stroke A stroke is a loss of brain functions caused by a lack of blood to areas of the brain. The blockage usually occurs when a clot or piece of plaque breaks away from another area of the body and lodges within the brain. The left side of the brain controls movement of the right side of the body. Depending on severity, a stroke affecting the left side of the brain may result in loss of speech, loss of function and movement of the right side of the body. 14 FAST Recognition of a Stroke 15 FAST Recognition of a Stroke (cont) (Cincinnati PrePre-Hospital Stroke ScaleScale-1997) Face–weakness on one side of the face. (Ask the person to smile. This will show if there is drooping or weakness in the muscles on one side of the face.) Arm–weakness or numbness in one arm. (Ask the person to raise both arms to find out if there is weakness in the limbs.) Speech–slurred speech or trouble speaking. (Ask the person to say a simple sentence to listen for slurred or distorted speech.) Time–time to call 911. (Note the time when the signals began.) 16 Poisoning 17 Poisoning--Absorption Poisoning A poison is any substance that can cause injury, illness or death when introduced into the body. Poisons enter the body in four ways– •Inhalation (Breathing in) •Ingestion (Swallowed) •Absorption (Through skin/body tissue) •Injection (To force/drive into the body) 18 Contact dermatitis is the reaction of a sensitive person's skin to poison ivy, oak or sumac. Contact with these plants produces an itchy rash, redness, blisters and scaling. AVOID SCRATCHING. 19 3 National Poison Control Center General Care for Poisonings Check level of consciousness and breathing. Care for life-threatening conditions. If the person is conscious, ask questions for more information. Look for bottles or containers. Call 911 or the National Poison Control Center, 800-222-1222. Follow their directions. This national number will let you talk to experts in poisoning. It’s free and confidential. All local poison control centers in the U.S. use this national number. You should call if you have any questions about poisoning or poison prevention. It does NOT need to be an emergency. You can call for any reason, 24 hours a day, 7 days a week. 20 Allergic Reactions Insect bites, stings or contact with certain drugs, medications, foods and chemicals can cause an allergic reaction. •Check–Call–Care •The person may have a medical kit (epinephrine auto-injector) to treat a severe allergic reaction known as anaphylaxis. Assist the person as needed with using the kit until help arrives. 21 Allergy to Medications 22 Allergy to Bee Stings Allergic reaction to bee stings occurs when a person becomes sensitized to bee venom from a previous sting. The allergic reaction comes when the immune system is oversensitized to the venom and produces antibodies to it. Persons who develop an allergy to bee stings should carry prescription kits to counteract the bee venom. 24 A true allergy to a medication is different than a simple adverse reaction to the drug. The allergic reaction occurs when the immune system, having been exposed to the drug before, creates antibodies to it. On subsequent exposure to the drug these antibodies release histamines. If severe, this reaction can result in anaphylactic shock. 23 Stinger Removal To remove a stinger, scrape a straight-edged object across the stinger. Do not use tweezers since it may squeeze the venom sac and increase the amount of venom into the wound. Next wash with soap and water. Place an ice pack on the site to reduce swelling. If needed an antihistamine can be applied to help reduce the itching. Over the next several days watch for signs of infection. 25 4