Lectures 1 Lecture 2
advertisement
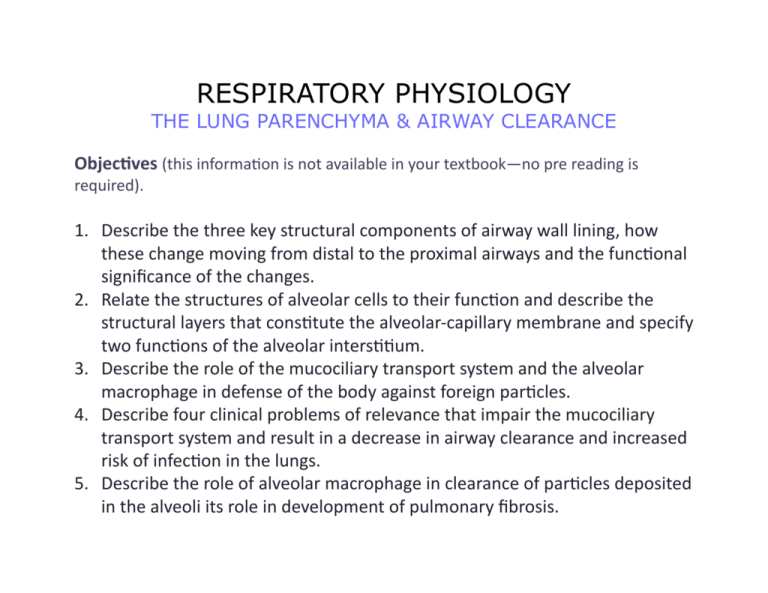
RESPIRATORY PHYSIOLOGY THE LUNG PARENCHYMA & AIRWAY CLEARANCE Objec&ves (this informa-on is not available in your textbook—no pre reading is required). 1. Describe the three key structural components of airway wall lining, how these change moving from distal to the proximal airways and the func-onal significance of the changes. 2. Relate the structures of alveolar cells to their func-on and describe the structural layers that cons-tute the alveolar-­‐capillary membrane and specify two func-ons of the alveolar inters--um. 3. Describe the role of the mucociliary transport system and the alveolar macrophage in defense of the body against foreign par-cles. 4. Describe four clinical problems of relevance that impair the mucociliary transport system and result in a decrease in airway clearance and increased risk of infec-on in the lungs. 5. Describe the role of alveolar macrophage in clearance of par-cles deposited in the alveoli its role in development of pulmonary fibrosis. CELLULAR TRANSITION From the conducting airways to the alveoli thinner epithelium-­‐ loss of car-lage -­‐ loss of smooth muscle – loss of mucous glands THE ALVEOLUS IS DESIGNED FOR GAS EXCHANGE 300 million alveoli each in contact with 100s of pulmonary capillaries SEM X2200 THE ALVEOLUS IS COMPOSED OF 3 CELL TYPES TYPES OF ALVEOLAR CELLS TYPE I: The PNEUMOCYTE 1. flat “squamous epithilium” – analogous to a fried egg! 2. covers 95% of the alveolar surface area 3. thin, 0.1-­‐0.3 microns in width [nucleus analogous to an egg yolk] 2 total alveolar surface area ≈ 100 m (about half of a tennis court) TYPES OF ALVEOLAR CELLS TYPE II: GRANULAR PNEUMOCYTE (or ALVEOLAR SEPTAL CELL) 1. cuboidal shape 2. contains lamellar inclusion bodies that store pulmonary surfactant, a surface ac-ve agent that reduces alveolar surface tension 3. pulmonary surfactant is a mixture of lipids (mostly) and proteins. Diphospha-dylcholine [DPPC] is its key surfactant (surface tension reducing agent) TYPES OF ALVEOLAR CELLS TYPE III: ALVEOLAR MACROPHAGE “DUST CELL” • located on the extracellular lining of alveolar surface • migratory & phagocy-c-­‐ defends against foreign par-cles alveolar macrophage ruffles next to E-coli THE ALVEOLAR-CAPILLARY MEMBRANE THE AIR-BLOOD BARRIER THE ALVEOLAR-CAPILLARY MEMBRANE air surfactant alveolar epithelium inters&&um capillary endothelium blood plasma ALVEOLAR INTERSTITIUM 1. joins & supports the structural elements via an elaborate fiber system [collagen & elas-n fibers] 2. a fluid space between air & blood barrier in series with the lympha-c system allowing excess fluid drainage into the lympha-c system AIRWAY CLEARANCE AIRWAY CLEARANCE DEFENSE AGAINST INHALED PARTICLES Particles > 10 µm in diameter 1. filtered & trapped by nasal hairs 2. irritant receptors lining the nasal passages initiate the sneeze reflex → removal of particles Particles 2-10 µm in diameter 1. mucociliary transport system lining the airways proximal to the terminal bronchioles 2. irritant receptors in airway lining→ cough→ removal of particles THE MUCOCILIARY TRANSPORT SYSTEM mucous blanket with 2 layers: a gel or mucus layer and a sol or aqueous periciliary, layer Surface view of ciliated epithelium of a bronchus. SEM X2865 MUCOCILIARY ESCALATOR & AIRWAY CLEARANCE Ciliary beat frequency ~17-25 strokes/sec IMPAIRMENT OF THE MUCOCILIARY TRANSPORT SYSTEM CLINICAL PROBLEMS OF RELEVANCE ↓ AIRWAY CLEARANCE & ↑ INFECTION 1. SMOKING ↓ciliary mo-on & ↑mucus produc-on 2. PATHOGENIC MICROBES release substances that paralyze ciliary mo-on (e.g. pseudonomas) 3. PRIMARY CILIARY DYSKINESIA cilia dysfunc-on due to a structural defect (an inherited disease) 4. CYSTIC FIBROSIS defec-ve chloride channels involved in transport of water & sodium across the epithelium result in forma-on of viscous, s-cky mucus hard to clear from the lungs & pancrea-c ducts (an inherited disease) AIRWAY CLEARANCE DEFENSE AGAINST INHALED PARTICLES Par-cles <2 µm in diameter reach the alveoli 1. Migra-ng & phagocy-c macrophages engulf foreign par-cles on alveolar surface & degrade them. 2. Non-­‐degradable par-cles with sharp profiles, such as silica dust & asbestos fibers, injure the alveolar epithelium & the alveolar macrophages leading to inflamma-on, scar forma-on [collagen deposi-on] and in turn: pulmonary fibrosis. alveolar macrophage & E. coli asbestos fibers embedded in lung tissue