What is a vasectomy? - Urologic Specialists
advertisement

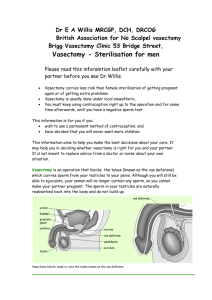
Vasectomy The decision to proceed with a vasectomy is a very personal one. It is important that you have a clear understanding of what a vasectomy is and what it is not. Most patients can expect to recover completely in less than a week and many are able to return to their job as early as a day after the procedure. Sexual activity can usually be resumed within a week following a vasectomy. The following will provide you with information that will assist you in deciding whether or not a vasectomy is an appropriate form of contraception for you. What happens under normal conditions? The testicles produce sperm and testosterone and are located in the scrotum at the base of the penis. Once produced, the sperm exit the testicle through a tube called the epididymis, where they stay until they are fully matured. Each epididymis is connected to the prostate by a tube called the vas deferens. This tube extends from the lower portion of the scrotum into the inguinal canal (site of most hernias) and then into the pelvis continuing behind the bladder. It is at this point that the vas deferens joins with the seminal vesicle and forms the ejaculatory duct. During ejaculation, seminal fluid mixes with sperm to form semen which is expelled through the urethra. What is a vasectomy? A vasectomy is a minor surgical procedure designed to interrupt the sperm transportation system between the testicle and the urethra by blocking the vas deferens. How is a vasectomy performed? Most vasectomies are performed in the urologist's office. However, the procedure may be done at an ambulatory surgery center or in a hospital setting if the patient and urologist have determined that intravenous sedation or general anesthesia is preferable. The decision to proceed in that type of setting may be based upon the patient's anatomy, anxiety or the need for associated surgical procedures. On the day of the procedure, the patient will be asked to sign a surgical consent form. We ask that the scrotal area be shaved the day of or the day prior to the procedure and to then wash off the extra hair in a warm shower. The patient will be brought into the procedure room and the area will then be washed with an antiseptic solution. Local anesthesia will be injected to numb the area but the patient will be aware of touch, tension and movement during the procedure. The local anesthetic should eliminate any sharp pain. The patient is awake during the procedure so, if necessary, he can let the urologist know if he is experiencing pain so more local anesthesia can be given. With a vasectomy, the urologist makes one or two small openings in the skin of the scrotum to access the vas deferens. The vas deferens is cut, and a small piece may be removed leaving a short gap between the two remaining ends. Next, the urologist will cauterize the ends of the vas, then ties the cut ends with suture material or use clips. The scrotal incision is then closed with dissolvable stitches. If the scalpel-less technique is used, the skin may not be closed, but instead covered with antibiotic ointment, and the opening will heal on its own. The entire procedure is then repeated on the other side either through the same initial incision or through a second scrotal incision. What should the patient expect after a vasectomy? Wear an athletic supporter or jock strap for several days. It may be worn for as many days as you desire. It often is more comfortable to wear this for the first week. Use an ice pack on/off for 1-2 days. It will lessen the discomfort. Avoid strenuous physical activity for three to five days. Intercourse may be uncomfortable for the first week. Use your best judgment. You may shower on the second day. Apply soapy water gently to the scrotum to wash. Rinse and dry by blotting the skin. Do not rub. All sutures are dissolvable and do not require removal. If a stitch comes out prematurely, the incision may open slightly and a small amount of discharge from the wound may develop. Wash it gently with hydrogen peroxide and place Bacitracin, Neosporin or triple antibiotic ointment on the incision and cover it with a small gauze pad. Do this two to three times a day. You may purchase these gauze sponges at most drugstores. Pain medicine will be prescribed for after the procedure. Use as necessary according to the instructions. Often, Tylenol or Motrin/Ibuprofen will be adequate for the discomfort after the procedure. Slight oozing of blood, some tenderness and mild swelling in the areas of the incision is not uncommon and should subside within 3 - 7 days. If there is an unusual amount of pain or a large amount of swelling to the scrotum, your urologist should be notified. Before proceeding with unprotected intercourse, you must produce a semen sample in which no sperm are found. A vasectomy, even though successful, is not effective immediately. The time until disappearance of sperm from the ejaculate varies from patient to patient. If sperm continue to be present in the ejaculate, you must continue to use contraception. After waiting for three months or 20 ejaculates, one in five men will still have sperm in their ejaculate, and will need to wait longer for the sperm to clear. You should not assume that the vasectomy is effective until the semen analysis demonstrates the absence of sperm. Instructions for obtaining the semen sample will be given at the post vasectomy appointment. If you have any questions, do not hesitate to call the office. If the office is already closed, your call will be connected to the answering service and they will assist you in contacting the doctor. Are there any risks associated with a vasectomy? Bleeding and Pain: In the immediate postoperative period there is the risk of bleeding into the scrotum. If the patient notices a significant increase in the size of his scrotum or significant scrotal discomfort, he should contact his urologist immediately. A patient experiencing fever, scrotal redness or tenderness should also be evaluated by the urologist as this may indicate an infection. Patients will often complain of mild lower abdominal discomfort similar to what one would experience from getting hit in the genitalia. Vasal Granuloma: A benign lump, or granuloma, may develop because there is a leakage of sperm from the cut end of the vas into the scrotal tissues. It may occasionally be painful or sensitive to touch or pressure. Post-vasectomy pain syndrome: This is a chronic pain syndrome that follows a vasectomy. The cause of this syndrome and its incidence are unclear. It is generally treated with anti-inflammatory agents. Occasionally, patients will elect to undergo vasectomy reversal in an attempt to alleviate this syndrome. Unfortunately, the response to surgical intervention is unpredictable. Testicular injury/loss: Testicles may be injured during a vasectomy as a result of injury to the testicular artery. This can result in the loss of a testicle. Other complications such as a collection of blood (hematoma) or infection may also occur. Future Health Issues: There has been some debate in the past as to whether vasectomies predispose a man to any future health problems. However, there is no conclusive evidence that men who have undergone a vasectomy have a higher risk of cardiovascular disease, prostate cancer, testicular cancer or other health problems. Frequently Asked Questions: Can my partner tell if I have had a vasectomy? There is no significant change in one's ejaculate after a vasectomy since the sperm contributes a small amount to the overall ejaculate volume. Your partner may on occasion be able to feel the vasectomy site. This is particularly true if you have developed a granuloma. Will my sense of orgasm be altered by having a vasectomy? Ejaculation and orgasm are generally not affected by vasectomy. The only exception to this is the occasional patient who has developed post-vasectomy pain syndrome. Can I become impotent after a vasectomy? An uncomplicated vasectomy cannot cause impotence. Can a vasectomy fail? First, it is important to be certain that a vasectomy has been successful and that all sperm are absent from the ejaculate prior to stopping other forms of contraception. Even if the vasectomy has been demonstrated to be effective, there is a small chance that a vasectomy may fail. This occurs as a result of sperm leaking from one end of the cut vas deferens (the testicular end) and finding a channel to the other end (the abdominal end). The failure rate has been reported to be between 0.025%-0.05%. This is a lower failure rate than any other form of birth control. Can I have children after my vasectomy? Yes, but if you have not stored frozen sperm, you will require an additional procedure. The vas deferens can be micro surgically reconnected (in a procedure called a vasectomy reversal) to allow normal conception to occur. Alternatively, sperm can be extracted from the testicle or the epididymis and utilized for in vitro fertilization. These procedures are costly and may or may not be covered by insurance. Additionally, they are not successful 100% of the time. Therefore, one should carefully consider nonsurgical alternatives for contraception prior to deciding to proceed with a vasectomy. Post Vasectomy Semen Analysis This notice is to inform you of the need for a semen analysis after your vasectomy. This will need to be done 2-3 months after the vasectomy or 20-30 ejaculations, whichever comes first. It is essential that we obtain laboratory confirmation of your sterility before you can proceed with unprotected intercourse. You are not considered sterile until this test is negative. It will be your responsibility to contact the lab/hospital to be certain that you are going to an in-network facility for the semen analysis. You will need to contact the lab/hospital to find out at which times they will accept the specimen. Take the semen sample to the lab/hospital within 2 hours of collection. Do not refrigerate, freeze, or expose to direct sunlight. We will give you further instructions on specimen collection and other necessary forms on your post-operative check-up appointment. Signature: ___________________________________ Print name: __________________________________ Date: _______________________________________ Vasectomy Consent Form I hereby authorize ____ _ and whomever he may designate as his assistant to perform the operation know as bilateral vasectomy. I fully understand that bilateral vasectomy means the removal of a segment of each vas deferens, which carries the sperm. I understand that this operation will cause sterility in the person operated on. This is usually but not always permanent. The word sterility means inability to produce children or cause pregnancy in a female partner. I am aware of the implications of this operation. I understand that this operation in no way affects sexual potency or the sexual act. I understand that in rare cases, recanalization or reconnection of the vas deferens may occur and therefore, a semen specimen must be collected for examination following the vasectomy. I understand that I must present a specimen of my semen so that absence of sperm in the semen can be determined. I understand that I am not sterile until there is a negative semen analysis. Risks involved in the procedure include bleeding, infection, loss of life, vasal granuloma, post vasectomy pain syndrome and spontaneous reversal as well as others. Signature: ___________________________ Print Name: __________________________ Date: _______________________________ For more information visit: http://www.youtube.com/watch?v=77fkgF4DA9I http://www.youtube.com/watch?v=tW1BDiWMvrc&feature=related