reading1 - Smith Lab
advertisement

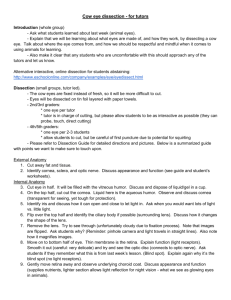
CHAPTER 1 Outline of Development of the Eye GENERAL PRINCIPLES1-8 The layers of embryo become evident by the end of three weeks of gestations these layers are ectoderm, mesoderm and endoderm, the ectoderm is the outer most. The endoderm does not participate in the formation of the eyes. The ectoderm proliferates successively to form neural plate, neural groove, neural fold and neural tube. From the anterior most part of neural tube develops forebrain. A small optic pit becomes evident at this stage, one on each side of primitive forebrain. This pit gradually fills up and starts out pouching on either side of the mid line forming optic vesicle. The optic vesicle has a globular shape with a narrow neck by which the interior of the optic vesicle communicates with interior of forebrain, the optic vesicle enlarges and its vortex touches the inner side of the surface ectoderm. The space surrounding the optic vesicles is filled by para axial mesoderm. The spot where the optic vesicle touches the surface ectoderm is the place that will gradually develop into the lens plate and get separated from the surface ectoderm. The optic vesicle continues to grow after touching the surface ectoderm and its surface bows inside to form a depression called optic cup that has two layers. This two layered cup is not complete it is open distally and inferiorly. If the optic vesicle fails to invaginate, a cystic eye ball results. In later stage the mesoderm will find its access inside the optic cup to form the vasculature of the eye. The axon of ganglion cells will come out to form the optic nerve. This groove under the optic cup is called embryonic or choroidal fissure. It gradually narrows to close down completely. The closure begins in the middle and extends on each end. The closure should be complete by sixth week. If it fails to fuse, the deficiency results in typical coloboma of uvea. Non fusion of posterior end in less common than that of anterior end, hence coloboma of posterior fundus including optic disc is less frequent than coloboma of anterior uvea. Deficiency in mid fundus is least common. DEVELOPMENT OF INDIVIDUAL STRUCTURES Development of the Lens The lens is solely ectodermal in origin. The development of the lens begins at an early stage of 4 mm. 1 C-8\C:\N-AGE\NEW-C1.PM5 2 PEDIATRIC OPHTHALMOLOGY The development of lens has two distinct stages : 1. A short period when the lens vesicle develops between 4.5 mm to 10 mm. 2. A longer period of development of lens fibers that continues even after the birth of the child. The lens fibers are laid down in two phases of primary and secondary fibers. The cells at the spot where the neuro ectoderm has come in contact with the surface ectoderm starts proliferating to form lens plate. The cells on each side of the lens plate increase and inveginate inwards in the form of a depression called lens pit. The pit gradually deepens to form a deeper cavity with an anterior opening. The opening slowly shortens and the cavity is converted into a hollow spherical structure called lens vesicle. The lens vesicle is single layered which ultimately separates from the surface ectoderm and is pushed towards the optic cup to lie freely within the lips of the optic cup. The surface ectoderm quickly bridges the gap and converts it into an uninterrupted layer of surface ectoderm that will form future corneal epithelium. The space between the surface ectoderm and the lens vesicle is invaded by mesoderm. In early stages of development the lens vesicle is a circular lumen surrounded by single layer of cuboidal cells. The anterior cells remain single layered and cuboidal for rest of the life. . The cells on the posterior part and equator are converted into elongated cells. The elongation of these cells and their multiplication obliterate the lumen of the vesicle. These elongated cells are called the primary lens fibers. From the central core of these fibers will develop the embryonal nucleus. The cavity of the lens vesicles is gradually obliterated, the anterior part of these cells ultimately touch the inner surface of the anterior cuboidal cells and formation of embryonic nucleus is complete. The outer most cells of the lens vesicle form lens capsule, which is in fact a true basement membrane produced by these cells. The so-called lens capsule is thickest at the equator and thinnest posteriorly. After the embryonic nucleus is formed, lens fibers continue to be laid down over it. This procedure continues through out the life and the fibers are called secondary lens fibers. In adult lens there are no nuclei in these cells. This is one of the factors contributing to transparency of lens. The fibers deposited at various times produces zones belonging to different ages. The oldest fibers are more centrally placed than the younger. They show optical difference. Fibers developing later are more transparent than those developing earlier. These various zones are called various nuclei according to chronology of their appearance. They are embryonal, foetal, infantile, (formed during last weeks of foetal life up to puberty) adult and cortex. The cortex is a homogenous material softer than nuclei. Zonules of the lens The Zonules of the lens develop separately along with vitreous, it is both ectodermal and mesodermal in origin. It is also known as tertiary vitreous. It starts developing in the fourth month of intra uterine life between the lens and the ciliary body. If there is a coloboma of ciliary body the zonules at that area become deficient. Development of zonule starts at 65 mm stage and completed at 110 mm stage. The zonuler fibers are derived from both primary vitreous and non pigmented epithelium of ciliary body. C-8\C:\N-AGE\NE-C1.PM5 OUTLINE OF DEVELOPMENT OF THE EYE 3 Vitreous Development of vitreous is complex; its exact origin is not well under stood. It is said to be derived from both mesoderm and ectoderm . The ectoderm mostly develops form inner layer of optic cup in the form of delicate fibrils. The mesodermal tissue forms hyloid vessels. The development of vitreous is divided into three parts : 1. The Primary Vitreous is presumed to be derived from both mesoderm and ectoderm. The hyloid vascular system is mesodermal, while fibrils are ectodermal, secreted by inner layer of optic cup. The surface ectoderm does not contribute to formation of primary vitreous. Primary vitreous starts developing in first month of intrauterine life. The primary vitreous is not atrophied. It lies behind the posterior lens capsule as a conical structure. It is surrounded by secondary vitreous. 2. The Secondary Vitreous starts forming from second month onward replacing primary vitreous that is completely replaced by sixth month, except the Coloquet canal which also disappears at birth. 3. The tertiary vitreous is the zonule of the lens. The Cornea The spot where the optic vesicle touches the surface ectoderm is converted into lens plate that gives rise to lens vesicle which is pinched off from the surface ectoderm. The remaining part of it gives rise to corneal epithelium. Rest of the cornea is mesodermal. The mesoderm encroaches in between the surface ectoderm and the lens. This mesoderm is divided into two distinct parts : 1. Anterior mesoderm that gives rise to stroma and endothelium of the cornea. 2. Posterior mesoderm that gives rise to iris stroma. In the space between the two layers of mesoderm develops the anterior chamber. The Descemet membrane develops from endothelium while Bownan’s membrane develops due to condensation of stroma under the corneal epithelium. The Development of Sclera1,2,4 Sclera is fully mesodermal in origin. It develops due to condensation of paraxial mesoderm around the optic cup. Its development is divided in two phases: 1. The development of anterior sclera 2. The development of posterior sclera. The sclera is fully differentiated by fifth month. Initially, the limbus is farther back near the future equator where the extra ocular muscles get attached later. By 12th week the posterior condensation encircles the optic nerve and the lamina develops. The scleral spur develops by 16th week and the Tenons capsule by 12th week along with insertion of recti muscles. The sclera plays little part in development of globe that depends upon development of retina. In contrast to this sclera plays an important part in growth of orbit. At birth the sclera is thin and gets a bluish tinge due to under lying uvea. C-8\C:\N-AGE\NE-C1.PM5 4 PEDIATRIC OPHTHALMOLOGY The Development of Extra Ocular Muscles13 All voluntary muscles develop from paramedian mesoderm. The extra ocular muscles are no exception. The extra ocular muscles develop from a common mesodermal mass that is separated as three different groups. From each will develop muscles that are supplied by different cranial nerves i.e. third, fourth and sixth. The nerves grow from brain towards individual muscle mass marked for each nerve. The individual extra ocular muscle starts differentiating at about 9mm stage and can be identified as separate muscle by 20mm stage except the levator. The levator develops from the dorsomedial aspect of the superior rectus. The nerve supply to levator passes through the superior rectus mass hence simultaneous congenital under action of both are a common feature. The Uvea The uvea develops from neuroectoderm and mesoderm. The Iris and ciliary body develop partly from neuroectoderm (that is part of optic cup), and partly from mesoderm. The structures that originate from neuroectoderm are pigment epithelium of iris sphinter and dilator pupilae of iris, epithelium of ciliary body. Melanocytes also arise from ectoderm. Bruch’s membrane is partly neuro ectodermal and partly mesodermal. The mesoderm gives rise to strom of iris, ciliary muscle, connective tissue and blood vessels. 1. The Iris. The part of the iris that develops from mesoderm is its stroma. It develops between the lens and surface ectoderm. The anterior tip of the optic cup develops over the scaffolding of mesodermal stroma. The tip of the cup develops into two layered pigment epithelium of the iris. The anterior layer is the continuation of outer layer of optic cup while the posterior layer is continuation of inner layer of optic cup. The pupillary membrane is a transient structure that lateron atrophies and disappears. Initially this stretches across the lip of the optic cup. It is formed by the mesodermal tissue surrounding the margin of the optic cup and tunica vasculosa lentis. Later the pupillary membrane separates from tunica vesculosa lentis. The peripheral part of the pupillary membrane gets vascularised. The central part of the pupillary membrane is eventually completely absorbed forming the pupil. Incomplete absorption of the pupillary membrane is called persistent pupillary membrane. The iris is fully pigmented after birth. If there is less of pigment the iris takes a blue colour. Some times fine vessels are visible on the iris of a new born. 2. The Ciliary body. The ciliary muscle develops from paraaxial mesoderm. The ciliary muscles become evident by third month and is gradually differentiated into longitudinal, oblique and circular muscles. The ciliary epithelium is neuro ectodermal in origin. It develops from the lips of the optic cup. The outer layer is pigmented while the inner layer is non pigmented the ciliary epithelium give rise to 70-75 ciliary processes. 3. The Choroid. Structure wise choroid differs from iris and ciliary body. It does not have an epithelium like the former two. It lacks stroma as in iris or musculature of ciliary body. It is mostly mesodermal except the Bruchs membrane that has both ectodermal and mesodermal origin. The choroid is mostly vascular with connective tissue inbetween. Its C-8\C:\N-AGE\NE-C1.PM5 OUTLINE OF DEVELOPMENT OF THE EYE 5 vasculature develops in three stages. Earliest is development of chriocapillaries. In second phase larger tributaries of venae verticosae develops by the third month of gestation.. The third phase consists of development of vessels from short ciliary vessels. The Anterior Chamber The anterior chamber develops as a cleavage in the paraxial mesoderm that lies between the corneal endothelium and iris stroma. Its presence is noticed at 20mm stage. Anterior chamber starts as a chink in the centre of this mesoderm and spreads to the periphery. Initially it is very shallow but at birth it is fully formed. The angle of anterior chamber is not formed before 6 month i.e. two months after the canal of Schlemm is visible. Schlemm’s canal starts as venous channel derived from various plexus at the margin of the optic cup. The Retina The retina develops from both the layers of optic cup. The inner layer gives rise to nine layers of sensory retina while the outer layer that remains single layered gives rise to pigment epithelium. The space between the two layers is very large in early stage of development that gradually shrinks to a potential space at the time of complete development of retina. By the time the fetal fissure begins to close the inner layer starts to thicken to form various layers of sensory retina. The pigment epithelium starts acquiring pigment granules at this stage. By seventh month of gestation all the layers of retina are well developed except in macula. The Macula Development of the macula differs from rest of the retina. Initially there is fast development in area of macula upto third month of life, then there is a slowing of growth while rest of retina grows in usual pace. This state of retardation persists upto eighth month then it start growing in the same manner as rest of the retina. Thus its development is not complete by ninth month. To attain full development macula has to wait up to fourth month post natal. At sixth month of foetal life it is thicker than rest of the retina. By seventh - eighth months it starts thinning. The thinning is due to spreading out of ganglion cells from the central part i.e. the fovea which at birth has only one layer of ganglion cells left. The outer nuclear layer is also single layered. The Optic Nerve The optic stalk that joins the fore brain and the interior of the optic vesicle is the future optic nerve. The foetal fissure that develops at the under side of the optic vesicle extends in to the stalk also. The axons of the retina and blood vessels pass through this opening. By third month the mesoderm that forms the connective tissue of optic nerve along with minute capillaries enter the optic nerve. The outer covering of the nerve i.e. dura, arachnoid and pia develop between third and seventh months, the lamina cribrosa develops late. Myelination of optic nerve starts at about seventh month of foetal life towards cephalicend, extending towards the lamina and stops short at lamina. In few cases the myelination may extend on the surface of the retina as medulated nerve fibers. C-8\C:\N-AGE\NE-C1.PM5 6 PEDIATRIC OPHTHALMOLOGY Intra Ocular Vasculature Intra ocular vasculature can be divided into three components : 1. The hyaloid system 2. The uveal system 3. The retinal circulation All of these arise from paraxial mesoderm that get into the eye through the fetal fissure. Besides supplying nutrient to the eye they play an important part in development of the eye itself. 1. The hyaloid system comprises of : (a) Vessels of pupillary membrane (b) Tunica vasculosa lentis (c) Hyloid artery (a) The vessels of pupillary membranes are formed by small buds from annualar vessels. The central part of the pupillary membrane is almost devoid of any vessel. It forms the pupil as it atrophies. The peripheral thick part persists as part of iris stroma. (b) The tunica vasculosa lentis. It has three parts i.e. the posterior, lateral and anterior. It completely engulfs the developing lens and supplies blood to it. It also forms a connecting channel between intra and extra ocular circulation. (c) The hyaloid artery is a branch of dorsal ophthalmic artery. It supplies blood to the developing lens. This passes through the foetal fissure and courses through middle a developing vitreous, stretching from posterior part of the optic vesicle to posterior pole of the lens. Before reaching the lens it divides into smaller branches and called Vasa hyaloidea propria that anastomose with each other in the primary vitreous and form the posterior part of tunica vasculosa lentis. Atrophy of the hyaloid system. Once the hyaloid system has reached its peak of development and finishes the main task of blood supply to the developing lens it starts to atrophy and disappears completely. Exact stimulus for disappearance of hyaloid system is not well under stood. The posterior part of the tunica vasculosa lentis is first to start to atrophy, followed by lateral. The anterior tunica is last to atrophy without leaving any trace. In hyaloid artery the anterior branches start disappearing first. Sometimes leaving a small part attached to the posterior pole of the lens as Mittendrof ’s spot. A small part may remain unabsorbed in the Cloquet’s canal or may remain attached to the optic nerve head as Bergmeister’s papillae. 2. The Uveal Circulation. The uveal circulation becomes evident at very early stage as vessels round the posterior part of the optic vesicle. The primitive internal carotid gives off two branches that are precursors of long posterior ciliary arteries i.e. dorsal and ventral ophthalmic artery, the former develops to become temporal long posterior ciliary artery while the latter is destined to become medial long posterior ciliary artery. The dorsal ophthalmic artery also gives rise to short posterior ciliary arteries. The anterior uvea is supplied by muscular branches of ophthalmic artery which form the anterior ciliary system. C-8\C:\N-AGE\NE-C1.PM5 OUTLINE OF DEVELOPMENT OF THE EYE 7 3. The retinal circulation. Exact mode of development of retinal circulation is controversial. Most widely accepted hypothesis is that central retinal artery buds from the posterior end of hyloid artery at the level of optic cup but does not atrophy like rest of the hyloid system and then branches off as temporal and nasal branches that divide into superior and inferior branches. Development of Lid, Conjunctiva and Lacrimal System 1. The Lid. The lid has dual origin, the main mass of the lid is formed by mesoderm while the skin and conjunctiva develop from surface ectoderm. At about 18mm stage, the mesoderm condenses outside the optic vesicle in the form of lid fold. The upper lid develops from frontonasal process in two parts i.e. smaller medial and larger lateral part, while the lower lid develops from maxillary process. Fault in fusion of medial and lateral frontonasal mesoderm results in coloboma of upper lid that may very from a simple notch at the lid margin to extensive loss of tissue. The upper and lower lids are fused between third and sixth month then they separate. Separation is completed well before birth. Failure to separate will result in ankyloblepharon of various degrees. 2. The Conjunctiva. The conjunctiva, cilia, meibomian gland, lacrimal gland and accessory lacrimal glands also develops from surface ectoderm and are associated with development of the lid. 3. Development of lacrimal system7. (a) The lacrimal gland. Lacrimal gland develops from the superior temporal conjunctival fornix, as solid cords of ectodermal cells 8-10 in number which are surrounded by mesoderm that develop into connective tissue of the gland. The ectodermal cords gradually canalise and ramify. (b) The Lacrimal Passage. The lacrimal passage develops in the groove between the maxillary proces and lateral nasal process, the groove or cleft is converted in to a tube. The surface ectoderm gets buried in the mesoderm and progress upwards, at the same time a similar cord of ectoderm develops from the nasal cavity. The upper end will form the two canaliculi, puncta and sac. Subsequently the two cords i.e. the upper and nasal will join each other to form a continuous structure. During third month the central cells of the cord begin to disintegrate and form the nasolacrimal duct. The disintegration is patchy in nature but ultimately becomes continuous. The upper part thickens and dilates to form the lacrimal sac. Development of the Orbit The walls of the orbit develop from the mesoderm around the eye. The floor and lateral walls develop from maxillary mesoderm. The medial wall develops from the lateral nasal process. The roof differs little from these walls, it develops from the mesoderm covering the forebrain. By 14th week the boundaries of orbit are well differentiated. Up to 28th week the orbital margin is at the level of developing equator of the globe, there after it grows rapidly and the rim occupies more anterior position than the globe. The size of orbit is so small at this stage that its walls are snug with the globe. At birth the orbital rim is almost circular, its diameter is relatively large as compared to face. C-8\C:\N-AGE\NE-C1.PM5 8 PEDIATRIC OPHTHALMOLOGY CONGENITAL ANOMALIES OF THE GLOBE8,9,10 The Congenital anomalies of globe are caused due to faulty embryogeneses before the closure of the embryonic fissure. They can happen : A. During formation and development of primary optic vesicle i.e. Cyclopia, anophthalmos, and extreme degree of microphthalmos. B. During development of optic cup i.e. Congenital cystic eye ball, colobomatous cyst and typical coloboma of eye. (Uvea, retina disc.) C. Maldevelopment of formed eye is Microphthalmos (True nanophthalmos) 1. Cyclopia. This is an extremely rare congenial anomaly that has either a single mid line eye or two developing eyes with deformity of the forebrain and multiple anomalies of mid line. There is either one orbit or two maldeveloped fused orbits. There is one palpebral fissure with two rudimentary lids, and lacrimal apparatus. The IPA is wide, the lids do not close, the rudimentary cornea and conjunctiva are exposed. These children have neonatal death. 2. Anophthalmos. Strictly speaking term anophthalmos is reserved for a condition where no ocular tissue is present in the orbit due to non formation of optic vesicle. However in clinical practice eye with minimal ocular tissues are also called clinical anophthalmos. Generally these eyes do not have any evidence of formed globe. They are also known as extreme microphthalmos. Anophthalmos differs from enophthalmos. In enophthalmos a fully developed globe is pushed back in the orbit due to secondary causes. 3. Microphthalmos. These include all eyes that have size less than normal eye due to congenital cause. They can be unilateral or bilateral. In bilateral cases both eyes are smaller than normal but not of equal size. The defects in one eye need not be the same in other eye. In unilateral cases the other eye may be normal and remain so for rest of the life. Microphthalmos has been divided in following groups more on clinical features rather than embryological. (a) Pure microphthalmos (Nanophthalmos) (b) Colobomatous microphthalmos. (c) Complicated microphthalmos. (d) Microphthalmos with cyst. (e) Microphthalmos associated with systemic syndromes. (a) Nanophthalmos11,12 (pure microphthalmos). Nanophthalmos is a rare congenital condition where a fully developed eye fails to grow like any other eye. This is caused due to failed growth after the embryonic fissure has closed from end to end. There are no colobomas present in the globe, it occupies normal position in the orbit, has normal movement but may be strabismic due to associated high axial hypermetropia. The cornea is smaller, AC is shallow. The sclera is thickened and the vertex veins are narrow11. There is pseudoneuritis, hypoplasia of macula, nystagmus, amblyopia. There are various types of glaucoma i.e. late onset of simple glaucoma, narrow angle glaucoma, precipitation of glaucoma following mydriasis13. These children require high hyper meteoric correction may require near correction. They have been described as phakia children with aphakic correction. The nanophthalmic eyes with glaucoma do not respond well either to medical or surgical treatment, the later is generally C-8\C:\N-AGE\NE-C1.PM5 OUTLINE OF DEVELOPMENT OF THE EYE 9 associated with Chroroideal effusion syndrome13 that may follow any intra ocular surgery or injury to the globe. (b) Colobomatous microphthalmos. colobomatous microphthalmos is a congenitally small eye that have associated failure of embryonic fissure. These eyes have multiple colobomatous defects at the site of fusion of embryonal fissure, mostly in uvea and or retina. These eyes are small in all dimensions, the coloboma may range from a small notch in iris to coloboma extending up to optic nerve. (c) Complicated microphthalmos. Is a term used to denote a congenitally small eye that develops cataract, iridocorneal defects, defects in iris, retina and vitreous. These are due to (i) Failure of development of primary optic vesicle. (ii) Arrest of development after the primary optic vesicle has formed. (d) Microphthalmos with cyst. In case only retinal tissue protrudes through the embryonic cleft a cystic eye ball with coloboma results. The colobomatous cyst may have an almost normal eye with a small indistinguishable cyst or the cyst may be so large that the small eye is not visible. In between are the cases where a formed eye is associated with colobomatous cyst. (e) Microphthalmos associated with various syndromes. There is a long list of conditions that are associated with microphthalmos most of which are cranio facial or mandibulo facial anomalies. BUPHTHALMOS This condition is just reverse of microphthalmos it is a large eye associated with various types of congenital glaucoma. DEVELOPMENT OF OCULAR STRUCTURE FORM EMBRYONIC GERMLAYER 1. The eye along with its adnex develop from ectoderm and mesoderm. The Bruch’s membrane and the tertiary vitreous (zonule) have duel origin. Bruchs membrane develops from neural ectoderm and mesoderm. While zonules develop from surface ectoderm and mesoderm. No part of the eye or its adnexa develop from endoderm. 2. The surface ectoderm gives rise to : A. The Lens B. Corneal Epithelium C. Epithelium of all the ocular adnexa i.e. conjunctiva, meibomian gland, glands of Zies and Moll, lacrimal gland, lacrimal passage. 3. The neural ectoderm gives rise to Sensory retina, retinal pigment epithelium, epithelium of ciliary body, pigment epithelium of iris, sphinter and dilator muscle of iris, melanoeytes, neural part of optic nerve. C-8\C:\N-AGE\NE-C1.PM5 10 PEDIATRIC OPHTHALMOLOGY 4. The Mesoderm gives rise to : A. Corneal stroma and endothelium of cornea. B. Iris stroma, ciliary muscles and chroid C. Sclera, vitreous and extra ocular muscles. D. Bony orbit E. Blood vessels. REFERENCES 1. Duke Elder.S. ; System of Ophthalmology, Vol-III, Part-I, First edition, Henry Kimpton, London, 1964. 2. Mann Ida ; Development of Human Eye, Third Edition, British Medical Association, London, 1964. 3. Barber A.N. ; Embryology of Human Eye, The C.V. Mosby St. Louis 1955. 4. Kozart D.M. ; Embryology of the human Eye in Text Book of Ophthalmology, Ninth Edition p79-92, Edited by Schcie H.G., and Albert D.M., W.B. Saunders Company, London, 1977. 5. Vaughan D and Asbury T. ; General ophthalmology, Ninth Edition p9-13, Lange medical publication, California 1980. 6. Hamming Nancy and Apple D. ; Anatomy and embryology of the eye in Principles and Practice of Ophthalmology, Vol-I, p3-20, First Indian edition. Edited by Peyman G.A., Sander D.R. and Goldberg M.F. Jay. Pee Brothers, New Delhi, 1987. 7. Buffam F.V. ; Lacrimal diseases in Text book of ophthalmology, Vol-4, Edited by Podos S.M. p7.1 to 7.3, Gower Medical Publication, London 1993. 8. Nema H.V. Singh V.D and Nema N. ; Congenital anomalies of the eye and its adnexa in Anatomy of the Eye and its Adnexa. Second edition. p162-165, Jay Pee Brothers, New Delhi 1991. 9. Duke Elder.S. ; System of Ophthalmology, Vol-III, Part-2, First Edition p415-495, Henry Kimpton London,1964. 10. Schaffer D.B. ; Abnormalities of the eye as a whole in Text Book of Ophthalmology Ninth Edition., p209-293, Edited by Scheie H.G. and Albert D.M., W.B. Saundes Company, Philaddphia 1977. 11. Dutta L.C. ; Uveal effusion syndrome in Ophthalmology, First Edition p-122-123 Current Books International, Kolkota 1995. 12. Shields M.B. ; Nanophthalmos in Text Book of Glaucoma, Fourth Edition, p-280, William and Wilkins Philadelphia 1999. C-8\C:\N-AGE\NE-C1.PM5