12 - The Core Content Review of Family Medicine

Volume 39 • No. 1 • January 2008
ANSWER BOOKLET
2
A
B
C
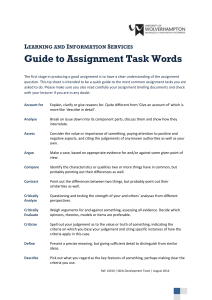
Strength of Recommendation Taxonomy (SORT)
Strength of
Recommendation
Strength-of-Recommendation Grades
Basis for Recommendation
Consistent, good-quality patient-oriented evidence*
Inconsistent or limited-quality patient-oriented evidence*
Consensus, disease-oriented evidence*, usual practice, expert opinion, or case series for studies of diagnosis, treatment, prevention or screening
*-Patient-oriented evidence measure outcomes that matter to patients: morbidity, mortality, symptom improvement, cost reduction and quality of life. Disease-oriented evidence measures intermediate, physiologic or surrogate end points that may or may not reflect improvements in patient outcomes (e.g., blood pressure, blood chemistry, physiologic function, pathologic findings).
Strength of Recommendation Based on Body of Evidence
Is the key recommendation for clinicians regarding diagnosis or treatment that merits a label?
No Strength of
Recommendation not needed
No Is the recommendation based on patient-oriented evidence (i.e., an improvement in morbidity, mortality, symptoms, quality of life, or cost)?
Is the recommendation based on opinion, bench research, a consensus guideline, usual practice, clinical experience or a case series study?
Yes
Strength of
Recommendation =
C
Is the recommendation based on one of the following:
• Cochrane Review with a clear recommendation
• USPSTF Grade A recommendation
• Clinical Evidence rating of beneficial
• Consistent findings from at least two goodquality randomized controlled trials or a systematic review/meta-analysis of same
• Validated clinical decision rule in a relevant population
• Consistent findings from at least two goodquality diagnostic cohort studies or systematic review/meta-analysis of same
Yes
No
Strength of recommendation = A
Strength of recommendation = B
Algorithm for determining the strength of recommendation based on a body of evidence (applies to clinical recommendations regarding diagnosis, treatment, prevention or screening). While this algorithm provides a general guideline, authors and editors may adjust the strength of recommendation based on the benefits, harms, and costs of the intervention being recommended. (USPSTF – U. S. Preventive Services Task
Force)
Reproduced with permission: Ebell M, Siwek J, Weiss BD, http://www.aafp.org/afp/20040201/548.html
et al. taxonomy (SORT). Am Fam Physician 2004; 69(3):548-556.
Strength of recommendation
Accessed December 200
THE CORE CONTENT REVIEW OF FAMILY MEDICINE
1
1 1 D DISCUSSION
Blood pressure (BP) measurement is one of the most common procedures performed at medical offices. Measurements can be made with manual or automated blood pressure cuffs. Automated cuffs are easier to use but may be inaccurate if the patient has an irregular heart beat. Additionally, in one study of acutely ill patients, automatic readings were consistently higher than manual cuff readings, causing the authors to suggest not using automatic readings for triage and management in these patients. In healthy patients, automated blood pressure cuffs should be checked for accuracy before they are used to assist in management of blood pressure.
The American Heart Association Council on
High Blood Pressure Research recommends that persons measuring blood pressure follow certain guidelines to maintain accuracy. Caffeine, alcohol and exercise should be avoided 30 minutes prior to the reading, and the patient should relax for 5 minutes before any reading
is taken (SOR C; Ref. 1). All clothing should be removed at the site of the cuff placement, and measurement should be made either in the sitting or the supine position. With the patient sitting with back supported and feet uncrossed and flat on the floor, the middle of the cuff should be at the level of the right atrium (mid-point of the sternum). This means that blood pressure should not be taken with the patient sitting on an examination table with feet dangling and back unsupported. When the patient is in the supine position, the arm should be supported with a pillow to approximate the level of the right atrium. The potential effects of body position on BP measurement are shown in Table 1.
Choosing the right cuff is mandatory to obtain an accurate blood pressure. The recommendations are to use a cuff with a bladder length that is 80 percent and a width that is at least 40 percent of arm circumference (a length-to-width ratio of 2:1). A cuff that is too small will give a falsely high reading, while a cuff that is too large will give a falsely low reading.
To manually record the blood pressure, the cuff is inflated to a pressure higher than the expected blood pressure. The stethoscope is placed over the brachial artery and the cuff is slowly deflated (deflation rate,
2 mmHg/second). The first of 2 or more “tapping” sounds (Korotkoff sounds) is the systolic blood pressure. The sounds will increase in intensity and then become muffled. When the sound disappears, this is the diastolic blood pressure.
Selected references:
1. American Heart Association. Recommendation for blood pressure measurement in humans and experimental animals: Part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure
Research. National Guideline Clearinghouse. http://www.guideline.gov/ summary/summary.aspx?ss=15&doc_id=6527&nbr=4093
Accessed December
2007.
2. Celis J, Singh D. Home blood pressure measurement appears useful for diagnosis and prognosis in routine clinical practice. Evid Based
Cardiovasc Med 2006; 10(1):18-20.
3. Cienki JJ, Deluca LA, Daniel N. The validity of emergency department triage blood pressure measurements. Acad Emerg Med
2004; 11(3):237-43.
4. Davis JW, Davis IC, Bennink LD, et al.
Are automated blood pressure measurements accurate in trauma patients? J Trauma 2003;
55(5):860-3.
5. Shevchenko Y, Tsitlik J. 90 th Anniversary of the Development by Nikolai S. Korotkoff of the Auscultatory Method of Measuring
Blood Pressure. Circulation 1996; 94:116-118.
Body Position
Supine
Unsupported back
Crossed legs
Arm level
Arm tension
Table 1 – Effects of Body Position on Blood Pressure Measurement
Effect on Blood Pressure Measurement
Diastolic measurement is approximately 5 mm Hg lower; systolic measurement may be up to
8 mm Hg higher
Diastolic measurement may be increased by 6 mm Hg
Systolic BP may be increased by 2-8 mm Hg
Arm below level of right atrium will elevate reading, arm level above will lower the reading; change approximately 2 mm Hg/inch
Isometric muscle tension will elevate pressure
ANSWER BOOKLET: VOLuME 39, NO. 1, JANuARY, 2008 3
1 2 C DISCUSSION
Co-sleeping is defined as bed sharing between an infant and adults or other children. Co-sleeping is popular internationally and was the norm in the
United States until the 1900s when certain historical factors reduced its prevalence. With the medicalization of birth, more U.S. women delivered in hospitals, and mothers were more often separated from their infants after delivery. Homes became larger, and separate bedrooms for children were more common. Separate beds were assumed to decrease the transmission of germs between the family and neonate. In the 1970s, infant formula became more readily available, increasing options for infant feeding. Over the same period, more women were entering the workforce.
Despite this, co-sleeping has seen a resurgence in popularity in the U.S. over the past 2 decades. Referred to as the “family bed,” co-sleeping is most common in Hispanic families. Black families are more likely to co-sleep with infants than white families.
The American Academy of Pediatrics (AAP) Task force on sudden infant death syndrome (SIDS) has issued a policy statement on co-sleeping. Recommendations include the “back to sleep” supine sleeping position for all infants. A firm mattress with a fitted sheet is best. Soft objects like pillows, quilts, stuffed toys and loose bedding are best kept out of the crib.
While maternal smoking during pregnancy is an established, major risk for SIDS, the link between parental smoking after delivery and neonatal risk is less well understood. SIDS risk likely increases in a dose-dependent mechanism depending on the number of family members who smoke and
duration of exposure (SOR C; Ref. 3).
The AAP recommends that infants not co-sleep
(SOR C; Ref. 1). Breast-feeding or comforting the baby in the family bed is reasonable, but infants should be returned to a separate place when they are ready to sleep. As the risk of SIDS is reduced when the infant sleeps in the same room as the parents, the bassinet or crib should be close by.
When providing advice on co-sleeping, it is important to realize that these AAP recommendations are primarily based on expert opinion. Potential advantages of co-sleeping include facilitating breastfeeding, improving maternal and infant sleep cycles and encouraging family bonding.
If a mother chooses to co-sleep with her infant, certain issues should be discussed. An association exists
4 between SIDS and maternal alcohol consumption, fatigue and infants sleeping with people other than their parents. Adults who have medical conditions such as obstructive sleep apnea or who take narcotics, hypnotics or other sedating medications should avoid sharing a bed with an infant. Parents should also be counseled on the availability of sidecar cribs.
These attach directly to the parents’ bed, allowing for close proximity for breast-feeding while providing an individual infant sleep area.
Selected references:
1. American Academy of Pediatrics Task Force on Sudden Infant
Death Syndrome. The changing concept of sudden infant death syndrome: diagnostic coding shifts, controversies regarding the sleeping environment, and new variables to consider in reducing risk.
Pediatrics 2005; 116(5):1245-1255. http://aappolicy.aappublications.org/cgi/ content/full/pediatrics;116/5/1245 Accessed December 2007
2. Baddock SA, Gallard BC, Taylor BJ, et al . Sleep arrangements and behavior of bed-sharing families in the home setting. Pediatrics 2007;
119(1):e200-e207. http://pediatrics.aappublications.org/cgi/content/abstract/119/1/ e200 Accessed December 2007
3. Fleming P, Blair P. Sudden infant death syndrome and parental smoking. Early Hum Dev (2007):electronic version http://www.ashaust.
org.au/pdfs/SIDSreview07.pdf
Accessed December 2007
4. Onusko E, Pathrose M. Issues in infant care. Primary Care Reports
2001; 7(19):161-170.
1 3 C DISCUSSION
Asbestos is a small, naturally occurring, heat-resistant fiber that is used in many industries. It is an occupational hazard for workers such as insulation workers, boilermakers, pipe fitters, plumbers, steamfitters, welders, shipyard workers, railroad workers and janitors.
Asbestos exposure may lead to respiratory diseases such as lung cancer (small cell and non-small cell carcinoma), asbestosis, pleural plaques, pleural effusion and malignant mesothelioma. Although some nonrespiratory cancers (gastrointestinal, laryngeal, bladder) have been linked to asbestos exposure, epidemiologic studies have not confirmed a strong association with exposure to asbestos.
Asbestosis is one of the pneumoconioses because it is a fibrotic lung disease caused by inhalation and deposition of mineral dust. It usually results in only minor symptoms. Pleural plaques (often calcified) are the most common pathologic response to asbestos inhalation; there is no evidence that these plaques will become malignant lesions. While benign pleural effusions are the most common sign of pleural disease due to asbestos, new effusions may represent malignancy.
Patients with new effusions should have tuberculosis skin testing plus diagnostic thoracentesis.
THE CORE CONTENT REVIEW OF FAMILY MEDICINE
Asbestos lung diseases are dependent on the cumulative exposure to asbestos, and symptoms usually appear after a latent period of 20 years or longer. Intense exposure may lead to disease earlier. In some cases, however, significant disease may occur with minimal exposure. Tobacco smokers who have been exposed to asbestos have a far greater-than-additive risk for lung cancer than do nonsmokers who have been exposed.
Although asbestos has been attributed to lung disease since the late 1900s, the United States did not enact its first legislation limiting exposure until 1971.
The most common symptom of asbestos lung disease is dyspnea upon exertion. Other symptoms may include nonproductive cough, chest pain, weight loss and fatigue. Patients with dyspnea on exertion and a significant history of asbestos exposure should be assessed with a chest x-ray and spirometry; if either test is abnormal, full pulmonary function tests, including measurement of lung volumes and diffusion capacity, should be obtained. Severe asbestos lung diseases will usually show a restrictive lung pattern on spirometry.
High-resolution computed tomography (CT) may be considered if the initial tests are negative in symptomatic patients. For patients with established pleural disease, the American Thoracic Society recommends that chest x-ray and spirometry be performed every 3 to 5 years (SOR C; Ref.
1), however, there is no good evidence that surveillance for development of lung cancer with these tests improves outcomes.
Treatment is supportive and consists of removing asbestos exposure, smoking cessation and vaccination for influenza and pneumococcus. Currently, no treatment alters the course of asbestos lung diseases, or results in cure.
Selected references:
1. American Thoracic Society. Diagnosis and initial management of nonmalignant diseases related to asbestos. Am J Respir Crit Care
Med 2004; 170:691-715.
2. Asbestosis. Agency for Toxic Substances & Disease Registry 2007. http://www.atsdr.cdc.gov/Asbestos/asbestos/health_effects/index.html
Accessed
December 2007.
3. Centers for Disease Control and Prevention. Changing patterns of pneumoconiosis mortality – United States, 1968-2000. MMWR
Morb Mortal Wkly Rep 2004; 53:627-632. http://www.cdc.gov/mmwr/ preview/mmwrhtml/mm5328a1.htm
Accessed December 2007
4. O’Reilly KM, McLaughlin AM, Beckett WS, et al.
Asbestos-related lung disease. Am Fam Physician 2007; 75(5):683-688. http://www.aafp.
org/afp/20070301/683.pd
f Accessed December 2007
4. Work-Related Lung Disease Surveillance Report 2002; Division of
Respiratory Disease Studies, U.S. Department of Health and Human
Services, Public Health Service, Centers for Disease Control and
Prevention, DHHS (NIOSH) number 2003-111, May 2003. http:// www.cdc.gov/niosh/docs/2003-111/2003-111.html
Accessed December 2007
1 4 A DISCUSSION
1 5 D Ulcerative colitis (UC) is a chronic disease characterized by diffuse mucosal inflammation of the colon that has a bimodal peak between ages 15 and
30 years and again between ages 55 and 65 years. It always involves the rectum (proctitis) and may extend proximally in a contiguous pattern to involve the sigmoid colon (proctosigmoiditis), the descending colon (left-sided colitis) or the entire colon (pancolitis). Although the exact etiology is unknown, one current hypothesis is that primary dysregulation of the mucosal immune system leads to an excessive immunologic response to normal microflora. Current cigarette smokers have a 40 percent lower risk of developing ulcerative colitis than nonsmokers; however, former smokers are approximately 1.7 times more likely to develop the disease than those who have never smoked. Interestingly, smokers are more likely to have flares (recurrences) of UC. There has been no consistent link of diet to the development of ulcerative colitis. While an association between the use of nonsteroidal anti-inflammatory drugs (NSAIDs) and the development of UC has been suggested, careful epidemiological studies have failed to confirm that this association is causal.
The typical presentation of UC is chronic bloody diarrhea associated with tenesmus (constant feeling of the need to defecate) and rectal urgency. Extraintestinal manifestations of UC are common and include arthritis, pyoderma gangrenosum, oral ulcerations and uveitis. The differential diagnosis of chronic diarrhea includes ischemic colitis, infectious colitis, Crohn’s colitis and irritable bowel syndrome, and recommended laboratory studies include stool culture, test for Clostridium difficile toxin and complete blood count. Colonoscopy with biopsy is recommended for patients suspected of having UC and for those with chronic diarrhea who have negative stool studies.
Blood tests for perinuclear antineutrophilic cytoplasmic antibodies (pANCA) and antisaccharomyces cerevisiae antibodies (ASCA) have been evaluated for differentiating between UC and Crohn’s colitis in patients with chronic diarrhea and an inconclusive colonoscopy. In one study the combination of positive pANCA and negative ASCA was specific but not sensitive for UC when studied in a pediatric subset
ANSWER BOOKLET: VOLuME 39, NO. 1, JANuARY, 2008 5
of patients. Further studies are needed before these tests can be routinely recommended.
The majority of patients with UC (80 percent) will have a disease course characterized by flares and remissions. Half of patients will have mild disease at the time of their first attack. Following the first flare, 5-10 percent of patients will have a continuous course, while 40-65 percent will have an intermittent course. As many as 10 percent of patients will have an initial attack that is so severe that colectomy is required. Even after 25 years, 90 percent of patients will still experience flares.
First-line therapy for UC is 5-aminosalicylic acid
(5-ASA) compounds, which suppress inflammatory mediators in the colon. UC proctitis should be treated with topical 5-ASA enemas, but more extensive disease requires a combination of oral and topical 5-ASA compounds. UC that does not respond to 5-ASA compounds should be treated with oral corticosteroids. If patients still do not respond, they should be hospitalized and considered for intravenous steroids or immunomodulating therapy with azathioprine
(generic, Imuran ® ) or infliximab (Remicade ® ). Some studies using probiotics have shown benefit. In one study nonpathogenic Escherichia coli N issle 1917 was found to be comparable to 5-ASA compounds in the treatment of UC.
How UC increases the risk of colorectal cancer is shown in Table 2.
Table 2 – Risk of Colon Cancer in
Patients with Ulcerative Colitis
Years Since UC Diagnosis Risk of Colorectal Cancer
First 10 Years
First 20 Years
First 30 Years
2%
8
18
Patients with strictly proctitis or proctosigmoiditis are not considered to be at increased risk for colon cancer.
Recommendations for surveillance of patients with
UC vary according to organization, but in general, the recommendation is for initial colonoscopy
8-10 years after disease onset (SOR C; Ref. 1) for patients with extensive disease or pancolitis and
15-20 years after the onset of left-sided disease, with repeat colonoscopies every 1-3 years (depending on the organization) in the second decade of the disease for those with pancolitis. Those organizations
6 that have the 3-year screening interval in the second decade have a shorter interval in the third decade.
Colonoscopy with 4 quadrant biopsies every
10 centimeters (minimum of 32 samples) is the recommended screening examination (SOR
C; Ref. 1).
No prospective randomized trials compare medical treatment to surgery for any indication in UC.
Colectomy with ileostomy for the treatment of UC is indicated in patients who develop dysplasia or cancer, have disease resistant to maximum medical therapy, depend upon steroids for remission and for those with massive hemorrhage, perforation or toxic megacolon.
Toxic megacolon, which is a presentation of fulminant
UC, is characterized by dilation of the transverse colon to more than 5.5 cm on a supine abdominal radiograph and requires emergent surgical evaluation.
Potential complications of surgery include bowel obstruction, pouchitis, stricture, pouch dysfunction and the possibility of decreased fertility in women.
Selected references:
1. American Society for Gastrointestinal Endoscsopy. ASGE guideline: endoscopy in the diagnosis and treatment of inflammatory bowel disease. http://www.guideline.gov/summary/summary.aspx?ss=15&doc_id
=9307&nbr=004977&string=inflammatory+AND+bowel+AND+disease
Accessed
December 2007
2. Carter MJ, Lobo AJ, Travis SPL. Guidelines for the management of inflammatory bowel disease in adults. Gut 2004; 53(Suppl V): v1-v16.
3. Cima RR, Pemberton JH. Medical and surgical management of chronic ulcerative colitis. Arch Surg 2005; 140:300-10.
4. Kruis W, Fric P, Pokrotnieks J, et al. Maintaining remission of ulcerative colitis with the probiotic Escherichia coli Nissle 1917 is as effective as standard mesalazine. Gut 2004; 53(11):1617-1523.
5. Reese GE, Constantinides VA, Simillis C, et al . Diagnostic precision of anti-Saccharomyces cerevisiae antibodies and perinuclear antineutrophil cytoplasmic antibodies in inflammatory bowel disease.
Am J Gastroenterol 2006; 101(10):2410-22.
6. Su C, Lichtenstein GR. Ulcerative colitis. In: Feldman M, Friedman LS, Brandt LJ, eds, Sleisenger and Fordtran’s Gastrointestinal and Liver. 8 th ed. Philadelphia: Saunders Elsevier 2006:electronic version.
1 6 B DISCUSSION
Approximately 330,000 hip fractures occur in the
United States annually. It is a particularly prominent problem in the elderly where osteoporosis, dementia, poor balance, alcohol use and decreased vision are risk factors. Falls cause 95 percent of hip fractures.
Morbidity and mortality are high in the elderly, with the one-year overall mortality ranging from 15 to 20 percent. Between one quarter and one third of all hip fractures occur in men. For at least 2 years after fracture, men with hip fractures have a mortality rate
THE CORE CONTENT REVIEW OF FAMILY MEDICINE
twice that of women. One half of elderly patients who lived independently before the fracture are left with prolonged institutionalization and ongoing disability. Up to 80 percent will fail to regain their functional independence. One year after surgery, 54 percent of patients can ambulate unaided.
On physical examination, patients with hip fractures usually have shortening of the leg with abduction and external rotation of the hip on the affected side.
Patients typically have localized pain and tenderness and limited range of motion and are unable to ambulate. Occasionally, patients may have normal ambulation with vague pain in the buttocks, knee, thigh, groin or back. X-rays confirm the diagnosis in most cases. Magnetic resonance imaging (MRI), bone scans (performed after 72-hour delay) and computed tomography (CT) may be used for ambiguous cases.
Hip fractures are classified by location (see Figures
1-3), which helps predict prognosis and complications.
Intracapsular fractures (femoral neck) frequently disrupt the blood supply to the femoral head, leading to avascular necrosis. They can be subcapital or transcervical. The fragile cancellous bone also provides poor anchorage for fixation device, leading to high rates of nonunion or malunion. Among extracapsular injuries, intertrochanteric fractures are rarely associated with nonunion or malunion, while subtrochanteric fractures have a high rate of nonunion due to the high mechanical stresses in the region.
Figure 2 – Intertrochanteric Fracture
Figure 1 – Intracapsular
(Femoral Neck) Fracture
Figure 3 – Subtrochanteric Fracture
Anticoagulation should start as soon as possible postoperatively and continue at least 10 days
(up to 28-35 days, particularly in patients at
high risk) (SOR A; Ref. 1); the incidence of deep venous thrombosis (DVT) after hip fracture surgery is approximately 50 percent among patients who are not prophylactically treated. Unfractionated heparin
(UFH) and low-molecular-weight heparin are equally efficacious at preventing DVT and fatal pulmonary embolism (PE), although UFH is associated with a higher rate of thrombocytopenia. Fondaparinux
(Arixtra ® ), a synthetic polysaccharide that inactivates factor Xa by antithrombin activity, is approved for the prevention of venous thromboembolism in hip fracture patients. Warfarin is also effective. Aspirin reduces the rate of DVT and PE but is less than effective than anticoagulants and should not be used alone.
Selected references:
1. American College of Chest Physicians. Prevention of venous thromboembolism: the seventh ACCP conference on antithrombotic and antithrombolytic therapy. Chest 2004; 126(3 Suppl):338s-340s. http://www.ngc.gov/summary/summary.aspx?ss=15&doc_id=5892&nbr=003878&stri ng=DVT+AND+%22hip+fracture%22
Accessed December 2007
ANSWER BOOKLET: VOLuME 39, NO. 1, JANuARY, 2008 7
2. Brunner LC, Eshilian-Oates L, Kuo TY. Hip fractures in ddults. Am
Fam Physician 2003; 67(3):537-542. http://www.aafp.org/afp/20030201/537.
html Accessed December 2007
3. Handoll H, Parker M. Hip fracture. Clin Evid 2005;
14:1414-1440.
4. Orwig DL, Chan J, Magaziner J. Hip fracture and its consequences: differences between men and women. Orthop Clin North Am 2006;
37(4):611-622.
5. Rao SS, Cherukuri M. Management of hip fracture: the family physician’s role. Am Fam Physician 2006; 73(12):2195-2200. http:// www.aafp.org/afp/20060615/2195.html
Accessed December 2007
1 7 B DISCUSSION
Hip fractures are fairly common in the elderly and accounted for 330,000 hospitalizations in 2003.
Morbidity and mortality are high; only 25 percent of patients recover completely, and 1-year mortality is
15-20 percent. The most common causes of mortality are deep venous thrombosis (DVT) and fatal pulmonary embolism (PE), pneumonia and other infections.
Optimal recovery requires coordinated preoperative and postoperative care from a multidisciplinary team, including the orthopedic surgeon, family physician, physical therapist and occupational therapist.
Family physicians are often asked to perform the preoperative assessment of patients with hip fracture.
Evaluation should be prompt, since some studies have shown increased mortality with surgery occurring more than 48 hours from the initial injury.
Delayed surgery is associated with a higher incidence of decubitus ulcers, confusion and fatal PE. Patients with acute myocardial infarction, unstable angina, decompensated congestive heart failure and significant dysrhythmias have high perioperative cardiac risk; surgery may be delayed up to 72 hours to stabilize these patients. Evidence has shown that beta-blockers given at time of surgery for patients at high cardiac risk decrease morbidity and mortality. Similar data do not exist for angiotensin converting enzyme (ACE) inhibitors.
Evidence suggests little or no benefit for DVT prophylaxis prior to surgery immediately after injury but strong benefit postoperatively. The American College of Chest Physicians recommends prophylaxis for at least 10 and up to 28-35 days after surgery, especially if the patient has at least one of the following: a history of venous thromboembolism, obesity, poor ambulation shortly after discharge, advanced age or a history of cancer. Effective medications include lowdose unfractionated heparin (LDUH), low-molecularweight heparin (LMWH), fondaparinux (Arixtra ® )
8 and warfarin (target INR 2.5). If surgery is delayed for medical stabilization or other reasons, preoperative prophylaxis with LDUH or LMWH is
recommended (SOR C; Ref. 2). Pneumatic hose are also effective for DVT prophylaxis immediately after surgery and should be used in patients who are at high risk for bleeding. Aspirin alone is inadequate for DVT prophylaxis.
Urinary tract infections are common after surgery, with indwelling catheters being a major risk factor.
Evidence supports the recommendation to remove indwelling catheters within 24 hours of surgery to reduce the likelihood of urinary retention. If retention occurs, the catheter can be reinserted for another
24 to 48 hours and then removed, or intermittent catheterization can be performed.
Perioperative antibiotics against Staphylococcus aureus have been shown to significantly decrease the risk of wound infections (superficial and deep) as well as urinary tract infections. Antibiotics (usually first- or second-generation cephalosporins) should be given
2 hours prior to surgery and for 24 hours postoperatively.
Selected references
1. Eagle KA, Berger PB, Calkins H, et al.
ACC/AHA guideline update for perioperative cardiovascular evaluation for noncardiac surgery. Circulation 2002; 105:1257-1267. http://americanheart.org/downloadable/heart/1013454973885perio_update.pdf
Accessed December 2007
2. Geerts WH, Pineo GF, Heit JA, et al.
Prevention of venous thromboembolism: the seventh ACCP conference on antithrombotic and thrombolytic therapy. Chest 2004; 126:338-400. http://www.ngc.gov/ summary/summary.aspx?ss=15&doc_id=5892&nbr=003878&string=DVT+AND+%2
2hip+fracture%22 Accessed December 2007
3. Guzman S, Warshaw GA. Preoperative and postoperative management of patients with hip fracture. http://www.aafp.org/online/en/home/ cme/selfstudy/cmebulletin/hipfracture/article/read.html
Accessed December
2007
4. Handoll HH, Farrar MJ, McBirnie J, et al.
Heparin, low molecular weight heparin and physical methods for preventing deep vein thrombosis and pulmonary embolism following surgery for hip fractures. Cochrane Database Syst Rev 2002; (4):CD000305. http:// www.cochrane.org/reviews/en/ab000305.html
Accessed December 2007
5. Maggio PM, Taheri PA. Perioperative issues: myocardial ischemia and protection – beta-blockade. Surg Clin North Am 2005;
85:1091-1102.
6. Novack V, Jotkowitz A, Etzion O, et al.
Does delay in surgery after hip fracture lead to worse outcomes? A multicenter survey. Int
J Qual Health Care 2007; 19(3):170-176.
1 8 D DISCUSSION
Nonalcoholic steatohepatitis (NASH) is also referred to as the silent liver disease. It is a condition characterized by inflammation and both fatty and fibrous changes in the liver. NASH tends to be seen in obese
THE CORE CONTENT REVIEW OF FAMILY MEDICINE
persons, diabetics, patients with hyperlipidemia and insulin-resistant individuals. Metabolic syndrome seems to be closely linked to NASH. Other predisposing factors may be total parenteral nutrition, rapid weight loss and intravenous glucose administration.
A partial list of medications associated with NASH includes corticosteroids, tamoxifen, amiodarone and methotrexate. The pathophysiology of NASH is still not very clear, although it is thought to be related to either insulin insensitivity or accumulated oxidative stress. When evaluating patients with elevated transaminases and/or gamma glutamyl transpeptidase
(GGT), clinicians should carefully question the patient about alcohol use.
NASH is most commonly seen in middle-aged females. The natural course is extremely hard to predict, but in general, most people live out their lives without any major sequelae. Up to 20 percent will go on to develop liver cirrhosis and hepatic failure. In most of the others, it is a chronic state and may go undiagnosed. Typically, there are no obvious physical findings with the exception of possible hepatomegaly.
Acanthosis nigricans (a reactive skin pattern in the flexural areas most commonly seen in association with obesity, cancer and other systemic disorders) may be seen in some instances. Sometimes patients with advanced disease may present with fatigue, malaise, weight loss or weakness for no apparent reason, and the workup may lead to the diagnosis of NASH.
Aspartate aminotransferase (AST) and alanine aminotransferase (ALT) are typically elevated. GGT levels may be high but below that of alcoholic liver disease.
Mild elevations in coagulation times and low proteins may also be seen. Imaging studies (computed tomography, magnetic resonance imaging or ultrasound) may show presence of fat in the liver. Confirmation must be by liver biopsy that reveals inflammation, fibrosis or cirrhosis and by further investigation that reveals no evidence of any other organic liver disease.
Important caveat: The mere presence of fat in
the liver does not diagnose NASH. Most commonly, fatty liver is a manifestation of a different state called nonalcoholic fatty liver disease (NAFLD) that affects 10-20 percent of Americans. Of these, only
10 percent meet the criteria for NASH. NASH is a subset of NAFLD that includes liver inflammation, fibrosis and cirrhosis.
There are currently no specific therapies available for early noncirrhotic cases of NASH. The most common approach is to modify the associated risk factors.
Commonly, obesity, hyperlipidemia and diabetes are addressed if present. While weight loss, metformin and thiazolidinediones all help improve insulin sensitivity, there is no evidence that they cure
NASH (SOR C; Ref. 1). In very advanced cases of
NASH, liver cirrhosis can necessitate liver transplantation. In fact, NASH is one of the most common reasons for liver transplants in the U.S.
Surgery is not indicated for NASH without cirrhosis.
Chelating and antiviral agents offer no benefit, as toxins and infectious agents play no role in NASH.
Selected references:
1. Angulo P. Non-alcoholic fatty liver disease N Engl J Med 2002;
346:1221-1331.
2. Bayard M, Holt J, Boroughs E. Nonalcoholic fatty liver disease.
Am Fam Physician 2006; 72(11):1961-1968. http://www.aafp.org/ afp/20060601/1961.html
Accessed December 2007
3. Belfort R, Harrison SA .
Placebo-controlled trial of pioglitazone in subjects with nonalcoholic steatohepatitis. N Engl J Med 2006;
355:2297-2307.
4. Clark JM, Brancati F, Diehl A. Nonalcoholic fatty liver disease.
Gastroenterology 2002; 122:1649-1657.
1 9 C DISCUSSION
10 A Providing quality care for a terminally ill cancer patient is a complex and difficult challenge.
Common physical problems related to cancer progression and toxicity of chemotherapy include fatigue, anorexia, weight loss (cachexia) and pain. Depression, spirituality concerns and psychosocial dysfunction are common concomitants to physical symptoms as patients face the dying process. The case-based question focuses on the physical symptom of fatigue and its management in the dying patient. Although much has been learned over the last decade regarding the pathophysiology and treatment options for terminal cancer syndromes, nothing is more important than an in-depth understanding of a patient’s goals and needs.
Open communication between the physician, the patient and his primary caregivers is the cornerstone of successful palliative care.
Cancer-related fatigue (CRF) has an overall prevalence of 60 percent. Fatigue may be an early symptom of malignancy, with as many as 40 percent of patients complaining of fatigue that predates the time of diagnosis. Fatigue can be related to the cancer itself or to treatment. In one study 90 percent of patients receiving radiation therapy and 80 percent of those receiving chemotherapy complained of fatigue. It is important to remember that fatigue can persist for
ANSWER BOOKLET: VOLuME 39, NO. 1, JANuARY, 2008 9
months or even years after therapy is completed in approximately one third of patients.
Fatigue is the most common and debilitating symptom described by patients with progressive malignant disease. Evaluation of patients should begin with a search for treatable underlying contributing factors such as depression, sleep disturbance, metabolic or drug-induced syndromes and poor pain control. In patients not on chemotherapy, the 2 most common direct causes of fatigue are the malignancy itself and treatment, or disease-related anemia. Progressive malignancy is associated with high levels of certain cytokines such as interleukin-1, interleukin-6 and tumor necrosis factora . Elevated levels of these proteins have been correlated with fatigue and anorexia/ cachexia syndrome in advanced malignant disease.
Preliminary studies are looking at inhibitors of tumor necrosis factora as therapy for CRF, but there are no reports of significant benefit thus far. Corticosteroids
(prednisone 15 to 30 mg/day) have been shown in randomized trials to increase the feeling of well-being and energy levels in a subset of patients with advanced malignancy and may be of help for short-term therapy. Adverse effects associated with long-term use and insomnia associated with even short-term use may limit usefulness. While psychostimulants such as methylphenidate (generic, Ritalin ® ) or modafinil
(Provigil ® ) can be considered after ruling out other causes, current evidence is insufficient to support a recommendation for routine use.
Nonpharmacologic therapy for cancer-related fatigue has been studied more widely and with more success than pharmacologic treatments. In patients who are able, a moderate symptom-limited walking exercise program (i.e., 15-20 minutes/day on 5-6 days/week) can result in significant improvement in energy and in functional capacity and a decline in mood disturbance and fatigue. Psychosocial interventions including support groups and individual counseling have also shown in controlled trials to decrease anxiety, fatigue and mood disturbance (SOR
A; Ref. 1).
Cancer-associated anemia is a multifactorial problem related largely to bone marrow effects of treatment
(chemotherapy and radiation) and the cytokinedriven anemia of chronic disease (ACD). ACD is characterized by lowered erythropoietin (EPO) levels, decreased bone marrow responsiveness to EPO, iron
10 trapping in the reticuloendothelial system (RES) and a shortened red cell survival time. There is strong evidence that anemia in cancer patients contributes significantly to the CRF syndrome and that correction of anemia will lessen fatigue
and improve quality of life (SOR A; Ref. 1).
Recombinant erythropoietin (Procrit ® , Epogen ® ) was first approved for use in renal failure patients in 1989.
Numerous studies in patients with cancer both on and off treatment have shown a median improvement in hemoglobin of 2 grams over 8-10 weeks of therapy coincident with significant improvement in qualityof-life parameters including fatigue. If erythropoietin is to be used, it is important to exclude other causes of anemia, especially iron deficiency, B
12
or folate deficiency, gastrointestinal bleeding and hemolytic anemia. Erythropoietin will not be effective until these treatable causes of anemia have been addressed.
Quality of life is maximized by increasing hemoglobin to target levels of 11-12 g/dL; recent studies indicate that hemoglobin levels >12 g/dL are associated with adverse outcomes. Of note, erythropoietin does not have the FDA indication for the treatment of anemia in cancer patients not on chemotherapy. ( For more information about the safety issues regarding erythropoietin, see question/discussion 35 in the October 2007 issue of
Core Content Review.)
There is no evidence that hyperalimentation, either enteral or parenteral, would be of any benefit in decreasing this patient’s fatigue. The role of hyperalimentation in cancer patients is limited to postoperative nutritional support and the rare patient with a curable malignancy (lymphoma, testicular cancer) that is unable to maintain adequate caloric intake, compromising their ability to maintain curative dose intensity. Some small studies using L-carnitine show some benefit for cancer-related fatigue, but larger blinded randomized controlled studies are needed.
Selected references:
1. Agency for Healthcare Research and Quality. Management of
Cancer Symptoms: Pain, Depression, and Fatigue. Evidence Report
/Technology Assessment Number 61. http://www.ahrq.gov/downloads/pub/ evidence/pdf/cansymp/cansymp.pdf
. Accessed December 2007
2. Ahlberg K, Ekman T, Gaston-Johansson F, et al.
Assessment and management of cancer-related fatigue in adults. Lancet 2003;
362:640-650.
3. Carroll JK, Kohli S, Mustian KM, et al. Pharmacologic treatment of cancer-related fatigue. Oncologist 2007; 12(Suppl 1):43-51.
4. Cortesi E, Gascon P, Henry D, et al. Standard of care for cancerrelated anemia: improving hemoglobin levels and the quality of life.
Oncology 2005; 68(Suppl 1):22-32.
THE CORE CONTENT REVIEW OF FAMILY MEDICINE
5. Groopmen J, Itri L. Chemotherapy-induced anemia in adults. J
Nat Cancer Inst 1999; 91:1616-1634.
6. Hofman M, Ryan JL, Figueroa-Moseley CD, et al. Cancerrelated fatigue: the scale of the problem. Oncologist 2007; 12(Suppl
1):4-10.
7. Lesage P, Portenoy RK. Management of fatigue in the cancer patient. Oncology 2002; 16:373-378.
8. Lower E, Fleishman S, Cooper A, et al.
A phase III, randomized placebo-controlled trial of the safety and efficacy of d-MPH as new treatment of fatigue and “chemobrain” in adult cancer patients. J
Clin Oncol 2005 ASCO Meeting Abstract 8000.
9. Mustian KM, Morrow GR, Carroll JK, et al. Integrative nonpharmacologic behavioral interventions for the management of cancerrelated fatigue. Oncologist 2007; 12(Suppl 1):52-67.
10. National Comprehensive Cancer Network Clinical Practice
Guideline in Oncology. Cancer Related Fatigue V.3.2007. http:// www.nccn.org/professionals/physician_gls/PDF/fatigue.pdf
. Accessed December
2007
11. Rozans M, Dreisbach A, Lertora JL, et al.
Palliative uses of methylphenidate in patients with cancer: A review. J Clin Oncol
2002; 20:335-339.
12. Stasi R, Abriani L, Beccaglia P, et al.
Cancer-related fatigue: evolving concepts in evaluation and treatment. Cancer 2003;
98:1786-1801.
11 D DISCUSSION
Blowout fractures commonly occur with blunt ocular trauma. Falls, assaults, motor vehicle accidents and sports-related injuries cause the majority of blunt ocular trauma. The mechanisms of blowout fractures are a sudden pressure increase within the orbit from globe compression and direct transmission of force through the orbital rim with buckling of the orbital floor.
Fractures of the orbital bones more commonly occur in the paper-thin floor and medial wall. (See Figure
4.) One case series of 34 pediatric patients found that floor fractures were by far the most common fracture type (71 percent). In contrast, the supraorbital roof is a heavy bone structure and rarely fractured.
Orbital blow-out fractures can be divided into the following types: trapdoor fractures (caused by low force), medial wall blow-out fractures (caused by intermediate force) and lateral wall blow-out fractures
(caused by high force). While many blowout fractures heal without morbidity, others are complicated with nerve or extraocular muscle entrapment, associated fractures and injury to adjacent tissue. Patients may present with edema and ecchymosis of the eyelids and periorbital areas. When there is a rupture into the sinuses, periorbital subcutaneous emphysema may be palpated and air-fluid levels may be seen on sinus xrays. Other signs include diplopia, enophthalmos and displacement of the globe (with trapdoor fractures).
ANSWER BOOKLET: VOLuME 39, NO. 1, JANuARY, 2008
Figure 4 – Magnetic Resonance Image of Orbital Fracture
Reproduced with permission from the Kellogg Eye Center, Department of Ophthalmology and Visual Sciences, University of
Michigan.
Trapdoor fractures, the diagnosis in this patient, are a pure orbital-floor fracture, linear in form, running along the canal of the infraorbital nerve and hinged medially, which allows herniation of orbital contents through the fracture and then entraps these herniated contents. Marked extraocular muscle motility restriction and nausea/vomiting should alert clinicians to the possibility of a trapdoor-type fracture.
If orbital floor fractures cause entrapment of the inferior rectus muscle or inferior oblique muscle, ophthalmoplegia with limited vertical movement and pain with vertical gaze may occur. Horizontal gaze is rarely affected. Involvement of the infraorbital nerve will result in ipsilateral numbness of the cheek and the upper lip in 60-70 percent of patients. Medial orbital wall fractures may extend into the ethmoid sinuses and are frequently associated with epistaxis. Although uncommon, there may also be injury to the medial rectus muscle and the nasolacrimal system, resulting in nasolacrimal duct obstruction and tearing.
Management of blowout fractures is evolving. Nonre- solving oculocardiac reflex (slowing heart rate with compression of the globe), the “whiteeyed” blowout fracture (entrapment of the inferior rectus muscle causing upward gaze), trapdoor fractures and early enophthalmos are indications for urgent surgical repair (SOR C;
Ref. 1). Surgery within 2 weeks is recommended in cases of symptomatic diplopia with positive forced
11
ductions (eye movements) and evidence of orbital soft tissue entrapment on computed tomographic scan or large orbital floor fractures that may cause latent enophthalmos. Early medical management consists of nasal decongestant spray, antiemetics, avoidance of sneezing or nose blowing, ice packs and, possibly, antibiotics. Early consultation with a plastic surgeon, ophthalmologist or maxillofacial surgeon is encouraged, as approximately half of orbital fracture patients require surgery.
Selected references:
1. American College of Occupational and Environmental Medicine (ACOEM). Eye. http://www.guideline.gov/summary/summary.aspx?doc_
id=8550&nbr=4759&ss=6&xl=999
Accessed December 2007
2. Bansagi ZC, Meyer DR. Internal orbital fractures in the pediatric age group: characterization and management. Ophthalmology 2000;
107(5):829-36.
3. Grant JH 3rd, Patrinely JR, Weiss AH, et al . Trapdoor fracture of the orbit in a pediatric population. Plast Reconstr Surg 2002;
109(2):482-9.
4. Shoff WH, Shepherd SM. Ocular Trauma. In: Ferrera PC, Colucciello SA, Marx JA, et al ., eds, Trauma Management: An Emergency
Medicine Approach. St. Louis: Mosby, 2001:208-210.
5. Tse R, Allen L, Matic D. The white-eyed medial blowout fracture.
Plast Reconstr Surg 2007; 119(1):277-86.
12 A DISCUSSION
Appendicitis is one of the most common surgical emergencies; lifetime incidence is estimated at 7 percent in the general population. The peak incidence shows a unimodal distribution and occurs between the ages of 10-30 years, although it is reported across all groups, including neonates. The classic symp- toms of appendicitis are anorexia, migration from periumbilical to right lower quadrant pain, vomiting and fever; this stereotypical sequence only occurs in 50 percent of patients but has diagnostic accuracy of 95 percent that is not improved with radiologic imaging. Such patients should go directly to surgery (SOR
C; Ref. 3).
Pain may be described in the epigastrium, periumbilical region, right lower quadrant, left lower quadrant and even the right flank; the latter finding may occur when the appendix is located in a retrocecal position.
A positive psoas sign (pain on hyperextension of the right thigh) suggests retrocecal position and has high specificity (95 percent). Given many cases do not involve retrocecal positioning, the sensitivity of the psoas sign is low (16 percent). Fever is present in approximately two thirds of patients, while vomiting occurs in approximately one half of patients.
12
In women of child-bearing age, pelvic inflammatory disease, gastroenteritis, urinary tract infection, ruptured ovarian follicle and ectopic pregnancy are the most common misdiagnoses. In pregnancy, the enlarged uterus may displace the appendix superiorly and the pain may be mistaken for biliary disease.
The most common diagnosis that is mistakenly given for appendicitis is acute gastroenteritis. A history of vomiting before pain suggests gastroenteritis over appendicitis in adults. In contrast, onset of pain prior to emesis has 100 percent sensitivity for appendicitis and 64 percent specificity.
The laboratory evaluation of patients with appendicitis is also subject to many limitations. Ureteral irritation from an inflamed appendix may lead to pyuria in up to 40 percent of patients and the erroneous diagnosis of urinary tract infection. Although the serum white blood cell count is often used as a marker for infection, it is elevated (greater than 10,000 cells/ mL) in only 70 to 90 percent of patients. Abdominal radiographs may show an appendicolith suggesting appendicitis, but this finding occurs in <10 percent of cases.
When the clinical evaluation is equivocal, abdominopelvic computed tomography (CT) has become the diagnostic test of choice and has reported accuracy of 93-98 percent – higher when intravenous or enteral contrast is used. The negative predictive value (NPV) is 95 percent, which is more favorable than the NPV of 76 percent for ultrasound. CT does have disadvantages to include cost and radiation exposure. It is also not recommended in pregnancy and carries the risk of contrast exposure for patients with renal insufficiency. Ultrasound may be used as an alternative technique (especially in patients who cannot undergo CT) but is operator-dependent, less accurate than CT and more difficult in patients with large body habitus.
The misdiagnosis or delayed diagnosis of appendicitis is not infrequent. It is incorrectly diagnosed in 10 percent of adults on the initial visit. This rate is higher in elderly and pediatric populations; children will be misdiagnosed in 25-30 percent of initial visits. Elderly patients may be slower to seek medical care, and the longer duration of symptoms may distract physicians from the proper diagnosis. Appendicitis represents the fifth most expensive source of claims with failure to diagnose as the leading cause in successful cases
THE CORE CONTENT REVIEW OF FAMILY MEDICINE
Selected references:
1. Graff L, Russell J, Seashore J, et al.
False-negative and falsepositive errors in abdominal pain evaluation: failure to diagnose acute appendicitis and unnecessary surgery. Acad Emerg Med 2000;
7:1244-1255.
2. Hardin DM. Acute appendicitis: review and update. Am Fam
Physician 1999; 60(7):2027-34. http://www.aafp.org/afp/991101ap/2027.html
Accessed December 2007
3. Old JL, Dusing RW, Yap W, et al . Imaging for suspected appendicitis. Am Fam Physician 2005; 71(1):71-8. http://www.aafp.org/ afp/20050101/71.pdf
Accessed December 2007
4. Paulson EK, Kalady MF, Pappas TN. Suspected appendicitis. N
Engl J Med 2003; 348(3):236-42.
5. Rybkin AV, Thoeni RF. Current concepts in imaging of appendicitis. Radiol Clin North Am 2007; 45(3):411-422.
13 E DISCUSSION
14 E Sexuality has normal fluctuations during different phases in life, and pregnancy is one such phase.
Approximately 90 percent of couples continue to engage in sexual activity during the second trimester, and couples tend to resume sexual activity around the
7 th week postpartum. Mothers who breast-feed their babies resume sexual activity later and may experience less sexual satisfaction in the postpartum period
(possibly related to vaginal dryness and low estrogen levels). Interestingly, sexual activity is resumed earlier following cesarean section than after spontaneous vaginal deliveries.
A decrease in sexual desire and coital frequency occurs from the first to the third trimester in most women (83 to 100 percent). Women and couples report a variety of reasons for this decrease. Early in pregnancy, some women report fears that intercourse will lead to miscarriage. During the third trimester, some couples have concerns that intercourse or orgasm may either harm the fetus or increase the risk of infection. Other reasons for decreased coital frequency include physical discomfort associated with intercourse (particularly in the missionary position) and loss of interest in sex. Contraindications to sexual activity are listed in Table 3.
Table 3 – Contraindications to Sexual
Activity During Pregnancy
Vaginal bleeding during pregnancy due to threatened miscarriage, infections, preterm labor or placenta previa
Cervical incompetence
Multiple gestation (during late pregnancy)
Preterm labor
Ruptured membranes
In the postpartum period, women report numerous reasons for delaying vaginal intercourse. Pain related to an episiotomy or perineal trauma during delivery causes discomfort in up to 75 percent of primiparas
(no good data for multiparous women). Persistent vaginal bleeding or discharge is problematic for some women, and fatigue lasting up to a year is present in
50 to 87 percent of women. Changes in body image after childbirth (feeling less attractive) reduce sexual interest, and lower estrogen levels immediately postpartum are known to decrease vaginal lubrication and libido.
Frequency of sexual intercourse is not related to preterm delivery or recurrent preterm delivery. In contrast to conventional wisdom, women who are sexually active late in pregnancy are actually less likely than pregnant women who are abstinent to deliver before 37 weeks of gesta-
tion (SOR B; Ref. 5). This is in contrast to the previously held belief that prostaglandins in the semen induce labor. Following an uncomplicated delivery, obstetric providers should not recommend a blanket
6-week abstinence from intercourse; intercourse should be resumed when comfortable for the
woman – whether that is at 2 weeks or 12 weeks.
Table 4 – Counseling Recommendations for
Pregnant Women Regarding Sexual Activity
1. Sexual activity during pregnancy is permissible as often as the couple desires, and activities other than intercourse (kissing, cuddling, massage, oral sex) may be practiced.
2. Sexual activity in pregnancy does not lead to miscarriage or preterm labor and is not harmful to the fetus.
3. Orgasms during pregnancy do not cause premature labor.
4. Position during intimacy is determined by maternal comfort. Missionary position may cause nausea and syncope because of pelvic compression by the enlarged uterus.
5. Cunnilingus during pregnancy is safe provided air is not blown into the vagina (may lead to air embolism).
6. Condoms may be used during pregnancy, and their use is advisable if either the woman or her partner has new sexual contacts during pregnancy.
7. Abstain from sexual activity with a partner who has or may have a sexually transmitted disease (STD) since some
STD can be transmitted to the infant.
8. Discuss the changing needs and desires of the woman with both her and her partner to help avoid conflict.
Counseling by the prenatal care provider can help dispel myths regarding sexual activity during pregnancy.
(See Table 4.) A frank discussion with the woman’s partner about appropriate sexual activity, frequency and need to respect the woman’s desire can help the
ANSWER BOOKLET: VOLuME 39, NO. 1, JANuARY, 2008 13
couple navigate this challenging period with a minimum of physical or psychological discomfort.
Selected references:
1. Blenning CE, Paladine H. An approach to the postpartum office visit. Am Fam Physician 2005; 72(12):2491-2497. http://www.aafp.org/ afp/20051215/2491.html
Accessed December 2007
2. Byrd JE, Hyde JS, DeLemaster JD, et al . Sexuality during pregnancy and the year postpartum. J Fam Pract 1998; 47(4):305-308.
3. De Judicibus MA, McCabe MP. Psychological factors and the sexuality of pregnant and postpartum women. J Sex Res 2002;
39(4):94-103.
4. Olsson A, Lundqvist M, Faxelid E, et al . Women’s thoughts about sexual life after childbirth: focus group discussions with women after childbirth. Scand J Caring Sci 2005; 19(4):381-387.
5. Sayle AE, Savitz DA, Thorp JM Jr., et al . Sexual activity during late pregnancy and risk of preterm delivery. Obstet Gynecol 2001;
97(2):283-289.
15 D DISCUSSION
Unintentional injuries are the leading cause of death in children and adolescents in the United States. Providing anticipatory guidance about injury prevention is an important part of the routine childhood visit.
Suffocation accounts for the majority of injury-related deaths in infants. The American Academy of Pediatrics
(AAP) recommends that infants sleep in supine position in the same room as the caregiver, but in a separate bed. Beds or cribs should have a firm mattress and not contain bulky covers or stuffed animals. Falls are a significant cause of nonfatal injuries in infants.
Infant walkers increase the risk of falls, especially falls down stairs. The AAP recommends banning the manufacture and sale of infant walkers (SOR
B; Ref. 2).
Although drowning is a major cause of injury-related death in toddlers, motor vehicle accidents account for the majority of deaths in this age group. Drowning is most prevalent in children ages 1-3 years. Children
4 years and under should be supervised by an adult while in bathtubs, pools, spas or near open water.
The supervising adult should be within one arm’s length and avoid other distracting activities. Swim- ming pools should be completely surrounded by fencing that is hard to climb and does not
access the house (SOR A; Ref. 8). Scalding is the most common reason for hospitalization with toddler burn injuries. Preventive measures include reducing hot water heater temperatures to less than
130°F (54.4°C).
Anticipatory guidance on poisoning includes using child-resistant medication packaging and keeping toxic substances out of reach of children. The AAP
14 recommends against using ipecac because it does not effectively remove poison from the stomach. Often used inappropriately or unnecessarily, ipecac may induce intractable vomiting that hinders later use of oral binding agents or antidotes. The use of “Mr.
Yuck” stickers on dangerous household products is not recommended. Stickers may draw children’s attention to dangerous items, and studies do not indicate a benefit.
Motor vehicle accidents cause the majority of fatal injuries in school-age children and are the leading cause of injury in adolescents. Proper seat belt use decreases the risk of injury and death. Teenage drivers have higher crash rates due to inexperience and risky driving patterns. Having teenage passengers in the car, particularly if they are male, further increases risk.
Driver education courses are not effective in preventing crashes and may actually lead to an increased crash risk if course completion allows for earlier licensing of younger teenage drivers.
Selected references:
1. Adler MR, Hyderi A, Hamilton A. What are safe sleeping arrangements for infants? J Fam Pract 2006; 55(12):1083-1087.
2. American Academy of Pediatrics Committee on Injury and Poison Prevention. Injuries associated with infant walkers. Pediatrics
2001; 108:790-792. http://aappolicy.aappublications.org/cgi/content/full/pediatrics;108/3/790 Accessed December 2007
3. American Academy of Pediatrics Committee on Injury, Violence, and Poison Prevention. Poison treatment in the home. Pediatrics
2003; 112:1182-1185. http://aappolicy.aappublications.org/cgi/content/full/ pediatrics;112/5/1182 Accessed December 2007
4. Brenner RA. Prevention of drowning in infants, children, and adolescents. Pediatrics 2003; 112:440-445.
5. National Center for Injury Prevention and Control. WISQARS leading causes of death reports, 1999-2003. http://webappa.cdc.gov/sasweb/ ncipc/leadcaus10.html
Accessed December 2007
6. Roberts I, Kwan I and the Cochrane Injuries Group Driver
Education Reviewers. School-based driver education for the prevention of traffic crashes. Cochrane Database Syst Rev 2001;
(3):CD003201. http://www.cochrane.org/reviews/en/ab003201.html
Accessed
December 2007
7. Schnitzer PG. Prevention of unintentional childhood injuries.
Am Fam Physician 2006; 74(11):1864-1869. http://www.aafp.org/ afp/20061201/1864.html
Accessed December 2007
8. Thompson DC, Rivara FP. Pool fencing for preventing drowning in children. Cochrane Database Syst Rev 1998; (1):CD001047. http:// www.cochrane.org/reviews/en/ab001047.html
Accessed December 2007
9. Ytterstad B, Sogaard AJ. The Harstad Injury Prevention Study: prevention of burns in small children by a community-based intervention. Burns 1995; 21:259-66.
16 E DISCUSSION
Heartburn (dyspepsia) is the most common presenting symptom associated with gastroesophageal acid reflux (GERD). Forty percent of the U.S. population
THE CORE CONTENT REVIEW OF FAMILY MEDICINE
experience heartburn at least monthly. Most people self-medicate with over-the-counter (OTC) antacids or histamine 2-receptor antagonists (H2RAs). A 2007 meta-analysis compared the placebo response, which ranged between 37 and 64 percent to common OTC agents; the relative benefit increase was up to 41 percent with H2RAs, 60 percent with alginate/antacid combinations (such as Gaviscon ® ) and 11 percent with antacids alone.
Proton pump inhibitors (PPIs) such as omeprazole/
Prilosec OTC ® provide greater GERD pain relief at
4 weeks compared to H2RAs. PPIs appear to have similar clinical effectiveness when compared to one another for treating GERD (SOR A; Ref.
2). Also, PPIs and fundoplication surgery appear to be similarly effective in relieving symptoms and improving quality of life. Even if surgery is chosen, 10-65 percent of surgical patients still require medications
1 year later.
Empiric therapy is recommended for new dyspepsia patients. Step-up therapy, beginning with a H2RA once or twice daily, then PPIs has historically been a useful and economical choice. Others favor stepdown therapy, beginning with twice-daily PPI for 2 weeks, then H2RA to maintain symptom-free state.
On-demand PPI use in place of continuous daily maintenance therapy was recently shown effective in the long-term management of GERD. Modifications, such as avoiding spicy foods, elevating the head of the bed and avoiding foods before bedtime, may be helpful for some patients but have not been shown to significantly improve symptoms in all people.
Older patients (55 years of age or older) with new-onset dyspepsia should undergo upper gastrointestinal endoscopy. Other red-flag indications for endoscopy include anemia, melena, hematemesis, weight loss (>5 percent), persistent vomiting, dysphagia (difficulty swallowing) and odynophagia (painful swallowing) (SOR
C; Ref. 5). These patients have an elevated risk for gastric carcinoma, although even in this subgroup the prevalence is small. Poor correlation exists between severity of symptoms and endoscopic findings. Routine endoscopy is not recommended for patients with heartburn alone in the absence of red-flag or alarm symptoms, even if more than twice weekly. Endos- copy to screen for Barrett’s esophagus is indicated for patients requiring chronic continu-
ANSWER BOOKLET: VOLuME 39, NO. 1, JANuARY, 2008 ous therapy with PPIs and those with chronic symptoms at risk for Barrett’s esophagus (i.e., duration of symptoms >5 years, white males,
>50 years of age) (SOR C; Ref. 5).
Selected references:
1. Agency for Healthcare Research and Quality (AHRQ). Comparative Effectiveness of Management Strategies for Gastroesophageal
Reflux Disease. http://effectivehealthcare.ahrq.gov/reports/topic.cfm?topic=7& sid=30&rType=4&sType=2 . Accessed December 2007
2. Ebell M. All PPIs equivalent for treatment of GERD. http://www.
aafp.org/afp/20060101/tips/3.html
Accessed December 2007
3. Howden CW, Chey WD. Gastroesophageal reflux disease. J Fam
Pract 2003; 52: 240-7.
4. Klok RM, Postma MJ, van Hout BA, et al.
Meta-analysis: comparing the efficacy of proton pump inhibitors in short-term use.
Aliment Pharmacol Ther May 15, 2003; 17:1237-45.
5. Medical Advisory Panel for the Pharmacy Benefits Management Strategic Healthcare Group. VHA/DoD clinical practice guideline for the management of adults with gastroesophageal reflux disease in primary care practice. http://www.guideline.gov/summary/summary.aspx?ss=15&doc_id=5188&nbr=003570&string=GERD Accessed
December 2007
6. Pace F, Tonini M, Pallotta S, et al . Systematic review: maintenance treatment of gastro-oesophageal reflux disease with proton pump inhibitors taken ‘on-demand.’ Aliment Pharmacol Ther 2007;
26:195-204.
7. Tran T, Lowry AM, El-Serag HB. Meta-analysis: the efficacy of over-the-counter gastro-oesophageal reflux disease therapies. Aliment
Pharmacol Ther 2007; 25:143-53.
17 A DISCUSSION
18 E The American Cancer Society (ACS) released updated recommendations for cancer screening in
January 2006; a minor revision regarding method of fecal testing was added in March 2007. Screening is designed to detect disease in asymptomatic patients at average risk of disease. Different screening schedules are recommended for symptomatic patients or those at increased risk.
Colorectal cancer screening begins at age 50 years for men and women with 5 options.
1. Yearly fecal occult blood test (FOBT) or fecal immunochemical test (FIT)
2. Flexible sigmoidoscopy every 5 years
3. Yearly FOBT or FIT, plus flexible sigmoidoscopy every 5 years
4. Double-contrast barium enema every 5 years
5. Colonoscopy every 10 years
For FOBT, the take-home multiple sample method should be used; the combination of fecal testing plus sigmoidoscopy is preferred over either option alone.
Colonoscopy is the follow-up test of choice if any of the other options are positive. Screening may be started earlier for patients with the following risk
15
factors: a strong family history of colorectal cancer or polyps (cancer or polyps in a first-degree relative
[parent, sibling, or child] younger than 60 years or in
2 first-degree relatives of any age), a personal history of chronic inflammatory bowel disease and a family history of a hereditary colorectal cancer syndrome.
Cervical cancer screening should begin 3 years
after first sexual intercourse or by age 21 years
(SOR C; Ref. 2). This is a modification from the old recommendation of testing soon after first sexual intercourse or by age 18 years. At age 30 years, women with 3 normal Pap tests in a row may be screened every 2 to 3 years. At age 70 years, women with 3 normal Pap tests in a row and no abnormal
Pap test in the last 10 years may choose to stop with further cervical cancer screening. Women who have had a hysterectomy for benign causes (not cancer or precancerous cervical changes) may discontinue Pap smears.
Breast cancer screening with mammography should begin at age 40 years and continue yearly as long as a woman is in good health. Because population studies have failed to demonstrate benefit, breast self examination (BSE) is considered an option (not a recommendation) by the ACS. Clinical breast examination
(CBE) is recommended as part of periodic health screening (every 3 years for women in their 20s and
30s and annually for women 40 years and older).
For women estimated by one of the clinical prediction models to be at high risk (>20% lifetime risk), annual breast magnetic resonance imaging (MRI) is recommended. It should be noted that insurer criteria for payment of MRI in high-risk women may differ from this recommendation. (Editor’s note: For additional information about MRI and breast cancer screening, see question/discussion 37 in the July 2007 issue of Core
Content Review.)
Prostate cancer screening should be offered annually beginning at age 50 years to men who have at least a 10-year life expectancy; both the prostate-specific antigen (PSA) blood test and digital rectal examination (DRE) should
be included (SOR C; Ref. 2). Men at higher risk (African American men; men with first-degree relatives having prostate cancer) should begin testing earlier, usually age 45 years. Men with multiple first-degree relatives with prostate cancer at an early age should be considered for testing at age 40 years.
16
While patients should be informed of the potential benefits and risks of PSA testing, discouraging testing is not appropriate. The ACS encourages testing for patients who are uncertain and defer the decision to their physician.
Selected references:
1. American Cancer Society Guidelines for Breast Screening with
MRI as an Adjunct to Mammography. American Cancer Society. http://caonline.amcancersoc.org/cgi/content/full/57/2/75
Accessed December
2007
2. American Cancer Society Guidelines for the Early Detection of
Cancer. American Cancer Society. Revision updated 3/28/07. http:// www.cancer.org/docroot/PED/content/PED_2_3X_ACS_Cancer_Detection_Guidelines_36.asp
. Accessed December 2007
3. Barclay L, Nghiem H. American Cancer Society Updates Annual
Guidelines for Early Cancer Detection. Medscape Medical News. http://www.medscape.com/viewarticle/522758
Accessed December 2007
19 C DISCUSSION
Major depressive disorder is a serious and highly recurrent condition. A substantial percentage of patients treated with antidepressants either do not achieve an adequate response to the agent or appear to lose their initial response over weeks, months or years. There are many possible explanations for a failed, inadequate or diminishing response to an antidepressant, whether the agent preferentially inhibits serotonin reuptake or not.
The term tachyphylaxis is often used to refer to a diminishing drug response, but specific definitions vary. The putative pathophysiology of tachyphylaxis involves progressive loss of neuronal sensitivity to a drug; however, the phenomenon is poorly understood.
Preliminary evidence suggests that tachyphylaxis is associated with “melancholic” depression, characterized, for example, by severe weight loss, pronounced psychomotor change and autonomous (nonresponsive) mood. Tachyphylaxis may also be more likely to develop in patients taking purely serotonergic antidepressants (selective serotonin reuptake inhibitors [SSRIs]) than in those taking agents acting on both serotonin and norepinephrine (serotoninnorepinephrine reuptake inhibitors). These findings, however, require further confirmation. In contrast to true pharmacological tolerance, tachyphylaxis does not appear to be overcome by increasing the dose of the drug; indeed, paradoxically, anecdotal reports suggest that drug responsiveness is occasionally restored by decreasing antidepressant dose or briefly interrupting treatment. However, systematic validation of this maneuver has not been carried out.
THE CORE CONTENT REVIEW OF FAMILY MEDICINE
Approximately 5-10 percent of patients maintained on antidepressants relapse yearly. This is sometimes attributed to tachyphylaxis. However, as Thase aptly observes, “Before attributing relapse or recurrence to diminished responsiveness to antidepressant medication at the neurochemical level, clinicians should ensure that the patient has been adherent to therapy as prescribed and consider other explanations.” In studies of antidepressant treatment resistance, the most common explanation is simply inadequate dose and/or insufficient duration
of treatment (SOR B; Ref. 8). Although recent data have challenged the teaching that antidepressant response does not occur for several weeks (e.g., one can find statistically significant improvement on the
Hamilton Depression Scale even within 1-2 weeks), it is nevertheless the case that many patients will require
4, 6, or even 12 weeks to achieve a robust clinical response to an antidepressant. However, patients with little or no response during the first month of treatment usually turn out to be poor responders with extended treatment. Adequate antidepressant dose and/ or blood levels are also crucial to achieving a robust clinical response, and apparent treatment resistance is often seen with underdosing. (Although precise therapeutic blood levels for newer, nontricyclic antidepressants have not been established, extremely low or negligible blood levels may point to nonadherence or to unusually rapid drug metabolism.)
Incorrect or missed diagnosis has been implicated in some cases of poor or diminishing response to antidepressant medication. In particular, failure to diagnose bipolar spectrum disorder may lead to inappropriate treatment with antidepressants, often in the absence of the required mood stabilizer. This may lead to an initial (sometimes rapid) improvement in depression, followed soon by
“roughening” of mood; precipitation of a mixed or manic episode; or complaints of agitation, insomnia or irritability. Screening instruments such as the
Mood Disorder Questionnaire (MDQ) and Bipolar
Spectrum Diagnostic Scale (BSDS) may aid primary care physicians in making the diagnosis of a bipolar spectrum disorder. Failure to recognize co-morbid substance abuse or underlying metabolic or endocrine disorder (e.g., hypothyroidism) in a depressed patient may also lead to unexplained treatment resistance.
Some very recent research suggests that the apparent
“petering out” of antidepressant response may be due
ANSWER BOOKLET: VOLuME 39, NO. 1, JANuARY, 2008 to loss of initial placebo response and that true tachyphylaxis is relatively rare. In effect, the patient may never really have had a true antidepressant response during the initial weeks of treatment but, rather, a placebo response that simply faded with time.
Selected references:
1. Ghaemi, SN, Miller CJ, Berv DA, et al.
Sensitivity and specificity of a new bipolar spectrum diagnostic scale. J Affect Disord 2005;
84:273-277.
2. Nierenberg AA, Amsterdam JD. Treatment-resistant depression: definition and treatment approaches. J Clin Psychiatry 1990;
51(Suppl):39-50.
3. Pies R. How long should you wait for an antidepressant to work?
Current Psychiatry 2007; 6(6):online.
4. Posternak MA, Zimmerman M. Dual reuptake inhibitors incur lower rates of tachyphylaxis than selective serotonin reuptake inhibitors: a retrospective study. J Clin Psychiatry 2005; 66(6):705-707.
5. Sharma V, Khan M, Smith A. A closer look at treatment resistant depression: is it due to a bipolar diathesis? J Affect Disord 2005; 84(2-3):251-257.
6. Solomon DA, Leon AC, Mueller TI, et al.
Tachyphylaxis in unipolar major depressive disorder. J Clin Psychiatry 2005; 6(3):283-290.
7. Thase ME: Preventing relapse and recurrence of depression: a brief review of therapeutic options. CNS Spectr 2006; 11(12 Suppl
15):12-21.
8. Zimmerman M, Thongy T. How often do SSRIs and other new-generation antidepressants lose their effect during continuation treatment? evidence suggesting the rate of true tachyphylaxis during continuation treatment is low. J Clin Psychiatry 2007;
68(8):1271-1276.
20 C DISCUSSION
Hypertensive crises are common clinical problems both in outpatient and emergency department settings. These crises range from merely uncontrolled, chronic hypertension to hypertensive emergencies
(blood pressure >180 systolic or >120 diastolic) with progressive target organ damage. Patients with hypertensive urgency, generally defined as severe but relatively asymptomatic hypertension without target organ damage, do not carry the same poor prognosis or need for rapid therapy as those with true hypertensive emergencies. The Joint National Commit- tee on Detection, Evaluation and Treatment of
High Blood Pressure VI defined hypertensive urgencies as “situations where it is desirable
to reduce blood pressure within a few hours”
(SOR C; Ref. 3). Usually, patients with hypertensive urgency are most appropriately treated by making adjustments to chronic blood pressure medications.
Though the frequency of complications associated with hypertensive emergencies has been described, the risk factors for progression from hypertensive urgency to hypertensive emergency are not well understood. One study identified poor control of systolic blood pressure as the strongest risk factor.
17
The most critical clinical task of the physician caring for a patient with a severely elevated blood pressure is identifying those patients who present with target organ damage. Target organ damage includes cerebral infarction, intracerebral or subarachnoid hemorrhage, encephalopathy, pulmonary edema, congestive heart failure, myocardial infraction or unstable angina, renal failure, retinal hemorrhages and aortic dissection. Discovering these complications can be a difficult clinical proposition and involves a careful history, physical exam, laboratory evaluation and imaging studies. Even taken together, these are not sufficient to identify all cases of target organ damage and certainly laboratory studies alone are insufficient.
Though rapid lowering of blood pressure with intravenous medications is a mainstay of treatment for hypertensive emergencies, it is not recommended for most hypertensive urgencies. Indeed, rapid lowering of blood pressure in the setting of hypertensive urgency has been associated with ischemic stroke in some cases. Hence, adjustment of chronic oral medications with ongoing blood pressure monitoring is the best approach to management of hypertensive urgency in a patient with previously treated hypertension. Short term follow-up is indicated.
In the previously untreated patient who presents with asymptomatic, elevated blood pressure readings in the hypertensive urgency range, risks related to persistence of the elevated blood pressure and the risks related to rapid reduction of blood pressure
(myocardial infarction, cerebral ischemia) must be considered. Treatment with a rapidly acting agent such as furosemide (generic, Lasix ® ), clonidine (generic,
Catapres ® ) or captopril (generic, Capoten ® ) should be given and the patient observed for several hours with the goal of a 20-30 mm reduction in blood pressure.
The patient should then be started on an antihypertensive medication that is deemed most appropriate for chronic administration.
Selected references:
1. Aggarwal M, Khan IA. Hypertensive crisis: hypertensive emergencies and urgencies. Cardiol Clin 2006; 24(1):135-146.
2. Bakris GL. Management of severe asymptomatic hypertension
(hypertensive urgencies). In: Rose BD, ed, UpToDate. Wellesley,
MA:UpToDate 2006.
3. National Institutes of Health. The Seventh Report of the Joint
National Committee on Prevention, Detection, Evaluation, and
Treatment of High Blood Pressure. National Institutes of Health.
NIH Publication No. 04-5230 August 2004. http://www.nhlbi.nih.gov/ guidelines/hypertension/jnc7full.pdf
Accessed December 2007
4. Stewart DL, Feinstein SE, Colgan R. Hypertensive urgencies and
18 emergencies. Prim Care 2006; 33(3):613-623.
5. Tisdale JE, Huang MB, Borzak S. Risk factors for hypertensive crisis: importance of out-patient blood pressure control. Fam Pract
2004; 21(4):420-424. http://fampra.oxfordjournals.org/cgi/content/full/21/4/420
Accessed December 2007
21 D DISCUSSION
22 B Vaginal bleeding during the third trimester of
23 B pregnancy is a true emergency and requires immediate evaluation. Providers must act rapidly and decisively to avert mortality for both the
mother and the fetus (SOR C; Ref. 6). Fortunately, some bleeding is due to nonthreatening causes.
Bloody show is due to cervical dilatation during normal labor and does not present any risk to the pregnancy. Other causes are extrauterine (cervicitis, cervical ectropion, cervical polyps and cervical cancer) and rarely cause any significant risk to the pregnancy.
Third-trimester intrauterine etiologies of vaginal bleeding include placenta previa, placental abruption and vasa previa. These may result in fetal or maternal mortality.
Complete placenta previa occurs when the placenta implants over the internal cervical os. Risk factors for placenta previa are listed in Table 5.
Table 5 – Risk Factors for Placenta Previa
Chronic hypertension
Multiparity
Multiple gestations
Advanced maternal age
Previous cesarean section
Tobacco use
Uterine curettage
History of placenta previa
The bleeding from placenta previa is typically painless and bright red. The initial evaluation of third trimester bleeding usually consists of a transabdominal or transvaginal ultrasound to exclude placenta previa.
If ultrasound is not immediately available, a sterile speculum examination is acceptable, but digital examinations should not be performed until placenta previa is excluded. Laboratory tests should include hematocrit, platelet count, blood type and antibody screen. Fibrinogen level and coagulation studies will evaluate for a consumptive coagulopathy. Rho (D) immune globulin (RhoGAM ® , BayRho-D ® ) should be administered to patients with vaginal bleeding
THE CORE CONTENT REVIEW OF FAMILY MEDICINE
who are Rh negative. The usual 300 mcg intramuscular dose of RhIg may not be sufficient to prevent sensitization, since it only contains enough anti-D immunoglobulin to prevent sensitization to 15 mL of
D-positive fetal red blood cells (30 mL of fetal blood).
Thus, testing for fetal red blood cells in the maternal circulation (Kleihauer-Betke or erythrocyte rosette test) should be performed and the dose of RhIg adjusted according to manufacturer recommendations.
Continuous fetal monitoring should be established.
Management of vaginal bleeding from placenta previa is based on whether the pregnancy is term. Emergent cesarean delivery is indicated if the pregnancy is >37 weeks. For pregnancies that are <37 weeks gestation, the stability of the mother and fetus should be assessed. If unstable, immediate cesarean delivery is indicated. If stable and the pregnancy is at least 34 weeks, the patient should be admitted and observed until fetal lungs are mature. If stable and the pregnancy is <34 weeks gestation, the patient should be admitted for observation and given corticosteroids
(betamethasone [Beta-Val ® ; Celestone ® ] 12 mg IM,
2 doses 24 hours apart or dexamethasone [Intensol ® ;
Maxidex ® ] 6 mg IM, 4 doses 12 hours apart) to help develop fetal lung maturity. After 34 weeks, corticosteroid administration has not shown any benefit to the fetus. Amniocentesis can be performed at 36 to
37 weeks to document pulmonary maturity. Cesarean section is indicated once fetal lungs are mature or the pregnancy is term.
Placental abruption is separation of the placenta from the uterine wall before delivery. Risk factors are listed in Table 6.
Table 6 – Risk Factors for
Placental Abruption
Chronic hypertension
Multiparity
Trauma
Preeclampsia
Short umbilical cord
Tobacco use
Uterine fibroids
History of placental abruption
Cocaine use
Sudden uterine decompression
Ultrasonography is unreliable in diagnosing placental abruption because acute blood clots and the placenta are both hyperechoic and
difficult to distinguish (SOR C; Ref. 6). Management of placental abruption includes stabilization and rapid delivery.
Vasa previa occurs with the velamentous insertion of the umbilical cord into the membranes in the lower uterine segment. This places the fetal vessels between the cervix and the presenting part. (See Figure 5.)
Risk factors include in vitro fertilization, placenta previa, multiple gestation and succenturiate-lobed
(accessory-lobed) and bilobed placentas. The usual presentation is bleeding at the time of amniotomy or spontaneous rupture of membranes. The Apt test can be performed to confirm the presence of fetal blood cells or fetal hemoglobin in the vaginal vault.
It is performed by obtaining a sample of blood from the vaginal vault and mixing it with tap water to lyse the red blood cells. After 5 minutes of centrifugation, the supernatant is removed and mixed with
1 percent NaOH. A pink color indicates fetal hemoglobin, while brown indicates adult hemoglobin.
Women at high risk can be screened with transvaginal color-flow Doppler. If membranes are not ruptured and the fetal heart rate is not reassuring, immediate cesarean section should be performed. Since fetal exsanguination is the cause of death in this disorder, preparation should be made to care for a neonate in shock (SOR C; Ref. 6).
Figure 5 – Vasa Previa
From UK Vasa Praevia Awareness http://www.vasapraevia.co.uk/
ANSWER BOOKLET: VOLuME 39, NO. 1, JANuARY, 2008 19
Selected references:
1. Ananth CV, Oyelese Y, Yeo L, et al . Placental abruption in the
United States, 1979 through 2001: temporal trends and potential determinants. Am J Obstet Gynecol 2005; 192:191-198.
2. Bhide A, Prefumo F, Moore J, et al . Placental edge to internal os distance in the late third trimester and mode of delivery in placenta praevia. BJOG 2003; 110:860-864.
3. Faiz AS, Ananth CV. Etiology and risk factors for placenta previa: an overview and meta-analysis of observational studies. J Matern
Fetal Neonatal Med 2003; 13:175-190.
4. Hladky K, Yankowitz J, Hansen WF. Placental abruption. Obstet
Gynecol Surv 2002; 57:299-305.
5. Lijoi AF, Brady J. Vasa previa diagnosis and management. JABFP
2003; 16(6):545. http://www.jabfm.org/cgi/content/full/16/6/543?maxtoshow=
&HITS=10&hits=10&RESULTFORMAT=&fulltext=vasa+previa&searchid=1&FIR
STINDEX=0&sortspec=relevance&resourcetype=HWCIT
Accessed December
2007
6. Sakornbut E, Leeman L, Fontaine P. Late pregnancy bleeding. Am Fam Physician 2007; 75(8):1199-1205. http://www.aafp.org/ afp/20070415/1199.html
Accessed December 2007.
24 B DISCUSSION
The patient has adult-onset asthma, as defined by diagnostic criteria from the National Heart Lung and
Blood Institute Expert Panel Report; the exposure to chemicals in the workplace suggests occupational asthma. In this case, car body paint is the occupational exposure. Urethane paints contain isocyanates and are the probable sensitizing agents. Once someone is sensitized, decreasing amounts of inhalational exposure can trigger asthmatic reactions, and continued exposure to the offending agent in the workplace will likely worsen symptoms over time. Sustained coughing or rhinitis symptoms are early manifestations of occupational asthma; chest tightness, wheezing and shortness of breath are likely to follow if exposure continues. Symptoms may improve during a week away from work and then recur when the person returns to work.
Radioallergosorbent tests (RAST) that detect specific
IgE antibodies are unreliable in assessing occupational asthma and are considered inferior to the difficult-tofind gold standard: specific inhalational challenge testing (SIC). Combining RAST with nonspecific bronchial provocation (e.g., methacholine) or skin prick testing has been proposed, but additional research is required to determine the optimal combination to match SIC. At present, serial peak flow testing at home and work is a readily available option to make the diagnosis; if peak flow variation is not observed over repeated measurements at work, other diagnoses should be considered.
Withdrawal from the workplace source is an important first step in controlling occupational asthma. However,
20 occupational asthma typically does not resolve entirely after removal from the exposure source – 70 percent of affected persons have persistent symptoms despite complete avoidance of the original trigger. Symp- toms may worsen irrespective of subsequent exposure status as well (SOR A; Ref. 1).
Prognostic indicators favoring recovery after cessation of exposure include short duration of symptoms before diagnosis, lower workplace exposures, compliance with personal protective equipment, enrollment in a health surveillance program and normal lung function after bronchodilators at time of diagnosis. Approximately one third of workers with occupational asthma are unemployed up to 6 years after diagnosis.
Occupational asthma treatment mirrors standard asthma therapies (such as bronchodilators and inhaled glucocorticoids); leukotriene receptor antagonists remain alternative options to first-line management but have little supporting trial data.
Selected references:
1. Agency for Healthcare Research and Quality. Diagnosis and
Management of Work-Related Asthma, Structured Abstract. October
2005. Agency for Healthcare Research and Quality, Rockville, MD. http://www.ahrq.gov/clinic/tp/asthworktp.htm
Accessed December 2007
2. British Occupational Health Research Foundation Occupational
Asthma Guidelines. http://www.occupationalasthma.com/bohrf.aspx
Accessed
December 2007
3. Chan-Yeung M, Malo JL. Occupational asthma. N Engl J Med
1995; 333(2):107-112. Accessed October 2007
4. Kogevinas M, Zock JP, Jarvis D, et al.
Exposure to substances in the workplace and new-onset asthma: an international prospective population-based study (ECRHS-II). Lancet 2007; 370:336-41.
5. National Health Service Occupational Asthma Clinical Knowledge
Summary. http://www.cks.library.nhs.uk/asthma/in_summary/scenario_occupational_asthma
Accessed December 2007
6. Tarlo SM, Vandenplas O. Statement of the American Thoracic Society: Diagnosis and Management of Occupational Asthma. Am J Respir Crit Care Med 2004; 167:460–462. http://www.thoracic.org/sections/ publications/statements/pages/eoh/occup.html
Accessed December 2007
25 D DISCUSSION
Medial epicondylitis, or golfer’s elbow, is the most common cause of medial elbow pain. It is usually an overuse injury from repetitive tension overloading of the wrist flexor/pronator muscles at their origin on the anterior medial epicondyle. In addition to golfing, this can be seen in athletic activities such as tennis, bowling and racquetball as well as occupations such as carpentry, plumbing and meat cutting. The pathophysiology results from microtears in the tendinous insertion at the epicondyle. When the damaged tendon heals inappropriately, tendinosis and chronic inflammation develop. Less commonly, an acute injury
THE CORE CONTENT REVIEW OF FAMILY MEDICINE
and inflammation may be the cause of medial epicondylitis. Tennis elbow, or lateral epicondylitis, is caused by repetitive tension overloading of the forearm and wrist extensors and is 10 times more frequent than medial epicondylitis.
The diagnosis of medial epicondylitis is made clinically. Patients will usually have tenderness over the anterior aspect of the medial epicondyle and pain with resisted wrist flexion and forearm pronation.
Pain is also made worse with valgus stress at the median epicondyle. One half of patients may have an associated ulnar neurapraxia and complain of numbness or tingling that radiates into their 4 th and 5 th fingers. Stress fractures are not associated with medial epicondylitis and x-rays are typically negative but may show small calcific deposits.
Most patients will improve with conservative management. This includes rest, splinting the wrist in flexion, nonsteroidal anti-inflammatory medications and wrist flexion curl exercises. Other methods of splinting that may be helpful are compression with a medial counterforce brace or a nighttime elbow extension splint if ulnar involvement is present. Corticosteroid injections can be considered if 3-4 weeks of conservative therapy have failed (SOR C; Ref.
1). There is evidence of short-term efficacy of steroid injections, although no long-term efficacy has been demonstrated. Surgery is performed for refractory cases and the tendons attached to the medial epicondyle are split to reveal the underlying scar tissue. The scar tissue is subsequently removed. If the ulnar nerve is involved, it can be surgically decompressed.
Selected references:
1. American College of Occupational and Environmental Medicine. http://www.guideline.gov/summary/summary.aspx?ss=15&doc_id=10883&nbr=00568
1&string=medial+AND+epicondylitis
Accessed December 2007
2. Cardone DA, Tallia AF. Diagnostic and therapeutic injection of the elbow region. Am Fam Physician 2002; 66:2097-2100. http://www.aafp.
org/afp/20021201/2097.html
Accessed December 2007
3. Cicotti MC, Schwartz MA, Cicotti MG. Diagnosis and treatment of medial epicondylitis. Clin Sports Med 2004; 23(4):693-705.
4. Mehlhoff TL, Bennett JB. Elbow injuries. In: Mellion MB, Walsh
WM, Shelton GL, eds. The Team Physician’s Handbook. 2 nd ed.
Philadelphia: Hanley & Belfus, 1997:467-468.
26 C DISCUSSION
27 A The development of long-acting opiates has greatly enhanced the management of chronic pain.
Although they cannot eliminate pain, longacting opiates provide better pain control for malignant and nonmalignant pain than shorter
acting agents (SOR C; Ref. 5). Although many long-acting agents are derived from shorter acting agents, (MS Contin ® and Avinza ® are long-acting morphine analogs, OxyContin ® is long-acting oxycodone), the longer acting agents have the advantage of providing a continuous and steady release of analgesia. This long-term release not only provides better pain control but also reduces the potential for rebound pain; shorter acting agents may require escalation in dosage due to more frequent peaks and troughs. In addition, long-acting agents do not contain acetaminophen, reducing the potential for hepatotoxicity associated with large dosages of shorter acting agents that contain acetaminophen.
Long-acting opioids share some unfavorable characteristics with shorter acting agents. These include the risk of medication abuse, constipation, sedation, histamine release and respiratory depression. In patients with chronic obstructive pulmonary disease
(COPD), respiratory depression and the release of histamine that may cause bronchospasm require caution in the use of opioid agents. Long-acting agents may provide some protection against shorter acting agents by providing continuous medication release versus sudden boluses that may suppress respiration.
Morphine derivatives should be used with great caution in reactive airway disease, as these agents are associated with the greatest histamine effect. Histamine release associated with morphine can cause pruritus and bronchospasm that can be difficult to differentiate from a true allergic reaction. Long-acting fentanyl and oxycodone are considered safer agents in patients with
COPD, but patients should still be monitored for the potential for respiratory depression. In patients with impaired renal or hepatic function, dosages of these agents should be reduced appropriately. Although it had been hoped that inhaled morphine given by nebulizer treatment would reduce respiratory side effects, inhaled morphine does NOT reduce respiratory depression and should not be used in patients with
COPD. Sedation associated with long-acting agents can increase the risk of falls, especially in frail individuals, and may further impair cognitive function in patients with dementia. Constipation problems must often be countered with bowel stimulants, not just with fiber or stool softeners, as tolerance does not develop to this side effect.
Methadone has received increasing attention in the management of chronic pain, both because it
ANSWER BOOKLET: VOLuME 39, NO. 1, JANuARY, 2008 21
is less expensive than the newer long-acting agents and because it may cause less euphoria. Methadone must be prescribed 2-3 times daily for pain relief in contrast to once-a-day dosing used for addiction therapy. Methadone can cause prolongation of the
QT interval, so it should be used with caution in patients with underlying heart block or in patients using other agents that may prolong the QT interval such as tricyclic antidepressants. (Editor’s note: For additional information on prolonged QT interval, see questions/discussions 19 & 20 in the November 2007 issue of Core Content Review.)
Because long-acting opioids do not completely eliminate pain, evaluation of pain management should include both an evaluation of pain reduction and improvement of in quality of life. Pain reduction can be determined using a 1-10 analog scale where patients are asked to indicate their average pain on a daily basis. A reduction in the average daily score indicates improved pain control. Quality-of-life scales such as the Ferrans & Powers Quality-of-Life Index can help to evaluate how pain management strategies impact lifestyle. This scale can be used for general pain conditions and has also been adapted for a number of specific conditions including arthritis.
The risks of medication abuse and diversion have become increasingly recognized problems with longacting opioid formulations. To help minimize these problems, the Federation of State Medical Boards
(FSMB) has recommended that physicians require a signed pain contract for patients at high risk of abuse.
High-risk patients include those with a history of substance abuse or alcohol abuse. The pain contract should include (1) a designated single provider responsible for writing all pain medications,
(2) a list of the medications to be prescribed
(including dose and frequency) and the sole pharmacy at which they are to be filled, (3) a method of preventing medication diversion and abuse, (4) a list of events that will break the contract and possibly preclude further medication prescribing and (5) a requirement that the patient make scheduled visits to de-
termine treatment efficacy (SOR C; Ref. 6). A sample pain contract can be found at the National
Pain Education Council website. No requirement exists for patient registration with the Drug Enforcement Agency (DEA). Because it may be difficult to determine who is at high risk of medication abuse,
22 some advocate the use of a chronic pain contract for
ALL patients on long-term narcotic therapy, although
Arnold, et al., found scant evidence of their benefit on outcomes when performing a systematic review in 2006.
The most frequently recommended method of monitoring medication diversion and abuse is random urine drug screening. Such screenings can be used to determine whether the patient is diverting medication (negative drug screen for opioids) or using nonprescribed or illegal medications (cocaine, benzodiazepines) in addition to the prescribed opioid agent. Drug screening should be performed once or twice a year in patients at high risk of diversion or abuse or in the event a patient exhibits unusual behavior (i.e., altered mental status). In the event the patient does not follow the contract (i.e., an abnormal drug screen, obtaining medications from other providers or multiple pharmacies), the contract may indicate it will be terminated and no other narcotics will be prescribed to the patient; standardization of how to handle contract violations is still unsettled
(the sample contract from the American Academy of
Pain Medicine does not mention consequences for contract violation).
Selected references:
1. Arnold RM, Han PK, Seltzer D. Opioid contracts in chronic nonmalignant pain management: objectives and uncertainties. Am J
Med 2006; 119(4):292-296.
2. Barkin RL, Barkin SJ, Barkin DS. Perception, assessment, treatment, and management of pain in the elderly. Clin Geriatr Med
2005; 21(3):465-490.
3. Ferrans & Powers Quality-of-Life Index Scale. http://www.
uic.edu/orgs/qli/questionaires/questionnairehome.htm Accessed
December 2007
4. Foral PA, Malesker MA, Huerta G, et al . Nebulized opioids use in COPD. Chest 2004; 125(2):691-694.
5. Marcus DA. Tips for managing chronic pain. Postgrad Med J 2003;
113(4):49-66, 98. http://www.postgradmed.com/issues/2003/04_03/marcus.htm
Accessed December 2007
6. National Pain Council Sample Pain Contract. http://www.npecweb.
org/clinicaltoolbox.asp?id=26&selMenu=15,0
Accessed December 2007
7. Rabe KF, Hurd S, Anzueto A, et al.
Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD Executive Summary. Am J Respir Crit
Care Med 2007; 176:532–555. http://www.goldcopd.com/Guidelineitem.
asp?l1=2&l2=1&intId=996 Accessed December 2007
28 C DISCUSSION
Hyperosmolar hyperglycemic syndrome accounts for just over 10,000 hospital admissions per year with a mortality rate that ranges between 10 and 50 percent; it may be the presenting feature for patients not previously diagnosed with diabetes. The incidence of this
THE CORE CONTENT REVIEW OF FAMILY MEDICINE
syndrome is expected to increase since the incidence of type 2 diabetes has increased dramatically over the last few years. The definition of this syndrome is blood glucose level >600 mg/dL, arterial pH level
>7.3, bicarbonate level >15 mEq/L, effective serum osmolality >320 mOsm per kg of water and marked dehydration. The incidence is higher in the elderly.
Patients who develop hyperosmolar hyperglycemic syndrome can present with central nervous system signs such as depressed mental status or coma. Other physical findings include signs of significant fluid depletion such as dry, mouth, poor skin turgor, sunken eyes and tachycardia with or without hypotension.
Weight loss, weakness, abdominal cramps, visual disturbances and polyuria may be present as well.
Because of the severe dehydration that occurs with this syndrome, renal failure, vascular occlusion and/or electrolyte abnormalities can also be present.
Regarding other diagnostic options, renal failure is a possibility with this patient’s longstanding hypertension. As renal function declines in the elderly, mental status can concomitantly decline. In this case, however, renal failure is an unlikely cause of the patient’s change in mental status, given the extreme elevation in blood sugar and the absence of proteinuria. Renal failure could be a secondary complication in this case if the patient’s dehydration was severe and he continued his angiotensin converting enzyme (ACE) inhibitor despite the hyperosmolar hyperglycemic syndrome.
Patients with Alzheimer’s disease have a slow, usually steady decline in their mental capabilities. Dramatic change in their baseline mental status should be investigated for acute triggers, such as elevated blood sugars, infectious diseases, renal failure, cardiac diseases and medications.
Infection can cause an acute change in mental status in older patients. One of the most common infections that can cause acute declines in mental status is urinary tract infections with or without urosepsis.
In this patient, incontinence of urine was an acute change and could indicate a urinary tract infection; however, his urine was negative for leukocyte esterase and nitrates, making this possibility less likely.
Diabetic ketoacidosis (DKA) can occur in patients with type 2 diabetes but is more common in those with type 1 diabetes. In this case, the patient had no ketones in his urine, so the diagnosis of DKA is less likely. To definitively exclude the diagnosis of
DKA, arterial pH and serum ketones would
need to be drawn (SOR C; Ref. 3). Patients who have elevated blood sugars need to be assessed for DKA even if they are type 2 diabetics, since one third of hyperglycemic patients exhibit characteristics of DKA and hyperosmolar hyperglycemia.
Selected references:
1. Kitabchi AE, Umpierrez GE, Murphy MB, et al . Hyperglycemic crises in diabetes. Diabetes Care 2004; 27(Suppl 1):S94-102. http:// www.guideline.gov/summary/summary.aspx?doc_id=4694&nbr=003428&string=hype rglycemia+AND+diabetes Accessed December 2007.
2. Nugent BW. Hyperosmolar hyperglycemic state. Emerg Med Clin
North Am 2005; 23(3):629-648.
3. Stoner, G. Hyperosmolar hyperglycemic state. Am Fam Physician
2005; 71(9):1723-1730. http://www.aafp.org/afp/20050501/1723.html
Accessed December 2007
29 A DISCUSSION
The clinical picture favors an encephalitic process.
The marked lymphocytic pleocytosis and elevated protein in the cerebrospinal fluid (CSF) suggests a viral process. A hemorrhagic temporal lobe lesion combined with increased red blood cells in the cerebrospinal fluid makes this herpes simplex virus (HSV) encephalitis until proven otherwise. In addition to headache, fever and mental status changes, an important clue to herpes simplex encephalitis is localization to the temporal lobe. The diagnosis is also supported by the presence of partial complex seizures (i.e., lips smacking and staring in this case).
HSV encephalitis, although rare (incidence of 1 in
250,000 to 500,000 persons), is the most common identified cause of acute, nonepidemic viral encephalitis in the United States. HSV encephalitis is usually associated with HSV type 1 (HSV-1). Active lesions elsewhere (such as cold sores) are not necessary for and are usually not present at the time of HSV encephalitis diagnosis. Early recognition is critical to permit treatment with intravenous acyclo-
vir (SOR A; Ref 5). Acyclovir is usually started presumptively because the drug is relatively benign, while sequelae from untreated encephalitis can be devastating. The formal diagnosis is made using CSF polymerase chain reaction (PCR) for HSV-1 DNA.
This test is positive in up to 90 percent of cases and has high sensitivity and specificity during the first few weeks of infection. PCR has supplanted the need for a brain biopsy to confirm the diagnosis.
Administration of acyclovir will not interfere with the interpretation of imaging studies or PCR test-
ANSWER BOOKLET: VOLuME 39, NO. 1, JANuARY, 2008 23
ing. Prognosis is directly related to timely initiation of antiviral therapy. Sixty percent of patients who receive early therapy recover with normal function;
90 percent of untreated patients either die or have significant residual neurologic deficits.
Progressive multifocal encephalopathy is typically associated with severe immunocompromise.
Creutzfeldt-Jakob disease, a prion-related disorder, presents as subacute dementia and is associated with startle myoclonus and periodic sharp discharges on electroencephalogram (EEG). Bacterial and tuberculous meningitis typically have different findings on cerebrospinal fluid examination. Bacterial meningitis is associated with polymorphonuclear (PMN) pleocytosis, elevated protein and low glucose in the CSF.
While tuberculous meningitis can have CSF results similar to the case presentation, the CSF white blood cell count and protein are more markedly elevated.
Selected references:
1. Al-Shekhlee A, Kocharian N, Suarez JJ. Re-evaluating the diagnostic methods in herpes simplex encephalitis. Herpes 2006;
13:17-19.
2.de Luca M, Gonzalez Mandly A, Gutierrez A, et al.
Computed tomography perfusion in early imaging diagnosis of herpes simplex virus encephalitis. Acta Radiol 2006; 47:878-881.
3. Domingues RB, Lakeman FD, Mayo MS, et al . Application of the competitive PCR to cerebrospinal fluid samples from patient with herpes simplex encephalitis. J Clin Microbiol 1998; 36:2229-2234.
4. Rimon A, Straussberg R, Amir J. West Nile encephalitis mimicking herpes encephalitis. Pediatr Neurol 2006; 35:62-64.
5. Steiner I, Budka H, Chaudhuri A, et al.
Viral encephalitis: a review of diagnostic methods and guidelines for management. Eur J Neurol
2005; 12(5):331-343.
6. Tyler KL. Update on herpes simplex encephalitis. Rev Neurol
Dis 2004; 1:169-178.
7. Whitley RJ. Herpes simplex encephalitis: adolescents and children.
Antiviral Res 2006; 71:141-148.
30 C DISCUSSION
Bell’s palsy is the most common cause of facial paralysis in the world. It is a sudden, unilateral facial paresis or paralysis of uncertain etiology. The most popular belief is that the facial nerve becomes inflamed and is compressed as it passes through the temporal bone. It is most prevalent in those aged 15-45 years but may occur in any age.
It is important to distinguish Bell’s palsy from other causes of facial weakness such as stroke because misguided treatment may be extremely harmful. In a stroke, the injury occurs to the neuronal cell bodies in the cortex or their axons that project to the motor nucleus of the facial nerve (cranial nerve 7).
24
This is an upper motor neuron lesion and results in a contralateral weakness or paralysis of the lower facial muscles of expression. The contralateral upper facial muscles of expression are unaffected because of the bilateral innervation to the motor nucleus of cranial nerve 7 that innervates the upper facial muscles of expression. Consequently, a patient with a right-sided stroke may present with a left mouth droop and loss of left nasolabial fold but should not have an eyebrow droop or smoothing of the forehead creases.
With Bell’s palsy, the injury is a lower motor neuron lesion to the facial motor nucleus. As a result, the upper and lower facial muscles of expression on the affected side become weak or
paralyzed. The patient will have ipsilateral findings of facial droop, loss of nasolabial fold, eyebrow droop and smoothing of forehead creases. The patient in this question likely has Bell’s palsy. His facial findings, along with the absence of other neurologic deficits, make stroke unlikely.
In general, imaging is not recommended for suspected
Bell’s palsy. In rare instances, magnetic resonance imaging (MRI) or computed tomography (CT) of the facial nerve area may be useful in detecting the source of inflammation. Although the patient’s blood pressure is elevated, he has no symptoms of end-organ damage from uncontrolled hypertension. Intravenous anti-hypertensives would not be indicated. Since the patient is unlikely to have a stroke, aspirin, saline infusion and hospitalization are not necessary. Most researchers have supported a viral, specifically herpes virus, etiology to Bell’s palsy. In some endemic areas,
Lyme disease may be a prominent cause and testing should be considered.
Selected references:
1. Gilden DH. Bell’s palsy. N Engl J Med 2004; 351(13):
1323-1331.
2. Walling AD. New concepts in Bell’s palsy improve treatment options. Am Fam Physician 2005. http://www.aafp.org/afp/20050701/tips/6.
html Accessed December 2007
3. Wang MM. Acute peripheral neurologic lesions. In: Tintinalli JE,
Kelen GD, Stapczynski JS, eds, Emergency Medicine: A Comprehensive Study Guide. 5 th ed. New York: McGraw-Hill, 2000:1475.
31 B DISCUSSION
Although there is no specific cure for Bell’s palsy, management is directed at decreasing the inflammation to the facial nerve and preventing complications.
Studies have shown that steroids have resulted in significantly better outcomes. The proposed mecha-
THE CORE CONTENT REVIEW OF FAMILY MEDICINE
nism is the reduction of inflammation and swelling in the narrow channel through which the facial nerve travels.
Since the herpes virus is believed to be a probable etiology for Bell’s palsy, acyclovir (generic, Zovirax ® ) or famciclovir (Famvir ® ) has frequently been used in the treatment of the disease. Studies showing definitive benefit are lacking, but the American Academy of Neurology (AAN) states that the use of antivirals is safe and possibly effective when combined with prednisone at improving facial functional outcomes.
Despite this recommendation, the largest random- ized trial to date on Bell’s palsy treatment released in 2007 (after the ANN guidelines were published) showed no benefit to acyclovir use, whether used as monotherapy or in combination with steroids. Steroids alone did improve complete recovery at 3 months compared to placebo, from 64 to 83 percent, NNT=5. (SOR
A; Ref. 3)
Most patients with Bell’s palsy will have an improvement in their symptoms within 2 weeks of the onset of symptoms. This is generally true with or without treatment. Twenty to 30 percent of untreated patients, however, may still have symptoms after 3 months and
10 percent may develop permanent symptoms. If steroids are used within 72 hours of symptom onset, 83 percent will fully recover at 3 months and 94 percent will recover by 9 months. In addition, 2-7 percent of patients will experience a recurrence of the disease.
Supportive eye care should be given to patients with
Bell’s palsy. Due to the palsy, affected patients are often unable to completely blink or close their eyelids.
When the eyelid blinks and closes, it moves tears across the surface of the eye, and the closed eyelid retains moisture in and on the surface of the eye during sleep. When the eyelid loses these functions, the cornea is exposed to the environment and dries out.
The eye is also exposed to foreign bodies while sleeping, and an eye patch may be used. Bell’s palsy does not usually cause a decreased production of tears.
Facial nerve decompression for Bell’s palsy is highly controversial. The procedure has severe risks, such as hearing loss and permanent nerve damage. There is no clear evidence that this surgery improves the outcome over prompt medical treatment. Statistics have shown that the procedure has shown no benefit if performed more than 3 weeks after the nerve is damaged.
ANSWER BOOKLET: VOLuME 39, NO. 1, JANuARY, 2008
Selected references:
1. Bell’s palsy: a review of treatment using antiviral agents. Ann
Pharmacother 2006. http://www.theannals.com/cgi/content/abstract/40/10/1838
Accessed December 2007
2. National Institute of Neurological Disorders and Stroke. Bell’s
Palsy Fact Sheet 2007. http://www.ninds.nih.gov/disorders/bells/detail_bells.
htm Accessed December 2007
3. Sullivan FM. Early treatment with prednisolone or acyclovir in
Bell’s palsy. N Engl J Med 2007; 357(16):1598-1607.
4. Tiemstra JD, Khatkhate N. Bell’s palsy: diagnosis and management. Am Fam Physician 2007; 76(7):997-1002. http://www.aafp.org/ afp/20071001/997.html
Accessed December 2007
5. Wang MM. Acute peripheral neurologic lesions. In: Tintinalli JE,
Kelen GD, Stapczynski JS, eds, Emergency Medicine: A Comprehensive Study Guide. 5 th ed. New York: McGraw-Hill, 2000:1475.
32 D DISCUSSION:
The term hemolytic anemia describes anemia where red blood cells are undergoing intravascular or extravascular destruction. Intravascular hemolysis results from endothelial damage, G6PD deficiency, complement activation or infectious agents such as malaria that lead to direct intravascular red cell destruction.
Extravascular hemolysis is much more common and occurs as a result of red cell destruction and removal by macrophages in the spleen and liver. Hemolytic anemias should be considered whenever anemia is accompanied by reticulocytosis and evidence of red cell destruction. Red cell destruction causes increased indirect bilirubin and lactic dehydrogenase (LDH), reduction in haptoglobin and, in severe cases, clinical signs of jaundice.
Evaluation of hemolytic anemias begins with
peripheral smear review (SOR C; Ref. 1). Review of the complete blood count is necessary to exclude platelet or white blood cell abnormalities that can exist concurrently with hemolysis and may indicate malignancy.
While normal red cells are donut-shaped, round and pink, one abnormality that may be seen is the presence of spherocytes, spherically shaped red cells that result from an alteration in the red cell membrane.
This alteration may result from a hereditary defect, as in hereditary spherocytosis, or it may result from antibody-induced membrane alteration. Although these cells are functioning red cells, they are fragile and can be easily damaged while passing through the splenic cords. In the case of hereditary spherocytosis, partial splenectomy has been shown to effectively decrease hemolysis while preserving phagocytic function in the spleen. In the case of antibody-related spherocytosis (evidenced by a positive direct Coombs test),
25
antibodies not only change the red cell membrane but incite macrophage activity in the spleen or liver, leading to red cell destruction. In the clinical scenario above, the patient’s exposure to penicillin could cause antibody-induced membrane changes and spherocytic red cells on the peripheral smear.
Another potential abnormality is schistocytes, which are sharp, fragmented, injured red cells. They are most commonly seen in microangiopathic hemolytic anemia. This form of intravascular hemolysis is caused by endothelial damage, associated with fibrin and platelet adhesion to the damaged endothelium. Examples include eclampsia, hemolytic-uremic syndrome, thrombotic thrombocytopenic purpura, disseminated intravascular coagulation (DIC) and malignant hypertension. Artificial cardiac valves and vascular shunts may also lead to microangiopathic hemolysis.
Pale target cells can be seen in hemolysis associated with hemoglobinopathies like beta-thalassemia. The hallmark of beta-thalassemia is microcytic hypochromic anemia in the absence of iron deficiency. Confirmation of beta-thalassemia is made by hemoglobin electrophoresis. Sickle cells are seen in patients with sickle cell disease that is also detected by electrophoresis. While these patients may simply have fatigue, sickle disease would be suspected if acute vasoocclusive pain crisis, acute chest syndrome or jaundice was present.
Selected references:
1. Dhaliwal G. Hemolytic anemia. Am Fam Physician 2004;
69(11):2599-2606. http://www.aafp.org/afp/20040601/2599.html
Accessed
December 2007
2. Vandendries ER. Drug-associated disease: hematologic dysfunction.
Crit Care Clin 2006; 22(2):347-355, viii.
3. Zetola-Burneo N. Cases from the Osler Medical Service at Johns
Hopkins University. Am J Med 2004; 116(3):198-200.
33 D DISCUSSION
The Framingham risk score is traditionally used to quantify individual risk for coronary artery events.
Recent studies explore whether coronary artery calcium (CAC) scores better predict coronary artery disease (CAD) events than the Framingham score. The
CAC score is obtained using fast computed tomography techniques – electron-beam CT (EBCT) or multidetector CT (MDCT). The ability to noninvasively assess asymptomatic patients becomes important because coronary artery disease (CAD) events occur mainly in patients with moderate to severe atherosclerosis.
In the largest trial of its kind, the St. Francis Heart
Study group prospectively examined 4,903 asymptomatic persons between 50 and 70 years of age.
EBCT scanning was used to calculate CAC scores of all subjects; subjects were followed for 4.3 years. One hundred nineteen study participants suffered a CAD event by the termination of the study. Events included death, nonfatal myocardial infarction (MI), surgical or percutaneous coronary revascularization, nonhemorrhagic stroke and peripheral vascular surgery. The
CAC score predicted CAD events independently of both standard risk factors and C-reactive protein. Additionally, it was statistically superior to Framingham in predicting cardiac events and better stratifying risk for patients in various Framingham categories.
In another study involving 10,746 asymptomatic adults between the ages of 22 and 96 years, CAC scores correlated extremely well with CAD events and remained significant even after adjustment for
CAD risk factors. CAC was associated with CAD events in persons with no CAD risk factors. Increas- ing CAC scores are directly associated with increased risk for CAD events in asymptomatic men and women, though the increase is not
directly related to the score (SOR C; Ref. 5).
There has been some controversy regarding the role of CAC testing. A recent expert consensus document was released by the American College of Cardiology
Foundation and the American Heart Association
Table 7 – Recommendations for the Use of Coronary Artery Calcium Testing
Population
Low CAD risk (<10% estimated
10-year risk)
Intermediate CAD risk (10-20% estimated 10-year risk)
High CAD risk (>20% estimated
10-year risk)
Recommendation
Testing not recommended; general population testing not recommended
May be reasonable to test; such patients may be classified into a higher risk status and management may be modified
Testing not recommended because patients are already at high risk and should receive intensive therapy
26 THE CORE CONTENT REVIEW OF FAMILY MEDICINE
in early 2007. The recommendations are shown in
Table 7.
There is no evidence that intermediate-risk patients who have postscreening CAC results of 0 should reduce the intensity of their treatment of risk factors.
Selected references:
1. American College of Cardiology. ACCF/AHA 2007 clinical expert consensus document on coronary artery calcium scoring by computed tomography in global cardiovascular risk assessment and in evaluation of patients with chest pain. J Am Coll Cardiol 2007;
49(3):378-402. http://www.guideline.gov/summary/summary.aspx?ss=15&doc_ id=10767&nbr=5595 Accessed December 2007
2. Arad Y, Goodman KJ, Roth M, et al.
Coronary calcification, coronary disease risk factors, C-reactive protein, and atherosclerotic cardiovascular disease events. J Am Coll of Cardiol 2005; 46(1):1-8.
3. LaMonte MJ, FitzGerald SJ, Church TS, et al.
Coronary artery calcium score and coronary heart disease events in a large cohort of asymptomatic men and women. Am J Epidemiol 2005; 162:1-9.
4. Michos ED, Nasir K, Braunstein JB, et al.
Framingham risk equation underestimates subclinical atherosclerosis risk in asymptomatic women. Atherosclerosis 2006; 184(1):201-20.
5. Pletcher MJ, Tice JA, Pignone M, et al.
Using the coronary artery calcium score to predict coronary heart disease events. Arch Intern
Med 2004; 164:1285-292
6. Vliegenthart R, Oudkerk M, Hofman A, et al.
Coronary calcification improves cardiovascular risk prediction in the elderly. Circulation 2005; 112:572-577.
34 B DISCUSSION
35 B Diabetes mellitus is common. A wide range of treatment options is now available for its management. Treatment can be divided into lifestyle modifications (to include dietary changes, exercise and smoking cessation), oral medications, injectable hypoglycemics and insulin.
Metformin is a good first choice for the pharmacotherapy of diabetes. It acts by decreasing hepatic glucose production and increasing muscle insulin sensitivity. Because it does not stimulate endogenous insulin secretion, metformin alone will not typically induce hypoglycemia. This is an important benefit in all patients with diabetes, but it is of particular importance in the management of older patients with diabetes where hypoglycemia and an associated loss of consciousness could result in a fall and serious injury.
The 2006 consensus algorithm for the treatment of diabetes states that metformin should be the first- line medication to treat diabetes in all patients
(SOR A; Ref. 2). It typically lowers hemoglobin
A1C by about 1.5 percentage points. Metformin tends to be weight neutral.
The most common adverse effect of metformin is gastrointestinal disturbance. Almost 50 percent
ANSWER BOOKLET: VOLuME 39, NO. 1, JANuARY, 2008 of patients experience nausea, abdominal pain or diarrhea. These adverse effects may be reduced by administrating the medication with meals, starting at a low dose of 500 mg daily and titrating upward slowly over several weeks. The extended-release formulation of metformin has a similar frequency but decreased severity compared to the immediate-release formulation.
Because of this patient’s recent diagnosis of diabetes, recent prescription of metformin and the temporal relationship between the initiation of metformin and the onset of diarrhea, the best first step is to discontinue this medication. Because of the high rate of gastrointestinal complication associated with the use of metformin, patients recently started on the medication should be asked about gastrointestinal symptoms, since many will discontinue their metformin and fail to inform their physician.
According to the prescribing information, metformin is contraindicated in individuals who are at risk of developing lactic acidosis. This includes patients with decreased glomerular filtration rates (serum creatinine concentration of >1.5 mg/dL in men or >1.4 mg/ dL in women [normal, 0.6-1.3 mg/dL]), dehydration, hepatic dysfunction, congestive heart failure or alcoholism. Metformin should also be withheld in individuals with an acute illness severe enough to require hospitalization and perioperatively. It should also be held for 48 hours after radiologic procedures involving contrast media until the serum creatinine concentration has been documented as normal. This is in direct contrast to a Cochrane review published in 2002 that found no increased risk of lactic acidosis (SOR A; Ref. 4).
Stool cultures may be part of the evaluation of this patient but are not an initial action. His blood glucose, while elevated, does not warrant intravenous insulin.
Selected references:
1. Misbin RI, Green L, Stadel BV, et al . Lactic acidosis in patients with diabetes treated with metformin. N Engl J Med 1998;
338:265-266.
2. Nathan JM, Buse JB, Davidson MB, et al . Management of hyperglycemia in type 2 diabetes: A consensus algorithm for the initiation and adjustment of therapy. A consensus statement from the American
Diabetes Association and the European Association for the Study of
Diabetes. Diabetes Care 2006; 29:1963-1972. http://care.diabetesjournals.
org/cgi/content/full/29/8/1963?maxtoshow=&HITS=10&hits=10&RESULTFORM
AT=&fulltext=consensus+algorithm&searchid=1&FIRSTINDEX=0&sortspec=relevan ce&resourcetype=HWCIT
Accessed December 2007
27
3. Saenz A, Fernandez-Esteban I, Mataix A, et al . Metformin monotherapy for type 2 diabetes mellitus. Cochrane Database of Systematic
Reviews 2005; (3)CD002966. http://www.cochrane.org/reviews/en/ab002966.
html
Accessed December 2007.
4. Salpeter S, Greyber E, Pasternak G, et al . Risk of fatal and nonfatal lactic acidosis with metformin use in type 2 diabetes mellitus. Cochrane Database of Systematic Reviews 2002; (2):CD002967. http:// www.cochrane.org/reviews/en/ab002967.html
Accessed December 2007
5. Setter SM, Iltz JL, Thams J, et al . Metformin hydrochloride in the treatment of type 2 diabetes mellitus: a clinical review with a focus on dual therapy. Clin Ther 2003; 25:2991-3026
36 C DISCUSSION
The infant’s most likely diagnosis is transient tachypnea of the newborn (TTN). Tachypnea, associated with grunting and nasal flaring in a term infant delivered via cesarean, supports this diagnosis. Onset usually occurs within hours of birth. Mild cyanosis and retractions are sometimes noted. TTN occurs in both term and near-term infants. It is associated with both prolonged labor (failure to progress) and cesarean section. TTN is thought to result from excess fluid in the lungs. Theories regarding the etiology of the increased fluid include lack of vaginal chest compression (in the case of cesarean section) and the possible role of catecholamines, corticosteroids and other substances.
TTN is associated with prominent perihilar markings on chest x-ray. Fluid may be seen in the fissures. While patchy infiltrates may be present, they generally clear within 48 hours. A diffuse reticulogranular pattern with air bronchograms is more suggestive of respiratory distress syndrome (RDS). Hypoxemia is common with TTN; respiratory failure is rare. Resolution of symptoms occurs within 24 hours in mild cases but may extend beyond 72 hours in severe cases.
Treatment of TTN is supportive. Oxygenation is monitored and supplemental oxygen given as indicated. Intravenous fluids may be necessary in infants whose respiratory status precludes oral feeding. While antibiotics do not alter the course of TTN, they are often given for 48-72 hours until infectious sources are ruled out. Once resolved, TTN does not recur.
Surfactant is helpful with RDS, but not TTN. Corticosteroids have no role. The Cochrane Database of Systematic Reviews states that oral furosemide cannot be recommended as treatment for transient tachypnea of the newborn and it should not be used unless additional data
become available (SOR B; Ref. 3). This recommendation is based on the fact that infants receiving
28 oral furosemide did not have better outcomes (shorter duration of tachypnea, less severe symptoms or shorter hospitalizations) and lost more weight.
TTN has historically not been associated with later respiratory dysfunction. Recent research suggests that this may not be the case. Several studies show an association between TTN and childhood asthma or wheezing. The reason is unclear. Genetic predisposition may be responsible, as maternal asthma is also a risk factor for TTN.
Selected references:
1. Birnkrant DJ, Picone C, Markowitz W, et al. Association of transient tachypnea of the newborn and childhood asthma. Pediatr
Pulmonol 2006; 41(10):978-984.
2. Jain L, Dudell GG. Respiratory transition in infants delivered by cesarean section. Semin Perinatol 2006; 30(5):296-304.
3. Lewis V, Whitelaw A. Furosemide for transient tachypnea of the newborn. Cochrane Database of Systematic Reviews 2002;
(1):CD003064. http://www.cochrane.org/reviews/en/ab003064.html
Accessed
December 2007
4. Liem JJ, Huq IS, Ekuma O, et al. Transient tachypnea of the newborn may be an early clinical manifestation of wheezing symptoms.
J Pediatr 2007; 151(1):29-33.
5. Miller MJ, Fanaroff AA, Martin RJ. Respiratory disorders in preterm and term infants. In: Martin RJ, Fanaroff AA, Walsh MC, eds, Fanaroff and Martin’s Neonatal-Perinatal Medicine. 8 th ed.
Philadelphia: Mosby Elsevier, 2006:electronic version.
37 D DISCUSSION
38 E The U.S. Preventive Services Task Force
(USPSTF) makes recommendations on screening, counseling and preventive medicine topics. Each of the recommendations is graded based on strength of evidence and magnitude of net benefit (benefits minus harms). Grades of recommendations are shown in Table 8. (Editor’s note: This entire discussion is evidence-based and SOR A ).
Breast cancer screening is accomplished by mammography with or without clinical breast exam every
1-2 years for women age >40 years old (B recommendation). Neither teaching self-breast exam nor performing clinical breast exam alone have sufficient evidence to make a recommendation for or against (I recommendation). There is also inconclusive evidence that screening yearly is superior to every other year beyond age 50 years; however, the mortality benefit of mammography is strongest in women between
50-69 years of age.
Colorectal cancer screening in men and women at age
>50 years is strongly recommended (A recommendation). Options for screening include home fecal occult blood testing (FOBT), flexible sigmoidoscopy, FOBT
THE CORE CONTENT REVIEW OF FAMILY MEDICINE
I
D
B
C
Grade
A
Table 8 – USPSTF Grades of Recommendations
Description
The USPSTF strongly recommends that clinicians provide [the service] to eligible patients. The uSPSTF found good evidence that
[the service] improves important health outcomes and concludes that benefits substantially outweigh harms.
The USPSTF recommends that clinicians provide [the service] to eligible patients. The uSPSTF found at least fair evidence that [the service] improves important health outcomes and concludes that benefits outweigh harms.
The USPSTF makes no recommendation for or against routine provision of [the service]. The uSPSTF found at least fair evidence that [the service] can improve health outcomes but concludes that the balance of benefits and harms is too close to justify a general recommendation.
The USPSTF recommends against routinely providing [the service] to asymptomatic patients. The uSPSTF found at least fair evidence that [the service] is ineffective or that harms outweigh benefits.
The USPSTF concludes that the evidence is insufficient to recommend for or against routinely providing [the service]. Evidence that [the service] is effective is lacking, of poor quality, or conflicting, and the balance of benefits and harms cannot be determined.
plus flexible sigmoidoscopy, colonoscopy and air contrast barium enema (ACBE). Each has advantages and disadvantages. The screening interval depends on the method (colonoscopy every 10 years, flexible sigmoidoscopy and ACBE every 5 years, FOBT annually).
Digital rectal exam (DRE) with a single office FOBT is not adequate for screening. Screening for colorectal cancer should begin at age 50 years for those at average risk and earlier in those at higher risk due to a first-degree relative with familial polyposis or with colon cancer diagnosed before age 60 years. Patients with ulcerative colitis are also at increased risk and may warrant screening earlier. (Editor’s note: For additional information about colon cancer risk and ulcerative colitis, see questions/discussions 4 & 5 in this issue.)
Cervical cancer screening in sexually active women with a cervix is strongly recommended (A recommendation). Screening intervals of 1-3 years are recommended. There is a recommendation against screening (D recommendation) after age 65 years in women with adequate recent screening (3 or more documented, consecutive, technically satisfactory normal/negative cervical cytology tests and who have had no abnormal/positive cytology tests within the last
10 years) and no high-risk factors (history of cervical neoplasia, infection with HPV or other sexually transmitted diseases or high-risk sexual behavior). There is also a recommendation against screening women without a cervix if the cause for hysterectomy was benign disease (D recommendation).
Ovarian cancer screening on a routine basis in not recommended (D recommendation); it actually causes harm due to the low disease prevalence and high false-positive rate of currently availability screening tests (bi-manual examination, pelvic ultrasound and
CA-125 screening). In women at average risk, the positive predictive value of an abnormal screening test is, at best, approximately 2 percent (i.e., 98 percent of women with positive test results will not have ovarian cancer).
Hormone therapy (including both estrogen and progesterone replacement and unopposed estrogen replacement) is not recommended for the prevention of chronic disease (D recommendation). Patients should be considered for hormone therapy on an individual basis and the risks and benefits for hormone therapy must be weighed. The patient should share in an informed decision regarding hormone replacement for the treatment of postmenopausal symptoms (mainly vasomotor symptoms).
Evidence is insufficient to recommend for or against screening asymptomatic individuals for lung cancer using low-dose computerized tomography (LDCT), chest x-ray (CXR), sputum cytology or a combination of these (I recommendation).
There is insufficient evidence to recommend for or against screening for type 2 diabetes mellitus, impaired glucose tolerance or impaired fasting glucose in asymptomatic adults on a routine basis (I recommendation). Adults with hypertension or hyperlipidemia should be screened for type 2 diabetes (B recommendation). The optimal interval for screening is not known, but the American Diabetic Association suggests every 3 years, more often in patients with multiple risk factors. The preferred screening test is fasting plasma glucose (FPG) rather than glucose tolerance testing (GTT) because it is easier and faster to perform, more convenient and acceptable
ANSWER BOOKLET: VOLuME 39, NO. 1, JANuARY, 2008 29
to patients and less expensive than other screening tests. If the initial FPG is elevated, confirmatory FPG testing should be done before formally making the diagnosis of diabetes mellitus. Compared with the
FPG test, the 2-hour 75 gram GTT may lead to more individuals being diagnosed as diabetic, due to its higher sensitivity.
Screening for lipid disorders on a routine basis in males age >35 years and females >45 years is recommended (A recommendation). Screening younger adults should be considered if they have other risk factors for coronary heart disease (B recommendation). If screening for lipid disorders, obtaining total cholesterol (TC) and high-density lipoprotein (HDL) measurements is recommended (B recommendation).
There is insufficient evidence to recommend for or against routine triglyceride screening (I recommendation).
In conclusion, there is little evidence to support some of what physicians and patients have considered a complete physical in the past. For example, nowhere in the USPSTF guidelines is there evidence supporting routine complete blood counts, comprehensive metabolic panels, thyroid hormone levels or urinalyses. In fact, the evidence seems to change our focus away from actual head-to-toe physical examination in an asymptomatic individual and instead engage in important preventive medicine advice and utilization of proven screening tests. Of course, each patient should be treated individually, after consideration of all information including medical/surgical history, comprehensive review of systems, family history, social history, risk factors, socioeconomic issues and psychological/spiritual factors.
Selected references:
1. Armstrong K, Moye E, Williams S , et al . Screening mammography in women 40 to 49 years of age: a systematic review for the American College of Physicians. Ann Intern Med 2007; 146(7):516-26.
2. U.S. Preventive Services Task Force Guide to Clinical Preventive
Services, 2005 . AHRQ Publication No. 05-0570, June 2005. Rockville, MD: Agency for Healthcare Research and Quality. http://www.
ahrq.gov/clinic/pocketgd05/
Accessed December 2007
3. White E, Miglioretti DL, Yankaskas BD, et al. Biennial versus annual mammography and the risk of late-stage breast cancer. J Natl
Cancer Inst 2004; 96(24):1832-1839.
39 D DISCUSSION
The history and physical exam findings support a diagnosis of herniated lumbar disc. A history of position-related trauma to the lower back and subsequent radiating leg pain is a typical presentation for
30 this problem. The disc presses on a sacral nerve root that composes part of the sciatic nerve. Other causes of sciatic nerve injury include low back or buttock trauma, fractures of the pelvis or femur, hip dislocation, sacral plexus stretching during vaginal delivery, paraspinous infection and tumors. Less common etiologies include hematoma and inadvertent injection of intramuscular drugs near the plexus. Occasionally, diabetes, alcoholism, syphilis, gout, gonorrhea, arsenic or lead poisoning and inflammatory conditions of the sciatic nerve or component nerve roots are responsible.
At initial presentation, conservative therapy alone is often adequate. Activity restriction for up to 3 days, anti-inflammatory medication or acetaminophen and muscle relaxants are effective first-line modalities in treating acute low back
pain. (SOR A; Ref. 3) Steroid injections may relieve short-term pain but do not provide long-term benefit.
In combination with physical therapy, recovery with conservative management is likely.
In patients with intractable symptoms or a neurological deficit that is evolving, imaging and more aggressive intervention become necessary. In this case, magnetic resonance imaging (MRI) will likely show a herniated intervertebral disc with right L5 nerve root compression. Denervation of affected muscles can be diagnosed using electromyelogram (EMG). Foot drop
(weakness of foot dorsiflexion) results from denervation of the anterior tibialis muscle innervated by the common peroneal nerve. The common peroneal is the most frequently affected branch of the sciatic nerve. When denervation is diagnosed and there are evolving symptoms, surgical intervention may become necessary. While discectomy is commonly performed, newer, less invasive techniques are increasingly employed. Epidural neuroplasty is a minimally invasive procedure that lyses adhesions of the affected nerve root. It is particularly useful in patients with chronic sciatica, poor surgical candidates for discectomy and those with postsurgical sciatic pain. Postsurgical management includes physical therapy for strengthening and a temporary ankle-foot orthosis (AFO) brace to stabilize the foot drop.
Epidural abscess is an infection in the epidural space.
Clinical presentation is often variable. The combination of fever, back pain and neurologic deficits is not present in most patients. The infection is often subtle
THE CORE CONTENT REVIEW OF FAMILY MEDICINE
and atypical on initial presentation. Sequential localized spinal pain is followed by radicular pain, muscle and sensory abnormalities and eventual paralysis.
Paraspinal hematomas are more common following acute trauma and manifest symptoms more rapidly.
Paraspinal tumors and congenital anomalies are not as often linked with back injury and are less acute in symptomatology.
Selected references:
1. Barnsley L. Lumbar epidural corticosteroid injections provided only short-term relief of symptoms and pain in unilateral sciatica.
ACP J Club 2006; 145:15.
2. Katayama Y, Matsuyama Y, Yoshira H, et al.
Comparison of surgical outcomes between macro discectomy and micro discectomy for lumbar disc herniation: a prospective randomized study with surgery performed by the same spine surgeon. J Spinal Disord Tech
2006; 19:344-347.
3. Kinkaid S. Evaluation and treatment of acute low back pain. Am
Fam Physician 2007; 75(8):1181-8. http://www.aafp.org/afp/20070415/1181.
html
Accessed December 2007
4. Manchikaniti L. Role of neuraxial steroids in interventional pain management. Pain Physician 2002; 5:182-199.
5. Veihelmann A, Devens C, Trouillier H, et al.
Epidural neuroplasty versus physiotherapy to relieve pain in patients with sciatica: a prospective randomized blinded clinical trial. J Orthop Sci 2006;
11:365-369.
6. Webster BS, Courtney TK, Huang YH, et al . Survey of acute low back pain management by specialty group and practice experience.
J Occup Environ Med 2006; 48:723-732.
40 D DISCUSSION
41 A The intrauterine contraceptove device (IUD) is an effective, safe, long-acting and reversible method of contraception. Benefits of IUDs include privacy, convenience, spontaneity and that they do not interfere with lactation. Although only 1 percent of women in the United States choose an IUD for contraception, around 10 percent of women worldwide choose this form of contraception.
Types of IUDs include copper, hormone-releasing and inert. The two devices currently available in the
United States are the copper-containing TCu380A
(ParaGard ® ) and the levonorgestrel intrauterine system
(IUS) (Mirena ® , LNg 20). The TCu380A is a T-shaped polyethylene frame around which fine copper wire is wound. The frame is impregnated with barium sulfate, rendering it radiopaque. A 3mm ball at the base of the
T reduces the risk of cervical trauma and attaches to a clear polyethylene monofilament. (See Figure 6.)
Figure 6 – ParaGard IUD
The hormone-releasing IUS is a T-shaped polyethylene frame that contains 52 mg of levonorgestrel and releases 15 mcg of levonorgestrel daily during placement. This device is also radiopaque. (See Figure 7.)
Figure 7 – Mirena IUS
IUD/Ss may be inserted at any time during the menstrual cycle. Obtaining a pregnancy test is recommended, even in women who are certain of their last period. When insertion is performed in the luteal phase (from ovulation until menses), a second form of nonhormonal contraception should be used until the next menses. Routine antibiotic prophylaxis is not indicated, as antibiotics provide little benefit (SOR A; Ref. 4). Prophylaxis is also
ANSWER BOOKLET: VOLuME 39, NO. 1, JANuARY, 2008 31
not indicated during insertion or removal in women at risk for endocarditis (SOR C; Ref.
1).
Duration of efficacy varies by IUD/S type. The
TCu380A is approved for 10 years’ use but is effective for around 12 years. Failure rates at 1 year are 0.5 to 0.8 percent. The cumulative pregnancy rate from
7-12 years is 1.6 to 2.2 percent. The levonorgestrel
IUS is approved for up to 5 years of use but is effective for up to 7 years. With typical use, the first-year pregnancy rate is 0.1 to 0.2 percent. With 7 years’ continuous use, the cumulative pregnancy rate is 1.1 percent
Both methods are extremely cost-effective. Estimated cost (2007) for the Mirena IUS is $412, while Para-
Gard runs around $375. Professional charges for placement vary. Although initial costs of the IUD/S and placement charges are higher than with other types of contraception, the overall cost per year for an IUD/S makes it one of the least expensive contraceptive options. Neither type of IUD/S protects against sexually transmitted disease (STD).
Research is conflicting in terms of which mechanism of action primarily accounts for
the efficacy of IUDs. (SOR B; Ref. 5) The mechanism of action probably involves a combined foreign-body effect and an inflammatory endometrial response that inhibits sperm migration. Copper IUDs raise the copper concentration of cervical mucus.
This impairs sperm motility and reduces the ability of sperm to fertilize an ovum. The levonorgestrel IUS causes atrophy and decidualization of the endometrium and may inhibit sperm survival.
Optimal IUD candidates are parous women in monogamous relationships who desire effective, lowmaintenance and reversible contraception. IUD efficacy increases with advancing age, possibly because fertility rates decrease with age. The IUD is also a good option for women with medical contraindications to estrogen-containing methods. The copper
IUD is useful for women who wish to avoid or have contraindications to hormonal contraception. The copper IUD can also be placed within 120 hours of unprotected intercourse as a form of emergency contraception.
Contraindications to IUD insertion are listed in Table
9. Absolute contraindications include uterine anomalies, recent or recurrent pelvic infections, undiagnosed
32 genital bleeding and pregnancy. Caution is indicated with women at risk for STD or with a history of
STD within the past 3 months. Menstrual disorders may be worsened with copper IUD use. Women who have used an IUD in the past and became pregnant or had IUD expulsion, perforation or heavy bleeding are not disqualified from future IUD use. Nulliparous women in monogamous relationships can safely use either type of IUD. While efficacy rates and risk of infection are similar to those of multiparous women, nulliparas have a higher risk of expulsion and discomfort. Nulliparous IUD users younger than 20 years of age may also have higher failure (pregnancy) rates.
Although IUDs do not increase the risk of infertility or tubal pregnancy per se, women using IUDs who do become pregnant are at increased risk for ectopic gestations. The copper IUD may be used in women with uncomplicated valvular heart disease and other co-morbid illness (diabetes mellitus, migraine, smoking, obesity, epilepsy or thyroid disease). Women with breast cancer, liver or gallbladder disease should not use the levonorgestrel IUS. IUD use is associated with lower risks of endometrial and cervical cancer.
Reasons for early IUD/S removal differ between the two devices. Copper IUDs may increase the risk for pelvic inflammatory disease after exposure. The most common reasons for removal in the first year of use are menorrhagia and dysmenorrhea. While average menstrual blood loss increases over 50 percent with the copper IUD, most women do not develop anemia.
The main reasons for discontinuing the levonorgestrel
IUS are irregular bleeding and amenorrhea. Menstrual flow is decreased by around 40 percent with this IUD.
Dysmenorrhea and menorrhagia are both reduced and the risk of PID may be lessened.
Selected references:
1. American Heart Association. Prevention of Infective Endocarditis. Circulation 2007; 115:1-19. http://circ.ahajournals.org/cgi/reprint/
CIRCULATIONAHA.106.183095v1
Accessed Decmeber 2007
2. Carusi DA, Goldberg AB. Insertion of an intrauterine contraceptive device. In: Rose BD, ed, UpToDate. Wellesley, MA:UpToDate
2007.
3. Dean G, Goldberg AG. The intrauterine contraceptive device. In:
Rose BD, ed, UpToDate. Wellesley, MA:UpToDate 2007.
4. Grimes DA, Schulz KF. Antibiotic prophylaxis for intrauterine contraceptive device insertion. Cochrane Database Syst Rev 2001;
(1):CD001327. http://www.cochrane.org/reviews/en/ab001327.html
Accessed
December 2007
5. Johnson BA. Insertion and removal of intrauterine devices. Am
Fam Physician 2005; 71(1):95-102. http://www.aafp.org/afp/20050101/95.
html Accessed December 2007
6. Stanford JB, Mikolajczyk RT. Mechanisms of action of intrauter-
THE CORE CONTENT REVIEW OF FAMILY MEDICINE
Table 9 – Contraindications to IUD Placement
Absolute contraindications for IUD/S use
• Undiagnosed vaginal bleeding
• Confirmed or suspected pregnancy
• Active, recent (within 3 months) or recurrent pelvic infection
• Genital actinomycosis
• History of ectopic pregnancy
• Acute liver pathology, jaundice
• Known or suspected pelvic malignancy
• Uterine anomaly (bicornuate uterus, cervical stenosis or distorting leiomyomata)
Relative contraindications for IUD/S use
• Risk factors for STD (history of STD, multiple partners)
• Immunodeficiency state, immunosuppressive treatment
• Dysmenorrhea or menorrhagia*
• Copper allergy*
• Wilson’s disease*
• Multiple sexual partners
• Postpartum endometritis/ septic abortion
within 3 months
*Copper IUD
Adapted from Carusi DA, Goldberg AB. Insertion of an intrauterine contraceptive device. In: Rose BD, ed, UpToDate. Wellesley,
MA:UpToDate 2007, and Johnson BA. Insertion and removal of intrauterine devices. Am Fam Physician 2005; 71(1):95-102.
ine devices: update and estimation of postfertilization effects. Am J
Obstet Gynecol 2002; 187(6):1699-1708.
7. Weir E. Preventing pregnancy: a fresh look at the IUD. CMAJ
2003; 169(6):585. http://www.cmaj.ca/cgi/content/full/169/6/585 Accessed
December 2007
42 E DISCUSSION
Recommending NPO (Latin for “nothing by mouth”) after midnight on the day of surgery is believed to have originated in 1946, when Mendelson reported a high incidence of pulmonary aspiration among obstetric patients receiving general anesthesia.
The main reason for preoperative fasting diet is to decrease potential risk of regurgitation and subsequent pulmonary aspiration with development of pneumonia (Mendelson syndrome). This information should be presented to the patient and their understanding of fasting requirements achieved.
There is no specific diet prior to colorectal surgery.
The American Society of Anesthesiologists (ASA) recommends that adults should take their last light meal
(clear liquids and toast) at least 6 hours before having surgery with general anesthesia, regional anesthesia, sedation or analgesia and may have a clear liquid diet up to at least 2 hours prior to surgery. The routine use of gastrointestinal stimulants, antacids, gastric acid secretion blockers, antiemetics and anticholinergics to decrease the risk of pulmonary aspiration in otherwise healthy patients is not recommended.
Patients should be specifically asked about prescription medications, herbal medications and dietary supplements that they may be taking prior surgery. Routinely, any medication containing aspirin, salicylates and/or salicylamides is held 1 week before surgery due to the fact that the lifespan of platelets is 5-10 days and aspirin-induced cyclooxygenase inhibition is irreversible in the anucleate platelet. Vitamin E (alphatocopherol) has an antiplatelet adhesive effect, and the combination of vitamin E with an arachidonic acid inhibitor such as aspirin results in an additive effect upon the suppression of platelet function. Vitamin E has also been shown to inhibit collagen healing and should be discontinued 2 weeks prior surgery.
It is known that 35 percent of the U.S. population use products and services of complementary and alternative medicine, while 19 percent take herbal therapy.
Patients taking traditional Chinese herbal medicines are more likely to have a preoperative event (adjusted relative risk, 2.21; 95 percent
CI, 1.14-4.29) such as hypokalemia or impaired hemostasis (as measured by prolonged INR and activated partial-thromboplastin time) (SOR
B; Ref. 5). Ginseng is known to produce hypoglycemia and to interfere with drugs such as warfarin
(generic, Coumadin ® ). There is evidence that garlic, ginseng, grape seed extract, feverfew and ginkgo can interfere with coagulation. St. John’s wort and echinacea change the metabolism of immunosuppressant and cancer chemotherapy by stimulating/inhibiting hepatic cytochromes.
Specific considerations are usually taken about alcohol intake and tobacco smoking before surgery. Acute alcohol consumption prior to surgery may prolong the duration of action of drugs such as propranolol (generic, Inderal ® ) and phenobarbital. According to Tøn-
ANSWER BOOKLET: VOLuME 39, NO. 1, JANuARY, 2008 33
nesen, et al ., a population that chronically consumed more than 60 grams of ethanol (about 5 drinks) per day had 70 percent postoperative morbidity compared to 11 percent in control group (P < 0.01). Smoking and alcohol abuse were found to be major risk factors for anastomotic leakage after colorectal surgery (relative risks for smoking 3.18 and 7.18 for alcohol abusers). A randomized controlled trial in 1999 revealed that one month of withdrawal from alcohol consumption significantly reduces the rate of
postoperative complications (31 vs. 74 percent, p=0.02) (SOR A; Ref. 7).
Selected references:
1. American Society of Anesthesiologists Task Force on Preoperative
Fasting. Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures. Anesthesiology 1999; 90:896-905. http://www.asahq.org/publicationsAndServices/
NPO.pdf
Accessed December 2007
2. Brady M, Kinn S, Stuart P. Preoperative fasting for adults to prevent perioperative complications. Cochrane Database Syst Rev 2003;
(4):CD004423. http://www.cochrane.org/reviews/en/ab004423.html
Accessed
December 2007
3. Hodges PJ, Kam PC. The peri-operative implications of herbal medicines. Anaesthesia 2002; 57(9):889-99.
4. Kaye AD, Kucera I, Sabar R. Perioperative anesthesia clinical considerations of alternative medicines. Anesthesiol Clin North Am
2004; 22(1):125-39.
5. Lee A, Chui PT, Aun CS, et al.
Incidence and risk of adverse perioperative events among surgical patients taking traditional Chinese herbal medicines. Anesthesiology 2006; 105(3):454-61. http://www.
anesthesiology.org/pt/re/anes/fulltext.00000542-20060900000007.htm;jsessionid=HT qV55zfS0hM2pDxt3MSp74pqvvpJzfy621PDjQt13zmhb1Rm1qT!1071114923!181195
629!8091!1?index=1&database=ppvovft&results=1&count=10&searchid=2&nav=search
Accessed December 2007
6. Soreide E, Ediksson LI, Hirlekar G, et al. Pre-operative fasting guidelines: an update. Acta Anaesthesiol Scand 2005;
49(8):1041-1047.
7. Tonnesen H, Rosenberg J, Nielsen HJ, et al.
Effect of preoperative abstinence on poor postoperative outcome in alcohol misusers: randomised controlled trial. BMJ. 1999 May 15; 318(7194):1311-6. http://www.bmj.com/cgi/content/full/318/7194/1311?maxtoshow=&HITS=10&hits
=10&RESULTFORMAT=&fulltext=misusers+1999&searchid=1&FIRSTINDEX=0& resourcetype=HWCIT
Accessed December 2007
43 E DISCUSSION
44 C Hearing loss is one of the most commonly encountered congenital anomalies. Incidence may be as high as 2-3 per 1,000 live births. Multiple risk factors are associated with congenital hearing loss. A history of neonatal intensive care admission longer than 2 days or a family history of hereditary childhood sensorineural hearing loss (SNHL) is important.
Craniofacial abnormalities or syndromes linked with hearing loss such as Usher (hearing loss and retinitis pigmentosa) or Waardenburg (hearing loss, differently
34 pigmented eyes and skin/hair pigmentary changes) syndromes are also risk factors. Prenatal risks include maternal infection with cytomegalovirus, syphilis, rubella or toxoplasmosis. Maternal gestational diabetes and drug abuse are also linked with hearing abnormalities at birth. Unfortunately, 50 percent of children affected by congenital hearing loss lack identifiable risk factors. Universal newborn screening is proposed as a means for identifying hearing loss earlier in the general population.
Universal newborn hearing screening is recommended by the National Institutes of Health Consensus
Development Conference on Early Identification of
Hearing Impairment in Infants and Children (NIH), the Joint Committee on Infant Hearing, the American
Academy of Pediatrics (AAP) and the Centers for
Disease Control and Prevention (CDC). It is mandatory in 37 states. The U.S. Preventive Services
Task Force (USPSTF) concludes that evidence is insufficient to recommend for or against routine screening of newborns for hearing loss after birth. (SOR C; Ref. 4). A recent Cochrane
Review examines randomized controlled trials comparing universal neonatal screening with either high-risk screening or risk-based screening. The long-term effectiveness of universal screening is not well established at this time.
No large prospective studies compare outcomes of children who are screened using mandatory hearing programs with those managed using a risk-factor approach.
Early detection of hearing loss prevents abnormal development of speech, language and cognition. Studies show that children with hearing loss have significant delays in language development and academic achievement. Without newborn screening, the average age when hearing loss is diagnosed is 2-3 years of age.
Parents may be unaware of hearing deficits because children compensate by using visual cues. One study finds that screening lowers the mean age of diagnosis of hearing loss to 3.9 months. Intervention prior to 6 months of age improves the chances of a hearing-impaired infant developing normal
speech and language (SOR B; Ref. 5). Hearing aids are beneficial in infants as young as 3 months of age.
The two commonly used tests for newborn screening are the automated auditory brainstem response
(ABR) and the otoacoustic emissions test (OAE).
THE CORE CONTENT REVIEW OF FAMILY MEDICINE
ABR evaluates the hearing pathway from the external ear to the lower brainstem. Earphones emit soft clicks presented at 35 decibels. Auditory brainstem response to the clicks is measured using electrodes placed on the infant’s forehead, nape and mastoid. The waveforms detected are compared to normal and a pass/fail result is generated. The ABR is not useful for determining the cause or severity of hearing loss. The
OAE primarily evaluates the cochlea and measures the sounds that are generated by the cochlear hair cells in response to specific acoustic stimuli. A miniature microphone is placed in the infant’s external auditory canal to detect these sounds.
Both ABR and OAE are automated and portable, making them useful for newborn screening. OAE requires less time to set up and administer. It may be performed while the infant is awake, feeding or using a pacifier. OAE is also not influenced by movement artifact. It is dependent on normal middle-ear anatomy, and canal occlusion with vernix results in an abnormal test. ABR must be performed while infants are asleep and still. ABR detects hearing loss in infants with auditory neuropathy; OAE does not.
Infants who fail a newborn hearing screen should receive follow-up testing within 1 month. Although either test may be used for screening, false-positives and -negatives are possible. Using a different type of hearing test is sometimes recommended, although repeat screening with the initial test is also reasonable. If the second test is abnormal, a diagnostic ABR or a diagnostic OAE is recommended. These tests are usually administered by an audiologist. Testing with visual reinforcement audiometry (VRA) is the preferred method of hearing assessment in no-verbal children but cannot be performed reliably in infants prior to 8 months of age.
Selected references:
1. American Academy of Pediatrics Joint Committee on Infant
Hearing. Year 2000 Position Statement: Principles and Guidelines for Early Hearing Detection and Intervention Programs. Pediatrics
2000; 106:798-817. http://www.aap.org/policy/jcihyr2000.pdf
Accessed
December 2007
2. Centers for Disease Control and Prevention. National Center on
Birth Defects and Developmental Disabilities. Hearing loss. http:// www.cdc.gov/ncbddd/dd/ddhi.htm
Accessed December 2007
3. Puig T, Municio A, Meda C. Universal neonatal hearing screening versus selective screening as part of the management of childhood deafness. Cochrane Database of Syst Rev 2005; (2):CD003731. http:// www.cochrane.org/reviews/en/ab003731.html
Accessed December 2007
4. U.S. Preventive Services Task Force. Recommendations and rationale: newborn hearing screening. 2001. http://www.ahrq.gov/clinic/uspstf/ uspsnbhr.htm
Accessed December 2007
5. Wrightson AS. Universal newborn hearing screening. Am Fam
Physician. 2007; 75(9):1349-1352. http://www.aafp.org/afp/20070501/1349.
html Accessed December 2007
45 E DISCUSSION
The U.S. Preventive Services Task Force (USPSTF) concluded in 2006 that evidence is insufficient to recommend routine screening for developmental dysplasia of the hip (DDH) in infants as a means to prevent adverse outcomes. (Rating: I Recommendation). The current literature on screening and treatment for DDH simply suffers too much from significant methodological shortcomings; screening does lead to earlier diagnosis, but the earlier diagnosis does not improve outcomes. The USPSTF concluded that 60 to 80 percent of the newborn hips identified by physical examination and more than 90 percent identified by ultrasonography as abnormal or as suspicious for DDH resolve spontaneously and require no intervention.
The term DDH has replaced the older term, congenital dislocation of the hip, because it is a more accurate representation of the spectrum of anatomic abnormalities in which the femoral head and the acetabulum are aligned improperly or grow abnormally.
Estimates of the incidence of DDH in infants vary between 1.5 and 20 per 1,000 births. Risk factors for
DDH include breech presentation, female sex, positive family history, firstborn status and oligohydramnios.
While risk-factor identification is often sought, the majority of patients diagnosed with DDH have no identifiable risk factor in retrospect; between 1 and 10 percent of infants with risk factors have DDH.
There is no best first test to order when trying to diagnose DDH during the newborn period. One should start with a detailed physical exam, especially in infants determined to be at high risk; the classic Barlow and Ortolani maneuvers are still utilized most frequently despite their
low specificity early in life (SOR C; Ref. 2).
Sensitivity and specificity increase after 3-6 months of age. Serial examination will increase the value of these maneuvers. Ultrasonography has been recommended for infants 6 weeks to 6 months of age to clarify a clinical finding suggestive of DDH, to assess a high-risk infant and to monitor DDH as it is observed or treated.
Despite the high rate of spontaneous resolution, nonsurgical treatment with abduction devices is tra-
ANSWER BOOKLET: VOLuME 39, NO. 1, JANuARY, 2008 35
ditionally used in early treatment (up to 6 months age) and includes the commonly prescribed Pavlik harness. Surgical intervention is used when DDH is severe or diagnosed late or after an unsuccessful trial of nonsurgical treatments. Long-term complications of DDH include premature degenerative joint disease, impaired walking and chronic pain.
Selected references:
1. Shipman SA, Helfand M, Moyer VA, et al . Screening for developmental dysplasia of the hip: a systematic literature review for the
U.S. Preventive Services Task Force. Pediatrics 2006; 117(3):e557-76. http://pediatrics.aappublications.org/cgi/reprint/117/3/e557?maxtoshow=&HITS=10
&hits=10&RESULTFORMAT=&fulltext=review&searchid=1&FIRSTINDEX=0&vol ume=117&issue=3&resourcetype=HWCIT Accessed December 2007
2. Storer S, Skaggs D. Developmental dysplasia of the hips. Am Fam
Physician 2006; 74(8):1310-1316. http://www.aafp.org/afp/20061015/1310.
html
Accessed December 2007
3. U.S. Preventive Services Task Force. Screening for developmental dysplasia of the hip. http://www.ahrq.gov/clinic/uspstf/uspshipd.htm
Accessed
December 2007
46 B DISCUSSION
47 D Acute alcoholic hepatitis involves hepatic injury associated with liver enlargement, inflammation and, often, liver tenderness on clinical examination.
Alcohol’s toxic effects on the liver are extensively described, with oxidative stress, cytokine injury and immunologic factors contributing to hepatic injury.
Histologic features include parenchymal necrosis, varying degrees of steatosis, intra-sinusoidal and pericentral collagen deposition and hepatic infiltration by polymorphonuclear cells. The classic histological feature of alcoholic hepatitis is the presence of Mallory bodies.
Patients with alcoholic hepatitis are often asymptomatic but may present with anorexia, abdominal pain, malaise, fever, weight loss or nausea and vomiting.
Jaundice is often pronounced, especially in patients with repeated episodes of hepatitis. Hepatomegaly with or without mild tenderness is characteristic of alcoholic hepatitis. Patients with severe hepatitis or acute illness superimposed on cirrhosis most likely present with ascites. Palmar erythema and spider angiomas are common.
In acute alcoholic hepatitis, both aspartate amino transferase (AST) and alanine aminotransferase (ALT) are usually elevated; values are generally below 300 IU/mL. Typically, AST is higher than ALT. More than 80 percent of
patients have AST/ALT ratios >2 (SOR C; Ref.
7). Compared with acute viral hepatitis, transaminase
36 levels are only modestly increased. The AST/ALT ratio also helps distinguish alcoholic hepatitis from acute viral hepatitis where the ALT tends to be higher than AST. All patients with elevated liver enzymes should be screened for viral hepatitis. Leukocytosis and an elevated mean corpuscular volume (MCV) are commonly noted. The white blood cell count is often elevated in the 12,000 to 20,000/mm 3 range, although it may be even higher with leukemoid reactions. Thrombocytopenia is often seen; though usually transient, it tends to persist when concomitant cirrhosis is present.
Despite treatment advances, severe alcoholic hepatitis is still associated with 30-40 percent mortality. The
Maddrey Discriminant Function test is the most widely used clinical tool for predicting mortality.
The less complicated Glasgow Alcoholic Hepatitis
Score (GAHS) is gaining increased acceptance due to its relative simplicity and high predictive value for short-term mortality. The scoring system (Table 10) is derived from five independent variables associated with short-term mortality. One study finds that a day 1 GAHS score > 9 has an overall accuracy of 81 percent for predicting 28-day mortality.
The patient described in this question has a number of poor prognostic indicators – age over 50 years,
PT/INR >2, blood urea nitrogen (BUN) > 15 mg/ dL and bilirubin >7.4 mg/dL. The patient does not have typical signs or symptoms suggestive of alcohol withdrawal (e.g., fever, diaphoresis, hallucinations and tremor). His mental status changes are more likely attributed to acute medical illness such as delirium or alcoholic encephalopathy. Although not part of
GAHS, the development of encephalopathy portends poor prognosis.
Despite enormous progress in elucidating the physiology of acute alcoholic hepatitis, less progress has been made in its treatment. Acute alcoholic hepatitis causes significant mortality. It also leads to chronic liver disease and hepatic cirrhosis. About 30 percent of all U.S. deaths from liver disease are alcohol-related.
Numerous controlled trials of medical management of acute alcoholic hepatitis have been done. Agents studied include corticosteroids, anabolic steroids, vitamins, herbal treatment and monoclonal antibodies to TNFα (infliximab, [Remicade ® ]). Most trials are either negative or inconclusive. Current treatment guidelines do not recommend using specific
THE CORE CONTENT REVIEW OF FAMILY MEDICINE
Table 10 – Glasgow Alcoholic Hepatitis Score (GAHS)
Variable
Age (years)
White blood cell count (mm 3 )
Blood urea nitrogen (mg/dL)
Prothrombin time ratio/Internation Normalized Ratio
Total bilirubin (mg/dL)
1
<50
<15,000
<14 mg/dL
<1.5
<7.4
Score
2
>50
>15,000
>14 mg/dL
1.5-2.0
7.4-14.8
3
>2.0
>14.8
Adapted from Forrest EH, Evans CD, Stewart S, et al. Analysis of factors predictive of mortality in alcoholic hepatitis and derivation and validation of the Glasgow alcoholic hepatitis score. Gut 2005; 54:1173-1179. medications to decrease liver inflammation or
reduce the likelihood of secondary cirrhosis
(SOR C; Ref. 6). Supportive care aims to maintain fluid and electrolyte balance while concomitant problems such as infection, renal failure or alcohol withdrawal are addressed. Patients with alcoholic hepatitis require adequate nutritional support, since they are generally malnourished. In one study provision of 3,000 kcal/day was associated with decreased mortality. No benefit exists with parenteral versus enteral feeding.
Alcohol abstinence is the most important factor in both short- and long-term survival. Complete abstinence from alcohol and other potentially hepatotoxic drugs is of primary importance in patients who survive acute alcoholic hepatitis. Individuals with alcohol dependence require appropriate psychosocial treatment. Once acute hepatitis is no longer present, adjunct medical therapies for alcohol dependence
(e.g., naltrexone) are an option for those unable to remain abstinent. Hepatocellular damage may proceed regardless of cessation, however. Only 25 percent of abstinent patients show complete histological normalization on liver biopsy; 15-20 percent ultimately develop cirrhosis.
Selected references:
1. Forrest EH, Evans CD, Stewart S, et al. Analysis of factors predictive of mortality in alcoholic hepatitis and derivation and validation of the Glasgow alcoholic hepatitis score. Gut 2005; 54:1173-1179.
2. Kim WR, Brown S Jr., Terrault N, et al.
Burden of liver disease in the United States: summary of a workshop. Hepatology 2002;
(36):227-242.
3. Mathurin P, Mendenhall CL, Carithers L. Corticosteroids improve short term survival in patients with severe alcoholic hepatitis (AH): individual data analysis of the last three randomized placebo controlled double blind trials of corticosteroids in severe AH. J Hepatol
2002; 36:480-487.
4. Naveau S, Chollet-Martin S, Dharancy S. A double-blind randomized controlled trial of infliximab associated with prednisolone in acute alcoholic hepatitis. Hepatology 2004: 39:1390-1397.
5. O’Shea RS, McCullough AJ. Treatment of alcoholic hepatitis. Clin
Liver Dis 2005; 9(1):103-134.
6. Rambaldi A, Gluud C. Anabolic-androgenic steroids for alcoholic liver disease. Cochrane Database of Systematic Reviews 2006; (4)
CD003045. http://www.cochrane.org/reviews/en/ab003045.html
Accessed
December 2007
7. Sass DA. Hepatitis. Clin Liver Dis 2006; 10(2):219-237.
48 D DISCUSSION
This patient illustrates stroke in the young. The differential diagnosis is quite broad for younger patients compared to more common mechanisms in older patients with the traditional risk factors for stroke
(hypertension, chronic smoking, diabetes mellitus, heart disease and hyperlipidemia). Although oral contraceptives may have contributed to this patient’s cerebral infarction, the absolute risk for this complication is relatively low (1 in 11,000 users); it is more commonly seen in older women who have other risk factors such as chronic smoking, familial predisposition to early atherosclerosis or hyper-coagulability.
Cerebral vasculitis (due to autoimmune disease) and
Moyamoya disease (progressive intracranial vascular stenoses of the circle of Willis, resulting in successive ischemic events) are certainly in the differential diagnosis; however, these are relatively rare disorders and are not typically associated with trauma as in this case. There is no history of illicit drug use, but a drug screen is advisable in a young person presenting with symptoms of stroke. Cocaine is well recognized for its ability to be associated with stroke and myocardial infarction. Epidural hemorrhage, usually due to middle meningeal artery injury, is known for fluctuating levels of consciousness prior to neurologic deterioration; sequelae may include brainstem herniation and death.
Based on the minor neck trauma preceding the event and current findings, the clinical presentation is sup-
ANSWER BOOKLET: VOLuME 39, NO. 1, JANuARY, 2008 37
portive of vertebral artery dissection (VAD). VAD is caused by an expanding hematoma within the vertebral artery wall (intraluminal). The subsequent low-flow state may allow thromboemboli to form, subsequently leading to cerebral infarction. The risk is relatively low, reported to be approximately 2.5-3 cases/100,000. Suspicion of VAD requires immediate neurovascular imaging such as color Doppler ultrasound, magnetic resonance angiography or computed tomograph (CT) angiography to confirm the diagnosis. The intra-arterial cerebral arteriogram remains the gold standard if there is any diagnostic question, but it is generally avoided due to its invasiveness and potential serious complications. Because of the potential for thrombosis propagation from the low-flow state, anticoagulation is the preferred initial treatment if there are no contraindications such
as subarachnoid hemorrhage (SOR C; Ref. 5).
A convincing clinical trial of anticoagulant versus antiplatelet therapy has never been performed. Serial noninvasive studies are used to document response to therapy. Endovascular techniques with stenting are now available as well, and may be considered as a therapeutic option.
Selected references:
1. Beletsky V, Nadareishvili Z, Lynch JL, et al ., for the Canadian
Stroke Consortium. Cervical arterial dissection. Time for a therapeutic trial? Stroke 2003; 34:2856-2860.
2. Hagan IG, Burney K. Radiology of recreational drug abuse. Radiographics 2007; 27:919-940.
3. Nikas D, Reimers B, Eliabetta M, et al.
Percutaneous interventions in patients with acute ischemic stroke related to obstructive atherosclerotic disease or dissection of the extracranial carotid artery.
J Endovas Ther 2007; 14:279-288.
4. Pandian JD, Perel R, Henderson RD, et al.
Unusual triggers for stroke. J Clin Neurosci 2007; 14:786-787.
5. Schievink WI. The treatment of spontaneous carotid and vertebral artery dissections. Curr Opin Cardiol 2000; 15(5):316-21.
6. Williams LS, Biller J. Vertebrobasilar dissection and cervical spine manipulation. A complex pain in the neck. Neurology 2003;
60:1408-1409.
49 A DISCUSSION
50 D Parkinson’s disease is a common, progressive neurodegenerative disorder with an increasing incidence with age; 1 percent of the U.S. population over age 60 years are affected. The pathophysiology involves degeneration of dopaminergic neurons in the substantia nigra and eosinophilic intracytoplasmic inclusions (Lewy bodies) in the residual dopaminergic neurons. The diagnosis is clinical, as no specific laboratory or radiologic test improves diagnostic accuracy.
Bradykinesia, rigidity (often cogwheel) and resting
38 tremor (found in 80 percent of patients, typically
“pill-rolling”) are the cardinal features; asymmetric onset of symptoms, late-onset postural instability, decreased olfaction and micrographia are other typical characteristics. One of the symptoms with the highest positive predictive value (PPV=13) is difficulty rolling over in bed.
The differential diagnosis consists of other disease processes that cause a similar group of symptoms called Parkinsonism but that may have additional signs or symptoms. It is important to evaluate these
Parkinsonism-plus patients carefully, as they may have reversible etiologies. One example is drug-induced
Parkinsonism due to antipsychotics, antiemetics, reserpine or metoclopramide. One study found 20 percent of Parkinson’s disease patients actually had drug-induced Parkinsonism. If the offending agent is stopped, normal function usually returns but may take several months.
In contrast to the relatively benign drug-induced cases, up to 25 percent of patients may have more serious disorders with worse prognoses such as Shy-
Drager syndrome, corticobasal degeneration, progressive supranuclear palsy, dementia with Lewy bodies and normal pressure hydrocephalus. These disorders are suggested by poor response to levodopa as well as the presence of hallucinations, vertical gaze disorders, early dementia or early autonomic dysfunction.
Unlike idiopathic, classical Parkinson’s disease, these patients are often referred early to a neurologist due to the atypical clinical presentation.
Currently, no known medication has been shown to alter the progression of Parkinson’s disease. Hence, medications should begin at the first sign of significant functional impairment. The American Academy of Neurology recommends levodopa or a dopamine agonist for initial therapy. Levodopa is combined with carbidopa in the U.S. because carbidopa inhibits peripheral levodopa metabolism. Levodopa is the most effective medication for motor compli-
cations (40-50 percent symptom reduction) but is limited due to motor fluctuations as the drug wears off and irreversible drug-induced dyskinesias. (SOR
A; Ref. 3, 5). Long-acting versus immediate-release levodopa has similar efficacy. A trial of levodopa should last 3 months with titration aimed at 1,000 mg daily before concluding any patient is levodoparesistant.
THE CORE CONTENT REVIEW OF FAMILY MEDICINE
Dopamine agonists (bromocriptine [generic, Parlodel ® ], pramipexole [Mirapex ® ], ropinirole [Requip ® ], apomorphine [Apokyn ® ]) stimulate the dopamine receptors and also can be used as a first-line medication alone or in combination with levodopa. Dopamine agonists have a lower rate of motor complications but a higher rate of short-term complications such as somnolence, hallucinations and edema. Cochrane
Review states that bromocriptine may be beneficial in delaying motor complications and dyskinesias comparable to levodopa in those who can tolerate the drug (SOR A; Ref. 6).
They reduce motor symptoms by 30 percent. Once motor complications develop, monoamine oxidase
B (MAO-B) inhibitors (selegiline [Eldepryl ® ]) or catechol-O-methyl transferase (COMT) inhibitors
(tolcapone [Tasmar ® ], entacapone [Comtan ® ]) may be added with levodopa to reduce the motor fluctuations. COMT inhibitors inhibit peripheral levodopa metabolism, while MAO-B inhibitors prevent the degradation of dopamine. Amantadine or anticholinergics may improve symptoms during the early stages, but they are not recommended as first-line therapy due to side effects or reduced efficacy.
Patients who are refractory to medications or have contraindications to medications should be referred for neurosurgery evaluation. Thalamotomy and pallidotomy are effective at relieving severe motor symptoms. A recent advance is deep brain stimulation with a surgically implanted device. Surgery is not indicated for mild disease or to augment adequate medication response.
Selected references:
1. Agency for Healthcare Research and Quality. Diagnosis and treatment of Parkinson’s disease: a systematic review of the literature. http://www.ahrq.gov/clinic/epcsums/parksum.htm
Accessed December 2007
2. Dickerson LM, Young SE, Simpson WM, et al . FPIN’s Clinical
Inquiries. Treatment of early Parkinson’s disease. Am Fam Physician 2005; 72:497-9. http://www.aafp.org/afp/20050801/fpin.html
Accessed
December 2007
3. Miyasaki JM, Martin W, Suchowersky O, et al . Practice parameter: initiation of treatment for Parkinson’s disease: an evidence-based review: report of the Quality Standards Subcommittee of the American
Academy of Neurology. Neurology 2002; 58:11-17. http://www.neurology.org/cgi/content/abstract/58/1/11?ijkey=532e4a2532cf4ed2789a9ee8932a7826db2 de362&keytype2=tf_ipsecsha Accessed December 2007
4. Nutt JG, Wooten GF. Clinical practice. Diagnosis and initial management of Parkinson’s disease. N Engl J Med 2005; 353:1021-7.
5. Rao SS, Hofmann LA, Shakil A. Parkinson’s disease: diagnosis and treatment. Am Fam Physician. 2006; 74(12)2046-54. http://www.aafp.
org/afp/20061215/2046.html
Accessed December 2007
6. van Hilten JJ, Ramaker CC, Stowe RL, et al . Bromocriptine versus levodopa in early Parkinson’s disease. Cochrane Database of Systematic Reviews 2000; (3):CD002258. http://www.cochrane.org/ reviews/en/ab002258.html
Accessed December 2007
51 C DISCUSSION
Asymptomatic proteinuria is not uncommonly found on routine urinalysis. Major constituents of normal urine protein include albumin, low-molecular-weight proteins filtered from the blood and larger proteins derived from the urinary tract. Excess urine protein reflects abnormal glomerular permeability that allows leakage of proteins during glomerular filtration.
Microalbuminuria signals early disease when only smaller proteins (albumin) can leak through, hence its preferability for use as a screening test with the microalbumin-to-creatinine ratio. Macromolecules, such as larger proteins, do not escape until later in the disease process when greater glomerular filter damage occurs. If total protein is elevated indicating large molecules are leaking, testing for small molecule leakage (albumin) is redundant. A urine dip stick will usually not turn positive until total protein is being excreted at a rate of 300-500 mg/day or the spot protein is above a concentration of 10 to 20 mg/dL.
Although dipsticks are common first-line urine tests, a positive protein dipstick on a spot urine does not accurately estimate the total quantity of protein excretion in 24 hours. Protein quantification has historically been done with a 24-hour urine collection; however, patients often have a difficult time collecting all their urine for 24 hours and sampling errors are common. The National Kidney Foundation recommends use of spot protein-to-creatinine ratios in place of 24-hour urine collections.
This is an excellent estimate of the daily protein excretion (correlation coefficient r=0.90)
and is much easier to obtain (SOR A; Ref. 1).
First morning void samples are preferred, but random urine samples are also acceptable. This calculation is done by taking the spot urine protein concentration
(mg/dL) and dividing it by the spot urine creatinine
(mg/dL) concentration. The units cancel and the resulting value is in grams protein/day . This distinction is critical, as most clinicians think of protein quantification in milligrams protein/day . Consequently, a ratio of
0.15 gm/day estimates a 24-hour protein excretion of 150 mg/day. Once you have clearly identified the level of proteinuria, the next step in the evaluation should be more apparent. Levels of proteinuria are shown in Table 11.
ANSWER BOOKLET: VOLuME 39, NO. 1, JANuARY, 2008 39
Level
Normal total protein
Microalbuminuria
Trace proteinuria
Mild proteinuria
Moderate proteinuria
Nephrotic range proteinuria
Table 11 – Levels of Proteinuria
Amount Excreted in 24 Hours
<300 mg
30-300 mg (specifically albumin)
150-500 mg
500 mg-1 gram
1-3 grams
>3 grams
An abdominal computed tomography (CT) scan would not clarify the level of proteinuria. Reassurance only after 2 positive screening tests runs the risk of failing to identify a potentially reversible cause of proteinuria and preventing serious morbidity. Referral to a kidney specialist may eventually be indicated but not until basic tests are performed to quantify the severity of the proteinuria and likely etiologies have been evaluated.
Proteinuria may be transient and related to stress, congestive heart failure and dehydration. It can also be associated with exercise, fever and upright posture (orthostatic proteinuria). Less than 1.5 percent of patients with asymptomatic proteinuria will have associated significant renal disease.
Selected references:
1. Assessment of Proteinuria. National Kidney Foundation Guideline
2002. http://www.kidney.org/professionals/KDOQI/guidelines_ckd/p5_lab_g5.htm
Accessed December 2007
2. Gaspari F, Perico N, Remuzzi G. Timed urine collections are not needed to measure urine protein excretion in clinical practice. Am
J Kidney Dis 2006; 47(1):1-7.
3. Lane C, Brown M, Dunsmuir W, et al. Can spot urine protein/ creatinine ratio replace 24 hour urine protein in usual clinical nephrology? Nephrology 2006; 11(3):245-249.
4. Price CP, Newall RG, Boyd JC. Use of protein:creatinine ratio measurements on random urine samples for prediction of significant proteinuria: a systematic review. Clin Chem 2005; 51:1577-1586. http://www.clinchem.org/cgi/content/full/51/9/1577 Accessed December
2007
5. Shidham G, Hebert LA. Timed urine collections are not needed to measure urine protein excretion in clinical practice. Am J Kidney
Dis 2006; 47(1):8-14.
6. Simerville JA, Maxted WC, Pahira JJ. Urinalysis: comprehensive review. Am Fam Physician 2005; 71(6):1153-1162. http://www.aafp.org/ afp/20050315/1153.html
Accessed December 2007
52 C DISCUSSION
53 A Erectile dysfunction (ED) is defined as the persistent inability to attain or maintain penile erection sufficient for sexual intercourse; no suspicion of hypogonadism or hyperprolactinemia should be
40 present. A randomized survey of men aged 40 to 70 years in the late 1980s showed that 52 percent had some form of ED. Other studies estimate that 10 to 20 million men in the U.S. have some degree of ED.
Normal erectile function requires complex interactions between neural and vascular responses elicited by at least two mechanisms. The psychogenic response is initiated centrally in response to various stimuli, while the reflexogenic response results from spinal interactions with penile sensory receptors. Upon arousal, parasympathetic fibers start a cascade that releases nitric oxide (NO) and increases concentrations of cyclic guanosine monophosphate (cGMP).
Increased cGMP relaxes penile vascular and trabecular smooth muscle, resulting in rapid blood flow into the corpus cavernosum and decreased venous outflow.
The rise in intracavernosal pressure causes penile rigidity and erection.
Diabetes and vascular disease are the most common organic causes of ED, accounting for 70 percent of cases. High-density lipoprotein (HDL) levels are inversely correlated with ED; normalizing lipid levels helps to restore erectile function. The prevalence of
ED in diabetes ranges from 27 to 75 percent. Higher rates are noted with advancing age, longer duration of diagnosis, poor glycemic control, obesity and diabetic complications such as neuropathy and retinopathy.
While hypertension is traditionally considered an independent risk factor for ED, a recently completed review of 1,370 men finds that ED may be more closely linked to specific antihypertensive medications rather than hypertension per se. (See Table 12.)
Smoking and obesity are associated with ED. While prevalence of ED is higher in patients who smoke, the rate of ED in former smokers is similar to nonsmokers. The influence of obesity is less clear. A BMI over 28 doubles the risk of ED. Low BMI (<24) is not associated with ED.
THE CORE CONTENT REVIEW OF FAMILY MEDICINE
Antihypertensives
Psychotropic agents
Antidepressants
Endocrine agents
Other Agents
Table 12 – Medications Implicated in Erectile Dysfunction
Diuretics
Beta-blockers
Hydralazine (generic, Apresoline ® )
Centrally-acting alpha agonists
Phenothiazines
Lithium
Benzodiazepines
Tricyclic antidepressants
Selective serotonin reuptake inhibitors
Monoamine oxidase inhibitors
Antiandrogens
Estrogens
Leuteinizing hormone-releasing hormone analogues
Cimetidine (generic, Tagamet®)
Digoxin
Carbamazepine (generic, Tegretol®)
Phenytoin (generic, Dilantin®)
Antiretroviral therapy
<4 METs
Vacuuming
Cooking
Walking 2 mph
Writing
Table 13 – Metabolic Equivalent Units for Various Activities
4-7 METs
Cycling
Climbing a flight of stairs
Golf (without cart)
Walking 4 mph
Yard work
>7 METs
Squash
Jogging (6 mph)
Scrubbing floors
Singles tennis
Treatment of ED begins with a review of the pertinent medical history, with particular attention paid to the above risk factors. Psychological factors are often implicated in ED and, if present, should be addressed as part of the treatment plan. Tobacco cessation and optimizing treatment of hypertension, diabetes and hyperlipidemia reduce the incidence of ED. If the patient is taking medications linked with ED, switching to another medication can be considered.
Men should be healthy enough to engage in sexual activity prior to receiving any pharmacological therapy for ED. Asymptomatic men, including those with risk factors for cardiac disease, do not require coronary evaluation prior to treatment. However, it is reasonable to determine whether a man can perform the equivalent of 4 to 6 metabolic equivalents (METs) of activity before prescribing any therapy. (See Table
13.) Men with anginal symptoms must undergo coronary evaluation prior to treatment for ED.
The American Urological Association (AUA) guidelines states that oral PDE-5 inhibitors, unless contraindicated, be offered as a first-line therapy for erectile dysfunction (SOR A; Ref.
1). The phosphodiesterase enzyme-5 (PDE-5) inhibitors (sildenafil [Viagra ® ], tadalafil [Cialis ® ] and vardenafil [Levitra ® ]) are the mainstay of pharmacological treatment of ED. These medications enhance the effect of natural sexual stimulation by NO-mediated increases in cGMP. No evidence currently supports the selection of one PDE-5 inhibitor over another, although duration of action and other individual characteristics should be taken into consideration when prescribing these medications. (See Table 14.) It is important to note that PDE-5 inhibitors do not work without adequate sexual stimulation and that 4-6 trials with a particular medication and dose may be required before an adequate erection is obtained.
In 2007 the Food and Drug Administration (FDA) added a labeling change to all PDE-5 inhibitors, making the risk of sudden hearing loss more prominent in the product information. While no causal relationship was proven, the FDA felt that evidence was sufficient
ANSWER BOOKLET: VOLuME 39, NO. 1, JANuARY, 2008 41
Characteristic
Trade name
Dosage
Duration of action
Instructions
Adverse effects
Drug interactions
Table 14 – Comparison of Phosphodiesterase Inhibitors
Sildenafil
Viagra ®
Vardenafil
Levitra ®
Tadalafil
Cialis ®
Initial dose 50 mg; decrease to 25 mg if side effects; maximal dose
100 mg
Onset: 30 minutes Duration: up to
4 hours
Take on empty stomach (fat interferes with absorption)
Initial dose 10 mg; 2.5 mg and
5 mg available if lower dose needed; maximal dose 20 mg
Take on empty stomach
Initial dose 10 mg; 5 mg available if lower dose needed; maximal dose 20 mg
Onset: 30 minutes Duration: up Onset: 16 minutes Duration: up to 4 hours to 36 hours
No precautions needed
Flushing (12%), headache (11%), Headache (13%), flushing (10%), Headache (8-14%), dyspepsia dyspepsia (5%), visual disturbance – rhinitis (5%), dyspepsia (4%), blue vision (3%), nasal dizziness (2%), visual
(5-10%), flushing (4-6%), rhinitis
(5%), back pain (6% at 20 mg congestion, rash disturbance (<2%) dose), visual disturbance (<2%), myalgias
CYP-34A inhibitors and inducers can alter levels and efficacy;
CYP-2C9 inhibitors and inducers to a lesser extent; relative contraindication with alpha-blockers
Strong CYP-34A inhibitors may increase blood levels; alpha-blockers may cause hypotension
Strong CYP-34A inhibitors may increase blood levels; alpha- blockers (other than 0.4 mg tamsulosin) may cause hypotension to warrant this change. The sudden-onset hearing loss occurred with or without ringing, vertigo or dizziness and was usually unilateral. Hearing loss was partial or complete. In one third of cases, hearing returned.
The most important drug-drug interaction for PDE-5 inhibitors is concomitant use with nitrates, resulting in severe hypotension. Men taking PDE-5 inhibitors must avoid the use of medications such as nitroglycerin. While a safe interval between administration of a PDE-5 inhibitor and nitrates is not established, the
AUA recommends greater than 24 hours for sildenafil and greater than 48 hours for tadalafil. An accurate medication list is crucial prior to prescribing these medications. Patients should be counseled to disclose use of the drug if they require an emergency department evaluation for chest pain.
An evaluation of cardiovascular status is indicated in men who fail to respond to a PDE-5 inhibitor. In one study of 540 nonresponders, most had uncontrolled hypertension, 40 percent had hyperlipidemia, 25 percent were glucose intolerant and 20 percent were obese. When 121 of these patients achieved treatment goals, 50 percent of hypertensive patients, 60 percent of hyperlipidemic patients and 30 percent of patients with glucose intolerance responded to ED therapy.
Patients who truly do not respond, cannot tolerate or have contraindications to PDE-5 inhibitors may be considered for intracavernosal alprostadil (Cav-
42 erject ® ) or intraurethral alprostadil (Muse ® ) therapy.
Surgical intervention, including penile prostheses, is usually reserved for patients who do not respond to any therapy or have injury-related causes for ED.
No evidence currently supports the effectiveness of yohimbine or other herbal therapies for the treatment of ED; herbal therapies are not recommended
(SOR C; Ref. 1).
Selected references:
1. American Urological Association. The management of erectile dysfunction: an update.
http://www.auanet.org/guidelines/edmgmt.cfm
Accessed December 2007
2. Champion HC. Erectile dysfunction and cardiovascular disease: carrots, sticks, and better men’s health. Adv Stud Med 2006;
6(4):163-70.
3. Food and Drug Administration. Revisions to labels for Cialis,
Levitra and Viagra. http://www.fda.gov/bbs/topics/NEWS/2007/NEW01730.
html Accessed December 2007
4. Francis ME, Kusek JW, Nyberg LM, et al.
The contribution of common medical conditions and drug exposures to erectile dysfunction in adult males. J Urol 2007; 178:591-6.
5. Karnath BM. Preoperative cardiac risk. Am Fam Physician 2002;
66:1889-96. http://www.aafp.org/afp/20021115/1889.html
Accessed December 2007
6. Miller TA. Diagnostic evaluation of erectile dysfunction. Am Fam
Physician 2000; 61:95-104. http://www.aafp.org/afp/20000101/95.html
Accessed December 2007
7. Seftel AD, Mohammed MA, Althof SE. Erectile dysfunction: etiology, evaluation and treatment options. Med Clin North Am
2004; 88(2):387.
8. Sildenafil. In: Nissen D, ed, Mosby’s Drug Consult. St. Louis:
Mosby, Inc., 2004:electronic version.
9. Tadalafil. In: Nissen D, ed, Mosby’s Drug Consult. St. Louis: Mosby,
Inc., 2004:electronic version.
THE CORE CONTENT REVIEW OF FAMILY MEDICINE
10. Vardenafil. In: Nissen D, ed, Mosby’s Drug Consult. St. Louis:
Mosby, Inc., 2004:electronic version.
54 D DISCUSSION
55 A Thrombocytosis (elevated platelet count) is further classified into three categories: primary thrombocytosis (essential thrombocythemia), secondary thrombocytosis (reactive) and pseudothrombocytosis.
The initial step in the evaluation of thrombocytosis is confirming that the platelet count actually is abnormal. Automated complete blood counts (CBCs) occasionally show a factitiously elevated platelet count. On automated tests, red blood cell fragments, microcytic red cells or cryoglobulin protein precipitates may be incorrectly counted as platelets. Pseudothrombocytosis is diagnosed using a peripheral blood smear with manual platelet count.
When the platelet count is truly elevated, reactive thrombocytosis is the most common cause. Platelet counts may become excessively elevated (>1 million) in response to iron-deficiency anemia, acute blood loss, infection or conditions such as inflammatory bowel disease and rheumatoid arthritis. In reactive thrombocytosis, platelets are elevated secondary to increased bone marrow activity. Reactive thrombocytosis does not increase the risk of vascular occlusion per se but does increase the risk for venous thrombosis if immobility is a factor. When a postoperative diagnosis of reactive thrombocytosis is made in a patient who has limited mobility, deep-venous thrombosis (DVT) prophylaxis is indicated. (See
Table 15.) Both unfractionated heparin (UFH) and low-molecular-weight heparin (LMWH) reduce venous thromboembolic events. LMWH is more effective than UFH for reducing deepvenous thrombosis (DVT). UFH is more effective when dosed 3 times a day rather than
twice daily (SOR A; Ref. 8). Evaluation for blood loss, infection, iron-deficiency anemia and inflammatory conditions is also prudent. While elevated
C-reactive protein (CRP) supports the presence of reactive thrombocytosis, it is not a sensitive marker for thrombocytosis itself.
Primary thrombocytosis (essential thrombocythemia) is a disorder in which platelets are produced in the bone marrow at an abnormally high rate. Primary thrombocytosis is further classified as either clonal or hereditary. Clonal thrombocythemias result from an acquired mutation in hematopoietic stem cells, while hereditary thrombocythemia is due to a hereditary mutation. Thrombocythemia must be differentiated from other clonal bone marrow disorders including polycythemia vera and chronic myelogenous leukemia
(CML). These conditions have no primary platelet abnormality; platelet counts are elevated because of rapid marrow production of red or white blood cells.
The World Health Organization (WHO) recently revised the criteria for diagnosing essential thrombocythemia. Proposed criteria are as follows:
1. Sustained platelet count over 450 x 10 9 /L
2. Bone marrow biopsy with megakaryocytic proliferation; no significant increases in neutrophils or erythrocytes
3. Not meeting WHO criteria for polycythemia vera or other myeloid neoplasm
4. Presence of Janus kinase 2 (JAK2) exon 12 mutation ( JAK 2617V>F) or other clonal marker
5. No evidence of reactive thrombocytosis
The JAK 2617V>F exon 12 mutation is found in
50 percent of individuals with essential thrombocythemia; 95 percent and 50 percent of individuals with polycythemia vera and primary myelofibrosis, respectively, also possess this genetic mutation.
Primary thrombocythemia increases the risk of both venous and arterial occlusion. Age (>60 years), history of prior thrombotic events and cardiovascular risk factors are all major predictors for thrombosis in patients
Table 15 – Deep Venous Thromboembolism Prophylaxis for Orthopedic Surgery
Medication
Low-dose unfractionated heparin (UFH)
Low-molecular-weight heparin (LMWH)
• Dalteparin (Fragmin ® )
• Enoxaparin (Lovenox ® )
• Tinzaparin (Innohep ® )
Route
SC
SC
SC
SC
Postoperative Dosing (Daily)
5,000 units every 8 to 12 hours
5000 units starting 12 to 24 hours postoperatively
30 units every 12 hours starting 12 to 24 hours postoperatively
75 units per kg starting 12 to 24 hours postoperatively
ANSWER BOOKLET: VOLuME 39, NO. 1, JANuARY, 2008 43
with primary thrombocythemia. Cardiovascular risk factors include hypertension, smoking, obesity, diabetes and lipid disorders. In low-risk patients, the risk for thrombotic death is minimal. Low-dose aspirin therapy (30 to 500 mg daily) can be used to control symptoms such as hemiparesis, amaurosis fugax and migraines. Patients at low risk have an annual rate of cardiovascular events of 1.9 percent. Using low-dose aspirin for primary prophylaxis of vascular events is useful in polycythemia vera, although formal clinical trials have not been done in primary thrombocythemia. Whether to treat patients at intermediate risk for thrombosis is unclear.
The annual rate of thrombosis in high-risk patients is
10.7 percent. High-risk patients should be considered for cytoreductive treatment in addition to aspirin therapy. Hydroxyurea (HU) is considered the treatment of choice due to its efficacy and rare toxicity.
While associated with an increased risk of leukemia in patients with polycythemia vera, HU risk in primary thrombocytosis is uncertain. Anagrelide (Agrylin ® ), an oral imidazoquinazoline derivative that prevents platelet aggregation, is also available. Anagrelide may be an option for patients who fail hydroxyurea treatment or in those who have concerns about HU’s possible link with leukemia. Hydroxyurea plus aspirin is safer and more effective than the more expensive alternative of anagrelide plus aspirin (SOR B;
Ref. 4). Alfa-interferon is used primarily in patients who fail both hydroxyurea and anagrelide treatment or in patients who are pregnant, as both hydroxyurea and anagrelide are contraindicated in pregnancy. Children with ET are generally treated with aspirin alone unless they have a high risk for thrombosis.
Selected references:
1. Frenkel EP. Sticky platelet syndrome and thrombocythemia. Hematol Oncol Clin North Am 2003; 17(1):63-83.
2. George TI. Pathology of the myeloproliferative diseases. Hematol
Oncol Clin North Am 2003; 17(5):1101-1127.
3. Harrison CN. Essential thrombocythemia. Hematol Oncol Clin
North Am 2003; 17(5):1175-1190, vii.
4. Harrison CN, Campbell PJ, Buck G, et al.
, for the United
Kingdom Medical Research Council Primary Thrombocythemia 1
Study. Hydroxyurea compared with anagrelide in high-risk essential thrombocythemia. N Engl J Med 2005; 353:33-45.
5. Penninga EI, Bjerrum OW. Polycythaemia vera and essential thrombocythaemia: current treatment strategies. Drugs 2006;
66(17):2173-87.
6. Prchal JT. Classification and molecular biology of polycythemias
(erythrocytoses) and thrombocytosis. Hematol Oncol Clin North
Am 2003; 17(5):1151-1158, vi.
7. Tefferi A, Thiele J, Orazi A, et al . Proposals and rationale for revision of the World Health Organization diagnostic criteria for poly-
44 cythemia vera, essential thrombocythemia, and primary myelofibrosis: recommendations from an ad hoc international expert panel. Blood
2007; 110:1092-1097.
8. Wein L, Wein S, Haas SJ, et al . Pharmacological venous thromboembolism prophylaxis in hospitalized medical patients: a metaanalysis of randomized controlled trials. Arch Intern Med 2007;
167:1476-86.
56 B DISCUSSION
57 A An elevation of the white blood cell count
58 C is an important laboratory finding that needs explanation. A first step is to determine the differential of the circulating leukocytes and to review the peripheral blood smear. Mild leukocytosis
(10,000-25,000 cells/µL) in asymptomatic patients with predominant neutrophilia is commonly caused by drugs (see Table 16), hyposplenism, physical and emotional stress or a benign chronic neutrophilia of uncertain cause. Pseudoleukocytosis, caused by ethylenediamine tetraacetic acid (EDTA)-induced platelet clumping, results from platelet clumps being counted as leukocytes by the Coulter counter. Review of the peripheral smear will eliminate this rare occurrence.
Acute infection, acute myocardial infarction and a variety of other major illnesses (diabetic ketoacidosis, bowel infarction, inflammatory bowel disease, pancreatitis, etc.) commonly cause leukocytosis and neutrophilia with a left shift to more immature myeloid cells. In the absence of signs or symptoms of infection, a white blood count greater than
30,000cells/ µ L should raise concern about a leukemic or myeloproliferative process (SOR
C; Ref. 9).
Table 16 – Drugs That Can
Induce Leukocytosis
Steroids
Smoking
Lithium
Beta-agonist, theophylline
Filgrastim (Neupogen ® ) – granulocyte-colony stimulating
factor
Cocaine/methamphetamine
The patient presented in the case history has been ill for at least 2 months. He has palpable lymphadenopathy and atypical mononuclear cells noted on his blood smear. Clearly a neoplastic etiology, a lymphoproliferative disorder would seem highly likely. The tests that would be least helpful as initial evaluation would be either the positron emission tomography
(PET) scan or chest computed tomography (CT) scan,
THE CORE CONTENT REVIEW OF FAMILY MEDICINE
since he has no chest symptoms and a normal chest x-ray. Blood cultures are always important in a febrile patient, and lactate dehydrogenase (LDH) enzyme activity is a critical parameter when considering acute or chronic leukemia and lymphoproliferative diseases.
Epstein-Barr virus titers would not be useful in spite of atypical lymphocytes in the peripheral smear.
Acute leukemia
In acute leukemia, patients generally feel ill with bone pain, bleeding or fever, and 95 percent of these patients will have anemia and/or thrombocytopenia as well. The differential white cell count will show neutrophils and large immature blast cells with little evidence of maturing myeloid precursor cells. This situation is an oncologic emergency and requires immediate referral to a qualified specialist.
Chronic leukemia
Chronic leukemias seldom present as acute emergencies unless white blood cell levels >400,000 cells/ m L cause hyperviscosity symptoms. Urgent leukophoresis and cytoreductive chemotherapy are indicated in this situation. Chronic leukemias are often diagnosed during routine blood tests for other reasons. Hypermetabolic symptoms (low-grade fever, sweats, weight loss) and left upper quadrant discomfort from splenomegaly are the most common symptoms of chronic myelogenous leukemia (CML), while lymphadenopathy and infection are problems are related to chronic lymphocytic leukemia (CLL).
CML is caused by a single translocation of genetic material between chromosome 9 and 22 (Philadelphia chromosome). This translocation results in a mutant protein that is an activated tyrosine kinase that through signaling pathways promotes uncontrolled production of myeloid cells. Imatinib (Gleevec ® ) inhibits tyrosine kinase and is extraordinarily effective in controlling this disease. Imatinib has markedly reduced the number of allogenic bone marrow transplants performed to treat CML.
CLL is a disease of the elderly and behaves indolently in most patients with a median survival approaching 10 years. Hypogammaglobulinemia and
T-cell dysfunction make these patients susceptible to infection. Ten percent of patients with CLL will have disease that transforms to a high-grade, diffuse, largecell lymphoma (Richter’s syndrome) with a poor prognosis despite aggressive therapy. On peripheral smear, CLL will have abnormal circulating lympho-
ANSWER BOOKLET: VOLuME 39, NO. 1, JANuARY, 2008 cytes. Since several other lymphoproliferative disease entities also have abnormal circulating lymphocytes, flow cytometry of the peripheral blood is critical in establishing the correct diagnosis. (See Table 17.) Flow cytometry helps “fingerprint” the protein distribution on the surface of a monoclonal population of cells.
Interpretation of the pattern of protein expression reflects a specific disease. Fortunately, flow cytometry fails to show evidence of a monoclonal population of lymphocytes in benign causes of reactive lymphocytosis including infectious mononucleosis, pertussis, cytomegalovirus, human immunodeficiency virus and toxoplasmosis.
Table 17 – Other Diseases Associated with
Circulating Malignant Lymphocytes
Prolymphocytic leukemia
Hairy cell leukemia
Mantle cell lymphoma
Sézary syndrome (mycosis fungoides)
Splenic lymphoma with circulating villous lymphocytes
T cell large granular lymphocyte leukemia
Follicular lymphoma
Leukemoid reaction
A leukemoid reaction is an elevation of the white blood cell to >50,000 WBC/mm 3 that can be confused with CML. These patients always have a severe underlying disease process (malignancy or disseminated granulomatous infection) and have less immaturity of granulocytic precursors on peripheral smear, an elevated leukocyte alkaline phosphatase (always low in CML) and absence of the 9/22 chromosomal translocation.
Myeloproliferative disease
Polycythemia vera (PV), essential thrombocytosis (ET) and agnogenic myeloid metaplasia (AMM) are part of the myeloproliferative disease syndromes. White blood cell elevation as high as 20,000 cells/ µ L with a predominance of neutrophils can be seen in ET and early AMM. PV can have white cell counts as high as
50,000 cells/µL with a mild left shift that may cause some confusion with CML. Most patients with PV will have an elevated leukocyte alkaline phosphatase and absence of a chromosome 9/22 translocation; most important, patients with PV will have increased red cell mass (hematocrit level >52 percent in white men, >47 percent in blacks and women) (SOR C; Ref. 9).
45
Selected references:
1. Abbott BL. Recent advances in chronic lymphocytic leukemia.
Cancer Invest 2006; 24:302-309.
2. Bain BJ. Diagnosis from the blood smear. N Engl J Med 2005;
353:498-507.
3. Chiorazzi N, Raik R, Ferrarini M. Mechanism of disease: chronic lymphocytic leukemia. N Engl J Med 2005; 352:804-815.
4. Goldman JM, Melo JV. Mechanisms of disease: chronic myeloid leukemia – advances in biology and new approaches to treatment.
N Engl J Med 2003; 349:1451-1464.
5. Pui CH, Relling MV, Downing JR. Mechanism of disease: acute lymphoblastic leukemia. N Engl J Med 2004; 350:1535-1548.
6. Ravandi F, O’Brien S. Chronic lymphoid leukemias other than chronic lymphocytic leukemia: diagnosis and treatment. Mayo Clin
Proc 2005; 80:1660-1674. http://www.mayoclinicproceedings.com/inside.
asp?AID=1073&UID= Accessed December 2007
7. Tefferi A, Barbui T. Bcr/abl-negative, classic myeloproliferative disorders: diagnosis and treatment. Mayo Clin Proc 2005; 80:1220-1232. http://www.mayoclinicproceedings.com/inside.asp?AID=1014&UID=
Accessed
December 2007
8. Tefferi A, Dewald GW, Litzow ML, et al.
Chronic myeloid leukemia: current application of cytogenetics and molecular testing for diagnosis and treatment. Mayo Clin Proc 2005; 80:390-402. http://www.mayoclinicproceedings.com/inside.asp?AID=863&UID= Accessed
December 2007
9. Tefferi A, Hanson C, Inwards D. How to interpret and pursue abnormal complete blood cell count in adults. Mayo Clin Proc 2005;
80:923-936. http://www.mayoclinicproceedings.com/inside.asp?AID=957&UID=
Accessed December 2007
59 E DISCUSSION
60 E The normal pregnant woman is euthryroid,
61 B but significant increases in thyroxine-binding
62 B globulin (TBG) concentration due to estrogen stimulation cause the thyroid gland to enlarge about 13 percent (not large enough to be detected by physical examination) and increase in vascularity.
The follicles enlarge with abundant colloid formation, resulting in follicular hyperplasia and increased synthesis and secretion of thyroid hormone despite a decrease in plasma iodine due to increased renal clearance. Thus, while free thyroid hormone is stable, total body thyroid hormone is increased. In spite of free thyroid hormone levels being stable, the basal metabolic rate is elevated during pregnancy.
TBG levels are elevated 2- to 3-fold by the 12 th week of gestation. Minor elevations of free thyroxine
(T4) and triiodothyronine (T3) in the first trimester correlate directly with HCG levels (HCG has weak thyroid-stimulating activities) and indirectly with serum TSH concentrations (TSH drops appropriately in response to elevated free T3 and T4). By the end of the first trimester, TSH begins to rise again while
HCG falls, and this continues during the remainder of the pregnancy. Despite all of these changes, the serum
46 levels of the free T4, free T3, and TSH remain within the normal nonpregnant range during gestation. Progesterone and human lactogen have no bearing on thyroid hormone levels.
Stimulation of the thyroid follicles by HCG early in pregnancy and the estrogen-induced increases in TBG cause the levels of total T4 and total T3 to rise sharply to a plateau that is maintained until after delivery.
However, the levels of free T4 and T3 are unchanged during pregnancy. There is little to no transplacental passage of T4, T3, or TSH. However, thyroid-stimulating immunoglobulins and thyroid-releasing hormone
(TRH) do cross the placenta.
Overt clinical hypothyroidism is rarely diagnosed in pregnancy, since women with significantly reduced thyroid function are often infertile. Hypothyroidism is usually secondary to Hashimoto’s disease, thyroid surgery/ablation or antithyroid medications. The most sensitive test for the detection of primary hypothyroidism in pregnancy is the measurement of
TSH. However, the American College of Ob- stetricians and Gynecologists states that there is insufficient evidence to warrant testing of asymptomatic pregnant women for hypothy-
roidism (SOR C; Ref. 2). Nonspecific symptoms of hypothyroidism include lethargy, weakness, weight gain, cold sensitivity, and hair loss – all findings that make this a difficult clinical diagnosis, especially during pregnancy. Therapy consists of sufficient thyroid replacement medication. In some women with previously diagnosed hypothyroidism, thyroxine replacement needs can increase by 30 to 50 percent during pregnancy. Patients on thyroid replacement should have their TSH levels checked every trimester during pregnancy (SOR C; Ref. 2,
3). After delivery, thyroxine replacement requirements return to prepregnancy levels over several weeks.
Thyrotoxicosis occurs in 0.2 percent of pregnancies.
Most women with mild to moderate hyperthyroidism tolerate pregnancy well, but severe hyperthyroidism is complicated by spontaneous abortion, premature labor, low birthweight, stillbirth, preeclampsia and heart failure .
The most frequent cause of thyrotoxicosis during pregnancy is Graves’ disease. TSH is decreased in hyperthyroidism with increased levels of free and total T4 and free and total T3. Hyperthyroidism can result from toxic nodular goiter, thyrotoxicosis factitia (surreptitious intake of thyroid hormone) and
THE CORE CONTENT REVIEW OF FAMILY MEDICINE
gestational trophoblastic diseases as seen with an excess of HCG production by hydatiform moles or choriocarcinoma. Suppressed TSH levels also can accompany other conditions. Patients with hyperemesis gravidarum may have a transient increase in serum thyroid levels with a slight decrease in TSH levels.
Hyperthyroidism is generally treated with propylthiouracil (generic, PTU ® ) 100 mg 3 times daily.
Methimazole (Tapazole ® ) is not used due to rare reports of aplasia cutis (congenital focused absence of skin). Beta-blockers may be necessary to control the initial symptoms listed above. PTU treatment usually reduces the thyroid hormone level within 3 to 4 weeks, at which time the dose can usually be reduced.
Thyroid function should be monitored monthly, and the therapeutic goal is the lowest PTU dose needed to maintain maternal thyroid hormone levels in the high-normal range.
Hyperthyroidism may be difficult to recognize because pregnancy itself can lead to a hyperdynamic cardiovascular state and heat intolerance. Total T
4
T
3
levels are increased due to elevated TBG levels, but free T
4
and
values >15 m g/dL strongly suggest hyperthyroidism. During the postpartum period, the mother risks developing new Graves’ disease, a recurrence of previously quiescent Graves’ disease or postpartum thyroiditis. Newborns delivered of mothers with
Graves’ disease can have a state of transient hyperthyroidism due to placental passage of thyroid-stimulating immunoglobulins (TSI).
Thyroid storm can be encountered in undiagnosed or undertreated patients. In pregnancy, it may also follow an infection or surgery or accompany labor and delivery. There is exaggerated hypermetabolism characterized by hyperpyrexia (temperature >103°F), tachycardia out of proportion to the fever and agitation. Blood pressure is usually normal. Atrial dysrhythmia, hypotension, congestive heart failure and cardiovascular collapse are potential complications.
Postpartum thyroid dysfunction often results in subclinical thyroid disease and occurs in
8-10 percent of patients. During pregnancy, there is possible suppression of both humoral and cellular immunity, increasing the likelihood of an autoimmune etiology (such as Hashimoto’s thyroiditis). Early in gestation an underlying autoimmune thyroid disease may improve, then worsen after delivery. Postpartum thyroid dysfunction usually results in hyperthyroid-
ANSWER BOOKLET: VOLuME 39, NO. 1, JANuARY, 2008 ism after delivery, lasting 6-12 weeks postpartum.
The patient may experience fatigue and palpitations before resolving to a euthyroid state or moving into a transient hypothyroidism for 3 to 9 months. Diagnosis is made by the presence of a new-onset abnormal
TSH, free T4 or both. No treatment is usually needed other than symptomatic management of the hyperthyroid state and/or a 6-month course of thyroid replacement therapy for the hypothyroid phase with testing at the end of 6 months. A small percentage of patients do not recover from hypothyroidism and require long-term replacement therapy. Women who have postpartum thyroiditis are likely to have a
recurrence following future pregnancies.
Selected references:
1. Alexander EK, Marqusee E, Lawrence J, et al.
Timing and magnitude of increases in levothyroxine requirements during pregnancy in women with hypothyroidism. N Engl J Med 2004; 351:241.
2. American College of Obstetricians and Gynecologists. Thyroid disease in pregnancy. http://www.guideline.gov/summary/summary.
aspx?ss=15&doc_id=3985&nbr=003124&string=thyroid+AND+pregnancy
Accessed
December 2007
3. Elliot D. Pregnancy: hypertension and other common medical problems. In: Goldman L, Ausiello D, eds, Cecil Medicine. 23 rd ed.
Philadelphia: Saunders Elsevier 2008:electronic version.
4. Ladenson P, Kim M. Thyroid. In: Goldman L, Ausiello D, eds,
Cecil Medicine. 23 rd ed. Philadelphia: Saunders Elsevier 2008:electronic version.
5. Surks MI, Ortiz E, Daniels GH, et al.
Subclinical thyroid disease: scientific review and guidelines for diagnosis and management.
JAMA 2004; 291:228.
6. Yasmeen S, Cress R, Romano PS, et al . Thyroid cancer in pregnancy. Int J Gynaecol Obstet 2005; 91:15.
63 B DISCUSSION
64 A The dizzy patient is always a challenge for a
65 C busy physician. Initial questioning should be
66 B directed at distinguishing true vertigo from other complaints such as weakness, malaise, presyncope, drug effects, cardiovascular or psychiatric symptoms.
Vertigo is a sensation of movement or spinning of either the patient or of his/her surroundings. Once the physician has established that the patient has vertigo, it is important to determine if the vertigo is peripheral or central. Peripheral vertigo is usually not life threatening, but central vertigo has a high rate of morbidity and mortality.
Important history includes onset and duration of symptoms, factors that provoke or worsen it and associated neurological symptoms such as vision or hearing changes, dysarthria, ataxia, weakness or altered
47
level of consciousness. Other important clues include medications, exposure to toxins, history of migraines, trauma, diabetes, hypertension and risk factors for cerebrovascular disease.
Peripheral vertigo refers to disorders in the labyrinth of the ear, where the semicircular canals provide information on angular movement and the otolithic structures (utricle and saccule) give the body’s orientation with respect to gravity. Auditory symptoms such as fullness, tinnitus or hearing loss may be present. Typically, symptoms are of sudden onset, short duration (seconds or minutes; occasionally, hours or days) and intermittent in nature. The vertigo is usually positional. The nystagmus is always horizontal or horizontorotary and it is suppressed by visual fixation on a stationary object. It rarely has associated neurological findings. Repetitive Dix-Hallpike maneuvers will cause the symptoms to fatigue.
Central vertigo refers to any part of the vestibular system in the brainstem or cerebellum. It is usually gradual in onset and the symptoms are continuous and mild and may last weeks or months. Nystagmus may be in any direction and is not suppressed by visual fixation. The vertigo is present in any position.
There are often neurological findings but rarely auditory abnormalities. Repetition of the Dix-Hallpike maneuver does not fatigue symptoms.
An ear, nose and throat exam may show obvious causes of peripheral vertigo such as otitis media, cerumen impaction, vesicles from herpes zoster or cholesteatoma. Pneumatic otoscopy or Valsalva maneuver may cause vertigo in patients with perilymphatic fistula. The patient should be assessed for sensorineural or conductive hearing loss that is commonly seen in peripheral vertigo yet rarely occurs in stroke involving the anterior inferior cerebellar artery.
Ocular examination should include funduscopic exam for increased intracranial pressure and should note direction of nystagmus. Examination of the cranial nerves should always be undertaken. An abnormal cranial exam points toward central pathology; subtle changes in corneal reflex, pupillary reflex or extraocular movements may be the only clues.
The Dix-Hallpike maneuver can be employed to induce vertigo and nystagmus. The Dix-Hallpike is done with the patient seated on the edge of the cot with the head turned 45° toward one side. The patient is then moved rapidly to a supine position with his/ her head slightly extended over the edge of the cot.
As the patient looks toward the ipsilateral direction of the head turn, symptoms may be reproduced along with nystagmus. Caution should be exercised in the elderly, as hyperextension of the neck could induce a vertebral-basilar stroke.
An exam of cerebellar function should also be done including finger-to-finger and finger-to-nose. The patient should be examined as he/she moves from sitting to standing and while standing still to look for the lurching and swaying motion of truncal ataxia. If the patient is able to walk, heel-to-toe tandem gait and general gait should be noted. The typical gait of cerebellar dysfunction is broad-based and staggering with inability to stop or turn precisely. Heel-to-toe walking is impossible. A patient with peripheral vertigo should have normal gait findings.
Table 18 – Distinguishing Peripheral vs. Central Causes of Vertigo
Feature
Nystagmus
Imbalance
Nausea/vomiting
Hearing loss/tinnitus
Peripheral Vertigo
Combined horizontal and torsional; inhibited by fixation of eyes onto object; fades after a few days; does not change direction with gaze to either side
Mild to moderate; able to walk
May be severe
Common
Nonauditory neurologic symptoms
Rare
Latency following provocative Longer (up to 20 seconds) diagnostic maneuver
Central Vertigo
Purely vertical, horizontal or torsional; not inhibited by fixation of eyes onto an object; may last weeks to months; may change direction with gaze toward fast phase of nystagmus
Severe; unable to stand still or walk
Varies
Rare
Common
Shorter (up to 5 seconds)
Reproduced with permission: Labuguen RH. Initial evaluation of vertigo. Am Fam Physician 2006; 73(2):244-51.
48 THE CORE CONTENT REVIEW OF FAMILY MEDICINE
Orthostatic blood pressure changes in patients with vertigo may show autonomic dysfunction or dehydration. Differences of blood pressure between arms may show subclavian steal syndrome that may be related to vertebrobasilar insufficiency.
Laboratory testing is usually not diagnostic or necessary; less than 1 percent of patients have their etiology discovered by lab testing (SOR
C; Ref. 3). Audiometry helps establish the diagnosis of Ménière’s disease if low-frequency hearing loss is found.
Radiologic studies are not needed in patients who clearly have peripheral vertigo (SOR C;
Ref. 3). However, neuroimaging should be done in any patient who has neurological signs or symptoms, risk factors for cerebrovascular disease or progressive unilateral hearing loss. Magnetic resonance imaging
(MRI) is generally preferred over computed tomography (CT) because it is superior in visualizing the posterior fossa where most central causes of vertigo are found. Conventional or magnetic resonance angiography may useful to diagnose vascular causes of vertigo.
Causes of vertigo are shown in Table 19.
References
1. Bauer CA. Jenkins HA. Chapter 126. Otologic symptoms and syndromes. In: Cummings CW, Flint PW, Haughey BH, et al., eds, Cummings: Otolaryngology: Head & Neck Surgery. 4 th ed.
Philadelphia: Mosby, Inc., 2005:electronic version.
2. Chawla N, Olshaker JS. Diagnosis and management of dizziness and vertigo. Med Clin North Am 2006; 90(2):291-304.
3. Labuguen RH. Initial evaluation of vertigo. Am Fam Physician
2006; 73(2):244-51. http://www.aafp.org/afp/20060115/244.html
Accessed
December 2007
4. Olshaker JS. Dizziness and vertigo. In: Marx JA, Hockberger RS,
Walls RM, et al ., eds, Rosen’s Emergency Medicine: Concepts and
Clinical Practice. 6 th ed. Philadelphia: Mosby, Inc., 2006:electronic version.
5. Swartz R, Longwell P. Treatment of vertigo. Am Fam Physician
2005; 71(6):1115-22. http://www.aafp.org/afp/20050315/1115.html
Accessed
December 2007
67 D DISCUSSION
68 A More than 13.5 million people went to the
69 D doctor for shoulder problems in 2003, last
70 C year for which data are available. Acute injuries usually are sports-related from activities with excessive overhead motion such as swimming, tennis, throwing and weightlifting. Some patients will complain of chronic shoulder pain and may have overuse injuries. Some occupations that are prone to overuse injuries include nursing, painting, carpentry, tree pruning, fruit picking and grocery clerking.
One of the most common overuse shoulder injuries is an injury to the rotator cuff muscles. The rotator cuff consists of 4 muscles and their tendons, and it functions to lift and rotate the arm. The four muscles are the supraspinatus, infraspinatus, subscapularis and teres minor. The large muscle forming the rounded contour of the shoulder is the deltoid muscle. (See
Figures 8 & 9.)
Peripheral
• Acoustic neuroma (becomes central as it enlarges)
• Acute otitis media
• Benign positional vertigo
• Cerumen or hair against tympanic membrane
• Cervical spine muscle and ligamentous injury
• Cholesteatoma
• Drug side effect or toxicity
• Foreign body in ear canal
• Herpes zoster oticus
• Labyrinthitis (suppurative, serous, toxic, chronic –
decreased hearing)
• Ménière’s disease
• Motion sickness
• Otosclerosis
• Perilymphatic fistula
• Trauma (labyrinth concussion)
• Vestibular neuronitis (intact hearing)
Table 19 – Causes of Vertigo
Central
• Cerebellar hemorrhage or infarction
• Drug side effect or toxicity
• Infection (encephalitis, meningitis, brain abscess)
• Multiple sclerosis
• Postconcussive syndrome
• Post-traumatic injury (temporal bone fracture)
• Subclavian steal syndrome
• Temporal lobe epilepsy
• Toxins
• Tumor
• Vertebral basilar artery insufficiency
• Vertebral basilar migraine
• Vitamin B
12
deficiency
ANSWER BOOKLET: VOLuME 39, NO. 1, JANuARY, 2008
Systemic
• Diabetes mellitus
• Hypothyroidism
49
Figure 8 – Muscles of the Rotator Cuff
(Anterior View) against resistance suggest an injury to the supraspinatus. Sensitivity and specificity for this test are 84-89 percent and 100 percent, respec-
tively. (See Figure 10.)
Figure 10 – Empty Can Test
Figure 9 – Muscles of the Rotator Cuff
(Posterior View)
The main function of the subscapularis is internal rotation. This muscle is tested with the patient’s arm rotated behind the back at mid-lumbar level. Pain and weakness as the patient attempts to lift the hand away from the back suggest an injury to the subscapularis.
(See Figure 11.) Alternatively, the examiner can hold the positioned arm away from the back and then let go. The test is abnormal if the patient ca not maintain the position and the dorsum of the hand rests on the back. Sensitivity and specificity of this test are 62 percent and 100 percent, respectively. For the patient who cannot place his/her hand on his/her back, a modified test can be done with the hand placed on the abdomen and the patient resisting external rotation of the arm by the examiner.
Figure 11 – Lift-Off Test
Reprinted with permission. Anderson BC, Martin T, Martin S. Rotator cuff tear. In: Rose BD, ed, UpToDate. Wellesley, MA:UpToDate
2003.
The shoulder joint has the greatest range of motion of any joint in the body. Shoulder motions include flexion, extension, external rotation, internal rotation, arm abduction and arm adduction. Physical examination with shoulder range of motion and strength testing is helpful to determine which muscles are involved.
The supraspinatus is primarily responsible for arm abduction (along with the deltoid). It can be tested with the patient’s arm in 90° of abduction, 30° of forward flexion and internal rotation (thumb points down). Known as the empty can test, pain and weakness with downward pressure on the arm
50 THE CORE CONTENT REVIEW OF FAMILY MEDICINE
The infraspinatus and teres minor muscles are mainly responsible for external rotation. These muscles are tested with the patient’s arm adducted against the body, elbow flexed at 90°. Pain and weakness as the patient pushes outward with his/her hand against resistance from the examiner suggest an injury to the infraspinatus or the teres minor. (See Figure 12.)
Figure 12 – Testing of Infraspinatus and
Teres Minor Muscles
Rotator cuff tears increase in frequency with age and are more common in the dominant arm. The high- est incidence occurs in patients over 60 years of age. Less than 1 percent of all shoulder injuries in persons younger than 30 years result in complete rotator cuff tears. However, 35 percent of such injuries in patients older than
45 years of age result in complete rotator cuff
tears. Common injuries leading to a rotator cuff tear include a fall onto an outstretched arm, direct blow to the shoulder and a rapid accelerating injury such as pulling on a lawnmower starter cable.
Ninety-five percent of tears are caused by mechanical impingement as a result of repetitive overhead activities, acute trauma or subtle instability (atraumatic instability). Inflammation of the rotator cuff tendons and/or bursa caused by irritation against the coracoacromial arch may progress to a complete rotator cuff tear over time. An intrinsic degenerative process in the distal supraspinatus tendon may also be an important contributing factor. Although rotator cuff pathology is frequently associated with mechanical impingement, the impingement process may also be superimposed on intrinsic degenerative change that develops within the distal supraspinatus tendon with advancing age.
ANSWER BOOKLET: VOLuME 39, NO. 1, JANuARY, 2008
Selected references:
1. Clark RJ, Marchessault J, Sizer PS, et al. Isolated traumatic rupture of the subscapularis tendon. J Am Board Fam Pract 2002; 15:204-208. http://www.jabfm.org/cgi/reprint/15/4/304.pdf
Accessed December 2007
2. Deu RS, Carek PJ. Common sports injuries: upper extremity injuries. Clin Fam Pract 2005; 7(2):249-265.
3. Stevenson HJ, Trojian T. Evaluation of shoulder pain. J Fam Pract
2002; 51(7):605-611. http://www.jfponline.com/Pages.asp?AID=1234&issue=Ju ly_2002&UID= Accessed December 2007
4. Woodward TW, Best TM. The painful shoulder. Part I. Clinical evaluation. Am Fam Physician 2000; 61(10):3079-3088. http://www.
aafp.org/afp/20000515/3079.html
Accessed December 2007
71 C DISCUSSION
72 A Cervical spine injuries most commonly occur
73 B from falls or deceleration motor vehicle acci-
74 E dents. The cervical spine is composed of 7 discs. The first cervical vertebra, the atlas, has no vertebral body. Instead, it is a ring of bone composed of a thick anterior arch, two lateral masses and a thin posterior arch. (See Figure 13.) The second cervical vertebra, the axis, contains the odontoid process
(dens) that articulates through the ring of the atlas and is attached to the anterior arch by the transverse ligament. (See Figure 14.) The vertebrae are joined by a complex network of ligaments. (See Figure 15.)
As a unit, the cervical spine can be divided into 3 columns: anterior, middle and posterior.
Anterior column: anterior longitudinal ligament; anterior two thirds of the vertebral bodies, annulus fibrosis and intervertebral discs
Middle column: posterior longitudinal ligament; posterior one third of the vertebral bodies, annulus fibrosis and intervertebral discs
Posterior column: pedicles, transverse processes, articulating facets, laminae, spinous processes and spinal cord
Figure 13 – First Cervical Vertebra (Atlas)
51
Figure 14 – Second Cervical Vertebra (Axis) Odontoid (dens) fractures (see Figure 16) result from a combination of mechanisms of injury (flexion, extension and rotation). Patients often complain of pain with neck movement and that the head feels unstable on their spine (the patient in answer option A). Type
I fractures involve avulsion fractures of the tip of the odontoid process Type II fractures are the most common and involve the base of odontoid process. Type
III fractures extend into the body of the axis. This type of injury is considered unstable with a
significant likelihood of spinal cord injury. An odontoid radiograph (open mouth view) is sometimes necessary for visualization. (See Figure 17.)
Figure 16 – Odontoid fractures
Odontoid Fracture Type I
Figure 15 – Longitudinal View of Upper
Cervical Spine
Odontoid Fracture Type II
Odontoid Fracture Type III
The cervical spine is susceptible to 4 mechanisms of injury – flexion, extension, compression and rotation. Injury may also results from a combination of mechanisms.
52 THE CORE CONTENT REVIEW OF FAMILY MEDICINE
Figure 17 – Odontoid View While commonly associated with activities such as shoveling (snow, gravel, etc.) or using a pickax or scythe, it is named for its historical occurrence in clay miners. Avulsion fractures may also result from a direct blow to the spinous process. Clay shoveler’s fracture is a stable fracture and not associated with neurologic impairment. No treatment is usually necessary.
Figure 19 – Clay shoveler’s fracture
Reproduced with permission from the Emergency Medicine
Residency at New York Presbyterian-The University Hospital of
Columbia & Cornell.
Flexion injuries often results from head-on collisions and falls where there is rapid and forceful cervical spine flexion. Two common flexion injuries are bilateral facet dislocation and Clay shoveler’s fracture.
Bilateral facet joint dislocation (see Figure 18) disrupts the annulus fibrosis, anterior longitudinal ligament and posterior ligamentous complex. On lateral radiograph of the cervical spine, the affected area shows anterior displacement of the vertebra over the vertebra below.
This injury is extremely unstable and is associated with hyperflexion injuries. It has a strong
association with spinal cord injury. Patients are often neurologically intact at the time of injury only to develop neurologic sequelae (muscle weakness or quadriplegia) within hours to days
(as in the patient in answer option B).
Figure 18 – Bilateral Facet Joint Dislocation
Compression injuries (see Figure 20) occur after diving into shallow water (patient in answer option D) or receiving a forceful blow to the top of the head.
The compressive force causes the vertebra to shatter outward (burst fracture). Most fractures do not involve the posterior column (spinal cord) and, therefore, are stable. However, fractures with significant com-
pression, including burst fractures (see Figure
22), require computed tomography (CT) or magnetic resonance imaging (MRI) to evaluate for middle column retropulsion into the posterior column.
Figure 20 – Compression fracture
An avulsion fracture from the base of the spinous process is called a Clay shoveler’s fracture. (See Figure
19.) It usually occurs when abrupt neck flexion causes the supraspinous ligament to pull on the process with enough force to split off a piece of the bone
(the patient in answer option C). Pain is generally described as knife-like at the level of the fracture.
ANSWER BOOKLET: VOLuME 39, NO. 1, JANuARY, 2008 53
Figure 21 – Burst Fracture Extension injuries typically result from rear-end motor vehicle collisions and blows to the front of the skull. Despite the historical origin of the name, a Hangman’s fracture (see Figure 22) most commonly results from motor vehicle accidents causing hyperextension of the neck. In the case presented in answer option E, the impact from the dashboard likely caused hyperextension. The injury results in bilateral fractures through the pedicles of the second vertebrae. Although the fracture is considered unstable, neurologic injuries are unusual because the anteroposterior diameter of the spinal canal is greatest at this level.
Figure 22 – Hangman’s fracture
Reproduced with permission from Learning Radiology.com.
Selected references:
1. Graber MA, Kathol M. Cervical spine radiographs in the trauma patient. Am Fam Physician 1999; 60(5):1318-1322.
2. Hecht AC, Salcox DH, Whitesides TE. Injuries of the cervicocranium. In: Browner BD, Jupiter JB, Levine AM, et al., eds, Skeletal
Trauma: Basic Science, Management, and Reconstruction. 3 rd ed.
Philadelphia: WB Saunders Co., 2003:electronic edition.
3. Mirza SK, Anderson PA. Injuries of the lower cervical spine. In:
Browner BD, Jupiter JB, Levine AM, et al., eds, Skeletal Trauma: Basic
Science, Management, and Reconstruction. 3 rd ed. Philadelphia: WB
Saunders Co., 2003:electronic edition.
4. Wheeless’ Textbook of Orthopedics. Duke Orthopedics. http://www.
wheelessonline.com/ortho/cervical_spine
Accessed December 2007 p74pqvvpJzfy621PDjQt13zmhb1Rm1qT!1071114
54 THE CORE CONTENT REVIEW OF FAMILY MEDICINE
The Core Content Review of Family Medicine
Index of Subjects – January 2008
1 1 Measuring blood pressure
1 2 Co-sleeping
1 3 Asbestos exposure
1 4 Ulcerative colitis
1 5 Ulcerative colitis
1 6 Hip fracture
1 7 Management of hip fracture
1 8 Nonalcoholic steatohepatitis
1 9 Debilitating fatigue in cancer patients
10 Debilitating fatigue in cancer patients
11 Orbital trauma
12 Missed diagnosis of appendicitis
13 Sexual intercourse during pregnancy
14 Sexual intercourse during pregnancy
15 Preventing childhood injury
16 Dyspepsia
17 Adult cancer screening
18 Adult cancer screening
19 Antidepressant failure
20 Hypertensive urgency
21 Third trimester bleeding
22 Third trimester bleeding
23 Third trimester bleeding
24 Recognizing occupational asthma
25 Medial epicondylitis
26 Chronic pain management
27 Chronic pain management
28 Hyperosmolar hyperglycemia
29 Herpes simplex encephalitis
30 Bell’s palsy
31 Bell’s palsy
32 Hemolytic anemia
33 Coronary artery calcium
34 Metformin
35 Metformin
36 Transient tachypnea of the newborn
37 Adult female preventive services
38 Adult female preventive services
ANSWER BOOKLET: VOLuME 39, NO. 1, JANuARY, 2008
39 Herniated lumbar disc
40 Intrauterine contraception
41 Intrauterine contraception
42 Preoperative diet
43 Newborn hearing screening
44 Newborn hearing screening
45 Developmental dysplasia of the hip
46 Alcoholic hepatitis
47 Alcoholic hepatitis
48 Vertebral artery dissection
49 Parkinson’s disease
50 Parkinson’s disease
51 Asymptomatic proteinuria
52 Erectile dysfunction
53 Erectile dysfunction
54 Thrombocytosis
55 Thrombocytosis
56 Leukocytosis
57 Leukocytosis
58 Leukocytosis
59 Thyroid disease during pregnancy
60 Thyroid disease during pregnancy
61 Thyroid disease during pregnancy
62 Thyroid disease during pregnancy
63 Vertigo
64 Vertigo
65 Vertigo
66 Vertigo
67 Shoulder examination
68 Shoulder examination
69 Shoulder examination
70 Shoulder examination
71 Cervical fractures
72 Cervical fractures
73 Cervical fractures
74 Cervical fractures
75 Cervical fractures
55
56 THE CORE CONTENT REVIEW OF FAMILY MEDICINE