403
Page 1
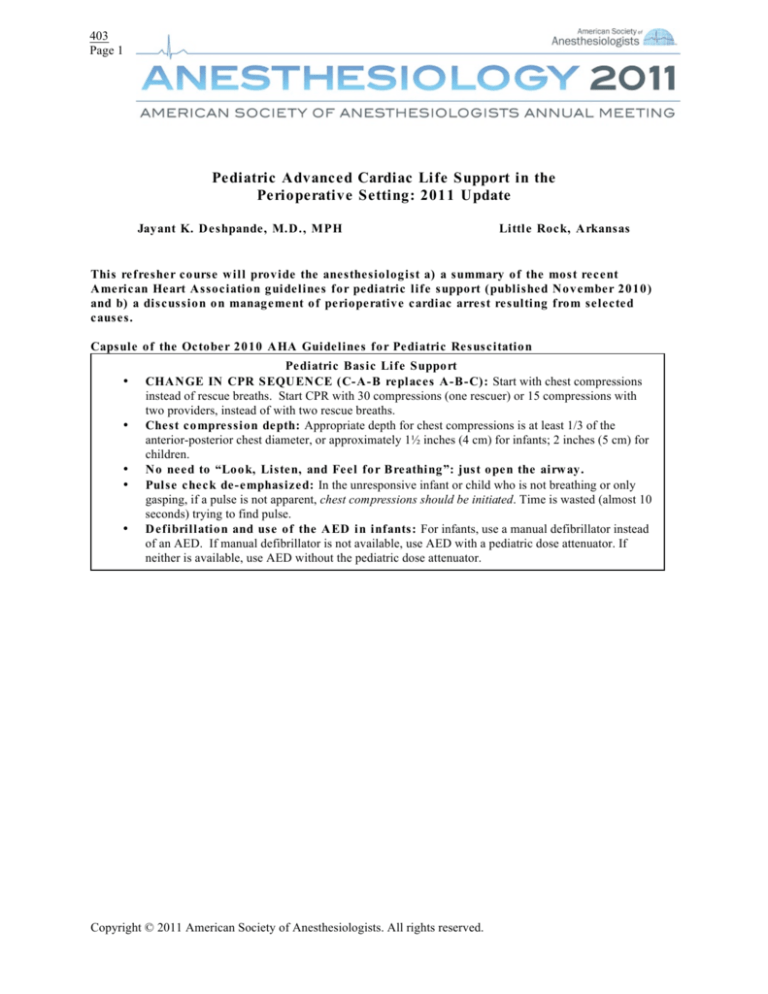
Pediatric Advanced Cardiac Life Support in the
Perioperative Setting: 2011 Update
Jayant K. Deshpande, M.D., MPH
Little Rock, Arkansas
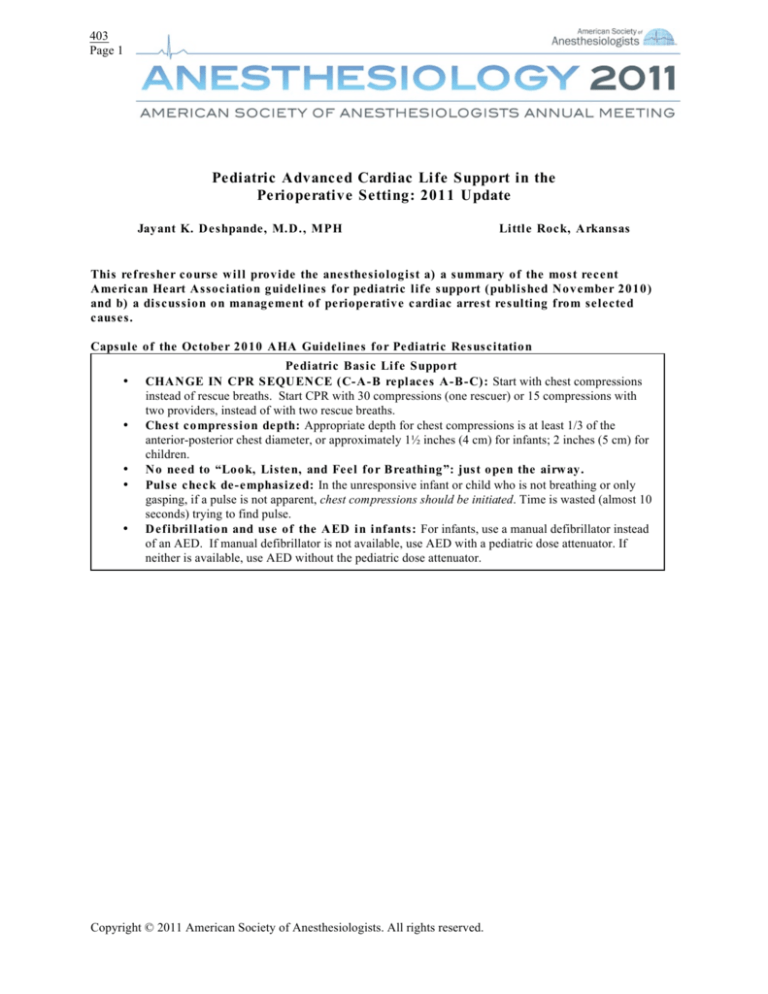
This refresher course will provide the anesthesiologist a) a summary of the most recent
American Heart Association guidelines for pediatric life support (published November 2010)
and b) a discussion on management of perioperative cardiac arrest resulting from selected
causes.
Capsule of the October 2010 AHA Guidelines for Pediatric Resuscitation
•
•
•
•
•
Pediatric Basic Life Support
CHANGE IN CPR SEQUENCE (C-A-B replaces A-B-C): Start with chest compressions
instead of rescue breaths. Start CPR with 30 compressions (one rescuer) or 15 compressions with
two providers, instead of with two rescue breaths.
Chest compression depth: Appropriate depth for chest compressions is at least 1/3 of the
anterior-posterior chest diameter, or approximately 1½ inches (4 cm) for infants; 2 inches (5 cm) for
children.
No need to “Look, Listen, and Feel for Breathing”: just open the airway.
Pulse check de-emphasized: In the unresponsive infant or child who is not breathing or only
gasping, if a pulse is not apparent, chest compressions should be initiated. Time is wasted (almost 10
seconds) trying to find pulse.
Defibrillation and use of the AED in infants: For infants, use a manual defibrillator instead
of an AED. If manual defibrillator is not available, use AED with a pediatric dose attenuator. If
neither is available, use AED without the pediatric dose attenuator.
Copyright © 2011 American Society of Anesthesiologists. All rights reserved.
403
Page 2
•
•
•
•
•
•
•
•
[Type text]
[Type text]
Pediatric Advanced Life Support
Monitor exhaled CO2: In addition to clinical assessment, use exhaled CO2 detection
(colorimetry or capnography) to confirm tracheal tube position for patients with a perfusing rhythm
in all settings and during interhospital/intrahospital transport. Continuous monitoring, when
available, can be beneficial during CPR to gauge effectiveness of chest compressions.
Defibrillation energy doses: Initial dose is 2-4 J/kg. For refractory VF, dose may be increased
start with 4 J/kg (biphasic) up to but not to exceed 10 J/kg (maximum dose 360 J monophasic).
Limit supplemental oxygen to minimum levels needed after resuscitation:
Oxyhemoglobin saturation (SpO2) should be monitored following return of circulation. Titrate the
FiO2 to maintain an SpO2 ≥ 94%.
Resuscitation of infants and children with congenital heart disease: The guidelines
include resuscitation measures for cardiac arrest in infants and children with single-ventricle
anatomy, Fontan or hemi-Fontan / bidirectional Glenn physiology, and pulmonary hypertension.
Medications during cardiac arrest and shock: The routine use of calcium during pediatric
cardiopulmonary arrest is not recommended. Calcium may be used to treat documented
hypocalcemia, calcium channel blocker overdose, hypermagnesemia, or hyperkalemia. In septic
shock, etomidate is not recommended.
Post-cardiac arrest care: Therapeutic hypothermia (32°C-34°C) may provide benefit for
adolescents who remain comatose after resuscitation following sudden witnessed out-of-hospital VF
cardiac arrest. Therapeutic hypothermia may also be beneficial for patients remaining comatose
after resuscitation from cardiac arrest.
A rapid response system in the inpatient setting may beneficial to reduce rates of cardiac and
respiratory arrest and in-hospital mortality.
Evaluation of sudden cardiac death victims: Past medical and family history, as well as
review of previous ECGs may point to the cause of sudden, unexplained cardiac death in a child or
young adult. When possible, tissue from the patient should be analyzed for the presence of
channelopathy.
(adapted from Gooden CK. SPA News, Society for Pediatric Anesthesia, 24(1),
Spring 2011 and Kleinman et al Circulation October 2010)
Perioperative cardiac arrest progressively has become less of a concern over the past two decades. Yet when it
occurs is a traumatic event for the anesthesiologist and perioperative care team. Knowledge of the epidemiology of
pediatric cardiac arrest and of current resuscitation techniques may further reduce the associated morbidity and
mortality. Recent studies of pediatric cardiac arrest (Flick et al 2007 ;Bhananker et al 2008 ) indicate that the
principal causes of perioperative arrest have remained fairly consistent throughout the years. In decreasing order
these are cardiovascular, respiratory, medication, equipment, combination of events and other miscellaneous causes.
Intraoperative arrests often are related to the cardiovascular system while respiratory events are more likely to cause
postoperative arrests. Higher ASA physical status and emergency procedures have the highest association with
perioperative cardiac arrest in children.
Copyright © 2011 American Society of Anesthesiologists. All rights reserved.
403
Page 3
[Type text]
[Type text]
Epidemiology
Common causes of arrest in infants and children differ between the out-of-hospital and in-hospital settings. These
causes are listed in the Table.
Table 1. Possible Causes of Cardiorespiratory Arrest in Infants and Children
Out-of-Hospital
In-Hospital
Perioperative
Trauma
Sudden infant death syndrome
(SIDS)
Submersion injury
Toxic ingestion
Choking/aspiration
Status asthmaticus
Viral bronchiolitis
Respiratory failure
Sepsis
Cardiovascular
Respiratory
Drug toxicity or overdose
Metabolic disturbances
Dysrhythmias
Medications
Equipment
Combination of events
Miscellaneous
Figure. Causes of Perioperative Cardiac Arrest by Phase of Care
Bhananker et al 2007
The American Heart Association (AHA) Committee on Pediatric Resuscitation completed an exhaustive process of
evidence review and expert consensus development to revise and update the guidelines for resuscitation of children.
This process culminated in the dissemination of the new AHA guidelines in November 2010 and significant
modification of the AHA Pediatric Advanced Life Support (PALS) course.
Cardiorespiratory arrest in infants and children is an infrequent phenomenon as compared to adults. In the majority
of cases the etiology is respiratory distress and failure which can lead to cardiac arrest if not treated and reversed in a
timely manner. Primary cardiac events leading to arrest are rare in infants and children, whereas in adults cardiac
arrest may be the primary event resulting from dysrhythmias, which can quickly deteriorate to a non-perfusing state.
Out-of-hospital arrests have a poor prognosis, with less than 9% survival to hospital discharge. For in-hospital
arrest, CPR is successful in restoring spontaneous circulation in over 60% of patients. However, the rate of survival
to discharge decreases rapidly to approximately 15% or less.
Copyright © 2011 American Society of Anesthesiologists. All rights reserved.
403
Page 4
[Type text]
[Type text]
Respiratory Failure
Successful cardiorespiratory resuscitation of infants and children begins with early recognition and reversal of
respiratory distress or shock.
Respiratory distress may be characterized by tachypnea, increased respiratory effort, nasal flaring, intercostal,
subcostal or substernal retractions, and stridor or grunting. Lethargy in a child with respiratory distress is a bad sign
indicating impending respiratory failure and requires immediate treatment. Other signs include inadequate or low
respiratory rate, decreased unilateral or bilateral breath sounds and pallor or cyanosis. Untreated, the patient will
suffer respiratory failure – defined as inadequate ventilation and possibly respiratory arrest.
Shock
Shock is defined as blood flow and oxygen delivery that is inadequate to meet metabolic demands. During the early
stage of compensated shock, tachycardia and peripheral vasoconstriction may sustain systemic blood pressure and
vital organ perfusion at marginally adequate levels. When the body’s ability to compensate is exceeded,
decompensated shock leads to rapid deterioration reflected as systemic hypotension and weak central pulses.
Because the normal values for vital signs vary with age, signs of compensated or decompensated shock may be easy
to miss. Bradycardic shock or arrest in infants and children is characterized by a heart rate significantly lower than
expected (usually under 100) in the presence of other signs of circulatory failure.
Airway
Airway problems are a leading cause of respiratory distress and failure in children. Young infants are obligate nose
breathers who may develop significant distress which may be relieved by suctioning of the nostrils. The infant
anatomy may contribute to airway obstruction because of the relatively large tongue, rostrally placed larynx (“more
anterior”) and large occiput. Proper positioning of the head and neck or placement of an oral airway may relieve an
apparent airway obstruction. Airway adjuncts including laryngeal mask airway and endotracheal intubation should
be used as appropriate.
Oxygen
Standard recommendations for resuscitation include the use of 100% oxygen. This recommendation is classified as
Indeterminate because of the possible adverse effects of 100% inspired oxygen. These effects include increased
cerebrovascular resistance, oxidative stress on lung, cardiac and other tissues, and atelectasis. Once the patient has
been resuscitated, the FiO2 should be decreased to a level sufficient to maintain adequate systemic oxygen levels.
Ventilation
Manual ventilation during resuscitation often results in significant overventilation. Overexpansion of infant lungs
may result in barotrauma and even pneumothorax, and impede proper venous return and affect cardiac output.
Hypocapnia may exacerbate brain hypoperfusion. Therefore, care should be used to provide ventilation that is
adequate to inflate the lungs while avoiding overdistention.
Cuffed Versus Uncuffed Tubes
Both cuffed and uncuffed tracheal tubes are acceptable for infants and children.If cuffed tracheal tubes are used,
avoid excessive cuff pressures. Appropriately sized endotracheal tubes should be used and care should be taken to
minimize glottic and subglottic trauma. Tube size can be approximated as (age in years/4) + 4 for uncuffed tubes
and (age in years/4) + 3 for cuffed tubes. Even in emergency situations, tube placement should be confirmed by
chest auscultation and by detection of exhaled CO2.
Vascular Access
PALS guidelines emphasize the need for timely vascular access. If peripheral access is not obtained within 90
seconds, intraosseous (I/O) needle placement is advised. All resuscitation carts and operating rooms should have
access to I/O needles. Experienced providers may be able to place a central line for more secure access, but the
Copyright © 2011 American Society of Anesthesiologists. All rights reserved.
403
Page 5
[Type text]
[Type text]
procedure may impede the ability to perform adequate chest compressions during cardiac arrest. In the absence of
IV or I/O access, most emergency medications may be administered via the endotracheal route but will require
higher doses than with the IV or I/O route.
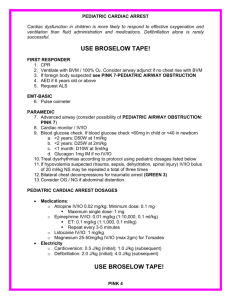
Cardiac Arrest
Pulseless arrest requires both ventilatory support and effective chest compressions. The likelihood of effective
resuscitation and return of spontaneous circulation improves with starting timely and adequate chest compressions.
The goal is to achieve longer periods of diastolic pressure sufficient to perfuse the coronaries. Therefore, the
pediatric recommendations are similar to those for adults. For single rescuer, 2 breaths are given after each 30
compressions. The two rescuer method involves a ratio of 15 compressions to 2 manual ventilations. Compressions
should be of sufficient depth (1/3 to 1/2 of the anterior-posterior chest diameter) and allow full recoil of the chest.
The compression rate for all ages is 100/minute.
Fluids and Medications
Dosing of fluids and medications in children is based on the child’s weight. Patients in hospital should have a
recently measured weight and pre-calculated doses of emergency medications available at the bedside. If the child’s
weight is unknown, length-based tape measures with pre-calculated doses have been validated and are commercially
available.
Isotonic crystalloid solutions should be used for resuscitation. Glucose containing solutions are not recommended
for routine use. Because infants are at high risk for developing hypoglycemia, blood glucose should be measured
early during the resuscitation.
Resuscitation medications for children are similar to those used in adults. Previous recommendations included the
use of “high dose” 0.1mg/Kg epinephrine in pulseless arrest. Studies in adults and case series reports in children
have shown that there is no benefit over the “standard dose” of 0.01 mg/Kg. The higher dose may in fact have
significant adverse effects including worse outcomes, , such as hypertension, ventricular ectopy, myocardial
necrosis and prolonged myocardial dysfunction.
Defibrillators in Pediatric Resuscitation
Because most pediatric arrests are a result of respiratory events, the most common dysrhythmias in children are
asystole and bradycardia with a wider QRS complex. Sudden cardiac arrest in children may result from ventricular
fibrillation (VF) or pulseless electrical activity (PEA). For children with VF, defibrillation may be a life-saving
intervention with the chance of survival approaching 20%. Out-of-hospital pediatric arrests are associated with 515% incidence of VF. For these children, especially those with witnessed sudden cardiac arrest, defibrillation has
resulted in rapid resuscitation and functional survival. Because of the significant benefit of automated external
defibrillators (AED’s), many communities have instituted Public Access Defibrillator (PAD) programs.
Supraventricular tachycardia (SVT) and ventricular tachycardia (VT) in children may be associated with a pulseless
state or pulses may be present. For the pulseless patient, treatment should be instituted according to the cardiac
arrest guidelines. If pulses are present, treatment should include oxygen and airway support and assessment of the
underlying cardiac rhythm. Narrow QRS complexes likely represent supraventricular tachycardia which may be
treated progressively with vagal stimulation, intravenous adenosine, and electrocardioversion. Amiodarone or
procainamide may be needed if the SVT is unresponsive to other treatments or the rhythm relapses. These
medications prolong the QT interval and therefore should be used with caution. Wide complex tachycardia may
represent SVT with aberrant conduction or VT. This rhythm may respond to electrocardioversion but often requires
amiodarone or procainamide as well.
Copyright © 2011 American Society of Anesthesiologists. All rights reserved.
403
Page 6
[Type text]
[Type text]
Torsade de Pointes
This is a polymorphic form of VT in children which may be congenital in origin or occur because of toxicity of
certain antiarrhythmics, antidepressants, or drug interactions. Intravenous magnesium sulfate is the treatment of
choice for torsade of any etiology. The initial dose of magnesium is 25 - 50 mg/Kg IV.
Miscellaneous
Cardiorespiratory arrest in children may occur as a result of toxic ingestion. A focused history and rapid diagnostic
tests may indicate the specific causative toxin or medication. Treatment of the systemic effects depends on the
ingested drug or toxin. Tricyclic antidepressants, β-blockers, calcium channel blockers, methamphetamine and
cocaine pose additional challenges.
Post-Resuscitation Neuroprotection
Preservation of brain function and prevention of secondary brain injury is an important goal of resuscitation.
Hyperventilation and hypocapnea should be avoided as there is no demonstrated benefit. Severe hypocapnea may
cause cerebral ischemia and myocardial dysfunction. Maintaining a normal body temperature is a foundational
practice in pediatric anesthesia. However, hyperthermia can have deleterious effects on brain recovery. Rapid
rewarming of a child during and after resuscitation is not necessary as it may result in hyperthermia. In patients who
remain comatose, therapeutic hypothermia (32oC-34oC) may improve brain recovery.
Family Presence During Resuscitation
Patient families may have a strong desire to be present during resuscitation. Family presence during procedures and
resuscitation has been endorsed by the Emergency Nurses Association and the national program for Emergency
Medical Services for Children. Although not practical in the operating room, it may be possible to have family
members present in the emergency department or hospital bedside during the resuscitation. For children with
chronic conditions, family members may be able to provide useful information about the child’s history and clinical
conditions. The healthcare team is encouraged to consider allowing families to be present during resuscitation and
to have a team member assigned to support the family.
Cardiac Arrest in the Perioperative Setting
Several special circumstances related to anesthetic management and surgery warrant mention. These will be
discussed in more detail during the Refresher Course. Anesthetic agent related effects include overdose of
Intravenous or Inhalation anesthetic. A high Neuraxial block may result in near-total sympathectomy. Unsuspected
Malignant hyperthermia or drug administration errors may result in circulatory compromise. Hypoxemia, Auto
PEEP, or Acute Bronchospasm may go undetected or untreated. Cardiovascular effects of interventions under
anesthesia may result cardiac arrest or circulatory compromise. Infants and young children with high
parasympathetic tone may experience severe bradycardia induced by Vasovagal reflex. Other conditions that can
result in arrest include Hypovolemic and/or hemorrhagic shock, Tension Pneumothorax, Anaphylactic Reaction,
Transfusion Reaction, Acute Electrolyte Imbalance (high K) – particularly after succinylcholine administration,
Severe Pulmonary Hypertension, Increased intraabdominal pressure (e.g., laparoscopy) and known or unrecognized
Prolonged Q-T syndrome, Pulmonary Embolism, Gas embolism.
Anaphylaxis
Common causes include IV contrast agents, latex, Beta lactam antibiotics, Non-depolarizing neuromuscular
blockers. The management of the patient with anaphylaxis consists of measures to interrupt the reaction and support
the patient. Surgery should be interrupted when feasible and the patient should be immediately supported with IV
fluid and vasopressors. It is imperative to remember that the Epinephrine administered to patients with anaphylaxis
is intended to interrupt the reaction, and not support the circulation. Thus it should always be given and at the full
recommended dose (0.01 mg/kg or approx 1mg in most adults).
Copyright © 2011 American Society of Anesthesiologists. All rights reserved.
403
Page 7
[Type text]
[Type text]
Complications of Central Venous Access
Pneumothorax is a well described and relatively rare complication of central line placement in perioperative
patients. Most practitioners astutely suspect this complication in patients who become unstable after undergoing
central venous cannulation. More recent analysis from the closed-claims database suggests that both hemopneumothorax and tamponade may be important and sometimes unrecognized fatal complications of patients who
undergo attempts at central venous cannulation. In those instances where a patient deteriorates following central line
placement, echocardiography should be considered in addition to chest radiography.
Local Anesthetics
Risk of local anesthetic toxicity is difficult to predict. In general, local anesthetics depress the heart in a dose
dependent fashion. Amongst the local anesthetics in widespread clinical use, bupivacaine is the most potent
myocardial depressant and most often associated with cardiac arrest. Most children receive local anesthetic blocks
while they are under general anesthesia. Therefore, clinical symptoms that may presage cardiac arrest in this setting
are usually masked. Signs of local anesthetic toxicity include PVCs, wide QRS complex EKG which can
subsequently deteriorate into EMD/PEA or asystole (bupivicaine), bradycardia or atrioventricular block (lidocaine
and etidocaine). Treatment includes stopping the administration of local anesthetic, CPR as indicated (pulseless for
>10 sec), Epinephrine 10 mcg/Kg, tracheal intubation and ventilation with 100% oxygen. Intralipid (20%)
1.5ml/Kg IV load, then 0.25ml/Kg/hr IV may be lifesaving. Sodium Bicarbonate should be used to maintain a pH
>7.25. Other treatment may include H1 and H2 blockers, transcutaneous or intravenous pacemakers for all
bradycardic rhythms. Continue CPR for at least 60 minutes, as very good neurologic recovery has been reported in
patients after very prolonged cardiac arrests from local anesthetic overdoses.
Summary
The guidelines for pediatric advanced life support emphasize early recognition and treatment respiratory failure and
shock. In cases where IV placement is difficult rapid placement of an intraosseous needle is recommended for
venous access. Vagal maneuvers are a first line intervention for SVT with progressive advancement to adenosine
and cardioversion, if the patient fails to improve. Amiodarone now is recommended for most dysrhythmias,
especially VT. Epinephrine remains a crucial medication in resuscitation. The standard dose of 0.01 mg/Kg is
recommended; while the high-dose (0.1 mg/Kg) may actually cause harm. AED’s are recommended to treat
children >1 year of age; their effectiveness in infants <1 year of age is unclear. Chest compressions during CPR
should be “hard and fast” maintaining a ratio of 15 compressions to 2 manual ventilations. Therapeutic hypothermia
may be neuroprotective. Family presence during resuscitation should be considered.
Copyright © 2011 American Society of Anesthesiologists. All rights reserved.
403
Page 8
[Type text]
[Type text]
Table 2. Summary of Selected Doses in Pediatric Resuscitation
Dosage Comment Adenosine 0.1 – 0.2 mg/Kg SVT Amiodarone 5 mg/Kg VT or SVT (up to 3 doses) Epinephrine 0.01 mg/Kg Pulseless or Bradycardic Arrest Magnesium 25 – 50 mg/Kg Torsade de Pointes Cardioversion 0.5 – 1 joule/Kg SVT Defibrillation 2 joules/Kg Ventricular fibrillation (max 4 joules/Kg) AED (Automatic External Defibrillation) Adult dose > 8 yoa Sudden Collapse Pediatric attenuator < 8 yoa Pulseness VT/VF See Circulation October 2010 for detailed guidelines and precautions.
Recommended Reading:
Aufderheide T, Lurie KG: Death by hyperventilation: a common and life-threatening problem during
cardiopulmonary resuscitation. Crit Care Med 2004; 32[Suppl]:S345-351.
Berg RA, Otto CW, Kern KB et al: A randomized, blinded trial of high-dose epinephrine versus standard-dose
epinephrine in a swine model of pediatric asphyxial cardiac arrest. Crit Care Med 1996, 24:1695-1700.
Bhananker SM, Ramamoorthy C, Geiduschek JM, Posner et al: Anesthesia-related cardiac arrest in children: update
from the pediatric perioperative cardiac arrest registry. Anesth Analg 2007;105:344 –50.
Boudreaux ED, Francis JL, Loyacano T: Family presence during invasive procedures and resuscitations in the
emergency department: a critical review and suggestions for future research. Ann Em Med 2002; 40:193-205.
Davis PG, Tan A, O’Donnell CPF et al: Resuscitation of newborn infants with 100% oxygen or air: a systematic
review and meta-analysis. Lancet 2004; 364:1329-1333.
Flick RP, Sprung J, Harrison TE, et al: Perioperative cardiac arrests in children between 1988 and 2005 at a tertiary
referral center. Anesthesiology 2007; 106:226–37.
Gabrielli A, O’Connor MF, Macchioli GA. Anesthesia Advanced Circulatory Life Support. American Society of
Anesthesiology Committee on Critical Care Medicine and American Society of Critical Care Anesthesiology.
February 2008. Downloaded May 2010 from <http://asahq.org/clinical/Anesthesiology-CentricACLS.pdf>.
Copyright © 2011 American Society of Anesthesiologists. All rights reserved.
403
Page 9
[Type text]
[Type text]
Gooden CK. 2010 Update: American Heart Association guidelines for pediatric resuscitation. SPA News, Society
for Pediatric Anesthesia, 24(1), Spring 2011.
Hazinski MF, Nolan JP, Billi JE, Böttiger BW, Bossaert L, de Caen AR, Deakin CD, Drajer S, Eigel B, Hickey RW,
Jacobs I, Kleinman ME, Kloeck W, Koster RW, Lim SH, Mancini ME, Montgomery WH, Morley PT, Morrison LJ,
Nadkarni VM, O'Connor RE, Okada K, Perlman JM, Sayre MR, Shuster M, Soar J, Sunde K, Travers AH, Wyllie J,
Zideman D. Part 1: Executive summary: 2010 International Consensus on Cardiopulmonary Resuscitation and
Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation. 2010;122(16 Suppl
2):S250-75.
Kleinman ME, de Caen AR, Chameides L, Atkins DL, Berg RA, Berg MD, Bhanji F, Biarent D, Bingham R,
Coovadia AH, Hazinski MF, Hickey RW, Nadkarni VM, Reis AG, Rodriguez-Nunez A, Tibballs J, Zaritsky AL,
Zideman D; Pediatric Basic and Advanced Life Support Chapter Collaborators. Part 10: Pediatric basic and
advanced life support: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency
Cardiovascular Care Science With Treatment Recommendations. Circulation. 2010;122(16 Suppl 2):S466-515.
Perondi M, Reis A, Paiva E, et al: A comparison of high-dose and standard-dose epinephrine in children with
cardiac arrest. N Engl J Med 2004; 350:1722-1730.
Ramamoorthy C, Haberkern CM, Bhananker SM, Domino KB, Posner KL, Campos JS, Morray JP. AnesthesiaRelated Cardiac Arrest in Children with Heart Disease: Data from the Pediatric Perioperative Cardiac Arrest
(POCA) Registry. Anesth Analg 2010; 110:1376-1382.
Reis AG, Nadkarni V, Perondi MB, et al: A prospective investigation into the epidemiology of in-hospital pediatric
cardiopulmonary resuscitation using the internation Utstein reporting style. Pediatrics 2002, 109:200-209.
Spittler KL: Family presence during CPR and invasive procedures. Pulmonary Reviews.Com 2006; 11(3). accessed
07/06/08 at [http://www.pulmonaryreviews.com/mar06/family.html].
Young KD, Gausche-Hill M, MCClung CD et al: A prospective population-based study of the epidemiology and
outcome of out-of-hospital pediatric cardiopulmonary arrest. Pediatrics 2004;114:157-164.
Copyright © 2011 American Society of Anesthesiologists. All rights reserved.
Disclosure
This speaker has indicated that he or she has no significant financial relationship with the
manufacturer of a commercial product or provider of a commercial service that may be
discussed in this presentation.