Instructional Guide to Psychiatric Evaluation
advertisement

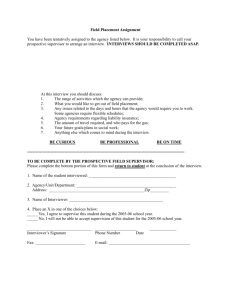
Louisiana Behavioral Health Partnership Instructional Guide to the 1915(i) Behavioral Health Interview The 1915(i) State Plan Amendment establishes home and community-based services for adults concurrent with the Behavioral Health 1915(b) waiver. In order to receive 1915(i) services, each participant must receive a needs-based assessment, performed by qualified staff. The Department of Health and Hospitals, through the SMO makes the final 1915(i) enrollment eligibility decisions. Persons eligible to receive 1915(i) services must be over the age of 18, and meet specific criteria in order to qualify. Because the evaluation and reevaluation must be performed by qualified personnel using the targeting and needs-based assessment criteria outlined in the 1915(i) State Plan Amendment and LOCUS assessment tool, individuals performing evaluations must be trained to administer the targeting and needs-based criteria evaluation, be a certified LOCUS screener, and must be an approved Licensed Mental Health Practitioner, as established in state plan and detailed in the Service Definition Manual. Persons who qualify to receive 1915(i) services must, therefore, meet the established and approved NeedsBased/Level of Care criteria. Therefore, each person must receive an objective face-to-face assessment with a person-centered process by an agent who is independent and qualified. Interviews and assessments must be performed in consultation with the individual and, if applicable, the individual’s authorized representative, and must include the opportunity for the individual to identify other persons to be consulted, such as, but not limited to , the individual’s spouse, family, guardian, and other treating and consulting health and support professionals caring for the individual. The assessment must be based on an examination of the individual’s relevant history, including findings from the independent evaluation eligibility, medical records, and objective evaluation of functional ability, and any other records or information needed to develop the plan of care. In addition, an examination of the individual’s physical, addiction, and mental health care and supports needs, housing needs, strength’s and preferences, must be included. Caregiver assessments should also be included, when unpaid caregivers will be relied upon to implement the plan of care. The independent assessment will serve as the basis for the individualized Plan of Care. Instructions For Completion of 1915(i) Behavioral Health Interview: Note: All sections must be completed. General: The 1915(i) Behavioral Health Interview Form is intended to be used in three ways: 1. As a hand-written worksheet and filed on the chart. In this case, use the spaces provided to address all items. If more space is required, write on the back of form sheets, making sure to time and date such entries appropriately. 2. As a work sheet or template for dictation. In this case, the original need not be filed on the chart, as long as the transcribed document appears on the patient’s chart within 24 hours of admission. For those who dictate, a brief note in the Multidisciplinary Progress Notes should address pertinent issues and inform the reader/reviewer that the Psychiatric Evaluation has been performed and dictated. 1 Revised 12/10/2012 3. As a worksheet used as an aid to make later entry into Magellan’s Electronic Health Record/Clinical Advisor. The Behavioral Health Interview in Clinical Advisor must be completed on the same date of service as performed. Specific Instructions: What follows are guidelines on how to complete specific items or blanks on the 1915(i) Behavioral Health Interview. 1915(i) State Plan/CMS requirements and Commission on Accreditation of Rehabilitation Facilities (CARF) guidelines were referenced when available, and some other resource texts are included where noted. Also referenced are established OBH and Clinical Advisor data standards where appropriate. Recipient Name (first, middle, last): On the paper version of this document, enter the recipient’s given formal first name, any middle names, and surname/family name in the space provided. (Note: once the form is part of Clinic Advisor, this section may be auto-populated from Client Demographic. –> PLAN TO AUTOPOPULATE FROM CA CLIENT MASTER. -> PLAN TO AUTOPOPULATE ITEMS FROM THIS SECTION INTO TREATMENT PLAN.) Note: nicknames should not be substituted for the actual formal given name of the individual. Interview Date: This is intended to include the actual date that the patient was interviewed for purposes of gathering information for this evaluation. In many cases this date will be the same as the date of admission, but in other cases, these dates may not be the same. If this interview is dictated, the date of dictation does not go here –only the date of the actual interview. The date of dictation should be tracked elsewhere. Age: The age in years of the client upon interview. –> PLAN TO AUTOPOPULATE FROM CA CLIENT MASTER. Date of Birth: Enter in mm/dd/yyyy format (e.g. 04/15/1973). –> PLAN TO AUTOPOPULATE FROM CA CLIENT MASTER. Race: Select the appropriate response from the list below. For individuals with parents of different races or for the individual unsure of their race, the race of the client’s mother should be used. –> PLAN TO AUTOPOPULATE FROM CA CLIENT MASTER. (Note: PLAN TO AUTOPOPULATE ITEMS FROM THIS SECTION INTO TREATMENT PLAN.) Sample Definitions for Race: White - An individual having origins in any of the original peoples of Europe (including Portugal), North Africa, or the Middle East. (Not of Hispanic Origin) Black/African American - An individual having origins in any of the original black racial groups of Africa. (Not of Hispanic Origin) American Indian - An individual having origins in any of the original peoples of North America and who maintains cultural identity through tribal affiliation or community recognition. Alaskan (Aleut, Eskimo, Indian) - An individual having origins in any of the original 2 Revised 12/10/2012 peoples of Alaska and who maintains cultural identity through tribal affiliation or community recognition. Native Hawaiian/Asian or Pacific Islander - An individual having origins in any of the original peoples of the Far East, Southeast Asia, the Indian subcontinent, or the Pacific Islands (e.g., Japan, China, Samoa, India, Korea, the Philippine Islands, Vietnam, Thailand, etc.). Unknown Other Hispanic - A default category for use in instances in which the client is not classified above or whose origin group, because of area custom, is regarded as a racial class distinct from the above categories. Ethnicity: –> PLAN TO AUTOPOPULATE FROM CA CLIENT MASTER. (Note: PLAN TO AUTOPOPULATE ITEMS FROM THIS SECTION INTO TREATMENT PLAN.) • • • • • • Non-Hispanic or Non-Latino, Hispanic or Latino -unknown origin Hispanic-Central or South American Hispanic-Mexican/Mexican American Hispanic-Puerto Rican Hispanic-Cuban Gender: Specify Male or Female ("M" or "F") –> PLAN TO AUTOPOPULATE FROM CA CLIENT MASTER. (Note: PLAN TO AUTOPOPULATE ITEMS FROM THIS SECTION INTO TREATMENT PLAN.) Marital Status: Select the definition that best indicates the current marital status of the client. –> PLAN TO AUTOPOPULATE FROM CA CLIENT MASTER. (Note: PLAN TO AUTOPOPULATE ITEMS FROM THIS SECTION INTO TREATMENT PLAN.) • • • • • • • Data Definitions for Marital Status: Unknown Never married - The client has never married (either legal or "common law") or the client's only marriage(s) ended in annulment. Married - The client has been married only once and is still married to the same spouse (includes "common law" marriages and those living together as a married couple). Remarried - The client has been married more than once and is now currently married (includes "common law" marriages and those living together as a married couple). Separated - The client is married, but is currently living apart from (or has been deserted by) his/her spouse because of marital discord (includes informal as well as legal separations). Divorced - The client is currently legally divorced. Widowed - The client's spouse is deceased and the client has not remarried. SSN (Social Security Number): Enter full nine (9) digit number, including hyphens (e.g. 000-00-000). 3 Revised 12/10/2012 Behavioral Health History I. Reason for Presentation/History of Present Illness (Note: PLAN TO AUTOPOPULATE ITEMS FROM THIS SECTION INTO TREATMENT PLAN.) A. Reason for Seeking Services Expressed in person’s own words): This section is intended for a narrative account of why the client is seeking specialized behavioral health services, and should include a quote from the client. Examples of why a given individual may be seeing services may vary considerably. Some may be seeking services as a condition of probation, at the order of a judge, etc. Others may be seeking services at the request of a family member or healthcare provider. Of course, some will be seeking services on their own accord due to one or more precipitating factors in their lives. (e.g. worsening feelings of depression, insomnia, suicidal thinking, difficulty functioning at work or in relationship, etc.) Whenever possible, this should be expressed in the client’s own words. B. Onset/Course of Issues (Include any known precipitation factors.) This section is meant to naturally follow the first section. As the client has expressed the reason he/she is seeking services, it should be natural to inquire about how and when this current episode began, and what precipitating factors may have been involved that led to the client finally deciding to seek services. C. Symptoms: At this point, even early in the interview process, some symptoms may well have already been expressed. (e.g. suicidal ideation, started hearing voices, worsening insomnia, etc.) In this section, the interviewer may inquire about additional symptoms and/or details which might be relevant to the presentation or reason he/she is seeking services. Such symptoms may well help establish a diagnosis and/or serve as foci for later recommendations in the Plan of Care or Treatment Plan. D. Functional Impact of Symptoms: While many individuals can readily express specific symptoms such as insomnia, forgetfulness, depression, fatigue, hallucinations, etc. it is also important to understand and document what, if any, functional impairment may be resulting from such symptoms. In this section, the interviewer may document such resulting symptoms or behaviors as inability to perform basic activities of daily living, or missing days of work or school. Attempts should be made to understand and document any impairment of functioning in such areas as employment, social and/or family relationships and community integration, and/or basic activities of daily living. E. Services Sought/Requested: Each individual presenting for treatment may have specific ideas or preferences regarding which services he or she is seeking. Part of assuring that services provided are individualized and consistent with a patient-centered approach is to elicit such preferences at the beginning of treatment. Some may be seeking psychotherapy, others psychopharmacologic management or other specified services. While some services may well be indicated, covered and available, others may be less so, and might require that referrals or linkages to other services providers or supports be facilitated. F. Recipient Expectations (Expressed in recipient’s own words.): Expressed in the recipients own words, space is provided for the recipient to list his or her own expectations regarding outcome of treatment. While a range of realistic and perhaps some unrealistic, expectations may be encountered, these should be documented and addressed in the course of treatment planning and provision. G. Additional Information (including information obtained from collateral sources, family, etc.): Additional space is provided in the event the above sections do not adequately capture relevant information. 4 Revised 12/10/2012 II. Urgent Needs: Assess potential risk of harm to self/others; include patterns of risk behavior and risk due to personality, substance use, criminality, exposure to elements, exploitation, abuse, neglect, suicidal or homicidal history, self-injury, psychosis, impulsiveness, etc. NOTE: Each urgent/critical need MUST be addressed directly or through referral. (Note: PLAN TO AUTOPOPULATE ALL ITEMS FROM BH INTERVIEW INTO TREATMENT PLAN.) A. RISK OF HARM TO SELF: Select any/all that apply from listed check box options provided. List any additional risks and/or provide relevant details in the “Other/Describe” space provided. B. RISK OF HARM TO OTHERS: Select any/all that apply from listed check box options provided. List any additional risks and/or provide relevant details in the “Other/Describe” space provided. C. RECIPIENT SAFETY AND OTHER IRSK FACTORS: Select any/all that apply from listed check box options provided. List any additional risks and/or provide relevant details in the “Other/Describe” space provided. D. PROBLEMS WITH BASIC NEEDS: Select any/all that apply from listed check box options provided. List any additional risks and/or provide relevant details in the “Other/Describe” space provided. E. ADVANCED DIRECTIVES: As promted on the form, describe recipient’s preferences and desires for addressing risk factors, including any Mental Health Advance Directives or plan of response to periods of decomposition/relapse (Ex. Resources recipient feels comfortable reaching out to for assistance in a crisis.). When given the option to describe, if the recipient is not able to describe or report any such preferences and/or desired, and is otherwise not comfortable reaching out to anyone else for assistance in a crisis, check “None Reported,” and describe. III. Substance Abuse/Dependence Issues (Including past use of primary, secondary, & tertiary current substance including type, frequency, method and age of first use.) (Note: PLAN TO AUTOPOPULATE ITEMS FROM THIS SECTION INTO TREATMENT PLAN.) A. Check any/all that apply in Past 12 Months: This section is intended to capture relatively recent historical use/abuse of substances, even if the recipient is not currently using or has not used any within the past 30 days or so. Select any/all that apply from listed check box options provided. List any additional substances or addiction/dependence-related behaviors and/or provide additional relevant details in the “Other/Describe” space provided. If there is no history of any such substance abuse/dependence behaviors in the past 12 months, check “None.” B. Substance Type/Dependence in Last 30 Days: This section is intended to capture most recent and current substance usage and/or dependence issues. In the table provided list ALL substances used in the 30 days prior to the interview, even if none have been used in the past week or so. In the appropriate column, list the Substance Type (See “Examples of Substance Types” below for examples.), Age of First Use (e.g. 12 y.o.), the number of Days In the Past 30 that the person used (e.g. 12 days of use in the past 30 = 12 days), Days Since Last Use, the Amount of Use (e.g. # drinks, # packs per day, # hits, etc.), and the Frequency of Use (e.g., 1-3 times, 1-2 times per week, 3-6 times per week, daily, frequency unknown, no use during past 30 days, etc.). In the column provided, check the appropriate Route of Administration (e.g. oral, nasal, smoking, Non-IV Injection, IV injection). If actual route of administration is not included as a listed option, provide detail 5 Revised 12/10/2012 under item “C,” Additional Substance Abuse/Dependence Comments. (Note: PLAN TO AUTOPOPULATE ITEMS FROM THIS SECTION INTO TREATMENT PLAN.) Examples of Substance Types/Dependencies (to be included in Clinical Advisor Drop Down list): alcohol, amphetamine, barbiturates, bath salts, benzodiazepine, cocaine/crack, ecstasy, gambling, hallucinogens, heroin, inhalants, marijuana/cannabis, Methadone, methamphetamine, other opiates and synthetics, other sedative and hypnotics, other stimulants, over-the-counter, Oxycontin, PCP, Soma, synthetic marijuana, tobacco/smokeless tobacco, tranquillizers, other, unknown. (Note: List needs to match CA Client demographic.) C. Additional Substance Abuse/Dependence Comments: Include any additional substance use history not adequately covered above and any known history of functional impairment associated with substance abuse/dependence. (Note: PLAN TO AUTOPOPULATE ITEMS FROM THIS SECTION INTO TREATMENT PLAN.) IV. PREVIOUS BEHAVIORAL HEALTH HISTORY AND SERVICES • MH OR AD: This is to allow interviewer to indicate whether the previous treatment was “Mental Health” (i.e. write in or choose “MH.”) or Addictions-related (i.e. Write in or choose “AD.”). • SETTING: Intended for a drop down/combo box multiple choice, options for this section include: None; Outpatient, IOP, Residential/Inpatient; Detox, and other. Describe/detail space provided under “Additional History/Comments. • • • • • FACILITY/PROVIDER NAME: This space is intended to allow interviewer to actually list the facility’s business name or the practitioner’s name (e.g., Central Louisiana State Hospital, Rosenblum Mental Health Clinic, Dr. Marcus Welby, M.D., etc.) DATES OF TREATMENT/SERVICE: List the approximate begin and end dates in the space provided. (e.g., June 2009 – January 2010.) DIAGNOSIS/REASON FOR TREATMENT: List the diagnosis, if known. Otherwise list the main reason for treatment, if known (e.g., depression, marital problems, suicidal, manic, hearing voices, etc.). Provide any supporting detail or clarification in the space provided under “Additional History/Comments.” OUTCOME OF TREATMENT: Provide a brief summarizing comment in the space provided (e.g., Completed. No further treatment required; Client referred to next level of care; Further treatment needed –new provider requested; Treatment rejected by client; Other Discharge. Provide any supporting detail or clarification in the space provided under “Additional History/Comments.” ADDITIONAL HISTORY/COMMENTS: Provide any additional relevant history or supporting detail or clarification in the space provided. PHYSICAL V. MEDICAL HISTORY: Check all that apply. Include important non-psychiatric medical history and treatment, surgeries, injuries, seizures, head trauma, recent labs, prescription medication, and treatment responses under this topic. Of special interest are those illnesses or symptoms that may affect mental status or response to treatment. If there is no prompt or check box for the reported condition, check “Other/Describe,” and provide needed detail. (Note: PLAN TO AUTOPOPULATE ITEMS FROM THIS SECTION INTO TREATMENT PLAN.) 6 Revised 12/10/2012 VI. • CURRENT AND PAST MEDICATIONS Medication Name: List current and/or past medication name (psychiatric and/or nonpsychiatric, generic or brand name) in this column (e.g., Metformin, Prozac, Seroquel, Lipitor, diphenhydramine, etc.) (Note: PLAN TO AUTOPOPULATE ITEMS FROM THIS SECTION INTO TREATMENT PLAN.) • • • • • VII. Dose: List dose (500 mg, 20 mg, 300 mg, 40 mg, 25 mg, etc.) Freq. List frequency that medication is/was taken (daily, 2 x daily, 3 x daily, weekly, monthly, etc.) Route: List how medication was taken (e.g. sub-lingual, oral, inhaled, injection, patch, etc.) Current: Indicate whether medication is currently being taken (i.e. YES) or not (i.e. NO). Provide any clarification is space provided under “Comments.” Comments: this space is intended for any detail regarding medications. If more space is needed, interviewer may use section IX. ADDITIONAL MEDICAL HEALTH HISTORY, ISSUES OR NEEDS. ALLERGIES/ADVERSE REACTIONS TO MEDICATION: Include any medications, foods or contact agents. Also include any adverse reactions to medications, even if not truly allergic in nature (e.g., nausea, excessive sedation, tremor, etc.) If none are indicated, check “No reported Allergies/Reactions.” Detail may be provided in the “other/Describe Reaction” space provided. (Note: PLAN TO AUTOPOPULATE ITEMS FROM THIS SECTION INTO TREATMENT PLAN.) VIII. PRIMARY CARE PHYSICIAN: If known, list the full name and contact phone number of the primary care physician(s). If there is no known primary care physician, check: “None Reported.” If “None Reported” is checked, the interviewer should provide a resource to the client, and then check the “Resources Given” box. If no such resources were provided, this box should not be checked. (Note: PLAN TO AUTOPOPULATE ITEMS FROM THIS SECTION INTO IX. ADDITIONAL MEDICAL HEALTH HISTORY, ISSUES OR NEEDS: This narrative space is provided for any additional important information related to the Medical History, including any special needs that client may have. Relevant information about past or current medical conditions may be listed here, as should be any additional information related to current or past medications, allergies, etc. (Note: PLAN TO AUTOPOPULATE ITEMS FROM THIS TREATMENT PLAN.) SECTION INTO TREATMENT PLAN.) CURRENT AND HISTORICAL LIFE SITUATION X. XI. XII. GENDER EXPRESSION: Selections from Clinical Advisor for this item include: 01 gender variant, 02 intersex, 03 man, 04 questioning, 05 transgender, 06 woman, 97 decline to answer, 98 NA due to age (<18 only) –> PLAN TO AUTOPOPULATE FROM CA CLIENT MASTER. SEXUAL ORIENTATION: Selections from Clinical Advisor for this item include: (01 asexual, 02 bisexual, 03 gay, 04 heterosexual, 05 lesbian, 06 questioning, 91 decline to answer, 98 NA due to age (<18 only) –> PLAN TO AUTOPOPULATE FROM CA CLIENT MASTER. CULTURAL AND LANGUAGE PREFERENCES: List any spiritual or culture-specific issues, needs or preferences in the space provided. (e.g. church as important support, religious cause of illnesses, bias for natural treatments, , shame or guilt related to mental health diagnosis, specific and relevant attitudes regarding lesbian, gay, bisexual or transgender issues, etc.) (Note: PLAN TO AUTOPOPULATE ITEMS FROM THIS SECTION INTO TREATMENT PLAN.) 7 Revised 12/10/2012 XIII. EDUCATION HISTORY A. Highest Grade or Completed Degrees: List numerical grade equivalent for the highest grade completed (e.g., 10th Grade, 12th Grade, etc.) or the specific degree obtained (e.g., BA, BS, MA, MS, PhD, etc.) Provide relevant detail under “Additional Comments (e.g., Grade Point Average, specific area of study or degree, etc.). Check “Yes” if High School Diploma was received or “GED Received,” if a high school equivalency diploma was received. If the client received special education classes or similar accommodations, please indicate so in the space provide and/or under Additional Comments. B. Estimated Literacy Level: This may be expressed as a grade level (e.g. 3rd grade or below, 4th to 6th grade, 7th to 8th grade, high school, above high school reading level, etc.) Further support or detail may be provided under “Additional Comments.” C. Difficulties with Reading/Writing: Check “Yes” or “No” on this item, based on discussion with client and/or other collaterals. Interviewer should also inquire whether client attended any special classes or needs any special accommodations to assist with literacy. (Note: PLAN TO AUTOPOPULATE ITEMS FROM THIS SECTION INTO TREATMENT PLAN.) D. XIV. Additional Comments: Include any relevant detail related to Educational History. The interviewer may support the estimated literacy level and/or provide explanation of any expressed difficulties with reading or writing. If any other specific accommodations (e.g., translation services, assistive devices, etc.) are requested or required, include them in the space provided. EMPLOYMENT HISTORY AND SOURCE OF INCOME A. CURRENT SOURCE OF INCOME AND ESTIMATED MONTHLY Demographic prompts include: disability, none, other, retirement/pension, SSI, FITAP, other public assistance, wages/salary. Interviewer may provide any additional relevant history under item “E.” below (i.e. Additional Employment/Income Comments) For “Estimated Monthly Income Amount, list gross monthly household income in dollars. Provide any relevant detail or clarification in the Additional Employment/Income Comments section. –> PLAN TO AUTOPOPULATE FROM CA CLIENT MASTER. B. CURRENT EMPLOYMENT STATUS: Recommended choices from Clinical Advisor Client Demographic: disabled, employed full time, employed part time, homemaker, in armed forces, in hospital, inmate or institution, jail/prison/training institution, occasional/seasonal worker, other, retired, shelter/non-competitive employment, student/preschool child, transitional employment placement, unemployed, unemployed (layoff), unemployed (looking), unemployed (not looking), unknown, unpaid rehabilitation activities, volunteer, work adjustment training) Provide any relevant detail or clarification in the Additional Employment/Income Comments section. –> PLAN TO AUTOPOPULATE FROM CA CLIENT C. PRIOR EMPLOYMENT HISTORY: Recommended Choices: None, Frequent Job Turnover, Episodes of steady employment, steady employment. Provide any relevant detail or clarification in the Additional Employment/Income Comments section. MILITARY STATUS: Recommended choices: None; Veteran; Active Duty, No Combat; Active Duty Combat. Also list whether or not client experienced any MASTER. D. 8 Revised 12/10/2012 XV. XVI. XVII. XVIII. military trauma in space provided. Provide any relevant detail or clarification in the Additional Employment/Income Comments section. E. ADDITIONAL EMPLOYMENT/INCOME COMMENTS: This space is intended for any relevant detail or explanation for items A through D above. LEGAL STATUS AND HISTORY A. Current Legal Status: This area was broken out for clarity and emphasis. As court dates and pending charges require special attention in many psychiatric clients, this separate legal status section was included. Provide relevant detail in narrative space provided. B. Past Legal History: List any know history of Driving While Intoxicated (DWI) violations or charges, prior arrests and incarcerations. Provide relevant detail in narrative space provided. FAMILY HISTORY A. ADVERSE CIRCUMSTANCES IN FAMILY OF ORIGIN: Choices provided for this section include the following: N/A (Not Applicable); Poverty; Criminal Behavioral; Mental Illness; Substance Use; Abuse; Neglect; Domestic Violence; Violence; and Trauma. Further describe and checked items with relevant detail in the “Other/Describe all checked items” section. B. ADDITIONAL FAMILY HISTORY: Interviewer may include any additional relevant family history, including any behavioral health diagnoses, treatments, and/or response to treatments in this section. (e.g. Biologic mother with depression responded well to Prozac.) TRAUMA HISTORY: recommended choices for this section include: None, Experienced, Witnessed, Abuse, Neglect, Violence, Sexual Assault, and Other/Describe. After checking appropriate box, provide any relevant detail after the “Other/Describe” section. LIVING SITUATION A. PRIMARY RESIDENCE AND FAMILY/HOUSEHOLD COMPOSITION: Recommended choices from client demographic include: primary residence, foster home or foster care, group home/halfway house, homeless/shelter, hospital, jail/prison, training inst., non permanent residence, nursing home or intermediate care facility, other quarters, private residence- dependent (adult), private residenceindependent (adult), private residence- w/family/ext. fly/ non-relatives (child), residential hotel, unknown) B. ADDITIONAL COMMENTS: This space is intended for any additional relevant detail related to the client’s living situation, including any psychological and/or social adjustments made to disabilities and/or disorders. (Note: PLAN TO AUTOPOPULATE ITEMS FROM THIS SECTION INTO TREATMENT PLAN.) XIX. SOCIAL/FAMILY RELATIONSHIPS AND COMMUNITY INTEGRATION A. CURRENT STATUS AND FUNCTIONING, RECREATIONAL AND SELFHELP ACTIVITIES: This section is intended for documentation regarding the client’s involvement in the community, including any known or described social supports, social activities, and/or any barriers to accessing social supports or activities. In the space provided, the interviewer should also document whether or not the client feels reasonably supported by friends or family. Such support might be of an emotional, financial or general assistance nature, and is subjective, but 9 Revised 12/10/2012 B. considered important in terms of identifying potential strengths and resources for the client. List any known or reported recreational activities in the space provided (e.g., Likes to walk, ride bicycles, watches TV, listens to music, drop-in-center, etc.) Recommended choices for Self-Help Activities from client demographic include: 1-3 times in the past month, 4-7 times in the past month, 8-15 times in the past month, 16-30 times in the past month, no attendance in the past month, some attendance but frequency unknown) Additional Comments: extra space is provided for relevant detail related to Social/family relationships and Community Integration. CURRENT STATUS XX. MENTAL STATUS The following guidelines are for reference only. Many explanations are derived from the "Concise Textbook of Clinical Psychiatry (from Kaplan and Sadocks’ Synopsis of Psychiatry, 7th edition). It should be noted that Joint Commission, CMS, and APA Practice Guidelines were also reviewed for this section. A. General Appearance: "This is a description of the patient’s appearance and overall physical impression conveyed to the interviewer as reflected by posture, poise, clothing, and grooming… Examples of items in the appearance category include body type, posture, poise, clothes, grooming, hair and nails. Common terms to describe appearance are healthy, sickly, ill at ease, poised, odd-looking, young-looking, disheveled, childlike, and bizarre…" (Kaplan and Sadocks’) B. Behavior & Psychomotor Activity: "This category refers to both the quantitative and the qualitative aspects of the patient’s motor behavior. Included are mannerisms, tics, gestures, twitches, stereotyped behavior, echopraxia, hyperactivity, agitation, combativeness, flexibility, rigidity, gait, and agility. Restlessness, wringing of hands, pacing, and other physical manifestations are described. Psychomotor retardation or generalized slowing of body movements should be noted. Any aimless, purposeless activity should be described." (Kaplan and Sadocks’) C. Attitude: "The patient’s attitude toward the examiner can be described as cooperative, friendly, attentive, interested, frank, seductive, defensive, contemptuous, perplexed, apathetic, hostile, playful, ingratiating, evasive, or guarded; any number of other adjectives can be used. The level of rapport established should be recorded." (Kaplan and Sadocks’) D. Speech: "This part of the report describes the physical characteristics of speech. Speech can be described in terms of its quantity, rate of production, and quality…Impairments of speech , such as stuttering, are included in this section. Unusual rhythms (termed dysprosody) and any accent that may be present should be noted. Is the patient’s speech spontaneous or not?" (Kaplan and Sadocks’) E. Mood: Mood is defined as a pervasive and sustained emotion that colors the person’s perception of the world…include depth, intensity, duration, and fluctuations…Mood may be labile…"(Kaplan and Sadocks’) 10 Revised 12/10/2012 Note: The term “alexthymic” may be used when person has difficulty identifying feelings to others and/or has a constricted imaginal process, with unempathathic and ineffective responses. The term “dysphoric” may be used when a person is experiencing intense feelings of depression, discontent, and indifference to the world around them. Use “euthmic” if person is apparently in a normal non-depressed and reasonably positive mood. F. Affect : Affect may be defined as the patient’s present emotional responsiveness. Affect is what the examiner infers from the patient’s facial expression, including the amount and the range of expressive behavior. Affect may or may not be congruent with mood." (Kaplan and Sadocks’) Some other commonly used adjectives for affect include: constricted, blunted, and flat. G. Perceptual Disturbances: "Perceptual disturbances, such as hallucinations and illusions may be experienced in reference to the self or the environment." (Kaplan and Sadocks’) Some examples may include auditory, visual, olfactory or tactile hallucinations. Hypnagogic hallucinations (occurring as one falls asleep) and hypnopompic hallucinations (hallucinations associated with the state of consciousness leading out of sleep) should be differentiated and described if present. Feelings of depersonalization and derealization are other examples of perceptual disturbance. Depersonalization is a relatively common and disturbing feeling that may exist if a person feels as if he/she is outside of one’s self, watching one’s self act, while having little or no control over a situation. Derealization is a term that might be used to describe an alteration in the perception or experience of the external world, so that it seems unreal. H. Thought Process: "Thought process (or form of thought) refers to the way in which a person puts together ideas and associations, the form in which a person thinks. Process or form of thought may be logical and coherent or completely illogical and even incomprehensible." (Kaplan and Sadocks’) Some words used to describe form of thought may include flight of ideas, loose associations, tangentiality, circumstantiality, rambling, evasiveness and perseveration. Additional descriptors might include word salad, clang associations, neologisms, and punning. Are the patient’s responses relevant or irrelevant? Is there poverty of ideas, rapid thinking, and does the patient have capacity for goal-directed thinking? I. Thought Content: Suggestions for this section include delusions, thought broadcasting, thought insertion, thought withdrawal, ideas of reference, and ideas of influence. "Disturbances in the content of thought include delusions, preoccupations (which may involve the patient’s illness), obsessions…compulsions…phobias, plans, intentions, recurrent ideas of suicide or homicide, hypochondriacal symptoms, and specific antisocial urges…Delusions may be mood congruent (in keeping with a depressed or elevated mood) or mood-incongruent…Ideas of reference and ideas of influence should also be described." (Kaplan and Sadocks’) 11 Revised 12/10/2012 J. Suicidal / Homicidal Ideations: Although suicidal and homicidal ideation may have been addressed in thought content above, these items were separated out for clarity and emphasis. These items may further be described in terms of presence of a plan or intent to follow through with ideas. In some cases patients will present with a history of recent suicidal or homicidal behavior, only to deny such thought thoughts at time of evaluation. When appropriate and indicated, inclusion of such recent information may be helpful. K. Sensorium / Cognition: Although only alertness, orientation and concentration are listed as examples on the form, descriptions of a patient’s sensorium and cognition can be more defined. This portion of the mental status examination seeks to assess organic brain function primarily, and should pay particular attention to alertness and level of consciousness, as well as orientation. No doubt, such items as capacity for abstract thought, intellectual functioning, and level of insight and judgment may also be addressed in this area, but are separated out in this document for clarity and emphasis. "Some terms used to describe the patient’s level of consciousness are clouding, somnolence, stupor, coma, lethargy, alertness, and fugue state." "Disorders of orientation are traditionally separated according to time, place, and person." (Kaplan and Sadocks’) Concentration and attention may be addressed by subtracting serial 7’s from one hundred, subtracting threes, or by asking the patient to spell the word "world" (or others) backward. The patient can also be asked to name five things that start with a particular letter. As above, other topics such as capacity to read and write, visuospacial ability, and abstract thinking may also be covered in this area, and inclusion of such items is left up to the evaluator. L. Memory: Include recall, recent and remote memory. Also include how memory was assessed. "Memory functions have traditionally been divided into four areas: remote memory, recent past memory, recent memory, and immediate retention and recall."(Kaplan and Sadocks’ Synopsis of Psychiatry) Note: "Confabulation (unconsciously making up false answers when memory is impaired) is most closely associated with cognitive disorders." (Kaplan and Sadocks’) M. Intellectual Functioning: Also a possible measure of cognitive impairment, this item too was separated for clarity and emphasis. Intellectual functioning may be described in terms like above average, average, low average, borderline intellectual functioning, mild mental retardation, moderate mental retardation, etc. A more descriptive assessment of the patient’s intellectual functioning is encouraged. Documentation to support conclusions about estimates intellectual functioning is also encouraged. N. Judgment: "Does the patient understand the likely outcome of his or her behavior, and is he or she influenced by that understanding? Can the patient predict what he or she would do in imaginary situations? For instance, what would the patient do if he or she smelled smoke in a 12 Revised 12/10/2012 crowded movie theater?" (Kaplan and Sadocks’) With the above examples in mind, the evaluator is encouraged to assess situations that may more directly apply to situations that the patient may likely encounter in his or her daily life. Of particular importance, are those situations that may prove dangerous to the patient or others if adequate judgment is lacking. O. Insight: "Insight is the patient’s degree of awareness and understanding that they are ill…" (Kaplan and Sadocks’) P. Impulse Control: It would be appropriate to include any recent history of violent, hypersexual, or other dangerously impulsive behaviors in this section. Recent fighting, assault, or employment of restraints by referring facility should be included. "Is the patient capable of controlling sexual, aggressive, and other impulses?…An assessment of impulse control is critical in ascertaining the patient’s awareness of socially appropriate behavior and is a measure of the patient’s potential danger to self and others." (Kaplan and Sadocks’) XXI. PRINCIPAL DIAGNOSIS (from the APA Diagnostic and Statistical Manual of Mental Disorders, 4th Edition –Text Revision) (Note: PLAN TO AUTOPOPULATE ITEMS FROM THIS SECTION INTO TREATMENT PLAN.) Diagnostic classification is made according to the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition –Text Revision (DSM-IV-TR). DSM-IV-TR uses a multi-axial classification scheme consisting of five axes, each of which should be covered in the diagnosis." Axis I: consists of all clinical syndromes (for example, mood disorders, schizophrenia, generalized disorder) and other conditions that may be of focus of clinical attention. Axis II: consists of personality disorders, mental retardation, and borderline intellectual functioning. Axis III: consists of any medical conditions (for example, epilepsy, cardiovascular disease, endocrine disorders). Axis IV: refers to psychosocial and environmental problems ( for example, divorce, injury, death of a loved one) relative to the illness. Axis V: relates to the Global Assessment of Functioning (GAF) exhibited by the patient during the interview (for example, social, occupational, and psychological functioning); for adults, the 100 point GAF rating scale can be used. XXII. STRENGTHS, NEEDS, ABILITIES/INTERESTS, AND PREFERENCES (Note: PLAN TO AUTOPOPULATE ITEMS FROM THIS SECTION INTO TREATMENT PLAN.) A. STRENGTHS: According to Tondora & Davidson (2006), “Focusing solely on deficits in the absence of a thoughtful analysis of strengths disregards the most 13 Revised 12/10/2012 critical resources an individual has on which to build in his or her efforts to adapt to stressful situations, confront environmental challenges, improve his or her quality of life, and advance in his or her recovery. Strengths-based approaches allow providers to balance critical needs that must be met with the resources and strengths that people possess to assist them in this process.” In “The Strengths Model: Case Management with People with Psychiatric Disabilities,” 2nd edition by Charles A. Rapp & Richard J. Goscha, four types of strengths are listed in a strengths model: 1) Personal qualities/characteristics (e.g., devotion to family, honest, caring, hopeful, hard-working, patient, friendly, willing to help others, etc.); 2) Skills/talents (e.g., plays instrument, cooking, mechanical inclination, photography, good memory, knowledgeable in a field, etc.); 3) Environmental Strengths (e.g., plays instrument, cooking, mechanical inclination, photography, good memory, knowledgeable in a field, etc.) ; and 4) Interests/aspirations (e.g., personal goals, loves to fish, watches old movies, spend more time with family/friends, sports, leisure, recreation, etc.) B. C. D. XXIII. Use the narrative/text box space provided to list strengths that might contribute to the meeting of treatment plan goals, especially as noted in the following areas: Education, Employment/Income, Living Situation/Basic Needs, Social/Family/Community Support and Integration, and/or other strengths. Any additional relevant strengths should be listed in this section as well. NEEDS: Document any needs described by the client in the following areas: Education, Employment/Income, Living Situation and Basic Needs, Social/Family/Community Support and Integration, and/or any other important needs. ABILITEIS/INTERESTS: Include any described abilities or interests in the following areas: Education, Employment/Income, Living Situation and Basic Needs, Social/Family/Community Support and Integration, and/or others. PREFERENCES: In this section, describe person’s global preferences/hopes for recovery, including any specific preferences related to Treatment, Education, Employment/Income, Living Situation and Basic Needs, Social/Family/Community Support and Integration, and/or Other Important stated preferences. INTERPRETIVE SUMMARY AND PLAN OF CARE: Completing this section is a required element of the interview documentation. The overall intent of this section is interpret assessment findings and to capture both covered services (e.g. Medication Management, Psychological Testing, Individual/Family/Group Therapy, CPST, ACT, etc.) within the LBHP, and any additional services or linkages needed (e.g. vocational, educational, medical or self-help services preferred or desired by the client, even if not offered as a covered service within the Louisiana Behavioral Health Partnership. The listing should include recommended treatments/assessments, level of care, duration, as well as other needs related to clinical/central theme, co-occurring disabilities, environmental and personal supports/needs. (Note: PLAN TO AUTOPOPULATE ITEMS FROM THIS SECTION INTO TREATMENT PLAN.) A. Interpretive Summary: According to CARF International’s 2012 Behavioral Health 14 Revised 12/10/2012 Standards Manual, “(t)he Interpretive Summary is written to integrate and interpret from a broader perspective all history and assessment information collected. It should identify cooccurring disabilities and address how they are considered when developing the personcentered plan. The Interpretive Summary could address: • • • • • • The central theme(s) apparent in the presentation of the person served. Histories and assessments (medical, psychosocial, spiritual, or vocational), with special emphasis on potential interrelationships between sets of findings. The perception of the person served of his or her needs, strengths, limitations, and problems. Clinical judgments regarding both positive and negative factors likely to affect the person’s course of treatment and clinical outcomes after discharge. Recommended treatments, including any special assessments or tests, as well as routine procedures (e.g., laboratory tests). A general discussion of the anticipated level of care, length, and intensity of treatment and expected focus (goals) with recommendations.” NOTE: Any Urgent Needs identified in section II above MUST be addressed here. B. C. D. 1915(i) Plan of Care Service Options: Check all that apply. Med Mgt.; Psychological Testing; Family Therapy; Individual Therapy; Group Therapy; Case Conference; Alcohol/Drug Assessment; Alcohol/ Drug Individual Therapy; Alcohol/Drug Group Therapy; Detoxification; Alcohol/Drug IOP; Alcohol/Drug Halfway House PSR; CPST; ACT; ICM. Use space provided to recommend any additional or other service options. Additional relevant comments may also be provided under item “C” of this section. Other Services/Linkages Needed: This section is intended to document any additional service needs that might not be part of the LBHP covered services benefit package. Choices for this section include: Vocational Services; Social Services; Educational Services; Medical Services/PCP; Self help Groups. Other services may be listed in space provided. Additional Comments: Space is provided for any relevant or clarifying detail. SIGNATURE • • • PRINTED NAME OF ASSESSOR: Interviewer/assessor must print full name, with credentials (e.g. MD, PhD, APRN-CNS, LCSW, etc.) legibly in space provided. SIGNATURE - For purposes of authentication, a signature of a qualified Licensed Mental Health Practitioner completing this evaluation is required. LMHP STATUS: Check the appropriate box: Psychiatrist, Psychologist, Medical Psychologist, APRN-CNS, LCSW, LPC or other. If “other” is chosen, provide detail in space provided. DATE - This is intended to include the actual date that the evaluation was printed, charted and/or signed by 15 Revised 12/10/2012 the practitioner who completed the evaluation. In some cases this date will be the same as the date of admission, but in other cases, these dates may not be the same. The date of dictation does not go here –only the date that the evaluation was completed, signed and authenticated. The date of dictation and transcription may be tracked elsewhere. 16 Revised 12/10/2012