A reflective account of a consultation in abortion care
advertisement

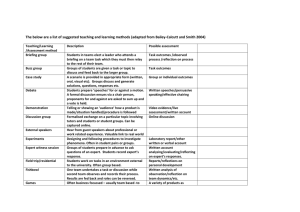
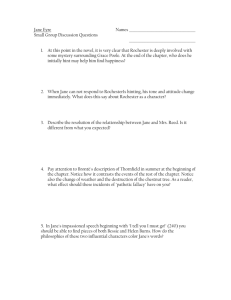
p35-39w35 24/4/09 15:45 Page 35 If you would like to contribute to the art and science section contact: Gwen Clarke, art and science editor, Nursing Standard, The Heights, 59-65 Lowlands Road, Harrow-on-the-Hill, Middlesex HA1 3AW. email: gwen.clarke@rcnpublishing.co.uk A reflective account of a consultation in abortion care Astbury-Ward E (2009) A reflective account of a consultation in abortion care. Nursing Standard. 23, 35, 35-39. Date of acceptance: December 1 2008. Summary This article presents a reflective account of a consultation in a pre-assessment clinic for women requesting abortion. The reflection is based on Johns’ model. Reflection enabled the author to address important issues that the consultation raised. These included the realisation that nurses do not always have to understand why patients make the choices they do, and the importance of allocating sufficient time for sensitive consultations. Author Edna Astbury-Ward is contraceptive and sexual health specialist nurse, Western Cheshire Primary Care Trust, and doctoral research fellow, Centre for Health and Community Research, Glyndwr University, Wrexham. Email: e.astburyward@glyndwr.ac.uk a six-year-old and a one-year-old, from previous relationships. She is a vibrant, lively and articulate person. She smiled easily and maintained good eye contact with me during the consultation. Jane requested her fourth abortion at the clinic and attended with her children. She estimated her current pregnancy to be between eight and nine weeks, but was unsure of her dates. Results of the ultrasound dating scan revealed a twin pregnancy of seven weeks’ gestation. I chose to reflect on this consultation because the circumstances of the case provoked a wide range of feelings and emotions in me, which broadened the scope for reflection. Keywords Introduction Abortion; Communication; Consultation skills; Reflective practice These keywords are based on the subject headings from the British Nursing Index. This article has been subject to double-blind review. For author and research article guidelines visit the Nursing Standard home page at nursingstandard.rcnpublishing.co.uk. For related articles visit our online archive and search using the keywords. The process of reflection is not new; Dewey (1933) suggested it is a process of active, persistent and careful consideration, which supports further conclusions. It has also been described as the internal examination and exploration of issues resulting in changes of thought (Boyd and Fales 1983) and as a process of review that informs learning (Reid 1993). Additionally, Clarke and Graham (1996) suggested that reflection allows us to make sense of experience and enables us to reach reasoned decisions. In some instances such a reflection might enable us to decide on distinctive and well-reasoned ways to progress, in other instances it can help us understand conundrums encountered. Reflection may help us to understand what we feel and identify our strengths and limitations. After careful consideration of the reflective process, I chose to use Johns’ (2000) model to structure my reflection as it offers the reflective practitioner greater capacity for exploration and expression of feelings. Johns’ (2000) model THE FOLLOWING EVENTS took place in a pre-assessment clinic (formerly known as a termination of pregnancy clinic) where patients are seen on an appointment basis. Routine tests include height, weight, blood tests, body mass index, blood pressure measurement, self-swab for Ch l a m y d i a and gonorrhoea, and ultrasound scanning. Consultation between the nurse and patient includes discussion of the various options for the current pregnancy, including adoption, and future contraceptive advice. The patient discussed in this article will be given the pseudonym of Jane. Jane is a 25-year-old single woman with two children, NURSING STANDARD may 6 :: vol 23 no 35 :: 2009 35 p35-39w35 24/4/09 15:45 Page 36 & art & science reflective practice covers a variety of issues that may arise during reflection. It provides a clear and guided approach, which allows the practitioner to structure his or her thoughts in a more detailed way than Gibbs’ (1988) reflective cycle. Johns’ (2000) model for reflection can be used as a guide for analysis of a critical incident or for general reflection on experience. It could also be useful in complex decision making and analysis. Johns (2000) considered that, by sharing reflections on learning experiences, greater understanding of those experiences could be achieved than by reflection alone. A reflective learning cycle was used in addition to the Johns’ (2000) model to assist with integrating new information into practice and evaluating its effect (Figure 1). The amount of care given in any therapeutic setting is governed by, among other factors, the amount of time spent interacting with the patient. However, this does not necessarily correspond to the quality of care given. When providing health care, time constraints may prevent the delivery of optimum care and may result in other areas of care being compromised and even neglected. Sub-standard care may have a long-term negative effect on the patient and family members, but may also affect the provider of that care. During my 25-year nursing career I have endeavoured to give the best care that I can, but on occasions I feel I have been prevented from doing so because of external forces beyond my FIGURE 1 Reflective learning cycle Evaluate or reflect on the impact of the decision Practice Integrate the decision into practice Make a decision and consider the impact External triggers Formulate a question/s Seek information Analyse, interpret or reflect on the information (Adapted from The College of Family Physicians of Canada 2009) 36 may 6 :: vol 23 no 35 :: 2009 control, for example time constraints. Jane’s case was one such occasion. The following reflection considers how being short of time in a therapeutically challenging encounter affected my feelings. Conflict and incongruence Because of time constraints I did not have the opportunity to assess Jane’s feelings fully, therefore I only observed briefly the depth and complexity of her situation. I speculated about the motives and circumstances associated with her abortion request. I felt frustrated that time constraints meant I was unable to enquire further about her circumstances and feelings, which may have provided further insight into her situation. On reflection this enquiry might have been an uncomfortable and intrusive experience for Jane. Had there been more time in the therapeutic setting, I would ideally have liked to explore issues of self-esteem, attachment, intimacy and loss to gain a better understanding of Jane’s private and personal functioning. I may also have explored her childhood experiences and whether she felt this had any relevance to her current situation. However, would retrospective assessment and knowledge of Jane’s circumstances have had any bearing on the outcome, and why did I feel the need to know these things? This after all was not a counselling session. However, exploring the decision-making process with Jane may have provided me with greater insight and understanding and an opportunity to offer more sensitive support. Perhaps more relevant to the consultation were the circumstances of her sexual experiences and the impact they had on her, for example whether she was forced into a situation where she was unable to refuse sex or whether she was able to access contraception. For Jane, the ‘real’ problem arose when the results of the unltrasound revealed a twin pregnancy. Jane had initially made the decision to terminate the pregnancy based on her assumption that she had a singleton pregnancy. Although Jane was shocked by the thought of being pregnant with twins, this did not change her decision to have an abortion. As health professionals it is our duty to provide advice and information to enable patients to make informed decisions. However, it is not always easy to accept situations where patients have ignored the advice given and put themselves at risk of further harm. Jane had made her decisions based, in part, on the information I had given her. However, I was concerned and felt that she had exposed herself to unnecessary suffering and grief, both mentally and physically. I considered that the key issue was Jane’s right to exercise choice and free will. NURSING STANDARD p35-39w35 24/4/09 15:45 Page 37 I began to think about the myriad factors she needed to consider to enable her to make this choice, including thinking about what it might be like to give birth to twins and then to give them up for adoption. Choice and decision making The notion of choice implies the exercise of free will, which enables a person to arrive at a considered decision based on the understanding of all relevant facts. Fox (2002) argued that people may make a choice based on temperament or unconscious desire rather than reason or conscious motivation. Healthcare professionals need to address the issues associated with clinical decision making, such as patient autonomy and the wider psychosocial influences governing patient choice. Coulter et al (1999) considered that patients cannot express informed preferences unless they are given sufficient and appropriate information including detailed explanations. Knowledge of this contributed to my feelings that I had failed Jane, because I was unable to give her as much information as I thought she needed to make her decision. The frustration for me was that I had access to detailed information about abortion options, but I was unable to deliver it comprehensively because of insufficient time available to spend with Jane. The other aspect of Jane’s situation that concerned me was the reasons she was requesting abortion for the fourth time. The decision to continue with a pregnancy or not is a complex one (Family Planning Association 2000, Royal College of Obstetricians and Gynaecologists (RCOG) 2004) and many circumstantial factors affect women’s abortion experiences (Astbury-Ward 2008). We can only make decisions if we understand why something is problematic and are aware of the possible solutions. We will only know the possible solutions if we have been told what options exist, or have researched or experienced them ourselves. Jane may have arrived at her decision to end the pregnancy because she may already have felt she knew what the possible outcomes would be as she had experienced them previously. Her decision may have been based on those experiences. If patients choose not to research their problems or have no previous experience of them, then they may rely solely on the quality and accuracy of the information that is given to them by healthcare professionals. I felt that Jane had made her choice based mainly on previous experience rather than on the information I had provided. It is important to ensure that an adequate amount of time is allocated to give each individual the information needed to enable her to make an informed choice. New ways of working have now been NURSING STANDARD implemented, releasing sufficient time for all consultations to allow full discussion of options for the patient. Nurses working in pre-assessment clinics now obtain consent from patients and remain with patients throughout the consultation process. This allows greater opportunity to form a therapeutic alliance to develop and a full discussion of all possible options. As mentioned, Jane made her decision based primarily on experience. However, other patients may be entirely dependent on the information provided at the consultation. If the information given is either insufficient or inaccurate, it could be argued that informed consent has not been gained. In contrast, some people do not necessarily need (or want) to receive all the facts before they make a decision, preferring to put their faith in the medical and nursing professions. Motherhood and myths As healthcare providers, we do not need to know or understand all of the reasons why patients make the choices that they do. I began to think about the many reasons, psychological, social and practical, why a woman may chose to have an abortion (Walker 2001). I also considered the issues surrounding pregnancy. I thought that for some women the desire to be pregnant might not necessarily be the same as the desire to have a baby. Pregnancy for some women makes them feel alive and invigorated – a way of experiencing their female identity and a way of making them feel special or the centre of attention. To become pregnant reminds and perhaps reassures the woman about her fertility. For these women perhaps the end of the pregnancy, heralds the onset of emptiness, and the need for the void to be filled with another pregnancy. I had many unanswered questions about Jane. I wondered if pregnancy made her feel special and about her experience of motherhood. The experience of motherhood is complex. Richardson (1993) believed that in our society motherhood is considered necessary for full adult status as a normal and feminine woman, although this view is arguably changing now. Martin (1987) suggested that a woman’s body subordinates her free will to the uniquely female responsibility of serving the needs of nurturing the newly conceived embryo. In this sense, by saying no to the prospect of motherhood Jane might be saying yes to ultimate control over her body, to pursuing a career, and to giving her existing children better opportunities. Grey (2001) considered that in circumstances of abortion it may be impossible not to become critical or judgemental. Abortion provokes strong feelings; some may not see it as a great maternal sacrifice, but a drastic rejection of may 6 :: vol 23 no 35 :: 2009 37 p35-39w35 24/4/09 15:45 Page 38 & art & science reflective practice motherhood, and an act of selfish and gratuitous abandonment. Zoja (1997) believed that the act of abortion may not be directed at the fetus but is a rejection of motherhood itself and the values and certainties associated with it at this time. Jane had already experienced being a mother, so she knew exactly what she was giving up. She was also aware that she would again be entering motherhood alone because she was no longer with her partner. In some sections of society, unmarried mothers have been blamed for moral, economic and psychological decline in the nation (Roseneil and Mann 1996). I speculated whether the stigma attached to being a single mother may have affected Jane’s decision. I wondered if the negative representation of single mothers as an underclass in society had affected her decision. Repeat abortions Grey (2001) indicated that women who have repeat abortions – 32% of women, according to the Office for National Statistics (2007) – present the greatest challenge. Zoja (1997) claimed that even the most convinced supporters of the right to abort felt a certain uneasiness when faced with women who aborted repeatedly. I also felt a little uncomfortable about the apparent ease with which Jane came to the decision to abort for a fourth time. Requests for repeat abortions might generate negative feelings in the nurse, such as anger at the woman’s ‘irresponsibility’, frustration at her contraceptive choice or lack of it and distress, confusion and resentment for ‘wasting time’. Hayter (1996) suggested that nurses are not removed from the social forces that create and reinforce negative stereotypes of individuals, and implies that nurses are not immune to feelings or to prejudice. I too had formed assumptions about Jane before I met her. I assumed that she would be of low intelligence, lacking in communication skills, sad, vulnerable, needy and emotionally affected by previous abortions. In the clinical setting, nurses should put aside any prejudices if they are to provide objective, sensitive and non-judgemental care. This is a skill that requires self-analysis. Atkins (2004) suggests that a process of self-analysis should be encouraged without making people feel threatened. The process of self-analysis and reflection makes the nurse aware of his or her prejudices, enabling the provision of unbiased information in a manner which will not influence the patient’s decision. For some staff who have deep religious convictions the right to 38 may 6 :: vol 23 no 35 :: 2009 conscientious objection enables them to withdraw from treating or caring for individuals in certain circumstances. Some individuals believe that a legal obligation compelling them to act contrary to their religious convictions is a profound violation of their ethical and human rights (Dickens and Cook 2000). Although we might like to consider that we treat everyone in the same way, Rose (2004) argued that the complexity of human nature often leads to confusion when our beliefs and values are challenged in clinical practice. Walker (2001) commented that the irrational nature of human reproduction is not easy to quantify scientifically, and that there are a number of problems associated with research on psychological responses to abortion, partly because women are often reluctant to participate in this research (Howie et al 1997), and because of the secret nature of abortion (Boorer and Murty 2001). However, Bennett (2004) argued that the irrationality of a choice does not make the choice immoral. He suggests that if we value individual freedom to determine our own lives, then we should also accept those decisions even if they appear to have no rational justification. Accordingly, if we accept abortion as a woman’s right, the nature of that right does not alter despite the number of times it has been exercised. Whatever the women’s reasons for choosing abortion, the role of the nurse is to provide informed, up-to-date, objective care for those involved. Most women, though not all, have already made their decision to end the pregnancy before approaching the health service and they expect non-judgemental support, information and prompt referral (Kumar et al 2004). There is still much to improve in relation to the quality and level of support given to women throughout the pre and post-abortion period. Discrepancies in access to abortion services in the UK were highlighted in the House of Commons health committee’s (2003) report on sexual health with a postcode lottery for accessing NHS funded abortions which varied between 46% and 96% in some areas. The RCOG (2004) identified that there are still large geographical variations in access to NHS-funded abortion, and there is much that we do not know about women’s experiences in the long and short-term following abortion. Conclusion Reflection has changed my way of thinking and broadened my perspectives. For me the journey through the reflective process has been difficult because initially I was a little hostile to it, not because of my beliefs and value systems, but because the process and skill of reflection need NURSING STANDARD p35-39w35 24/4/09 15:45 Page 39 to be learnt (Wampold and Holloway 1997). Gordon (2004) concluded that whatever stage of professional development practitioners are at, they may benefit by occasionally trying out a less familiar reflective strategy. Comfort with a particular model or process of reflection might not always challenge the person sufficiently to think beyond the confines of the model and therefore move forward. Reflection enabled me to recognise that it is not necessary that I know or understand all of the reasons why patients make certain decisions. Focusing on Jane’s situation helped me to understand that not all patients will agree with the advice or information offered by healthcare professionals. Jane has changed my way of thinking – not because of her situation, but because the process of reflecting on her case has shown me that I do not have to spend more time searching for the reasons why people do what they do. However, I do need to accept their right to bodily integrity and autonomy and I have found this liberating. Reflection provided me with the opportunity to assess how I deal with women requesting repeat abortions and I now feel better equipped to provide care that is objective yet sensitive to the needs of the individual NS References Astbury-Ward E (2008) Emotional and psychological impact of abortion: a critique of the literature. Journal of Family Planning and Reproductive Health Care. 34, 3, 181-184. Atkins S (2004) Developing underlying skills in the move towards reflective practice. In Bulman C, Schutz S (Eds) Reflective Practice in Nursing. Third edition. Blackwell Publishing, Oxford, 25-46. Bennett R (2004) Human reproduction: irrational but in most cases morally defensible. Journal of Medical Ethics. 30, 4, 379-380. Boorer C, Murty J (2001) Experiences of termination of pregnancy in a stand-alone clinic situation. Journal of Family Planning and Reproductive Health Care. 27, 2, 97-98. Fox NJ (2002) What a ‘risky’ body can do: why people’s health choices are not all based in evidence. Health Education Journal. 61, 2, 166-179. Gibbs G (1988) Learning by Doing: A Guide to Teaching and Learning Methods. www2.glos.ac.uk/GDN /gibbs (Last accessed: April 16 2009). Gordon C (2004) Counsellors’ use of reflective space. Counselling and Psychotherapy Research. 4, 2, 40-44. Grey K (2001) Unplanned pregnancy. In Andrews G (Ed) Women’s Sexual Health. Second edition. Harcourt Publishers, London, 189-208. Hayter M (1996) Is non-judgemental care possible in the context of nurses’ attitudes to patients’ sexuality? Journal of Advanced Nursing. 24, 4, 662-666. Boyd EM, Fales AW (1983) Reflective learning: key to learning from experience. Journal of Humanistic Psychology. 23, 2, 99-117. House of Commons Health Committee (2003) Third Report of Session (20022003) Sexual Health. The Stationery Office, London. Clarke DJ, Graham M (1996) Reflective practice, the use of reflective diaries by experienced registered nurses. Nursing Review. 15, 1, 26-29. Howie FL, Henshaw RC, Naji SA, Russell IT, Te m p l eton AA (1997) Medical abortion or vacuum aspirat i o n? Two year fo l l ow up of a patient preference trial. British Journal of Obstetrics and Gynaecology. 104, 7, 829-833. Coulter A, Entwistle V, Gilbert D (1999) Sharing decisions with patients: is the information good enough? British Medical Journal. 318, 7179, 318-322. Dewey J (1933) How We Think. A Restatement of the Relation of Reflective Thinking to the Educative Process. Heath, Boston DC. Dickens BM, Cook RJ (2000) The scope and limits of conscientious objection. International Journal of Gynaecology and Obstetrics. 71, 1, 71-77. Family Planning As so c i at i o n ( 20 0 0) Abortion: Just So You Know. FPA, Lo n d o n . NURSING STANDARD Johns C (2000) Becoming a Reflective Practitioner. Blackwell Science, Oxford. Kumar U, Baraitser P, Morton S, Massil H (2004) Decision making and referral prior to abortion: a qualitative study of women’s experiences. Journal of Family Planning and Re p ro d u ct i ve Health Care . 30, 1, 51-54. Martin E (1987) The Woman in the Body. A Cultural Analysis of Reproduction. Beacon Press, Boston. Office for National Statistics (2007) NHS Contraceptive Services, England 2005-06. The Information Centre, Leeds. Reid B (1993) ‘But we’re doing it already!’ Exploring a response to the concept of reflective practice in order to improve its facilitation. Nurse Education Today. 13, 4, 305-309. Richardson D (1993) Women, Motherhood and Childrearing. Macmillan Press, London. Rose C (2004) Class matters. Counselling and Psychotherapy Journal. 15, 8, 10-12. Roseneil S, Mann K (1996) Unpalatable choices and inadequate families: lone mothers and the underclass debate. In Silva EB (Ed) Good Enough Mothering? Feminist Perspectives on Lone Mothering. Routledge, London, 191-210. Royal College of Obstetricians and Gynaecologists (2004) The Care of Women Requesting Induced Abortion. Evidence-based Clinical Guideline Number 7. RCOG, London. The College of Family Physicians of Canada (2009) Mainpro® – Background Information. www.cfpc.ca/English/ cfpc/cme/mainpro/maintenance%20of%2 0proficiency/background%20info/default. asp?s=1 (Last accessed: April 24 2009). Walker A (2001) Pregnancy, pregnancy loss and induced abortion. In Miller D, Green J (Eds) The Psychology of Sexual Health. Blackwell Science, Oxford, 304-319. Wampold BE, Holloway EL (1997) Methodology, design and evaluation in psychotherapy supervision research. In Watkins CE (Ed) Handbook of Psychotherapy Supervision. John Wiley, New York, NY, 11-30. Zoja EP (1997) Abortion: Loss and Renewal in the Search for Identity. Routledge, London. may 6 :: vol 23 no 35 :: 2009 39