Radiation Exposure in Nuclear Medicine
advertisement

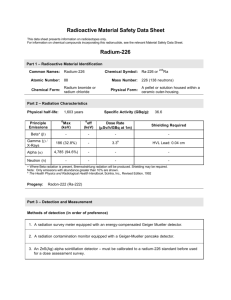
Radiation Exposure In Nuclear Medicine Darlene Metter, MD FACR DISCLOSURE STATEMENT I have no relevant financial relationships with commercial interests to disclose. Ionizing Radiation in Medical Imaging • • • • > 100 years Beneficial to patient care New & emerging technologies Revolutionized the practice of medicine Learning Objectives • Describe the trends in the use of NM procedures • Identify major sources of radiation exposure to: • the patient • the technologist • List 3 occupational radiation safety dose strategies for the NM technologist Pre-Test Question #1 • In 2006, the average annual radiation exposure in the US from medical imaging is estimated at: • • • • A. 30% B. 40% C. 50% D. 60% Question # 2 • Which one of the following is an example of a non-stochastic radiation effect? • • • • A. Cataracts B. Cancer C. Genetic defects D. Autism Question # 3 • Which one of the following exams has the highest pt radiation exposure? • • • • A. Cardiac (201Tl 4 mCi) B. Cardiac (99mTc 40 mCi, 1 day) C. Octreoscan (111In 6 mCi) D. F18 FDG 20 mCi Question # 4 • Which NM technologist task is generally associated with the highest work-related dose? • • • • A. Radiopharmaceutical preparation B. Radiopharmaceutical injection C. Patient scanning D. Patient transfers Question # 5 • Which NM procedure is generally associated with the highest occupational dose to the NM tech? • • • • A. Bone SPECT B. MUGA C. 131I WB post therapy scan D. Stress 99mTc MIBI Current Trends/Usage of NM Procedures Current Trends/Usage of NM Procedures • 2007 US medical procedures: highest source of ionizing radiation to the public • Inc in diagnostic imaging using ionizing radiation (F Mettler, 2008) – CT, vascular interventional, NM ACR Response: White Paper* • 2007 ACR Blue Ribbon Panel on Radiation Dose in Medicine • To assess current dose issue in medical procedures • Develop guidelines to protect & inform the public Amis et al “ACR White Paper on Radiation Dose in Medicine” 2007 JACR Vol 4 (5). P 272-284 ACR Panel Conclusion 1. Education of stakeholders in radiation safety 2. Appropriate utilization of imaging 3. Standardization of radiation dose data for archiving: benchmarking good practice 4. Identify pts who have reached certain thresholds; alternate imaging? Includes Nat Acad of Science; Nat Acad of Engineering; IOM; National Research Council 1.5 day meeting with ACR input Increasing public concern* * SNM Smart Brief 11/28/2011 ACR Panel Report • 1980 • 2005 • CT 3 million • NM 7 million • CT 60 million • NM 20 million Est # NM Exams (X1000) (US)* 1970 Brain 1250 GU 110 Bone 80 Lung 330 Thyroid 450 CV 25 Total 3230 Pop (106) 209 1975 2100 150 220 600 630 50 4800 215 1980 870 200 1300 900 650 600 5850 227 2005 <100 470 3450 740 <100 9800 19,000 300 • Mettler FA 2008 “Medical Effects of Ionizing Radiation Est # NM Exams (X1000) (US)* 1970 Brain 1250 GU 110 Bone 80 Lung 330 Thyroid 450 CV 25 Total 3230 Pop (106) 209 1975 2100 150 220 600 630 50 4800 215 1980 870 200 1300 900 650 600 5850 227 2005 <100 470 3450 740 <100 9800 19,000 300 • Mettler FA 2008 “Medical Effects of Ionizing Radiation Est # NM Exams (X1000) (US)* 1970 Brain 1250 GU 110 Bone 80 Lung 330 Thyroid 450 CV 25 Total 3230 Pop (106) 209 1975 2100 150 220 600 630 50 4800 215 1980 870 200 1300 900 650 600 5850 227 2005 <100 470 3450 740 <100 9800 19,000 300 • Mettler FA 2008 “Medical Effects of Ionizing Radiation Gamma Camera Sales • 11/23/11 Global Industry Analysts, Inc • Report: global market for gamma cameras projected to inc to $846.6 million by 2017 • US is the largest global market • Why? Aging pop, inc death rate assoc w/ cancer, cardiac & CNS disease • Inc public awareness of advanced imaging What About PET? • Bio-Tech Sys of Las Vegas: market researcher providing insight into new technologies & trends • Predict: PET procedures to increase • SPECT: 2010 $758 million to 2018 $1.68 billion Why? • Wider availability of FDG & PET technology • Wider physician & patient acceptance • Increased approved indications (ie reimbursement) • Emerging novel tracers: oncology, cardiology, neurology PET Procedures • 2009: increase 9% • 2010: increase 9% • PET agents:* – 2010 $391.8 million – 2018 $4.31 billion • CMS reimbursement issues, but PET users adapted to reimbursement requirements** * Bio-Tech Systems ** NOPR 2006-09 expanded CMS coverage; NOPR 2009 FDG Sales • Reflection of PET procedures • 2009: $300 million for FDG • 2017: projected $800 million for FDG • 2017: projected $3.43 billion for all PET RP Average Annual Radiation Exposure* • 1987: radon/NORM majority medical imaging 15% (XR, NM) • 2006: medical imaging 51% radon 30% internal/therapies 6% cosmic 6% * Mettler FA 2008 “Medical Effects of Ionizing Radiation” Average Annual Radiation Exposure* • 1987: radon/NORM majority medical imaging 15% (XR, NM) • 2006: medical imaging 51% radon 30% internal/therapies 6% cosmic 6% • US avg: 6.27 mSv/y (WW: 2.4 mSv/y) • Mettler FA 2008 “Medical Effects of Ionizing Radiation Radon • Decay product of uranium • t½: 4.5 billion yr • Largest component in background radiation, granite bedrock (earth’s crust) – 3 mSv or 300 mrem/yr per person in US • Gas accumulating in buildings: – attics, basements – indoor air contaminant – Texas: low–mod potential NO high potential San Antonio Orlando ACR Panel Report • Japanese atomic bomb survivor data – most compreh epidem study supporting radiation induced carcinogenesis • Statistically signif inc in CA at doses > 50 mSv; below ?? - controversial • CT-NM studies dose estimates: 10-25 mSv/study • Implication of multiple studies ACR Panel Report • “1 yr collective dose estimate from medical procedures in the US = total WW collective dose generated by the nuclear catastrophe at Chernobyl” ACR Panel Report • Radiation induced CA latency: 10-20 years or longer • Effects of current inc dose not evident for many years • Difficult to attribute “radiation induced CA” from a study from normal risk* ~ 40% of population dx w/ CA in lifetime * Can’t distinguish radiation induced CA from others Review: Trends in NM Procedures • Since 1980, inc number of NM proced • Major sources of radiation to public: –A medical exposure, background SIX fold increase in 26 years! radiation & radon • Mettler (2008) population per caput Or a 600% increase in one annual dose from medical radiation:* generation – 1980: 0.54 mSv – 2006: 3.2 mSv (> bkgd 2.3 mSv) * Huda W, Mettler FA Radiol: Vol 258(1) Jan 2011; p 236-242 Question #1 • In 2006, the average annual radiation exposure in the US from medical imaging is estimated at: • • • • A. 30% B. 40% C. 50% D. 60% Question #1 • In 2006, the average annual radiation exposure in the US from medical imaging is estimated at: • • • • A. 30% B. 40% C. 50% D. 60% NM PROCEDURE DOSES TO: the PATIENT Courtesy L Gordon, MD Med Univ of SC Understanding Patient Exposure • Most physicians do not understand • Goal: education; can then weigh a procedure’s risks & benefits • Mettler: – NM study avg pt dose: 0.3-20 mSv – average annual effective dose from background radiation: 2.5-3 mSv Radiation Protection in US • Before 1950, concern was occupational exposure • Mid-1950s, public concern included - patient & individual - population: progeny, genetic pool as a whole Terminology 1. Stochastic vs Non-stochastic effects 2. Quantification of radiation exposure Stochastic Effects* • “Effects that occur by chance, generally occurring without a threshold level of dose, whose probability is proportional to the dose and whose severity is independent of the dose. In the context of radiation protection, the main stochastic effects are cancer and genetic effects.” NRC website: www.nrc.gov Stochastic Effects • Uncertain if chronic low dose radiation leads to adverse latent effects: CA • Appears most low dose radiation → cellular repair → no adverse effects • What are the adverse cellular effects of radiation? Radiation: Adverse Cellular Effects • Cells vary in radiosensitivity (“cell death”*) – degree of proliferation, differentiation, duration of mitosis • Cell radiosensitivity: function of cell type – Low: non-dividing, fixed post-mitotic • mature RBC, bone, cartilage • muscle, ganglion cells • mature connective tissue • Radiation cell death caused by the double-stranded DNA break Radiation: Adverse Cellular Effects • High: less differentiated, divide quickly • Lymphocytes, immature hematopoietic, intestinal epithelium, spermatogonia, ovarian follicular cell BEIR Committee • National Academy of Science: Biological Effects of Ionizing Radiation Committee • Claims future CA risk for low level ionizing radiation uses a nonthreshold, linear model for cancer induction • Data: atomic bomb survivors BEIR VII* • Supports “linear-no-threshold” model • CA risks proceeds linearly at low doses w/o a threshold, smallest dose has the potential to cause a small inc in CA risk • Low dose: up tp 100 mSv * Biologic Effects of Ionizing Radiation (June 2005), Nat Acad Sciences 100 people BUT other 42 are naturally occurring. One 100 mSv exposure 1 Cancer Background Cancer in Population • Cancer diagnosis: ~ 42/100 people • 1/1000 could be from a single 10 rem (0.1 Sv) dose above background radiation* • Since the BEIR Committee assumes the linear no threshold model, risks from cancer can be calculated * BEIR VII report Stochastic Effects • But there appears to be a threshold to adverse effects at 0.05-0.1 Sv, but to be conservative, NRC assumes: – no threshold – linear response – ALARA principle ALARA Principle • “As-Low-As-Reasonably-Achievable” • 3 tenets: time, distance, appropriate shielding • ALARA I: 125 mrem/quarter • ALARA II: 375 mrem/quarter • Helps to set “checkpoints,” if reached should justify investigation & action Non-Stochastic Effects* • “ The health effects of radiation, the severity of which vary with the dose and for which a threshold is believed to exist. Radiation-induced cataract formation is an example of a nonstochastic effects (also called a deterministic effect).” NRC website: www.nrc.gov Radiation Cataractogenesis • • • • • Non-linear Dose-related threshold:~2 Gy/200 rad Doses > 7 Gy: 100% cataracts Latency: ~ 15 yrs High LET, greater RBE (factor 2 or >) – e.g. shorter duration at a higher dose, faster cataract formation Radiation Effects • Stochastic • Non-stochastic • Severity: independent of dose • Probability of occurrence: inc with dose • Threshold: No • Severity: increases with dose • Probability of occurrence: inc with dose • Threshold: Yes Question # 2 • Which one of the following is an example of a non-stochastic radiation effect? • • • • A. Cataracts B. Cancer C. Genetic defects D. Autism Question # 2 • Which one of the following is an example of a non-stochastic radiation effect? • • • • A. Cataracts B. Cancer C. Genetic defects D. Autism Quantification of Radiation Exposure Quantification of Radiation Exposure • • • • • Measured quantities Exposure Absorbed dose Equivalent dose Effective dose Quantification of Radiation Exposure • Measured quantities: (Curie, Ci; Bequerel, Bq) administered activities • Exposure • Absorbed dose • Equivalent dose • Effective dose Quantification of Radiation Exposure • Measured quantities • Exposure: (Coulomb/kg; Roentgen, R) exposure in air; amt of X- or gamma rays producing a given amt of ionization in each unit of air • Absorbed dose • Equivalent dose • Effective dose Quantification of Radiation Exposure • Measured quantities • Exposure • Absorbed dose: (Gray, Gy; rad) amt of energy absorbed per unit mass • Equivalent dose • Effective dose Quantification of Radiation Exposure • • • • Measured quantities Exposure Absorbed dose Equivalent dose: (Sievert, Sv, rem) absorbed dose X quality factor; QF for photons = 1 (beta, gamma); quantifies biologic harm to tissue related to type of radiation • Effective dose Quantification of Radiation Exposure • • • • • Measured quantities Exposure Absorbed dose Equivalent dose Effective dose: (Sievert, Sv; rem) equiv dose X tissue weighting factor; whole body dose estimates via dose to & sensitivity of each organ; calculated; allows comparison between ionizing radiation sources Effective Dose • “Individual dose is best calculated by determining the mean doses to all radiosensitive tissue combining with age, sex & organ specific coefficients.” • Example: – avg EDE background radiation: 2.5 mSv/y – EDE chest xray: ~ 0.1 mSv – Annual dose near Chernobyl: ~ 6 mSv/y Effective Dose • Calculations based on anthropomorphic phantoms with internal dosimeters or by the Monte Carlo method of computational algorithms – easy to measure • Patient actual dose from a NM procedure: very difficult American Nuclear Society NM Procedures : Sources of Patient Doses 1. General NM 2. CT: – SPECT/CT – PET/CT 3. PET tracers 5 min NM Procedures : Sources of Patient Doses 1. General NM 2. CT: – SPECT/CT – PET/CT 3. PET tracers Est # NM Exams (X1000) (US)* 1970 Brain 1250 GU 110 Bone 80 Lung 330 Thyroid 450 CV 25 Total 3230 Pop (107) 209 1975 2100 150 220 600 630 50 4800 215 1980 870 200 1300 900 650 600 5850 227 2005 <100 470 3450 740 <100 9800 19,000 300 • Mettler FA 2008 “Medical Effects of Ionizing Radiation Growth in Imaging • CARDIAC • BONE • 1970: 25,000 • 1970: 80,000 • 2005: 9,800,000 • 2005: 3,450,000 • Effective dose: ~ • Effective dose: 10 mSv or 1 rem 5.2 mSv (24 mCi MDP) Effective Dose in NM Imaging • • • • > 85% labeled with Tc99m 100-1100 MBq (2.7-29.8 mCi) ED: 1-10 mSv PET/CT ED: 20-37 mSv (2-3.7 rem) – FDG: 14.1 mSv (20 mCi) – CT: 10-15 mSv Effective Doses in NM • • • • • • Brain: HMPAO FDG Thyroid: 123I TCO4 Parathyroid MUGA ED (mSv) 6.9 14.1 1.9 4.8 6.7 7.8 mCi 20 20 0.15 10 20 30 Effective Doses in NM • Cardiac: 201Tl • MIBI (2 d • MIBI (1d) • • FDG • Lung: MAA 133 Xe • • DTPA • GI Bleed ED (mSv) 37 12.8 9.4 11.4 14.1 2 0.5 0.2 7.8 mCi 4 40 30 40 20 5 20 35 30 Effective Doses in NM • Renal: DTPA • MAG3 • DMSA • GH • Bone: • • ED (mSv) 1.8 2.6 3.3 2.0 6.3 5.2 3.5 mCi 10 10 10 10 30 24 16 Effective Doses in NM • • • • • • • • ED (mSv) 67Ga 15 Octreoscan 26 WBC: 111In 7 HMPAO 8.1 Tumor: FDG 14 PET/CT 37 MIBG: 131I 7.4 mSv/mCi 123I 0.67 mSv/mCi mCi 4 6 0.5 20 20 0.5-1 5-10 Effective Doses in NM • • • • • • • • ED (mSv) 67Ga 15 Octreoscan 26 WBC: 111In 7 HMPAO 8.1 Tumor: FDG 14 PET/CT 37 MIBG: 131I 7.4 mSv/mCi 123I 0.67 mSv/mCi mCi 4 6 0.5 20 20 0.5-1 5-10 111In • • • • • Octreotide SPECT/CT* Package insert, 70 kg pt 4.35 mSv/mCi 6 mCi = 26 mSv (SPECT) CT: 10 mSv SPECT/CT: 26 + 10 = 36 mSV •Sheu et al U of Pittsburgh MC “SPECT/CT and PET/CT: What Radiation Dose are Your Patients Getting and What Does It Mean to Them? 2010 RSNA NM Imaging • So what does this all mean? • How does one quantitate this? • How does this relate to one’s cancer risk? ACR Website • Equates studies with a time equivalent of background radiation and cancer risk • NOTE: 1 in 5 will die from CA • Risk of dying from CA due to exam: - v low: 1 in 104 to 105 - low: 1 in 103 to 104 - moderate: 1 in 500 to 103 Equivalence (background radiation) and CA Risk • • • • • • • • • • Abd/pelv Abd/pel: -/+ Coronary CTA Ca++ score CT colon BE Spine Chest Chest CTA/PE Head 15 mSv 5 yr 30 10 16 5 3 1 10 3 8 3 6 2 7 2 15 5 2 8 mo low mod low low low low low low low v low Extrapolate the Dose to NM procedures • Mod risk: 201Tl 37 mSv: 4 mCi Octreoscan SPECT/CT: 36 mSv FDG/PET CT: 20-37 mSv 67Ga 30 mSv: 8 mCi • Risk of dying from CA: 1 in 500 to 1000 Extrapolate the Dose to NM procedures • Low risk: Cardiac 99mTc (MPI, MUGA) • MDP, WBC • Brain HMPAO/FDG • V/Q, GI & GU • MIBG, Thyroid/parathyroid • Risk of dying from CA: 1 in 1000 to 10,000 (from the exam) Procedure Equivalence (CXR) • • • • • • • Study Eff Dose (mSv) Dental 0.005-0.01 CXR 0.1 MMG 0.4 CT 2-16 NM 0.2-41 Interventional Fluoroscopy >70 # CXR 0.25-0.5 1 20 100-800 10-2050 250-3500 Question # 3 • Which one of the following exams has the highest pt radiation exposure? • • • • A. Cardiac (201Tl, 4 mCi) B. Cardiac (99mTc , 40 mCi, 1 day) C. Octreoscan (6 mCi) D. F18 FDG 20 mCi Question # 3 • Which one of the following exams has the highest pt radiation exposure? • A. Cardiac (201Tl, 4 mCi) CT Dose Reduction CT Acquisition Parameters • kVp: kinetic energy of the electron; inc kVp → inc dose; inc penetrating power; dec contrast (~ 120 kVp) • mAs: photon flux; inc mAs → inc # photons, inc dose (~ 120 mAs or >) • Pitch: how far CT table travels per xray source rotation; inc pitch → dec dose: dec z-axis resol + recon artifact Which Parameter Has a Greater Effect on Dose: kVp or mAs? • • • • • • • kVp 90 90 120 120 140 140 mAs 25 300 25 300 25 300 Brain (mGy) 1.39 17.00 3.21 37.79 5.08 65.07 Eye 1.94 20.31 3.71 49.72 5.44 69.75 Which Parameter Has a Greater Effect on Dose: kVp or mAs? • • • • • • • kVp 90 90 120 120 140 140 mAs 25 300 25 300 25 300 Brain (mGy) 1.39 17.00 3.21 37.79 5.08 65.07 Eye 1.94 20.31 3.71 49.72 5.44 69.75 Which Parameter Has a Greater Effect on Dose: kVp or mAs? • • • • • • • kVp mAs Brain (mGy) Eye 90 25 1.39 1.94 dose with inc 20.31 kVp 90RESULTS: 300 Inc 17.00 & mAs, inc with mAs 3.71 is linear, 120 25but the 3.21 the inc300 with kVP37.79 is squared. 49.72 120 140 25 5.08 5.44 140 300 65.07 69.75 Strategies to Decrease Pt Dose • Modulate kVp & mAs depending on pt size & body part scanning • Use low dose for: – localization (dec dose: 50-65%) – attenuation correction (dec dose: 97%) – chest CT (lung) – small patient Other Strategies to Consider • Appropriateness of the procedure • Dec radiopharmaceutical doses (inc imaging time) • Dec CT acquisition parameters if a diagnostic CT will not add to the current available information NM PROCEDURE DOSES TO: the TECHNOLOGIST US NRC Maximal Annual Permissible Limits for Occupational Exposure • Whichever is more limiting: – Total EDE OR – Sum of deep DE to org/tissue (except lens) 50 mSv 500 mSv • Shallow DE to skin/extremity • Eye/lens (nonstochastic) • Minors (<18 yrs) 10% of above 500 mSv 150 mSv 3 Tenets of ALARA • Time • Distance • Appropriate shielding Time • Greater time near a radiation source → greater exposure • Major radiation source: • Common clinical settings: – dosing room, patient transfers (to and from the imaging room/table), imaging time, uptake time, waiting time Time • Greater time near a radiation source → greater exposure • Major radiation source: the patient • Common clinical settings: – dosing room, patient transfers (to and from the imaging room/table), imaging time, uptake time, waiting time Why are the technologists here? While the patient is here? Limit their occupational dose. Time Suggestion Strategies • Be aware of the proximity of injected patients • Explain proced/pt questions before inject RP • Hall or room where injected pt are waiting to be scanned (take an alternate route) • Injected patient bathroom (use alternate) • Video tracking of pt • Work related phone or “break” near injected patients (move the phone) • Wait for tracer to decay Distance • The “Newton’s Inverse Square Law” • The intensity of radiation is inversely proportional to the square of the distance from the source. Intensity = 1/d2 Distance • The intensity of radiation becomes weaker as it spreads out from the source since the same amount of radiation is spread over a larger area. • Example: Heat from a fireplace Shielding • Depending on the type of ionizing radiation, use appropriate shielding • alpha radiation: No shielding, poor penetration, high energy – major concern: internal contamination by ingestion, absorption or inhalation Polonium 210 Alpha Radiation Precautions • Apply basic lab safety: NO eating, drinking, smoking, or applying makeup in the radiopharmacy or clinic. Shielding • Alpha radiation precautions: • Personal Protective Equipment (PPE) – laboratory coat – gloves (esp if skin is not intact) – other Shielding • Beta radiation: • Low Z shielding – plastic, glass • No high Z due to Bremsstrahlung radiation which is highly penetrating Shielding • Gamma radiation, PET tracers: • High Z shielding with the amount dependent on the energy of the radiation & HVL of the shielding material • Generally, 10 HVL needed to achieve background radiation HVL in NM • Radioisotope • 99mTc • 131I • 133 Xe • 111 In • 137 Cs • 201Tl • 125 I keV 140 364 81 245 662 70 35.5 HVL Pb (cm) ~0.02 ~0.30 ~0.03 ~0.10 ~0.65 ~0.03 ~0.01 HVL in NM • Radioisotope • 99mTc • 131I • 133 Xe • 111 In • 137 Cs • 201Tl • 125 I keV 140 364 81 245 662 70 35.5 HVL Pb (cm) ~0.02 ~0.30 ~0.03 ~0.10 ~0.65 ~0.03 ~0.01 Shielding • J Nucl Med Tech (03/2011) Sonmez et al (Turkey): • Conclusion: 2 mm lead shield dec NMT dose by ½ for common proced. - TCO4 thyroid, bone, cardiac MIBI & thallium, DMSA - highest dose: MIBI cardiac FDG shielded shipping box and syringe shield. Weight: 70 # Courtesy of J Thomas FDG syringe shield and pig Courtesy of J Thomas Radiopharmacy Wheeled cart with FDG in syringe shield enroute to dosing room. Courtesy of J Thomas Occupational Radiation Exposure • Primary exposures for NM technologist: – radiopharmaceutical preparation – injecting patients – radioactive patients Occupational Radiation Exposure • Primary exposures for NM technologist: – radiopharmaceutical preparation – injecting patients – radioactive patients Occupational Radiation Exposure Issues • Devise strategies to reduce workrelated exposure. • What tasks expose the NMT to the highest radiation dose? Work-related Tasks 1. Radiopharmaceutical preparation/administration 2. Patient transfers to & from the imaging room; on & off the imaging table 3. Patient imaging to include “set up” 4. Therapeutic procedures 5. PET studies Question • How can one minimize exposure during those tasks with the highest radiation dose? • ALARA principle & monitoring Badges: Monitor WorkRelated Dose 1. Who needs to be badged? 2. Where are the badges worn? Badge requirements • Anybody who is likely to receive > 10% of occupational dose limits • Any minor or pregnant female likely to receive >100 mrem • Where are badges worn? Courtesy of F Mettler Badge requirements • TLD or other device usually placed on upper torso Courtesy of F Mettler • 2002 Lundberg (Australia) “Measuring & Minimizing the Radiation Dose to the NMT”* • Looked at rationale for anterior torso badging. Is it reliable to quantify dose? • Assumption: uniform beam, incident from front J Nucl Med Technol 2002;30:25-30. • 3 dosimeters on a NMT X 3 months: front collar, front waist, back waist • Recorded dose q 30 min (0730-1800) • Task recorded in journal; alternated injecting RP & scanning; weekly • Limitations: one NMT data J Nucl Med Technol 2002;30:25-30. Results • Uniform beam confirmed: anterior collar & waist readings similar • Except: injection of tracers, collar 70% higher than waist (position of NMT torso for RP injection) • Collar readings – more conservative J Nucl Med Technol 2002;30:25-30. Results • 1/3 of the time, back > front waist readings: likely when NMT back to pt in imaging room or from other source • Average doses: • inject: 2 µSv/h/12 µSv/d/3.2 mSv/y • scan: 0.2-2 µSv/h/5.4 µSv/d/1.4 mSv/y J Nucl Med Technol 2002;30:25-30. RP Preparation/Administration • Routine handling of RP • Activity adds to NM dose, esp fingers • Monitor hand exposure with ring dosimeters: - dominant hand, base of ring finger Badge requirements • Ring dosimeter Film should be facing usually palm on 4thof hand finger (dominant hand) Courtesy of F Mettler Hand Exposures • 2008 Wrzesien et al (Poland) “Hand Exposure to Ionizing Radiation of NM Workers” • Measured RP finger doses with TLDs • Reference: 4th ring finger TLD; 5 X lower than thumb, index or middle fingers (RP higher doses than NMT) • 4th finger TLD may underestimate dose Hand Exposures • 2005 Guillet et al (France) “Technologist Radiation Exposure in Routine Clinical Practice with 18F-FDG PET.” • FDG > dose but concept important • Finger dose: 50% dec exposure with monodose c/w multidose vials • Data also supported: semiautomatic FDG injector & pt video tracking Guillet et al J Nucl Med Tschol. 2005 Sep;33(3):175-9. Syringe Shields Syringe Shields • Important to significantly reduce hand exposure in preparing & injecting RP • Disadvantage: cumbersome • Hand dose reduction depends on the RP & shield material, but is generally 75 to > 90% • Tungsten, leaded glass, lead Patient Transfers • 2004 Smart et al (Australia) “Task Specific Monitoring of NMT’s Radiation Exposure” • Constant monitoring of NMT q 32 sec (0830-1700) dose rate in µSv/hr • Pocket dosimeter at anterior waist • Procedure journal w/ start & stop times of individual tasks Activities with the Highest Dose* 1. Transferring incapacitated pt from imaging table to hospital gurney 2. Difficult injections w/o syringe shields 3. Setting pt up for cardiac gated studies * Smart et al Rad Protection Dosimetry Vol 109, No 3, Oxford Univ Press, 2004. Average Doses • Post MDP transfer: 0.54 µSv (40% of total dose 1.3 µSv) • Injecting 24 mCi HDP + tungsten syringe shield: 0.57 µSv (difficult pt: 1.6 µSv) • Setting up pt for gated MIBI: – 1.1 µSv – with 0.5 mm Pb apron: 0.6 µSv – dec by factor of 2 * Smart et al Rad Protection Dosimetry Vol 109, No 3, Oxford Univ Press, 2004. Recommended 1. While waiting for pt transfer, NMT stands away (distance) 2. Use tungsten shield (shielding) 3. Use of a 0.5 mm Pb apron for high activities of Tc99m (shielding) * Smart et al Rad Protection Dosimetry Vol 109, No 3, Oxford Univ Press, 2004. Question # 4 • Which NM technologist task is generally associated with the highest work-related dose? • • • • A. Radiopharmaceutical preparation B. Radiopharmaceutical injection C. Patient scanning D. Patient transfers Question # 4 • Which NM technologist task is generally associated with the highest work-related dose? • • • • A. Radiopharmaceutical preparation B. Radiopharmaceutical injection C. Patient scanning D. Patient transfers In the final stretch…. ….so stand up & stretch! Patient Imaging • Injected pt is a significant radiation source • NM imaging times are extended • Rec: depending on pt condition & imaging protocol, NMT need not remain in room • Time & Distance tenets (ALARA) • Average 0.3-3 mrem/procedure to NMT of which 50-90% can come from imaging* * Mettler Scanning Doses: Many Variables • RP • Administered activity • Amount of pt contact, dec with pt requiring no or limited assistance • Back doses: 30% of front doses • Procedure type Variability with Procedure Type • Highest: • MUGA > stress MIBI & Bone scans • Lowest: • Thyroid, thallium cardiac • Post I31I WBS low with “distance” Higher Dose Procedures • MUGA/cardiac: – high administered activities – pt contact during “set up” time • Bone scans: – potentially high dose with inc pt contact – limited contact once pt is on the imaging table Question # 5 • Which NM procedure is generally associated with the highest NM technologist occupational dose? • • • • A. Bone SPECT B. MUGA C. 131I post therapy scan D. Stress Tc99m MIBI Question # 5 • Which NM procedure is generally associated with the highest NM technologist occupational dose? • A. Bone SPECT • B. MUGA FDG vs General NM Exposure • • • • 2 yr prospective study PET/NM (quarterly): 771 & 524 µSv Estimated PET proced dose: 4.1 µSv FDG IV (w/o & w/ 1° shield): 2.5→1.4 µSv • Trolley-mounted 2° shield: 3.6→1.9 µSv *Roberts FO et al “Radiation Dose to PET Technologists & Strategies to Lower Occupational Exposure.” J Nucl Med Technol.2005 Mar;33(1):44-7 PET NMT Task & Scheduling* • PET/CT: 8-10 studies/day • 2 technologists: weekly rotation of FDG injection and scanning to include pt transfers • Q 3 month rotation (preferably per yr) * Teaching site in San Antonio, Texas PET NMT Tasks • Injection: – Time: < 30 sec (IV running before) explain procedure to pt before inject FDG & answer questions – Distance: close to pt & FDG – Shielding: PET syringe shield in a shielded carrier in shielded room PET NMT Tasks • Scanning/Pt transfer: – Time: 1-2 min (pt w/o assistance); scanner is in adjacent room; brief re-explanation, pt on & off table, position pt – Distance: close – Shielding: Pb glass in scanner control room 2009 NMT Ring (mrem) Body 1st A B A B A B A B 2nd 3rd 4th 136 669 425 483 629 92 254 2407 110 126 141 111 250 78 115 262 NMT PET exposures • • • • 2009 (quarterly rotation of 2 NMT) Ring dose >> body dose (factor 2-4) Ring: 636/483 mrem (2 outliers) Body: 149/142 mrem • 2010 (2 quarters) • Ring dose twice body dose • Ring 151 mrem; Body 78 mrem NMT PET exposures • • • • 2009 (quarterly rotation of 2 NMT) Ring dose >> body dose (factor 2-4) Ring: 636/483 mrem (2 outliers) Body: 149/142 mrem • 2010 (2 quarters); NMT education! • Ring dose twice body dose • Ring 151 mrem; Body 78 mrem Summary • Inc medical imaging using ionizing radiation, CT, NM, VIR (1980) • Concern for latent effects of radiation (CA induction, genetic effects): medical, epidemiological, economic Summary • Inc NM procedures, inc occupational exposure (NMT) • NRC limits & ALARA, can help reduce & minimize work-related exposure • Strict adherence: time, distance, shielding • Monitoring: wear badges