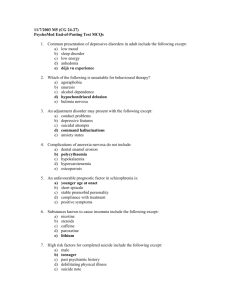
5. General overview of the management of schizophrenia and
advertisement

5. General overview of the management of schizophrenia and incipient psychotic disorder In order to establish the general guidelines for the management of schizophrenia and incipient psychotic disorder, diagnosis and the pertinent assessment are firstly considered. Secondly, the general aspects of psychiatric management and its components, such as the therapeutic alliance, monitoring, care provision and selection of the scope of treatment, are developed. 5.1. Diagnosis and assessment 5.1.1. Diagnosis An initial, complete diagnostic study should be performed on every patient, including: • Psychiatric and general medical history. • Psychosocial history and family psychiatric history. • Examination of the mental state. • Physical assessment that includes a neurological examination. • The necessary complementary examinations to rule out disorders that resemble an incipient psychotic disorder or a schizophrenic disorder, determine the presence of associated disorders, establish baseline characteristics for the administration of antipsychotic drugs and guide habitual medical care if necessary should be performed. Patients who abuse alcohol or other drugs or who present alcohol- or drug-induced psychosis should receive specific treatment. The risk of inflicting injury on oneself or on others and the presence of hallucinations issuing orders should be assessed and proper precautions taken whenever the safety of the patient or others is uncertain .47 In order to diagnose mental disorders in our setting, the Diagnostic and Statistical Manual of Mental Disorders, DSM-IV-TR, and the tenth revision of the International Classification of Diseases’ (ICD-10) Classification of Mental and Behavioural Disorders are employed. DSM-IV-TR Classification criteria for schizophrenia The DSM-IV-TR classification establishes the following criteria:67 CLINICAL PRACTICE GUIDELINES FOR SCHIZOPHENIA AND INCIPIENT PSYCHOTIC DISORDER 38 Criterion A. Characteristic symptoms: two (or more) of the followinga, each present for a significant portion of time during a 1-month period (or less if successfully treated): 1) delusions; 2) hallucinations; 3) disorganized speech, incoherence; 4) catatonic or grossly disorganized behaviour; 5) negative symptoms, for example, affective flattening, alogia o avolition. Criterion B. Social/occupational dysfunction: For a significant portion of the time since the onset of the disturbance, one or more major areas of functioning such as work, interpersonal relations, or self-care are markedly below the level achieved prior to the onset (or when the onset is in childhood or adolescence, failure to achieve expected level of interpersonal, academic, or occupational achievement). Criterion C. Duration: Continuous signs of the disturbance persist for at least 6 months. This 6-month period must include at least 1 month of symptoms (or less if successfully treated) that meet Criterion A and may include periods of prodromal or residual symptoms. During these prodromal or residual periods, the signs of the disturbance may be manifested by only negative symptoms or two or more symptoms listed in Criterion A present in an attenuated form (e.g., odd beliefs, unusual perceptual experiences). Criterion D. Schizoaffective and mood disorder exclusion: Schizoaffective Disorder and Mood Disorder with Psychotic Features have been ruled out because either: a. No major depressive, manic, or mixed episodes have occurred concurrently with the active-phase symptoms, or b. If mood episodes have occurred during active-phase symptoms, their total duration has been brief relative to the duration of the active and residual periods. Criterion E. Substance/general medical condition exclusion: The disorder is not due to the direct physiological effects of a substance (e.g., a drug of abuse, a medication) or a general medical condition. Criterion F. Relationship to a pervasive developmental disorder: If there is a history of autistic disorder or another Pervasive Developmental Disorder, the additional diagnosis of Schizophrenia is made only if prominent delusions or hallucinations are also present for at least a month (or less if successfully treated). • Classification of longitudinal course according to the DSM-IV-TR: determined by whether the course is continuous or episodic and by the presence of psychotic symptoms. a Only one symptom from Criterion A is required if delusions are strange, consist of a voice that continuously comments on the individual’s thoughts or behavior, or if two or more voices talk to each other. CLINICAL PRACTICE GUIDELINES FOR SCHIZOPHENIA AND INCIPIENT PSYCHOTIC DISORDER 39 • − Episodic With Interepisode Residual Symptoms (episodes are defined by the reemergence of prominent psychotic symptoms); also specify if: With Prominent Negative Symptoms. − Episodic With No Interepisode Residual Symptoms. − Continuous (prominent psychotic symptoms are present throughout the period of observation); also specify if: With Prominent Negative Symptoms. − Single Episode In Partial Remission; also specify if: With Prominent Negative Symptoms. − Single Episode In Full Remission. − Other or Unspecified Pattern. − Less than one year since the onset of the first active-phase symptoms. Schizophrenia subtypes according to the DSM-IV-TR: defined according to the type of presentation seen during the most recent episode and can be therefore modified over time. − Paranoid type, in which preoccupation with delusions or auditive hallucinations are a prominent characteristic. − Disorganized type, in which disorganized speech and behaviour and flattened or inappropriate affect are prominent. − Catatonic type, in which characteristic motor symptoms stand out. − Undifferentiated type, which is an unspecific category, used when symptoms are present but are not sufficiently formed or specific enough to classify in the other subtypes. − Residual type, in which there are no positive symptoms but there are other remaining signs of disturbance (for example, negative symptoms or attenuated positive symptoms). Although the prognosis and therapeutic implications of these subtypes are variable, the disorganized type tends to present the most impairment and the paranoid type the least.47 ICD-10 Schizophrenia classification criteria The ICD-10, like the DSM-IV-TR, indicates that there are no patagnomonic symptoms, but certain associated psychopathological phenomena that are especially significant for the diagnosis of schizophrenia. These phenomena are:68 1) Thought echo, thought insertion or withdrawal, and thought broadcasting. CLINICAL PRACTICE GUIDELINES FOR SCHIZOPHENIA AND INCIPIENT PSYCHOTIC DISORDER 40 2) Delusions of control, influence, or passivity, clearly referred to body or limb movements or specific thoughts, actions, or sensations; delusional perception. 3) persistent delusions of other kinds that are culturally inappropriate and completely impossible, such as religious or political identity, or superhuman powers and abilities (e.g. being able to control the weather, or being in communication with aliens from another world). 4) Persistent hallucinations in any modality, when accompanied either by fleeting or halfformed delusions without clear affective content, or by persistent over-valued ideas, or when occurring every day for weeks or months on end. 5) Breaks or interpolations in the train of thought, resulting in incoherence or irrelevant speech, or neologisms. 6) Catatonic behaviour, such as restlessness, posturing, or waxy flexibility, negativism, mutism, and stupor. 7) "Negative" symptoms such as marked apathy, paucity of speech, and blunting or incongruity of emotional responses, usually resulting in social withdrawal and lowering of social performance; it must be clear that these are not due to depression or to neuroleptic medication. 8) A significant and consistent change in the overall quality of some aspects of personal behaviour, manifest as loss of interest, aimlessness, idleness, a self-absorbed attitude, and social withdrawal. • ICD-10 Diagnostic guidelines: The normal requirement for a diagnosis of schizophrenia is that a minimum of one very clear symptom (and usually two or more if less clear-cut) belonging to any one of the groups listed as (1) to (5) above, or symptoms from at least two of the groups referred to as (5) to (8), should have been clearly present for most of the time during a period of 1 month or more. Conditions meeting such symptomatic requirements but of duration less than 1 month (whether treated or not) should be diagnosed in the first instance as acute schizophrenia-like psychotic disorder and are classified as schizophrenia if the symptoms persist for longer periods. The first symptom on the list above is only applied to simple schizophrenia and requires a minimum of one year duration. • ICD-10 Course classification: continuous; episodic with progressive defect; episodic with stable deficit; episodic with complete remissions; incomplete remission; other; course uncertain, period of observation too short. • ICD-10 Course subtypes: paranoid schizophrenia, hebephrenic schizophrenia, catatonic schizophrenia, undifferentiated schizophrenia, postschizophrenic depression, residual schizophrenia, simple schizophrenia, other schizophrenia, and unspecified schizophrenia. CLINICAL PRACTICE GUIDELINES FOR SCHIZOPHENIA AND INCIPIENT PSYCHOTIC DISORDER 41 Classification and grouping of psychotic symptoms In addition to the classifications described, symptoms are also frequently classified and group into three categories: positive symptoms (delusions and hallucinations), negative symptoms (affective flattening, alogia, avolition/apathy and attention difficulties) and “disorganization” symptoms (which include disorganized speech, thought disorder, disorganized behaviour and attention deficit). Positive symptoms are the most relevant features in the acute phases of these disorders, whereas negative symptoms and cognitive impairment are the deterministic symptoms in social and occupational dysfunction. Negative symptoms and cognitive impairment are extremely important, clinically speaking and in terms of rehabilitation, given that they affect the patient’s ability to work, relationships with others and emotional ties; that is, the patient’s capacity to develop a life in normal circumstances. 5.1.2. Differential diagnosis The following aspects of the differential diagnosis are considered:28,69 Differential diagnosis for schizophrenia should be performed to distinguish it from other psychic, organic and/or toxic clinical pictures. In terms of psychic clinical pictures, it should be distinguished from schizoaffective disorder; mood disorder with psychotic features; schizophreniform disorder; brief psychotic disorder; delusional disorder; pervasive developmental disorder; schizotypal, schizoid or paranoid personality disorders; borderline personality disorder; dissociative hysterical psychosis, and puerperal psychoses. Differential diagnosis relating to organic medical conditions should be carried out with brain tumours (frontal, temporal); temporal lobe disease; epilepsy; viral encephalopathy-encephalitis; brain abscesses; postencephalitis; thyrotoxicosis; acute intermittent porphyria; and psychotic disorder due to delirium or dementia. Finally, as far as substance abuse clinical pictures, the following should be taken into account: chronic consumption of cannabis, amphetamines, LSD, digital, steroids, alcoholic hallucinosis, and others. 5.1.3. Clinical condition and continued assessment It is important to assess, at the very least, these four critical circumstances: risk of inflicting injuries on self or on others; access to means to carry out suicidal or homicidal objectives; presence of hallucinations that issue orders; and self-care abilities.47 5.1.4. Comorbidity with other mental disorders The symptoms of other mental disorders, especially depression, but also obsessive and compulsive symptoms, somatic preoccupations, dissociative symptoms and other anxiety or mood symptoms, can be present in schizophrenia. Whether they are symptoms or disorders CLINICAL PRACTICE GUIDELINES FOR SCHIZOPHENIA AND INCIPIENT PSYCHOTIC DISORDER 42 associated with this disease, these manifestations can significantly worsen prognosis and often require specific care and therapeutic planning. 5.1.5. Comorbidity with substance- and alcohol-use related disorders The use and dependency of alcohol and other substances should be assessed. Together with general medical conditions, the most frequently associated disorder seems to be substance use, especially the consumption of alcohol and stimulants, such as cocaine and amphetamines; other frequently used substances are nicotine, cannabis, phencyclidine and LSD.47 5.1.6. Comorbidity with other diseases and past medical history The general state, along with cardiac function, medications and other treatments the patient is receiving, should be assessed. The most frequent concomitant clinical pictures and risk factors that should be assessed and treated are: obesity, HIV risk behaviours, tobacco smoking and hypertension.4 Based on the specific circumstances of each case, the assessment of medical complications or substance use, diabetes and cardiovascular problems should be considered. If necessary, the general practitioner should be consulted. In a patient who presents a first crisis, laboratory tests should be requested: basic analyses to perform the differential diagnosis with other disorders that may appear to be schizophrenia, analyses to rule out the presence of toxic substances, general biochemistry, complete haemogram and urine analysis.28 Depending on the circumstances of each patient, the following complementary tests should also be considered: pregnancy test, electrocardiogram, computerized tomography or magnetic resonance imaging, neuropsychological studies and general psychometry. 5.1.7. Psychiatric history It is important to assess at least four of these circumstances: prior episodes, danger to the patient or other people, response to prior treatments and prior use of substances. 5.1.8. Psychosocial history and family psychiatric history Based on expert consensus, it is important to record the frequency and quality of the social relationships maintained by the patient throughout his/her life, as well as the current significant relationships. The assessment of family structure and relationship patterns is important to establish a therapeutic plan. It is essential to assess the factors related with social and family relationships that may represent elements of stress or vulnerability, as well as those which may serve as protection factors.70 CLINICAL PRACTICE GUIDELINES FOR SCHIZOPHENIA AND INCIPIENT PSYCHOTIC DISORDER 43 Information on premorbid function should also be retrieved, including employment history, the highest occupational and/or educational level attained, occupational functioning, significant relationships in the work place, and specific difficulties. 5.1.9. Annual general check-ups According to McEvoy and collaborators, the following recommendations apply to all patients: medical history and physical exploration that includes size and weight, blood pressure and complete hemogram.28 Based on the circumstances of each patient, the following tests and examinations are recommended: general biochemistry, electrocardiogram, dental check-up, pelvic examination/Pap smear, rule out the presence of toxic substances, tuberculin test, lipid profile, mammography, prostate specific antigen and blood test to rule out hepatitis and detect HIV. Coordination with the primary care physician during examinations is important given that his/her role is key in the detection and quick referral of relapses, as well as in the follow-up of the general health state. 5.2. Psychiatric management 5.2.1. General overview In the development of a treatment plan for a patient with schizophrenia or incipient psychotic disorder cross-sectional issues, such as the current clinical condition, and longitudinal issues, such as clinical course and frequency, severity, treatment and consequences of previous episodes, should be taken into account. Whenever possible, patient and family should be involved in the treatment plan in active collaboration by means of an integrated approach of appropriate pharmacological and psychosocial interventions. The general objectives are the improvement of the clinical course, as well as the reduction of the frequency, severity and psychosocial consequences of the episodes. A further aim will be to optimize psychosocial functioning between episodes. Specific objectives will depend on the phase of the disorder and the patient’s specific characteristics. 5.2.2. Components of psychiatric management Treatment of the patient with schizophrenia or incipient psychotic disorder is facilitated by overall knowledge of the patient, which includes the assessment of his/her objective and subjective needs; objectives; intrapsychic conflicts and defences; coping styles; personal capacities; and biological, interpersonal, social and cultural factors which affect the patient’s adaptation. CLINICAL PRACTICE GUIDELINES FOR SCHIZOPHENIA AND INCIPIENT PSYCHOTIC DISORDER 44 Professionals who are involved in the care of the patient must work to develop an integrated and coordinated treatment plan given that they several professionals and services frequently take part in care, both simultaneously and successively. The main elements that comprise the therapeutic plan are related with its influence on the evolution of the disease and treatment efficacy. It also includes issues that are present in the treatment of all psychiatric diseases.4 • Symptom assessment and establishment of a diagnosis For treatment to be effective and appropriate, precise and pertinent diagnostic and clinical evaluations should be performed. In the case of schizophrenia, diagnosis has significant consequences on the short and long term planning of treatment. • Development of a treatment plan Once the diagnosis and clinical and psychosocial circumstances of the patient have been assessed, a treatment plan should be formulated and applied. This process entails the selection of therapeutic modalities, the type of treatment or specific treatments and their context. Depending on the severity of the clinical situation and due to the fact that sometimes the information on the patient’s history and the clinical assessment are progressively obtained, it is possible that the process may have to be repeated and modified for as long as the patient-physician relationship lasts. • Establishment of the therapeutic alliance and stimulation of treatment compliance It is essential for the psychiatrist who treats the patient to establish and maintain a supportive therapeutic alliance, from which treatment will be carried out. This alliance provides very important information to the psychiatrist and increases the patient’s trust and desire to collaborate with treatment. • Education and therapy for the patient and family Working with patients so that they learn to recognize early symptoms of relapse prevents a complete exacerbation of the disease. Informing the family on disease characteristics and providing them with strategies to cope with the disease can reduce relapses and significantly increase the patient’s quality of life. • Treatment of comorbid diseases There are several psychiatric, social and medical disorders that are much more frequent in people with schizophrenia than in the general population. The therapeutic team should assess this disease periodically. Some frequent comorbidities, such as major depression, substance-induced disorders and post-traumatic stress disorder, can often be detected by performing clinical examinations and talking to the patient and close friends and family, as well as by carrying out longitudinal observation of the patient’s behavioural patterns. • Social circumstances and functioning of the patient The patient’s social circumstances and functioning can greatly influence treatment compliance and the response to treatment. Living conditions, the family’s participation, the source and amount of income, the legal situation and relationships with close people can be CLINICAL PRACTICE GUIDELINES FOR SCHIZOPHENIA AND INCIPIENT PSYCHOTIC DISORDER 45 both stressful and protective situations. Hence, they are aspects that psychiatry professionals could explore periodically. • Integration of treatments administered by different physicians Many patients with schizophrenia receive several treatments that are often administered by different physicians. This situation could potentially lead to the fragmentation of therapeutic efforts for those patients who normally have difficulties planning and organizing. • Treatment documentation Most people with schizophrenia are treated by many different physicians over the course of their disease. This is a result of changes in the treatment setting (hospital, out-hospital settings, assertive community treatment, etc.), the availability of programs, their place of residence and health care staff. Given that in order to plan treatment it is essential to have detailed knowledge of the patient’s treatment history and the treatments that he/she is currently receiving, it is crucial to maintain good documentation. A A therapeutic alliance enables the psychiatrist to acquire essential information regarding the patient and enables the patient to gain trust in the psychiatrist and the desire to cooperate in treatment. The identification of the patient’s objectives and aspirations and relating them with results promotes treatment adherence, together with the therapeutic relationship. 4 5.3. Development of the therapeutic plan 5.3.1. Design of the therapeutic plan Firstly, and if possible, the short-, mid- and long-term objectives of the therapeutic plan should be established. Secondly, the type of treatment or intervention to be carried out should be taken into account with the participation of the patient and his/her family. The different alternatives of pharmacological treatment (antipsychotics and other coadjuvant drugs) and psychosocial interventions (psychological and relating to psychosocial rehabilitation) are then described. Thirdly, the setting where treatment will be applied will be determined based on the clinical state, the phase of the disorder and the treatment chosen. In order to reach treatment objectives, it is recommended to assess positive and negative symptomatology, depression, suicidal ideation and behaviour, substance abuse, medical comorbidities, post-traumatic stress disorder and an array of potential community adjustment problems, including being homeless, isolation, unemployment, victimization and involvement in the criminal justice system.4 CLINICAL PRACTICE GUIDELINES FOR SCHIZOPHENIA AND INCIPIENT PSYCHOTIC DISORDER 46 5.3.2. Choosing the treatment setting Patients should be seen in the least restrictive setting possible, where safety is ensured and an effective treatment can be applied. In this sense, patients with schizophrenia should be seen in several settings. The selection of the setting for treatment should be based on the patient’s clinical situation, his/her preferences and those of his/her family, the demands of the treatment plan and the characteristics of available treatment settings. Different settings differ in terms of the availability of different therapeutic possibilities, degree of support, limitation of and protection from harmful behaviour, working hours, capacity to manage psychotic or severely agitated patients, and general setting and philosophy of treatment.47 • Factors to consider when choosing the intervention setting Some of the criteria that should be taken into account when choosing the most appropriate intervention setting at each moment are: The patient’s psychopathological state Risk of aggression to self or others Need for hospitalization Intervention modality or required interventions Autonomy and capacity for self-care Family support Access to support and social resources in the community Patient and family preferences CLINICAL PRACTICE GUIDELINES FOR SCHIZOPHENIA AND INCIPIENT PSYCHOTIC DISORDER 47