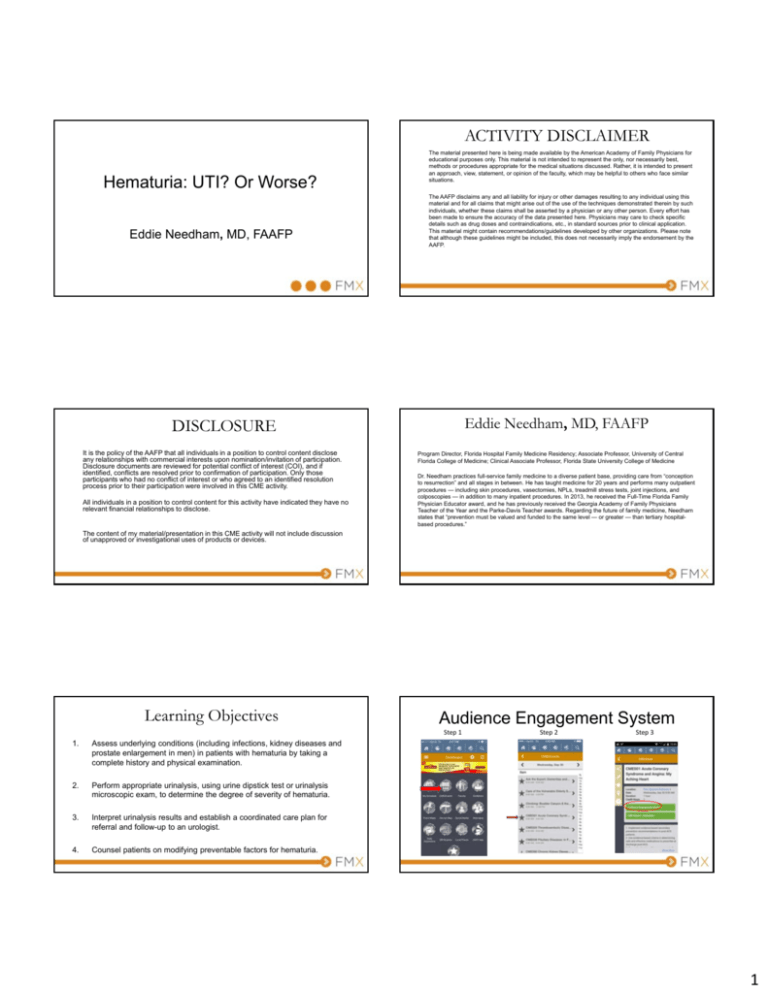
ACTIVITY DISCLAIMER
Hematuria: UTI? Or Worse?
Eddie Needham, MD, FAAFP
The material presented here is being made available by the American Academy of Family Physicians for
educational purposes only. This material is not intended to represent the only, nor necessarily best,
methods or procedures appropriate for the medical situations discussed. Rather, it is intended to present
an approach, view, statement, or opinion of the faculty, which may be helpful to others who face similar
situations.
The AAFP disclaims any and all liability for injury or other damages resulting to any individual using this
material and for all claims that might arise out of the use of the techniques demonstrated therein by such
individuals, whether these claims shall be asserted by a physician or any other person. Every effort has
been made to ensure the accuracy of the data presented here. Physicians may care to check specific
details such as drug doses and contraindications, etc., in standard sources prior to clinical application.
This material might contain recommendations/guidelines developed by other organizations. Please note
that although these guidelines might be included, this does not necessarily imply the endorsement by the
AAFP.
Eddie Needham, MD, FAAFP
DISCLOSURE
It is the policy of the AAFP that all individuals in a position to control content disclose
any relationships with commercial interests upon nomination/invitation of participation.
Disclosure documents are reviewed for potential conflict of interest (COI), and if
identified, conflicts are resolved prior to confirmation of participation. Only those
participants who had no conflict of interest or who agreed to an identified resolution
process prior to their participation were involved in this CME activity.
All individuals in a position to control content for this activity have indicated they have no
relevant financial relationships to disclose.
Program Director, Florida Hospital Family Medicine Residency; Associate Professor, University of Central
Florida College of Medicine; Clinical Associate Professor, Florida State University College of Medicine
Dr. Needham practices full-service family medicine to a diverse patient base, providing care from “conception
to resurrection” and all stages in between. He has taught medicine for 20 years and performs many outpatient
procedures — including skin procedures, vasectomies, NPLs, treadmill stress tests, joint injections, and
colposcopies — in addition to many inpatient procedures. In 2013, he received the Full-Time Florida Family
Physician Educator award, and he has previously received the Georgia Academy of Family Physicians
Teacher of the Year and the Parke-Davis Teacher awards. Regarding the future of family medicine, Needham
states that “prevention must be valued and funded to the same level — or greater — than tertiary hospitalbased procedures.”
The content of my material/presentation in this CME activity will not include discussion
of unapproved or investigational uses of products or devices.
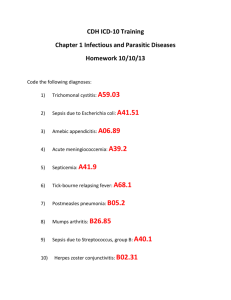
Learning Objectives
Audience Engagement System
Step 1
1.
Assess underlying conditions (including infections, kidney diseases and
prostate enlargement in men) in patients with hematuria by taking a
complete history and physical examination.
2.
Perform appropriate urinalysis, using urine dipstick test or urinalysis
microscopic exam, to determine the degree of severity of hematuria.
3.
Interpret urinalysis results and establish a coordinated care plan for
referral and follow-up to an urologist.
4.
Counsel patients on modifying preventable factors for hematuria.
Step 2
Step 3
1
Hematuria Evaluation
• Mr. Jones is a 57 year old male who presents for follow up of
hypertension of ten years duration.
• He is asymptomatic.
• His blood pressure is 145/87.
• His creatinine is 1.1.
• His urinalysis shows 2+ blood, no protein, and 7-10 red blood
cells (RBCs)/high power field (HPF) on microscopic exam.
• What should the family physician do next?
Polling Question
• 57 yo male with asymptomatic microhematuria.
What is the best initial action the family
physician can perform?
A.
B.
C.
D.
Refer to nephrology
Order an intravenous pyelogram (IVP)
Order an abdominal helical CT w/ and w/o contrast
Order an ultrasound of the kidneys
AAFP ASA 2010 Responses
AAFP ASA 2012 Responses
AAFP ASA 2013 Responses
Hematuria Introduction
• Up to 9-18% of otherwise healthy individuals have some degree
of hematuria.
• Hematuria can serve as a marker for infection, stone disease, or
cancer.
• Most frequently, the cause of hematuria is not found.
• Hematuria may be transient, occurring on a single instance in
39% of soldiers over 12 years, and occurring in 16% on more
than one instance over the same period.1
1Froom P, Ribak J, Benbassat J. Significance of microhaematuria
in young adults. Br Med J (Clin Res Ed) 1984;288:20‐2.
2
Hematuria Definition
• According to the American Urological Association, hematuria is
defined as 3 or more RBCs/HPF on urine microscopy on two of
three urinalyses.
• Other references have used 5 or more RBCs/HPF as abnormal.
• It is important to partner with local laboratory resources to
determine local standards.
Grossfeld GD, Litwin MS, Wolf JS, Hricak H, Shuler CL, Agerter DC, et al. Evaluation of asymptomatic microscopic hematuria in adults: the American Urological Association best practice policy—part I: definition, detection, prevalence, and etiology. Urology. 2001;57:599–603.
AUA Risk Factors for Significant Disease in Patients With
Microscopic Hematuria
• Smoking history
• History of chronic urinary
tract infection
• Occupational exposure to
chemicals or dyes (e.g.,
• Analgesic abuse
benzenes, aromatic amines)
• History of pelvic irradiation
• Age older than 35 years
• History of exposure to known
• Male gender
carcinogen
• History of urologic disorder or • History of chronic indwelling
disease
foreign body
• History of irritative voiding
symptoms
Davis R, Jones S, Barocas D, et al, Diagnosis, Evaluation and Follow‐up of Asymptomatic Microhematuria (AMH) in adults: AUA guideline, Published online at http://www.auanet.org/common/pdf/education/clinical‐guidance/Asymptomatic‐
Microhematuria.pdf, May 2012
Hematuria - severity
• “Macroscopic hematuria” describes urine that is visibly stained
red or brown. This is also called gross hematuria.
• > 50 RBCs/HPF is defined as “severe hematuria.”
• “Microscopic hematuria” describes urine that is not tinged red or
brown eye but dips positive for blood.
• Additionally, microscopic hematuria will have ≥ 3 RBCs/HPF on
urine microscopy.
Signs and Symptoms associated with
hematuria
• Symptoms of cystitis
include:
–
–
–
–
Dysuria
Suprapubic pain
Urgency
Frequency
• Dysuria can be present in
prostatitis and urethritis
Gross hematuria
Urine visibly stained
red or brown
Creative commons license at:
http://en.wikipedia.org/wiki/File:HematuriaTrauma.JPG
Signs and Symptoms associated with
hematuria
• Pain radiating from the flank to the groin can be found in several
conditions:
– Renal colic/ureteral distention from nephrolithiasis (stones)
– Blood clots
– Papillary necrosis
• Costovertebral angle tenderness is common with pyelonephritis,
trauma/hematoma, and bleeding or infection in a renal cyst.
3
Why kidney stones hurt!
Signs and Symptoms associated with
hematuria
• Patient complaints of skin rash …
Scanning Electron Microscopy of the surface of a calcium oxalate kidney stone
Creative commons license at: http://en.wikipedia.org/wiki/File:Surface_of_a_kidney_stone.jpg
Signs and Symptoms associated with
hematuria
• A bride recently back from her honeymoon in
Jamaica…
• Honeymoon cystitis
• Systemic Lupus Erythematosus (SLE)
Signs and Symptoms associated with hematuria
• Patient complains of skin rash, achy joints, and occasional abdominal pain…
• Henoch Schonlein Purpura (HSP)
Creative commons licenses at: http://en.wikipedia.org/wiki/File:Purpura.jpg
http://en.wikipedia.org/wiki/File:Henoch‐Sch%C3%B6nlein_nephritis_IgA_immunostaining.jpg
http://dermis.net/dermisroot/en/24695/image.htm
Signs and Symptoms associated with hematuria
Signs and Symptoms associated with
hematuria
• Sixteen year old female had a
sore throat last week and now has a rash…
• Sixty-five year old male with decreased appetite and
weight loss …
• Scarlet fever with post‐streptococcal glomerulonephritis
• Renal Cell Cancer
Creative commons licenses at: http://en.wikipedia.org/wiki/File:Scarlet_fever_2.jpg
http://en.wikipedia.org/wiki/File:Scharlach.JPG
4
Signs and Symptoms associated with
hematuria
• Family history of renal failure and cerebral
aneurysms:
– Polycystic Kidney Disease (PKD)
Creative commons license at: http://en.wikipedia.org/wiki/File:Adpkd.jpg
Characteristics of hematuria in localizing
etiology
• Glomerular/renal bleeding will be consistent throughout the urine
stream.
• Hematuria or clots at the beginning of the urinary stream are
suggestive of a urethral cause.
• Terminal hematuria or clots suggest a bladder, trigonal, or
prostatic source.
Creative commons license at:
Hematuria. Emerg Med Clin North Am. 19: 2001; 621‐632.
http://en.wikipedia.org/wiki/File:Polycystic_kidneys,_gross_pathology_20G0027_lores.jpg
Polling question
• What percentage of time will a patient with
gross hematuria have bladder or kidney
cancer?
A.
B.
C.
D.
3-5%
5-10%
10-20%
20-25%
Etiologies of gross hematuria
Etiology
Cancer
Urolithiasis
Urinary tract infection
Congenital anomaly
Hypercalcemia
Renal disease
Idiopathic
Children, n = 228
1 (0.4%)
2 (0.8%)
1 (0.4%)
5 (2.2%)
51 (22.4%)
77 (33.8%)
86 (37.7%)
Adults, n = 1200
270 (22.5%)
130 (10.8%)
394 (32.8%)
NA
NA
NA
101 (8.4%)
Tu, W. H. & Shortliffe, L. D. (2010) Evaluation of asymptomatic, atraumatic hematuria in children and adults, Nat. Rev. Urol. doi:10.1038/nrurol.2010.27
5
Outcomes of Evaluation for Visible
Hematuria (gross hematuria)
• 1804 pts with median age 67 with visible
hematuria underwent evaluation:
– Upper track imaging, urine cytology, cystoscopy
• Pts with initial negative work up with persistent
hematuria more than 1 year later were reevaluated.
Mishriki SF et al. Half of visible and half of recurrent visible hematuria cases have underlying pathology: Prospective large cohort study with long‐term follow up. J Urol 2012 May;187:1561.
Outcomes of Evaluation for Visible
Hematuria
• Outcomes:
– Bladder cancer 18%
– Large bleeding prostate
13%
– Renal or ureteral calculi
6%
– Infections 2%
– Renal cancer 2%
– Bladder stones 2%
– Urethral strictures 2%
– No cause identified 53%
• 69 patients with recurrent
hematuria:
– 8 bladder or renal cancers
(12%)
• 0.45% of original cohort
– 34 patients (49%) still with
negative workup
Mishriki SF et al. Half of visible and half of recurrent visible hematuria cases have underlying pathology: Prospective large cohort study with long‐term follow up. J Urol 2012 May;187:1561.
Etiologies of microscopic hematuria
Etiology
Cancer
Urolithiasis
Urinary tract infection
Congenital anomaly
Hypercalcemia
Renal disease
Idiopathic
Children, n = 342
0 (0%)
1 (0.4%)
0 (0%)
5 (1.5%)
56 (16.4%)
10 (2.9%)
274 (80.1%)
Adults, n = 1689
86 (5.1%)
84 (5.0%)
73 (4.3%)
NA
NA
37 (2.2%)
717 (43.0%)
Any brief questions?
Tu, W. H. & Shortliffe, L. D. (2010) Evaluation of asymptomatic, atraumatic hematuria in children and adults, Nat. Rev. Urol. doi:10.1038/nrurol.2010.27
Hematuria - Diagnosis
• Many patients are diagnosed while
asymptomatic with a urine dipstick done for
other reasons (E.g., HTN, DM care).
• The urinalysis with microscopy is the best initial
test to evaluate for hematuria before
proceeding to any imaging studies.
General comments about the urinalysis
• Urine microscopy should be performed on all samples positive
for blood and those that are negative but have a high index of
suspicion.
• Samples should be evaluated within one hour as casts begin to
disintegrate and RBCs lyse.
• Placing the specimen in the refrigerator may preserve the
sample for a few more hours.
6
Microscopy and localization
Microscopy and localization
• Dysmorphic cells in combination with proteinuria and RBC casts
are suggestive of glomerular disease.
• RBCs from a nonglomerular source resemble a
peripheral blood smear.
National Institutes of Health
Creative commons licenses at: http://en.wikipedia.org/wiki/File:MicroHematuria.JPG
Hematuria - Diagnosis
Dipstick results for hematuria
• The dipstick test for blood detects the peroxidase activity of
erythrocytes.
• This reaction results in a green color change that is visible on the
dipstick.
• The sensitivity of the dipstick to detect hematuria at a
concentration of more than 3 RBCs/HPF is 91-100%. 1,2
• The specificity is 65-99%. 2
1
Hematuria. Emerg Med Clin North Am. 19: 2001; 621‐632.
Woolhandler S, Pels RJ, Bor DH, et al. Dipstick urinalysis screening of asymptomatic adults for urinary tract disorders. I. Hematuria and proteinuria. JAMA. 1989;262:1214–9.
2
Urinalysis Results
False Positive
False Negative
•
•
•
•
•
•
•
•
•
Hemoglobinuria
Myoglobinuria
Dehydration
Exercise
Menstrual blood
Elevated specific gravity
pH<5.1
Proteinuria
Vitamin C
Substances that may cause red pigmenturia
Endogenous Sources
Foods
Drugs
Bilirubin
Myoglobin
Hemoglobin
Porphyrins
Rhubarb
Blackberries
Blueberries
Paprika
Rifampin
Nitrofurantoin
Sulfonamides
Metronidazole
Beets
Phenytoin
Fava beans
Artificial food
colorings
Prochlorperazine
Phenolphthalein
Quinine
Chloroquine
Phenazopyridine
Creative commons licenses at:
http://en.wikipedia.org/wiki/File:Beets.jpg
http://en.wikipedia.org/wiki/File:Pyridiumurine.jpg
Levodopa
Methyldopa
Adriamycin
Desferoxamine
Sokolosky MC: Hematuria. Emerg Med Clin North Am 2001;19:621‐632.
7
Common Nonglomerular Renal Causes of
Hematuria
Glomerular Causes of Hematuria
Alport’s syndrome
Fabry’s disease
Goodpasture’s syndrome
Hemolytic uremia
Henoch‐Schönlein purpura
Immunoglobulin A nephropathy
Lupus nephritis
Membranoproliferative glomerulonephritis
Mesangial proliferative glomerulonephritis
Nail‐patella syndrome
Other postinfectious glomerulonephritis: endocarditis, viral
Poststreptococcal glomerulonephritis
Thin basement membrane nephropathy
(benign familial hematuria)
Wegener’s granulomatosis
Consult Nephrology
Extrarenal Causes of Hematuria
•
•
•
•
•
Benign prostatic hyperplasia
Calculi
Coagulopathy
Infection – prostate, bladder, urethra
Inflammation – drugs, radiation
– Cyclophosphamide
• Trauma
• Tumor
Causes of benign transient hematuria
• Vigorous exercise
– March hematuria in the military
– Runner’s hematuria
• Trauma to urethra
– Insertion of foley catheter
• Menstruation
• Medication
• Sexual intercourse
• Digital rectal exam
• If the patient’s history
suggests one of these
causes, repeat the
urinalysis in 48 hours.
• If the hematuria has
resolved, no further
workup is necessary in a
low risk patient.
•
•
•
•
•
•
•
Acute tubular necrosis
Polycystic kidney disease
Infection – pyelonephritis, tuberculosis
Interstitial nephritis – drug, connective tissue disease
Renal cell cancer
Vascular malformations
Sickle cell disease
Needham’s Mnemonic
• “HITS”
• Hematologic disturbances
– Sickle cell disease, hemophilia
• Infection, Infarction, Inflammation
– UTI, pyelonephritis, ATN, papillary necrosis, AIN,
glomerulonephritis
• Trauma, Tumor, TB
• Stones, “Systs,” “S/Cyclophosphamide”/meds
Hematuria - Evaluation
• Historically, patients with suspected upper tract cause of
hematuria were evaluated with an intravenous pyelogram (IVP).
• Emergency Departments currently use helical CT in most
instances.
• Ultrasound is another diagnostic modality used to evaluate
hematuria.
• Urine cystoscopy studies the lower urinary tract.
Cohen RA, Brown RS. Clinical practice. Microscopic hematuria. N Engl J Med 2003;348:2330‐8.
8
Plain films often helpful
Intravenous Pyelography
• Benefits
– Visualizes the urinary tract from the kidneys to the bladder
– Relatively low cost
– Widely available
• Disadvantages
–
–
–
–
Less sensitive for smaller lesions
Not as useful for evaluating the bladder or urethra
Exposure to contrast media
A follow up CT is often recommended to further delineate IVP findings
Reproduced with permission from Medical Management of Common Urinary Calculi, July 1, 2006, Vol 74, No 1, issue of American Family Physician Copyright © 2006 American Academy of Family Physicians. All Rights Reserved.
IVP demonstrating mass in renal pelvis
Intravenous Pyelography
• Gray Sears et al found that IVP identified 85% of lesions > 3
cm in diameter.
• However, IVP only identified 21-52% of smaller lesions.
Reproduced with permission from Assessment of Microscopic Hematuria in Adults, May 15, 2006, Vol 73, No 10, issue of American Family Physician Copyright © 2006 American Academy of Family Physicians. All Rights Reserved."
Computed Tomography
• Benefits
– Unenhanced renal CT has excellent sensitivity in diagnosing calculi in
patients with renal colic.
• Sensitivity = 97%, specificity = 96%1
– Evaluates surrounding structures to aid in the diagnosis
– Fast and frequently available in 2015
– Less radiation than IVP
– Contrast CT can identify smaller lesions, abnormal vessels, and
abscesses
– CT is frequently used as the follow up study for abnormal IVP and/or
ultrasound.
1Diagnostic procedures for the urogenital
Gray Sears CL, Ward JF, Sears ST, Puckett MF, Kane CJ, Amling CL. Prospective comparison of computerized tomography and excretory urography in the initial evaluation of asymptomatic microhematuria. J Urol 2002;168:2457‐60.
Computed Tomography
• Disadvantages
– Dye load can cause acute kidney insufficiency
– Cost
system. Emerg Med Clin North Am. 19: 2001; 745‐761
9
Ureteral Stone
Kidney Stone
Reproduced with permission from Medical Management of Common Urinary Calculi, July 1, 2006, Vol 74, No 1, issue of American Family Physician Copyright © 2006 American Academy of Family Physicians. All Rights Reserved.
Creative commons license at: http://en.wikipedia.org/wiki/File:3mmstone.png
Kidney Mass/Tumor
Renal ultrasonography
• Benefits
– Least expensive
– No exposure to ionizing radiation or contrast media
– Can be used during pregnancy
• Disadvantage
– Not as accurate in lesions < 3cm in size1
– Sensitivity at detecting renal calculi = 64-96%, significantly less than CT2
1Jamis‐Dow CA, Choyke PL, Jennings SB, Linehan WM, Thakore KN, Walther MM. Small (< or = 3‐cm) renal masses: detection with CT versus US and pathologic correlation. Radiology 1996;198:785‐8.
2Jaffe JS, Ginsberg PC, Gill R, Harkaway RC. A new diagnostic algorithm for the evaluation of microscopic hematuria. Urology 2001;57:889‐94.
Reproduced with permission from Assessment of Microscopic Hematuria in Adults, May 15, 2006, Vol 73, No 10, issue of American Family Physician Copyright © 2006 American Academy of Family Physicians. All Rights Reserved."
Polycystic Kidney Disease
Hematuria – lower tract assessment
• Urine Cytology
– No longer recommended for routine assessment of
asymptomatic microhematuria
• Cystoscopy
– Insertion of cystoscope through urethra into bladder for
direct visualization.
1Cohen RA, Brown RS. Clinical practice. Microscopic hematuria. N Engl
J Med 2003;348:2330‐8.
Creative commons license at: http://commons.wikimedia.org/wiki/File:PKD_cat.jpg
10
Urine cytology … is out
Cystoscopy
• In July 2012, the American Urologic Association released
an updated guideline for asymptomatic microscopic
hematuria (AMH).
• The AUA recommends cystoscopy in all patients greater than
35 with hematuria and in higher risk patients who may be
younger1
• The sensitivity of cystoscopy for detecting bladder cancer is
87%2
– In this guideline, urine cytology is no longer routinely
recommended for any steps in the work up of AMH. “The use of
urine cytology and urine markers (NMP22, BTA-stat, and UroVysion
FISH) is no longer recommended as a part of the routine evaluation
of the asymptomatic microhematuria patient. “
Grossfeld GD, Litwin MS, Wolf JS, Hricak H, Shuler CL, Agerter DC, et al. Evaluation of asymptomatic microscopic hematuria in adults: the American Urological Association best practice policy—part I: definition, detection, prevalence, and etiology. Urology. 2001;57:599–603.
1Davis R, Jones S, Barocas
D, et al, Diagnosis, Evaluation and Follow‐up of Asymptomatic Microhematuria (AMH) in adults: AUA guideline, Published online at http://www.auanet.org/common/pdf/education/clinical‐guidance/Asymptomatic‐
Microhematuria.pdf, May 2012
2Cohen RA, Brown RS. Clinical practice. Microscopic hematuria. N Engl
J Med 2003; 348:2330‐8.
Cystoscopy
• Benefits
– Only reliable method for detecting transitional cell cancer
of the bladder and urethra.
• Disadvantages
– Patient discomfort
– Limited ability to detect carcinoma in situ in the bladder
Davis R, Jones S, Barocas D, et al, Diagnosis, Evaluation and Follow‐up of Asymptomatic Microhematuria (AMH) in adults: AUA guideline, Published online at http://www.auanet.org/common/pdf/education/clinical‐guidance/Asymptomatic‐Microhematuria.pdf, May 2012
11
Follow up of asymptomatic microscopic
hematuria
Preventable factors for hematuria
• Stop smoking
• Avoid occupational exposures
– Dyes, benzenes, aromatic amines
• Decrease analgesic/high risk medication use if possible
• If a patient with a history of persistent asymptomatic
microhematuria has two consecutive negative annual urinalyses
(one per year for two years from the time of initial evaluation or
beyond), then no further urinalyses for the purpose of evaluation
of AMH are necessary. Expert Opinion
• For persistent asymptomatic microhematuria after negative
urologic work up, yearly urinalyses should be conducted.
Recommendation (Evidence Strength Grade C)
• For persistent or recurrent asymptomatic microhematuria after
initial negative urologic work-up, repeat evaluation within three to
five years should be considered. Expert Opinion
Davis R, Jones S, Barocas D, et al, Diagnosis, Evaluation and Follow‐up of Asymptomatic Microhematuria (AMH) in adults: AUA guideline, Published online at http://www.auanet.org/common/pdf/education/clinical‐guidance/Asymptomatic‐
Microhematuria.pdf, May 2012
Risk of urologic malignancy in hematuria
• May be present in up to 10% of patients with microscopic
hematuria
• May be present in up to 25% of patients with macroscopic
hematuria
• 12.1% overall prevalence of malignant disease among patients
with hematuria in a cohort of 4020 patients with hematuria
Negative initial complete evaluation for hematuria associated with low risk
of developing bladder or other urologic cancer in men ≥ 50 years old
•
•
•
•
•
Edwards TJ, Dickinson AJ, Natale S, Gosling J, McGrath JS. A prospective analysis of the diagnostic yield resulting from the attendance of 4020 patients at a protocol‐driven haematuria clinic. BJU Int. 2006 Feb; 97(2):301‐5
Subsequent urologic cancer unlikely following negative initial evaluation
in patients with asymptomatic dipstick hematuria
•
•
•
•
•
•
Prospective cohort study
292 consecutive patients evaluated in tertiary urologic care for asymptomatic dipstick
hematuria were followed for 13 years
16 patients (5.4%) had urologic malignancy on initial evaluation
21 patients (7%) were lost to follow-up
42 patients died of unrelated causes
Among 213 remaining patients followed for 13 years
– 180 (84.5%) had subsequent negative urinalysis, of whom none had urologic
malignancy
– 33 (15.5%) had persistent dipstick hematuria, of whom 1 had new bladder tumor
Prospective cohort study
258 men ≥ 50 years old with asymptomatic microhematuria detected on bladder
cancer home urine screening were followed for 14 years
Any man with ≥ 1 positive test had complete evaluation including
– lab tests
– urine cytology
– IV urography or computed tomography
– cystoscopy
Among 234 men with no evidence of bladder or other urologic cancer following initial
complete evaluation, 2 developed bladder cancer during follow-up period, 6.7 and 11.4
years after negative initial evaluation
0.93% of men originally screened who tested negative for hematuria went on to
develop bladder cancer
Madeb R, Golijanin D, Knopf J, et al. Long‐term outcome of patients with a negative work‐up for asymptomatic microhematuria. Urology, 2010. Jan;75(1):20‐5
Recommendations for screening for bladder
cancer
• United States Preventive Services Task Force (USPSTF) recommends
neither for nor against routine screening for bladder cancer in adults (grade I
recommendation)
• American Cancer Society has no specific guidelines on screening for
bladder cancer
• Canadian Task Force on the Periodic Health Examination recommends
against routine screening of asymptomatic patients for hematuria to detect
urologic malignancies
Mishriki SF, Nabi G, Cohen NP. Diagnosis of urologic malignancies in patients with asymptomatic dipstick hematuria: prospective study with 13 years' follow‐up. Urology. 2008 Jan; 71(1): 13‐6
12
Summary
• When evaluating a patient with hematuria, common things are
common:
– Urinary tract infection
– Renal and ureteral stones
– Benign prostatic hyperplasia
– Urologic cancer
• Urine cytology is no longer indicated for initial evaluation.
• Nephrology refer should be considered in patients with a glomerular
source of bleeding
Practice Recommendations
• Choose helical CT to evaluate the upper urinary
tract in all patients who can tolerate the
procedure.
– SORT B, ref on slide 51
• Evaluate the lower urinary tract with cystoscopy.
– SORT C, ref on slide 60
• A patient with an initial negative evaluation has a
low likelihood of subsequent urologic cancer.
– SORT B, refs on slides 68 and 69
HITS Mnemonic
• Hematologic disturbances
– Sickle cell disease, hemophilia
• Infection, Infarction, Inflammation
– UTI, pyelonephritis, ATN, papillary necrosis, AIN,
glomerulonephritis
• Trauma, Tumor, TB
• Stones, “Systs,” “S/Cyclophosphamide”/meds
Thank you for your time and attention
Eddie.Needham.MD@FLHosp.org
Office phone: 407 646 7757
13