Blood Lab First Week
advertisement

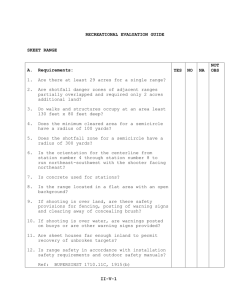
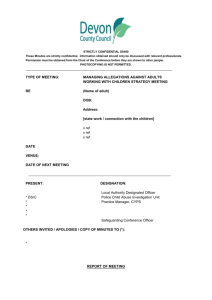
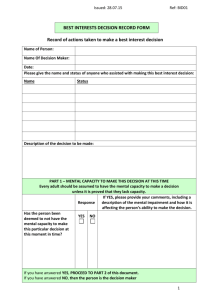
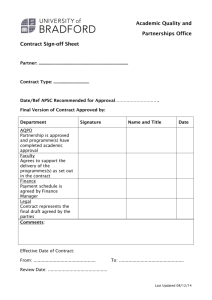
Blood Lab First Week This is a self propelled powerpoint study atlas of blood cells encountered in examination of the peripheral blood smear. It is a requirement of this course that you begin review of these slides with the first day of class in order to familiarize yourself with terms used in describing peripheral blood morphology. Laboratory final exam questions are derived directly from these slides. The content of these slides may duplicate slides (1-37) listed on the Hematopathology Website. You must familiarize yourself with both sets of slides in order to have the best learning opportunity. Before Beginning This Slide Review • Please read the Laboratory information PDF under Laboratory Resources file to learn about – Preparation of a blood smear – How to select an area of the blood smear for review of morphology and how to perform a white blood cell differential – Platelet estimation – RBC morphology descriptors • • • • Anisocytosis Poikilocytosis Hypochromia Polychromatophilia Normal blood smear. Red blood cells display normal orange pink cytoplasm with central pallor 1/3-1/2 the diameter of the red cell. There is mild variation in size (anisocytosis) but no real variation in shape (poikilocytosis). To the left is a lymphocyte. To the right is a typical neutrophil with the usual 3 segmentations of Med. Utah pathology the nucleus. Normal blood: thin area Ref 2 Normal peripheral blood smear. This field is good for exam of cell morphology, although there are a few minor areas of overlap of red cells. Note that most cells are well dispersed and the normal red blood cell central pallor is noted throughout the smear. Thick area of smear: Red cells are artifactually stacked on one another and do not uniformly show normal central pallor. White blood cells appear rolled up and nucleus can not always be distinguished from cytoplasm. This is not a good area to review of morphology Ref 2 Lymphocyte Tail edge, or feathered edge of smear. Not a good area to review red cell morphology. However, some large cells such as blasts may roll to the edge of the smear during preparation and may be more readily found there on visual scanning of the smear. Ref 2 Feathered edge or tail edge of smear. Again-this is not a good area to review for morphology. It is an area to scan for larger cells such as myeloblasts or more immature myeloid and lymphoid cells which are not normally found in the peripheral blood. Above are mainly lymphocytes and neutrophils Ref 2 Neutrophil Maturation Series Note, neutrophils are the most predominant white blood cell form in the peripheral blood smear. Occasional metamyelocytes and myelocytes may be seen but their presence in peripheral blood usually indicates infection, inflammation or a primary bone marrow process. The presence of progranulocytes or blast forms in the peripheral blood always indicates a serious disease process is present. nucleoli Myeloblast Faint red granules Normal Myeloblast: Note the large slightly ovoid nucleus which is eccentrically placed with a rim of blue cytoplasm. A small number of red granules are sometimes seen. The nucleus finely granular and stippled. There are generally 2-5 clear nucleoli that can be seen. Ref 1 lmphocyte Basophilic normoblast myeloblast Normal Myeloblast. Several basophilic normoblasts are also in this field. Note that their nuclei are much more condensed than the myeloblast and their nuclei are smaller. Compare the mature small lymphocyte which also has a U VA pathology more condensed nucleus and no nucleoli. Clumped platelets Promyelocyte. 12-25 µm; round or oval cell. Cytoplasm is more abundant than in the myeloblast. Note the red- purple primary granules indicating this cell is of the myeloid lineage. Also note the very large size of this cell and that its nucleus is greater than twice the diameter of the red blood cell. Also present are open nucleoli, also indicative of the immature stage of development of this myeloid precursor. Early chromatin clumping is noted in the nucleus. Ref 1 ashimagebank-2005-101356 Myelocyte: Nucleus occupies around 50% of cell area. Cytoplasm is smooth light blue-gray. Both azure primary granules and small number of specific granules are present. Neutrophilic granules are beyond resolution of light microscope and appear as lighter pinkish to tannish area often adjacent to nucleus (arrow). Ref U VA pathology Metamyelocyte. Nucleus: an indented oval, resembling kidney or bean; clumped chromatin; nucleoli absent Cytoplasm is completely filled with specific neutrophilic color (pink) granules. A few primary (azure) granules may be present Ref 2 Myeloid band form. 10-l5 µm. The nuclear chromatin has completely indented to form a C shape. Bands may also be occasionally coiled. Note the pink/purple granules dispersed throughout the cytoplasm, characteristic of the granulocytic lineage. The band is differentiated from a metamyelocyte by its thinner, longer nucleus with parallel sides and from the segmented form by having no filamentous indentation between nuclear lobes Ref 1 Myeloid band forms. Note that one band form is beginning the process of nuclear segmentation Ref 1 ashimagebank2005-101349 . Platelets Segmented neutrophil on right. Band form on left. Note the well dispersed fine pink to purple granules in the cytoplasm characteristic of the granulocytic series. 2 to 5 nuclear lobes are connected by fine filament Ref 1 Barr body Normal neutrophil. In normal females 2-3% of neutrophils have an appendage of condensed chromatin called a Barr body Ref 1 Large lymph Small lymphocyte Small lymphocytes have very dense, clumped chromatin in an ovoid or notched nucleus. Occasional larger lymphocytes may also be found in the peripheral blood. Ref 1 Atypical lymphocytes. These cells have very scant granules, if any, and abundant cytoplasm that is often draped around neighboring red blood cells on the smear. The nucleus is dense with the appearance of having been colored with a wide crayon. The nuceloli are not large and open as would be seen in a lymphoblast. These cells are characteristically seen in viral infections, particularly infectious mononucleosis. Ref 1 Atypical lymphocytes in infectious mononucleosis, also known as Downey cells Ref: U VA Pathology Monocyte: 12-20µm Often horse shoe, kidney or clover shaped nucleus that is lacey and less dense than a lymphocyte. Cytoplasm is usually abundant, pale gray-blue. A few coarse azure granules may be present; tiny azure dust-like granules may be present. May have cytoplasmic vacuoles which are seen as clear, colorless vacuoles in the Wright Giemsa stain. U VA Pathology Monocyte with vacuoles present. U VA pathology ashimagebank2005-101369 Compare: Upper panel meta myelocyte. Lower panel is a monocyte. Note the fine azurophilic granules in the cytoplasm of the metamyelocyte and the denser nucleus. The monocyte has more clear grey blue cytoplasm and a more lacey nucleus Mature Eosinophil: 2 to 3 nuclear lobes, bright orange/pink cytoplasm due to large, acidophilic granules. Ref 1 Mature basophil: 2 to 3 nuclear lobes, dark blue-purple cytoplasm due to large basophilic granules. These granules are rich in serotonin, histamine, and leukotrienes Med Utah Pathology Eosinophil Lymphocyte Abnormalities in Neutrophils Unrelated to Malignancy • Hypersegmentation • Pelger Huet anomaly • Leukemoid reaction Hypersegmented Neutrophil (Poly)- A neutrophil is considered hyersegmented if it has greater than or equal to 5 lobes. Characteristic of megaloblastic anemia, e.g. B12 or folate deficiency. University of Utah Pathology Ref 1 Leukemoid reaction. A response in the peripheral white blood count in which the white blood count has increased beyond 30,000 or when there is a pronounced shift to immaturity, usually in response to infection. Note toxic granulations and vacuolization in neutrophils. Note presence of myelocyte indicating release of young cells under conditions of stress into the peripheral blood. Rarely a promyleocyte will be seen. The finding of blasts in the peripheral blood is always worrisome for leukemia or a bone marrow process. Upper right hypersegmented granulocyte (poly) and small lymphoctye lower left. Also note that the red blood cells in this smear are macrocytic with some cells approaching the size of the nucleus of the small lymphocyte. Ref 1 Pelger Huet anomaly (bilobed nucleus) seen in the nucleus of these mature granulocytes. A benign inherited dominant disorder of nuclear segmentation. Pseudo-pelger cells are seen as an acquired phenomenon with leukemia or myelodysplasia Ref 1 Dohle body: aggregates of rough endoplasmic reticulum seen with infection. They are a faint bluish accumulation of material seen in the periphery of the granulocyte. Ref 1 Dohle body Ref 1 Platelets Platelet on top of red blood cell Normal platelets-note that normal platelets have redpurple granules present Lichtman’s Atlas of Hematology Large granular lymphocyte Agranular platelet Normal platelet Abnormalities in platelets Large platelet or macrothrombocyte Ref 2 Grey platelets, as in Grey Platelet Syndrome: Note decreased granules and larger than normal size platelets seen in this congenital disorder of platelet function and number Ref 2 Giant platelet Normal platelets Giant platelet. Note size compared to red blood cell and more normal platelets Ref 1 ashimagebank2004-101140 Red Blood Cell Morphology • Anisocytosis • Poikilocytosis • Red blood cell morphology changes due to changes in hemoglobin content • Characteristic red blood cell shape changes • Red blood cell inclusions Poikilocytosis: variation in shape-pencil forms, fragmented cell and tear drop noted Hypochromia: central pallor is greater than 1/3 diameter of red blood cell Ref 1 Marked (4+) Poikilocytosis: variation in shape of red blood cells Williams Hematology, 7th ed, 2006 Polychromatophilia or polychromasia: a bluish color of RBCs suggesting reticulocytosis, the presence of many young RBCs. Often seen in hemolytic anemias and acute sudden blood loss and are a sign of a normally functioning bone marrow Ref 1 ashimagebank2004-101122 Reticulocytes: Reticulocytes are suspected in the peripheral blood smear by the presence of polychromatophilia in the red blood cells. A special Ref 1 stain methylene blue or brilliant cresyl blue is required to identify them ashimagebank2005-101299 Orthochromatic normoblast Leukoerythroblastic blood smear: Note many immature red blood cell precursors normally found in marrow. This could be as a result of a severe hemolysis as seen in hemolytic disease of the newborn Ref 1 Lymphocyte Hypochromic microcytic red blood cells. Note the red blood cells are much smaller in diameter than the small lymphocytes on the smear. The central pallor is greater than 1/3 the red cell diameter. This indicates a disorder of heme synthesis, e.g. iron deficiency Med Utah Pathology Monocyte Lymphocyte Hypochromia: Note increased central pallor of red blood cells, greater than 1/3 the diameter of the red blood cell. Microcytosis: Red blood cell is less than 2/3 the diameter of the small lymphocyte. This picture is consistent with iron deficiency Ref 2 Macrocytes. Unfortunately there is no lymphocyte to compare size with in this view. Also note the poikilocytosis (variation in shape) with tear drop forms, microspherocytes and ovalocytes present. Anisocytosis is also evident on this smear with varying size of cells. Elliptocytes: a disorder of red blood cell membrane Ref 1 ashimagebank2004-101268 Spherocytes noted at arrows. Note the cells have loss of central pallor. This is not due to viewing a poorly dispersed section of the smear as many red blood cells demonstrate normal central pallor. A spherocyte represents the minimal amount of red blood cell membrane that can incorporate the contents of the cell. This is seen autoimmune hemolysis and in hereditary spherocytosis Ref 1 ashimagebank-2001-100214 Spherocytosis: The uniformity of the spherocytes in this smear is consistent with hereditary spherocytosis. In HS the deficiency is usually of ankyrin which destabilizes the red cell membrane so that it fragments, thus losing surface area and changing from a discocyte to a spherocyte. Williams Hematology, 7th edition, 2006 Target Cells Target cells. Target red blood cells occur when there is an excess of red blood cell membrane compared to hemoglobin content. Target cells are seen in thalassemia where there is a decrease in hemoglobin synthesis and liver disease in which there is an excess of membrane synthesized. Ref 1 Basophilic stippling: pathologic precipitation of ribosomes. This is a sign of disordered heme synthesis in erythrocytes. One example is lead intoxication. Nucleated red blood cell. Howell Jolly bodies present (arrows). The presence of nucleated red blood cells always indicates a disease process present such as early release of the RBCs from the marrow due to brisk hemolytic anemia or to a bone marrow process pushing early RBC forms out of the marrow prematurely for example. Howell Jolly bodies indicate absence of spleen. Tear drop cells: these stretched and deformed cells are seen in thalassemia and myelophthisic and myelofibrotic disorders Ref 3 Schistocytes: Fragmented red blood cells. In this case from mechanical valve hemolysis Ref Williams Hematology 7th ed 2006 Schistocytes: Note the variably misshapen red blood cells with randomly torn circumference. In this case the underlying disorder was disseminated intravascular coagulation Ref Williams Hematology 7th edition 2006 Hemoglobin C disease: target cells and a “box car” cell showing condensed hemoglobin Nucleated red blood cell Sickle Cells: Ref Williams Hematology 7th ed, 2006 Basophilic stippling: pathologic precipitation of ribosomes. This is a sign of disordered heme synthesis in erythrocytes. One example of a cause is lead intoxication. Ref 3 Rouleaux formation: stacking of red blood cells as a result of protein coating. Seen in hypergammaglobulinemic states Ref 1 Red blood cell agglutination as seen in cold agglutinins disease where agglutinating RBC antibodies (often IgM antibodies) bind to RBCs and cause agglutination Ref 1 lymphocytes Chronic lymphocytic leukemia. Numerous smudge cells noted by arrows. Smudge cellno cytoplasm present and nucleus appears to be disintegrating Leukemic blasts, in this case lymphoblasts, as recognized by scant blue cytoplasm surrounding the nucleus with no granules noted. Open nuceoli are present indicating an immature cell. Also note that the nucleus of these blasts are more than twice the diameter of a red blood cell. These features distinguish these cells from normal mature peripheral blood lymphocytes. Additional Good Sources to Review Peripheral Blood Cell Morphology • http://www.meded.virginia.edu/courses/path/innes/nh/morphology.cfm • http://library.med.utah.edu/WebPath/HEMEHTML/HEME IDX.html#2 • http://www.wadsworth.org/chemheme/heme/microscope/ celllist.htm • Williams Hematology Atlas http://online.statref.com.proxy.lib.umich.edu/Document/D ocument.aspx?FxID=167&DocId=1&SessionId=B27731 VURZQOKNVV Slide References • Ref 1- Williams Textbook of Hematology Atlas • Ref 2-ASH slide bank • Ref 3- U Va Pathology ©2007 University of Virginia Charles E. Hess, M.D. Lindsey Krstic, B.A. • Ref 4- University of Utah Pathology http://library.med.utah.edu/WebPath/HEMEHTML/HEMEIDX.html#2 • Ref 5http://images.google.com/imgres?imgurl=http://www.wadsworth.org/chemheme/heme/ microscope/pix/metamyelocyte_nw.jpg&imgrefurl=http://www.wadsworth.org/chemhe me/heme/microscope/metamyelocyte.htm&h=305&w=400&sz=14&hl=en&start=1&u m=1&tbnid=npegNYdkPtJRM:&tbnh=95&tbnw=124&prev=/images%3Fq%3Dwadsworth%2Bcenter%2B metamyelocyte%26svnum%3D10%26um%3D1%26hl%3Den%26sa%3DG