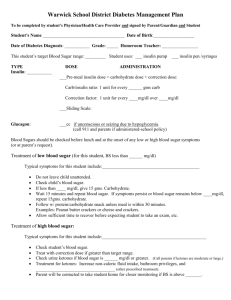
Recognition and Treatment of Hypo/Hyperglycemia
advertisement

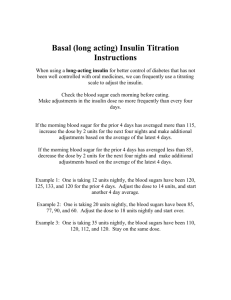
Recognition and Treatment of Hypo/Hyperglycemia (low and high blood sugars) Hypoglycemia Signs/symptoms of hypoglycemia (see additional info sheet): Shaking/trembling (especially look at their hands) Irritable/inexplicable crying Suddenly very hungry Lethargy/blank stares/inability to focus Pale Blurred vision Sweaty/clammy Hypoglycemia treatment: Ages = 5-10 Blood Sugar Check blood sugar if above symptoms are reported or observed. A blood sugar less than 80 is a low blood sugar. If the blood sugar is between 50 and 80, the standard is to give 15 grams of fastacting carbohydrates (carbs). If below 50, the standard is to give 30 grams fastacting carbs. This is a rule of thumb for average-age, average-sized kids. Many of your students will have specific school orders from their endocrinologists that list much more exact treatments for low blood sugars based on age and blood sugar range. If your student has these orders, refer to them for treatment and do not go by the above “rule of thumb.” The following is a commonly used treatment plan: Amount of Carbohydrate 60-80 50-60 40-50 30-40 10 20 30 40 Ages = 11-18 Blood Sugar Amount of Carbohydrate 60-81 50-61 40-51 30-41 15 30 45 60 Fast-acting carbs are any source of carb that is a “quick sugar.” These are items which are absorbed quickly through the stomach lining. Anything that contains fat or fiber is NOT a fast-acting carb (ie. chocolate, apples, peanut butter, etc). Examples of fast-acting carbs are: juice, regular soda, Smarties, Sweet Tarts, sugar packets or cubes, raisins, glucose tablets – anything that is all sugar, easily chewed and swallowed, and does NOT contain fat. Recheck blood sugar 15 minutes after student is treated with fast-acting carb. Repeat this treatment cycle until student’s blood sugar is >80. If child is not eating within the next hour, then they need eat a fat/fibercontaining snack to prevent the low blood sugar from recurring. Examples of these include cheese and crackers, peanut butter and crackers, milk (not skim), ice cream, lunch meat, etc. Follow the directions on the school orders or instructions from the family to determine whether or not you should give the student insulin for these snacks. If child is very low and unable to swallow, use glucose gel or cake gel and massage into cheek/gums while massaging throat to encourage swallowing. If unconscious or combative, use glucagon. This is an intramuscular shot to the child’s thigh, and can be given through their clothes (subcutaneous shots work more slowly). o Under age 6: 0.3 mL o Ages 6-18: 0.5 mL o Age 18 and above or for large teens: 1 mL Roll child on side after delivery and expect vomiting. Give carb-containing fluids after awake, and then at least a 30 gram protein/fiber containing snack when able to tolerate fluids. If no response, repeat dose if there is any left, and call 911. Hyperglycemia Signs/symptoms of hyperglycemia (see additional info sheet): Nausea/loss of appetite/vomiting Headache Blurred vision Irritable/inexplicable crying Fatigue/inability to concentrate You may notice that many of the signs of low blood sugars are similar to those of high blood sugar. If your student does not appear well or states that he/she “doesn’t feel right,” do a blood sugar check. Hyperglycemia treatment: Check blood sugar if above signs and symptoms are reported or observed. If blood sugar is over 300 for those students on insulin injections or over 250 for those students on insulin pumps, check urine ketones. If ketones are not present, have child drink lots of water and exercise if possible. If ketones are present in any amount, have child drink lots of water and rest (no exercise). Call the parent if ketones are present as insulin is the only way to eliminate ketones. If child is severely ill, call 911. May correct a pre-meal blood sugar if child has school orders to do so – follow the directions given on the school orders using the child’s correction factor. Child will need to have unlimited bathroom privileges and ability to drink water at desk if blood sugar is high. Child will feel sick with high blood sugar, especially if ketones are present, and will have difficulty concentrating – expect them not to perform well. As the school health care provider, you may have to educate teachers on this (ie the student may need to take a test on a different day, etc). Step-by-Step Guide to Checking Blood Glucose 1. Gather supplies. 2. Instruct student to wash hands with warm water. 3. Load lancet device with new lancet. NEVER reuse lancets – each use dulls the metal, and can leave metal shards in the skin. 4. Load test strip – most monitors turn themselves on when you do this. 5. Hold lancet device to side of fingertip. 6. Activate lancet by pressing button. 7. Turn finger down to get full drop of blood, may milk finger if necessary. Do not add blood to test strip-obtain result from one blood drop only. 8. Hold strip to drop of blood – the strip will absorb the blood by capillary action. 9. Record results (results help the student’s MD obtain patterns of blood sugars and see where changes may be needed with insulin). 10. Remove lancet from lancet device and dispose of properly. TIPS: Controls are done: Each time you open a new bottle of test strips, drop monitor, do not believe results, or if strips are left out in the heat. Different types of batteries are used depending on the meter. Some are AAA, others are watch batteries. The family can provide backups of these. Never share monitor with another student. Alternative sites are a great alternative to finger sticks and are reported to be less painful. However, do not use an alternative site if you think the student’s blood sugar is low. If you get a low blood glucose result, you need to retest on a fingertip. Disposable Pen Instructions: 1. Get Prepared: a. Wash hands. b. Check to see that Humalog/Novolog is clear. If cloudy, do not use. c. Check to see where the rubber stopper is located on the side of the pen (ie. is there enough insulin left to inject?) d. Wipe off rubber seal on the end of the Pen with alcohol. e. Remove the paper tab from the outer Pen needle shield. f. Screw the capped needle clockwise onto the end of the Pen until tight. Remove the inner Pen needle shield and discard into trash. 2. Prime the Pen: a. Lilly Prefilled Pen for Humalog: Turn the dose knob clockwise until the arrow appears in the magnifying dose window. Pull out the dose knob. A “0” will appear in the window. Turn the dose knob clockwise until a “2” appears. a. Novolog FlexPen, Humalog Kwikpen: Turn the dose knob clockwise until you reach the line next to the “2”. b. Remove the cover from the needle and point the Pen up. c. Tap the clear plastic barrel lightly then press the injection button in all the way until you see a drop or small stream of insulin. If no insulin comes out, repeat the priming steps until you do. 3. Dial the dose: a. Lilly Prefilled for Humalog: Turn the dose knob clockwise until the arrow appears in the magnifying dose window. Pull out the dose knob. A “0” will appear. Dial the number of units for the insulin dose. If the dose is dialed too high, turn the knob backward until the correct dose appears b. Novolog FlexPen, Humalog Kwikpen: Set the dose indicator to the appropriate number of units you want to inject. 4. Double check dose with student, if age appropriate, by checking dose window together and checking MD orders. 5. Deliver the dose: a. Place the needle into the subcutaneous tissue at a 90 degree angle (injection sites are: back of arms, abdomen, hips, thighs), and press the injection button down completely. Then, count slowly to 6 (One, one thousand, Two, one thousand, Three, one thousand etc). If all the insulin was given, a diamond or arrow should appear in the Lilly Prefilled Pen window. In the Novolog Flexpen and the Humalog Kwikpen, the dose indicator window should reset to zero. Remember to rotate sites. 6. Store the Pen/Document the Injection: a. Replace the outer needle shield. b. Unscrew the capped needle and dispose per school district sharps policy. c. Place the cap back on the Pen for storage and keep at room temperature (no higher than 86 degrees, and not in fridge). The pen can be used for 1 month at room temperature, provided the insulin doesn’t run out. d. Document injection: dose, time, site, BG reading and whether pre- or post meal. Injections should be done pre-meal in most children, though they are sometimes done post-meal in very young children (preschool, kindergarten) who are unsure what they will eat. NovoPen Jr. Instructions: 1. Introduction – these have a removable cartridge that is replaced and a better mechanism than disposable pens. The NovoPen Jr. is the only available insulin pen that can dose ½ units. Though there is between 0.1-0.2 units of error with the NovoPen Jr., this is far more accurate that even a well-trained nurse can do with a syringe and is therefore much safer for small children and much more accurate for teenagers. 2. If you have dialed too large a dose, follow the following instructions for turning the dose back to zero – this is a different procedure than with the disposable pens! 3. To remove an empty cartridge, you must unscrew the pen halves. After the halves are taken apart, the old cartridge will slide right out of the lower half of the pen. You only take apart a pen when a cartridge is empty, and NEVER replace an empty cartridge with a partially used cartridge, or refill from a vial. 4. To refill pen with a new cartridge, you must first wind the plunger back into the top half of the pen – this is done by manually twisting the plunger counter-clockwise backwards into the top part of the pen device. Once plunger is all the way back into pen device, you may now refill the pen with the new insulin cartridge. 5. After a new cartridge is placed in pen, it must now be primed. The initial priming of a brand new cartridge may take 2-8 units of insulin in 2 unit increments in order to get all the air out. First, you must place a needle onto the pen following the same instructions above used for disposable pens. Then, you turn the pen with the needle pointing up, and begin priming with 2 units of insulin. Repeat until several drops of insulin are seen coming out of the needle. Proceed to injection. 6. A function check of the pen should be performed whenever the pen is dropped or exposed to extreme temperatures, as well as once a month to ensure proper functioning. Please refer to following instructions. Tips Use a new needle with each dose. Prime before each injection or the dose may be inaccurate. Push the injection button all the way in. If the full dose wasn’t given, the magnifying/dose window will reveal the number of units left. Never leave the needle on after using an insulin pen. ALWAYS remove and replace with cap, otherwise insulin will leak out and air bubbles will enter the cartridge. Do not refrigerate insulin pens which are in use. Once a month, perform a function check on the NovoPen Jr. If the function check fails, repeat and if it fails again, do not use the Pen. When giving medications, you must have the drug in its original container and have followed the policies and procedures of the district that governs medication administration by having a written request/authorization from the parent and/or physician.