a09-RESPIRATORY PHYSIOLOGY
advertisement

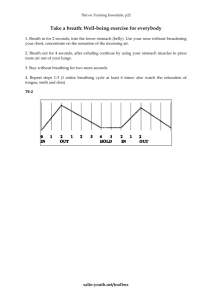
Respiratory Physiology Background Information: When inspiring, the pleura attached to the internal chest wall is pulled outward as the thoracic cavity expands. The pleural cavity [space between the outer (parietal) and inner (visceral) pleural layers] increases slightly in volume, causing a decrease in intrapleural pressure. The decrease in intrapleural pressure, and the surface tension of pleural fluid, cause the visceral pleura, and therefore the lungs, to be pulled outward along with the thoracic cavity. As the lungs increase in volume, the alveolar pressure decreases to below atmospheric pressure, and air enters the lungs. When the thorax decreases in size the lungs recoil, causing intrpleural pressure and alveolar pressure to increase. Air then leaves the lungs during exhalation. One resting breath, including both inspiration and expiration, has a relatively constant volume. The volume of this resting breath is called the tidal volume—the volume of air that is inhaled and exhaled at rest. It is possible, however, to both force additional air out of the lungs, and to inhale deeply (breath in more air volume). The volume of air that can be exhaled with a forced breath is known as the expiratory reserve volume; the volume of a ir that can be inhaled in addition to that inhaled during a normal resting breath is known as the inspiratory reserve volume. The sum of these three volumes—tidal, expiratory reserve and inspiratory reserve—is known as the vital capacity of the lung. Additional capacities, including inspiratory and functional residual capacity, can also be calculated knowing the three volumes above. A diagram of these volumes and capacities, along with some average measurements, is shown below. A spirometer is an instrument used to measure lung volumes and capacities. Of course, in addition to other secondary roles, one of the main functions of the respiratory system is to provide oxygen to and remove wastes from the various organs of the body. Blood flowing through these organs is responsible for transporting oxygen and gaseous wastes produced there (e.g., carbon dioxide). Although fluid, blood is technically considered a connective tissue. Plasma is the non- living matrix in which the living cells are suspended. Generally, of the 5L volume of blood in the average human, 55% is plasma. The remaining 45% is comprised of cells and cell fragments, the combination of which is also known as ‘formed elements’. Although the volume of a resting breath (i.e., tidal volume) is typically around 500ml, we all know that we can breathe more deeply or more shallowly if we desire. And even though ventilation is an autonomic/automatic process, we can also forcibly alter the rate at which we ventilate. When we forcibly alter our automatic breathing activity, we ultimately affect the amount of oxygen and CO 2 our blood is transporting. The level of these two gases is monitored and, when altered to a point that is perceived as dangerous, our brain will step in and override our forced breathing alterations. Although forced alterations change both circulating oxygen and CO 2 concentrations, the monitoring of the latter is more sensitive. Therefore, the brain is more sensitive to elevated CO 2 levels and when these levels increase, respiration rate and/or tidal volume will be increased in response. This autonomic control of our respiration ensures that an adequate supply of oxygen is delivered to our organs and that CO2 wastes do not build up to a level that will cause irreversible damage. The purpose of these exercises is to demonstrate respiratory mechanics, and to familiarize you with the assessment of ventilation, including use of a spirometer for measuring lung volumes and lung capacities. In addition, nervous responses to oxygen and CO2 concentrations and the subsequent induction of changes in respiration rate will also be observed. Finally, the composition of whole blood will be analyzed by performing a hematocrit to assess its capacity to transport gases. Experimental Protocol: Activity A 1.) In this activity, you will use the spirometer function of the BioPac to determine lung volumes and capacities. Since it is not possible to measure residual volume, assume that it is 1L for all subjects. 2.) When you approach the BioPac, it should be running, opened to Lesson 12 (L12-Lung-1), and calibrated. If this is not the case, consult your laboratory instructor who will assist you in setting up the equipment properly. 3.) Obtain a clean mouthpiece. Insert it into the air filter that is already attached to the airflow transducer. Be sure that the filter is attached to the Inlet side of the airflow transducer. 4.) Place a nose clip on your nose, or hold your nose very tightly by pinching it with your fingers. 5.) Wrap your lips tightly around the mouthpiece and begin breathing normally through the airflow transducer as shown in the diagram to the right. Be sure to hold the transducer parallel to the floor. 6.) When prepared, ask your lab partner to select “Record” and to remind you of each of the actions in step 7 below. 7.) When recording has begun, take three normal breaths (each breath = inhale + exhale). Then, inhale as deeply as possible; exhale to normal breathing for three normal breaths. Then exhale as much air as possible. Inhale back to normal breathing for three normal breaths. At the end of this cycle, ask your lab partner to select “Stop”. 8.) The recorded data should look similar to that shown in the diagram below. If the data look very different, ask your lab partner to select “Redo”, and repeat the actions outlined in step 7, making sure to pinch your nose tightly, to wrap your lips tightly around the mouthpiece and to hold the transducer upright. If the recorded data do look similar, have your lab partner select “Done ”, and “Yes” to stop the data recording and proceed to step 9. 9.) Select “Analyze current data file”. 10.) Observe how the channel numbers are designated: CH1—Airflow; CH 2—Volume. 11.) To set up the display for optimal viewing, hide CH 1—Airflow. To do this, hold down the control key while using the cursor to click on the channel box 1 (the small box with a ‘1’ in the upper left of the screen.) 12.) To analyze the data, set up the first pair of channel/measurement boxes at the top of the screen by selecting the flowing channel and measurement type from the drop down menu: 13.) Use the arrow cursor and select on the I-beam cursor box on the lower right side of the screen to activate the “area selection” function. Using the activated –beam cursor, highlight the region containing the first three normal breaths as shown in the figure at the top of the following page. 14.) Observe that the computer automatically calculates the p-p (peak to peak) value for the selected area. His measurement, calculated from the data by the computer, represents the difference between the highest and lowest values within the selected area. For the first three normal breaths, the p-p value represents the tidal volume (L). Record this value in the table below. 15.) Use the I-beam cursor to measure the IRV. Highlight from the peak of maximum inhalation to the peak of the last normal inhalation just before it Observe and record the ∆ value in the chart (to the nearest 1/100 liter). 16.) Use the I-beam cursor to measure the ERV. To do this, highlight from the trough of maximum exhalation to the trough of the last normal exhalation just before it. Observe and record the ∆ value in the chart (to the nearest 1/100 liter). 17.) Finally, use the I-beam cursor to measure the VC. To do this, highlight from the trough of maximum exhalation to the peak of maximum inhalation. Observe and record the p-p value in the chart (to the nearest 1/100 liter). 18.) When finished, select “Record from another subject” to leave the BioPac ready for your lab partner or another classmate. 19.) Using the measured data, calculate the capacities shown in the table at the top of the next page. Pulmonary Measurements Volumes Tidal Volume (TV) Inspiratory reserve volume (IRV) Expiratory reserve volume (ERV) Vital Capacity (VC) Residual volume (RV) Measurement (liters) 1.0 (assumed) Calculated Pulmonary Capacities Capacity Inspiratory capacity (IC) Expiratory capacity (EC) Functional residual capacity (FRC) Total Lung Capacity (TC) Formula = TV + IRV = TV + ERV = ERV + RV = TV + RV + IRV + ERV Calculation (liters) 20.) Calculate your predicted vital capacity using the appropriate formula below (for your gender). How does this predicted value compare to the actual measured value? Be able to explain any discrepancies. Activity B 1.) In this activity, you will directly observe the increase in thoracic volume that is necessary for ventilation. 2.) Obtain a tape measure. 3.) Place the tape measure around your lab partner’s chest as close to his/her armpits as possible in order to measure the thoracic circumference. 4.) As your lab partner breathes quietly, measure the maximum and minimum circumferences (maximum should be during inspiration and minimum during expiration). Record these numbers. 5.) Instruct your lab partner to inhale as deeply as possible. Measure and record the thoracic circumference. 6.) Instruct your lab partner to exhale as deeply as possible. Measure and record the thoracic circumference. 7.) My subtracting the smaller of the two circumferences from the larger measured during inhalation, determine how much your lab partner was able to increase the size of his/her thorax by forcibly breathing. By subtracting the smaller of the two circumferences from the larger during exhalation, determine how much your lab partner was able to decrease the size of his/her thorax by forcibly breathing. 8.) Have your laboratory partner repeat these measurements on you. Activity C 1.) In this activity you will auscultate breathing sounds (listen to them using a stethoscope). There are two sounds that can be heard as air enters and exits the lungs. The bronchial sounds are heard during inspiration and expiration, and are the sounds of air moving through the large respiratory passages. Vesicular breathing sounds are heard primarily during inspiration and are the sounds of air filling the alveolar sacs. 2.) Obtain a stethoscope and an alcohol wipe. 3.) Clean the stethoscope ear pieces with the alcohol wipe. 3.) Place the stethoscope diaphragm o n your lab partner’s throat, just below the larynx. 4.) Listen for bronchial sounds during both inhalation and exhalation. 5.) Place the stethoscope diaphragm over the following chest areas to hear the vesicular breathing sounds: a.) at various intercostal spaces; b.) on the area of the back where no muscle covers the rib cage (just medial to the inferior part of the scapula; c.) under the clavicle. 6.) Vesicular breathing should sound like a rustling or muffled breeze. Diseased respiratory tissue or the presence of mucus can produce ‘rales’(rasping sounds) or ‘wheezing’ (whistling sounds). Activity D 1.) In this activity, you will observe the influences of blood gas concentrations on respiration rate. 2.) Obtain a brown paper bag. 3.) Determine the resting respiratory rate during normal breathing for yourself and your laboratory partner(s) by counting the number of breaths taken in one minute. If you prefer, you can count the number of breaths taken in 10 seconds and multiply by six. Record the results from three separate measurements and average them to obtain the resting respiratory rate (the number of breaths/minute). 4.) Note: people who are inclined to dizziness, shortness of breath or fainting should not perform steps 3-5. One member of each laboratory group should breathe normally for 2 minutes. After this time, have this individual hold his/her breath for as long as possible. Record the duration. 5.) After three additional minutes of normal breathing, have the same person breathe deeply and rapidly for about one minute. Following an exhalation, determine how long the subject can hold his/her breath. Record. 6.) Have the same person breath normally for 3. After normal breathing, the subject should breathe normally into the paper bag for 2 minutes. Following an exhalatio n, determine how long the subject can hold his/her breath. Record. Be able to explain any differences observed between steps 3-6. Activity E 1.) In this activity, you will determine your hematocrit to assess the ability of your blood to transport respiratory gases. A hematocrit measures the packed volume of the cells in your blood (AKA: ‘packed cell volume’) and is determined by centrifuging whole blood so that the cells are packed into the bottom of a small capillary tube. Red blood cells, those that transport respiratory gases, are more dense than white blood cells and therefore collect at the lowest level of the tube following centrifugation. The white cells collect on the top of the red cells and form what is called a ‘buffy coat’. A hematocrit determines the relative percentage of RBCs in a blood sample. A normal hematocrit for men is 47 +/-7 and for women is 42 +/-5. A hematocrit measurement below the normal range may indicate anemia; a hematocrit measurement significantly above normal may signal polycythemia or dehydration. 2.) Obtain a lancet, alcohol wipe, heparinized capillary tube (it should have a red stripe on the tube), a tray of capillary tube sealer and a ruler. 3.) Clean a desired finger with the alcohol wipe and prick it with the lancet. Immediately discard the lancet in the biohazard sharps container. Collect the blood directly into the capillary tube by holding the tube over the finger prick. 4.) When the tube is full (to the line), seal the end by forcing it into the sealing tray. 5.) Place the tube into the centrifuge with the sealed end facing outward. Do not start the centrifuge; your laboratory instructor will run the centrifuge when a significant number of tubes have been placed in it. 6.) When 5 minutes of centrifugation are complete, retrieve your tube and measure the total length of both plasma and formed elements (i.e., cells) in the capillary tube. 7.) Also measure the length of just the formed elements. 8.) Calculate your hematocrit using the following formula: Hematocrit = Red blood cells (mm) Plasma + formed elements (mm) X 100