46
Shoulder Pain
SCOTT DAVID MARTIN •
THOMAS S. THORNHILL
KEY POINTS
Comprehension of functional anatomy allows diagnosis of
most causes of shoulder pain on clinical examination.
History and clinical examination aided by ancillary tests will
usually guide application of the most appropriate treatment
for shoulder pain.
The differential diagnosis of shoulder pain includes not only
common local disorders (e.g., of tendon and adjacent
structures) but should also include consideration of
etiologies arising from distant anatomic sites arising by
referred pain-mediated pathways.
A variety of specific diagnostic tests can greatly aid in
diagnosis of shoulder pain.
Most causes of shoulder pain can be treated with a
structured physical therapy program. Successful treatment
programs understand potential surgical candidates including
those who fail conservative treatment.
Systemic arthroopathies can occasionally present with
shoulder disease and often involve the shoulder over time.
Early assessment in such patients is essential.
Shoulder pain is one of the most common musculoskeletal
complaints that may arise from diverse causes. Accurate
diagnosis of shoulder pain is made difficult by the unique
anatomy and position of the shoulder, which serves as a link
between the upper extremity and the thorax. One of the
most complex and mobile joints of the body, the shoulder
is traversed by muscle, tendon, and bone, and is surrounded
by major neurovascular structures, all of which may serve as
potential sources of local and referred pain.
Determining the source of shoulder pain is essential in
recommending the proper method of treatment. The examining physician must be able to differentiate the occurrence
of shoulder pain caused by intrinsic, or local factors, and
extrinsic, or remote factors, or a combination of the two.
Intrinsic factors originate from the shoulder girdle and
include glenohumeral and periarticular disorders, whereas
extrinsic factors occur outside of the shoulder girdle with
secondary referral of pain to the shoulder (Table 46-1).
Examples of extrinsic factors include left shoulder pain as
the initial presentation of coronary artery disease; hepatic,
gallbladder, and splenic disease also may initially manifest
as shoulder pain.
Accurate evaluation, diagnosis, and treatment require a
thorough understanding of shoulder anatomy, including
pain referral patterns. A complete and systematic physical
examination is crucial for an accurate diagnosis. During the
initial evaluation, care must be taken to discern all possible
causes of shoulder pain. Final diagnosis may require repeated
office examinations and correlation of diagnostic tests with
symptoms and response to selective injections. Improvements in diagnostic tests, such as magnetic resonance
imaging (MRI), computed tomography (CT)-arthrography,
ultrasonography, and electromyography (EMG), have facilitated early diagnosis of shoulder pain and have provided a
better understanding of shoulder pathology.
This chapter provides practical guidelines for the diagnosis and treatment of painful shoulder disorders that may
be encountered in a rheumatology or general practice. A
detailed analysis of shoulder problems and information on
the treatment of major trauma are beyond the scope of this
chapter and have been addressed by other authors.
ANATOMY AND FUNCTION
Because of its complexity, an understanding of the structural
and functional anatomy of the shoulder is required for the
clinician who is treating shoulder pain. The shoulder joint
is the most mobile joint of the body, although mobility is
gained at the sacrifice of stability. Only 25% of the humeral
head surface has contact with the glenoid at any time. The
labrum increases the contact area of the articular surface
and confers stability to the joint.6 Lesions of the labrum may
result from instability, and the type of lesion may indicate
the type of instability. Labral tears also may be a source of
pain from internal derangement of the shoulder.7 Joint stability is provided by a thin capsule and by the glenohumeral
ligaments, which are thickenings of the capsule anteriorly,
posteriorly, and inferiorly.6 Anterior stability is predominantly conferred by the anterior band of the inferior glenohumeral ligament.
The rotator cuff provides dynamic stability of the joint.
It is composed of four musculotendinous units: the supraspinatus, infraspinatus, and teres minor posteriorly, and the
subscapularis anteriorly. The shoulder consists of three
joints: the acromioclavicular (AC), sternoclavicular, and
glenohumeral joints, and two gliding planes—the scapulothoracic and subacromial surfaces.
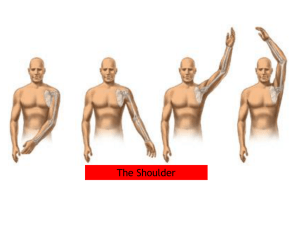
Figure 46-1 shows the musculoskeletal and topographic
localization of pain associated with common shoulder disorders. Figure 46-2 shows the relationship of the three posterior rotator cuff muscles coursing anteriorly underneath
the acromion to insert on the greater tuberosity. The subscapularis, the only anterior rotator cuff muscle, inserts on
the lesser tuberosity. By understanding the relationship
between the rotator cuff and the subacromial region,
bounded inferiorly by the humeral head and superiorly by
the undersurface of the acromion, the clinician can visualize
the problems of impingement syndrome and can accurately
639
640
PART 6 | DIFFERENTIAL DIAGNOSIS OF REGIONAL AND DIFFUSE MUSCULOSKELETAL PAIN
Table 46-1 Common Causes of Shoulder Pain
Intrinsic Causes
Periarticular Disorders
Rotator cuff tendinitis or impingement syndrome
Calcific tendinitis
Rotator cuff tear
Bicipital tendinitis
Acromioclavicular arthritis
Glenohumeral Disorders
Inflammatory arthritis
Osteoarthritis
Osteonecrosis
Cuff arthropathy
Septic arthritis
Glenoid labral tears
Adhesive capsulitis
Glenohumeral instability
Extrinsic Causes
Regional Disorders
Cervical radiculopathy
Brachial neuritis
Nerve entrapment syndromes
Sternoclavicular arthritis
Reflex sympathetic dystrophy
Fibrositis
Neoplasms
Miscellaneous
Gallbladder disease
Splenic trauma
Subphrenic abscess
Myocardial infarction
Thyroid disease
Diabetes mellitus
Renal osteodystrophy
inject this space. Knowledge of the route of the tendon of
the long head of the biceps through the bicipital groove and
onto the superior aspect of the glenoid helps in understanding bicipital tendinitis. Before attempting to diagnose and
treat shoulder pain, the clinician should review in detail one
of the many sources describing the structural and functional
relationships of the shoulder girdle.2,3
DIAGNOSIS
Clinical Evaluation of the Shoulder
Accurate diagnosis and successful treatment of a shoulder
disorder begin with a thorough history and physical examination. Most of the information needed to make a correct
diagnosis can be elicited with basic clinical skills, rather
than by relying on expensive and highly technologic investigative aids. Diagnostic tests should be used only to confirm
an established diagnosis or to assist in cases with a challenging presentation.
History
In establishing a diagnosis, it is important to consider the
patient’s age and chief complaint. The differential diagnosis
of shoulder pain in a 70-year-old sedentary individual is
entirely different from that in a 20-year-old pitcher. Did the
pain occur slowly over time or suddenly with a particular
event? Gradual onset of pain over the anterolateral or
deltoid region that is increased with forward elevation of
the shoulder and nocturnal pain suggest impingement with
rotator cuff tendinopathy. The presence of significant weakness with pain on overhead activities suggests impingement
with rotator cuff tear. Pain and weakness may also be noted
with reaching behind the back with the shoulder in extension and external rotation, as when reaching into the back
seat of a car. Initiating factors relative to the onset of symptoms should be elicited, and any history of shoulder pain or
trauma should be carefully documented.
Pain intensity, character, location, and periodicity and
aggravating or alleviating factors should be assessed. Pain
should be graded on a visual analog scale of 0 to 10, with 0
indicating no pain, and 10 indicating the worst pain the
patient has ever experienced. Another indication of the
severity of pain is disruption of sleep. The patient should be
asked whether the pain prevents sleep or awakens the
patient, and whether the patient can lie on the affected
shoulder. Is the pain sharp or dull? Sharp, burning pain over
the top of the shoulder indicates a neurogenic origin,
whereas a dull, aching pain over the lateral deltoid suggests
rotator cuff pathology with impingement. Location or distribution of the pain should be identified. Is it local around
the shoulder girdle, or does the pain radiate down the arm?
Is concomitant sensory loss or weakness present? Periodicity
of the pain as constant or intermittent should be determined, as should factors that aggravate or alleviate the pain.
Pain caused by rotator cuff tendinopathy usually is exacerbated by repetitive activities that involve the elbow away
from the side of the body.
Any history of neck pain should be considered, along
with history of radicular pain. Radicular-type pain frequently extends below the elbow and is associated with
sensory loss and weakness. Pain located in the paracervical
region may indicate a cervical origin, or it can be localized
to the trapezius. Trapezial pain often is associated with
shoulder pain and results from the patient trying to favor
the shoulder. Assuming a military brace position may
produce fatiguing, spasm, and trigger points of the
trapezius.
Any pertinent medical history, such as a history of malignancy, should be considered. Neurologic, visceral, and vascular disease can produce referred pain to the shoulder and
should always be considered, especially in a patient with a
painless range of motion.
Physical Examination
Proper physical examination of the shoulder includes close
inspection of the shoulder girdle from the front and back.
The evaluation is started by standing behind the patient,
who has both shoulders exposed. The normal shoulder is
always inspected and compared with the injured shoulder.
Examination can be performed with the patient in the
sitting or standing position. Contour and symmetry are
observed and compared between shoulders, and any atrophy
or asymmetry in shoulder position or level is assessed. Spinatus muscle atrophy may result from disuse, chronic cuff
tear, or suprascapular or brachial neuropathy.8 If scapular
winging is evident, the patient should be asked to do a wall
push-up, which accentuates winging.
CHAPTER 46 3
1
| Shoulder Pain
641
7
4
5
6
2
8
B
A
2
1
6
3
7
5
8
4
C
D
Figure 46-1 Musculoskeletal (A and B) and topographic (C and D) areas localizing pain and tenderness associated with specific shoulder problems.
1, Subacromial space (rotator cuff tendinitis/impingement syndrome, calcific tendinitis, rotator cuff tear). 2, Bicipital groove (bicipital tendinitis, biceps
tendon subluxation and tear). 3, Acromioclavicular joint. 4, Anterior glenohumeral joint (glenohumeral arthritis, osteonecrosis, glenoid labrum tears,
adhesive capsulitis). 5, Sternoclavicular joint. 6, Posterior edge of acromion (rotator cuff tendinitis, calcific tendinitis, rotator cuff tear). 7, Suprascapular
notch (suprascapular nerve entrapment). 8, Quadrilateral space (axillary nerve entrapment). These areas of pain and tenderness frequently overlap.
Coracoclavicular ligament:
Subscapularis tendon
Trapezoid ligament
Coracoid
Supraspinatus
Conoid ligament
process
tendon
Infraspinatus
tendon
Teres minor
tendon
Supraspinatus
muscle
Clavicle
Clavicle
Subscapularis
muscle
Acromion of
scapula
Coracoacromial
ligament
Spine of scapula
Superior margin of scapula
Infraspinatus muscle
A
Supraspinatus
muscle
Coracoid
process
Acromioclavicular joint
Acromion
Coracoacromial
ligament
Supraspinatus
tendon
Subscapularis
tendon
Greater
tuberosity
Lesser
tuberosity
Humerus
Bicipital tendon groove
B
Figure 46-2 A, Superior view of the rotator cuff musculature as it courses anteriorly underneath the coracoacromial arch to insert on the greater
tuberosity. B, Anterior view of the shoulder reveals the subscapularis, which is the only anterior rotator cuff muscle inserting on the lesser tuberosity.
It internally rotates the humerus and provides dynamic anterior stability to the shoulder. (A and B, From the Ciba Collection of Medical Illustrations,
Volume 8, Part I. Netter Illustration from www.netterimages.com ©Elsevier Inc. All rights reserved.)
642
PART 6 | DIFFERENTIAL DIAGNOSIS OF REGIONAL AND DIFFUSE MUSCULOSKELETAL PAIN
Range of motion should be carefully recorded, along with
notation of any absence of rhythmic shoulder motion or
excessive scapulothoracic motion that may compensate for
the lack of glenohumeral motion. Internal rotation of the
shoulder is checked by having the patient reach behind the
back with the thumb while the examiner notices the vertebral level. Loss of internal rotation is seen early with shoulder pain and usually indicates some tightness of the posterior
shoulder capsule. The biceps tendon; the coracoid, lesser,
and greater tuberosities; and the posterior cuff are palpated,
and any tenderness is gauged (Figure 46-3A). Tenderness
on palpation of the long head of the biceps frequently is
associated with rotator cuff tendinopathy and tenderness of
the greater tuberosity. Any spasm or tenderness of the trapezius or levator scapulae may be associated with rotator
cuff disease or cervical spine disease. Cervical range of
motion and palpation of the paracervical muscles are carried
out. Paracervical tenderness and limited range of motion of
the neck may indicate cervical spondylosis or neurogenic
disease. A Spurling test is done by flexing the neck laterally
Sternoclavicular Acromioclavicular joint
joint
Subdeltoid bursa
Bicipital
tendon
groove
while applying axial compression to the skull. Pain that
radiates to the ipsilateral shoulder is considered a positive
test result and indicates radiculopathy.
To elicit the impingement sign, the shoulder is elevated
passively in forward flexion, while the scapula is depressed
with the opposite hand, forcing the greater tuberosity
against the anterior acromion and producing pain in cases
of impingement (Figure 46-3B).9 This maneuver also may
be painful in conditions such as adhesive capsulitis,
glenohumeral and acromioclavicular (AC) arthritis, glenohumeral instability, and calcific tendinitis. A dynamic
impingement test, the circumduction-adduction shoulder
maneuver, also called the Clancy test, is 95% sensitive and
95% specific for diagnosing rotator cuff tendinopathy,
including partial tears.10 The test is done with the patient
in the standing position and with the head turned to the
contralateral shoulder. The affected shoulder is circumducted and adducted across the body to shoulder level,
while the elbow is kept in extension, the shoulder in internal rotation, and the thumb pointing toward the floor
Examiner elevates
shoulder here and...
Arm
adducted
across
chest
Examiner
applies force
here
Greater
tuberosity
Lesser
tuberosity
A
Glenohumeral
joint space
B
Pain on palpation =
acromioclavicular
joint
impingement
...depresses
scapula
here (from
back)
C
Patient
resists
force
here
Patient attempts
external rotation
of the shoulder
30
Pain on palpation
= tight posterior
capsule
D
Examiner
applies
force
here
90
E
Examiner
applies
force here
F
Patient resists
force here
Figure 46-3 A, Tenderness on palpation of trigger points may help localize the site of pathology. Tenderness on palpation of the long head of the
biceps and greater tuberosity suggests impingement with possible cuff tendinopathy. B, To elicit the impingement sign, the shoulder is elevated in
forward flexion while the scapula is depressed with the opposite hand, forcing the greater tuberosity and the rotator cuff against the anterior acromion
and producing pain when impingement exists. Relief of pain after injection of local anesthetics (i.e., impingement test) provides additional evidence
of subacromial pathology. C, The Clancy test is performed with the patient standing and with the head turned toward the contralateral shoulder. The
affected shoulder is circumducted and adducted across the body to shoulder level, keeping the elbow in extension with the arm internally rotated
with the thumb pointed toward the floor. In this position, the patient is asked to resist maximally as a uniform downward force is applied to the
extended arm by the examiner. Production of pain or weakness localized to the anterior lateral portion of the shoulder is considered a positive test
result. D, The test is performed by forward flexion of the arm at 90 degrees and subsequent cross-chest adduction of the arm. Pain localized to the
acromioclavicular joint is considered a positive test result. E, The test is performed with the patient’s elbow flexed at 90 degrees and held at the
patient’s side by the examiner. The patient is asked to attempt external rotation of the shoulder from a neutral position (0 degrees of adduction) as
the examiner applies resistance to the forearm. Strength is compared with that of the contralateral arm. F, Abduction strength testing is performed
with the patient’s shoulder in 30 degrees of forward flexion and 90 degrees of abduction and with the thumb pointed toward the floor. The patient
is asked to resist as the examiner exerts a downward force on the abducted arm. Strength is compared with the contralateral shoulder. (From Martin
TL, Martin SD: Rotator cuff tendinopathy, Hosp Med 12:23–31, 1998.)
CHAPTER 46 (Figure 46-3C). In this position, the patient is instructed to
resist maximally as a uniform downward force is applied to
the extended arm by the examiner. The test result is considered positive if pain or weakness is elicited during the
maneuver, with pain localized to the anterolateral aspect of
the shoulder. A strong positive correlation of pain and
weakness is noted with complete cuff tear.10
The sternoclavicular and AC joints should be observed
for prominences and palpated for stability and tenderness.
Many patients with impingement have tenderness on direct
downward palpation of the AC joint owing to impingement
on the cuff from undersurface osteophytes of the distal
clavicle.2,8
AC joint tenderness may also result from primary AC
joint arthrosis and should be differentiated by physical
examination, including the cross-chest adduction test and
O’Brien’s test.11 Radiographic evidence of AC joint arthrosis is common in patients older than 40 years, but this
condition is not usually painful.12
The cross-chest adduction test or the horizontal adduction test is performed by forward flexing the shoulder 90
degrees with subsequent cross-chest adduction of the arm
(Figure 46-3D). Pain localized to the AC joint is considered
a positive test result. If pain occurs posteriorly over the
shoulder, a tight posterior capsule with impingement is suspected. O’Brien’s test is performed by forward flexing the
arm 90 degrees and adducting the arm 10 degrees out of
the sagittal plane of the body. The first part of the test is
performed with the hand maximally pronated with the
thumb pointed down. In this position, the patient is asked
to resist as the examiner applies a downward force on the
arm. If the test elicits pain, the patient is asked if the pain
is on top of the shoulder or deep inside. Pain localized to
the top of the shoulder indicates AC joint pain, and pain
deep inside the shoulder indicates a superior labrum anterior
posterior (SLAP) lesion. In the second part of the test, the
patient is asked to supinate the hand maximally, while the
examiner applies a downward force to the arm. If the patient
notices significantly less pain, the test result is positive for
a SLAP lesion. If the pain is unchanged and is located on
top of the shoulder, the test result is positive for AC joint
pathology.11
If the cause of AC joint tenderness is still in question, a
lidocaine injection should be administered. The clinician
should carefully avoid injecting the subacromial space by
advancing the needle too far inferiorly through the AC
joint; this can lead to false interpretation. Painful degenerative changes of the AC joint may exist concomitantly with
subacromial impingement and should be evaluated thoroughly when surgical treatment (i.e., distal clavicle excision) is being considered.13
In patients with pain out of proportion to objective findings, other causes of shoulder pain should be sought, including calcific tendinitis, infection, reflex sympathetic
dystrophy, and fracture. Patients with significant wasting of
the supraspinatus and infraspinatus muscles and posterior
shoulder pain, especially younger patients, may have suprascapular neuropathy or brachial neuropathy (ParsonageTurner syndrome).8,14
Patients with chronic cuff disease frequently have variable disuse atrophy of the supraspinatus and infraspinatus
fossae; in cases of chronic massive cuff tears, atrophy and
| Shoulder Pain
643
weakness can be severe. Strength testing of external rotation should be done with the elbow at the side and supported by the examiner; the patient is asked to attempt
external rotation of the shoulder from a neutral position (0
degrees of adduction), while the examiner applies resistance
(Figure 46-3E).15 Weakness in this position may suggest a
tear of the infraspinatus tendon. Abduction strength testing
against resistance is done with the shoulder in 30 degrees
of forward flexion and 90 degrees of abduction, and with the
thumb pointed toward the floor (Figure 46-3F).16,17 Weakness in this position may suggest a tear of the supraspinatus
tendon. A lift-off test should be performed with the shoulder in internal rotation; the patient is asked to try to hold
the hand away from the back. Inability to do so indicates a
subscapularis tear.
If after a thorough physical examination impingement is
suspected, an impingement test should be performed with
injection of 5 mL of local anesthetic into the subacromial
space.18,19 Before the test is performed, the patient is asked
to grade the pain during the impingement signs on a visual
analog scale of 0 to 10, with 0 equal to no pain and 10 equal
to the most severe pain the patient has ever experienced.
The injection may be done anteriorly, laterally, or posteriorly, depending on the physician’s preference. Ten minutes
after injection of local anesthetic into the subacromial
space, the patient should be re-examined and asked to
regrade the pain on the same visual analog scale. A 50% or
greater reduction in pain is thought to be a positive test
result for impingement; otherwise, an alternative cause of
shoulder pain should be sought, or inadequate placement of
the anesthetic should be suspected. If the AC joint is
thought to be contributing to the shoulder pain, 1 to 2 mL
of local anesthetic should be injected into the joint, and the
shoulder should be re-examined. When subacromial
impingement and the AC joint are thought to be contributing to shoulder pain, serial injections during separate office
visits may be needed to evaluate the shoulder while minimizing discomfort to the patient.12
In cases of suspected bicipital tendinitis, Speed’s test is
performed by having the patient flex the shoulder and
extend the elbow while a downward force is applied to the
arm. The production of pain over the long head of the biceps
is a positive test result and suggests bicipital tendinitis.
Upper extremity strength testing should be performed
and compared with the contralateral side so that any atrophy
is detected. Grip strength is checked, and the hands are
examined carefully for evidence of intrinsic atrophy. The
biceps (C5), triceps (C7), and brachioradialis (C6) reflexes
are checked for symmetry and briskness.
Light touch sensory testing should be conducted, and the
dermatomal distribution of any deficits that may suggest
cervical radiculopathy should be identified. The cervical,
supraclavicular, axillary, and epitrochlear regions should be
palpated for enlarged lymph nodes, which may suggest
malignancy.
Imaging
Radiographic Assessment
For nontraumatic painful shoulder evaluation, standard
radiographic profiles are used. An impingement series
644
PART 6 | DIFFERENTIAL DIAGNOSIS OF REGIONAL AND DIFFUSE MUSCULOSKELETAL PAIN
should be obtained, which includes anteroposterior views
with a 30-degree caudal tilt (Rockwood view), an outlet
view (scapular Y with 10- to 15-degree caudal tilt), and an
axillary view. Internal and external rotational views may be
obtained if calcific tendinitis or instability is suspected. The
Rockwood view can reveal any osteophytes off the anterior
acromion and AC joint.20 In cases of traumatic injury, a
trauma series is obtained that includes a true anteroposterior
view, a scapular Y view, and an axillary view. The axillary
view is useful in assessing posterior or anterior subluxation
of the humeral head. Additional views, such as the West
Point view, which evaluates the glenoid for evidence of a
bony Bankart lesion, or the Styker notch view, which
assesses the humeral head for a Hill-Sachs lesion, may be
obtained to assist evaluation if the diagnosis of instability is
in doubt. Secondary impingement-type rotator cuff tendinitis may be caused by increased anterior translation with
subluxation of the humeral head. In such cases, an axillary
view or fluoroscopy can help show the subluxation.21,22
When AC joint pathology is suspected, a 10-degree,
cephalic tilt view of the AC joint at 50% penetrance, as
described by Zanca,23 should be obtained (Figure 46-4).
Stress views of the AC joint may be obtained by strapping
5 to 10 lb of weight to the patient’s forearms and determining AC separation. Comparing the coracoclavicular distance of both shoulders may be helpful. When clinically
indicated, cervical spine radiographs should be obtained to
exclude cervical spondylosis as a cause of shoulder pain.
Scintigraphy
Tc 99m methyl diphosphonate (MDP) or gallium may be of
diagnostic help in evaluating skeletal lesions around the
shoulder joint. Bone scans generally are not helpful in the
RC
AC
BT
Figure 46-5 Normal double-contrast arthrography shows the inferior
edge of the rotator cuff (RC) as it courses through the subacromial space
to the greater tuberosity, the tendon of the long head of the biceps (BT),
and the articular cartilage of the humeral head (AC).
diagnosis of non-neoplastic or noninfectious shoulder
disease.
Scintigraphy may have a role in identifying patients with
complete rotator cuff tears that proceed to cuff-tear arthropathy. This is an important distinction because patients with
complete rotator cuff tears may do well, whereas those who
develop progressive changes of cuff-tear arthropathy have
progressive arthritis, pain, and significant functional impairment. Synovitis or calcium pyrophosphate deposition
disease may be an important factor in the pathogenesis of
cuff-tear arthropathy. In such cases, scintigraphy may show
the increased blood flow and blood pooling associated with
chronic synovitis.
Arthrography
X-ray
10°
Figure 46-4 Zanca view of the acromioclavicular joint is obtained with
a 10-degree cephalic tilt and 50% penetrance. (From Rockwood CA Jr,
Young DC: Disorders of the acromioclavicular joint. In Rockwood CA Jr,
Matsen TA III, editors: The shoulder, Philadelphia, 1985, WB Saunders, pp
413–476.)
Double-contrast arthrotomography (DCAT) can be used to
evaluate problems of the rotator cuff, glenoid labrum, biceps
tendon, and shoulder capsule.24-27 Figure 46-5 shows normal
DCAT of the shoulder. Rotator cuff tears can be shown by
single-contrast or double-contrast studies. Proponents of
double-contrast arthrography believe that the extent of the
tear, the preferred surgical approach, and the quality of the
rotator cuff tissue are best determined by double-contrast
studies.24-29 Arthrography without MRI or CT can be misleading and may result in underestimation of the extent of
a rotator cuff tear. Multidetector CT can enhance the accuracy of diagnosing labral and rotator cuff tears, especially in
patients for whom MRI is not possible (Figure 46-6).
Tears of the glenoid labrum without shoulder dislocation
are sources of anterior shoulder pain in athletes.7 Glenoid
labrum tears (Figure 46-7), with or without associated glenohumeral subluxation, frequently can be identified by
DCAT.27,28 Kneisl and colleagues30 described 55 patients
who underwent DCAT followed by diagnostic shoulder
CHAPTER 46 | Shoulder Pain
645
Figure 46-6 Multidetector computed tomography revealing a superior
labral tear of the shoulder.
arthroscopy. DCAT predicted the arthroscopic findings in
76% of anterior labrum studies and 96% of posterior labrum
studies. This test was 100% sensitive and 94% specific in
diagnosing complete rotator cuff tears. Partial rotator cuff
tears identified at arthroscopy were missed in 83% of patients
undergoing DCAT. Investigators believed that DCAT was
better in diagnosing intra-articular and cuff pathology in
cases of instability than when pain alone was the presenting
diagnosis.30
Shoulder arthrography can confirm a diagnosis of adhesive capsulitis by showing a contracted capsule with an
obliterated axillary recess (Figure 46-8). The use of subacromial bursography has been beneficial in visualizing the outer
surface of the rotator cuff and the subacromial space in cases
of impingement.31,32 Fukuda and associates33 reported a
small series of younger patients (average age, 41.8 years)
who underwent subacromial bursography after a negative
glenohumeral arthrographic result. These patients showed
pooling of contrast medium on the bursal side of a tear,
which was confirmed at the time of surgery. Subacromial
Figure 46-8 Double-contrast arthrography of a patient with calcific
tendinitis (arrow) and adhesive capsulitis. Notice the contracted capsule
with diminution of the synovial space and obliteration of the axillary
recess.
bursography is not routinely used diagnostically, and, in
our opinion, it is of little value in planning surgical
procedures.
Computed Tomography
CT is helpful in evaluating the musculoskeletal system, and
CT combined with contrast arthrography (CT-arthrography)
has become a major diagnostic tool for the evaluation of
glenoid labrum tears, loose bodies, and chondral lesions
(Figure 46-9). Rafii and co-workers34 reported using
CT-arthrography in an evaluation of shoulder derangement.
This study found 95% accuracy of CT-arthrography for
investigating lesions of the labrum and articular surface.34
More recently, multidetector CT-arthrography scans have
been used to evaluate partial cuff tears (Figure 46-10A),
cystic lesions (Figure 46-10B), and calcific tendinopathy
(Figure 46-10C).
Ultrasonography
Figure 46-7 Double-contrast arthrotomography shows a tear of the
anterior-inferior portion of the glenoid labrum (arrow).
Technologic improvements in ultrasound equipment have
led to improved ultrasound study of the rotor cuff. The
technique is noninvasive, is rapid, and involves no radiation
exposure.30-32,35 The cuff is examined in the horizontal and
transverse planes with the arm in different positions to
allow visualization of various areas of the cuff. These techniques generally provide visualization of the distal cuff,
where most rotator cuff tears are located. Figure 46-11 shows
normal and abnormal ultrasound images of the rotator cuff
in longitudinal and transverse planes.
Several studies report high sensitivity and specificity for
the diagnosis of a rotator cuff tear by ultrasound.32-35 The
specificity and sensitivity of the procedure are reported to
be greater than 90% as determined by arthrographic and
surgical correlations.34,35 This technique also has been used
for the postoperative evaluation of a rotator cuff repair and
for evaluation of abnormalities of the biceps tendon.36-40
646
PART 6 A
| DIFFERENTIAL DIAGNOSIS OF REGIONAL AND DIFFUSE MUSCULOSKELETAL PAIN
B
C
D
Figure 46-9 CT-arthrography of the shoulder. A, Normal findings. B, Tear of the anterior glenoid labrum. C, Large defect of the articular surface of
the posterior portion of the humeral head (Hill-Sachs lesion) (arrow). D, Loose body in the posterior recess (arrow).
Gardelin and Perin41 reported ultrasound to be 96% sensitive in determining rotator cuff and biceps tendon pathology. Mack and associates36 found ultrasound to be valuable
in evaluating postoperative patients with recurrent shoulder
symptoms. In a prospective study, Hodler and colleagues39
compared ultrasound with MRI and arthrography in evaluating rotator cuff lesions in 24 shoulders. Ultrasound identified 14 of 15 torn cuffs, MRI identified 10 of 15, and
arthrography identified 15 of 15.39 Ultrasound identified 7
of 9 intact rotator cuffs, whereas MRI was accurate in 8 of
9 intact cuffs.39 Vestring and colleagues42 found ultrasound
to be as accurate as MRI in the diagnosis of humeral head
defects and joint effusions, but inferior to MRI in the diagnosis of labrum lesions, rotator cuff lesions, subacromial
spurs, and synovial inflammatory disease. In the hands of an
experienced sonographer, ultrasound may be the most costeffective test for the initial evaluation of a rotator cuff
injury, but most surgeons require CT-arthrography or MRI
confirmation before beginning surgical exploration.36,39,41-43
Arthroscopy
The use of arthroscopy for the diagnosis of shoulder pathology increased in the 1980s, in part because of its accuracy,
which was far greater than that of clinical examination and
better than the accuracy of other diagnostic modalities of
the time. With technologic advances in fiberoptics, video
output, and arthroscopic instrumentation, the use of arthroscopy to diagnose and treat shoulder problems exponentially
increased to include procedures previously used only for
open techniques.44
Compared with DCAT, arthroscopy is more accurate in
the diagnosis of intra-articular lesions associated with a
painful shoulder.30 An additional benefit is that arthroscopy
can be used to diagnose and treat shoulder problems of the
glenohumeral joint and the subacromial region. With
increased accuracy of MRI-arthrography in detecting partial
cuff tears and labral lesions, diagnostic shoulder arthroscopy
has become less common in the absence of clear indications
and specific treatment plans. In combination with a detailed
history and physical examination, and along with examination under anesthesia, shoulder arthroscopy has been helpful
in the diagnosis of chronic instability patterns of the glenohumeral joint.44-47
The indications and usefulness of shoulder arthroscopy
in the treatment of common pathologic conditions have
continued to increase as the technology improves, and as
understanding of the pathophysiology of shoulder problems
grows. Shoulder arthroscopy has been used routinely to
confirm and treat SLAP lesions, labral tears, partial cuff
CHAPTER 46 A
C
tears, refractory adhesive capsulitis, partial biceps tendon
tears, and multidirectional instability. Other conditions
that are routinely treated arthroscopically include rotator
cuff tears, glenohumeral instability, AC joint pathology,
loose bodies, sepsis, osteochondritis dissecans, synovitis,
chondral lesions, subacromial impingement, and calcific
tendinitis.7,13,44,47
Magnetic Resonance Imaging
MRI has been used to diagnose partial-thickness and fullthickness rotator cuff tears, biceps tendon tears, impingement of the rotator cuff, synovitis, articular cartilage damage,
and labral pathology associated with glenohumeral
instability.48-50 In rheumatoid arthritis, MRI is reported to
be more sensitive than plain radiographs in determining soft
tissue abnormalities and osseous abnormalities of the glenoid
and humeral head.51
One of the most valuable diagnostic uses of MRI is in
rotator cuff pathology. Morrison and Offstein52 studied 100
patients with chronic subacromial impingement syndrome
using arthrography and MRI. MRI was 100% sensitive but
only 88% specific in confirming arthrography-proven rotator
cuff tears. Nelson and associates53 studied 21 patients with
shoulder pain and found MRI to be more accurate than
CT-arthrography or ultrasound in identifying partialthickness cuff tears. These investigators also reported MRI
| Shoulder Pain
647
B
Figure 46-10 Multidetector computed tomography–arthrography.
A, Partial rotator cuff tear (coronal view). B, Cystic humeral head erosions with calcification (axial view). C, Calcification within rotator cuff
tendon (coronal view).
to be as accurate as CT-arthrography in the diagnosis of
abnormalities of the glenoid labrum.53
Characteristic MRI findings in rotator cuff tears include
a hypointense gap within the supraspinatus muscle tendon
complex on T1-weighted films, absence of a demonstrable
supraspinatus tendon with narrowing of the subacromial
space, and an increased signal within the supraspinatus
tendon on T2-weighted images.54 Seeger and colleagues,55
reporting the results of 170 MRI studies, found that
T1-weighted images were highly sensitive for identifying
abnormalities within the supraspinatus tendon, but
T2-weighted images were required to differentiate tendinitis
from a small supraspinatus tendon tear. Large full-thickness
tears could be identified, however, on T1-weighted and
T2-weighted images. Figure 46-12 depicts common shoulder pathology as seen by MRI. MRI is almost as sensitive as
and is more specific than scintigraphy in the diagnosis of
osteonecrosis and neoplastic lesions around the shoulder.
Electromyography and Nerve Conduction
Velocity Studies
EMG and nerve conduction velocity studies can help differentiate shoulder pain from pain of neurogenic origin.
They also may be beneficial in determining the localization
of neurogenic pain to a particular cervical root, the brachial
plexus, or a peripheral nerve.56,57
648
PART 6 | DIFFERENTIAL DIAGNOSIS OF REGIONAL AND DIFFUSE MUSCULOSKELETAL PAIN
4
4
3
3
2
5
2
1
1
A
C
B
D
Figure 46-11 A, Normal longitudinal view of rotator cuff by ultrasound shows the humeral head (1), the superior articular surface (2), the rotator
cuff (3), the deltoid tendon (4), and tapering of the cuff to its insertion on the greater tuberosity (5). B, Transverse view of a normal intact rotator cuff
covering the humeral head. C, Rotator cuff tear, showing a hypoechoic area (arrow) on a longitudinal view. D, Rotator cuff tear, showing hypoechoic
area (arrows) on a transverse view.
Injection
Potential Diagnostic Tests
Injection of local anesthetics and glucocorticoids is a useful
technique for the diagnosis and treatment of shoulder pain.58
The physician must have a thorough understanding of the
anatomy of the shoulder girdle and a presumptive diagnosis
to direct the injection properly. Injection of referred pain
areas may be misleading. In a patient with lateral arm pain
secondary to deltoid bursal involvement from calcific tendinitis of the supraspinatus tendon, injection should be
performed in the subacromial space, rather than in the
area of referred pain in the deltoid muscle. It is often better
to use a posterior or lateral subacromial approach when
injecting a rotator cuff tendinitis in a patient with anterior
impingement symptoms because it is easier to enter the
subacromial region posteriorly or laterally, and this approach
is less traumatic for contracted anterior structures.
The instillation of rapidly acting local anesthetics can be
beneficial in determining the source of shoulder pain. Obliteration of pain by injection of a local anesthetic along the
bicipital groove can confirm a diagnosis of bicipital tendinitis. The use of local anesthetics is less helpful when the
subacromial space is injected because of its extensive communication with the rest of the shoulder girdle, but relief of
symptoms by such an injection can exclude pain from conditions such as cervical radiculopathy or entrapment
neuropathy.
Table 46-2 lists reimbursement and charges for various
shoulder diagnostic tests based on 2011 Medicare fee schedules and 2011 charges at a single institution. The choice of
a specific test depends on its sensitivity, specificity, and costbenefit analysis. History and physical examination are the
most important factors in establishing diagnosis of the
painful shoulder. Plain radiographs (three views) should be
the first radiographic tests performed. Although not as sensitive as the more sophisticated tests, plain radiographs can
identify arthritic change, calcific tendinitis, established
osteonecrosis, and most neoplasms.
If intra-articular pathology (e.g., labrum tear, capsular
tear, loose body, chondral defect) is suspected, MRIarthrography is preferable to CT-arthrography. In diagnosing acute rotator cuff tears in a younger patient, ultrasound
is the most cost-effective test to confirm a clinical suspicion.
In cases of impingement syndrome, MRI is sensitive, but it
is difficult to differentiate tendinitis, partial tears, and small
complete tears without MRI-arthrography. Orthopedic surgeons prefer MRI-arthrography for verification of labral
tears or partial rotator cuff tears. In the case of a suspected
full-thickness rotator cuff tear, MRI is preferred to determine the size of the tear, the amount of muscle atrophy and
tendon retraction, and the quality of remaining tissue for
repair.
CHAPTER 46 A
| Shoulder Pain
649
B
B
A
A
A
B
C
E
B
D
F
Figure 46-12 A, Magnetic resonance imaging (MRI) proton density–weighted coronal view shows the supraspinatus tendon as a black
band (A) that has an increased signal as it nears insertion on the greater tuberosity (B). B, Similar view in a T2-weighted image shows increased signal
as gray (arrow), indicating a partial-thickness tear or tendinitis. C, MRI proton density–weighted coronal view shows abrupt end of supraspinatus
tendon as it courses right to left (A). From A to B is an area of increased signal followed by a short portion of tendon (B) inserting at the greater tuberosity. D, Similar view in a T2-weighted image shows increased signal as white (fluid density), indicating fluid in the gap of a complete rotator cuff tear.
E, MR arthrography shows a normal rotator cuff. F, MR arthrography shows a chronic cuff tear with retraction.
INTRINSIC FACTORS CAUSING
SHOULDER PAIN
Periarticular Disorders
Shoulder Impingement and Rotator
Cuff Tendinopathy
One of the most common nontraumatic causes of shoulder
pain is impingement with rotator cuff tendinopathy. In
1972, Neer9 described his results of 100 anatomic shoulder
dissections and coined the term impingement syndrome.
Impingement may be defined as the encroachment of the
acromion, coracoacromial ligament, coracoid process, or
AC joint on the rotator cuff as it passes beneath them
during glenohumeral motion. The function of the posterior
rotator cuff is to abduct and externally rotate the humerus.
The cuff with the biceps tendon serves as a humeral head
depressor to maintain the head centered within the glenoid
fossa as the cuff and to use the deltoid to elevate the
arm.59-61
Controversy continues, however, as to the exact cause of
impingement, that is, whether it is a primary, intrinsic,
degenerative event within the tendon with superior
migration of the head on arm elevation and secondary
650
PART 6 | DIFFERENTIAL DIAGNOSIS OF REGIONAL AND DIFFUSE MUSCULOSKELETAL PAIN
Table 46-2 Relative Costs of Shoulder Diagnostic Procedure in 2011
Procedure
Initial Fee (USD)
Technical Fee (USD)
Interpretation Fee (USD)
36.28
156.08
74.70
531.28
233.06
78.53
23.09
34.07
41.62
81.42
66.77
39.69
371.00
533.00
801.00
3831.00
1860.00
36.00
302.00
119.00
350.00
203.00
Medicare B Fee Schedule
Initial office visit (30 min)
Plain radiography (3 views)
Arthrography
Ultrasonography
Magnetic resonance imaging
Computed tomography
Tomography
154.00
Institutional Charges
Initial office visit (30 min)
Plain radiography (3 views)
Arthrography
Ultrasonography
Magnetic resonance imaging
Computed tomography
196.00
USD, U.S. dollars.
impingement on the acromion, or purely mechanical attrition of the tendon with primary impingement against the
acromion. The mechanical impingement of the rotator cuff
may be influenced by variations in the shape and slope of
the acromion.62,63 The supraspinatus outlet may become
narrowed from proliferative spur formation of the acromion
or degenerative changes in the AC joint. These changes,
along with intrinsic degenerative changes of the rotator
cuff, may lead to rotator cuff tear, but the exact pathogenesis
remains controversial. Many studies have found a strong
correlation between degenerative hypertrophic spur formation, with its resulting narrowing of the supraspinatus outlet,
and the presence of full-thickness cuff tears,9,19,64-71 but clinical studies have failed to confirm whether hypertrophic
changes in the coracoacromial arch are caused by the cuff
lesions, or whether these changes themselves cause the
lesions.
Neer9 developed a staging system for description of
impingement lesions of the shoulder. A stage I lesion
involves edema and hemorrhage of the rotator cuff and is
typically found in individuals younger than 25 years who
are active in overhead athletics. The condition usually
responds to conservative treatment that includes rest, antiinflammatory medication, and physical therapy. Stage II
lesions usually occur in the 30s or 40s and represent the
biologic response of fibrosis and thickening of the tendon
after repeated episodes of mechanical impingement over
time. Lesions are treated conservatively, as in stage I, but
attacks may recur. If symptoms persist despite adequate conservative management for longer than 6 to 12 months,
surgical intervention is warranted. Stage III lesions involve
rotator cuff tears, biceps tendon rupture, and bone changes,
and they rarely occur before age 40. Patients may present
with pain, weakness, or supraspinatus atrophy, depending
on the chronicity of the tear. Surgical treatment depends
on the patient’s age, loss of function, weakness, and pain.
Patients usually present to the clinician with a complaint
of pain that has failed to resolve after a variable period. Pain
can be sudden and incapacitating in cases of traumatic cuff
tears, or more commonly may manifest as a dull ache in
cases of chronic impingement. Pain usually is located over
the anterior and lateral aspects of the shoulder and may
radiate into the lateral deltoid. It may worsen with sleeping
on the affected extremity and is exacerbated by overhead
activity. Tenderness on palpation may be elicited over the
greater tuberosity and the long head of the biceps within
the bicipital groove, indicating an associated biceps tendinitis. In cases with concomitant degenerative changes in
the AC joint, tenderness may be noted on palpation over
the AC joint, as an offending osteophyte impinges on the
rotator cuff beneath.
The impingement sign as described by Neer9 (Figure
46-13) is useful in the diagnosis of rotator cuff tendinopathy.
The patient often describes a catch as the arm is brought
into the overhead position. The patient may be observed to
raise the arm by abduction and external rotation to clear
the greater tuberosity of the acromion, bypassing the painful
area. A typical painful arc usually occurs between 70 degrees
and 110 degrees of abduction. Neer9 also described an
impingement test that involves injection of lidocaine into
the subacromial bursa. Relief of pain is a positive impingement test result and usually indicates rotator cuff origin of
the shoulder pain.
Figure 46-13 The impingement sign is elicited by forced forward elevation of the arm. Pain results as the greater tuberosity impinges on the
acromion. The examiner’s hand prevents scapular rotation. This maneuver may be positive in other periarticular disorders. (From Neer CS II:
Impingement lesions, Clin Orthop Relat Res [173]:70, 1983.)
CHAPTER 46 Radiographs in the early stages of cuff tendinopathy may
be normal or may reveal a hooked acromion. As the disease
progresses, sclerosis, cyst formation, and sclerosis of the
anterior third of the acromion and the greater tuberosity
may be observed. An anterior acromial traction spur may
appear on the undersurface of the acromion lateral to the
AC joint and represents contracture of the coracoacromial
ligament. Late radiographic findings include narrowing of
the acromiohumeral gap, superior subluxation of the
humeral head in relation to the glenoid, and erosive changes
in the anterior acromion.71 Arthrography, MRI, and ultrasound may be helpful in diagnosing a full-thickness tear of
the rotator cuff in association with stage III disease. In some
cases of chronic large rotator cuff tears, proximal migration
of the humeral head leads to a pattern of degenerative
arthritis termed cuff-tear arthropathy.
The choice of treatment and frequently its result are
functions of the stage of the impingement and the response
to pain. In stage I disease, in which little mechanical
impingement occurs, most patients respond to rest. It is
important to avoid immobilizing the shoulder for any period
because contraction of the shoulder capsule and periarticular structures can produce an adhesive capsulitis. After a
period of rest, a progressive program of stretching and
strengthening exercises generally restores the shoulder to
normal function. Use of aspirin and other nonsteroidal antiinflammatory drugs (NSAIDs) may shorten the symptomatic period. Modalities such as ultrasound, neuroprobe, and
transcutaneous electrical nerve stimulation generally are
not helpful. Patients with stage I or II disease may have a
dramatic response to local injection of glucocorticosteroids
and local anesthetic agents. For stage II disease in which
fibrosis and thickening occur anteriorly, it is frequently
better to inject through a posterior approach. We prefer a
combination of 3 mL of 1% lidocaine (Xylocaine), 3 mL of
0.5% bupivacaine, and 20 mg of triamcinolone. This injection combines a short-acting anesthetic to help confirm the
diagnosis, a longer-acting anesthetic for analgesic purposes,
and a steroid preparation in a depot form.
An integrated program of occupational and physical
therapy often precludes the need for surgery in patients with
stage II disease. Job modification for individuals with
impingement syndrome caused by overuse may alleviate
symptoms. Businesses are becoming increasingly aware of
the cost savings associated with proper job ergonomics.72,73
The initial rehabilitation in stage II impingement consists of cessation of repetitive overhand activity. Ice,
NSAIDs, and local injections also may be beneficial. Initial
physical therapy includes passive, active-assisted, and active
range of motion combined with stretching and mobilization
exercises to prevent contracture. As pain and inflammation
subside, isometric or isotonic exercises are used to strengthen
the rotator cuff musculature. Isokinetic training at variable
speeds and in variable positions is instituted before the
patient is returned to full activity. For patients with a jobrelated injury, it is crucial to review and modify job mechanics to prevent recurrent episodes that can cause further
disability and may precipitate the need for surgery.72
Neer19 suggested that a patient with refractory stage II
disease may respond to division of the coracoacromial ligament and bursectomy of the subacromial bursa. Open anterior acromioplasty as described by Neer has become accepted
| Shoulder Pain
651
as the procedure of choice for stage II and III impingement
lesions, with many investigators reporting high success rates
in treating impingement syndrome and rotator cuff tears.74-77
Reported results show good and excellent relief of symptoms
in 71% to 87% of patients treated by the open surgical
procedure.78-81
In 1985, Ellman45 described the technique of arthroscopic
subacromial decompression. His initial results46 and the
results of others are comparable with those of open surgical
techniques.47,82 Arthroscopic subacromial decompression
has become a widely accepted treatment for refractory stage
II and III impingement lesions. The procedure can be done
as outpatient surgery, and because no deltoid is detached, as
with the open technique, the procedure facilitates rehabilitation and increases overall recovery rates.
Calcific Tendinitis
Calcific tendinitis is a painful condition around the rotator
cuff that is associated with deposition of calcium salts, primarily hydroxyapatite.83-85 The cause of calcific tendinitis is
unknown. The commonly accepted cause is degeneration of
the tendon, which leads to calcification through a dystrophic process.85 A common clinicopathologic correlation is
seen in three distinct phases of the disease process: the
precalcific or formative phase, which can be relatively painless; the calcific phase, which tends to be quiescent and may
last months to years; and the resorptive or postcalcific phase,
which tends to be painful, as calcium crystals are resorbed.83
Although it is more common in the right shoulder, at least
a 6% incidence of bilaterality has been reported. Patients
with bilateral shoulder involvement often have the syndrome of calcific periarthritis, in which calcium hydroxyapatite crystals are found at multiple sites.86 Patients usually
present with impingement-type pain in the affected shoulder during overhead activity. The pain may seem to be out
of proportion to any objective physical findings. The patient
may describe difficulty sleeping on the shoulder and trouble
falling asleep. Symptoms may last a few weeks or a few
months.
The incidence of calcific tendinitis varies in the literature among asymptomatic individuals from 2.7% to 20%.
Most calcification occurs in the supraspinatus tendon, and
57% to 76.7% of patients are women. The average age of
patients is 40 to 50 years.83,87
Codman1 pointed out the localization of calcification
within the tendon of the supraspinatus. He provided a
detailed description of the symptoms and the natural history
of this condition. In describing the phases of pain, spasm,
limitation of motion, and atrophy, he noted the lack of correlation between symptoms and the size of the calcific
deposit. According to Codman, the natural history includes
degeneration of the supraspinatus tendon, calcification, and
eventual rupture into the subacromial bursa. During the
latter phase, pain and decreased motion can lead to adhesive capsulitis (see Figure 46-8).
Several factors may affect localization of calcium within
the supraspinatus. Many patients have an early stage of
impingement, which compresses the supraspinatus tendon
on the anterior portion of the acromion.9,19 This longstanding impingement may lead to local degeneration
of tendon fibers. In patients without impingement,
652
PART 6 | DIFFERENTIAL DIAGNOSIS OF REGIONAL AND DIFFUSE MUSCULOSKELETAL PAIN
localization of calcium within the supraspinatus may be
related to the blood supply of the rotator cuff, which normally is derived from an anastomotic network of vessels
from the greater tuberosity or from the bellies of the short
rotator muscles.84 The watershed of these sources is just
medial to the tendinous attachment of the supraspinatus.88
Rathburn and Macnab89 referred to this watershed as the
critical zone and pointed out that during abduction this area
was rendered ischemic.
Treatment of calcific tendinitis depends on the clinical
presentation and the presence of associated impingement.
Patients can have an acute inflammatory reaction that may
resemble gout. The acute inflammation can be treated with
local glucocorticoid injection, NSAIDs, or both. Ultrasound may be beneficial. If impingement is associated, treatment depends on the stage at presentation. The radiographic
appearance of the calcification can direct and perhaps
predict the response to therapy. In the resorptive state,
deposits appear floccular, suggesting that the process is in
the phase of repair, and that a conservative program is
indicated.
Patients with discrete calcification and perhaps associated adhesive capsulitis (see Figure 46-8) may be at a stable
phase, in which calcium produces a mechanical block and
is unlikely to be resorbed. For these patients, mechanical
removal of calcific deposits and correction of associated
pathologic lesions may be necessary.90-92 Percutaneous disruption of calcified areas may be performed using a needle
directed by fluoroscopy. This technique allows lavage and
injection, but does not treat associated impingement. Subacromial arthroscopy allows mechanical débridement of
calcific deposits under direct visualization. This technique
can be combined with arthroscopic removal of the inflamed
bursa and decompression of associated impingement.
Improved results have been noted with complete removal
of calcific deposits.93 In many cases of refractory calcific
tendinitis associated with impingement, open or arthro­
scopic acromioplasty, subacromial bursectomy, and decompression are indicated.
Rotator Cuff Tear
Pathophysiology
Spontaneous tear of the rotator cuff in an otherwise normal
individual is rare.19 It can occur in patients with rheumatoid
arthritis or systemic lupus erythematosus as part of the
pathologic process with invasion from underlying pannus.
Metabolic conditions such as renal osteodystrophy and
agents such as glucocorticoids occasionally are associated
with cuff tears. Most patients report a traumatic episode,
such as falling on an outstretched arm or lifting a heavy
object. The usual presenting symptoms are pain and weakness of abduction and external rotation. Crepitus and even
a palpable defect may be associated. Long-standing tears
generally are associated with atrophy of the supraspinatus
and infraspinatus muscles. It may be difficult to differentiate
a painful tendinitis from a partial-thickness or a small fullthickness cuff tear.
Controversy continues about the exact cause of cuff tendinopathy.88,92,94,95 Most likely, the pathophysiology involves
a combination of factors, including decreased vascularity
and cellularity of the tendon, along with changes in the
collagen fibers of the tendon that occur with aging.
Loss of motion with subsequent capsular tightness, particularly in the posterior capsule, may lead to cephalad
migration of the humeral head, with subsequent impingement of the cuff under the coracoacromial arch.96 Rehabilitation exercises stress regaining a normal range of motion.
To achieve full, painless motion, the normal relationship
of glenohumeral to scapulothoracic motion must be
achieved.16,17,97
Diagnosis
History. Patients with nontraumatic tears of the rotator
cuff report symptoms of chronic impingement. Loss of
motion and a feeling of stiffness are often noted with
extremes of motion, along with difficulty during activities
of daily living, such as combing the hair, hooking a bra
strap, putting on a shirt or coat, and reaching into the back
pocket. In chronic cases of cuff tendinopathy, loss of motion
usually occurs. Limitation of internal rotation occurs initially, is caused by posterior capsular contracture, and is
often associated with posterior shoulder pain with adduction of the ipsilateral shoulder. Further shoulder impingement occurs with forward flexion because of superior
migration of the humeral head against the anterior inferior
acromion. This upward translation is analogous to the
action of a yo-yo climbing on a string.96,98 Over time, loss
of forward flexion, abduction, and external rotation occurs
with passive and active motion of the shoulder.
Imaging. In acute cases, a history of trauma, such as
a fall onto the affected shoulder, may be reported. In
cases involving an anterior shoulder dislocation with subsequent profound weakness of the rotator cuff, a large cuff
tear or a greater tuberosity avulsion should be suspected,
in addition to axillary nerve palsy. In younger patients,
traumatic failure of the cuff under tensile overload may
result in cuff failure caused by forced adduction of the
affected shoulder or active abduction against resistance,
and this may occur with traumatic dislocation. Repetitive
tensile overload also can result in partial rotator cuff tears
in an overhead athlete.
Plain radiographs are used in initial evaluation of
impingement-type shoulder pain with cuff tendinopathy.
An impingement series should be ordered, including an
anteroposterior radiograph with a 30-degree cephalic tilt
(Rockwood view), which can reveal osteophytes of the
anterior os acromion and AC joint; a scapular Y view with
a 10-degree cephalic tilt (supraspinatus outlet view), which
can evaluate the type of acromion and reveal anterior and
AC osteophytes; and an axillary view, which can evaluate
the acromion for possible os acromionale. Calcific deposits
within the rotator cuff tendon can be viewed best with
rotational anteroposterior radiographs. Cuff arthropathy
should be suspected if the acromial-humeral distance is less
than 7 mm, or with the presence of cyst formation within
the greater tuberosity, humeral head osteopenia, sclerosis
around the greater tuberosity, or humeral head collapse. In
advanced stages of cuff arthropathy, complete loss of glenohumeral joint space may be seen with superior migration
and abutment of the humeral head against the undersurface
of the acromion.59
CHAPTER 46 In the past, shoulder arthrography was considered the
“gold standard” for diagnosing full-thickness and partialthickness rotator cuff tears, with greater than 90% sensitivity and specificity.33,99 Currently, arthrography with CT or
MRI is routinely used to diagnose rotator cuff pathology,
including full-thickness and partial-thickness tears.
Ultrasonography has been accurate in the diagnosis of
full-thickness rotator cuff tears.39,100-103 Ultrasonography
offers the advantages of being inexpensive and noninvasive,
but disadvantages include unproven effectiveness in determining subacromial impingement, capsular and labral
abnormalities, and partial cuff tears. The procedure and its
results are technician dependent. Ultrasonography may
have a useful role in determining the postoperative integrity
of the cuff repair.38
MRI has been invaluable in evaluating rotator cuff tears.
Sensitivity and specificity of MRI for diagnosing fullthickness cuff tears are 100% and 95%.104 Through the use
of gadolinium or saline, partial tears that are otherwise difficult to detect with conventional imaging can be detected.
Diagnosing cuff tears with MRI usually is based on discontinuity of the tendon on T1-weighted images and consistency with fluid signal on T2-weighted images. Ancillary
findings include fluid in the subacromial space on
T2-weighted images, loss of the subacromial fat plane on
T1-weighted images, and proliferative spur formation of the
acromion or AC joint. Large, chronic cuff tears also may be
associated with cephalad migration of the humeral head and
fatty atrophy of the spinatus muscle. Periarticular soft
tissues, including the capsulolabral complex and the biceps
tendon, as well as the rotator cuff can be thoroughly examined. The degree of tear and tendon retraction and evidence
of muscle atrophy can be evaluated, all of which are crucial
in preoperative planning for possible cuff repair.
Treatment
Nonsurgical Treatment. Codman and Akerson64 recommended early operative repair for acute full-thickness
rotator cuff tears and reported the first documented repair
in 1911. McLaughlin66 recommended early repair in cases
of grossly displaced tuberosity fractures or massive tears.
Several other clinical studies have supported the concept
that a full-thickness tear does not preclude good shoulder
function. DePalma105 reported that 90% of patients
with rotator cuff tears responded to conservative measures,
such as rest, analgesics, anti-inflammatory agents, and
physiotherapy.
The reported percentage of patients responding to nonsurgical treatment in the literature varies from 33% to
90%.3,18,106 Conservative treatment includes pain control
with NSAIDs, ultrasound, heat before shoulder stretching
and exercise, and ice after overhead activity. Deep massage
therapy is employed to reduce trigger point tenderness
within the trapezius, levator scapulae, and periscapular
muscles. Patients on long-term anti-inflammatory medications are monitored periodically for evidence of gastrointestinal bleeding and for hepatic or renal toxicity. Opiate-based
drugs are used only in the acute setting, such as after a fall,
or in the perioperative period.
Steroid and local anesthetic injections are used when the
patient has significant pain that prohibits rehabilitation.
| Shoulder Pain
653
Injections may be repeated once every 3 months if needed;
injection into the cuff tendon is to be avoided. If the patient
fails to improve after 3 months of conservative treatment,
or does not continue to improve after three sequential injections, surgical options should be discussed.
The mainstay of conservative therapy is exercise. Rehabilitation stresses pain relief with exercises aimed at restoring shoulder motion and strengthening remaining cuff
muscles, deltoid, and scapular stabilizers. Therapy can be
divided into three phases. The goals of the initial phase of
therapy are to relieve pain and restore shoulder motion.
Motion therapy includes pendulum exercises, passive
motion with use of a wand with assistance of the uninvolved
shoulder, an overhead pulley system, and posterior capsular
stretching. The arc of motion is gradually increased and is
guided by the patient’s discomfort to avoid painful impingement arcs.
The second phase of therapy is entered after the patient
has return of motion and little discomfort with overhead
activity. Emphasis is placed on strengthening the remaining
rotator cuff musculature and deltoid and periscapular
muscles. Strengthening with elastic surgical tubing provides
variable degrees of resistance, depending on the size of the
tubing. Initial strengthening is performed out of the
impingement arc (70 to 120 degrees of shoulder flexion).
The goal of this phase is to strengthen the shoulder
to prevent dynamic proximal humeral migration with
impingement during active shoulder elevation.59,61 Normal
shoulder kinematics relies on combined and synchronous
glenohumeral flexion and scapular rotation.60,92 In addition
to strengthening the cuff and deltoid, the scapular rotators,
including the trapezius and the serratus anterior muscles, are
emphasized.107
After the patient has successfully completed phase two
of the rehabilitation program with minimal symptoms and
good shoulder function, the final phase is entered. Phase
three is characterized by a gradual return to normal overhead activities, including work and sporting activities. This
part of the rehabilitation program should be tailored to the
individual patient’s needs and the demands placed on the
shoulder.
Surgical Treatment. A Cochrane review of the effectiveness of surgery for rotator cuff disease failed to reach any
firm conclusions about the effectiveness or safety of rotator
cuff surgery.108
Severity and duration of pain are the primary indications
for surgical intervention in a rotator cuff tear. Other factors
important in surgical decision making include shoulder
dominance, activity level, physiologic age, acuteness of
the tear, degree of tear, loss of function, amount of
tendon retraction, and fatty atrophy of the remaining cuff
musculature.
A systematic review of indications for rotator cuff surgery
found that earlier surgical intervention may be needed for
patients with cuff tears with weakness and significant functional disability. In addition, older chronologic age did not
portend a worse outcome; however, pending workman’s
compensation claims, it did negatively affect treatment
results.109
Acute Tears. Acute tears of the rotator cuff can be
treated with conservative measures of periscapular and cuff
strengthening along with capsular stretching to restore
654
PART 6 | DIFFERENTIAL DIAGNOSIS OF REGIONAL AND DIFFUSE MUSCULOSKELETAL PAIN
motion. Early surgical intervention should be considered in
a young patient, especially an overhead athlete. Conservative shoulder rehabilitation should be maintained for 3 to
6 months before a decision is made regarding surgery for an
older sedentary patient, in whom functional results without
surgery may be acceptable. Many older patients may function well with chronic cuff tears, but they may become
debilitated if an acute tear is superimposed on chronic
changes. Surgical intervention may be required in these
cases to return the patient to baseline function by repairing
the acute tear and attempting to repair the chronic tear if
possible.
Chronic Tears. For elderly patients whose pain and
weakness do not create a functional problem, a conservative
program is preferable for chronic tears. Pain unresponsive
to conservative management is the main indication for
surgery in an older patient with a chronic rotator cuff tear.
In these cases, surgery should be considered on an individual
basis after at least 3 months of conservative treatment,
including subacromial steroid injection. If the cuff tear is
massive and irreparable, débridement and subacromial
decompression may provide good pain relief without extensive surgery and prolonged immobilization.46,82,110-114 In a
younger patient with a chronic tear and weakness, surgery
to repair the cuff may be indicated to improve strength and
prevent further extension of the tear.112
In cases of rotator cuff arthropathy with glenohumeral
joint degeneration, a reverse total shoulder replacement
may be indicated. This type of total shoulder replacement
reverses the normal relationship between scapular and
humeral components, moving the center of rotation medially and distally to increase the lever arm length of the
deltoid muscle. The deltoid compensates for the deficient
rotator cuff, allowing as near-normal function as possible
(Figure 46-14). A recent publication also suggested reverse
Figure 46-14 Reverse total shoulder replacement in a 72-year-old man
who had severe cuff arthropathy.
total shoulder arthroplasty for the treatment of irreparable
rotator cuff tear with disability and no glenohumeral
arthritis.115
Bicipital Tendinitis and Rupture
The long head of the biceps passes through the bicipital
groove, crosses over the head of the humeral, and inserts on
the superior rim of the glenoid (see Figure 46-1A).116 The
biceps tendon aids in flexion of the forearm, supination of
the pronated forearm if the elbow is flexed, and forward
elevation of the shoulder.3 Bicipital tendinitis, subluxation
or dislocation of the biceps tendon within the bicipital
groove, and rupture of the long head of the biceps generally
are associated with anterior shoulder pain.
Bicipital tendinitis is sometimes an associated feature of
a rotator cuff tear. The rotator cuff tear compromises centering of the humeral head on the glenoid. This compromise
results in increased mechanical loading of the long head of
the biceps, which initiates a hypertrophic tendinitis.117
Dislocation of the long head of the biceps usually is
combined with a lesion of the subscapularis tendon.12 Isolated rupture of the long head of the biceps tendon is rare
when the rotator cuff is intact. Rupture of the long head of
the biceps is common, however, when a coexisting rotator
cuff tear is present.118 The effects of rotator cuff tear and
concomitant biceps tendon rupture on strength can be
substantial.12
Early phases of bicipital tendinitis are associated with
hypervascularity, edema of the tendon, and tenosynovitis.119
Persistence of this process leads to adhesions between the
tendon and its sheath, along with impairment of the normal
gliding mechanism in the groove. Stretching of the adhesions may be associated with chronic bicipital tendinitis.120
The diagnosis of bicipital tendinitis is based on localization
of tenderness. It is often confused with impingement symptoms and is frequently seen with an impingement syndrome.24 Isolated bicipital tendinitis can be differentiated
by the fact that the tender area migrates with the bicipital
groove as the arm is abducted and externally rotated. Many
eponyms are associated with tests to identify bicipital tendinitis.3 Yergason’s supination sign refers to pain in the
bicipital groove when the examiner resists supination of the
pronated forearm with the elbow at 90 degrees. Ludington’s
sign refers to pain in the bicipital groove when the patient
interlocks the fingers on top of the head and actively abducts
the arms.
Biceps tendon rupture can occur in some patients who
report no history of shoulder pain. Patients often complain
of an acute onset of pain and ecchymosis around the anterior shoulder and sagging of the biceps muscle belly. In these
cases, a concomitant rotator cuff injury should be excluded
by clinical examination. More often, the biceps tendon
rupture is preceded by painful shoulder symptoms that often
improve or disappear after the rupture.120,121
Treatment generally is conservative and consists of rest,
analgesics, NSAIDs, and local injection of glucocorticoids.
The use of ultrasound and a neuroprobe is more beneficial
in this condition than in isolated rotator cuff tendinitis.
Patients with refractory bicipital tendinitis and recurrent
symptoms of subluxation are treated by arthroscopic biceps
tenodesis or open tenodesis, that is, opening the bicipital
CHAPTER 46 groove and resecting the proximal portion of the tendon
with tenodesis of the distal portion into the groove or
beneath the pectoralis tendon.
Acromioclavicular Disorders
The AC joint is a common source of shoulder pain. Acute
causes of AC joint pain are often related to direct trauma
of the affected shoulder that may result in a distal clavicle
injury with an intra-articular chondral fracture, or in AC
joint instability from ligamentous disruption.122
Post-traumatic distal clavicle osteolysis, with resorption
of the distal clavicle, may ensue 4 weeks after a shoulder
injury, leading to AC joint pain.123,124 Osteolysis may be
caused by microfracture of the subchondral bone and subsequent attempts at repair.125 Other authors believe the
cause to be an autonomic nerve dysfunction affecting the
blood supply to the clavicle. The increased blood supply
leads to resorption of bone from the distal clavicle.123,126
More commonly, chronic osteolysis results from repetitive
microtrauma to the AC joint from activities such as weight
lifting, gymnastics, and swimming.125,127,128
The underlying pathophysiology is believed to be an
inflammatory process caused by stress fracture of the subchondral bone with hyperemic resorption of the distal
clavicle.125,129 Other causes of osteolysis include rheumatoid
arthrosis, hyperparathyroidism, and sarcoidosis, which
should be considered in the differential diagnosis, especially
in bilateral cases.123,124 Patients with atraumatic osteolysis of
the distal clavicle should be forewarned that bilateral
involvement may occur; an incidence of 70% was reported
for one long-term follow-up.130 Other chronic causes of AC
pain include idiopathic, intra-articular disk pathology, posttraumatic degenerative arthrosis from joint incongruity,
primary degenerative arthrosis, and rheumatoid arthrosis.
Evaluation should always include a detailed history,
physical examination, and radiographic evaluation. A
history of trauma to the AC joint from a direct fall or blow
to the ipsilateral shoulder may be reported. Less commonly,
the AC joint may have been injured indirectly, as during a
fall on the outstretched arm with forces transmitted through
the arm to the AC joint.122,131 Patients with osteolysis of the
distal clavicle sometimes give a history of acute trauma,
although the more common cause is repetitive microtrauma
to the AC joint caused by activities such as weight lifting
or gymnastics.123,124,127,128
Patients frequently complain of pain over the AC joint
when adducting the ipsilateral shoulder, such as during a
golf swing or when buckling a seat belt. Often, pain occurs
when sleeping on the affected shoulder. Athletes may experience AC joint pain on bench pressing, push-ups, and
dips.130,132,133 Pain and weakness of the affected shoulder also
may be experienced with forward flexion and adduction of
the arm.123
On physical examination, a visible step-off may be
observed between the medial acromion and the distal clavicle, indicating a probable AC separation. Pain usually can
be elicited on direct palpation of the AC joint and is made
worse by a cross-arm adduction maneuver. This test is performed by internally rotating the arm, which is maximally
adducted across the chest, and is considered positive if pain
is produced in the AC joint (see Figure 46-3D). Pain also
| Shoulder Pain
655
may be elicited by moving the arm from a horizontally
abducted position to the extended position and on maximal
internal rotation of the shoulder.132,134 These tests cause
rotation and compression of the AC joint and are sensitive
but less specific. They also may be positive with other
disorders of the shoulder, such as posterior capsular
stiffness.135
Frequently, AC joint pain coexists with subacromial
impingement and rotator cuff pathology. In these cases,
impingement signs are positive, and rotator cuff weakness
may be present. Otherwise, no muscle weakness should be
detectable on manual resistance testing, and no evidence of
muscle atrophy should be found.130,135,136 The AC joint and
the subacromial space may have to be injected on separate
occasions to determine the true source of the symptoms.
Some physicians have noticed an association of AC joint
symptoms with shoulder instability.130 Glenohumeral
motion can vary, depending on chronicity and isolation of
the problem to the AC joint. In isolated cases, some loss
of internal rotation of the affected shoulder may be caused
by pain.
Radiographs should include anteroposterior views of the
shoulder in the scapular plane in neutral, internal, and
external rotation; a transcapular Y view; an axillary view;
and a 15-degree cephalic tilt view of the AC joint at 50%
penetrance, as described by Zanca (see Figure 46-4).23 Stress
views may be obtained by strapping 5 to 10 lb of weight to
the forearms and determining AC separation. Comparing
the coracoclavicular distance of both shoulders also may be
helpful. When clinically indicated, cervical spine radiographs should be obtained to exclude cervical spondylosis.
Radiographic evaluation may reveal AC joint arthrosis
with microcystic changes in the subchondral bone, sclerosis,
osteophytic lipping, and joint space narrowing.137 In cases
of osteolysis, radiographs may reveal loss of subchondral
bone detail with microcystic appearances in the subchondral region of the distal clavicle and osteopenia of the
lateral one-third of the clavicle.124,125,127,128 In late stages of
osteolysis, resorption of the distal end of the clavicle results
in marked widening of the AC joint and sometimes complete resorption of the distal clavicle. AC separation may
be evident with widening of the coracoclavicular distance
and post-traumatic ossification of the coracoclavicular
ligaments.
AC symptoms do not always correlate with the radiographic appearance of the joint. DePalma138 found AC joint
degeneration to be an age-related process, with symptoms
not always correlating with radiographic findings of AC
joint arthrosis.23 AC joint pain may occur despite normal
radiographs.139
A technetium 99m phosphate bone scan may assist in
the diagnosis, revealing increased uptake in the distal clavicle and the medial acromion.125 In cases of atraumatic osteolysis of the distal clavicle, increased uptake may be isolated
to the distal clavicle, but in approximately 50% of cases,
scintigraphic activity of the adjacent medial acromion is
increased.130 The bone scan may reveal pathologic changes
in the AC joint when plain radiographs appear normal.
In selected cases, MRI can be valuable in determining a
diagnosis and evaluating the glenohumeral and subacromial
regions for coexisting pathology (Figure 46-15). AC joint
involvement may reveal increased fluid with synovitis, soft
656
PART 6 | DIFFERENTIAL DIAGNOSIS OF REGIONAL AND DIFFUSE MUSCULOSKELETAL PAIN
clavicle has been described with results similar to open
resection.13,129,134-136,143-146
Glenohumeral Disorders
Figure 46-15 Sagittal section magnetic resonance imaging of the
shoulder in a 32-year-old weight lifter complaining of shoulder pain.
Fat-suppressed proton density fast spin echo images of bursal-side highgrade partial cuff tear (arrowheads).
The various arthritides that affect the shoulder joint are
discussed in detail in other chapters. They are presented
here to address aspects that are unique to the glenohumeral
joint. The usual presentation of intra-articular disorders
consists of pain with motion and symptoms of internal
derangement, such as locking and clicking. Pain is generalized throughout the shoulder girdle and sometimes is referred
to the neck, back, and upper arm. The usual response to
pain includes decreased glenohumeral motion and substitution with increased scapulothoracic mobility. Patients with
adequate elbow and scapulothoracic motion require little
glenohumeral motion for activities of daily living; patients
with glenohumeral arthrodesis can achieve adequate function.147,148 The response to pain consists of diminution of
motion and secondary soft tissue contractures with muscle
atrophy. With increasing weakness and involvement of
adjacent joints, pain, limitation of motion, and weakness
can cause a substantial functional deficit.
Inflammatory Arthritis
tissue enlargement, and periarticular ossifications with
encroachment on underlying bursal and cuff tissue.
Patients with AC joint pain usually respond well to nonoperative treatment; however, complete relief of symptoms
may require an extended period. Conservative therapy
includes heat, NSAIDs, steroid injections, shoulder rehabilitation, and avoidance of painful positions and activities.
Steroid injections are repeated at 3-month intervals if
painful conditions persist.
Open resection of the distal clavicle for chronic AC
joint pain was initially reported by Gurd140 and by
Mumford,141 both with good results. Since that time, other
surgeons have reported similar good results with open resection, but significant morbidity, such as disruption of the
deltotrapezial fascia and anterior deltoid rupture, can
occur.123,124,137,139,142 Arthroscopic resection of the distal
A
Although the most common inflammatory arthritis involving the shoulder joint is rheumatoid arthritis (RA), other
systemic disorders, such as systemic lupus erythematosus,
psoriatic arthritis, ankylosing spondylitis, reactive arthritis,
and scleroderma, may cause glenohumeral degeneration.
Motion is limited by splinting of the joint with secondary
soft tissue contractures, or by primary soft tissue involvement with scarring or rupture. Plain radiographs confirm
glenohumeral involvement (Figure 46-16A). Narrowing of
the glenohumeral joint space may occur, with erosion and
cyst formation and without significant sclerosis or osteophytes. As the disease progresses, superior and posterior
erosion of the glenoid with proximal subluxation of the
humeral head may occur. Eventually, secondary degenerative changes and even osteonecrosis of the humeral head
may occur.
B
Figure 46-16 Plain radiographs. A, Rheumatoid arthritis with loss of joint space, cyst formation, glenohumeral erosion, and early proximal subluxation
of the humerus, indicating a rotator cuff tear. B, Osteoarthritis with narrowing of the glenohumeral joint space, sclerosis, and osteophyte formation.
Notice the preservation of the subacromial space, suggesting an intact rotator cuff.
CHAPTER 46 Treatment is initially conservative and is directed toward
controlling pain, inducing a systemic remission, and maintaining joint motion through physical therapy. The use of
intra-articular glucocorticoids may be beneficial in controlling local synovitis. In rheumatoid arthritis, the involvement of periarticular structures with subacromial bursitis
and rupture of the rotator cuff magnifies the functional
deficit. When synovial cartilage interactions produce significant symptoms and radiographic changes that cannot be
controlled by conventional therapy, glenohumeral resurfacing should be considered.
When following an RA patient with shoulder involvement, the rheumatologist should assess range of motion
carefully and should obtain periodic radiographs. Patients
with progressive loss of motion or radiographic destruction
should be referred for evaluation for possible surgical treatment. The treatment of choice is an unconstrained total
shoulder arthroplasty.149,150 Total shoulder arthroplasty is
best performed in patients with rheumatoid arthritis before
end-stage bony erosion and soft tissue contractions have
occurred.151,152 Acute inflammatory arthritis of the glenohumeral joint may be associated with gout, pseudogout,
hydroxyapatite deposition of renal osteodystrophy, and
recurrent hemophilic hemarthrosis.
Osteoarthritis
Osteoarthritis of the glenohumeral joint is less common
than that in the hip, its counterpart in the lower
extremity; this condition is caused by non–weight-bearing
characteristics of the shoulder joint and the distribution of
forces throughout the shoulder girdle. Osteoarthritis is
divided into conditions associated with high unit loading of
articular cartilage and conditions in which an intrinsic
abnormality within the cartilage causes abnormal wear at
normal loads. Because the shoulder is normally a non–
weight-bearing joint and is not usually susceptible to
repeated high loading, the presence of osteoarthritis of the
glenohumeral joint should alert the physician to consider
other factors. Has the patient engaged in unusual activities,
such as boxing, heavy construction, or long-term use of a
pneumatic hammer? Has some disorder, such as epiphyseal
dysplasia, created joint incongruity with high unit loading
of the articular cartilage? Is this a neuropathic process
caused by diabetes, syringomyelia, or leprosy? Have associated hemochromatosis, hemophilia, or gout altered the
ability of articular cartilage to withstand normal loading? Is
unrecognized chronic dislocation responsible?
Pain is the usual presentation, but generally it is not as
acute or it may be associated with the spasm seen in inflammatory conditions. Plain radiographs show narrowing of the
glenohumeral joint, osteophyte formation, sclerosis, and
some cyst formation (Figure 46-16B). Because the rotator
cuff usually is intact, less bone erosion of the glenoid and
proximal subluxation of the humerus is noted. Patients with
osteoarthritis of the glenohumeral joint frequently do well
with functional adjustments and conservative therapy.
Analgesics and NSAIDs may provide symptomatic relief.
The use of glucocorticoid injections is less beneficial, unless
evidence of synovitis is observed. Patients with severe
involvement who fail to respond are best treated by shoulder arthroplasty.149-152
| Shoulder Pain
657
Osteonecrosis
Osteonecrosis of the shoulder refers to necrosis of the
humeral head seen in association with a variety of conditions. Symptoms are due to synovitis and joint incongruity
resulting from resorption, repair, and remodeling. Pathogenesis and various causes are discussed in Chapter 103.
The most common cause of osteonecrosis of the shoulder
is avascularity resulting from a fracture through the anatomic neck of the humerus.153 Fracture through this area
disrupts intramedullary and capsular blood supplies to the
humeral head.154 Another common cause of osteonecrosis
of the shoulder is steroid therapy provided in conjunction
with organ transplantation, systemic lupus erythematosus,
or asthma. Other conditions associated with osteonecrosis
of the humeral head include hemoglobinopathies, pancreatitis, and hyperbarism.
Early diagnosis is difficult because the presence of symptoms is often delayed. Bone scans may be helpful in early
cases, before radiographic changes are evident. MRI is
highly sensitive and is more specific than scintigraphy. Plain
radiographs show progressive phases of necrosis and repair
(as discussed in Chapter 103). In early stages, the films
may be normal or may show osteopenia or bone sclerosis.
A crescent sign representing subchondral fracture or
demarcation of the necrotic segment appears during the
reparative process. Patients who fail to remodel show collapse of the humeral head with secondary degenerative
changes. A considerable discrepancy is often noted between
symptoms and radiographic involvement. Patients with
extensive bone changes may be asymptomatic. Treatment
should be directed by the patient’s symptoms rather than by
the radiographs and is similar to that provided for osteoarthritis. Arthroscopy occasionally is helpful by removing
loose chondral fragments and débriding chondral incongruities.155 Patients with severe symptoms that cannot be controlled by conservative means are best treated with
unconstrained shoulder arthroplasty, hemiarthroplasty, or
resurfacing arthroplasty.149
Cuff-Tear Arthropathy
In 1873, Adams described the pathologic changes that characterize rheumatoid arthritis of the shoulder and a condition
that has since that time been referred to as Milwaukee shoulder or cuff-tear arthropathy.156 McCarty called the condition
Milwaukee shoulder and reported that factors predisposing
to this syndrome included deposition of calcium pyrophosphate dihydrate crystals, direct trauma, chronic joint
overuse, chronic renal failure, and denervation.157 Patients
with Milwaukee shoulder have elevated levels of synovial
fluid 5-nucleotidase activity and elevated levels of synovial
fluid inorganic pyrophosphate and nucleotide pyrophosphohydrolase activity.158
Neer and colleagues159 reported a similar condition in
which untreated massive tears of the rotator cuff with proximal migration of the humeral head are associated with
erosion of the humeral head. Erosion of the humeral head
differs from that seen in other arthritides and is presumed
to be caused by a combination of mechanical and nu­
tritional factors acting on the superior glenohumeral
cartilage.
658
PART 6 | DIFFERENTIAL DIAGNOSIS OF REGIONAL AND DIFFUSE MUSCULOSKELETAL PAIN
Patients with cuff-tear arthropathy present a difficult
therapeutic problem because bone erosion and disruption of
the cuff jeopardize the functional result from an unconstrained prosthesis.151 Hemiarthroplasty or a reverse total
shoulder arthroplasty may be indicated.160,161 The major
challenge in treating cuff-tear arthropathy is to determine
which patients with massive rotator cuff tears will proceed
to the syndrome of cuff-tear arthropathy. Patients with
massive rotator cuff tears who develop localized calcium
pyrophosphate disease may be predisposed to further proximal migration and further joint destruction. This situation
poses a dilemma for the treating physician. Many patients
with massive rotator cuff tears remain stable and require
little or no treatment. Occasionally, symptomatic patients
can be treated by arthroscopic débridement of the cuff tear.
In a recent study, patients with massive rotator cuff tears
without arthritis did well when treated with reverse total
shoulder arthroplasty.115 It is crucial to define the patient
who will proceed to the syndrome of cuff-tear arthropathy.
If crystal deposition disease predisposes patients to proximal
migration and joint destruction, joint aspiration with crystal
analysis and scintigraphy to determine synovial reaction
may be helpful diagnostic tools.
Hamada and co-workers162 followed 22 patients with
massive rotator cuff tears treated conservatively. Radiographic findings included narrowing of the acromiohumeral
interval and degenerative changes in the humeral head,
tuberosities, acromion, AC joint, and glenohumeral joint.
Five of seven patients followed for longer than 8 years progressed to cuff-tear arthropathy. Investigators concluded
that progressive radiographic changes were associated
with repetitive use of the arm in elevation, rupture of the
long head of the biceps, impingement of the humeral
head against the acromion, and weakness of external
rotation.162
Septic Arthritis
Septic arthritis can masquerade as any of the conditions
classified as periarticular or glenohumeral disorders (see
Chapters 99 and 110). Sepsis must be included in any differential diagnosis of shoulder pain because early recognition and prompt treatment are necessary to achieve a good
functional result. The diagnosis is confirmed by joint aspiration with synovial fluid analysis and culture. Cultures should
include aerobic, anaerobic, mycobacterial, and fungal
studies.
Labral Tears
The glenoid labrum increases the depth of the glenoid and
serves as an anchor for the attachment of the glenohumeral
ligaments. Historically, labral tears have been difficult to
diagnose. Findings on physical examination can be confused
with impingement and rotator cuff tendinopathy and bicipital tendinitis. Diagnosis can be confirmed with MRIarthrography, CT-arthrography, and DCAT.27 Arthroscopy
has greatly increased our knowledge of the glenoid labrum
in normal and pathologic situations and has aided clinicians
in the diagnosis and treatment of labral lesions.
Labral tears can be divided into tears associated with
symptoms of internal derangement and tears associated with
anterior or posterior instability. A soft tissue Bankart lesion
is associated with a tear of the anterior band of the inferior
glenohumeral ligament and with anterior instability. Isolated labral tears that do not involve detachment of the
ligaments can cause internal derangement and may have an
arthroscopic appearance similar to that of a meniscal tear
of the knee.
Andrews and associates7 first described lesions of the
anterior superior labrum in throwing athletes; these lesions
were often associated with biceps tendon tears (10%),
which may result from traction of the biceps tendon.
Snyder and co-workers163 introduced the term SLAP lesion
in 1990 to describe an injury involving the long head
of the biceps tendon and the superior portion of the
glenoid labrum.
The long head of the biceps tendon originates at the
supraglenoid tubercle and the glenoid labrum in the
superior-most portion of the glenoid. The major portion of
the tendon blends with the posterior superior aspect of the
labrum. The most common mechanism of a SLAP injury is
a fall onto an outstretched arm with the shoulder in abduction and slight forward flexion.163 The lesion also can result
from acute traction on the arm and from an abduction and
external rotation mechanism.164,165
Patients usually complain of pain with overhead activities and a frequent catching or popping sensation in the
shoulder. The most reliable diagnostic test is O’Brien’s test.
The test is performed against resistance with the arm in
forward flexion and with the elbow extended and the
forearm pronated. In the second part of the test, the arm is
supinated. Less pain during the latter part of the test suggests a SLAP lesion.163 The most accurate diagnostic test is
MRI-arthrography with gadolinium.166 Treatment for symptomatic SLAP lesions is surgical.
Adhesive Capsulitis
Adhesive capsulitis, or frozen shoulder syndrome (FSS), is
a condition characterized by limited motion of the shoulder
joint with pain at the extremes of motion. It was first
described by Putman167 in 1882 and later by Codman.1 The
initial presentation is pain, which is generalized and is
referred to the upper arm, back, and neck. As pain increases,
loss of joint motion ensues. The process generally is selflimiting and in most cases resolves spontaneously within 10
months, unless an underlying problem is present.
The exact cause of FSS is unknown.92,168 It is frequently
associated with conditions such as diabetes mellitus, parkinsonism, thyroid disorders, and cardiovascular disease. When
one of these conditions exists, a history of some mild trauma
that initiated the frozen shoulder is often reported. Major
skeletal trauma and soft tissue injury may coexist with FSS.
It also may be seen with a variety of other conditions,
including apical lung tumor, pulmonary tuberculosis, cervical radiculopathy, and post myocardial infarction.169-171 In
one review of FSS, 3 of 140 patients with this syndrome had
local primary invasive neoplasms.172 Another study described
3 patients with adhesive capsulitis who subsequently were
found to have a neoplastic lesion of the midshaft of the
humerus.173 In a high-risk patient with an underlying disorder, even minor surgery or trauma in a remote location, such
as the hand, can precipitate FSS.92,174,175
CHAPTER 46 The pathophysiology involves a diffuse inflammatory
synovitis with subsequent adherence of the capsule and loss
of the normal axillary pouch and joint volume, which leads
to significant loss of motion. Capsular contracture is thought
to result from adhesion of the capsular surfaces or fibroblastic proliferation in response to cytokine production.168,174,176
The condition is common in women in their 40s and 50s.
Typically, the patient relays a history of diffuse, dull aching
around the shoulder, with weakness and loss of motion
occurring over a few months.
Usually, three distinct clinical stages of the syndrome
can be identified. Stage one is the painful inflammatory or
freezing phase. During this stage, pain is severe, is exacerbated by any attempts at movement, and usually lasts a few
weeks or months. The patient usually feels most comfortable with the arm at the side in an adducted and internally
rotated position. Phase two, the adhesive or stiffening
phase, generally lasts 4 to 12 months. Pain is usually
minimal during this phase, although periscapular symptoms
may develop from compensatory motion to achieve elevation of the arm. The third phase of the syndrome is the
resolution or thawing phase, which may last 5 to 26 months.
During this time, pain eases and motion slowly improves,
although some patients may improve dramatically over a
short period.177
In the early stages, any attempts at motion may produce
severe pain and associated weakness. The syndrome usually
is associated with a prolonged period of immobilization.178
Night pain is common, along with an inability to sleep on
the associated shoulder; this is similar to findings of impingement syndrome.
In patients with a history of minimal or no trauma and
FSS, a metabolic cause should be excluded. Complete blood
cell count, erythrocyte sedimentation rate, serum chemistry,
and thyroid function tests are done as a screening panel.
Further testing is done if results suggest that the patient may
have a systemic illness. Plain radiographs should include
true anteroposterior, axillary, and scapular Y views of the
shoulder. In patients with no underlying detectable illness
and a negative workup, a Tc 99m pertechnetate scan may
show increased uptake in FSS, but more important, it is used
to exclude occult lesions or metastasis.179
Literature review reveals a multitude of treatment options
along with significant deficits on accurate reporting of
disease staging with response to treatment.180
Treatment of FSS is mainly conservative and consists of
intra-articular injections, heat, gentle stretching, NSAIDs,
and modalities such as transcutaneous electrical nerve stimulation. The disease usually is self-limited and after the
painful phase is not severely disabling. Communication
between the physician and the patient, together with a
thorough explanation of the condition, is essential because
resolution of the syndrome occurs slowly over time. Closed
manipulation and surgery (open and arthroscopic) are
reserved for patients whose condition is recalcitrant to conservative measures, or for whom the diagnosis is in question.
Paramount in the prevention of FSS is avoiding overimmobilization in a minor shoulder injury, in addition to
careful identification of patients at risk for FSS.
Fareed and Gallivan181 reported good results with hydraulic distention of the glenohumeral joint using local anesthetic agents. Rizk and associates182 conducted a prospective,
| Shoulder Pain
659
randomized study to assess the effects of steroid or local
anesthetic injection in 48 patients with FSS. No significant
difference in outcome was noted between individuals who
received intrabursal or intra-articular injection. Steroid
with lidocaine offered no advantage over lidocaine alone in
restoring shoulder motion. However, transient pain relief
occurred in two-thirds of steroid-treated patients.182
General anesthesia occasionally is indicated for closed
manipulation. Hill and Bogumill183 reported the results of
manipulation of 17 frozen shoulders in 15 patients who did
not respond to physical therapy. On average, 78% of individuals who were working before their shoulder problems
returned to work 2.6 months after manipulation. Investigators concluded that manipulation allowed patients to return
to a normal lifestyle and to work sooner than the reported
natural history of the condition.183 Surgical intervention for
adhesive capsulitis should be limited to treatment of an
underlying problem, such as calcific tendinitis or an impingement syndrome.
Glenohumeral Instability
Glenohumeral instability is a pathologic condition that
manifests as pain associated with excessive translation of
the humeral head on the glenoid during shoulder motion.
Instability can range from excessive laxity with episodes of
subluxation to frank dislocation of the joint. Traumatic
dislocation of the glenohumeral joint reveals characteristic
clinical and radiographic findings that are beyond the scope
of this chapter and have been reviewed in detail elsewhere.184 The most common type of instability is anterior,
although posterior and multidirectional laxity of the shoulder is increasingly recognized as a cause of shoulder pain.
Anterior dislocation usually occurs with the arm in an
abducted and externally rotated position, and the diagnosis
is usually obvious. Posterior dislocation is frequently associated with convulsive disorders or unusual trauma with the
arm in a forward flexed and internally rotated position. The
diagnosis is often missed and should always be suspected in
the patient who is unable to rotate the arm externally after
trauma.
Recurrent subluxation without dislocation may be difficult to diagnose and may be mistakenly identified as
impingement with chronic cuff tendinitis. An overhead
athlete may experience repetitive stresses to the shoulder,
causing microtrauma to the static stabilizers. Jobe and colleagues21 described a syndrome of shoulder pain in overhead
or throwing athletes that manifests as impingement but is
caused by anterior subluxation of the joint, with the humeral
head impinging on the anterior aspect of the coracoacromial arch. Fu and co-workers185 underscored this distinction
by dividing the causes of rotator cuff tendinitis into primary
impingement of the tendon on the coracoacromial arch and
anterior subluxation with secondary impingement in young
athletes performing overhead movements. Walch and colleagues186 described intra-articular impingement between
the undersurface of the rotator cuff (supraspinatus and infraspinatus) and the posterior superior glenoid rim and labrum.
This “internal impingement” usually is observed in overhead athletes with subtle anterior glenohumeral instability
and results in tendinitis or partial tears of the rotator cuff
(see Figure 46-16).
660
PART 6 | DIFFERENTIAL DIAGNOSIS OF REGIONAL AND DIFFUSE MUSCULOSKELETAL PAIN
The diagnosis of glenohumeral instability with subluxation in one or multiple directions is made with the combination of a detailed history and physical examination and
the use of adjuncts, such as arthrography, CT, MRI, and
arthroscopy with examination under anesthesia. The syndrome of multidirectional instability has been recognized in
patients with symptomatic inferior instability, in addition
to anterior or posterior instability. Approximately 50% of
affected patients have evidence of generalized laxity. Frequently, the syndrome occurs in young athletic patients who
are loose jointed, in particular in the dominant arm of
pitchers, racket sports players, and swimmers. In this type
of athlete, repetitive microtrauma may cause stretching of
the shoulder, resulting in a large capsular pouch without
labral detachment. A traumatic event may damage the
shoulder, resulting in the syndrome of multidirectional
instability and a Bankart lesion.187
The most common manifestation in these patients is
pain, which is often mistakenly considered to be rotator cuff
tendinitis. The patient may relate a history of minor trauma
causing acute pain and a “dead arm” syndrome lasting
minutes or hours. Other associated symptoms include a
sense of instability, weakness, and radicular symptoms suggestive of neuropathy. Few or no positive physical findings
may be associated with chronic subluxation or multidirectional instability. The patient may have signs of generalized
ligamentous laxity, and pain may be reproduced by subluxating the glenohumeral joint in multiple directions. One
particularly helpful sign of inferior laxity is the sulcus sign,
which refers to the subacromial indentation that occurs
when longitudinal traction is applied to the humerus with
the arm at the side. This sign occurs with inferior translation of the humeral head. Because this syndrome frequently
occurs in athletes with highly developed musculature
around the shoulder girdle, physical findings of subluxation
may be difficult to reproduce in the office setting.
Plain radiographs are generally normal, although some
inferior subluxation may be shown on stress radiographs
obtained with the use of weights. Special radiographs, as
discussed previously, may show a Bankart lesion (i.e., avulsion of the anterior inferior glenoid rim) or a Hill-Sachs
lesion (i.e., osteochondral defect of the posterior humeral
head) with subluxation of the humeral head in front of the
anterior glenoid rim. CT-arthrography or MRI-arthrography
may show increased capsular volume, a labral detachment,
or a Hill-Sachs lesion (see Figure 46-9). When surgery is
indicated, examination under anesthesia and shoulder
arthroscopy may assist in diagnosing the primary direction
of instability in the syndrome of multidirectional instability.
In selected patients with traumatic anterior dislocation who
have no history of multidirectional instability, arthroscopic
stabilization may be done with stabilization of the capsulolabral complex.
Treatment of patients with chronic subluxation or the
syndrome of multidirectional instability is first directed
toward prolonged rehabilitation. Activities that stress the
shoulder and produce symptoms are avoided. Strengthening
exercises of the shoulder girdle may control symptoms,
dynamically stabilizing the glenohumeral joint, and may
obviate the need for surgical intervention. If a conservative
treatment program fails, surgery is performed on the side
associated with the greatest clinical instability. Stabilization
is directed toward tightening of the capsular structures to
stabilize the glenohumeral joint.187,188
EXTRINSIC OR REGIONAL FACTORS
CAUSING SHOULDER PAIN
Because the shoulder girdle connects the thorax with the
upper extremity, and because major neurovascular structures
pass in proximity to the joint, shoulder pain is a hallmark
of many nonarticular conditions.
Cervical Radiculopathy
Cervical pathology may manifest with associated shoulder
pain. The area of referred pain has a dermatomal pattern,
consistent with the distribution of dermatomal nerve roots.
Isolation of the pain usually defines the exact location of
associated cervical pathology. Pain can be differentiated
from shoulder pain on the basis of history, physical examination, EMG, cervical radiographs, and myelography or MRI
when indicated. Because conditions causing cervical neck
pain and conditions causing shoulder pain, such as calcific
tendinitis and cervical radiculopathy, may coexist, it is often
difficult to distinguish which lesion is responsible for the
symptoms. These conditions often can be differentiated by
injection of local anesthetics to block certain components
of the pain.
The thoracic outlet is an interval created by the anterior
and middle scalene muscles and the first rib through which
the brachial plexus and vessels pass to the arm. In thoracic
outlet syndrome, compression of these nerves and vessels
often manifests as vague shoulder pain with numbness of
the ipsilateral fourth and fifth digits. Cervical rib or hypertrophy of the scalene muscles can be related to the onset of
pain.189-191 The occurrence of pain also has been related to
scapular ptosis, poor posture, and clavicular fracture with
malunion or copious formation of callus.
Brachial Neuritis
In the 1940s, Spillane192 and Parsonage and Turner193,194
described a painful condition of the shoulder associated
with limitation of motion. As pain subsided and motion
improved, muscle weakness and atrophy became apparent.
The deltoid, supraspinatus, infraspinatus, biceps, and triceps
are the most frequently involved muscles,195 although diaphragmatic paralysis also has been reported.194,196 The cause
is unclear, but the clustering of cases suggests a viral
or postviral syndrome.193,194 Occasionally, an associated
influenza-like syndrome or previous vaccination has been
reported.195
Hershman and colleagues197 described acute brachial
neuropathy in athletes. Findings that suggest an acute brachial neuropathy include acute onset of pain without
trauma; persistent, severe pain that continues despite rest;
and patchy neurologic signs. The diagnosis is confirmed by
EMG and nerve conduction studies.197 The prognosis for
recovery is excellent, although full recovery may take 2 to
3 years. Tsairis and associates198 reported 80% recovery
within 2 years and more than 90% recovery by the end of
3 years.
CHAPTER 46 Nerve Entrapment Syndromes
Peripheral compression neuropathies of the upper extremities may produce referral pain to the shoulder. Distant compression neuropathies, such as carpal tunnel (median nerve)
and cubital tunnel (ulnar nerve) syndromes, may manifest
with concomitant and separate shoulder impingement with
rotator cuff disease. Associated numbness and paresthesias
with mapping of the dermatomal distribution and with
peripheral neuropathy often direct the examiner to the
appropriate diagnosis. Patients often give a history of dropping objects and a feeling of clumsiness with the affected
hand. A Tinel sign may be elicited over the region of entrapment at the elbow or wrist. Provocative maneuvers such as
Phalen’s test may be positive and usually indicate median
nerve compression at the wrist. Diminished vibratory sensation is an early finding in the disease and is easily reproducible,199,200 whereas decreased two-point discrimination and
intrinsic atrophy are late findings of peripheral compression
neuropathy.199
The diagnosis usually can be made by clinical examination with exclusion of other possible causes. EMG and nerve
conduction velocity tests may reveal slowed conduction and
latency at appropriate compression points to aid in diagnosis. Spinal accessory nerve injury with subsequent denervation of the trapezius may cause weakness and pain in the
shoulder consistent with impingement. The injury can
occur from traction injury to the neck or a direct blow or
pressure to the base of the neck. Iatrogenic nerve injury may
result from surgical procedures on the neck such as lymph
node biopsy.201 The injury produces weakness in shoulder
abduction with associated pain that radiates from the neck
into the trapezius and shoulder. Subsequent atrophy of the
trapezius may lead to dyssymmetry and ptosis of the involved
shoulder, with narrowing of the supraspinatus outlet and
secondary impingement with shoulder pain. Definitive diagnosis can be made by EMG examination.
Early treatment is conservative. If return of function is
not evident at 6 months, surgical exploration of the nerve
with possible tendon transfers may be indicated.202
Injury to the long thoracic nerve (cervical fifth, sixth,
and seventh roots) can lead to scapular winging. The resultant scapular dysrhythmia and weakness can lead to a
painful shoulder that may mimic rotator cuff disease.201
Patients also complain of pain and discomfort with active
forward flexion of the shoulder. Patients who remain symptomatic after conservative treatment may require surgery for
scapulothoracic fusion or tendon transfer with use of the
pectoralis major or minor to stabilize the scapula.203,204
In quadrilateral space syndrome, the axillary nerve is
compressed by fibrous bands in the quadrilateral space.201,205,206
This syndrome typically occurs when the arm is held in
abduction and external rotation, with subsequent tightening of fibrous bands across the nerve.207 It is most commonly
seen in the dominant shoulder of young athletic individuals
such as pitchers, tennis players, and swimmers who function
with excessive overhead activity. Pain may occur throughout the shoulder girdle and may radiate down the arm in a
nondermatomal pattern. Neurologic and EMG testing may
be normal. Diagnosis often is made by an arteriogram of
the subclavian artery. A positive arteriogram reveals compression of the posterior humeral circumflex artery as it
| Shoulder Pain
661
traverses the quadrangular space when the arm is in the
abducted and externally rotated position. Surgical intervention may be required to release the fibrotic bands or the
tendon of the teres minor if the patient fails conservative
treatment.201,208
Suprascapular nerve entrapment syndrome can be caused
by a traction lesion resulting from repetitive overhead activities, a compression lesion, or both, to the nerve, caused by
tethering of the nerve at the suprascapular notch by the
suprascapular ligament, or the spinoglenoid notch by the
transverse ligament. It also can result from direct compression of a space-occupying lesion, such as a ganglion or a
lipoma. Rengachary and co-workers209 described variations
in size and shape of the suprascapular notch that may predispose the nerve to entrapment. Several authors have
noted an association of suprascapular neuropathy with
massive rotator cuff tears, presumably resulting from a traction injury to the nerve.210,211
The resulting suprascapular neuropathy produces pain in
the posterolateral aspect of the shoulder that may radiate
into the ipsilateral extremity, shoulder, or side of the neck.
Although this condition is uncommon, it can have a prolonged and disabling course when undiagnosed. Because the
suprascapular nerve has no cutaneous innervation, no
numbness, tingling, or paresthesias are associated. Weakness
is usually noted in abduction and external rotation, and
significant atrophy is often observed at diagnosis. The pain
frequently is described as a deep burning or aching that can
be well localized and often can be elicited by palpation over
the region of the suprascapular notch. Any activity that
brings the scapula forward, such as reaching across the
chest, may aggravate the pain.212 The location of pain and
other symptoms can mimic more common entities, such as
impingement, rotator cuff disease, cervical disk disease, brachial neuropathy, biceps tendinitis, thoracic outlet syndrome, AC disease, and instability of the shoulder.213
Fritz and colleagues214 reported the efficacy of MRI in the
diagnosis of suprascapular nerve entrapment secondary to
space-occupying lesions. Definitive diagnosis is made with
EMG and nerve conduction studies. EMG changes usually
reveal spontaneous activity in the muscle at rest and fibrillations indicating motor atrophy and denervation. Nerve
conduction studies may reveal slowing across the site of
entrapment. As with axillary nerve entrapment, the syndrome is often associated with young, athletic individuals
with excessive overhead activity.215 It also has been associated with trauma.213,216,217
Lack of consensus continues regarding the optimal treatment of suprascapular neuropathy.6,213,215,218-220 Post and
Grinblat218 reported good to excellent results with surgical
treatment in 25 of 26 cases. No difference in residual
atrophy and in strength deficits has been shown, however,
for operative and nonoperative treatments. Ferretti and coworkers215 evaluated 96 top-level volleyball players from the
1985 European Championships and found that 12 had isolated suprascapular neuropathy with atrophy of the infraspinatus of the dominant shoulder. All players were unaware
of any impairment, however, and played without limitations. After a space-occupying lesion has been excluded, a
6-month trial of conservative treatment may be indicated
for some individuals. If the entrapment does not improve,
or if symptoms worsen with conservative treatment, surgical
662
PART 6 | DIFFERENTIAL DIAGNOSIS OF REGIONAL AND DIFFUSE MUSCULOSKELETAL PAIN
decompression for pain relief is warranted; however, resolution of atrophy and strength gains can vary.213
Sternoclavicular Arthritis
Occasionally, traumatic, nontraumatic, or infectious conditions can cause pain around the sternoclavicular joint (see
Figure 46-1). The most common problem involves ligamentous injury and painful subluxation or dislocation. This can
be diagnosed by palpable instability and crepitus over the
sternoclavicular joint. Sternoclavicular views may radiographically show dislocation.221
Inflammatory arthritis of the sternoclavicular joint has
been associated with rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, and septic arthritis. The association of palmoplantar pustulosis with sternoclavicular
arthritis has been reported.222 Seven of 15 patients who
underwent biopsy for this condition had cultures positive
for Propionibacterium acnes, suggesting an infectious origin
of the condition.222
Two other conditions involving the sternoclavicular
joint are Tietze’s syndrome, a painful, nonsuppurative swelling of the joint and adjacent sternochondral junctions, and
Friedrich’s syndrome, a painful osteonecrosis of the sternal
end of the clavicle.3 Condensing osteitis of the clavicle is a
rare benign idiopathic lesion of the medial one-third of the
clavicle. This condition, which is better described as aseptic
enlarging osteosclerosis of the clavicle, is most commonly
seen in middle-aged women and manifests as a tender swelling over the medial one-third of the clavicle.223
Reflex Sympathetic Dystrophy
Since its original description by Mitchell224 in 1864, reflex
sympathetic dystrophy (RSD) has remained a poorly understood and frequently overlooked condition. Its cause is
unknown but may be related to sympathetic overflow or
short-circuiting of impulses through the sympathetic system.
Any clinician who deals with painful disorders must be
familiar with the diagnosis and treatment of this condition.
Bonica’s225 excellent review covers the clinical presentation, various stages of the disease, and the importance of
early intervention to ensure a successful outcome.
RSD has been called causalgia, shoulder-hand syndrome,
and Sudeck’s atrophy, which has caused some confusion. It
is generally associated with minor trauma and is to be differentiated from causalgia, which involves trauma to major
nerve roots.224 RSD is divided into three phases, which are
important in determining appropriate treatment.225 Phase
one is characterized by sympathetic overflow with diffuse
swelling, pain, increased vascularity, and radiographic evidence of demineralization. If left untreated for 3 to 6
months, the condition may progress to phase two, which is
characterized by atrophy. The extremity may now be cold
and shiny, with atrophy of the skin and muscles. Phase three
refers to progression of trophic changes, with irreversible
flexion contracture and a pale, cold, painful extremity. It
has been speculated that phase one is related to peripheral
short-circuiting of nerve impulses, phase two represents
short-circuiting through the internuncial pool in the spinal
cord, and phase three is controlled by higher thalamic
centers.225,226
Steinbrocker227 reported that recovery is possible as long
as vasomotor activity with swelling and hyperemia is
evident. After the trophic phase two or three is established,
the prognosis for recovery is poor. Prompt recognition of the
syndrome is important because early intervention to control
pain is mandatory. Careful supervision and reassurance are
crucial because many of these patients are emotionally
labile as a result of the pain or an underlying problem. The
syndrome may be remarkably reversed by a sympathetic
block. Patients who receive transient relief from sympathetic blockade may be helped by surgical sympathectomy.
Neoplasms
Primary and metastatic neoplasms may cause shoulder pain
by direct invasion of the musculoskeletal system or by compression with referred pain.2,228 Primary tumors are more
likely to occur in younger individuals. More common lesions
have a typical distribution, such as the predilection of a
chondroblastoma for the proximal humeral epiphysis or an
osteogenic sarcoma for the metaphysis.229 The differential
diagnosis of spontaneous onset of shoulder pain in older
individuals should include metastatic lesions and myeloma.
Neoplasms are best identified by plain radiographs, MRI, Tc
99m MDP scintigraphy, and CT.
Neoplasms also may involve the shoulder region through
metastases to the region. An associated history of carcinomas should alert the examiner to the possibility of a
bone tumor, especially in patients who have had malignancies with a predilection for metastasis to bone (e.g.,
thyroid, renal, lung, prostate, breast). Pain often is present
at rest and is exacerbated at night. Atypical pain distribution that is not relieved by injection without specific
dermatomal distribution should alert the examiner to other
underlying possibilities. Plain radiographs should be evaluated thoroughly for any cortical destruction and for lytic
lesions.
Pancoast syndrome or apical lung tumor may manifest as
shoulder pain or cervical radiculitis caused by invasion of
the brachial plexus or invasion of C8 or T1 roots.230-232 With
invasion of the cervical sympathetic chain, the patient also
may develop Homer’s syndrome.
Miscellaneous Conditions
With increasing numbers of patients undergoing long-term
maintenance hemodialysis, a shoulder pain syndrome
known as dialysis shoulder arthropathy has been described. It
consists of shoulder pain, weakness, loss of motion, and
functional limitation. The cause and pathogenesis of this
syndrome are unclear, although rotator cuff disease, pathologic fracture, bursitis, and local amyloid deposition have
been implicated as causative factors.233 Surgical or necropsy
data are insufficient to confirm a specific diagnosis. Patients
generally respond poorly to local measures of injection,
heat, and NSAIDs, but their condition may improve with
correction of underlying metabolic disorders, such as osteomalacia and secondary hyperparathyroidism.
In patients older than 50 years of age with bilateral
shoulder pain and stiffness, polymyalgia rheumatica should
be considered as a diagnosis. It is twice as common among
females and is almost exclusively found in whites.234 Most
CHAPTER 46 patients have sedimentation rates greater than 40 mm/hr
and respond to low doses of corticosteroids.235
Selected References
1. Codman EA: The shoulder: rupture of the supraspinatus tendon and other
lesions in or about the subacromial bursa, Boston, 1934, Thomas Todd.
2. Bateman E: The shoulder and neck, ed 2, Philadelphia, 1978, WB
Saunders.
3. Post M: The shoulder: surgical and non-surgical management, Philadelphia, 1988, Lea & Febiger.
4. Caillet R: Shoulder pain, ed 2, Philadelphia, 1981, FA Davis.
5. Greep JM, Lemmens HAJ, Roos DB, et al: Pain in the shoulder and
arm: an integrated view, The Hague, 1979, Martinus Nijhoff.
6. O’Brien SJ, Arnoczky SP, Warren RF: Developmental anatomy of the
shoulder and anatomy of the glenohumeral joint. In Rockwood CA,
Matsen FA III, editors: The shoulder, Philadelphia, 1990, WB
Saunders.
7. Andrews JR, Carson W, McLeod W: Glenoid labrum tears related to
the long head of the biceps, Am J Sports Med 13:337, 1985.
8. Martin SD, Warren RF, Martin TL, et al: The non-operative management of suprascapular neuropathy, J Bone Joint Surg Am 79:1159,
1997.
9. Neer CS II: Anterior acromioplasty for the chronic impingement
syndrome in the shoulder: a preliminary report, J Bone Joint Surg Am
54:41, 1972.
10. Martin SD, Al-Zahrani SM, Andrews JR, et al: The circumduction
adduction shoulder test. Presented at Sixty-Third Annual Meeting
of the American Academy of Orthopedic Surgeons, February 22,
1996, Atlanta.
11. O’Brien SJ, Pagnani MJ, McGlynn SR, et al: A new and effective
test for diagnosing labral tears and AC joint pathology. Presented at
Sixty-Third Annual Meeting of the American Academy of Orthopedic Surgeons, February 22, 1996, Atlanta.
12. DePalma AF: Surgical anatomy of the acromioclavicular and sternoclavicular joints, Surg Clin North Am 43:1540, 1963.
13. Martin SD, Baumgarten T, Andrews JR: Arthroscopic subacromial
decompression with concomitant distal clavicle resection, J Bone
Joint Surg Am 85:328, 2001.
14. Dillin L, Hoaglund FT, Scheck M: Brachial neuritis, J Bone Joint Surg
Am 67:878, 1985.
15. Kelly BT, Kadrmas WR, Speer KP: The manual muscle examination
for rotator cuff strength, Am J Sports Med 24:581, 1996.
16. Saha AK: Theory of shoulder mechanism, Springfield, IL, 1961, Charles
C Thomas.
17. Saha AK: Mechanics of elevation of glenohumeral joint: its application in rehabilitation of flail shoulder in upper brachial plexus injuries
and poliomyelitis and in replacement of the upper humerus by prosthesis, Acta Orthop Scand 44:668, 1973.
18. Brown JT: Early assessment of supraspinatus tears: procaine infiltration as a guide to treatment, J Bone Joint Surg Br 31:423, 1949.
19. Neer CS: Impingement lesions, Clin Orthop Relat Res 173:70, 1983.
20. Rockwood CA: The role of anterior impingement in lesions of the
rotator cuff, J Bone Joint Surg Am 62:274, 1980.
21. Jobe FW, Kvitne RS, Giangarra CE: Shoulder pain in the overhead
or throwing athlete: the relationship of anterior instability and
rotator cuff impingement, Orthop Rev 18:963, 1989.
22. Dalton SE, Snyder SJ: Glenohumeral instability, Baillieres Clin Rheumatol 3:511, 1989.
23. Zanca P: Shoulder pain: involvement of the acromioclavicular joint
(analysis of 1000 cases), AJR Am J Roentgenol 112:493, 1971.
24. Goldman AB: Shoulder arthrography, Boston, 1982, Little, Brown.
25. Goldman AB, Ghelman B: The double contrast shoulder arthrogram:
a review of 158 studies, Radiology 127:655, 1978.
26. Mink J, Harris E: Double contrast shoulder arthrography: its use in
evaluation of rotator cuff tears, Orthop Trans 7:71, 1983.
27. Braunstein EM, O’Connor G: Double-contrast arthrotomography of
the shoulder, J Bone Joint Surg Am 64:192, 1982.
28. Ghelman B, Goldman AB: The double contrast shoulder arthrogram:
evaluation of rotator cuff tears, Radiology 124:251, 1977.
29. Goldman AB, Ghelman B: The double contrast shoulder arthrogram,
Cardiology 127:665, 1978.
30. Kneisl JS, Sweeney HJ, Paige ML: Correlation of pathology observed
in double contrast arthrotomography, Arthroscopy 4:21, 1988.
31. Strizak AM, Danzig L, Jackson DW, et al: Subacromial bursography,
J Bone Joint Surg Am 64:196, 1982.
| Shoulder Pain
663
32. Lie S: Subacromial bursography, Radiology 144:626, 1982.
33. Fukuda H, Mikasa M, Yamanaka K: Incomplete thickness rotator cuff
tears diagnosed by subacromial bursography, Clin Orthop Relat Res
223:51, 1987.
34. Rafii M, Minkoff J, Bonana J, et al: Computed tomography (CT)
arthrography of shoulder instabilities in athletes, Am J Sports Med
16:352, 1988.
35. el-Khoury GY, Kathol MH, Chandler JB, et al: Shoulder instability:
impact of glenohumeral arthrotomography on treatment, Radiology
160:669, 1986.
36. Mack LA, Matsen FA, Kilcoyne RF, et al: US evaluation of the
rotator cuff, Radiology 157:206, 1985.
37. Crass JR, Craig EV, Bretzke C, et al: Ultrasonography of the rotator
cuff, Radiographics 5:941, 1985.
38. Harryman DT, Mack LA, Wang KA, et al: Integrity of the postoperative cuff: ultrasonography and function. Presented at FiftySeventh Annual Meeting of the American Academy of Orthopedic
Surgeons, February 9, 1990, New Orleans.
39. Hodler J, Fretz CJ, Terrier F, et al: Rotator cuff tears: correlation of
sonic and surgical findings, Radiology 169:791, 1988.
40. Middleton WD, Edelstein G, Reinus WR, et al: Ultrasonography of
the rotator cuff: technique and normal anatomy, J Ultrasound Med
3:549, 1984.
41. Gardelin G, Perin B: Ultrasonics of the shoulder: diagnostic possibilities in lesions of the rotator cuff, Radiol Med (Torino) 74:404, 1987.
42. Vestring T, Bongartz G, Konermann W, et al: The place of magnetic
resonance tomography in the diagnosis of diseases of the shoulder
joint, Fortschr Geb Rontgenstr Neuen Bildgeb Verfahr 154:143, 1991.
43. Ahovuo J, Paavolainen P, Slatis P: Diagnostic value of sonography
in lesions of the biceps tendon, Clin Orthop Relat Res 202:184, 1986.
44. Ogilvie-Harris DJ, D’Angelo G: Arthroscopic surgery of the shoulder,
Sports Med 9:120, 1990.
45. Ellman H: Arthroscopic subacromial decompression, Orthop Trans
9:49, 1985.
46. Ellman H: Arthroscopic subacromial decompression: analysis of oneto three-year results, Arthroscopy 3:173, 1987.
47. Paulos LE, Franklin JL: Arthroscopic shoulder decompression development and application: a five year experience, Am J Sports Med
17:235, 1990.
48. Zlatkin MB, Reicher MA, Kellerhouse LE, et al: The painful shoulder: MRI imaging of the glenohumeral joint, J Comput Assist Tomogr
12:995, 1988.
49. Meyer SJ, Dalinka MK: Magnetic resonance imaging of the shoulder,
Orthop Clin North Am 21:497, 1990.
50. Seeger LL, Gold RH, Bassett LW: Shoulder instability: evaluation
with MR imaging, Radiology 168:696, 1988.
51. Kieft GJ, Dijkmans BA, Bioem JL, et al: Magnetic resonance imaging
of the shoulder in patients with rheumatoid arthritis, Ann Rheum Dis
49:7, 1990.
52. Morrison DS, Offstein R: The use of magnetic resonance imaging in
the diagnosis of rotator cuff tears, Orthopedics 13:633, 1990.
53. Nelson MC, Leather GP, Nirschl RP, et al: Evaluation of the painful
shoulder: a prospective comparison of magnetic resonance imaging,
computerized tomographic arthrography, J Bone Joint Surg Am 73:707,
1991.
54. Reeder JD, Andelman S: The rotator cuff tear: MR evaluation, Magn
Reson Imaging 5:331, 1987.
55. Seeger LL, Gold RH, Bassett LW, et al: Shoulder impingement syndrome: MR findings in 53 shoulders, AJR Am J Roentgenol 150:343,
1988.
56. Nakano KK: Neurology of musculoskeletal and rheumatic disorders,
Boston, 1979, Houghton Mifflin.
57. Leffert RD: Brachial plexus injuries, N Engl J Med 291:1059, 1974.
58. Buchbinder R, Gren S, Youd J: Corticosteroid injections for shoulder
pain, Cochrane Database Syst Rev (1):CD004016, 2003.
59. Altchek DW, Schwartz E, Warren RF, et al: Radiologic measurement
of superior migration of the humeral head in impingement syndrome.
Presented at the Sixth Open Meeting of the American Shoulder and
Elbow Surgeons, February 11, 1990, New Orleans.
60. Inman VT, Saunders JB, Abbott LC: Observations on the functions
of the shoulder joint, J Bone Joint Surg Am 26:1, 1944.
61. Poppen NK, Walker PS: Normal and abnormal motion of the shoulder, J Bone Joint Surg Am 58:195, 1976.
62. Bigliani LU, Morrison D, April EW: The morphology of the acromion and its relationship to rotator cuff tears, Orthop Trans 10:228,
1986.
664
PART 6 | DIFFERENTIAL DIAGNOSIS OF REGIONAL AND DIFFUSE MUSCULOSKELETAL PAIN
63. Morrison DS, Bigliani LU: The clinical significance of variations in
acromial morphology, Orthop Trans 11:234, 1987.
64. Codman E, Akerson TB: The pathology associated with rupture of
the supraspinatus tendon, Ann Surg 93:354, 1911.
65. Fukuda H, Hamada K, Yamanaka K: Pathology and pathogenesis of
bursal side rotator cuff tears: views from en-bloc histological sections,
Clin Orthop Relat Res 254:75, 1990.
66. McLaughlin HL: Lesions of the musculotendinous cuff of the shoulder. I. The exposure and treatment of tears with retraction, J Bone
Joint Surg Am 26:31, 1944.
67. Neer CS II, Flatow EL, Lech O: Tears of the rotator cuff: long term
results of anterior acromioplasty and repair. Presented at Fourth Open
Meeting of the American Shoulder and Elbow Surgeons, February
1988, Atlanta.
68. Ogata S, Uhthoff HK: Acromial enthesopathy and rotator cuff tears:
a radiographic and histologic postmortem investigation of the coracoacromial arch, Clin Orthop Relat Res 254:39, 1990.
69. Olsson O: Degenerative changes in the shoulder joint and their connection with shoulder pain: a morphological and clinical investigation with special attention to the cuff and biceps tendon, Acta Chir
Scand 181(Suppl):1, 1953.
70. Ozaki J, Fujimoto S, Nakagawa Y, et al: Tears of the rotator cuff of
the shoulder associated with pathologic changes of the acromion: a
study in cadavers, J Bone Joint Surg Am 70:1224, 1988.
71. Skinner HA: Anatomical consideration relative to ruptures of the
supraspinatus tendon, J Bone Joint Surg Br 19:137, 1937.
72. Ellman H: Occupational supraspinatus tendinitis: the rotator cuff
syndrome, Ugeskr Laeger 151:2355, 1989.
73. Scheib JS: Diagnosis and rehabilitation of the shoulder impingement
syndrome in the overhand and throwing athlete, Rheum Dis Clin
North Am 16:971, 1990.
74. Jackson DW: Chronic rotator cuff impingement in the throwing
athlete, Am J Sports Med 4:231, 1976.
75. Hawkins RJ, Kennedy JC: Impingement syndrome in athletes, Am J
Sports Med 8:151, 1980.
76. McShane RB, Leinberry CF, Fenlin JM: Conservative open anterior
acromioplasty, Clin Orthop Relat Res 223:137, 1987.
77. Rockwood CA, Lyons FA: Shoulder impingement syndrome: diagnosis, radiographic evaluation, and treatment with a modified Neer
acromioplasty, J Bone Joint Surg Am 75:1593, 1993.
78. Hawkins RJ, Brock RM, Abrams JS, et al: Acromioplasty for impingement with an intact rotator cuff, J Bone Joint Surg Br 70:797, 1988.
79. Stuart MJ, Azevedo AJ, Cofield RH: Anterior acromioplasty for
treatment of the shoulder impingement syndrome, Clin Orthop Relat
Res 260:195, 1990.
80. Bigliani LU, D’Alesandro DF, Duralde XA, et al: Anterior acromioplasty for subacromial impingement in patients younger than 40 years
of age, Clin Orthop Relat Res 246:111, 1988.
81. Bjorkheim JM, Paavolainen P, Ahovuo J, et al: Surgical repair of the
rotator cuff and the surrounding tissues: factors influencing the
results, Clin Orthop Relat Res 236:148, 1988.
82. Levy HJ, Gardner RD, Lemak LJ: Arthroscopic subacromial decompression in the treatment of full-thickness rotator cuff tears, Arthroscopy 7:8, 1991.
83. McKendry RJR, Uhthoff HK, Sarkar K, et al: Calcifying tendinitis of
the shoulder: prognostic value of clinical, histologic, and radiographic features in 57 surgically treated cases, J Rheumatol 9:75, 1982.
84. Uhthoff HK, Sarkar K, Maynard JA: Calcifying tendinitis, a new
concept of its pathogenesis, Clin Orthop Relat Res 118:164, 1976.
85. Sarkar K, Uhthoff HK: Ultrastructure localization of calcium in calcifying tendinitis, Arch Pathol Lab Med 102:266, 1978.
86. Hayes CW, Conway WF: Calcium hydroxyapatite deposition disease,
Radiographics 10:1031, 1990.
87. Vebostad A: Calcific tendinitis in the shoulder region: a review of 43
operated shoulders, Acta Orthop Scand 46:205, 1975.
88. Moseley HF, Goldie I: The arterial pattern of the rotator cuff of the
shoulder, J Bone Joint Surg Br 45:780, 1963.
89. Rathburn JB, Macnab I: The microvascular pattern of the rotator
cuff, J Bone Joint Surg Br 52:540, 1970.
90. Bosworth BM: Calcium deposits in the shoulder and subacromial
bursitis: a survey of 12,122 shoulders, JAMA 116:2477, 1941.
91. Bosworth BM: Examination of the shoulder for calcium deposits,
J Bone Joint Surg Am 23:567, 1941.
92. DePalma AF, Kruper JS: Long term study of shoulder joints afflicted
with and treated for calcified tendonitis, Clin Orthop Relat Res 20:61,
1961.
93. Rizzello G, Franceschi F, Ruzzini L, et al: Arthroscopic management
of calcific tendinopathy of the shoulder, Bull NYU Hosp Jt Dis 67:330,
2009.
94. Linblom K: Arthrography and roentgenography in ruptures of the
tendon of the shoulder joint, Acta Radiol 20:548, 1939.
95. Swiontkowski M, Iannotti JP, Herrmann HJ, et al: Intraoperative
assessment of rotator cuff vascularity using laser Doppler flowmetry.
In Post M, Morrey BE, Hawkins RJ, editors: Surgery of the shoulder,
St Louis, 1990, Mosby, pp 208–212.
96. Matsen FA III, Arntz CT: Subacromial impingement. In Rockwood
CA Jr, Matsen FA III, editors: The shoulder, Philadelphia, 1990, WB
Saunders, pp 623–646.
97. Neer CS II, Poppen NK: Supraspinatus outlet, Orthop Trans 11:234,
1987.
98. Clark J, Sidles JA, Matsen FA: The relationship of the glenohumeral
joint capsule to the rotator cuff, Clin Orthop Relat Res 254:29, 1990.
99. Samilson RL, Raphael RL, Post L, et al: Arthrography of the shoulder, Clin Orthop Relat Res 20:21, 1961.
100. Collins RA, Gristina AG, Carter RE, et al: Ultrasonography of the
shoulder, Orthop Clin North Am 18:351, 1987.
101. Crass JR, Craig EV, Feinberg SB: Ultrasonography of rotator cuff
tears: a review of 500 diagnostic studies, J Clin Ultrasound 16:313,
1988.
102. Crass JR, Craig EV, Feinberg SB: The hyperextended internal rotation view in rotator cuff ultrasonography, J Clin Ultrasound 15:415,
1987.
103. Mack LA, Gannon MK, Kilcoyne RF, et al: Sonographic evaluation
of the rotator cuff: accuracy in patients without prior surgery, Clin
Orthop Relat Res 234:21, 1988.
104. Iannotti JP, Zlatkin MB, Esterhai JL, et al: Magnetic resonance
imaging of the shoulder: sensitivity, specificity, and predictive value,
J Bone Joint Surg Am 73:17, 1991.
105. DePalma AF: Surgery of the shoulder, ed 2, Philadelphia, 1973, JB
Lippincott.
106. Wolfgang GL: Surgical repair of tears of the rotator cuff of the shoulder: factors influencing the result, J Bone Joint Surg Am 56:14, 1974.
107. Jobe FW, Moynes DR: Delineation of diagnostic criteria and a rehabilitation program for rotator cuff injuries, Am J Sports Med 10:336,
1982.
108. Coghlan JA, Buchbinder R, Green S, et al: Surgery for rotator cuff
disease, Cochrane Database Syst Rev (1):CD005619, 2009.
109. Oh L, Wolf B, Hall M, et al: Indications for rotator cuff repair, Clin
Orthop Relat Res 455:52, 2007.
110. Earnshaw P, Desjardins D, Sakar K, et al: Rotator cuff tears: the role
of surgery, Can J Surg 25:60, 1982.
111. Rockwood CA, Williams GR, Burkhead WZ: Debridement of
massive, degenerative lesions of the rotator cuff. Presented at Seventh
Open Meeting of the American Shoulder and Elbow Society Surgeons, March 10, 1991, Anaheim, CA.
112. Martin SD, Andrews JR: The rotator cuff: open and mini-open
repairs. Presented at American Orthopaedic Society for Sports Medicine 20th Annual Meeting, June 26, 1994, Palm Desert, CA.
113. Rockwood CA Jr: The shoulder: facts, confusion and myths, Int
Orthop 15:401, 1991.
114. Steffens K, Konermann H: Rupture of the rotator cuff in the elderly,
Z Gerontol 20:95, 1987.
115. Mulieri P, Dunning P, Klein S, et al: Reverse shoulder arthroplasty
for the treatment of irreparable rotator cuff tear without glenohumeral arthritis, J Bone Joint Surg Am 92:2544, 2010
116. Goss CM: Gray’s anatomy of the human body, ed 28, Philadelphia,
1966, Lea & Febiger.
117. Neer CS, Craig EV, Fukuda H: Cuff tear arthropathy, J Bone Joint Surg
Am 65:1232, 1983.
118. Neer CS II, Bigliani LU, Hawkins RJ: Rupture of the long head of
the biceps related to subacromial impingement, Orthop Trans 1:111,
1977.
119. Crenshaw AH, Kilgore WE: Surgical treatment of bicipital tendonitis, J Bone Joint Surg Am 48:1496, 1966.
120. Hitchcock HH, Bechtol CO: Painful shoulder: observations on the
role of the tendon of the long head of the biceps brachii in its causation, J Bone Joint Surg Am 30:263, 1948.
Full references for this chapter can be found on www.expertconsult.com.
CHAPTER 46 References
1. Codman EA: The shoulder: rupture of the supraspinatus tendon and other
lesions in or about the subacromial bursa, Boston, 1934, Thomas
Todd.
2. Bateman E: The shoulder and neck, ed 2, Philadelphia, 1978, WB
Saunders.
3. Post M: The shoulder: surgical and non-surgical management, Philadelphia, 1988, Lea & Febiger.
4. Caillet R: Shoulder pain, ed 2, Philadelphia, 1981, FA Davis.
5. Greep JM, Lemmens HAJ, Roos DB, et al: Pain in the shoulder and
arm: an integrated view, The Hague, 1979, Martinus Nijhoff.
6. O’Brien SJ, Arnoczky SP, Warren RF: Developmental anatomy of the
shoulder and anatomy of the glenohumeral joint. In Rockwood CA,
Matsen FA III, editors: The shoulder, Philadelphia, 1990, WB
Saunders.
7. Andrews JR, Carson W, McLeod W: Glenoid labrum tears related to
the long head of the biceps, Am J Sports Med 13:337, 1985.
8. Martin SD, Warren RF, Martin TL, et al: The non-operative management of suprascapular neuropathy, J Bone Joint Surg Am 79:1159,
1997.
9. Neer CS II: Anterior acromioplasty for the chronic impingement
syndrome in the shoulder: a preliminary report, J Bone Joint Surg Am
54:41, 1972.
10. Martin SD, Al-Zahrani SM, Andrews JR, et al: The circumduction
adduction shoulder test. Presented at Sixty-Third Annual Meeting
of the American Academy of Orthopedic Surgeons, February 22,
1996, Atlanta.
11. O’Brien SJ, Pagnani MJ, McGlynn SR, et al: A new and effective
test for diagnosing labral tears and AC joint pathology. Presented at
Sixty-Third Annual Meeting of the American Academy of Orthopedic Surgeons, February 22, 1996, Atlanta.
12. DePalma AF: Surgical anatomy of the acromioclavicular and sternoclavicular joints, Surg Clin North Am 43:1540, 1963.
13. Martin SD, Baumgarten T, Andrews JR: Arthroscopic subacromial
decompression with concomitant distal clavicle resection, J Bone
Joint Surg Am 85:328, 2001.
14. Dillin L, Hoaglund FT, Scheck M: Brachial neuritis, J Bone Joint Surg
Am 67:878, 1985.
15. Kelly BT, Kadrmas WR, Speer KP: The manual muscle examination
for rotator cuff strength, Am J Sports Med 24:581, 1996.
16. Saha AK: Theory of shoulder mechanism, Springfield, IL, 1961, Charles
C Thomas.
17. Saha AK: Mechanics of elevation of glenohumeral joint: its application in rehabilitation of flail shoulder in upper brachial plexus injuries
and poliomyelitis and in replacement of the upper humerus by prosthesis, Acta Orthop Scand 44:668, 1973.
18. Brown JT: Early assessment of supraspinatus tears: procaine infiltration as a guide to treatment, J Bone Joint Surg Br 31:423, 1949.
19. Neer CS: Impingement lesions, Clin Orthop Relat Res 173:70,
1983.
20. Rockwood CA: The role of anterior impingement in lesions of the
rotator cuff, J Bone Joint Surg Am 62:274, 1980.
21. Jobe FW, Kvitne RS, Giangarra CE: Shoulder pain in the overhead
or throwing athlete: the relationship of anterior instability and
rotator cuff impingement, Orthop Rev 18:963, 1989.
22. Dalton SE, Snyder SJ: Glenohumeral instability, Baillieres Clin Rheumatol 3:511, 1989.
23. Zanca P: Shoulder pain: involvement of the acromioclavicular joint
(analysis of 1000 cases), AJR Am J Roentgenol 112:493, 1971.
24. Goldman AB: Shoulder arthrography, Boston, 1982, Little, Brown.
25. Goldman AB, Ghelman B: The double contrast shoulder arthrogram:
a review of 158 studies, Radiology 127:655, 1978.
26. Mink J, Harris E: Double contrast shoulder arthrography: its use in
evaluation of rotator cuff tears, Orthop Trans 7:71, 1983.
27. Braunstein EM, O’Connor G: Double-contrast arthrotomography of
the shoulder, J Bone Joint Surg Am 64:192, 1982.
28. Ghelman B, Goldman AB: The double contrast shoulder arthrogram:
evaluation of rotator cuff tears, Radiology 124:251, 1977.
29. Goldman AB, Ghelman B: The double contrast shoulder arthrogram,
Cardiology 127:665, 1978.
30. Kneisl JS, Sweeney HJ, Paige ML: Correlation of pathology observed
in double contrast arthrotomography, Arthroscopy 4:21, 1988.
31. Strizak AM, Danzig L, Jackson DW, et al: Subacromial bursography,
J Bone Joint Surg Am 64:196, 1982.
32. Lie S: Subacromial bursography, Radiology 144:626, 1982.
| Shoulder Pain
664.e1
33. Fukuda H, Mikasa M, Yamanaka K: Incomplete thickness rotator cuff
tears diagnosed by subacromial bursography, Clin Orthop Relat Res
223:51, 1987.
34. Rafii M, Minkoff J, Bonana J, et al: Computed tomography (CT)
arthrography of shoulder instabilities in athletes, Am J Sports Med
16:352, 1988.
35. el-Khoury GY, Kathol MH, Chandler JB, et al: Shoulder instability:
impact of glenohumeral arthrotomography on treatment, Radiology
160:669, 1986.
36. Mack LA, Matsen FA, Kilcoyne RF, et al: US evaluation of the
rotator cuff, Radiology 157:206, 1985.
37. Crass JR, Craig EV, Bretzke C, et al: Ultrasonography of the rotator
cuff, Radiographics 5:941, 1985.
38. Harryman DT, Mack LA, Wang KA, et al: Integrity of the postoperative cuff: ultrasonography and function. Presented at FiftySeventh Annual Meeting of the American Academy of Orthopedic
Surgeons, February 9, 1990, New Orleans.
39. Hodler J, Fretz CJ, Terrier F, et al: Rotator cuff tears: correlation of
sonic and surgical findings, Radiology 169:791, 1988.
40. Middleton WD, Edelstein G, Reinus WR, et al: Ultrasonography of
the rotator cuff: technique and normal anatomy, J Ultrasound Med
3:549, 1984.
41. Gardelin G, Perin B: Ultrasonics of the shoulder: diagnostic possibilities in lesions of the rotator cuff, Radiol Med (Torino) 74:404, 1987.
42. Vestring T, Bongartz G, Konermann W, et al: The place of magnetic
resonance tomography in the diagnosis of diseases of the shoulder
joint, Fortschr Geb Rontgenstr Neuen Bildgeb Verfahr 154:143, 1991.
43. Ahovuo J, Paavolainen P, Slatis P: Diagnostic value of sonography
in lesions of the biceps tendon, Clin Orthop Relat Res 202:184, 1986.
44. Ogilvie-Harris DJ, D’Angelo G: Arthroscopic surgery of the shoulder,
Sports Med 9:120, 1990.
45. Ellman H: Arthroscopic subacromial decompression, Orthop Trans
9:49, 1985.
46. Ellman H: Arthroscopic subacromial decompression: analysis of oneto three-year results, Arthroscopy 3:173, 1987.
47. Paulos LE, Franklin JL: Arthroscopic shoulder decompression development and application: a five year experience, Am J Sports Med
17:235, 1990.
48. Zlatkin MB, Reicher MA, Kellerhouse LE, et al: The painful shoulder: MRI imaging of the glenohumeral joint, J Comput Assist Tomogr
12:995, 1988.
49. Meyer SJ, Dalinka MK: Magnetic resonance imaging of the shoulder,
Orthop Clin North Am 21:497, 1990.
50. Seeger LL, Gold RH, Bassett LW: Shoulder instability: evaluation
with MR imaging, Radiology 168:696, 1988.
51. Kieft GJ, Dijkmans BA, Bioem JL, et al: Magnetic resonance imaging
of the shoulder in patients with rheumatoid arthritis, Ann Rheum Dis
49:7, 1990.
52. Morrison DS, Offstein R: The use of magnetic resonance imaging in
the diagnosis of rotator cuff tears, Orthopedics 13:633, 1990.
53. Nelson MC, Leather GP, Nirschl RP, et al: Evaluation of the painful
shoulder: a prospective comparision of magnetic resonance imaging,
computerized tomographic arthrography, J Bone Joint Surg Am 73:707,
1991.
54. Reeder JD, Andelman S: The rotator cuff tear: MR evaluation, Magn
Reson Imaging 5:331, 1987.
55. Seeger LL, Gold RH, Bassett LW, et al: Shoulder impingement syndrome: MR findings in 53 shoulders, AJR Am J Roentgenol 150:343,
1988.
56. Nakano KK: Neurology of musculoskeletal and rheumatic disorders,
Boston, 1979, Houghton Mifflin.
57. Leffert RD: Brachial plexus injuries, N Engl J Med 291:1059, 1974.
58. Buchbinder R, Gren S, Youd J: Corticosteroid injections for shoulder
pain, Cochrane Database Syst Rev (1):CD004016, 2003.
59. Altchek DW, Schwartz E, Warren RF, et al: Radiologic measurement
of superior migration of the humeral head in impingement syndrome.
Presented at the Sixth Open Meeting of the American Shoulder and
Elbow Surgeons, February 11, 1990, New Orleans.
60. Inman VT, Saunders JB, Abbott LC: Observations on the functions
of the shoulder joint, J Bone Joint Surg Am 26:1, 1944.
61. Poppen NK, Walker PS: Normal and abnormal motion of the shoulder, J Bone Joint Surg Am 58:195, 1976.
62. Bigliani LU, Morrison D, April EW: The morphology of the acromion and its relationship to rotator cuff tears, Orthop Trans 10:228,
1986.
664.e2
PART 6 | DIFFERENTIAL DIAGNOSIS OF REGIONAL AND DIFFUSE MUSCULOSKELETAL PAIN
63. Morrison DS, Bigliani LU: The clinical significance of variations in
acromial morphology, Orthop Trans 11:234, 1987.
64. Codman E, Akerson TB: The pathology associated with rupture of
the supraspinatus tendon, Ann Surg 93:354, 1911.
65. Fukuda H, Hamada K, Yamanaka K: Pathology and pathogenisis of
bursal side rotator cuff tears: views from en-bloc histological sections,
Clin Orthop Relat Res 254:75, 1990.
66. McLaughlin HL: Lesions of the musculotendinous cuff of the shoulder. I. The exposure and treatment of tears with retraction, J Bone
Joint Surg Am 26:31, 1944.
67. Neer CS II, Flatow EL, Lech O: Tears of the rotator cuff: long term
results of anterior acromioplasty and repair. Presented at Fourth Open
Meeting of the American Shoulder and Elbow Surgeons, February
1988, Atlanta.
68. Ogata S, Uhthoff HK: Acromial enthesopathy and rotator cuff tears:
a radiographic and histologic postmortem investigation of the coracoacromial arch, Clin Orthop Relat Res 254:39, 1990.
69. Olsson O: Degenerative changes in the shoulder joint and their connection with shoulder pain: a morphological and clinical investigation with special attention to the cuff and biceps tendon, Acta Chir
Scand 181(Suppl):1, 1953.
70. Ozaki J, Fujimoto S, Nakagawa Y, et al: Tears of the rotator cuff of
the shoulder associated with pathologic changes of the acromion: a
study in cadavers, J Bone Joint Surg Am 70:1224, 1988.
71. Skinner HA: Anatomical consideration relative to ruptures of the
supraspinatus tendon, J Bone Joint Surg Br 19:137, 1937.
72. Ellman H: Occupational supraspinatus tendinitis: the rotator cuff
syndrome, Ugeskr Laeger 151:2355, 1989.
73. Scheib JS: Diagnosis and rehabilitation of the shoulder impingement
syndrome in the overhand and throwing athlete, Rheum Dis Clin
North Am 16:971, 1990.
74. Jackson DW: Chronic rotator cuff impingement in the throwing
athlete, Am J Sports Med 4:231, 1976.
75. Hawkins RJ, Kennedy JC: Impingement syndrome in athletes, Am J
Sports Med 8:151, 1980.
76. McShane RB, Leinberry CF, Fenlin JM: Conservative open anterior
acromioplasty, Clin Orthop Relat Res 223:137, 1987.
77. Rockwood CA, Lyons FA: Shoulder impingement syndrome: diagnosis, radiographic evaluation, and treatment with a modified Neer
acromioplasty, J Bone Joint Surg Am 75:1593, 1993.
78. Hawkins RJ, Brock RM, Abrams JS, et al: Acromioplasty for impingement with an intact rotator cuff, J Bone Joint Surg Br 70:797, 1988.
79. Stuart MJ, Azevedo AJ, Cofield RH: Anterior acromioplasty for
treatment of the shoulder impingement syndrome, Clin Orthop Relat
Res 260:195, 1990.
80. Bigliani LU, D’Alesandro DF, Duralde XA, et al: Anterior acromioplasty for subacromial impingement in patients younger than 40 years
of age, Clin Orthop Relat Res 246:111, 1988.
81. Bjorkheim JM, Paavolainen P, Ahovuo J, et al: Surgical repair of the
rotator cuff and the surrounding tissues: factors influencing the
results, Clin Orthop Relat Res 236:148, 1988.
82. Levy HJ, Gardner RD, Lemak LJ: Arthroscopic subacromial decompression in the treatment of full-thickness rotator cuff tears, Arthroscopy 7:8, 1991.
83. McKendry RJR, Uhthoff HK, Sarkar K, et al: Calcifying tendinitis of
the shoulder: prognostic value of clinical, histologic, and radiographic features in 57 surgically treated cases, J Rheumatol 9:75, 1982.
84. Uhthoff HK, Sarkar K, Maynard JA: Calcifying tendinitis, a new
concept of its pathogenesis, Clin Orthop Relat Res 118:164, 1976.
85. Sarkar K, Uhthoff HK: Ultrastructure localization of calcium in calcifying tendinitis, Arch Pathol Lab Med 102:266, 1978.
86. Hayes CW, Conway WF: Calcium hydroxyapatite deposition disease,
Radiographics 10:1031, 1990.
87. Vebostad A: Calcific tendinitis in the shoulder region: a review of 43
operated shoulders, Acta Orthop Scand 46:205, 1975.
88. Moseley HF, Goldie I: The arterial pattern of the rotator cuff of the
shoulder, J Bone Joint Surg Br 45:780, 1963.
89. Rathburn JB, Macnab I: The microvascular pattern of the rotator
cuff, J Bone Joint Surg Br 52:540, 1970.
90. Bosworth BM: Calcium deposits in the shoulder and subacromial
bursitis: a survey of 12,122 shoulders, JAMA 116:2477, 1941.
91. Bosworth BM: Examination of the shoulder for calcium deposits,
J Bone Joint Surg Am 23:567, 1941.
92. DePalma AF, Kruper JS: Long term study of shoulder joints afflicted
with and treated for calcified tendonitis, Clin Orthop Relat Res 20:61,
1961.
93. Rizzello G, Franceschi F, Ruzzini L, et al: Arthroscopic management
of calcific tendinopathy of the shoulder, Bull NYU Hosp Jt Dis 67:330,
2009.
94. Linblom K: Arthrography and roentgenography in ruptures of the
tendon of the shoulder joint, Acta Radiol 20:548, 1939.
95. Swiontkowski M, Iannotti JP, Herrmann HJ, et al: Intraoperative
assessment of rotator cuff vascularity using laser Doppler flowmetry.
In Post M, Morrey BE, Hawkins RJ, editors: Surgery of the shoulder,
St Louis, 1990, Mosby, p 208.
96. Matsen FA III, Arntz CT: Subacromial impingment. In Rockwood
CA Jr, Matsen FA III, editors: The shoulder, Philadelphia, 1990, WB
Saunders, p 623.
97. Neer CS II, Poppen NK: Supraspinatus outlet, Orthop Trans 11:234,
1987.
98. Clark J, Sidles JA, Matsen FA: The relationship of the glenohumeral
joint capsule to the rotator cuff, Clin Orthop Relat Res 254:29,
1990.
99. Samilson RL, Raphael RL, Post L, et al: Arthrography of the shoulder, Clin Orthop Relat Res 20:21, 1961.
100. Collins RA, Gristina AG, Carter RE, et al: Ultrasonography of the
shoulder, Orthop Clin North Am 18:351, 1987.
101. Crass JR, Craig EV, Feinberg SB: Ultrasonography of rotator cuff
tears: a review of 500 diagnostic studies, J Clin Ultrasound 16:313,
1988.
102. Crass JR, Craig EV, Feinberg SB: The hyperextended internal rotation view in rotator cuff ultrasonography, J Clin Ultrasound 15:415,
1987.
103. Mack LA, Gannon MK, Kilcoyne RF, et al: Sonographic evaluation
of the rotator cuff: accuracy in patients without prior surgery, Clin
Orthop Relat Res 234:21, 1988.
104. Iannotti JP, Zlatkin MB, Esterhai JL, et al: Magnetic resonance
imaging of the shoulder: sensitivity, specificity, and predictive value,
J Bone Joint Surg Am 73:17, 1991.
105. DePalma AF: Surgery of the shoulder, ed 2, Philadelphia, 1973, JB
Lippincott.
106. Wolfgang GL: Surgical repair of tears of the rotator cuff of the
shoulder: factors influencing the result, J Bone Joint Surg Am 56:14,
1974.
107. Jobe FW, Moynes DR: Delineation of diagnostic criteria and a rehabilitation program for rotator cuff injuries, Am J Sports Med 10:336,
1982.
108. Coghlan JA, Buchbinder R, Green S, et al: Surgery for rotator cuff
disease, Cochrane Database Syst Rev (1):CD005619, 2009.
109. Oh L, Wolf B, Hall M, et al: Indications for rotator cuff repair, Clin
Orthop Relat Res 455:52, 2007.
110. Earnshaw P, Desjardins D, Sakar K, et al: Rotator cuff tears: the role
of surgery, Can J Surg 25:60, 1982.
111. Rockwood CA, Williams GR, Burkhead WZ: Debridement of
massive, degenerative lesions of the rotator cuff. Presented at Seventh
Open Meeting of the American Shoulder and Elbow Society Surgeons, March 10, 1991, Anaheim, CA.
112. Martin SD, Andrews JR: The rotator cuff: open and mini-open
repairs. Presented at American Orthopaedic Society for Sports Medicine 20th Annual Meeting, June 26, 1994, Palm Desert, CA.
113. Rockwood CA Jr: The shoulder: facts, confusion and myths, Int
Orthop 15:401, 1991.
114. Steffens K, Konermann H: Rupture of the rotator cuff in the elderly,
Z Gerontol 20:95, 1987.
115. Mulieri P, Dunning P, Klein S, et al: Reverse shoulder arthroplasty
for the treatment of irreparable rotator cuff tear without glenohumeral arthritis, J Bone Joint Surg Am 92:2544, 2010
116. Goss CM: Gray’s anatomy of the human body, ed 28, Philadelphia,
1966, Lea & Febiger.
117. Neer CS, Craig EV, Fukuda H: Cuff tear arthropathy, J Bone Joint Surg
Am 65:1232, 1983.
118. Neer CS II, Bigliani LU, Hawkins RJ: Rupture of the long head of
the biceps related to subacromial impingement, Orthop Trans 1:111,
1977.
119. Crenshaw AH, Kilgore WE: Surgical treatment of bicipital tendonitis, J Bone Joint Surg Am 48:1496, 1966.
120. Hitchcock HH, Bechtol CO: Painful shoulder: observations on the
role of the tendon of the long head of the biceps brachii in its causation, J Bone Joint Surg Am 30:263, 1948.
121. Meyer AW: Spontaneous dislocation and destruction of the tendon
of the long head of the biceps brachii, fifty-nine instances, Arch Surg
17:493, 1928.
CHAPTER 46 122. Rockwood RA Jr, Williams GR, Young CD: Injuries to the acromioclavicular joint. In Rockwood CA Jr, Green DP, Bucholz RW,
editors: Fractures in adults, Philadelphia, 1991, JB Lippincott,
p 1181.
123. Jacobs P: Post-traumatic osteolysis of the outer end of the clavicle,
J Bone Joint Surg Br 46:705, 1964.
124. Murphy OB, Bellamy R, Wheeler W, et al: Post-traumatic osteolysis
of the distal clavicle, Clin Orthop Relat Res 109:108, 1975.
125. Cahill RB: Osteolysis of the distal part of the clavicle in male athletes, J Bone Joint Surg Am 64:1053, 1982.
126. Maden B: Osteolysis of the acromial end of the clavicle following
trauma, Br J Radiol 36:822, 1963.
127. Scavenius M, Iversen BF: Nontraumatic clavicular osteolysis in
weight lifters, Am J Sports Med 20:463, 1992.
128. Slawski DP, Cahill BR: Atraumatic osteolysis of the distal clavicle,
Am J Sports Med 22:267, 1994.
129. Meyers JF: Arthroscopic debridement of the acromioclavicular joint
and distal clavicle resection. In McGinty JB, Caspari RB, Jackson
RW, et al, editors: Operative arthroscopy, New York, 1991, Raven
Press, p 557.
130. Cahill BR, Lee MT: Atraumatic osteolysis of the distal clavicle. In
Torg JS, Shephard RJ, editors: Current therapy in sports medicine, St
Louis, 1995, Mosby, p 177.
131. Rockwood CA Jr: Disorders of the acromioclavicular joint. In Rockwood CA Jr, Matsen FA III, editors: The shoulder, Philadelphia, 1985,
WB Saunders, p 449.
132. Gartsman GM Jr, Combs AH, Davis PF, et al: Arthroscopic acromioclavicular joint resection: an anatomic study, Am J Sports Med 19:2,
1991.
133. Fink EP: Injuries to the acromioclavicular joint. In Torg JS, Shephard
RJ, editors: Current therapy in sports medicine, St Louis, 1995, Mosby,
p 174.
134. Gartsman GM: Arthroscopic resection of the acromioclavicular
joint, Am J Sports Med 21:71, 1993.
135. Flatow EL, Cordasco FA, Bigliani LU: Arthroscopic resection of the
outer end of the clavicle from a superior approach: a critical, quantitative, radiographic assessment of bone removal, Arthroscopy 8:55,
1992.
136. Flatow EL, Duralde XA, Nicholson GP, et al: Arthroscopic resection
of the distal clavicle with a superior approach, J Shoulder Elbow Surg
4:41, 1995.
137. Worcester JN, Green DP: Osteoarthritis of the acromioclavicular
joint, Clin Orthop Relat Res 58:69, 1987.
138. DePalma AF: The role of the disks of the sternoclavicular and acromioclavicular joints, Clin Orthop Relat Res 13:222, 1959.
139. Novack PJ, Bach BB, Romeo AA, et al: Surgical resection of the
distal clavicle, J Shoulder Elbow Surg 4:35, 1995.
140. Gurd FB: The treatment of complete dislocation of the outer end of
the clavicle: a hitherto undescribed operation, Ann Surg 63:1094,
1941.
141. Mumford EB: Acromioclavicular dislocation: a new operative treatment, J Bone Joint Surg Am 23:799, 1941.
142. Cook FF, Tibone JE: The Mumford procedure in athletes: an objective
analysis of function, Am J Sports Med 16:97, 1988.
143. Bigliani LU, Nicholson GP, Flatow EL: Arthroscopic resection of the
distal clavicle, Orthop Clin North Am 24:133, 1993.
144. Gartsman GM, Combs AH, Davis PF, et al: Arthroscopic acromioclavicular joint resection: an anatomic study, Am J Sports Med 19:2,
1991.
145. Kay SP, Ellman H, Harris E: Arthroscopic distal clavicle resection:
technique and early results, Clin Orthop Relat Res 301:181,
1994.
146. Tolin BS, Snyder SJ: Our technique for the arthroscopic Mumford
procedure, Orthop Clin North Am 24:143, 1993.
147. Cofield RH, Briggs BT: Glenohumeral arthrodesis, J Bone Joint Surg
Am 61:668, 1979.
148. Rowe CR: Arthrodesis of the shoulder used in treating painful conditions, Clin Orthop Relat Res 173:92, 1983.
149. Neer CS II, Watson KC, Stanton FJ: Recent experience in total
shoulder replacement, J Bone Joint Surg Am 64:319, 1982.
150. Cofield RH: Unconstrained total shoulder prosthesis, Clin Orthop
Relat Res 173:97, 1983.
151. Thornhill TS, Karr MJ, Averill RM, et al: Total shoulder arthroplasty,
the Brigham experience. Presented at Fiftieth Annual Meeting of
the American Academy of Orthopedic Surgeons, 1983, Anaheim,
CA.
| Shoulder Pain
664.e3
152. Thornhill TS, Barrett WP: Total shoulder arthroplasty. In Rowe CR,
editor: The shoulder, New York, 1988, Churchill Livingstone.
153. Neer CS II: Fractures and dislocations of the shoulder. In Rockwood
CA, Green DP, editors: Fractures, Philadelphia, 1975, JB
Lippincott.
154. Ficat RP, Arlet J: Ischemia and necrosis of the bone, Baltimore, 1980,
Williams & Wilkins.
155. Hayes JM: Arthroscopic treatment of steroid-induced osteonecrosis
of the humeral head, Arthroscopy 5:218, 1989.
156. McCarty DJ: Robert Adams’ rheumatic arthritis of the shoulder:
“Milwaukee shoulder” revisited, J Rheumatol 32:668, 1989.
157. Halverson PB, Carrera GF, McCarty DJ: Milwaukee shoulder syndrome: fifteen additional cases and a description of contributing
factors, Arch Intern Med 150:677, 1990.
158. Wortmann RL, Veum JA, Rachow JW: Synovial fluid 5-nucleotidase
activity: relationship to other purine catabolic enzymes and to
arthropathies associated to calcium deposition disease, Arthritis
Rheum 34:1014, 1991.
159. Neer CS II, Craig EV, Fukada H, et al: Cuff tear arthropathy. Exhibit
at the Annual Meeting of the American Academy of Orthopedic
Surgeons, 1982, New Orleans.
160. Post M, Haskell SS, Jablon M: Total shoulder replacement with a
constrained prosthesis, J Bone Joint Surg Am 62:327, 1980.
161. Post M, Jablon M: Constrained total shoulder arthroplasty: long term
follow-up observations, Clin Orthop Relat Res 173:109, 1983.
162. Hamada K, Fukuda H, Mikasa M, et al: Roentgenographic findings
in rotator cuff tears: a long-term observation, Clin Orthop Relat Res
254:92, 1990.
163. Snyder SJ, Karzel RP, Del Pizzo W, et al: SLAP lesions of the shoulder,
Arthroscopy 6:274, 1990.
164. Burkhart SS, Fox DL: SLAP lesions in association with complete
tears of the long head of the biceps tendon: a report of two cases,
Arthroscopy 8:31, 1992.
165. Maffet MW, Gartsman GM, Moseley B: Superior labrum-biceps
tendon complex lesions of the shoulder, Am J Sports Med 23:93, 1995.
166. Grauer JD, Paulos LE, Smutz WP: Biceps tendon and superior labral
injuries, Arthroscopy 8:488, 1992.
167. Putman JJ: The treatment of a form of painful periarthritis of the
shoulder, Boston Med Surg J 107:536, 1882.
168. Neviaser JS: Adhesive capsulitis of the shoulder: study of the pathologic findings in periarthritis of the shoulder, J Bone Joint Surg Am
27:211, 1945.
169. McLaughlin HL: The “frozen shoulder,” Clin Orthop Relat Res 20:126,
1961.
170. Johnson JTH: Frozen shoulder syndrome in patients with pulmonary
tuberculosis, J Bone Joint Surg Am 41:877, 1959.
171. Dee PE, Smith RG, Gullickson MJ, et al: The orthopedist and apical
lung carcinoma, J Bone Joint Surg Am 42:605, 1960.
172. Demaziere A, Wiley AM: Primary chest wall tumor appearing as
frozen shoulder: review and case presentations, J Rheumatol 18:911,
1991.
173. Smith CR, Binder AI, Paice EW: Lesions of the mid-shaft of the
humerus presenting as shoulder capsulitis, Br J Rheumatol 29:386,
1990.
174. Dickson JA, Crosby EH: Periarthritis of the shoulder: an analysis of
two hundred cases, JAMA 99:2252, 1932.
175. McLaughlin HL: On the frozen shoulder, Bull Hosp Jt Dis 12:383,
1951.
176. Lundberg BJ: The frozen shoulder, Acta Orthop Scand 119:59, 1969.
177. Rowe CR, Leffert RD: Idiopathic chronic adhesive capsulitis. In
Rowe CR, editor: The shoulder, New York, 1988, Churchhill Livingstone, p 155.
178. Coventry MB: Problem of the painful shoulder, JAMA 151:177,
1953.
179. Waldburger M, Meier JL, Gobelet C: The frozen shoulder: diagnosis
and treatment, Clin Rheumatol 11:364, 1992.
180. Neviaser AS, Hannafin JA: Adhesive capsulitis: a review of current
treatment, Am J Sports Med 38:2346, 2010.
181. Fareed DO, Gallivan WR Jr: Office management of frozen shoulder
syndrome: treatment with hydraulic distention under local anesthesia, Clin Orthop Relat Res 242:177, 1989.
182. Rizk TE, Pinalls RA, Talaiver AS: Corticosteroid injections in adhesive capsulitis: investigation of their value and site, Arch Phys Med
Rehabil 72:20, 1991.
183. Hill JJ Jr, Bogumill H: Manipulation in the treatment of frozen
shoulder, Orthopedics 11:1255, 1988.
664.e4
PART 6 | DIFFERENTIAL DIAGNOSIS OF REGIONAL AND DIFFUSE MUSCULOSKELETAL PAIN
184. Rowe CR: Dislocations of the shoulder. In Rowe CR, editor: The
shoulder, New York, 1988, Churchill Livingstone.
185. Fu FH, Harner CD, Klein AH: Shoulder impingement syndrome: a
clinical review, Clin Orthop Relat Res 269:162, 1991.
186. Walch G, Bioleau P, Noel E: Impingement of the deep surface of the
supraspinatus tendon on the posterosuperior glenoid rim: an
arthroscopic study, J Shoulder Elbow Surg 1:238, 1992.
187. Altchek DW, Warren RF, Ortiz G: T-plasty: a technique for treating
multidirectional instability in the athlete, Orthop Trans 13:560,
1989.
188. Neer CS, Foster CR: Inferior capsular shift for involuntary and multidirectional instability of the shoulder: a preliminary report, J Bone
Joint Surg Am 62:897, 1980.
189. Roos DB: Congenital anomalies associated with thoracic outlet syndrome: anatomy, symptoms, diagnosis and treatment, Am J Surg
132:771, 1976.
190. Leffert RD: Thoracic outlet syndrome. In Gelberman RH, editor:
Operative nerve repair and reconstruction, Philadelphia, 1991, JB Lippincott, p 1177.
191. Urschel HC, Paulson DL, MacNamara JJ: Thoracic outlet syndrome,
Ann Thorac Surg 6:1, 1968.
192. Spillane JD: Localized neuritis of the shoulder girdle: a report of 46
cases in the MEF, Lancet 2:532, 1943.
193. Parsonage MJ, Turner JWA: Neurologic amyotrophy: the shoulder
girdle syndrome, Lancet 1:1973, 1948.
194. Turner JWA, Parsonage MJ: Neurologic amyotrophy (paralytic brachial neuritis): with special reference to prognosis, Lancet 2:209,
1957.
195. Bacevich BB: Paralytic brachial neuritis, J Bone Joint Surg Am 58:262,
1976.
196. Walsh NE, Dumitru D, Kalantri A, et al: Brachial neuritis involving
the bilateral phrenic nerves, Arch Phys Med Rehabil 68:46, 1987.
197. Hershman EB, Wilbourn AJ, Bergfield JA: Acute brachial neuropathy in athletes, Am J Sports Med 17:655, 1989.
198. Tsairis P, Dyck PJ, Mulder DW: Natural history of brachial plexus
neuropathy, Arch Neurol 27:109, 1972.
199. Szabo RM: Carpal tunnel syndrome—general. In Gelberman RH,
editor: Operative nerve repair and reconstruction, Philadelphia, 1991,
JB Lippincott, p 869.
200. Slater RR, Bynum DK: Diagnosis and treatment of carpal tunnel
syndrome, Orthop Rev 22:1095, 1993.
201. Narakas AO: Compression and traction neuropathies about the
shoulder and arm. In Gelberman RH, editor: Operative nerve repair
and reconstruction, Philadelphia, 1991, JB Lippincott, p 1147.
202. Bigliani L, Perez-Sanz JR, Wolfe IN: Treatment of trapezius paralysis,
J Bone Joint Surg Am 67:871, 1985.
203. Chavez JP: Pectoralis minor transplanted for paralysis of the serratus
anterior, J Bone Joint Surg Br 33:21, 1951.
204. Marmor L, Bechtal CO: Paralysis of the serratus anterior due to
electric shock relieved by transplantation of the pectoralis major
muscle: a case report, J Bone Joint Surg Am 45:156, 1983.
205. Cahill BR, Palmer RE: Quadrilateral space syndrome, J Hand Surg
8:65, 1983.
206. Jobe FW, Tibone JE: The shoulder in sports. In Rockwood CA,
Matsen FA, editors: The shoulder, Philadelphia, 1990, WB Saunders,
p 961.
207. Cahill BR: Quadrilateral space syndrome. In Omer GE Jr, Spinner
MD, editors: Management of peripheral nerve problems, Philadelphia,
1980, WB Saunders, p 56.
208. Bretzke CA, Crass JR, Craig EV, et al: Ultrasonography of the rotator
cuff: normal and pathologic anatomy, Invest Radiol 20:311, 1985.
209. Rengachary SS, Neft JP, Singer PA, et al: Suprascapular entrapment
neuropathy: a clinical, anatomical and comparative study, Neurosurgery 5:441, 1979.
210. Mallon WJ, Wison RJ, Basamania CJ: The association of suprascapular neuropathy with massive rotator cuff tears: a preliminary report,
J Shoulder Elbow 15:395, 2006.
211. Costouros JG, Porramatikul M, Lie DT, Warner JJ: Reversal of suprascapular neuropathy following arthroscopic repair of massive supraspinatus and infraspinatus rotator cuff tears, Arthroscopy 23:1152,
2007.
212. Habermeyer P, Rappaport D, Wiedermann E, et al: Incisura scapulae
syndrome, Handchir Mikrochir Plast Chir 22:120, 1990.
213. Martin SD, Warren RF, Martin TL, et al: Suprascapular neuropathy,
J Bone Joint Surg Am 79:1159, 1997.
214. Fritz RC, Helms CA, Steinbach LS, et al: Suprascapular nerve
entrapment: evaluation with MR imaging, Radiology 182:437, 1992.
215. Ferretti A, Cerullo G, Russo G: Suprascapular neuropathy in volleyball players, J Bone Joint Surg Am 69:260, 1987.
216. Rask MR: Suprascapular nerve entrapment: a report of two cases
treated with suprascapular notch resection, Clin Orthop Relat Res
123:73, 1977.
217. Solheim LF, Roaas A: Compression of the suprascapular nerve after
fracture of the suprascapular notch, Acta Orthop Scand 49:338, 1978.
218. Post M, Grinblat E: Suprascapular nerve entrapment: diagnosis and
results of treatment, J Shoulder Elbow Surg 2:197, 1993.
219. Hadley MN, Sonntag VK, Pittman HW: Suprascapular nerve entrapment: a summary of seven cases, J Neurosurg 64:843, 1986.
220. Boykin RE, et al: Current concepts review: suprascapular neuropathy,
J Bone Joint Surg Am 92:2348, 2010.
221. Rockwood CA Jr: Fractures and dislocations of the shoulder, part II.
In Rockwood CA Jr, Green DP, editors: Fractures, Philadelphia, 1975,
JB Lippincott, p 262.
222. Edlund E, Johnsson U, Lidgren L, et al: Palmoplantar pustulosis and
sternocostoclavicular arthro-osteitis, Ann Rheum Dis 47:809, 1988.
223. Lissens M, Bruyninckx F, Rossele N: Condensing osteitis of the
clavicle: report of two cases and review of the literature, Acta Belg
Med Phys 13:235, 1990.
224. Mitchell SW: Phantom limbs, Popular Literature & Science 8:563,
1871.
225. Bonica JJ: Causalgia and other reflex dystrophies. In Bonica JJ, editor:
Management of pain, Philadelphia, 1979, Lea & Febiger, p 139.
226. Evans JA: Reflex sympathetic dystrophy, Surg Gynecol Obstet 82:36,
1946.
227. Steinbrocker O: The shoulder-hand syndrome: present perspective,
Arch Phys Med 49:388, 1968.
228. Brown C: Compressive invasive referred pain to the shoulder, Clin
Orthop Relat Res 173:55, 1983.
229. Dahlin DC: Bone tumors, Springfield, IL, 1978, Charles C Thomas.
230. DePalma AF: Loss of scapulohumeral motion, Ann Surg 135:193,
1952.
231. Pancoast HK: Importance of careful roentgen ray investigation of
apical chest tumors, JAMA 83:1407, 1923.
232. Vargo MM, Flood KM: Pancoast tumor presenting as cervical radiculopathy, Arch Phys Med Rehabil 71:606, 1990.
233. Brown EA, Arnold LR, Gower PE: Dialysis arthropathy: complication of long term treatment with haemodialysis, BMJ 292:163, 1986.
234. Salvarani C, Gabriel SE, O’Fallon WM, et al: Epidemiology of polymyalgia rheumatica in Olmsted County, Minnesota, 1970-1991,
Arthritis Rheum 39:369, 1995.
235. Ytterberg S: Polymyalgia rheumatica: clinical features and management, Primary Care Case Reviews 4:89, 2001.