interdisciplinary patient care assessment
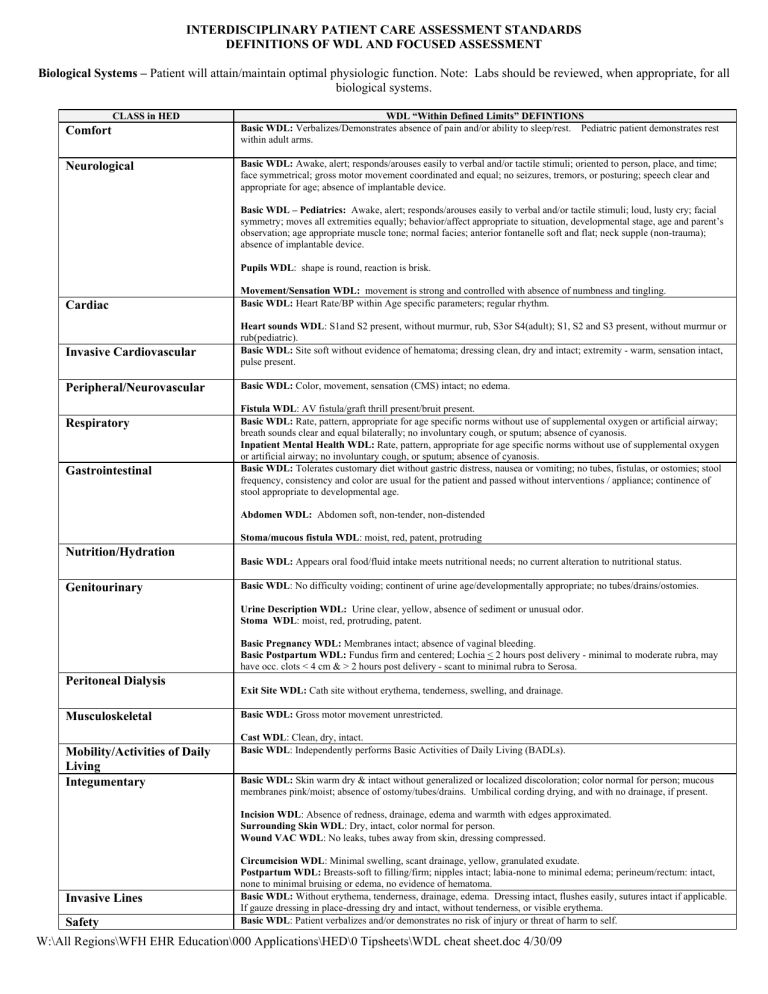
INTERDISCIPLINARY PATIENT CARE ASSESSMENT STANDARDS
DEFINITIONS OF WDL AND FOCUSED ASSESSMENT
Biological Systems – Patient will attain/maintain optimal physiologic function. Note: Labs should be reviewed, when appropriate, for all biological systems.
Comfort
CLASS in HED
Neurological
Cardiac
Invasive Cardiovascular
Peripheral/Neurovascular
Respiratory
Gastrointestinal
Nutrition/Hydration
Genitourinary
Peritoneal Dialysis
Musculoskeletal
Mobility/Activities of Daily
Living
WDL “Within Defined Limits” DEFINTIONS
Basic WDL: Verbalizes/Demonstrates absence of pain and/or ability to sleep/rest. Pediatric patient demonstrates rest within adult arms.
Basic WDL: Awake, alert; responds/arouses easily to verbal and/or tactile stimuli; oriented to person, place, and time; face symmetrical; gross motor movement coordinated and equal; no seizures, tremors, or posturing; speech clear and appropriate for age; absence of implantable device.
Basic WDL – Pediatrics: Awake, alert; responds/arouses easily to verbal and/or tactile stimuli; loud, lusty cry; facial symmetry; moves all extremities equally; behavior/affect appropriate to situation, developmental stage, age and parent’s observation; age appropriate muscle tone; normal facies; anterior fontanelle soft and flat; neck supple (non-trauma); absence of implantable device.
Pupils WDL : shape is round, reaction is brisk.
Movement/Sensation WDL: movement is strong and controlled with absence of numbness and tingling.
Basic WDL: Heart Rate/BP within Age specific parameters; regular rhythm.
Heart sounds WDL : S1and S2 present, without murmur, rub, S3or S4(adult); S1, S2 and S3 present, without murmur or rub(pediatric).
Basic WDL: Site soft without evidence of hematoma; dressing clean, dry and intact; extremity - warm, sensation intact, pulse present.
Basic WDL: Color, movement, sensation (CMS) intact; no edema.
Fistula WDL : AV fistula/graft thrill present/bruit present.
Basic WDL: Rate, pattern, appropriate for age specific norms without use of supplemental oxygen or artificial airway; breath sounds clear and equal bilaterally; no involuntary cough, or sputum; absence of cyanosis.
Inpatient Mental Health WDL: Rate, pattern, appropriate for age specific norms without use of supplemental oxygen or artificial airway; no involuntary cough, or sputum; absence of cyanosis.
Basic WDL: Tolerates customary diet without gastric distress, nausea or vomiting; no tubes, fistulas, or ostomies; stool frequency, consistency and color are usual for the patient and passed without interventions / appliance; continence of stool appropriate to developmental age.
Abdomen WDL: Abdomen soft, non-tender, non-distended
Stoma/mucous fistula WDL : moist, red, patent, protruding
Basic WDL: Appears oral food/fluid intake meets nutritional needs; no current alteration to nutritional status.
Basic WDL : No difficulty voiding; continent of urine age/developmentally appropriate; no tubes/drains/ostomies.
Urine Description WDL: Urine clear, yellow, absence of sediment or unusual odor.
Stoma WDL : moist, red, protruding, patent.
Basic Pregnancy WDL: Membranes intact; absence of vaginal bleeding.
Basic Postpartum WDL: Fundus firm and centered; Lochia < 2 hours post delivery - minimal to moderate rubra, may have occ. clots < 4 cm & > 2 hours post delivery - scant to minimal rubra to Serosa.
Exit Site WDL: Cath site without erythema, tenderness, swelling, and drainage.
Basic WDL: Gross motor movement unrestricted.
Cast WDL : Clean, dry, intact.
Basic WDL : Independently performs Basic Activities of Daily Living (BADLs).
Integumentary
Invasive Lines
Safety
Basic WDL: Skin warm dry & intact without generalized or localized discoloration; color normal for person; mucous membranes pink/moist; absence of ostomy/tubes/drains. Umbilical cording drying, and with no drainage, if present.
Incision WDL : Absence of redness, drainage, edema and warmth with edges approximated.
Surrounding Skin WDL : Dry, intact, color normal for person.
Wound VAC WDL : No leaks, tubes away from skin, dressing compressed.
Circumcision WDL : Minimal swelling, scant drainage, yellow, granulated exudate.
Postpartum WDL: Breasts-soft to filling/firm; nipples intact; labia-none to minimal edema; perineum/rectum: intact, none to minimal bruising or edema, no evidence of hematoma.
Basic WDL: Without erythema, tenderness, drainage, edema. Dressing intact, flushes easily, sutures intact if applicable.
If gauze dressing in place-dressing dry and intact, without tenderness, or visible erythema.
Basic WDL : Patient verbalizes and/or demonstrates no risk of injury or threat of harm to self.
W:\All Regions\WFH EHR Education\000 Applications\HED\0 Tipsheets\WDL cheat sheet.doc 4/30/09
Maternal Adaptation
Fetal Well-Being/Uterine
Activity
Coping
Spiritual/Cultural/Diversity/
Valuing
Routine Cares: tasks and activities guided by policies, procedures, and scope of practice
.
Intravenous Therapy
-IV site cares done per policy
-Tubing changes done per policy
- IV/site checks per policy.
Basic WDL: Activity/rest: reports physically rested, rejuvenated after sleep, has energy for cares; Self-concept: expresses feelings about self and birth experience, demonstrates positive affect and behavior; Role function: performs self and baby cares (if medically stable); Interdependence: demonstrates positive mom/baby interaction, support person present.
Basic Fetal Movement WDL: movement present and perceived as normal fetal movement per pt.
Basic Fetal Heart Tones WDL: baseline FHT’s 110-160 bpm and regular.
Basic Fetal Heart Rate Tracing WDL: FHR reactive for GA, average to moderate long-term variability.
Basic Uterine Activity WDL: Contractions/Cramping/Tightenings--Antepartum=less than 6 per hour; Intrapartum= contraction strength appropriate to stage of labor, lasting < 2 min., fully relaxed between contractions.
Basic WDL: The patient/family verbalizes/demonstrates emotional comfort/well being and/or effectively manages stressors (as evidenced by mood, emotion and affect).
Basic WDL: The patient/family will verbalize and/or demonstrate satisfaction that their beliefs, values, cultural, or spiritual practices have been accommodated and supported.
Personal Hygiene per patient condition/need/request may include but are not limited to:
- Bathing
- Linen Change
- Grooming
- Incontinence Care
- Skin Care
- Hand washing
- Assist or turn patients per policy.
- Pressure reductions to bony prominences.
- Encourage or provide weight shift frequently per patient condition.
- HOB <30 degrees unless contraindicated.
- Use appropriate equipment for lifting or transferring.
Pediatric Developmental Needs
- Age appropriate stimulation
- Comfort measures
Admission:
- Admission information provided.
- Report given/received if applicable.
- Orientation to room, call light, and bed controls
- ID bracelet applied
Safety
- Handoff communication given/received as applicable
- Alarms and equipment are engaged and appropriately set with signage when indicated.
- Call light and personal items within reach; reinforce call light use as needed.
- Bed in low position with wheels locked.
- ID/alert indicators on at all times.
- Communication devices are available to patients.
- Reinforcement of no smoking policy if needed.
- Side rails per patient condition/policy/procedure/need/request.
- Routine tubing/drainage system maintenance per policy.
- Standard precautions are used at all times.
Medication Teaching:
- Medication administered during the shift were reviewed with the patient/significant other.
- Initiation of a new medication.
- This may include: indications, actions, potential side effects and potential food-drug interactions.
In Continuity of Care:
Transfer:
- All records, medication, and belongings are transferred, the patient is accompanied by appropriate personnel and means of transport based on patient need.
- Report given/received per hand-off standard.
Discharge:
- Report given/received if applicable.
- Personal items & valuables returned to patient.
- The patient is discharged to the exit via appropriate mode of transportation and accompanied by personnel per policy.
- Sent home with prescriptions and DC instructions.
Interdisciplinary Standard of Care Definitions :
INTERDISCIPLINARY STANDARDS OF PRACTICE
Interdisciplinary Standards of Practice describe a competent level of patient care as demonstrated by critical thinking processes that include the components of assessment, diagnosis, outcomes identification, planning, implementation and evaluation. The critical thinking process encompasses all significant actions taken by clinicians, and forms the foundation for clinical decision-making. Each discipline provides care supporting these standards but also within their legally defined scope of practice.
STANDARDS OF PRACTICE
I.
Assessment: The clinician collects comprehensive data pertinent to the patient’s health or the situation. a.
Patient acute care needs are determined through a comprehensive assessment and screening. b.
Data is collected in a collaborative manner to avoid duplication. c.
Data collected is documented and retrievable by all disciplines. d.
Patient need and condition will determine the frequency of assessment.
For documentation purposes, the following are defined:
Basic assessment : minimum assessment performed each time a component is assessed.
Focused assessment : more detailed assessment based on information gathered in basic assessment; required whenever Basic assessment is not within defined limits, or whenever further assessment is required based on identified or potential risk.
•
Family refers to two or more persons who are related in any way – biologically, emotionally or legally. Patients and families define their
“family” and determine how they will participate in care and decision-making.