Facial Plast Surg Clin N Am 12 (2004) 311 – 321
Superficial skin resurfacing
Ranella J. Hirsch, MDa, Steven H. Dayan, MDb,*, Anil R. Shah, MDc
a
Skincare Doctors, 777 Concord Avenue, Cambrige, MA 02138, USA
Division of Facial Plastic Surgery, Department of Otolaryngology – Head and Neck Surgery, University of Illinois at Chicago,
2913 Commonwealth Street, Suite 430, Chicago, IL 60657, USA
c
Department of Otolaryngology – Head and Neck Surgery, University of Illinois at Chicago, 1855 West Taylor Street, Chicago,
IL 60612, USA
b
Anatomy of the skin
The approach to superficial resurfacing of the skin
necessitates a thorough understanding of the skin’s
distinct anatomy and histology. The epidermis is the
most superficial layer of the skin and provides a
critical barrier of protection. The principal building
block of the epidermis is a keratinocyte. The epidermis is composed of four distinct layers: the cornified,
granular, spinous, and basal layers. The cornified
layer is the most superficial and provides significant
protection to the skin. It is formed from flattened,
enucleate keratinocytes and compacted keratin granules. It varies in thickness, with the eyelid being the
thinnest and the palms and soles the thickest. The
granular cell layer contains keratinocytes and lamellar
bodies, which contribute to the cornification of the
skin. The spinous layer contains keratinocytes as well
as a variety of immunologic cells. The basal layer, the
deepest layer of the epidermis, contains basal cells
whose duplicative effort replaces the cells of the
superficial layers every 2 weeks. The basal layer also
contains melanin producing melanocytes, which provide pigmentation in the skin.
The dermis has the important function of thermoregulation and supports the vascular network to supply the avascular epidermis with nutrients. The dermis
is subdivided into two zones, a papillary dermis and
a reticular layer. The dermis contains mostly fibroblasts, which are responsible for secreting collagen,
* Corresponding author.
E-mail address: Docdayan@aol.com (S.H. Dayan).
elastin, and the viscous ground substance that gives
support and elasticity of the skin. Also present are
immune cells that are involved in defense against
foreign invaders passing through the epidermis.
There are two main types of collagen in the dermis.
Type I collagen, constituting 80% of dermal collagen,
imparts tensile strength to the dermis. Type III collagen, constituting 15% of dermal collagen, anchors the
epidermis to the dermis. Papillary dermis is made
primarily of Type III collagen with a small amount
of Type I collagen and fibronectin. Reticular dermis
is primarily made of Type I collagen with Type III
collagen and fibronectin serving adjunct roles [1].
Elastic fibers constitute approximately 3% of the
dermis and provide the skin elasticity and resilience.
Histopathology
After the age of 28, the first signs of skin aging
begin to appear [2]. Intrinsically aged skin results in
atrophy of skin components. Although aged skin is
thin with reduced elastic capacity, if there has been
minimal sun exposure clinically, aged skin is smooth
and unblemished. Collagen production and crosslinking of the distinct collagen bundles is decreased.
Dermal elastic fibers are fewer, thicker, and less
functional. Decreasing production of sebum that
accompanies maturation of the skin explains the
frequent finding of xerosis in mature patients.
Environmental factors such as sun exposure and
smoking greatly accelerate these changes [3]. Dermatoheliosis, also known as actinically damaged or
photoaged skin, is morphologically and histologically
1064-7406/04/$ – see front matter D 2004 Elsevier Inc. All rights reserved.
doi:10.1016/j.fsc.2004.02.006
312
R.J. Hirsch et al / Facial Plast Surg Clin N Am 12 (2004) 311–321
distinct from intrinsically, nonsolar exposed aged
skin. Photoaged skin clinically presents as deep
rhytides, uneven pigmentation and mottling, and in
its most severe form, a thickened texture reminiscent
of leather. Most cutaneous damage secondary to that
caused by ultraviolet radiation is to the dermal connective tissues, which is largely caused by increasing important matrix metalloproteinases responsible
for the orderly destruction of collagen fibers, which in
turn keeps in check total production [4]. Characteristic dermal findings of actinically damaged skin include haphazard arrangement of collagen and elastin
fibers, degradation of collagen, breakdown in elastic
fibers known as elastosis, and excess dermal melanosomes, telangiectasias, and precancerous lesions
known as actinic keratosis [5].
The term resurfacing encompasses many arenas.
This spectrum includes retinoids and other topical
preparations, varied depths of chemical peeling, dermabrasion and microdermabrasion, ablative and
nonablative resurfacing, and one of the newest technologies, radiofrequency coblation. Retinoids are
known to reverse photodamage and increase epidermal turnover and the production of dermal collagen
and elastin. Importantly, they have been shown to
stimulate neoangiogenesis, an effect that often can
be seen in the early period of titration. For those patients who cannot tolerate retinoids, retinols are an
option. Retinols are vitamin A aldehydes, and they
penetrate the skin well. They are converted into small
amounts of tretinoin but are tolerated with significantly less irritation.
Chemical peeling
Cutaneous resurfacing
Skin resurfacing by the cosmetic surgeon is a
process that causes a controlled injury to skin and
then stimulates a wound healing response. In response to injury, fibroblasts in the papillary dermis
increase production of type I and type III procollagen
in addition to transforming growth factor beta-1. The
collagen increase in turns thickens the dermis, which
enhances the tensile strength of the skin and yields
the clinical appearance of rejuvenation.
Skin resurfacing is most commonly classified on
the basis of injury depth. Superficial wounding
extends to the stratum granulosum or papillary dermis. Medium-depth wounding results from extension
into the upper reticular dermis. Deep wounding
extends into the midreticular dermis. If the resurfacing technique is limited to superficial injury to the
epidermis and superficial papillary dermis, healing
generally will occur without scarring. If the injury
extends deep into reticular dermis beyond adnexal
structures, scarring is the likely result [6]. Invasive
treatments for the treatment of solar damaged skin
and facial rhytids include ablative laser resurfacing
with carbon dioxide and erbium laser wavelengths,
dermabrasion, and deep chemical peeling agents.
Ablative resurfacing achieves the outcome of rejuvenation by the destruction of the outermost and thus
most photodamaged layers of the skin. The subsequent laying down of newly formed collagen and a
tightened skin appearance follows this removal [7].
Recently, multiple studies have been reported the use
of nonablative techniques for skin rejuvenation. In
this article, we review options we can offer patients
for skin rejuvenation.
Chemical peels are the application of chemical
agents that damage skin in a controlled manner.
These agents can be subdivided into superficial peels,
which remove the stratum corneum, and superficial
peels, which remove the entire epidermis. Superficial
peels require repetitive peeling sessions to obtain
optimal results. The limiting therapeutic factor of
superficial peels is its depth and dermal pigmentation,
particularly evident in cases of severe dermatoheliosis
and melasma, which will not be improved despite
repeated application.
Since the days of ancient Egypt when it was
rumored that Cleopatra used the debris of the bottom
of wine barrels for facial rejuvenation, people have
been using chemoexfoliation methods to rejuvenate
skin. The original chemoexfoliant was lactic acid, an
active ingredient of sour milk that was used topically
by the nobles as part of an ancient skin rejuvenation
regimen. In the Middle Ages, old wine with tartaric
acid as its active ingredient was used for the same
purpose. Today, these historical chemoexfoliants are
known to contain alpha hydroxy acids, which are the
active ingredients responsible for the skin exfoliation.
Modern day chemical peeling originally was promoted by dermatologists, such as P.G. Unna, who
first described the properties of salicylic acid, resorcinol, phenol, and trichloroacetic acid (TCA). Slowly,
the early practitioners of chemical peels began to
develop other peeling agents for varying depths of
penetration. In the 1960s, Baker and Gordon developed a deep peeling agent, which was able to smooth
deeper furrows, especially around the mouth. From
the 1980s to the present, an explosion has occurred in
the mass of research on this subject, with the eluci-
R.J. Hirsch et al / Facial Plast Surg Clin N Am 12 (2004) 311–321
Table 1
Chemical peel classification
Peel depth
Depth of penetration
Clinical depth
Superficial
Medium
0.06 mm
0.45 mm
Deep
0.6 mm
Granular layer
Papillary to upper
reticular dermis
Midreticular dermis
Adapted from Matarasso SL, Glogau RG. Chemical face
peels. Dermatol Clin 1991;9(1):131 – 50; with permission.
dation of many different types of peels, each for a
specific range of problems [8].
The chemical peel produces a controlled partial
thickness injury to the skin. After the insult to the
skin, a wound healing process ensues that can regenerate epidermis from surrounding epithelium and
adnexal structures, which leads to the development
of new dermal connective tissue. The result is an
improved clinical appearance of the skin, with fewer
rhytids and decreased pigmentary dyschromia.
To understand the peeling process, there are a few
key concepts. The concentration and pH of a peeling agent determine its effectiveness. Generally the
greater the concentration, the more potent the chemical agent; however, concentration may vary based on
the method of dilution. The strongest method is a
dilution of a saturated solution. The weakest method is
grams of acid crystal mixed to 100 mL of water. (The
weight to weight method and the weight to volume
method are intermediate in determining the concentration of the peeling agent.) The pH is also important
in determining the effectiveness of the peeling agent.
This occurs when the free acid component is biologically active, that is, when the pH is close to the pKA.
Chemical peeling is classified by the depth of
penetration (Table 1) [9]. The process of healing
involves coagulation and inflammation and is followed by reepithelialization, granulation tissue formation, angiogenesis, and a prolonged period of
collagen remodeling. It is this remodeling that
313
accounts for the continuing appearance of clinical
improvement in the months following the peel procedure. A useful grading system for pretreatment
classification is the Glogau system(Table 2) [10].
Peel depth can be modulated in response to the
individual patient’s classification.
Application of most peeling agents is similar.
Before application, the skin to be treated is first
defatted with acetone or rubbing alcohol. The clinical
endpoint is a brisk erythema. Because most chemical
peels are lipophobic, this facilitates greater depth
and promotes even distribution of the peel. The peel
is applied to subunits of the face with gauze or a
cotton-tipped applicator. To provide a consistent
effect it is important to apply the chemical peel
evenly and prevent pooling of the agent on the face.
The peel is blended with untreated skin by feathering
it at the edges.
Alpha hydroxy acids
Alpha hydroxy acids (AHAs) have been used for
thousands of years to improve the appearance of the
face. Chemically, AHAs are organic carboxylic acids
with a hydroxyl group at the alpha position. AHAs
are known to normalize keratinization by diminishing
corneocyte adhesion in the granular cell layer; this in
turn promotes improved cell turnover. Commonly
used AHAs derive from fruit and dairy products,
such as glycolic acid from sugar cane, lactic acid
from fermented milk, citric acid from fruits, tartaric
acid from grapes, and malic acid from apples. With
its particular affinity for the skin, glycolic acid is the
most commonly used.
The efficacy and penetrating depths of assorted
AHA preparations are greatly dependant on their
concentration, the vehicle, and the pH. Brands available for over the counter use are set at 3% to 10%
concentrations and induce a slow exfoliation over
several weeks. This strength can also be used as a
Table 2
Glogau classification of photoaging
Group I—Mild
Group II—Moderate
Group III—Advanced
Group IV—Severe
Age 28 – 35
Age 35 – 50
Age 50 – 60
Age 65 – 70
No keratoses
Little wrinkling
No scarring
Little makeup
Early actinic keratoses
Early wrinkling-smile lines
Mild scarring
Small amt makeup
Obvious actinic keratoses
Wrinkling at rest
Moderate acne scarring
Always wear makeup
Actinic keratoses/skin cancer
Wrinkling/laxity
Severe acne scarring
Makeup cakes on
Adapted from Glogau RG. Aesthetic and anatomic analysis of the aging skin. Semin Cutan Med Surg 1996;15(3):134 – 8;
with permission.
314
R.J. Hirsch et al / Facial Plast Surg Clin N Am 12 (2004) 311–321
pretreatment for a higher concentration peel or
another resurfacing modality. Higher strengths may
be used by supervised estheticians (8% – 30%) for
light peels. The highest strengths (40% – 70%) are
available for dermatologists and cosmetic surgeons
for in-office peels.
The cautions are intuitive. The surgeon must take
care to note the expiration date as the peel will lose
effective potency with time. Solutions with a pH
below 2 that contain only free glycolic acid have
the potential to induce crusting and necrosis. These
products can be buffered with an addition of sodium
bicarbonate or sodium hydroxide, resulting in a
higher pH and a weaker acid. This is independent
of the concentration used. The desquamative and
proliferation-stimulating effects of lactic acid are pH
and concentration dependent, suggesting the ‘‘free
acid’’ concentration is the active moiety [11].
Standard strength of professional grade AHA
peels is 50% or higher. Alpha hydroxy peels differ
from other peels in that they are time dependent. The
time to peel is dependent on both the concentration
and the pH of the peel. Higher concentrations and
lower pH require shorter peeling periods. After placement of an AHA preparation, the skin becomes
erythematous. A frost is not desirable in an alpha
hydroxy peel because it denotes penetration depth
into the dermis [12].]] The AHA peel requires neutralization with cold water or a basic solution. Mild
stinging and erythema typically disappears after
1 hour. The subsequent exfoliation takes place over
a few days with reepithelialization in about 1 week.
Multiple treatments may be required for the desired
result and should be spaced at least 3 weeks to allow
the epidermis to recover [13].
Complications of AHA peels are mild and temporary when the peel is performed by trained professionals using standard techniques. Care is taken to
be certain the eyes are protected and that the patient
has no known allergies to any of the peel’s ingredients. Standard of care is for prescription retinoid
users to cease use of the agent for 2 to 3 days before a
superficial peel to aviod excess irritation. Patients are
susceptible to postinflammatory skin pigmentation
and require UV-A and UV-B protection both before
and after the peel [14].
Deeper than intended peeling may occur if neutralization is not performed within the correct window. In our experience, we also have seen increased
erythema and inflammation surrounding peeled areas
over sites recently augmented with bovine collagen
implants. We either avoid these areas with peeling or
defer placement of filler agents for a 2-week period
before peeling.
Jessner’s peel
A Jessner’s peel is a combination of salicylic acid,
14%, lactic acid, 14%, and resorcinol, 14%, in alcohol. It is considered a mild peeling agent. Its ability to
disrupt the barrier function of the epidermis is used
as an ideal primer for tricholoracetic acid (TCA)
peels. This allows TCA peels to penetrate safely and
evenly. Jessner’s solution peeling action is through
intense keratolysis. Alone, Jessner’s is an easy to use
peeling agent without timing restriction. Skin sloughing occurs within 2 to 4 days with subsequent epidermal regrowth [15].
Tricholoracetic acid
TCA typically is used as a superficial-intermediate-to-deep peeling agent in concentrations ranging
from 20% to 50%. TCA (10% – 35%) has been used
for many years and is safe to use at lower concentrations. At higher concentrations, such as 50% and
above, TCA has a tendency to cause scarring and is
less manageable than other agents used for superficial
peels [16].
TCA is a keratocoagulant that produces a frost or
whitening of the skin, which is dependent on the
concentration used. Level I frosting, defined as erythema with streaky whitening of the face, is the
endpoint for superficial resurfacing. Level II frosting
is defined as white coated frosting with patches of
erythema showing through. Level III frosting, which
is associated with penetration through the papillary
dermis, is a solid white enamel frost with minimal
visible erythema. Level III frosting must be reserved
for areas of severe actinic damage [17].
TCA’s peeling mechanism of action at lower concentrations is through protein precipitation. Vigorous
rubbing of the agent, as compared with blotting,
yields a deeper penetration. This technique is not
time dependent, and the agent does not require neutralization. During the procedure, if frosting is not
uniform, reapplication may be performed until frosting of a desired plateau is reached. Once completed,
skin sloughing proceeds for several days, and reepithelialization is complete within 10 to14 days. Patient
discomfort is controlled with oral pain medications.
The results of TCA peels of superficial depths
are mild reversal of some fine wrinkles and improvement in dyspigmentation. The results may not be
that which is achieved by TCA 35% Jessner’s combination but the recovery period and risk are also
less [18].
R.J. Hirsch et al / Facial Plast Surg Clin N Am 12 (2004) 311–321
Salicylic acid
Beta hydroxy acids (BHA), also known as salicylic
acids, are not AHAs but are chemically defined as
having an organic carboxylic acid with a hydroxyl
group at the beta position. BHAs have more of a
predilection for sebum-containing cells and are lipid
soluble; therefore, they are an excellent peeling agent
for comedonal acne. Another benefit of salicylic acid
is that it does not need to be neutralized. After
applying BHA to the skin, salt formation on the skin
is seen [19].
Salicylic acid appears to provide a safe, mild rejuvenation to skin. A study by Grimes et al [20]
looked at concentrations of salicylic acid between
20% and 30% in Fitzpatrick skin types V and VI.
Eighty-eight percent of patients described a moderate
to significant improvement in acne, oily skin, textural
changes, melasma, and postinflammatory pigmentation. Minimal side effects occurred in 16% of patients.
Klingman et al [21] also demonstrated that BHAs
at 30% concentration were efficacious in photoaged
skin. They found reduction in fine lines, surface
roughness, and pigment spots.
Adverse effects, usually only found with high-dose
oral ingestion, include headache, nausea, and ringing
of the ears, each of which may be resolved with a few
glasses of water and rest. These have never been
reported with a peel procedure. Cutaneous side effects
are minimal and can include erythema and mild
irritation to the salt formation on the skin [22].
Dermabrasion
Dermabrasion is an older technique that removes
the epidermis and upper dermis by use of an abrasive
wheel driven by a high-speed engine. This mechanical removal yields a middermal wound. Healing is
achieved via reepithelialization and repigmentation
from the residual adnexae. Areas with diminished
numbers of adnexal structures, such as keloids and
hypertrophic scars, respond poorly to mechanical
dermabrasion, as these adnexae are not present [23].
Dermabrasion has been used less frequently since the
advent of laser resurfacing but still offers an excellent
option in the treatment of deep acne scars.
315
of performance and lack of downtime has made it a
patient favorite in the United States. Clinically, it is
mechanical debridement of the most superficial layers
of epidermis. It commonly involves the use of a
closed-loop, negative pressure system with debriding
aluminum oxide crystals to ablate the superficial
layers of the epidermis. Some systems use sodium
chloride, which is a positive pressure system [25].
Quality and purity can vary substantially among
the crystals. The substance most often used is aluminum oxide. It is usually preferred because of its
hardness, inertness, and superior abrasion qualities.
Alternative crystal mediums also are available and
range from bicarbonate sodium to salt. Advantages of
bicarbonate sodium is its purity and its ability to
dissolve in water during clean up, leaving no gritty
residue. A disadvantage is that it is softer than aluminum oxide and requires more passes.
Performance of a microdermabrasion treatment is
technically simple. No preoperative anesthesia or antibiotics are necessary. The handpiece has a vacuum
that draws in the skin as the handpiece is passed
over the area to be resurfaced. Depth of abrasion
is controlled by pressure of the crystals being propulsed, pressure of the handpiece, and speed of the
pass. The face typically requires two passes, with the
second pass perpendicular to the first one. Vertical
passes only are advisable for the neck area.
Historically, with microdermabrasion the assumption was that repetitive intraepidermal injury allowed
for gradual improvement of photodamaged skin by
stimulating fibroblast activity and new collagen
deposition in the dermis [26]. A recent study from
Freedman et al [27] suggests that microdermabrasion may indeed yield greater histologic improvement then previously realized, with treated patients
showing histologic evidence of thickening of the
epidermis and dermis, flattening of the rete pegs,
vascular ectasia, and perivascular inflammation, and
newly deposited collagen and elastic fibers as compared with control subjects. A study by Shim et al
[28] demonstrated a statistically significant improvement in roughness, mottled pigmentation, and overall
improvement in skin appearance in a small number
of patients.
Laser resurfacing
Microdermabrasion
Ablative
Microdermabrasion originated in Italy in 1985 by
Marini and Lo Brutto [24], who reported both gross
and histologic improvement in treated skin. Its ease
When performed by an experienced practitioner,
ablative laser skin resurfacing yields often dramatic
and reproducible improvement in the appearance of
316
R.J. Hirsch et al / Facial Plast Surg Clin N Am 12 (2004) 311–321
photoaged skin. It does so by reducing solar-induced
dyspigmentation and rhytids and improving allover
skin tone [29]. Histologically these changes correlate
with architectural normalization of the epidermis and
the formation of a dermal repair zone comprised of
parallel collagen arrays [30]. The two principal lasers used are the carbon dioxide (CO2) and erbium
yttrium-aluminum-garnet (Er:YAG) systems with
similar mechanisms: ablation of photodamaged skin,
thermal collagen contraction, and stimulation of immediate and delayed collagen remodeling.
Resurfacing requires an understanding of laser
biophysics and its interaction with skin. Laser is an
acronym for light amplification by stimulated emission of radiation. The therapeutic action of light
energy is the product of characteristics distinct to
laser light and resultant laser-tissue interactions. Laser light is monochromatic, that is, the emitted light is
of a single wavelength. At specific wavelengths,
specific absorption of light energy by a pigmented
target can occur. Another property is coherence, both
in time and space, analogous to a marching band in
step. A third property is collimation, which is the
emission of a powerful beam of light in a parallel
manner, which permits its focus into very small spot
sizes, which permits precise tissue destruction [31].
Lasers have several vital characteristics that influence their ultimate effects in tissue. The fluency,
power density, and frequency each function to adapt
the effect of laser light on tissue. Tissue ablation
occurs when the tissue is heated to its boiling point.
Depending on the absorbance of the host target tissue,
the laser may cause unintended damage to the surrounding tissue. This can be measured with the tissue
relaxation time. When the time of laser delivery is
greater than the tissue relaxation time, unintended
damage to the surrounding tissues results. When the
energy level is greater than the critical value for the
particular tissue and delivered in less than the thermal
relaxation time for that particular tissue, tissue is
ablated with minimal heat conduction to the surrounded tissues [32]. The understanding of this
principle of selective photothermolysis changed the
face of laser resurfacing and issued in a new era in the
treatment of photoaging.
The CO2 laser emits infrared light with a 10,600nm wavelength absorbed by intracellular and extracellular water. After this energy is absorbed, water is
immediately converted into steam with charring of
tissue and minimization of collateral tissue damage
[33]. Pulsed systems provide the further advantage of
minimizing damage to adjacent tissue [34]. In trained
hands, impressive results are achieved safely in the
treatment of severe photoaging. The major limiting
factor for this procedure is the extended duration
of recovery, with pronounced erythema for 3 to
6 months. Additionally, significant postoperative
complications such as oozing, bleeding, and infection
can occur [35]. Also of great concern is the risk of
delayed permanent hypopigmentation seen in up to
20% of patients when multiple-pass CO2 resurfacing
is performed [36,37].
The demand for less aggressive resurfacing modalities led to the development of the short-pulsed
Er:YAG laser. The Er:YAG laser, with a wavelength
of 2940 nm, produces laser irradiation in the near
infrared portion of the electromagnetic spectrum. This
wavelength corresponds to a main peak of water
absorption, one that is much more (10 – 15 times)
efficiently absorbed by superficial (densely water
containing) tissues. The Er:YAG arrived on the scene
to great enthusiasm as practitioners hoped for a
comparable clinical result to CO2 with more rapid
wound healing; however, Er:YAG resurfacing has
since been shown to yield less apparent clinical
improvement for rhytids than CO2 at equivalent
depths of treatment [38]. This is because the Er:YAG
system produces only about 5 to 20 mm of thermal
damage per pass, as opposed to the 50 to 125 mm of
thermal damage seen with each CO2 pass. Short
pulsed erbium treatment can be adjusted to go superficially, mimicking the benefit of a microdermabrasion, or it can go deeper with multiple stacked passes,
mimicking the benefits of CO2. Short pulsed erbium is
best used as a superficial treatment at the limits of
the dermis.
CO2 systems produce a significant amount of
thermal effect, which acts as a ‘‘heat sink’’ for the
next laser pass, thus yielding increased damaged
collagen and leading to an increase in new collagen
production [39]. Additionally, the Er:YAG system
offers the laser surgeon poor intraoperative hemostasis, unlike the excellent hemostasis provided by CO2.
Recently, modulated (short and long pulsed) Er:YAG
systems have been introduced to facilitate deeper
ablation of tissue and improve intraoperative hemostasis [40,41]. Indications favoring use of a short
pulsed Er:YAG system are mild to moderate photoaging and superficial dyspigmentation as well as
patients with darker skin phototypes [42]. The modulated systems offer results between that of CO2 and
short-pulsed Er:YAG systems.
Er:YAG systems yield photomechanical benefits
whereas the CO2 laser yields a photothermal effect.
The lack of a photothermal effect for the Er:YAG laser
means that heat does not dissipate deeper into the
surrounding tissues. There are fewer complications of
severe thermal damage with the Er:YAG laser; how-
R.J. Hirsch et al / Facial Plast Surg Clin N Am 12 (2004) 311–321
ever, this also translates to less collagen shrinkage
with the Er:YAG laser versus the CO2 laser [43].
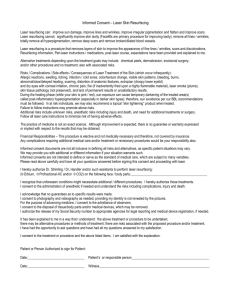
Er:YAG resurfacing may soon reemerge as a middle
ground option, providing patients with an moderate
improvement in skin texture and tone beyond that
achieved with microdermabrasion and superficial
treatments, yet without the associated downtime of
the deeper reaching modalities (Fig. 1).
Nonablative
The devices available for nonablative photorejuvenation can be split into two primary categories:
visible light devices 532 nm (green) and 585 nm
(yellow), light best suited to treat pigmentary and
vascular lesions. These wavelengths are strongly
absorbed by oxyhemoglobin and melanin in the epidermis and superficial dermis. Mid-infrared wavelength devices at 980 nm, 1320 nm, 1450 nm, and
1540 nm are coupled with cooling mechanisms that
serve to protect the epidermis while simultaneously
stimulating direct collagen remodeling in the dermis.
These mid-infrared wavelengths are absorbed primarily in water (intracellular and extracellular) and can
uniformly heat tissue independent of skin type [44].
317
While using a pulsed-dye laser for treatment of
vascular periocular lesions, it was noted that there
was a decrease in the clinical appearance of rhytids
[45]. Histologic improvement of dermal collagen also
was noted after treatment with the pulsed-dye laser.
Using these findings, Zelickson et al [46] evaluated
the use of a 585-nm pulsed-dye laser in the treatment
of facial rhytids and reported improvement. The
Zelickson report suggests that there also is potential
efficacy with lower fluences than used in the trial and
less associated purpura, the endpoint that patients
find least cosmetically acceptable.
The first system specifically designed for the
purpose of nonablative resurfacing was a 1320-nm
neodymium:yttrium-aluminum-garnet (Nd:YAG) laser (Cool Touch, Roseville, CA). The goal of this
system, similar to that of the previously described
systems, is improvement of rhytids without the creation of an open wound. The 1320-nm wavelength is
advantageous in its high scattering coefficient. Thus,
the laser irradiation scatters throughout the treated
dermis after nonspecific absorption by dermal water.
Studies have reported that this system is able to produce thermal stimulation of dermal fibroblasts within
the papillary and midreticular dermis while concomi-
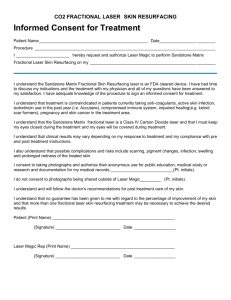
Fig. 1. Patient with mild rejuvenation seen after use of Er:YAG laser treatment. (A) Pretreatment. (B) Post treatment.
318
R.J. Hirsch et al / Facial Plast Surg Clin N Am 12 (2004) 311–321
tantly cooling the epidermis to protect it from undesired thermal injury [47].
Histologically, there is replacement of the irregular collagen bands with organized new collagen
fibrils [48]. In a 1999 study, Kelly et al [49] reported
the use of the 1320-nm wavelength Nd:YAG laser for
the treatment of facial rhytids. They reported statistically significant findings at 12 weeks. In another
study of similar technology, Goldberg et al [50] reported clinical improvement in 8 of the 10 patients in
the study. The Cooltouch was modified and reintroduced as the Cooltouch II, which delivers energy
densities up to 24 J/cm2 with a 10-mm spot handpiece. The laser handpiece has three roles: delivery of
the laser pulse, application of a thermal spray for
cryogen cooling, and a sensor for the assessment of
skin temperature at the surface.
Recently, Ross et al [51] described the Smoothbeam1450-nm diode laser system that was also
shown to be modestly effective for the nonablative
treatment of photoaged skin. The 1450-nm wavelength is extremely well absorbed by water. Sixteen
patients (14 periorbital, 2 perioral) with rhytids were
treated with split-face treatments: half had four visits
3 weeks apart with the 1450-nm laser device and the
contralateral side with cryogen cooling alone. The
laser uses spray cryogen cooling to protect the epidermis and permit selective dermal heating. The
authors reported mild to moderate improvement in
12 to 16 patients [51].
The long pulse 1064-nm laser with its low scattering coefficient and weak absorption by water and
melanin also has been shown to improve the appearance of coarse wrinkles and fine lines and to reduce
skin laxity. After seven treatment sessions spaced over
14 weeks, the patients’ subjectively graded improvements in their skin’s appearance mirrored masked
physician observers recognized improvements in the
same categories. This data reached statistical significance [52].
Intense pulsed light, a nonlaser light source, can
be delivered at a variety of wavelengths (590 to
1200 nm.) Filters permit the inclusion and exclusion
of given wavelengths [53]. With blockage of shorter
wavelengths, deeper wavelengths can be absorbed in
the dermis and yield nonablative dermal remodeling
[54]. Goldberg reported on five patients who underwent four sessions of intense pulsed light source
therapy and from whom pretreatment and 6-month
posttreatment biopsies were obtained. Their results
indicated histologic evidence of new upper papillary
dermal collagen formation [55]. The intense pulsed
light has particular utility for the treatment of dyschromias and mottling [56].
Thermal resurfacing
Thermal resurfacing, also referred to as cold ablation (coblation) or radiofrequency ablation is essentially removal of the outer layer of skin via bipolar
electrical current. It is a descendent of the bipolar
systems originally used in orthopedics to resurface
joint cartilage. Whereas lasers rely on heat to remove
tissue, coblation disrupts molecular bonds at the
cellular level by the movement of ions and free electrons, which strike the bonds and disrupt them [57].
The coblation procedure begins with application
of povidone iodine to the skin. A local anesthetic may
then be applied. Lastly, saline gel is placed over all of
the areas to be treated. This gel is essential because
the coblation device energizes particles in the saline
gel, which will consequently strike tissues and disrupt
tissues via their movement [58].
Coblation also can use a saline solution. Isotonic
saline is then passed over the stylet while the stylet
remains in constant contact with the skin. Three
bipolar strips separated by 1 mm are situated at the
end of a stylet. Ions within the isotonic saline are
energized by the bipolar frequency and form a
‘‘plasma’’ of charged ions able to break down molecular bonds within the tissue and cause separation
of the epidermal – dermal junction. The plasma is
theorized to form a plasma shield, decreasing both
the energy reaching the target tissue and reducing the
collateral tissue damage [59]. Skin is aggressively
precooled and cooled during electrical current production to protect the epidermis and dermis [60].
Topical and oral pain relief is given before the
procedure. For deeper treatments a local anesthetic
field block is performed. Antiviral and antibiotic
prophylaxis are given to all patients because the layer
of necrotic cobalted debris that will slough off after the treatment is a potential bacterial culture medium [61].
Coblation injury is reported to be in between that
of CO2 laser resurfacing and Er:YAG laser resurfacing. If the voltage is reduced so that the saline is not
transformed into plasma, small vessels can be coagulated, creating a bloodless field; however, some
authors have reported some bleeding with overaggressive wiping of skin, especially in those patients
with prominent extant telangiectasias at the time of
treatment. Ablation may be effective in some scar
revision. It is probably a less effective method to
reduce rhytids than CO2 or Er:YAG lasers [62].
Coblation also appears to have less erythema than
laser resurfacing. Grekin [63] reported less pronounced erythema and resolution within 2 months.
Coblation appears to offer potential as a superficial
R.J. Hirsch et al / Facial Plast Surg Clin N Am 12 (2004) 311–321
319
resurfacing device. Because of the limited studies on
thermal resurfacing, the ideal parameters of the device
are not yet known.
Contraindications to resurfacing
Given the significant potential morbidity after
cutaneous resurfacing procedures, all candidates must
receive an extensive preoperative treatment evaluation. Patients must be screened for their ability to
tolerate the necessary recuperation and unpleasant
cosmetic period immediately following the procedure. The preoperative medical evaluation should
include a complete medical history and any medication allergies. Patients with active cutaneous infections must be excluded from therapy.
Patients should be asked about any history of poor
scarring or keloid development, allergic tendencies,
connective tissue disorders, or a history of oral herpes
simplex virus. Recent literature suggests that patients
with a recent history of isotretinoin (Accutane) ingestion are at an increased risk for keloid development; consequently, these patients should not be
treated for 12 months after completion of the course
of therapy [64].
In expert hands, complications are minimal. The
exception is poor technique [65]. Most complications
occur during the postoperative reepithelialization
process. There are differing opinions on the prophylaxis of herpes infections [66,67]. We routinely prescribe prophylaxis for all Er:Yag and CO2 laser
procedures as well as TCA chemical peels regardless
of history. Seven percent of patients developing a
herpes infection after laser resurfacing do not report
any history of herpes labialis Fig. 2) By contrast,
superficial chemical peels limited to the epidermis
and superficial dermis that do not result in deepitheliazation are not routinely prophylaxed [68].
A history of resurfacing or surgical procedures
is another important possible contraindication. Some
authors list prior blepharoplasty or face lift within the
last 2 months as a relative contraindication to resurfacing because of the increased risk of scarring and
temporary altered blood supply postoperatively; however, there is documented evidence of successful
outcomes in patients who have had resurfacing done
simultaneously with facelifts. Nontheless, caution is
warranted when resurfacing an area with vascular
compromise secondary to a recent procedure. Additionally, patients who have had prior skin muscle flap
lower eyelid blepharoplasty through a subciliary
approach may have reduced lower lid laxity secondary to weakened orbicularis muscular support. Skin
Fig. 2. Severe herpes infection seen after laser resurfacing
with no history of herpes infections. The patient was treated
with valtrex and had a normal recovery.
contraction and further compromise to lower lid support following medium depth resurfacing of thin
lower eyelid skin can occurm placing the patient at
particular risk for ectropion.
Other pertinent historical facts include allergic or
hypersensitivity reactions to topical anesthetics, petrolatum, or lanolin. Although rare, allergies to these
agents can be problematic because they are used
routinely in superficial and deeper resurfacing protocols and can lead to extension of the dermal injury.
Also, patients with recurrent facial candidal or adenexal infections require precautionary measures before a superficial resurfacing procedure, and they may
be relatively contraindicated for a deeper treatment.
Summary
Best results for all rejuvenating modalities lie in
the joint hands of the cosmetic surgeon and the
patient. The absolute need for pretreatment education
and posttreatment care cannot be overemphasized.
Additionally, other adjunctive efforts such as judicious use of botulinum toxin and the use of filler
substances can optimize results. Ultimately it is a
combination of the surgeon’s skill and the patient’s
320
R.J. Hirsch et al / Facial Plast Surg Clin N Am 12 (2004) 311–321
compliance with instruction that determines the overall result. Setting realistic expectations for patients is
an absolute imperative and will serve to maximize
patient satisfaction.
References
[1] Gilchrest BA. Skin and aging process. Boca Raton, FL:
CRC Press; 1984. p. 1.120.
[2] Gilchrest BA. Cellular and molecular changes in aging
skin. J Geriatr Dermatol 1994;2:3 – 6.
[3] Hurley HH. Skin in senescience: a summation. J
Geriatr Dermatol 1993;1:55 – 61.
[4] Lavker RM. Topical therapy of aging skin. J Geriatr
Dermatol 1994;2:20 – 3.
[5] Lavker RM, Kligman AM. Chronic heliodermatitis:
a morphologic evaluation of chronic actinic dermal
damage with emphasis on the role of mast cells.
J Invest Dermatol 1988;90(3):325 – 30.
[6] Glogau RM. Chemical peeling and aging skin. J
Geriatr Dermatol 1994;2:30 – 5.
[7] Kauvar ANB, Geronemus RG. Histology of laser resurfacing. Derm Clinics 1997;15(3):459 – 67.
[8] Ridge JM, Siegle RJ, Zuckerman J. Use of alpha hydroxyl acids in the therapy of photoaged skin. J Am
Acad Dermatol 1990;23:932.
[9] Matarasso SL, Glogau RG. Chemical face peels.
Dermatol Clin 1991;9(1):131 – 50.
[10] Glogau RG. Aesthetic and anatomic analysis of the
aging skin. Semin Cutan Med Surg 1996;15(3):134 – 8.
[11] Thueson DO, Chan EK, Dechsli LH, Hahn GS. The
roles of pH and concentration in lactic acid-induced
stimulation of epidermal turnover. Dermatol Surg
1998;24(6):641 – 5.
[12] Van Scott E. Alpha hydroxyl acids: procedures for use
in clinical practice. Cutis 1989;43:222 – 8.
[13] Tung RC, Bergfeld WF, Vidimos AT, Remzi BK. Alpha-hydroxy acid-based cosmetic procedures: guidelines for patient management. Am J Dermatol 2000;
1(2):81 – 8.
[14] Tsai TF, Bowman PH, Jee SH, Maibach HI. Effects of
glycolic acid on light-induced skin pigmentation in
Asian and caucasian subjects. J Am Acad Dermatol
2000;43(2, pt. 1):238 – 43.
[15] Monheit GD. Advances in chemical peeling. Facial
Plast Surg Clin N Am 1994;2:5 – 9.
[16] Brody HJ. Variations and comparisons in medium
strength chemical peeling. J Dermatol Surg Oncol
1989;15:953 – 63.
[17] Rubin M. Manual of chemical peels. Philadelphia:
J.B. Lippincott; 1995.
[18] Monheit GD. The Jessner’s – TCA peel. Dermatol
Clin 1995;13:277 – 83.
[19] Leveque JL, Corcuff P, Rougier A, Pierard GE. Mechanism of action of a lipophilic salicylic acid derivative on normal skin. Eur J Dermatol 2002;12(4):
XXXV – XXXVIII.
[20] Grimes PE. The safety and efficacy of salicylic acid
chemical peels in darker racial-ethnic groups. Dermatol
Surg 1999;25(1):18 – 22.
[21] Kligman D, Kligman AM. Salicylic acid peels for the
treatment of photoaging. Dermatol Surg 1998;24(3):
325 – 8.
[22] Smith W. Hydroxy acids and skin aging. Soap Cosmet
Chem Spec 1993;9:55 – 6.
[23] Roenigk H. Dermabrasion:rejuvenation and scar revision. In: Roenigk RH, editor. Surgical dermatology.
London: Martin Dunitz; 1993. p. 509 – 16.
[24] Hopping S. The power peel: its emergence and future in cosmetic surgery. Int J Cosmet Surg 1999;6:
98 – 100.
[25] Freedman BM, Rueda-Pedraza E, Waddell SP. The
epidermal and dermal changes associated with microdermabrasion. Dermatol Surg 2001;27(12):1031 – 3
[discussion: 1033 – 4].
[26] Rubin MG, Greenbaum SS. Histologic effects of
aluminum oxide microdermabrasion on facial skin.
J Aesthetic Dermatol 2000;1:237 – 9.
[27] Freedman BM, Rueda-Pedraza E, Waddell SP. The
epidermal and dermal changes associated with microdermabrasion. Dermatol Surg 2001;27(12):1031 – 3
[discussion: 1033 – 4].
[28] Shim EK, Barnette D, Hughes K, Greenway HT. Microdermabrasion: a clinical histopathologic study. Dermatol Surg 2001;27:524 – 9.
[29] Hruza GJ, Dover JS. Laser skin resurfacing. Arch Dermatol 1996;132:451 – 5.
[30] Ross EV, McKinley JR, Anderson RR. Why does carbon dioxide laser resurfacing work? Arch Dermatol
1999;135:444 – 54.
[31] Hirsch RJ, Anderson RR. Principles of laser-skin interactions. In: Bolognia JL, Jorizzo JL, Rapini RP, editors. London: Elsevier Science; Dermatology, 2003.
[32] Anderson RR, Parrish JA. Selective photothermolysis:
precise microsurgery by selective absoption of pulsed
radiation. Science 1983;220:524 – 7.
[33] Garden JM. Dermatologic laser surgery. J Derm Surg
Onc 1990;16:156 – 68.
[34] Anderson RR, Parrish JA. Selective photothermolysis:
precise microsurgery by selective absorption of pulsed
radiation. Science 1983;220:524 – 7.
[35] Pappadivid E, Katsambas A. Lasers for facial rejuvenation: a review. Int J Dermatol 2003;42(6):480 – 7.
[36] Goldberg DJ. Er:YAG resurfacing: what is its role?
Aesthetic Surgery Journal 1998;18:255 – 60.
[37] Alster TS, Hirsch RJ. Single pass CO2 laser skin resurfacing of light and dark skin: extended experience with
52 patients. J Cosmet Laser Ther 2003;5:39 – 42.
[38] Khatri KA, Ross V, Grevelink JM, Margo MM, Anderson RR. Comparison of erbium:YAG and carbon
dioxide lasers in resurfacing of facial rhytids. Arch
Dermatol 1999;135:391 – 7.
[39] Alster TS. Cutaneous resurfacing with CO2 and
erbium: YAG lasers: preoperative, intraoperative, and
postoperative considerations. Plast Reconstr Surg
1999;103(2):619 – 32 [discussion: 633 – 4].
R.J. Hirsch et al / Facial Plast Surg Clin N Am 12 (2004) 311–321
[40] Alster TS. Cutaneous resurfacing with Er:YAG lasers.
Dermatol Surg 2000;26(1):73 – 5.
[41] Zachary CB. Modulating the Er:YAG laser. Lasers
Surg Med 2000;26(2):223 – 6.
[42] Alster TS. Cutaneous resurfacing with CO2 and
erbium: YAG lasers: preoperative, intraoperative, and
postoperative considerations. Plast Reconstr Surg
1999;103(2):619 – 32 [discussion: 633 – 4].
[43] Bass LS. Erbium:YAG laser skin resurfacing: preliminary clinical evaluation. Ann Plast Surg 1998;40:
328 – 34.
[44] Pham RT. Nonablative laser resurfacing. Facial Plast
Surg Clin North Am 2001;9(2):303 – 10 [ix.].
[45] Dayan S, Vartanian AJ, Menaker G. Nonablative laser
resurfacing using a long pulse 1064-nm Nd:YAG laser.
Arch Facial Plast Surg 2003;5:310 – 5.
[46] Zelickson BD, Kilmer SL, Bernstein E, et al. Pulsed
dye laser therapy for sun damaged skin. Lasers Surg
Med 1999;25(3):229 – 36.
[47] Lask GL, Lee PK, Seyfadeh M, et al. Nonablative laser treatment of facial rhytids. SPIE Proc 1997;2970:
338 – 49.
[48] Nelson JS, Millner TE, Dave D, et al. Clinical study
of non-ablative laser treatment of facial rhytides.
Lasers Surg Med 1998;17(Suppl 9):150.
[49] Kelly KM, Nelson JS, Lask GP, Geronemus RG, Bernstein LJ. Cryogen spray cooling in combination with
nonablative laser treatment of facial rhytides. Arch
Dermatol 1999;135(6):691 – 4.
[50] Goldberg DJ. Non-ablative subsurface remodeling:
clinical and histologic evaluation of a 1320-nm Nd:
YAG laser. J Cutan Laser Ther 1999;1(3):153 – 7.
[51] Ross EV, Hardaway C, Barnette D, Keel D, Paithankar
DY. Non-ablative skin remodeling with a 1450nm
laser. Proceedings of the 20th annual meeting of
the World Congress of Dermatology. July 2 – 6, 2002,
Paris, France.
[52] Rogachefsky AS, Becker K, Weiss G, Goldberg DJ.
Evaluation of a long-pulsed Nd: YAG laser at different
parameters: an analysis of both fluence and pulse duration. Dermatol Surg 2002;28:932 – 5.
[53] Goldberg DJ, Cutler KB. Non-ablative treatment of
rhytids with intense pulsed light. Lasers Surg Med
2000;26(2):186 – 200.
[54] Bitter PJ. Noninvasive rejuvenation of photoaged skin
[55]
[56]
[57]
[58]
[59]
[60]
[61]
[62]
[63]
[64]
[65]
[66]
[67]
[68]
321
using serial, full face intense pulsed light treatments.
Dermatol Surg 2000;26:835 – 43.
Goldberg DJ. New collagen formation after dermal
remodeling with an intense pulsed light source. J
Cutan Laser Ther 2000;2:59 – 61.
Goldberg DJ. Nonablative resurfacing. Clin Plast Surg
2000;27(2):287 – 92.
Bornick DP. Coblation: an emerging technology and
new technique for soft-tissue surgery. Plast Reconstr
Surg 2001;107(2):615.
Burns RL, Carruthers A, Langtry JA, Trotter MJ, West
TB, Alster TS. Electrosurgical skin resurfacing: a new
bipolar instrument. Dermatol Surg 1999;25(7):586.
Sherk HH, Black JD, Prodoehl JA, Diven J. The effects
of lasers and electrosurgical devices on human menicsal
tissue. Clin Orthop 1995;January (310):14 – 20.
Grekin RC, Tope WD, Yarborough JM, et al. Electrosurgcial resurfacing: a prospective multicenter study
of efficacy and safety. Arch Dermatol 2000;136(11):
1309 – 16.
Alster TS. Electrosurgical ablation: a new mode of
cutaneous resurfacing. Plast Reconstr Surg 2001;
107(7):1894.
Hirsch RJ, Lewis AB. Treatment of acne scarring.
Semin Cutan Med Surg 2001;20(3):190 – 8.
Grekin RC, Tope WD, Yarborough JM, Olhoffer Jr IH,
Lee PK, Lefell DJ, et al. Electrosurgcial resurfacing:
a prospective multicenter study of efficacy and safety.
Arch Dermatol 2000;136(11):1309 – 16.
Katz BE, Mac Farlane DF. Atypical facial scarring
after isotretinoin therapy in a patient with previous
dermabrasion. J Am Acad Dermatol 1994;30(5 Pt 2):
852 – 3.
Horton S, Alster TS. Preoperative and postoperative
considerations for carbon dioxide laser resurfacing.
Cutis 1999;64:399 – 405.
Walia S, Alster TS. Cutaneous CO2 resurfacing infection rate with and without prophylactic antibiotics.
Dermatol Surg 1999;25:857 – 61.
Nanni CA, Alster TS. Complications of carbon dioxide
resurfacing. Dermatol Surg 1998;24:315 – 20.
Manuskiatti W, Fitzpatrick RE, Goldman MP, KrejciPapa N. Prophylactic antibiotics in patients undergoing
laser resurfacing of the skin. J Am Acad Dermatol
1999;40:77 – 84.