ISP R
CONNECTIONS
UNITING SCIENCE AND PRACTICE
INTERNATIONAL SOCIETY FOR PHARMACOECONOMICS AND OUTCOMES RESEARCH
IN THIS ISSUE
LETTER FROM THE EDITOR
PRESIDENT’S MESSAGE
Translational Research and the Value Equation
POLICY ANALYSIS
The Age of Health Economics: The Impact of IQWIG on the German
Pharmaceutical Market
Levels of Association Between Health Care Expenditure and Health Care
Indicators in Economically Developed Countries
OUTCOMES
Raising the Bar in the USA: The Impact of Heightened Awareness of the Need
for Health-Economic Data in the Absence of a Regulatory Mandate
POLICY ANALYSIS
Commentary: Reflections on “Sicko” by Michael Moore from a European Point
of View
ISPOR CORNER
Board of Directors Take Action in 2007
ISPOR Board of Directors Election Candidates 2008
ISPOR Student Corner: Authorship Declines in Economic Evaluations
Recently Published Works: Using Pharmacoeconomics Innovatively
ISPOR 3rd Asia-Pacific Conference Call for Abstracts
ISPOR 13th Annual International Meeting Program
ISPOR 13th Annual International Meeting Short Courses
ISPOR 13th Annual International Meeting Promotional Information
ISPOR 13th Annual International Meeting Registration
JANUARY / FEBRUARY 2008 VOL. 14, NO. 1
ISPOR 2007-2008 BOARD OF DIRECTORS
PRESIDENT – Diana Brixner PhD, RPh, University of
Utah/Pharmacotherapy, dbrixner@hsc.utah.edu
PAST PRESIDENT – Michael F. Drummond PhD, University of
York, md18@york.ac.uk
PRESIDENT-ELECT – Chris L. Pashos PhD, HERQuLES,
chris_pashos@abtassoc.com
DIRECTORS – Marc Berger MD, Eli Lilly and Company,
bergerma@lilly.com; Lou Garrison, PhD, University of
Washington, lgarrisn@u.washington.edu; Shu-Chen Li PhD,
University of Newcastle, shuchuen.li@newcastle.edu.au; Uwe
Siebert MD, University of Health Sciences, Medical Informatics
& Technology, uwe.siebert@umit.at; Richard J. Willke PhD,
Pfizer, Richard.J.Willke@pfizer.com
TREASURER – Karen Rascati RPh, PhD, University of Texas,
krascati@mail.utexas.edu
FOUNDING EXECUTIVE DIRECTOR – Marilyn Dix Smith RPh,
PhD, ISPOR, mdsmith@ispor.org
ISPOR CONNECTIONS EDITOR & EDITORIAL BOARD
EDITOR-IN-CHIEF – Steven E. Marx PharmD, MS, Abbott
Laboratories, isporconnections@ispor.org
ASSOCIATE EDITORS-IN-CHIEF – Thomas Mittendorf PhD,
University of Hannover, tm@ivbl.uni-hannover.de; David
Thompson PhD, i3 Innovus, david.thompson@i3innovus.com
EDITORIAL BOARD – Rajesh Balkrishnan PhD, MS, Ohio State
University; Benjamin Craig PhD, University of South Florida;
Bonnie M. Korenblat Donato PhD, Bristol Myers Squib; Marc
Nuijten PhD, MD, MBA, Imta, Erasmus University; Michael
Wonder BSc, BPharm, Novartis Pharmaceuticals Australia;
Peter Wong RPH, MS, MBA, PhD, Good Samaritan Hospital
ISPOR CONNECTIONS PUBLISHING, SUBSCRIPTION,
AND ADVERTISING OFFICE:
ISPOR CONNECTIONS (ISSN 1538-5108) (USPS 019121)
is published bi-monthly by the International Society for
Pharmacoeconomics and Outcomes Research, 3100 Princeton
Pike, Building 3, Suite E, Lawrenceville, NJ 08648 USA.
Phone: 609-219-0773 Toll Free: 1-800-992-0643
Fax: 609-219-0774 Website: www.ispor.org
Annual membership dues include $30 for regular members and
$15 for student members for a 1-year subscription to ISPOR
CONNECTIONS.
Periodicals Postage paid at Trenton, New Jersey and at
additional mailing offices. POSTMASTER: Send address changes
to ISPOR CONNECTIONS, 3100 Princeton Pike, Building 3, Suite
E, Lawrenceville, NJ 08648 USA.
Managing Editor:
Stephen L. Priori, email: spriori@ispor.org
Advertising Manager:
Danielle Mroz, email: dmroz@ispor.org
LETTER FROM THE EDITOR
Ten Most Influential Authors in 2007:
Steve Marx's Picks
At the end of the year, we read about the ten best and worst
of movies, dressed, jobs, etc. But who in health economics & outcomes research were the most influential authors
to you? Well, I attempted again to identify them by
conducting a Medline search using the following search terms: cost-effectiveness
or quality of life from January 1, 2007 through December 31, 2007. There were
3,005 articles sited under cost-effectiveness and 10,686 articles under quality of
life, which are both slightly higher from last year. The initial screening criteria
requirement was first author of at least 3 articles that resulted in 20 costeffectiveness authors, and 62 quality of life authors. Of the 82 authors identified a
search of each authors name and articles related to cost-effectiveness or quality
of life were quantified and weighted for each term. The following top ten authors in
alphabetical order were identified:
2007 TOP TEN AUTHORS
Samuel Aballea
Dennis Revicki *
David Cella *
Thomas Rosemann
Greg de Lissovoy
Michael Schatz
Michael Drummond *
Andrew Shorr
Barbara Murphy
Kenneth Smith
* Last year winners
Congratulations to all the movers and shakers or the Chubby Checkers of health
economics & outcomes research for making a difference in 2007. Let's start doing
some of our own twisting and shouting, by presenting and authoring our own studies to demonstrate the value of health economics for decision makers. Again, these
are my picks, not the association. If you have suggestions on improving
the methodology to identify these authors next year, I look forward to your
suggestions.
On behalf of the editorial members and ISPOR staff, we look forward to and informative and productive New Year.
Direct advertising, photocopy permission, and reprint requests,
to Managing Editor.
All members of the Board of Directors serve in their personal capacity and do not
represent the views of their organization during Board activities. All members of the
Board of Directors annually disclose any conflicts of interest concerning business
relationships with the Society. See: http://www.ispor.org/board/index.asp.
Steve Marx, Editor-in-Chief
ISPOR CONNECTIONS
Copyright © 2008 International Society of Pharmacoeconomics and Outcomes Research (ISPOR) All rights reserved under International and Pan-American
Copyright Conventions. Published in the United States of America by the International Society for Pharmacoeconomics and Outcomes Research. No part of
this publication may be used or reproduced in any manner whatsoever or by any means – graphic, electronic, or mechanical, including photocopying, taping,
or information storage and retrieval systems without express written permission of the International Society for Pharmacoeconomics and Outcomes Research.
ISPOR and ISPOR CONNECTIONS are trademarks of the International Society for Pharmacoeconomics and Outcomes Research. Inquiries should be addressed
to: International Society for Pharmacoeconomics and Outcomes Research, 3100 Princeton Pike, Building 3, Suite E, Lawrenceville, NJ 08648 USA
2
January/February 2008 ISPOR CONNECTIONS
PRESIDENT’S MESSAGE
Translational Research and the Value Equation
Diana Brixner PhD, 2007-2008 ISPOR President and Associate Professor and Chair of the Department of Pharmacotherapy and
Executive Director of the Pharmacotherapy Outcomes Research Center at the University of Utah College of Pharmacy, Salt Lake
City, UT, USA
recent commentary published in the Journal
of the American Medical Association
addressed the “Meaning of Translational
Research and Why it Matters” [1]. In light of
ISPOR related topics such as outcomes
research, comparative effectiveness, cost-effectiveness, and pharmacoeconomics, it seems
timely to consider where these disciplines fit in
the continuum of translational research.
A
As Woolf acknowledges in his article, translational research means different things to different
people. The more traditional definition of “bench
IN THIS ISSUE
LETTER FROM THE EDITOR
2
PRESIDENT’S MESSAGE
Translational Research and the Value Equation 3
POLICY ANALYSIS
The Age of Health Economics: The Impact of
IQWIG on the German Pharmaceutical Market 4
Web Connections
Levels of Association Between Health Care
Expenditure and Health Care Indicators in
Economically Developed Countries
7
OUTCOMES
Raising the Bar in the USA: The Impact of
Heightened Awareness of the Need for HealthEconomic Data in the Absence of a Regulatory
9
Mandate
POLICY ANALYSIS
Commentary: Reflections on “Sicko” by Michael
Moore from a European Point of View
13
ISPOR CONNECTIONS Editorial Policy
14
ISPOR CORNER
Board of Directors Take action in 2007
15
ISPOR Board of Directors Election
Candidates 2008
16
ISPOR Student Corner: Authorship Decisions
in Economic Evaluations
23
Recently Published Works: Using
Pharmacoeconomics Innovatively
26
ISPOR 3rd Asia-Pacific Conference Call
for Abstracts
28
ISPOR 13th Annual International Meeting
Program
31
ISPOR 13th Annual International Meeting
Short Courses
36
ISPOR 13th Annual International Meeting
Promotional Information
38
ISPOR 13th Annual International Meeting
Registration
39
to bedside” encompasses drug discovery
(medicinal chemistry), drug formulation (pharmaceutics), drug testing (pharmacology and
clinical development), and patient care (pharmacotherapy). These definitions align particularly
well with the Departments in our own College of
Pharmacy at the University of Utah, and, most
likely, with various other colleges and pharmaceutical companies across the globe. The
Institute of Medicine (IOM) Clinical Research
Roundtable has labeled this definition as “translational block one”, or T1 [2]. The components
of T1 have been traditionally funded by individual
National Institutes of Health (NIH) institutes and
now collectively through the NIH roadmap initiative [3] and by the launch of the Clinical and
Translational Science Award (CTSA) with a goal
of $500 million in funding across 60 academic
centers by 2012.
An alternative definition of translational research,
perhaps more relevant to the disciplines represented by ISPOR and other population-based
organizations such as the International Society of
Pharmacoepidemiology, Academy Health,
Society for Medical Decision Making and others,
would be “translating research into practice”.
Here the disciplines of epidemiology, evidencebased synthesis, economics, public policy,
behavioral science, and biostatistics play a much
larger role in understanding how the real world of
clinical practice, patient behaviors, and concomitant disease can impact the predictions of the
highest quality research produced by randomized
clinical trials. The IOM Clinical Research
Roundtable labeled this as ”translational block
two” or T2 [2]. The challenges of this type of
research abound. In specific research on how a
new technology can be introduced into practice,
one must consider the nuances of a health care
system that has previously operated in the
absence of such technology. Treatment guidelines are reviewed and revised, systematic
reviews are redone, and documentation, such as
the Academy of Managed Care Pharmacy
(AMCP) Dossier and dossiers for other global
region reimbursement agencies, is prepared and
updated. The evidence that is created to support
these documents is largely conducted in patient
populations from primary care physician practices, integrated health care systems, and national administrative claims databases. This “real
world” research can include assessment of the
impact of therapeutic
guidelines on the
treatment and outcomes of disease, the
impact of disease or
medication therapy
management intervention programs,
and health services research to evaluate the benefit of vaccination or diagnostic screening programs. The practice-based component of this
research is primarily conducted in community or
ambulatory settings to provide insight on the
impact and outcomes of implementing new technologies. The practice-based research was
potentially referred to as T3 by Westfall and colleagues [4] to more specifically acknowledge
this practice-based approach. Either way the
dynamics of funding research in the T-2 T-3
arena is far different than the funding of the more
traditional T1 translational research. The adaptation of the NIH towards translational research had
dedicated $787 million of a $22.1 billion budget
to health services research, and the previously
mentioned resources have been directed towards
the CTSA, however, with a focus on T1. In fact
academic centers across the U.S have struggled
with how to incorporate community-based
primary care research and pharmacotherapy outcomes research into CTSA grant applications. A
more likely source for practice-based research
has been the Agency for healthcare Research and
Quality (AHRQ) with the charge that research
results are widely disseminated and used in
healthcare decision making [5]. However, the
funding for this mission is sparse with roughly a
$300 million budget initially targeted at translational research in practice grants with a shift
toward special project research on patient safety
and informatics.
A larger concern is that the conversation of defining translational research largely stops here.
Although we can study the implementation of
technologies into practice, we have neither discussed research that is focused on studying the
comparative effectiveness of different technologies nor the associated costs. Yet these two
disciplines are the core principles of ISPOR. The
benefit and limitations of conducting practice
based research have been largely recognized and
many of these same limitations apply to real
world effectiveness studies; however, there is >
January/February 2008 ISPOR CONNECTIONS 3
continued from page 3...
also acknowledged benefit of this information to
the payer. Drugs and/or other technologies
should not be expected to act the same way
when patient behaviors, disease states, and other
factors are not controlled as they are in randomized trials, and these differences can be important in making coverage decisions. The process
of rational health care resource allocation should
include economics, but how this information is
collected and how it is interpreted are important
considerations. These ongoing debates are also
reflected in the associated funding sources, both
for comparative and cost effectiveness, which at
this juncture are largely absent outside of those
vested in the results.
In summary, there is a continuum of research
from bench to bedside to practice to resource
allocation where the clarity of definition seems to
wane and the funding sources seem to diminish.
However, in all likelihood, this is a reflection of
the societal changes in how medicines are discovered, applied, and paid for to prevent disease
and improve human health. If we include comparative effectiveness and cost-effectiveness as
logical next steps in the continuum of translational research, we should be pleased to know
there is room for many more transitional states in
the future. IC
References
1. Woolf SH. The meaning of translational research and why it
matters. JAMA 2008;299:211-13.
2. Sung NS, Crowley EFJr., Genel M, et al. Central Challenges
facing the national clinical research enterprise. JAMA
2003;289:1278-87.
3. http://nihroadmap.nih.gov/ Accessed January 16, 2008.
4. Westfall JM, Mold J, Fagnan L. Practice Based research “blue highways” on the NIH roadmap. JAMA 2007;297:403-6.
5. Agency for Healthcare Research and Quality. Budget estimates for appropriations committees, fiscal year (FY) 2008:
performance budget submission for congressional justification.
Performance budget overview 2008
http://www.ahrq.gov/about/cj2008/cjweb08a.htm#statement
Accessed November 17, 2007.
POLICY ANALYSIS
The Age of Health Economics: The Impact of IQWIG On
The German Pharmaceutical Market
Frank-Ulrich Fricke PhD, MSc, Principal, IMS Health Economics & Outcomes Research, Nuremburg, Germany
Starting in February 2006, a wave of health care
cost-containment reforms swept through
Germany, designed to deliver 1.0 billion in
2006, rising to 1.3 billion in 2007 and 2008. A
further far-reaching package was agreed in July
2006 to restructure the financing of health care
and create a more cohesive, uniform system.
These reforms impact the German pharmaceutical market in a number of ways and include a
stronger role for IQWiG (Institut für Qualität und
Wirtschaftlichkeit im Gesundheitswesen) in the
evaluation of new drugs and technologies.
Frank-Ulrich Fricke, Principal, HEOR at IMS
Health, examines the implications of this change
and unfolds the new map that may help to guide
pharma across an unfamiliar landscape.
From 2008, after the amendment of its methodologies IQWiG - an independent foundation broadly equivalent to England's NICE (National Institute
for Health and Clinical Excellence) - will be able to
conduct cost-benefit assessments, initially on
4
January/February 2008 ISPOR CONNECTIONS
drugs considered 'high-profile'. This is in addition
to its previous remit for evaluating clinical benefit.
From that point on, Germany will join a growing
number of countries - the USA included - where
pharmaceutical products are measured with an
economic slide-rule before a penny of statutory
health insurance funds is made available to procure them. The only difference being that in
Germany a product will gain market access first
and then be assessed for subsequent restrictions
or withdrawal of prescribability. IMS currently
estimates that up to 140bn of annual global
pharmaceutical sales are subject to some form of
economic evaluation.
By satisfying IQWiG's criteria, a drug can be prescribed via the statutory health insurance thereby
allowing access to a wider prescription market.
Failure to demonstrate efficiency gains is likely to
limit the market to those citizens and private
health funds that are willing and able to pay up to
the full prescription price.
IQWiG carries out its work at the behest of Der
Gemeinsame Bundesausschuss or Federal Joint
Committee (G-BA). The G-BA - part of the selfgoverning body that oversees the German health
care system - is institutionalized as a legal entity
under public law. However, it does not have
responsibility for the licensing of drugs, which is
the preserve of the Federal Institute for Drugs and
Medical Products (BfArM). G-BA likens its role to
being the "eye of the needle" through which a new
drug or method must pass to gain a positive evaluation in terms of benefit and efficiency, before
qualifying for reimbursement in outpatient care
from the statutory health insurance (SHI) funds.
Together IQWiG and the G-BA act as the muscular
gatekeepers of the health care market in Germany.
Convincing these organisations that a new treatment
offers improved value for money over existing interventions has become the key to commercial success.
IQWiG assessments of new drugs, other interventions, current marketed drugs and additional
measures that may have a relevant budgetary
impact on the SHI, are typically commissioned by
the G-BA and serve as a basis for a number of
important decisions. These include whether to
include a drug in a reference pricing group, the
prescribability of drugs for SHI members, and
treatment guidelines. In addition, based on an
IQWiG assessment and according to the law, the
head association of the sick funds must set a
maximum reimbursement price.
The IQWiG assessment will be based on its own
pre-defined criteria which together with its data
sources will be set out early on in the process in
a 'report plan'. This is published as part of
IQWiG's operational procedures which also
involve a 'draft report' ahead of a 'final report' for
the G-BA. To complete the process the G-BA then
conveys its recommendations to the Ministry of
Health (BMG). The role of the Ministry is only to
consider whether the decisions taken by the GBA are legally robust.
The Current Situation
IQWiG is currently preparing its new assessment
methodology paper and is expected to finally
announce the selected methodologies, (Version
3) in Q4 2007. This will allow pharma companies
very little time to prepare for assessments beginning in 2008.
Statements emanating from IQWiG and G-BA officials suggest that the new process may involve a
health benefit assessment as the first step (as
before). If no such benefit is perceived, then no
cost-benefit assessment will be conducted. If,
however, there is believed to be benefit over
existing treatments then a cost-effectiveness
analysis will be conducted as the next step.
To determine whether any new drug offers a
health benefit gain, comparisons will be made
with the current care regimen for patients within
the SHI sector defined in the report plan. Based
on current IQWiG practice, many health benefit
assessments, but only a few cost-benefit
assessments, can be expected - mainly because
so far very few evaluations have revealed additional benefits from new therapies.
New treatments that are innovative, high-profile,
expensive, and likely to be in demand by a large
number of patients are the most likely G-BA targets for an IQWiG assessment. Staying 'off the
radar screen' of the G-BA and other institutional
players in health care may therefore become a
strategic necessity for some pharma companies
in Germany. Quite what constitutes 'expensive' is
not defined by IQWiG, but it is likely to be a highly moveable threshold.
Cost-effectiveness According to
IQWiG
Also unclear is what form IQWiG's technical costbenefit analysis will take. However, the following
'good practice' guidelines can be expected to
influence its final shape:
• Recommendations of the Panel on Costeffectiveness in Health and Medicine
• Published guidelines for authors and peer
reviewers of economic submissions to the
British Medical Journal
• New England Journal of Medicine policy on
cost-effectiveness analyses
• Set of German recommendations on the conduct of economic evaluations
IQWiG is also consulting a number of international experts regarding the potential methodology although again it is unclear on what basis these
'experts' were selected. >
< advertisement >
January/February 2008 ISPOR CONNECTIONS 5
New Imperative: Demonstrating
the Value of Medicines
To succeed in the reformed German health care
market pharma companies must focus on a
range of short- and long-term solutions that provide a clear pathway through an IQWiG assessment. In particular, they will need to revisit reimbursement and market access processes.
In the past, pharma companies could, following
market authorization, market their product, set
the price and receive full reimbursement. This will
change. With the new processes in place they
can still set the price but they will need to assess
the likelihood of an IQWiG/G-BA approval.
Developing health economic information, including a health technology evaluation, and preparing
thoroughly for an IQWiG assessment is therefore
essential. For some companies it will call for a
new set of skills and techniques.
What is also emerging is the opportunity for pharma managers to engage with IQWiG during the
assessment process which will begin with IQWiG
conducting a scoping workshop and inviting
stakeholders to comment on the extent of the
assessment. As a next step, consultations on the
report plan will be held, followed by hearings on
the draft reports. In between, evidence available
to be included in the assessments will be discussed informally. To be prepared for these
“encounters” pharmaceutical companies should
compile the evidence available and potentially
produce a parallel Health Technology
Assessment (HTA) of their own, based on internationally accepted standards (INAHTA or
DAHTA) and written by specialist authors.
Judging by the proposed IQWiG 'report plan' for
the assessment of a particular treatment, pharma
managers will need to compare the suggested
population, intervention, comparator and outcomes of mortality, morbidity and quality of life
with their own notions about their product. They
should also evaluate the criteria for study/article
evaluation selected, as well as the deployed
search algorithm. This can be done best by comparing the report plan with an HTA.
IQWiG's assessment process may last 12
months or longer and managers will need to follow this closely, especially with regard to publication of the draft report. This is issued with an
invitation for comments which will be subsequently discussed at a private hearing with
IQWiG. Thorough preparation is essential, based
on available evidence, but the timescale for turnaround is short - a mere four weeks.
IQWiG's final report should take into account revisions agreed at the draft report stage but there
6
January/February 2008 ISPOR CONNECTIONS
will be no scope at this point for a further appeal
to IQWiG regarding the final report it submits to
the G-BA.
The next opportunity for an appeal is directly to
the G-BA once their decision has been made.
Appeals can challenge the reference pricing
group set, the treatment guidelines laid down and
any prescribing exclusions from SHI funds. If this
proves unsuccessful, a final challenge can be
made and the case heard before the Social
Courts. A successful challenge may mean referral back to the G-BA for reconsideration. In the
meantime, the product in question remains on the
market and the manufacturer can establish the
brand. Thus, although the delay of the assessment can benefit the product, the process will
nevertheless incur additional costs.
Patients, too, benefit from the discount schemes
not only in terms of access to treatments they
would not otherwise have but also because the
presence of a discount contract enables sick
funds to release their patients from co-payments.
Patients and Prescribers - An
Alternative Scenario
Where pharma companies are unwilling or unable
to negotiate a discount contract, one effect of the
economic belt-tightening reforms may be to limit
the toolkit available for prescribers and reduce the
choice of treatment for patients. This, in turn,
may further differentiate the quality and quantity
of care, with those who are privately insured and/
or willing to pay more out of pocket having
access to those treatments which are more in line
with their individual preferences and potentially
more expensive.
Early Planning Critical
Companies hoping to supply pharma products in
Germany need to start looking for the positive
economic impact of their new healthcare intervention, early in their development process. In
doing so, they should consider patient potential,
current pathways of care, and the financial
impact of the illness. From this analysis they will
need to develop strong value hypotheses as well
as demonstrate the clinical difference their new
treatment will make. All this will need to be translated into financial terms.
For the major international Pharma companies
such a process is likely to fit in with current best
practice; for others some procedural adjustments
will be required. But even such a rigorous
approach might not be sufficient to secure prescribability, potentially resulting in the need to
consider discount pricing. However, this may not
be quite as damaging as it first sounds.
Discounting
The Social Code makes provision for manufacturers and sickness funds to agree discount contracts and most of the statutory health insurance
funds have these contracts in place. For Pharma,
an attractive feature of this scheme is that discount contracts do not affect public or reference
prices across the rest of Europe. In other words,
a discount in Germany does not mean a discount
elsewhere in Europe.
Recent experience in Germany shows that such
discount contracts can be an effective way of
either staying on the market (short acting insulin
analogues) or entering the market (generics). By
establishing a discount contract with a sickness
fund, those companies marketing generics have
been able to gain market share and, in some
cases, gained a handsome dividend.
Public reaction to this will in part depend on the
media attention attracted by IQWiG's work and
the strength of the patient lobby. The patient's
perspective - particularly in terms of health endpoints that describe a patient 'feeling better' - is
not fully considered by IQWiG. Over time such
neglect may lead to public dissatisfaction with
the changes to the health care system putting
reforms once again on the German health policy
agenda. IC
WEB CONNECTIONS
Does your research warrant an understanding
of existing hospitals within a certain area (within the United States). Do you need to control
for number of beds, discharges or total patient
revenue? Do you want to know the number of
hospitals available within a certain region?
Free hospital information is available through
the American Hospital Directory,
at:www.ahd.com/freesearch.php3.
What if your data needs for hospital information
goes beyond what is available at:
www.ahd.com/freesearch.php3? Visit another
site on ahd.com, the hospital statistics by state
site: www.ahd.com/state_statistics.html.
Here one can find, for each state, the number
of hospitals, staffed beds, total discharges,
patient days and gross patient revenue. All
data is for non-federal, short term, acute care
hospitals.
Do you know of any websites that you
would like to share with the ISPOR
community?
If so, contact Bonnie M. Korenblat
Donato PhD, at bonnie.donato@bms.com.
POLICY ANALYSIS
Levels Of Association Between Health Care Expenditure
And Health Care Indicators In Economically Developed
Countries
Ray Gani PhD, Heron Evidence Development Ltd, Letchworth Garden City, Hertfordshire, UK
ifferent health care systems with similar levels of resources per capita
often show wide variations in population health outcomes. One possible
explanation for this is that different health care systems choose to use the
resources available to them in different ways, some of which may be suboptimal. Sub-optimal resource use can lead to inefficiencies in health care
provision and poorer health outcomes. In an attempt to address the question
of quality of care, the WHO [1] and the OECD [2] both published reports
focusing on assessing the performance of health care systems in different
countries. However, neither addressed the issue of cost-effectiveness, or,
more specifically, which countries had the more cost-effective health care
systems. Using data published by the WHO relating to health care outcomes
and expenditure, we attempt to assess how health care performance indicators are related to wealth and health care expenditure, and to provide an indication of which countries may be providing the most cost-effective care.
D
Data from the OECD and WHO
The WHO has recently made publicly available an extensive database containing a range of health-related, demographic and economic variables
across a number of years [3]. The World Health statistics 2007 presents the
most recent health statistics for the WHO's 193 member states and are collated from publications and databases produced by the WHO's technical programmes and regional offices. A core set of health-related indicators was
selected for the database on the basis of their relevance to global health, the
availability and quality of the data, and the accuracy and comparability of
estimates. The statistics for the indicators are derived from an interactive
process of data collection, compilation, quality assessment and estimation
occurring among WHO's technical programmes and its member states.
The health care indicators (HCIs) that were collated for use in this study are
listed in Table 1. These were chosen as they can be viewed as representing
quality of life, and less subject to endogenous factors within particular countries. Male-to-female ratios were used to aggregate the health care indicators
(HCI) across gender. In addition, values for the per capita gross domestic
product (GDP), and the per capita health-care expenditure (HCE) in both US
and international dollars were also collated. An International dollar is the
hypothetical unit of currency which locally has the same purchasing power
that one US dollar has in the US.
Data were collated for the 30 OECD countries listed in Table 2 [2]. These
countries were chosen as they represented the countries which are most
economically developed and likely to have the most advanced health care
systems. They also represented countries for which the full range of data
was available. Including data from less developed countries would have
introduced unreasonable heterogeneity.
Once the data was collated, a series of analyses were performed. Univariable
regression analyses was conducted to explore the linear association between
each HCI and either GDP or HCE. This was repeated using the logarithms of
GDP and HCE, in US and international dollars. The proposed explanatory variable with the best predictive power was then used as a predictor of the HCI.
> TABLE 1 Health-care indicators used to assess the quality of healthcare in each country
Healthy life expectancy (HALE) at birth (years)
Infant mortality rate
Life expectancy at birth (years)
Maternal mortality ratio
Neonatal mortality rate
Probability of dying between 15 and 60 years
Probability of dying under five years of age
> TABLE 2 The 30 member countries of the Organisation for Economic
Co-operation and Development (OECD)
Australia Denmark
Austria Finland
Belgium France
Hungary Luxembourg Poland
Iceland Mexico
Portugal
Ireland Netherlands Republic
of Korea
Germany Italy
New Zealand Slovakia
Sweden
Switzerland
Turkey
Canada
United
Kingdom
United States
of America
Czech
Greece
Republic
Japan
Norway
Spain
Correlations Between Health Care Indicators And
Economic Data
The correlation coefficients (r) between the HCIs and the logged economic
variables in US dollars are shown in Table 3. Correlation with international
dollar economic variables was generally less statistically significant than with
US dollars, and these results are not shown. The correlations shown are all
statistically significant after adjusting for multiplicity (P<0.05). The HCIs
which were more strongly correlated with GDP than HCE were infant mortality rates, maternal mortality ratios, neonatal mortality rates and the probability of dying under five years of age. HCE was more strongly correlated than
GDP with healthy life expectancy (HALE) at birth, average life expectancy at
birth and the probability of dying between ages 15 and 60 years old.
> TABLE 3 Correlation coefficients between health-care indicators and
the logarithms of GDP and HCE
HCE
GDP
Health care indicator
Healthy life expectancy (HALE) at birth
0.81***
0.83***
Infant mortality rate
-0.73***
-0.65**
Life expectancy at birth
0.74***
0.77***
-0.53*
-0.59**
Maternal mortality ratio
Neonatal mortality rate
-0.72***
-0.62***
Probability of dying (15 to 60 years old)
-0.74***
-0.77**
Probability of dying (under five years old)
-0.73***
-0.63**
GDP = Per capita gross domestic product; HCE = Per capita health-care
expenditure. P-values are adjusted using Bonferroni method for multiple
comparisons. * P<0.05; ** P<0.01; ***P<0.001.
January/February 2008 ISPOR CONNECTIONS 7
>
The strongest correlation found was between healthy life expectancy (HALE)
and the logarithm of HCE, for which the correlation coefficient was 0.83
(P<0.001, Table 3). A regression model fitted to the logarithm of the HCE data
is shown in Figure 1. The mean cost was US$2400 and the mean health life
expectancy at birth was 69.1 years. The majority of data from countries fall
within the 95% confidence intervals. Outliers in this correlation were Japan,
Spain and Sweden, which have a higher than expected HALE, and the USA
and Hungary which have a lower than expected HALE for their given HCE.
> FIGURE 1 Per capita health care expenditure and healthly life
expectancy for the 30 OECD copuntries
strong correlation between total per capita health care expenditure and
healthy life expectancy, with lower than expected values of healthy life
expectancy given the health-care expenditure in Hungary and the USA. Whilst
this might indicate that the health care systems in these countries are under
performing, this does not imply a causal relationship.
There are a number of other factors that may influence health care indicators,
such as education, nutrition or public spending. To derive robust estimates
of the cost-effectiveness of different health care systems, these factors
would need to be accounted for. In effect this would require deriving a standardised control group against which the health-care systems within different countries could be compared.
Further data and analysis would help identify the costs and benefits of different health care systems to estimate the cost-effectiveness of health care
systems between countries. Such an analysis would be technically challenging, but potentially yield huge benefits. By identifying the most cost-effective
health care system, best practice could be identified and replicated, thereby
potentially leading to improvements across different health care systems
within different countries. IC
References
1. The World Health Report 2000: Health Systems: Improving Performance, Geneva, WHO, 2000
http://www.who.int/whr/2000/en/ Last accessed September 2007.
2. Smith P (ed). Measuring up: Improving health system performance in OECD countries, Paris,
OECD, 2002.
Discussion and Conclusions
In general there are high levels of correlation between economic and health
care indicators in economically developed countries. In particular there is a
3. World Health Statistics 2007, Geneva, WHO, 2007 http://www.who.int/whosis/en/index.html Last
accessed September 2007.
< advertisement >
8
January/February 2008 ISPOR CONNECTIONS
OUTCOMES
Raising the Bar in the USA: The Impact of Heightened
Awareness of the Need for Health-Economic Data in the
Absence of a Regulatory Mandate
Michael E. Minshall, Principal Health Economics and Outcomes Research, IMS Health®, and Adjunct Professor, Indiana University
School of Medicine, Department of Public Health, Noblesville, IN, USA; and John Watkins RPh, MPH, BCPS, Pharmacy Manager,
Formulary Development, Premera Blue Cross, and Clinical Associate Professor of Pharmacy, University of Washington, Seattle, WA, USA
Economic assessment of new health care technologies is practiced among
an increasing number of countries around the world. Today, the United States
is taking steps in requiring economic evaluation for new healthcare technologies. Michael E. Minshall and John Watkins consider some of the issues.
Health Technology Assessments (HTAs) are increasing in countries around
the world. To date, HTA requirements exist in about 30 countries, including
Australia, Canada, Germany, The Netherlands, Spain, Sweden and the UK.
There are discussions within a number of other countries, including China
and Korea, to add health economics and outcomes research (HEOR) data
into HTAs, making them requirements for formulary approval and access to
medical technologies, drugs and other kinds of medical treatment.
In the United States, the environment for health-economic data is changing.
The US health care market contains two major segments: the public payer
and the private payer groups, both representing about 50% of the market.
While most HTA work completed in the United States over the past 15 to 17
years has been in the private sector, the public sector, including government
entities such as Medicare and Medicaid, has initiated steps to consider HTAs
for technology adoption.
Two entities in the private sector that provide a good indication of where
HTAs are moving within the United States are the Academy of Managed Care
Pharmacy (AMCP) Guidelines and the more recently published Wellpoint
Guidelines. Additionally, USHTA requirements focus more on the budgetary
impact and less on the cost-effectiveness of new health technologies.
Moving forward, companies will be required to perform HTA analyses to get
new technologies on formulary and covered by private and public plans.
such as the National Institute for Health and Clinical Excellence (NICE) in the
UK, and are required by many managed care plans across the United States.
With three versions, including the latest, Version 2.1 (April 2005), which clarified the differences between budget-impact and cost-effective models, the
AMCP Guidelines are an invaluable tool for referencing the appropriate steps
to prepare dossiers for submissions. While not mandatory, the AMCP
Guidelines are known and followed by many industry professionals for HTAs.
Wellpoint Guidelines (Version 5.1, October 2005)
Wellpoint Health Networks, with about 32 million covered lives, is currently
the largest HMO in the US. The Wellpoint Guidelines establish two sets of
requirements - one for new products and the other for existing products, as
well as a reevaluation process and guidelines for assessing clinical performance, cost-effectiveness and system impact versus comparators.
Of particular note in the Wellpoint Guidelines is the distinction between new
and existing products. The Wellpoint Guidelines call for a reevaluation
process after several years, which represent a true departure from the AMCP
Guidelines and other guidelines' directives.
Seven Key Elements of the Wellpoint Guidelines
Evidentiary and Analytical Standards - While the Wellpoint Guidelines state
that evidence must meet accepted standards, what's of special interest is
Wellpoint's position that “claims made for treatment effect, cost-effectiveness and budget impact” must be done within the Wellpoint treating environment. This demonstrates that Wellpoint is initiating an analytical standards
component, monitoring clinical evidence, cost-effectiveness and budget
impact over time for verification.
HTA in the USA: What Led us to this Point?
The managed care revolution of the late-1980s and 1990s produced a
demand for evidence-based formulary placement. Additionally, it called for
the pharmaceutical and biotechnology industries to provide information on
budget impact and to establish the “value” of new medicine, including clinical, economic and humanistic ideals.
> FIGURE 1 Wellpoint Evidentiary and Analytical Standards
Today there are about 600 different health care providers in the US private
sector. Theoretically, all of them could have their own HTA requirements, as
there are no mandatory national guidelines within the United States.
However, when segmented by larger groups, it's evident that about 40 payers, or about 40 managed care plans, represent about 80 percent of the market.
HTA in the USA: The Existing Guidelines
AMCP Guidelines
The AMCP Guidelines are the first widely-followed and utilized guidelines for
HTA in the United States. They include explicit mentions of non-U.S. bodies,
>
January/February 2008 ISPOR CONNECTIONS 9
For example, if a company indicates the ICER for a new product is $20,000
per life year gained, Wellpoint will revisit this claim in three, four and five year
spans to determine if its standard is met. If not, renegotiations could occur
between the company and Wellpoint. For pharmaceutical and biotechnology
companies, this approach suggests that cost-effectiveness claims will need
to be reevaluated and verified after a given time period.
HTA in the U.S. private sector is extremely varied,
however much is being done to advance the
concept of value-based technology assessment.
Compared to Wellpoint, Premera Blue Cross is much
smaller and has fewer internal resources to support
HTA, but it deals with the same basic issues.
Outcomes Assessments - Wellpoint states that “where a previous submission
has been made detailing the epidemiology of the disease state and the product's
place in therapy, it is important to revisit this claim and confirm its relevance.”
This is significant regarding the verification of claims on a cost-effective, budget-impact basis. Comparators may “shift” to different products since the first
HTA was performed, potentially requiring pharmaceutical and biotechnology
companies to run comparative analyses again in three to five years time.
likely issue guidance in the next one to two years, but there is no mandatory time table.
The role of CEA has long been at issue. In 1989, Medicare formally proposed to include CEA as one of several criterions for approving new medical
technologies, but was turned away due to tremendous political opposition.
Reasons for the failure included:
• Americans desire and appetite for new medical technology,
• Distaste for setting coverage limits,
• U.S. population's sense of entitlement for Medicare funds,
• Wealthy country with a shortage in health care dollars,
• Special interest groups with political influence,
• A fragmented U.S. health care system with multiple payers.
The Medicare Modernization Act (MMA) of 2003 contains a provision calling
on the Agency for Healthcare Research and Quality (AHRQ) to conduct
research on outcomes, comparative clinical effectiveness, and appropriateness of healthcare, including prescription drugs.
Comparator Therapies - The Wellpoint Guidelines state that companies may
be asked to revisit their choice of comparator if after several years there's a
different, most-common comparator.
CMS released a Guidance document on April 11, 2006 on the National
Coverage Determination (NCD) process stating, “Cost-effectiveness is not a
factor CMS considers in making NCDs.” Additionally, MMA contains language forbidding Medicare from applying a “functional equivalence” standard to drugs or biologic agents, thereby eliminating the concept of “reference pricing” for drugs in the same class, which is widely practiced in
Europe.
Outcomes Claims - The Wellpoint Guidelines set a “gold standard” with
regards to randomized, comparative trials with a randomized, active comparator, as opposed to randomized controlled trials (RCTs) with a placebo
comparator. Additionally, its verbiage “with particular emphasis on well
designed pragmatic trials and their outcomes” is significant considering the
push by pharmaceutical and biotechnology firms over the last 10 to 14 years
for Phase IIIb and Phase IV trials, which are more naturalistic in design.
Finally, CMS encourages the use of data from practical clinical trials. This
includes increasing emphasis on health outcomes actually experienced by
patients, such as quality of life, functional status, duration of disability, and
morbidity and mortality, as well as decreasing emphasis on outcomes that
patients do not experience directly, such as changes in laboratory values,
radiographic response, sensitivity/specificity, physiologic parameters, and
other intermediate/surrogate outcomes.
Quality Adjusted Life Years (QALY) - While the Wellpoint Guidelines do not
mandate a generic cost-per-QALY, Wellpoint is encouraging companies to
present this information, which may help bring the U.S. guidelines into alignment with other global HTA groups, such as NICE and the Pharmaceutical
Benefits Advisory Committee (PBAC) in Australia.
Toward More Rigorous Health-Economic DecisionMaking: One Payer's Experience
New Data/Claims - Wellpoint favors a “Probabilistic Sensitivity Analysis” format related to cost-effectiveness analysis (CEA). This format is well known
to those in the UK and academics in the United States. Many HTA bodies
around the world require this technique to be used in comparative cost-effective analyses.
Premera Blue Cross, a Blue Cross Blue Shield affiliate, is a commercial PPO
operating primarily in the Pacific Northwest and covering 1.6 million lives
(1.2 million pharmacy lives). Premera recognizes that HTA is necessary
today because of rising health care spending as a percentage of US gross
domestic product (GDP) and a realization that this trend simply cannot continue, as it is becoming increasingly difficult for employers to provide full
drug coverage for their employees.
Centers for Medicare & Medicaid Services (CMS)
HTA in the U.S. private sector is extremely varied, however much is being
done to advance the concept of value-based technology assessment.
Compared to Wellpoint, Premera Blue Cross is much smaller and has fewer
internal resources to support HTA, but it deals with the same basic issues.
These include data limitations and evidence gaps caused by factors such as
ethical limitations on study design, industry sponsorship of clinical trials, and
the time and logistics required to conduct large-scale, long-term outcome
studies. To best handle these gaps, most organizations in the U.S. follow a
pure evidence-based medicine (EBM) doctrine, focusing exclusively on the
clinical evidence and often limited to large-scale, well-designed RCTs and
rigorous meta-analyses.
In the public sector, several significant issues relate to the CMS. Regarding
cost effectiveness, a legislative mandate to incorporate HTA into the formulary process is possible, but its outcome is unclear at this time. CMS will
Like other organizations, Premera focuses on high-quality, RCT evidence and
tries to incorporate best available evidence, which sometimes includes obser-
Budget Impact Analysis (BIA) - The Wellpoint Guidelines request that manufacturers “provide forecasts of the impact of the product on resource utilization, the
pharmacy budget, the medical budget and the total costs of treating the patients
in that disease or therapy area” and state that Wellpoint will assess such forecasts as part of ongoing product reevaluation. This is the largest departure or
advance from the AMCP Guidelines and will necessitate extra effort and
thoughts around the design, analysis, and interpretation of HTAs.
10 January/February 2008 ISPOR CONNECTIONS
vational study results. Since 2001, Premera has been considering CEA when
such information is available. Best available evidence implies a willingness to
trade a certain amount of rigor for speed. This more pragmatic approach
includes modeling data, CEA and BIA, when reasonable models are available.
Burden of Proof Always Lies with the New Technology
A cardinal principle of EBM is that the burden of proof always lies with the
new technology. This is contrary to predominant U.S. cultural assumptions.
There is a very strong sense in the United States that newer is always better,
unless proven otherwise. But in EBM, older is generally better, in that more
is known about the older product, such as its weak points and strengths.
Given the choice, Premera will usually choose the proven, older technologies
versus newer ones.
Figure 2 outlines the general thought process Premera pharmacy and therapeutics (P&T) committee members use to evaluate a new product. The
product must be safe, effective and cost-effective for the new technology to
be adopted. The first three steps with drugs are in the realm of Premera's
P&T, an external committee on which no Premera staff are allowed to vote.
The fourth step, BIA, is done internally on the business side.
> FIGURE 2 Premera's Thought Process for Technology Review
Premera uses the term “value” in its public statements, which essentially is
a lay term for incremental cost-effectiveness. If the new product costs more
than the comparator, adoption requires demonstration of a clinically meaningful improvement in outcome and offsetting cost savings - usually from the
payer perspective. However, if the new product costs less than the comparator, adoption requires a lesser standard of clinical evidence, assuming there
are no hidden costs to offset savings and basic safety and effectiveness are
achieved.
Figure 3 outlines Premera's HTA drug review process, which was created for
pharmaceutical products. This process is now being expanded to include
other technologies.
Three Examples regarding the Need for Targeted Diagnostics
Gleevec (imatinib) and Iressa (gefitinib) - Lowering the number needed to
treat (NNT) improves cost-effectiveness. To do this effectively, more responsive and sicker patients must be targeted, which becomes increasingly
important as the cost of the technology increases.
For example, in the case of Gleevec (imatinib) and Iressa (gefitinib), small
molecule, targeted oncology therapies, Gleevec came to market with genetic markers that identify the responders; Iressa did not. A review of patients
who received each of these drugs through Premera in 2006 found that 364
individuals had received Gleevec, while only 11 were treated with Iressa.
These numbers suggest that both physicians and payers respond favorably
to specific markers that guide them in patient selection.
Drug Example: Exenatide (Byetta) - Exenatide is a new diabetes drug with a
completely new harmacology. While it is fairly expensive compared to alternatives, when Premera first examined it, the company consulted with local opinion leaders who thought that it would have a place in therapy but had difficulty
in defining the most cost-efficient patient population. To aid in determining the
most efficient patient population for treatment with exenatide, Premera utilized
the CORE Diabetes Model, which was licensed by the drug manufacturer,
Amylin Pharmaceuticals. The information Premera sought included:
> FIGURE 3 Premera's HTA Review Process
• What is its place in therapy?
- New mechanism, costs more than alternatives
- No long-term clinical endpoint trials
- Probably a good drug, But for whom?
• CORE Diabetes Model
- Markov model structure using Monte Carlo simulation and tracker variables
- Submodels account for comorbidities and interactions between comorbidities
- Very flexible user inputs for cohort and treatment characteristics
• Test case (Hypothesis: change in patient weight would affect diabetes
outcomes)
- Assume cohort on Metformin
- Baseline HbA1c = 8.5% + 1
- BMI = 35 kg/m2 + 5 (base case = 27.5 kg/m2)
- Add exenatide vs. comparator agent or vs. continuing metformin
monotherapy
Exenatide was compared to generic glyburide, which costs about 5%as
much as exenatide, pioglitazone (Actos), insulin glargine (Lantus), and continuation of metformin. (Note: the metformin only treatment is referred to as
“placebo” in Table 1 that follows.) >
January/February 2008 ISPOR CONNECTIONS 11
> TABLE 1 Exenatide vs. Treatment Alternatives
highly likely that the requirements for private payers and public payers will
remain disparate and a multi-faceted approach to value determination will
remain a necessity in the US marketplace for manufacturers.
CEA will be rated at varying degrees of importance by major coverage
groups in the United States, including: the private sector, with HMOs and
PPOs; the public sector, with the CMS and government systems; and fee for
service, which is a smaller part. It's inevitable that CMS becomes more
involved in HTA processes. As part of the MMA of 2002, the U.S. Congress
mandated that CMS incorporate a technology assessment process based on
economics. Since CMS oversees a tremendous part of the medical market
in the United States, CMS can be considered a “bell-weather” entity that
other groups may follow in both the public and private sectors; however, only
time will tell.
It may take many years for the United States to achieve a nationalized, costeffectiveness requirement, and the country may never get there. The United
States spends about 14% of its GDP on healthcare, a tremendous part of its
entire GDP, and there are many competing interests with input into the
process. In short, a great number of people have a say about what happens
with U.S. health care dollars. IC
Table 1 lists the results for the above treatment options, modeled over a 30year time horizon. All comparisons yielded incremental cost-utility ratios of
less than $50,000 per QALY for all treatments.
Diagnostic Example: Oncotype DX - In this test for early-stage breast cancer,
a 21-gene panel gives a risk score that correlates with the likelihood of
distant recurrence of disease after surgery.
Details of the test include:
• 21 gene diagnostic panel for estrogen receptor positive, node negative
breast cancer
- Risk score (range 0-100) predicts likelihood of distant recurrence
- Stratified risk: low (<18), med (18-30) high (>30)
• Draft guidance document for dossier submission was provided to the
manufacturer
• Resulting submission was reviewed for medical policy determination
- Should Premera cover this test?
- If so, for which patients?
The proposed rationale for cost-effectiveness is Chemotherapy (CT) avoidance in low-risk patients and the basing of treatment strategies on test
results can lead to more informed decisions, improved outcomes and a
potential to reduce overall cost of care. In the Premera evaluation, the key
question was whether the results would be actionable for providers. When
Premera consulted the Premera Oncology Advisory Panel, a representative
group of community-based oncologists, the vast majority of them said they
would probably not advise their patients to forego chemotherapy simply
because of this test result. As a result of this evaluation, Premera approved
the test under very limited conditions in a subgroup of patients who would
be on the borderline and for whom the test might actually make a difference.
This exercise reaffirmed the principle that test results must be actionable in
order to be eligible for coverage.
Summary
The United States is moving, albeit slowly, towards some type of nationalized, cost-effectiveness requirement. What form that takes, whether it will be
a QALY format or straight mortality, is unclear at this time. Moreover, it is
12 January/February 2008 ISPOR CONNECTIONS
< advertisement >
POLICY ANALYSIS
Commentary: Reflections on 'Sicko' by Michael Moore
from a European Point of View
Wolfgang Greiner PhD, Health Economist, University of Bielefeld, Bielefeld, Germany, and Thomas Mittendorf PhD, Health
Economist, University of Hanover, Hanover, Germany
he documentary film Sicko by Michael Moore gives us a very grim insight
into the American health care system. A variety of individuals speak to the
audience, all of them having major problems as necessary health care services (like bone marrow transplantation) were denied to them by their health
care insurances in the past. The more urging problem in the United States,
namely its over 45 million uninsured citizens is very strikingly represented by
a man stitching an open wound on his leg by himself just like Sylvester
Stallone already showed us some 25 years ago in the film “Rambo: First
Blood”. Seeing all the sad and horrible cases some of the American viewers
may very well lower their heads in shame, some may be outraged. For others it also may only be an anecdotal line up of short glimpses at countries
around the world with a more or less 'socialized medicine'.
T
But one question remains: Do Europeans smile while watching this film?
Michael Moore has not been known in the past to present a completely balanced and unbiased picture of the given situation. He intelligently uses fast
cuts and a satirical undertone while commenting the pictures we see on the
big screen. In doing so he plays with the emotions of the audience aiming to
reach his goal of gaining attention for a specific element going wrong in the
ongoing development process of the American society. In this film especially Europeans are attracted to the content because Moore goes oversees to
France and the UK to search for the Holy Grail in solving the problems of the
US health care system. As much as we Europeans would like to sit back
knowing that we possess this final recipe for the perfect health care system,
we have to reflect for one moment if we actually are entitled to laugh and to
point our finger over the Atlantic.
The image of the American health care system sketched in the film needs a
second look at. It is true, that the health care market in the US compared to
other industrialized countries is the one with the highest rate of un- or underinsured citizens, having in mind that over 15% of the American public is
affected by this. Adding to that, in the European understanding of the phrase
'health insurance' this figure definitely will be much higher. Even public coverage schemes like Medicaid or Medicare bear a high financial risk to
patients, as drug costs and co-payments may be substantial. On the other
hand one has to keep in mind that the US health care system has high inherent innovative powers and a high rate and speed in the diffusion of treatment
innovations. So it may be that the overall life expectancy, which often is cited
in the film, isn't as high as in most European countries (but as in Cuba looking at WHO figures), on the other hand the survival rate after cancer treatment rather might be higher. Furthermore, the majority of developments in
organizational or funding issues in health care finally are to some extent rooted in the US market. Topics from recent European history include disease
management programs for chronic conditions, managed care or integrated
health care concepts. Another example is diagnosis related group (DRG) systems for hospital services which were enacted in most European counties
(like Germany) very recently. Europeans, especially German health politicians, tend to look exclusively to the US for new concepts having cost containment in the back of their head. The United States in the 80’s and 90’s
undoubtedly was the laboratory for new health care concepts for the rest of
the world.
The multilayered structure of the US health care market makes it a very competitive system, which is good, speaking as a health economist. But it also
becomes very non-transparent to consumers and the general public. This
problem is touched by Moore when he presents the tragic case of a mother
loos-ing her young daughter after urgent treatment is denied by a hospital
only because the health insurance insists on referral to another hospital the
company has a contract with. This case cannot be typical and must not happen in the US simply because any hospital is obliged to offer life-saving services regardless of insurance coverage. Showing this as an example of profit
maximizing insurance companies is unfair, since this simply seems to be a
sound legal case the mother should fight in the name of her daughter. One
thing this example does make crystal clear to a European, is that, in the US,
not every hospital or physician is there to treat every single citizen. We are
simply not used to the idea to be only entitled to go to those service providers
our health insurance has a contract with. This non-transparency would present a major problem in our perception of the system as a whole.
One approach to tackle non-transparent treatment processes is to base decisions on treatment alternatives on scientific medical and health economic
evidence and research. This trend has been and will be one of the most
important political topics in Europe and definitely will be one of the topics in
the US in the coming years. Some patients in the film do not receive specific treatments because supposedly no efficacy has been shown by scientific
research up to that point. The assessment if there is scientific proof or not is
very problematic in the hand of a single employee of an insurance, especially if this employee has an incentive to deny treatments simply because he
can raise his salary by doing so. But looking at medical benefits as well as
cost benefit ratios has been and must be an issue not only in Europe becoming more and more attractive in a world with budgetary constraints where
everybody has the vision of 'value for money'. For some treatments some
European countries (e.g. drugs for loosing weight in obese patients) reached
different conclusion for their decision on re-imbursement. This urges the
need for every health care system to evaluate innovations within its specific
context and to define an optimal level of 'adequate' health care.
Looking over to Europe, Moore speaks with an English hospital physician
who explains that he chooses a therapy only looking at the specific health
care need of a patient and not at funding issues. The film is blanking out the
long and painful time period the National Health Service (NHS) fought with
substantial under-funding making no investments in the infrastructure. These
days' problems with e.g. waiting lists for treatment are not so huge any more
and salaries of physicians have gone up. To reach this goal Great Britain had
to reach a broad societal consensus to spend a higher proportion of tax revenues on health care. This process was furthermore aided by the fact that
Great Britain was lucky to find itself in an economically prosperous phase. If
the stream of financial resources continues to flow in a recession still
remains to be seen. >
January/February 2008 ISPOR CONNECTIONS 13
In wrapping things up, what implications does this film
have to a European audience? We have the fear that a lot
of Europeans only will experience a comforting but creepy
sensation looking at this bizarre health care system which
luckily seems to be very distant from ones own experience and beliefs. But we shouldn't make ourselves too
comfortable in our cinema seat: An orientation of the
European health care systems towards a more competitive approach seems inescapable with a much worse
demographic change in Europe than in the United States
as well as rising costs for health care due to the progress
in medical technology. The vision at the end of the movie
everybody should be nice and help one another and not
only look at financial profits definitely cuts a long story too
short. Individuals who use wrongly set incentives within
the system for their own advantage exist everywhere
regardless of the underlying system. The conflict of goals
between general (and affordable) health care for all and a
health care system that searches for efficiency via substantial competition between its participants is not solved
as easily as Moore implies with his film.
With this in mind the scarecrow of 'socialized medicine'
existing in all its different facets in Europe surely is not the
Holy Grail for the US as their health care system isn't the
one and only blueprint for health care systems in Europe. IC
ISPOR CONNECTIONS Editorial Policy
The following editorial rules and regulations were established to ensure that the ISPOR
CONNECTIONS continues to serve as a scholarly, informative, and unbiased communication and networking tool for the benefit of ISPOR members around the world.
• All submissions are to be original contributions prepared by ISPOR members. Certain exceptions will apply
as determined by the editorial staff.
• All submissions are subject to editorial review, verification, edit, and preemption, and submission of an
article or column to ISPOR CONNECTIONS does not guarantee its publication.
• “Opinions” or “Letter to the Editor” submissions may be edited for space, grammar, and clarity, but NOT to
in any way alter the overall content or context of the submission.
• No overt or implied bias or advertisement for any commercial enterprise will be allowed within the editorial
pages of this publication. All advertisements are purchased and are located in a separate, readily identifiable
section of ISPOR CONNECTIONS.
• The Editor will accept submissions in the forms of original authored articles and columns; in-depth personal
interviews on subjects of interest and relevance to the discipline; and summary opinions and synopses of
published works, etc.
• All synopses, summaries of previously published works, or references must be properly sourced. They
should be listed and numbered consecutively in Arabic numerals in the order in which they are cited in the
text. Reference style should follow that of Index Medicus.
• All submissions must be in Microsoft Word (version 5.0 or later), double-spaced, approximately 1500-2000
words, and contain only limited formatting. Accompanying photos, graphs and tables with appropriate
captions are strongly encouraged.
• All submissions must contain the author/submitter’s name, credentials, title, company or affiliation, and
email address.
• All submissions must be electronically forwarded with all attachments to Steve Marx, ISPOR CONNECTIONS
Editor-in-Chief via isporconnections@ispor.org no later than the 15th of January, March, May, July, September,
or November of each year.
For further information, please contact Steve Marx, Editor-in-Chief, at
isporconnections@ ispor.org or Stephen Priori, Managing Editor, at spriori@ispor.org.
< advertisement >
14 January/February 2008 ISPOR CONNECTIONS
ISPOR CORNER
Boards of Directors Take Action in 2007
Marilyn Dix Smith PhD, ISPOR Founding Executive Director
ISPOR 2006-2007 Board of Directors (June 1-December 31, 2007): President - Michael Drummond, PhD, University of York; Past- President - Peter J.
Neumann, ScD, Tufts University School of Medicine; President-elect - Diana Brixner PhD, University of Utah, College of Pharmacy; Directors - Joyce Cramer,
Yale University School of Medicine; Scott Ramsey, MD, PhD, Fred Hutchinson Cancer Research Center; Shu Chuen Li PhD, National University of Singapore,
Department of Pharmacy Science; Uwe Siebert MD, ScD, University of Health Sciences, Medical Informatics & Technology; Marc Berger MD, Outcomes
Research & Management, Merck & Company, Inc.; Treasurer- Lorne Basskin, PharmD, Healthsouth Sunrise Rehabilitation Hospital; Executive Director - Marilyn
Dix Smith, RPh, PhD, ISPOR.
ISPOR 2007-2008 Board of Directors (July 1-December 31, 2007): President - Diana Brixner PhD, RPh, University of Utah, College of Pharmacy, President;
Past-President - Michael Drummond, PhD, University of York; President-elect - Chris L. Pashos, Abt Associated, HERQuLES; Directors - Marc Berger, MD, Eli
Lily and Company; Lou Garrison, PhD, University of Washington; Shu Chen Li, PhD, University of Newcastle; Uwe Siebert, MD, ScD, University of Health
Sciences, Medical Informatics & Technology; Richard Willke, PhD, Pfizer; Treasurer-Karen Rascati, PhD, RPh, University of Texas; Executive Director - Marilyn
Dix Smith, RPh, PhD, ISPOR.
The ISPOR 2006-2007 and 2007-2008 Boards of Directors had yet another busy year in 2007. The Boards met six times (4 teleconferences and 2 face-to-face
meetings). The Board approved the following:
ISPOR Vision Implementation
• To address new initiatives identified at the
2007 ISPOR Leadership Retreat:
Research Excellence: the Health Science
Policy Council should consider the following topics in the development of new ISPOR initiatives
[comparative effectiveness; methods for extrapolating beyond data (lifetime) and validating pharmacoeconomic models; better analysis of comorbidities & impact of disease; developing an
inventory of methods from other disciplines
including partnering with other disciplines;
patient advocacy council]
Reaching Out to Decision-makers: a Decisionmaker Ad Hoc Group were formed to consider
the following topics in the development of new
ISPOR initiatives [strategy to get key HTA individuals involved in ISPOR; work with decisionmaker organizations]
Promoting Education: the Education
Committee should consider the following topics
in the development of new ISPOR initiatives [for
distant learning, content development; for short
courses, train the educators & link with professional organizations to determine their
interest/needs]
International Growth: the Asia & Latin
America Consortia should develop a needs
assessment to identify issues (e.g. member's
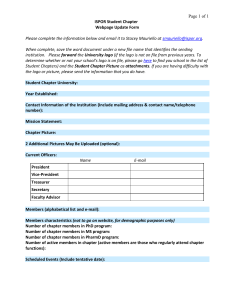
interest, barriers to becoming members & transfer of knowledge from the “west”)
• The Board approved the ISPOR Revised Code
of Ethics. A request for comments was sent to
the ISPOR members with a 30-day comment
period at:
http://www.ispor.org/workpaper/CodeOfEthics.asp.
A Board Ad Hoc Committee as well as the New
Code of Ethics Task Force Chair was formed to
review the comments and recommend actions.
Financial Actions:
• 2007 budget was approved.
• With the goal to improve the content of
ISPOR CONNECTIONS, the following benefits
were approved for the ISPOR CONNECTIONS
Editor-in-Chief: complimentary registration for
the ISPOR Annual International Meetings and
Annual European Congresses and travel reimbursement per ISPOR Travel Reimbursement
Policy and hotel room reimbursement for 4 days.
• The Board approved that annual meeting /
congress invited issue panelists and moderator
(except individuals employed by industry)
receive a complimentary registration, hotel room
(one night stay for intra-continental and two
nights for transcontinental travel), travel expense
reimbursement per ISPOR Travel
Reimbursement Policy.
• The Board confirmed the appointment of
Karen Rascati as the 2007-2010 ISPOR
Treasurer.
Student Actions:
The following Student Chapters were approved:
Warsaw School of Medicine Student Chapter
(Poland), University of Texas at Houston Student
Chapter (USA), and McMaster University
Student Chapter (Canada).
Local Chapter Actions:
The following ISPOR Local Chapters were
approved: Argentina, Chicago (USA), ChinaShanghai, Slovakia, Serbia, South Africa,
Colombia, Chile, Israel, Hungary, and Greece.
Award Actions:
• The ISPOR International Fellowship Award
description, nature of the awards, award
requirements, selection criteria, and selection
process were approved including a follow-up
report after the Fellowship experience and 2
years later.
• The Board recommended that “financial need
may be considered” is added to the selection
criteria for the ISPOR International Fellowship
Award.
• The deadline for candidate submission for the
ISPOR International Fellowship Award is
changed from September 30th to November
30th of each year.
• The Board approved Dr. David Eddy as the
2007 Avedis Donabedian Lifetime Achievement
Awardee, Dr. Todd Lee as the 2007 Bernie J.
O'Brien New Investigator Awardee; the ISPOR
Board of Directors Service Awardees (Peter
Neumann, 2005-2006 President; Joyce Cramer,
2005-2007 Director, Scott Ramsey, 2005-2007
Director; Lorne Basskin, 2004-2007 Treasurer)
and the ISPOR Distinguished Service Awardees
(Scott Ramsey, 12th Annual International
Meeting Program Committee Chair; Michael
Barry and Michael Drummond, 10th Annual
European Congress Program Committee Chairs;
Joyce Cramer, ISPOR Medication Compliance
and Persistence SIG Chair; and the 2006-2007
ISPOR Student Chapter Presidents); the recipient
of the 2007 ISPOR Research Excellence
Awardee in Methodology Anirban Basu, PhD, for
his paper "Scale of Interest vs. Scale of
Estimation: Comparing Alternative Estimators for
the Incremental Costs of a Co-morbidity," Health
Econ 2006:15:1091-107; and the recipient of
the 2007 ISPOR Research Excellence Awardee
in Practical Application John Hsu MD, MBA,
MSCE for his paper "Unintended Consequences
of Caps on Medicare Drug Benefits", N Engl J
Med 2006;54:349-59.
• The Board approved that the Value in Health
Co-editors, with 4 or more years of service and
who have resigned or whose term has ended,
receive an ISPOR Distinguished Service Award
during the Annual Meeting Awards Program
• The Board approved that the Chair and ViceChair of the ISPOR 1st Latin America
Conference, Diana Pinto and Rafael Alfonso, as
recipients of the ISPOR Distinguished Service
Awards. >
January/February 2008 ISPOR CONNECTIONS 15
Publication - Value in Health
Actions:
• The Board supported the recommendations of
the Value in Health Management Advisory Board
that Value in Health Editor-in-Chief, Editorial
(Co-editors) Board, and Editorial Advisory Board
policies and procedures are developed to define
responsibilities, term and criteria for term
renewal. The Board also recommended that coeditors receive a financial reward if 80% of the
time to first decision is <30 days each year;
provide honorarium to reviewers and provide
financial rewards to reviewers if the review is
completed in < 30 days.
• The Board approved the Value in Health
Editor-in-Chief, Editorial Board, and Editorial
Advisory Board polices & procedures.
• The Board approved the Value in Health
Editorial Board (Co-Editors) purpose, term, and
responsibilities
• The Board approved the Value in Health
Editorial Advisory Board purpose, term, and
responsibilities.
• The Board agreed with the increase in the
number of co-editors from 11 to 12 as recommended by the Editor-in-Chief.
• The Board approved Andrea Manca, PhD, Senior
Research Fellow, Centre for Health Economics,
University of York as Value in Health Co-editor.
• The Board approved Paul Schuffham as a
Value in Health Co-editor.
Publication - ISPOR CONNECTIONS
Actions:
• The Board approved Thomas Mittendorf PhD,
MSc, Universität Hannover, Hannover, Germany
and David Thompson PhD, Vice President,
Global Health Economics, Medford, MA, USA as
2008-2012 Co-Editors-in-Chief for ISPOR CONNECTIONS. The Co-Editors-in-Chief, along with
current Editor-in-Chief Steven Marx, and ISPOR
CONNECTIONS Managing Editor, Stephen Priori,
will develop the roles of each Editor-in-Chief.
Organizational/Policies and
Procedures Actions:
• The Board approved that the number of
Directors on the Board of Directors is increased
from 5 to 7 Directors and the Nominations
Committee is responsible to assure that the
Board is a balanced representation of the ISPOR
membership with respect to education, professional interests, work experience, geographic
location, and gender.
• The Board approved the policies and procedures
for the ISPOR Health Science Policy Council.
• The Board approved the policies & procedures for formation and naming of a task force.
• The Board approved the 2007-2008 Board
sub-Committee chairs and members.
Meeting Actions:
• The ISPOR Annual Meeting/Congress Program
Committee Chairs Standard Operating Procedure
(SOP) was approved with the recommendation
that in a teleconference, ISPOR staff, using the
SOP questionnaire, interview and summarize the
Program Committee Chairs issues and suggestions for improving the ISPOR Annual Meetings.
It was suggested that the next year's Program
Chair(s) also attend this teleconference.
• The Board acknowledged the new category of
abstract submissions for the ISPOR 12th Annual
International Meeting - Case Studies in Health
Care Decision using Costs and Outcomes
Research Data. This initiative is to address the
Vision 2010 goal to reach out to health care
decision-makers [i.e.:. .include individuals interested in the use of information on the costs and
consequences of health care interventions as
well as the processes by which health care
decisions are made]. These case studies are to
be submissions from health care decision
maker that describe situations where organizations attempted to integrate cost and outcome
information into their processes and procedures. Submissions describing successes,
works in progress, or failures are encouraged.
.
Special Interest Group/
Committee/Task Force/
Council/Consortium Actions:
• The Board approved Patient Reported
Outcomes (PRO) Good Research Practices Task
Forces to address the following topics: Use of
Existing PRO Instruments and their Modification,
PRO Instrument Creation, Changing Culture or
Language of PRO Application, Changing Mode
of Administration of PRO Instrument including
ePRO, and Development of PRO Instruments for
Children and Youth as recommended by the
Health Science Policy Council.
• The Board endorsed the ISPOR Fellowship
Standards Task Force initiative of publishing
guidelines for groups interested in developing
post-graduate pharmacoeconomic fellowship
programs and for students interested in pursuing such programs; 2) encouraged the collaboration of ISPOR Fellowship Standards Task
Force with the American College of Clinical
Pharmacy in the development of a joint statement to be published in Pharmacotherapy; and
3) recommended that the Task Force consider
submitting a Letter to the Editor to Value in
Health referencing the Pharmacotherapy article.
[Note: An article on the Pharmacoeconomic
Fellowship Guidelines could also be published in
ISPOR CONNECTIONS and at the ISPOR website
with a link to Pharmacotherapy. It was also suggested that an article on historical trends in the
types of training & implications for outcomes
research would be of interest.]
• The Board approved a Retrospective
Database Good Research Practice Task Force
with the goal to define good research practices
for longitudinal data analysis with time-varying
measures including time-dependent confounding variables and ensure internal validity and
improve causal inference from observational
studies using retrospective databases.
• The Board approved that the Health Care
Strategy Council is renamed the Health
Technology Assessment Council to be consistent with current initiatives of the Society and
that this Council continue to address the
missions as stated at: http://www.ispor.org/
councils/HTA_council.asp
ISPOR Comments on Public Policy:
• The Board approved that ISPOR provide
comments to the EUnetHTA Core Model. In this
approval the Board is not supporting any specific recommendation, but the process of providing comments to EUnetHTA. The approved
ISPOR Letter of Comments and the EUnetHTA
HTA Core Model is at: http://www.ispor.org/
workpaper/ispor_comments/index.asp.
ISPOR CORNER
ISPOR Board of Directors Elections 2008
he International Society for Pharmacoeconomics and Outcomes
Research is a member-driven organization. Your participation is critical.
The activities of the organization are response to member needs. As a member-driven organization, its governance is determined by the membership.
T
The ISPOR BOARD OF DIRECTORS is responsible for the general supervision
and management of the Society. The Board of Directors consists of the
Officers (President, President-Elect, Immediate Past President) and now
16 January/February 2008 ISPOR CONNECTIONS
seven Directors. The term of office is July 1 to June 30. The term of office
for the President is one year. The term of office for the Directors is two years.
In this election, the president-elect (term of office: president-elect 20082009 and as president 2009-2010) and five Directors' term of office will be
elected.
The Nominations Committee has paired the Director positions to assure a
balanced representation of the ISPOR membership on the Board of Directors
and to complement the professional and experience backgrounds of the
incumbent Board members. The candidates for the Board of Directors bring
diverse professional training and work experiences in clinical practice, outcomes research, health economics, pharmacoeconomics, and health technology assessment from the United States, Canada, Europe, and Asia.
You, as an ISPOR member, have an opportunity to choose the leadership of
this organization from the distinguished candidates.
MAKE YOUR VOICE HEARD. PLEASE VOTE.
YOUR BALLOT MUST BE RECEIVED BY April 4, 2008
To vote, go to the ISPOR website at: www.ispor.org
PRESIDENT-ELECT CANDIDATES
Michael Barry MD, PhD, FRCPI
Lorenzo Giovanni Mantovani PhD
For 10 years Dr. Michael Barry has been a Consultant Clinical
Pharmacologist and Senior Lecturer in Clinical Pharmacology
at the University of Dublin, Trinity College, Dublin, Ireland, and
head of the Irish National Centre for Pharmacoeconomics
which advises the Department of Health in relation to the pricing and reimbursement of pharmaceuticals in addition to conducting health technology assessments (HTAs). Dr. Barry has served on national advisory groups and is a board member of the newly formed Health Information & Quality
Authority (HIQA) whose remit includes HTA.
As a clinician he works at St. James's Hospital, Dublin performing both inpatient
and outpatient duties. He runs weekly clinics in cardiovascular and internal medicine
and lectures on clinical pharmacology and internal medicine to undergraduate medical
students at Trinity College. As a Royal College of Physicians of Ireland specialist trainer, he is actively involved in post-graduate medical teaching. He has been chair of local
research ethics committees.
Dr. Barry, a graduate of University College Cork, Ireland, qualified in medicine in
1984. He obtained a 1st honours BSc degree in pharmacology in 1981 and completed a PhD in pharmacology at Trinity College in 1990. He became a member and Fellow
of the Royal College of Physicians of Ireland in 1988 and 1995 respectively. Prior to
his current post, Dr. Barry was Consultant Pharmacologist and Senior Lecturer at the
University of Liverpool, UK, from 1990 -1998.
He has over 100 peer-reviewed publications on clinical pharmacology, general
medicine, HTA and pharmacoeconomics. Recent publications relate to the cost effectiveness of universal hepatitis B and pneumococcal vaccination strategies in the Irish
health care setting. As a member of ISPOR he co-chaired the 10th Annual European
Congress held in Dublin in October 2007.
Lorenzo Giovanni Mantovani was born in Milan, Italy. Currently
Dr Mantovani is Director of CIRFF, Center of Pharmacoeconomics, Federico II University of Naples, Naples, Italy. He
was Director and Co-founder of the Center of Pharmacoeconomics of the University of Milan. He has been coordinator
of the Master of Science in Pharmacoeconomics since 2001.
Dr. Mantovani holds a Degree in Economics from Bocconi University of Milan, Italy.
He has a Doctor of Science in Epidemiology from Erasmus University of Rotterdam,
the Netherlands, and received the ISPOR Distinguished Service Award in 2005 for his
service to ISPOR as the ISPOR 8th Annual European Meeting Program Committee Cochair. The main interests of Lorenzo are the economic and outcomes evaluation in rare
diseases, especially haemophilia, and, in general practice, with a focus on evaluation
of adherence and persistence to chronic therapies. He is member of the Haemophilia
International Prophylaxis Study Group, of the European Heamophilia Therapy
Standardisation Board, and Coordinator of the Health Economics Committee of the
Italian Society of General Practice. Lorenzo was President of the Italian Group for
Pharmacoeconomics Studies Executive Board (2002-2004).
He is field editor for pharmacoeconomics for the journal, Pharmacological
Research. He is author or co-author of more than 90 papers published on several journals including Value in Health, Pharmacoeconomics, Blood, European Journal of
Cancer, Human Reproduction, European Heart Journal, American Journal of Kidney
Diseases, Canadian Medical Association Journal, Haemophilia, Journal of
Hypertension, Allergy.
Beyond his academic activity, Dr. Mantovani is advisor for pharmacoeconomics for
several Italian regional health authorities, covering more than 16 millions enrollees.
Within this activity he is co-founder of DENALI, a data warehouse project collecting
and managing health care events of more than 9 millions citizens of the Lombardy
region in Italy.
ISPOR Vision Statement by Michael Barry MD, PhD, FRCPI
The 10th Annual European ISPOR Congress in Dublin 2007 hailed the health technology assessment (HTA) “revolution” and a future of great promise for our discipline.
Any vision for ISPOR must continue to place scientific excellence at its core as quality science is essential for the continued success of this international society. Coming
from a country that has recently embraced HTA, certain challenges are evident, and
these shape my vision for ISPOR. I have little doubt that “capacity” is one of the major
issues and a rate-limiting step. Therefore ISPOR should continue to identify, encourage and support the training and development of the next generation of researchers in
pharmacoeconomics and outcomes research. The support of regional ISPOR groups
would provide the organisational structure to deliver on this vision, particularly in the
resource limited setting.
In Ireland working closely with decision-makers frequently translates our work into
health policy bringing pharmacoeconomics 'to life' once again highlighting the importance of engaging decision-makers who still number too few in our organisation. As
the largest net exporter of pharmaceuticals worldwide, we appreciate the balance
between achieving value for money and supporting industry innovation; hence an
important component of my ISPOR vision is continuing our development of a multidisciplinary society. This includes reaching out to fellow clinicians who may not always
embrace our ideals.
Following the ISPOR European Congress in Dublin, I have witnessed the significant
impact on all stakeholders across the country and such meetings are central to my
vision for ISPOR. An essential component to deliver on any ISPOR vision is the excellent ISPOR team who I came to know very well whilst co-chairing the Dublin meeting.
The prospect of working with such colleagues and fellow members in contributing to
the future of ISPOR is a real honour for me.
ISPOR Vision Statement by Lorenzo Giovanni Mantovani PhD
In recent years ISPOR has invested much energy into scientific development, and into the
furthering of scientific understanding among members. While these efforts are acknowledged within the society, they are not fully recognised by decision-makers at large.
The ISPOR name quite literally stands for the synthesis of evidence related to costs,
clinical effects, and the health status of patients as follows: Costs: a major consideration for healthcare providers and payers; Clinical Effects: the primary focus for clinicians; Health Status: the foremost concern of patients. We must assert our collective
knowledge and experience of these three domains, and of the interconnections
between them. In order to fulfil the ISPOR mandate, we must become more visible,
more credible, and more influential within national and international healthcare
debates. This is fundamental to ISPOR's existence. To achieve this we must further
develop our collaborations with the three key decision-making bodies: 1) clinical
decision-makers; 2) payers; and 3) patients.
ISPOR and its members can be the catalyst that brings these three stake-holders
together, with ISPOR acting as a developer, guardian and guarantor of methods. It is
my vision that ISPOR should tighten its educational and research links with other medical scientific societies, with national/regional and local payers' associations, and with
patient advocacy groups. Joint sessions at major conferences, and multidisciplinary
research groups, can be the starting point to raise the ISPOR profile, and to develop
common dialogue with those who can benefit from the message of ISPOR and its
members.
>
January/February 2008 ISPOR CONNECTIONS 17
CANDIDATES FOR DIRECTOR (POSITION 1)
Dyfrig Hughes BPharm MSc, PhD,
MRPharmS
Dr. Dyfrig Hughes is Senior Research Fellow in
Pharmacoeconomics and Deputy Director of the Centre for
Economics and Policy in Health, Bangor University, Bangor,
Wales. He was previously at the University of Liverpool,
where he was lecturer at the Department of Pharmacology
and Therapeutics. He is a pharmacist and pharmacologist by training, having
completed his PhD in cardiovascular pharmacology. He was subsequently
awarded a National Health Service Post-Doctoral Fellowship in Health Economics,
and gained an MSc in Health Economics at the University of York.
His research interests include the assessment of the impact of non-compliance on the effectiveness and cost-effectiveness of pharmaceuticals, and economic evaluations of medicines and of pharmacogenetic testing. Dr. Hughes has
authored or co-authored over 60 articles and book chapters, including 20 pharmacoeconomic assessment reports that have directly informed national policy.
He received the 2004 Galen Award from the Royal Pharmaceutical Society of
Great Britain for pharmacy practice research.
Dr. Hughes is a member of the National Institute for Health and Clinical
Excellence (NICE) technology appraisal committee, and Deputy Health Economist
for the All Wales Medicines Strategy Group. In addition, Dr. Hughes is a member
of the British Pharmacological Society and the International Health Economics
Association, as well as a frequent reviewer for peer-reviewed journals in health
economics, clinical pharmacology and health services research. He serves on
the editorial boards of the journals PharmacoEconomics and Pharmacoepidemiology & Drug Safety.
Dr. Hughes is an enthusiastic member of ISPOR and has contributed to the
Society's activities in many capacities, including Chair of the ISPOR Medication
Compliance and Persistence Special Interest Group (SIG). He previously chaired
this SIG's Economics of Compliance & Persistence Working Group, and has contributed to the work of the ISPOR Drug Costs Standards Task Force.
ISPOR Vision Statement by Dyfrig Hughes BPharm MSc PhD MRPharmS
ISPOR's vision for 2010 includes building on past achievements by reaching out
to existing and new members to enhance its reputation through education, fostering of research and growth. As an ISPOR Board member, I will take an active
role to help ISPOR achieve the excellence for which it stands.
As a member of two national health care decision-making bodies, I am only
too aware of the importance of pharmacoeconomic evaluations and patientreported outcomes in informing challenging decisions on health technologies. In
the cost-conscious world that we live in, a greater understanding of the concepts
and methods involved is essential. For non-specialists, and for professionals in
countries with less experience in these fields, ISPOR can play a leading role, and
I will prioritise education by promoting the expansion of our local chapters, short
courses, student networks, and workshops.
I have a track record of leading international collaborative research through
ISPOR's Special Interest Groups. The Medication Compliance and Persistence
SIG has become the most active of ISPOR's SIGs, with over 40 members, several publications in Value in Health, and a number of ISPOR presentations and
workshops. ISPOR's SIGs are an excellent platform for fostering research excellence, and promoting collaborations. I will encourage the development of new
SIGs wherever possible.
I am delighted to have been nominated as a candidate for the ISPOR Board of
Directors, and if elected, I will strive to achieve ISPOR's vision for the future, and
serve its members honourably.
18 January/February 2008 ISPOR CONNECTIONS
Paul Kind
Paul has a wide-ranging, multidisciplinary background and
a research career that spans more than 30 years during
which he has majored in the development and application
of health status measures for use in clinical and economic
evaluation. Paul combines academic research with consultancy in the field of health-related quality of life measurement. He has provided expert advice to government, international agencies and
the pharmaceutical industry throughout the world. Until this year, he was
Professor of Health Economics in the Centre for Health Economics at the
University of York, York, UK and Principal Investigator in the Outcomes Research
Group, but has taken early retirement to concentrate on his consultancy, Quality
Outcomes, and its specialist services for the pharmaceutical industry. He has
held a number of academic positions across Europe and North America, including at the University of Uppsala, Sweden, McGill University, Montreal, Canada,
and the University of Wisconsin, Madison, Wisconsin, USA. He has been a faculty member of the Netherlands Institute for Health Sciences and an Honorary
Fellow of the National Centre for Quality of Life Research, St. Petersburg. He has
been an elected Board member of ISOQOL and played an active part in the formation of the ISPOR Quality of Life Special Interest Group, receiving a
Distinguished Service Award in 2001. He was ISPOR's representative on the FDA
“Harmonisation” Project that established the PRO. Paul is a regular contributor to
ISPOR meetings in Europe and the US, having first presented at APOR,
Philadelphia in 1997. He has participated in regional ISPOR meetings in Russia,
South America, and China. Paul is a Founder Member and past-President of the
EuroQoL Group and was centrally involved in the development of EQ-5D.; he currently Chairs the EuroQoL Group's Scientific Executive Committee. He serves on
the editorial advisory boards of several academic journals including Value in
Health and PharmacoEconomics.
ISPOR Vision Statement by Paul Kind
ISPOR is now the leading organisation in the field of outcomes measurement,
representing a natural locus between health care decision-makers, policy analysts and research scientists from both the public and private sectors. For those
of us who recall the pre-ISPOR days, there has been a considerable shift in its
structures, processes and outcomes. APOR (the original name of our Society)
naturally attracted a largely US membership with pharmacy or industry background. As the rebranded International Society, ISPOR sought to widen its geographical catchment area to embrace a worldwide audience - an objective that
has been emphatically achieved. The ISPOR Annual European Congress now
competes in scale with the ISPOR Annual International Meeting held in North
America; regional meetings provide access to a global membership. By widening
the scope of the research, applications and methods that are recognised through
its programme of meetings, ISPOR has moved away from its original pharmaceutical base. Diagnostics, devices and other technologies now form a legitimate
part of the ISPOR mainstream. This is not a rejection of the past - merely a reflection of a future in which research methods and their implementation have grown
beyond the boundaries of pharmacoeconomics.
For ISPOR to maintain its lead role it must continue to foster the practice of
high quality science and the communication of that product to patients, providers
and other relevant stakeholders - including national governments. It is not enough
to undertake technically competent work - having a leadership role means interpreting that knowledge for a wider, non-technical audience. That ethos extends to
the creation of an internationally recognised curriculum that ensures new entrants
to the field are properly qualified to meet the standards we have set. I would
make the achievement of these goals my personal priority and would be honoured to serve on the Board if so elected by the Society's membership.
CANDIDATES FOR DIRECTOR (POSITION 2)
Penny Mohr MA
Dennis W. Raisch, PhD, RPh
Penny Mohr, MA, is the Director of the Division of Research
on Health Plans and Drugs within the Office of Research,
Development, and Information at the Centers for Medicare
and Medicaid Services (CMS), Baltimore, MD, USA. The
division is responsible for conducting research and oversight of demonstration evaluations pertaining to the
Medicare prescription drug benefit, Medicare managed care, and the end-stage
renal disease program. In addition to her management responsibilities, Ms. Mohr
serves as a technical authority within the Agency on issues pertaining to the
adoption, diffusion, and cost-effectiveness of health care technology in the
Medicare program. She is a member of CMS' Council for Technology and
Innovation, charged with coordinating coverage, coding and payment processes
for new medical technologies, as well as promoting the exchange of information
on new technologies between CMS and other entities. She holds advisory board
positions on the National Institute of Diabetes, Digestive and Kidney Diseases' US
Renal Data System, the American Journal of Managed Care, and Tufts-New
England Medical Centers' Center for Value and Risk in Health Care, and serves
on the Steering Committee for Academy Health's economic interest group.
She has been a member of ISPOR for eight years, and is the Issues Panel
Review Committee Co-chair for the upcoming ISPOR 13th Annual International
Meeting in Toronto, Canada. Prior to joining CMS, she was a Senior Research
Director at Project HOPE's Center for Health Affairs, and outcomes research manager at MedSTAT, where she pursued longstanding interests in medical technology policy and cost-effectiveness research. She has published widely on a variety of health services research topics. Pertinent to this society, Ms. Mohr has
extensive international experience, having worked in more than a dozen countries
in Africa, Asia, the Caribbean, South America, and Eastern Europe. Ms. Mohr
received a Master's degree at the University of Sussex, England where she studied economics.
Dennis W. Raisch, PhD, RPh is Associate Center Director for
Scientific Affairs at the Veterans Affairs (VA) Cooperative
Studies Program Clinical Research Pharmacy (CSPCRP)
and Research Associate Professor at the University of New
Mexico College of Pharmacy, Albequerque, New Mexico,
USA. After practicing as a hospital pharmacist for nine
years, he earned his Masters and PhD degrees from University of Arizona. As a
faculty member of the University of New Mexico, he teaches graduate and undergraduate courses and mentors graduate students. He developed and supervises
a post-graduate pharmacoeconomics research fellowship at the VA CSPCRP.
His research endeavors involve performing health services research, assessing adverse drug reactions, and providing pharmaceutical support for large,
multi-center clinical trials. He participates on numerous national and international clinical trial executive committees. Currently, he is performing retrospective
pharmacoeconomic research of drug therapies using the national VA databases
and collaborating with the Research on Adverse Drug Reactions and Reports
(RADAR) team. RADAR's primary research objective is to identify, assess, and
describe rare, serious adverse drug reactions. He has numerous scientific presentations and over 75 research publications.
As an ISPOR member since 1998, he has served as a member of the Legislative
and Governmental Affairs Committee, the Heath Care Strategy Council, and the
Consensus Development Workshop “Building a Pragmatic Road Forward: An ISPOR
Workshop on the Future of the QALY”. In 2005, he received an ISPOR Distinguished
Service Award for coordinating the development of the ISPOR Managed Care
Research Digest, which was accomplished through the ISPOR Managed
Care/Pharmacy Benefits Management Special Interest Group. Since 2004 he has
chaired the Risk Benefit Management Special Interest Group (RBM-SIG). The RBMSIG conducted a members-based risk/benefit of medications survey, published in
ISPOR CONNECTIONS and presented at several ISPOR Annual meetings. He is also
co-faculty of an ISPOR Short Course on risk-benefit management.
ISPOR Vision Statement by Penny Mohr, MA
The rapid growth of ISPOR's membership is testament to the central place it has
assumed among pharmacoeconomics and outcomes researchers, and I am honored to have been nominated to serve on its Board of Directors. Since ISPOR's
inception, I have seen continual improvement in the scientific rigor of articles
published in its journal, Value in Health, and the caliber of presentations and
keynote addresses at its meetings. ISPOR has also been successful in helping
to enhance the scientific methods underpinning outcomes research, and educating its membership about cutting-edge techniques to measure the comparative
value of medical technology. I would like to see continuing improvement in these
areas, particularly in the quality of the peer review process for its scientific meetings, which is essential for its credibility.
ISPOR has not performed as well in reaching out to decision and policy-makers, although this is part of the organization's long-term vision. Users of outcomes research, including physicians, managed care representatives, and government decision-makers still represent only five percent of total membership. If
the ISPOR membership were to elect me to the Board, my key focus would be to
expand ISPOR's global reach among decision and policy-makers. I would encourage the Society to increase its efforts to engage in meaningful dialog between
industry, researchers, and decision-makers, enhance the ways in which research
can be translated into practice, and become an essential reference for policymakers interested in comparative effectiveness research. My previous involvement in organizations such as the International Society for Technology
Assessment in Health Care, which attracted a high proportion of public policymakers, past experience conducting outcomes research for private industry, and
current position working within the federal government afford me unique perspectives that can help ISPOR bridge the communication gap between research and
policies relating to medical technology.
ISPOR Vision Statement by Dennis W. Raisch, RPh, PhD
ISPOR is an organization that has incredible insight into the future of patient outcomes research and its application in health care delivery and decision-making.
This strength is related to the diversity of ISPOR membership, offering perspectives from industry researchers to academicians and from USA to world-wide.
Furthermore, ISPOR has consistently promoted cutting-edge debates from all
viewpoints of controversial issues relevant to patient outcomes research and its
application. As a member of the Board, my efforts will be to continue to promote these efforts as well as the Vision 2010 goals of education, international
growth, research excellence, and reaching out to decision-makers.
No matter how elegant patient outcomes research methodology is, if results do
not ring-true to decision-makers, our efforts are futile. In order to expand the
impact of our research and ISPOR activities, major emphasis must continue to be
directed toward communication with decision-makers; from the patient to the
provider to health care payers to society. The Board has already approved several strategies directed at assuring relevance of research findings to decisionmakers. I have a particular interest in achieving them and helping to develop new
strategies. We need to consider the continually increasing role of patients in
health care decision-making, both at an individual level and a political level.
Patients and providers are appropriately represented at the outer rings of influence in the ISPOR vision diagram. An important future direction of ISPOR is to
develop communication strategies that promote the relevance of our research
findings to those groups. Establishing new relationships and alignments with
patient and provider organizations will help strengthen ISPOR and augment the
application of patient outcomes research.
I am honored to be nominated for ISPOR Board membership and if elected, I
hope to provide a perspective that enhances the achievement of Vision 2010 Task
Force Recommendations.
>
January/February 2008 ISPOR CONNECTIONS 19
CANDIDATES FOR DIRECTOR (POSITION 3)
Zeba M. Khan RPh, PhD
Hong Li PhD, MPH
Zeba Khan is currently Executive Director and Head of U.S.
Pricing, Pricing Strategy & Policy at Novartis Pharmaceuticals
Corporation based in East Hanover, New Jersey, USA. She
leads the development and implementation of pricing and contracting strategy for general medicines. Dr. Khan joined
Novartis in January 2003 as Global Head of Pricing and Health
Economics Strategy, CVM, working and living in Basel, Switzerland for three years
prior to moving to the USA. Prior to joining Novartis, Dr. Khan was employed at
GlaxoSmithKline (GSK), Research Triangle Park, North Carolina, USA, for six years in
various leadership roles in health care management, managed markets and was Senior
Health Outcomes Scientist in North America, Department of Medical Affairs, where
she developed and implemented health economics and outcomes strategies to support market access. Prior to joining the pharmaceutical industry in 1997, Dr. Khan
was a clinical pharmacist at University Hospital, University of Utah Health Sciences
Center and Poison Center Specialist at the Intermountain Regional Poison Control
Center, both based in Salt Lake City, Utah, USA.
Dr. Khan earned her pharmacy degree from the University of Utah and her MS and
PhD in Pharmacy Administration, Pharmacoeconomics/Health Outcomes from The
University of Texas at Austin. Over her 18-year career, she has gained both USA and
global experience in strategic pricing and contracting, health economics, outcomes
research, managed markets, health care management, and clinical pharmacy. She has
authored/co-authored over 90 publications, patents, and podium/poster presentations.
Dr. Khan has been a member of ISPOR since 1996, and has served in many capacities, including membership on the ISPOR Vision 2005 Committee, ISPOR Fellowship
Committee, ISPOR Awards Committee, and ISPOR Program/Planning Committee.
Most recently, she serves as the Co-Chair of the ISPOR Short Course Committee and
has served over 8 years as the ISPOR Student Network Faculty Advisor.
Working out of Singapore, Dr. Li is Group Director, Department
of Global Epidemiology and Outcomes Research, Bristol-Myers
Squibb (BMS) Company. In this role, he supports and coordinates outcomes research activities for BMS products of multiple therapeutic areas in the Asia Pacific region. In addition to
the responsibilities in BMS, Dr. Li is an Adjunct Associate
Professor of University of Cincinnati. Furthermore, Dr. Li is a founding member of the
ISPOR Asia Consortium. From 2005 to 2007, Dr. Li served the role of the first Chair of
the Advisory Committee of the ISPOR Asia Consortium.
Dr. Li holds a Ph.D. degree in Health Services Research/Epidemiology and a Master
of Public Health (MPH) degree in International Health Policy from School of Public
Health, University of North Carolina at Chapel Hill, USA. His major academic research
interests are health care project evaluation, international health care policy evaluation,
and applied epidemiology methodology in health services research, such as drug utilization evaluation, evidence-based medicine, and naturalist study design.
Since mid-1990s, Dr. Li has publications in journals of JAMA, Value in Health,
Journal of Clinical Psychology, and Psychiatry Research. In addition, Dr. Li has coauthored in proceedings of various international conferences such as American
Psychiatry Association, European College of Neuropsychopharmacology (ECNP),
Collegium International Neuro-Psychopharmacologicum (CINP), International Society of
Pharmacoepidemiology (ISPE), and ISPOR conferences. Dr. Li has given presentations
on an array of topics to different audience including the World Health Organization,
China Ministry of Labor and Social Security, Thailand Food and Drug Administration,
Medical Association of Macau, Seoul National University, Beijing University, Fudan
University, the National Health Research Institute of Taiwan, the Bureau of National
Health Insurance of Taiwan, the Regional Conference of Health Care Cost Effectiveness
in Singapore, and Seoul International Digest Disease Symposium (SIDDS).
ISPOR Vision Statement by Zeba M. Khan RPh, PhD
ISPOR Vision Statement by Hong Li PhD, MPH
ISPOR has grown to become a strong, international organization in a short time. My
vision is to evolve an organization that is sustainable in an ever changing environment.
That evolution can only be accomplished through globalization, international growth,
collaboration and teamwork locally, regionally, and globally. Given the industry challenges, ISPOR must be the leader in establishing guidelines/standards that foster better research, leading to better decision-making and improved patient care. We must
also lead in developing and communicating health outcome and scientific information
while fostering continued education and shaping the future. These challenges can be
addressed by: 1) Strengthening educational activities, distance learning programs, and
short courses by considering feasibility of certification, leveraging the ISPOR
Educator's Toolkit, tapping into the ISPOR Speaker's Bureau, and reaching out to new
groups in our discipline globally; 2) Empowering our task forces and work groups to
advance the science, methods, interpretation, and their application; 3) Understanding
payer needs since the economic evidence required for decision-making may vary
depending on geography, regulations, and country-specific needs. ISPOR must reach
out to decision-makers at all levels to build partnerships; and 4) Supporting student
initiatives to ensure student representation in all ISPOR committees. Since students
are the future of ISPOR, they should be engaged early to develop future leaders and
provide growth for the organization.
My professional experience in the US and Europe and my active involvement with
ISPOR has prepared me to see this vision through to realization. Since 2004, I have
served as Co-Chair of the Short Course Committee which has focused on developing
content, building new courses, and evaluating courses for quality assurance. As a
result, attendance and the number of short courses have tripled since 1998. As the
ISPOR Student Advisor, I am proud of the accomplishments of the Student Network.
We have grown from 5 members in 1995 to over 400, comprising 15% of the ISPOR
membership with 38 ISPOR Student Chapters in the USA, Canada, Europe, and Asia.
I welcome the opportunity to work with you to continue to build a future ISPOR organization that is sustainable and recognizable across all scientific disciplines.
I envision ISPOR advancing the practice of pharmacoeconomics and outcomes research
globally and enabling decision-makers to best utilize health care resources locally.
A decade ago, the ISPOR annual conference in the USA was the only ISPOR meeting for members to attend; now, ISPOR conferences are also held in Europe, Asia
Pacific, and Latin America. I believe this is not simply a geographic expansion of the
organization but an evolution of outcomes research across the globe. As ISPOR is
engaged in more international activities, the issues that we face become more complex in terms of different health care systems, variable health care resources, cultures,
and values. Ideally, pharmacoeconomic and outcomes research methodologies will
continue being enhanced at the global level in a way that use of scientific evidence can
be translated into the best decision-making for health care resource utilization; yet, it
remains the critical challenge for all of us. To me and many ISPOR members as well,
however, the vision of ISPOR can turn this challenge into an opportunity and reality.
MAKE YOUR VOICE HEARD. PLEASE VOTE.
YOUR BALLOT MUST BE RECEIVED BY APRIL 4, 2008
TO VOTE, GO TO THE ISPOR WEBSITE AT:
www.ispor.org
20 January/February 2008 ISPOR CONNECTIONS
CANDIDATES FOR DIRECTOR (POSITION 4)
Hans-Peter Dauben MD
Don Husereau BScPharm, MSc
Dr. Hans-Peter Dauben, born in Moenchengladbach, Germany, is a
civil servant at the German Institution for Medical Documentation and
Information (DIMDI), Cologne, Germany, an institution within the
scope of the federal ministry of health. After finalizing his training as
a cardiac surgeon at the University of Duesseldorf, Germany, he
moved to DIMDI to establish the German Agency for HTA at DIMDI
on behalf of the federal ministry in 2000 and to develop a structure
to access HTA information, set priorities in HTA and monitor new technology developments
to establish a broad consensus on HTA in Germany. The experiences of information systems
developments lead to the nomination of Dr. Dauben as the national representative for information system development at the European medicine agency (EMEA) in London, UK. Since
2004 he is involved in different working groups developing information principles and systems in cooperation with public agencies and pharmaceutical companies. Since 2006 Dr.
Dauben is also working as a consultant for the public health institution (LIGA) of NorthrhineWestfalia in Bielefeld, Germany, a public institution within the scope of the state ministry of
health. Out of this activity he is involved in describing the need and requirements on how the
state government can set up a system to support innovations in health care environment.
Since 2006 he is also a member of the National Task Force for Public Health Genomic managed by LIGA.
At the University of Cologne he is giving lectures on HTA and evidence-based medicine
since 2002. In addition, he is mainly involved in courses on HTA with dedicated user groups
in the field of health quality assurance and control, pharmacists and physicians in cooperation with different professional organizations. His research interests are mainly focused on
informed decision-making processes, including the methodology development of HTA, systematic evaluation of health needs in health care systems, support systems for innovations
in health care management and improving knowledge management in evidence-based health
care systems.
Since 2000 Dr. Dauben is involved in different European projects. These projects are
related to HTA (ECHTA/ECAHI-EUnetHTA), to pharmaceutical information systems (PPRI)
and to regional implementation of informed decision-making processes (EUREGIO II).
Internationally, Dr. Dauben is a well-known speaker and organizer of conferences, workshops, and educational courses within his areas of experience and interests. He is a member of the ISPOR HTA Council.
Don Husereau is Director of Health Technology
Assessment Development at the Canadian Agency for
Drugs and Technologies in Health (CADTH), Ottawa, ON,
Canada. He received his Bachelor of Science in
Pharmacy in 1993 at the University of Alberta and
worked in community pharmacy practice until 1996. He
completed his MSc in Pharmacy and Pharmaceutical
Sciences (Biotechnology) in 2000, where he also served as a lecturer and
course facilitator for graduate and undergraduate courses. Prior to working at
CADTH, he worked as a consultant for both the International Atomic Energy
Agency and Canadian International Development Agency. He joined CADTH (formerly CCOHTA) in January, 2001. At CADTH, he has overseen the development
of several programs, including a rapid assessment service for policy-makers. In
2005, he led the completion of the 3rd edition of the CADTH Health Technology
Assessment (HTA) Guidelines for the Economic Evaluation of Health
Technologies: Canada. These guidelines represented the first attempt to create
a Canadian national health economic evaluation guideline that extended beyond
pharmaceutical interventions. In his current role at CADTH, he leads the identification and assignment of policy research. In this role, he acts as a convenor
for discussions among health care researchers, health program managers
(policy-makers), assessors, manufacturers, clinicians, and communications
specialists with the aim of meeting decision-maker needs through the optimal
application of research.
Don Husereau has led and served on several national and international committees. He is currently the chair of the Health Technology Analysis Exchange, a
network of Canadian Health Technology Assessors. He has also served as an
advisor for the development of the US Agency for Healthcare Research and
Quality Developing Evidence to Inform Decisions about Effectiveness (DEcIDE)
network.
Don Husereau has successfully fostered international HTA collaborations
with both the National Institute for Health Research HTA program (UK) and
DAHTA@DIMDI (Germany). Through his more recent involvement with ISPOR,
he has contributed to Health Technology Assessment Advisory Council discussions. He is also an academic editor for the Public Library of Science ONE journal and a member of the Cochrane Hypertension Review Group. His interests
include health economic evaluation and scientific epistemology.
ISPOR Vision Statement by Hans-Peter Dauben MD
ISPOR's development over the years has shown the need and the acceptance of the actual
goals described in the ISPOR vision 2010. I feel honoured to be selected as a candidate for
the ISPOR Board of Directors, and if elected, I will be involved in working towards these
goals. My personal experiences and actual work is focussed on three main topics: 1)
Knowledge sharing; 2) Methodology developments focussed on the assessment and support of innovations; and 3) Education and training. Living in Europe and working for
European institutions and projects, the need to learn from each other, the need for clear communication, and the need for requirements to overcome misunderstanding depending on
wordings is a daily challenge. Therefore, my vision for ISPOR is to aim for communication
and knowledge sharing.
Communication - regional growth and collaboration: The spread of our Society to all areas
of the world leads to new challenges in the sense of understanding, knowledge and acceptance of different cultures and health care systems. Regional growth of the Society will require
several efforts to form a basis for common understanding. Within the field of HTA, the ISPOR
HTA Council Roundtable discussions initiated by ISPOR are a first step to promote global evidence and to support and learn from the experience of the local implementation of this. As part
of this process the communication of the three main groups, the scientific community, the
industry and the decision-makers has to be promoted. Additionally topics as equity and fairness have to be integrated within the communication out of different cultures and societies.
Knowledge sharing: Scientific developments transfer and education: The exchange of
global evidence, based on clear and robust scientific methodologies and data is, for all
involved groups, of the highest importance to gain the efficiency needed. These scientific
developments within the different ISPOR work groups have to be transferred and implemented within the existing education institutions. Besides promoting the actual ISPOR courses,
the integration of this knowledge into academic curriculum is needed. Students are not only
a good basis for the future of the Society, but better training and education will also help to
overcome the lack of trained staff in many health management areas.
The scientific developments supported by ISPOR have to focus on feasible and reliable
methods. In the field of HTA, new ways have to be described on how institutions, groups,
members can be supported in implementing innovative technologies not only for pharmaceuticals, but also medical devices and health care management. Based on transparency
and standardization, actual resistance within the different groups can be overcome. I would
very much welcome the opportunity and challenge to work with and for you to foster our
society, to promote the excellence of the knowledge within the Society and to make ISPOR
the basis for including scientific work in daily life.
ISPOR Vision Statement by Don Husereau BScPharm, MSc
It is an honour to be asked to contribute to the leadership of ISPOR, an organization with esteemed and enthusiastic membership motivated by mass collaboration. Through transparency, education, sharing and acting globally, ISPOR
members are committed to applying their unique expertise to optimizing the care
of patients worldwide. It is clear that continued excellent leadership is required
to both achieve and go beyond ISPOR VISION 2010. I believe that ISPOR can
continue to be a model social network and reach its goals by providing
increased attention to several key areas:
Promoting health-focused research: ISPOR members represent a wide-ranging set of perspectives, spanning across key players and jurisdictions that are
responsible health delivery. Members know that excellent health, rather than
excellent health science is their ultimate goal. The shift of focus from health science to health requires continued promotion of methods of valuation of uncertainty, rational priority setting, and ideas sharing in Society meetings and communications.
Promoting health-focused judgement and decision-making: ISPOR has fostered growth in the area of judgement and decision-making through groups such
as the "Health Technology Assessment In Evidence-Based Decisions Group" and
"HTA in Reimbursement Economics Working Group". The complexity of health
decisions requires ISPOR members to increase their use of reliable knowledge
transfer and decision science methods to maximize health impact.
Promoting health beyond interventions: New service and delivery paradigms
for health mean decision-makers must consider organizational, health human
resources, environmental risk management and information technology issues
more than they have in the past. By furthering its Good Research Practice
Standards, ISPOR is in a position to lead future health research in these areas.
I believe I could quite effectively contribute to the ISPOR Board of Directors and
I look forward to your vote and working with you.
>
January/February 2008 ISPOR CONNECTIONS 21
CANDIDATES FOR DIRECTOR (POSITION 5)
Shanlian Hu MD, MSc
Vithaya Kulsomboon PhD
Shanlian Hu is Professor of Health Economics. Director of Training
Center for Health Management and Director of Pharmacoeconomics
Research and Evaluation Center at School of Public Health, Fudan
University, Shanghai, China. At present, he is the Chair of ISPOR
China Doctor Association Chapter. He is elected as Chair of 20082010 ISPOR Asia Consortium Executive Committee as well. He
made great contributions to ISPOR as the ISPOR 2nd Asia-Pacific
(AP) Conference Program Committee Co-Chair in Shanghai, China, in 2006, and is playing
a role in the planning of the upcoming ISPOR 3rd AP conference as Short Course
Committee Co-Chair. He helped to organize a delegation of 30 policy-makers' from China,
with Novo Nordisk Pharmaceutical Co., to attend ISPOR 10th Annual European Congress in
Dublin, Ireland in 2007.
He graduated from School of Public Health, Shanghai First Medical College, and further
pursued his Master Degree in Epidemiology in Shanghai Medical College, and MSc of
Medical Microbiology in the London School of Tropical Medicine and Hygiene, London, UK.
In 1980-1982, he was a WHO Fellow pursuing health service studies in UCLA, UC Berkeley,
and at Harvard in 1986. He has been a member of several China's Ministry of Health (MOH)
Advisory Committees, such as Health Policy and Management, New Type Rural Cooperative
Medical System and Urban Community Health Care. Recently, he is also appointed as
Director of Shanghai Health Development Research Center, under the leadership of Shanghai
Bureau of Health. He uses these platforms to conduct pharmacoeconomics and drug policy
research in China. In his career, he was the Deputy Director of National Health Economic
Institution in MOH and the Coordinator of China Network of Training and Research in Health
Economics and Financing between 1991 and 2005. He received several national advanced
science and technology awards in 1990s. Over the past decade, he was a consultant for the
World Bank, UNICEF, UNDP and AUSAID in China and several Asian countries. In the recent
years, he has been working in pharmacoeconomics education, compiling reference books,
disseminating pharmacoeconomics and outcomes research (PE & OR) knowledge to the
policy-makers, pharmacoeconomic analyses and disease management for several pharmaceutical companies, such as Merck International Foundation, Pfizer, Sanofi-Aventis, GSK,
Janssen. He is interested in drug pricing and reimbursement, national essential drug policy
and systematic reviews on health reform and development.
Dr. Vithaya Kulsomboon received the Bachelor of
Sciences degree in Pharmacy from the Faculty of
Pharmacy, Mahidol University, Bangkok, Thailand, in
1980 and Master Degree in Primary Health Care
Management in 1989 from ASEAN Institute for Health
Development (AIHD), Mahidol University. Dr. Kulsomboon
earned the Doctor of Philosophy degree in Pharmacy
Practice and Administrative Sciences from the University of Maryland at
Baltimore, Baltimore, Maryland, USA, in 2000, where he specialized in pharmaceutical policy and pharmacoeconomics. In 2007, he received the Distinguished
Alumni Award for Distinguished Research from the AIHD. Presently, Dr.
Kulsomboon is an Associate Professor in the Department of Social Pharmacy and
Director of the International Graduate Program in Social and Administrative
Pharmacy, Faculty of Pharmaceutical Sciences, Chulalongkorn University,
Bangkok, Thailand, where he teaches graduate course in pharmacoeconomics
and pharmacoepidemiology.
Dr. Kulsomboon is one of the leaders in Thailand who introduced the concept
of pharmacoeconomics at the national level. In 2007 he was appointed Chief
of the Advisory Committee on Health Economics, National Essential Drug
Committee. The Committee has been instrumental in introducing, for the first
time, the pharmacoeconomic principles and pharmacoeconomic evaluation to
the drug approval and selection process at the national level. The Committee
also introduced national guidelines for pharmacoeconomic evaluation and the
criteria establishing government willingness to pay for pharmaceuticals to the
National Essential Drug Committee.
Dr. Kulsomboon is one of the founding members of the ISPOR Thailand
Chapter, and has served as President of the Chapter since it was established in
2005. He is a member of the 2006-2008 Executive Committee of the ISPOR
Asia Consortium, founded in 2004. He, with other members of the Asia
Consortium, is helping to organize the ISPOR 3rd Asia-Pacific Conference in
South Korea, and along with the Thailand Chapter members, is organizing the
4th Asia-Pacific Conference to be held in Phuket, Thailand.
.
ISPOR Vision Statement by Shanlian Hu MD, MSc
ISPOR Vision Statement by Vithaya Kulsomboon PhD
Under the transition of demographic, epidemiologic and risk factors, disease pattern has
been changed through out the world. The quality and safety of medical services and universal coverage of health care and health insurance become the priorities of government health
reform agenda. The accessibility and affordability of health service are being ranked as the
first priority by the policy-makers. On the one hand, they are dealing with innovation of medicines and health technology which is essential for improving health status of population.
On the other hand, the value of money and its cost-effectiveness should be considered
because of the budget constraint. When searching all themes at ISPOR meetings in North
America, Europe and Asia-Pacific regions, evidence-based health care decision-making has
dominated. The new discipline of PE & OR are the tools to solve these problems. I am
pleased to see that ISPOR plays a great role in this field. Now promoting education and
actively reaching out to decision-makers is one of ISPOR's Vision 2010.
My professional experience is to disseminate PE & OR and health technology assessment knowledge in academic and education environment. Pharmacoeconomics and outcomes research have been placed in the education curriculum as a core or elective course
in the medical colleges and universities. In the policy research study, I have many chances
to work with policy-makers. I do think capacity building and leadership development are so
important that can make big change in the excellence of ISPOR.
It is a great honor to be recommended by the Board of Directors Nominations Committee
as a candidate to serve on the ISPOR Board of Directors. Actually, it is really a challenge for
me. I believe I will help the Society succeed in the following areas: 1) Working closely with
different stakeholders, including academia, policy-makers and pharmaceutical industry in
annual ISPOR activities; 2) Searching opportunities and funding from government and
industry side to conduct capacity building programs to develop pharmacoeconomics and
outcomes research and health technology assessment; and 3) Promoting PE & OR in the
Asia-Pacific region during my term as a Chair of 2008-2010 Asia Consortium Executive
Committee of ISPOR.
The global movement of economic evaluation in pharmaceutical health care
systems has encouraged us to recognize the critical importance of pharmacoeconomics. ISPOR's mission will foster the understanding of the disciplines
the Society represents and will bring the principles of pharmacoeconomics and
rigorous pharmacoeconomic analysis to the forefront in decision-making and
promulgation of health care policy worldwide.
To strengthen the Society as a premier leader in the field of pharmacoeconomics, the Board of Directors must vigorously promote ISPOR to recruit active
members from academia, industry, government and practice in the local,
national and international communities. I hereby propose that the Board adopt
the following five key strategies as the framework of our future endeavors.
These five strategies referred to as ISPOR are: 1) Strong Initiative; 2) Firm
Support; 3) Willing Participation; 4) Equal Opportunity; and 5) Utmost Respect.
ISPOR will identify and promote strong initiatives to make the Society vital
and dynamic. ISPOR will provide firm support to and encourage active participation of its members by sponsoring local chapters, seminars, workshops,
short courses, informal and formal publications as well as effective networking.
ISPOR will make it clear that there is equal opportunity for all of its members to
contribute to the Society and reap important benefits as a member of the
Society. Finally, ISPOR will respect the importance of its individual members,
recognize their personal aspirations as members of the Society, and assist them
to meet their goals regardless of their role, rank or status within their respective
institutions or practices. My devotion to the Society, which has already been
clearly demonstrated, will be further realized as a Member of the Board of
Directors of this august body. Thank you for your kind consideration of my nomination to the ISPOR Board. IC
MAKE YOUR VOICE HEARD. PLEASE VOTE. YOUR BALLOT MUST BE RECEIVED BY APRIL 4, 2008
TO VOTE, GO TO THE ISPOR WEBSITE AT: www.ispor.org
22 January/February 2008 ISPOR CONNECTIONS
ISPOR STUDENT CORNER
Authorship Decisions in Economic Evaluations
Benjamin M Craig PhD, ISPOR CONNECTIONS Editorial Advisory Board member and Assistant Professor, University of Wisconsin,
Department of Family Medicine, Madison, WI, USA
mong the research trades, authorship is a professional currency in addition to the trappings of
intellectual self worth. Ambiguities concerning authorship needlessly damage collaborations, impede publication, and deter career development. While
researchers are required to meticulously describe
their budgets, some fail to equally clarify ownership of
scientific spoils, proving detrimental for both the
authors and the research community.
A
To the best of my knowledge, no guidance has yet
been published in pharmacoeconomics and outcomes research regarding authorship decisions.
Naturally, our field requires the integration of clinical
expertise and research training, most often fulfilled by
interdisciplinary teamwork. Among the articles listed
in 2006 Recently Published Works section of ISPOR
Connections, 88% are multi-author publications, a
proportion which has changed little since 2000. For
our field, the mixing of expertise can be troublesome,
because conventions on authorship vary greatly by
discipline [1].
This paper outlines common guidance on authorship
and establishes three rules for streamlining the decision process. Because these rules are based on firsthand experience in pharmacoeconomics and outcomes research, they should be taken with a grain of
salt. Dilemmas regularly faced by seasoned and junior investigators are described not to provide a definitive statement on authorship; instead, their purpose is
to introduce issues surrounding authorship for reference by junior researchers and for discussion among
more seasoned ones.
Three Rules of Authorship
The person with the authority to determine authorship
is typically the lead author or the principle investigator
of the project. Regardless, these three rules are recommended:
expectations. For example, tasks such as modeling,
literature review, and editing can be assigned in trade
for a particular rank in authorship based on the effort
they require. Effort asked of a senior person is given
more weight, because they typically have greater
opportunity costs (i.e., higher wage rates), but they
are often more productive because of their wealth of
experience and training. A verbal description of other
author contributions may help calibrate evaluations
over rank. Consistent verbal repetition of these contracts helps to set precedent, so that later misunderstandings can be avoided.
How many authors does the paper merit? This number varies greatly by discipline. In economics, articles
generally have up to three authors, but the average
number of authors is increasing [2]. In the 2006
issues of the Journal of Health Economics, 23% of the
articles were sole authored and only 10.5% had over
three authors. On the contrary, epidemiology and clinical papers typically have over three authors. In the
2006 issues of New England Journal of Medicine,
98.1% of the original research articles had over three
authors, and most of those with fewer authors were
written by health economists.
Clinical articles increasingly use group titles (e.g.,
Clinical Trial Writing Group) instead of listing all
authors, which may be in response to Journal requirements and referencing rules. Because the value of
authorship may depend on whether the authors'
names are listed, discussions of a group name may
elicit varying responses. Health technology assessments do not require primary data collection, so the
manuscripts typically have less than four authors.
However, if an article will have more than six authors,
a group name may be substituted for the sixth or more
authors. Otherwise, these remaining coauthors may
be left out of the reference section under the default
convention of “et al.” in future references to the work.
Rule #1 Ask potential authors about their authorship expectations before the first meeting
Before a job begins, employees typically have some
sense of salary. “Everybody needs money. That's why
they call it money!” (Danny DeVito as Mickey
Bergman in "Heist”). In research, authorship is a commodity: it speaks to the intellectual caliber of investigators, and researchers who contribute to a project
will expect to be paid. As with salaries, authorship
negotiations are best handled one-on-one prior to the
start of the research activities.
Although clinical-economic trials are increasingly
prevalent, health technology assessment are usually
based on parameters taken from the literature or secondary data. When a primary researcher provides
parameters or data to another, authorship may be
expected in trade, even if the primary researcher does
not contribute further to the paper. Journals frown on
this bartering, but it is a known practice. Bartering
over data must be clarified before the project is initiated; otherwise, the primary author may rightfully withdraw their data from the paper, essentially gutting the
manuscript.
These negotiations entail a summary of the research
project, emphasizing the contributions and expectations of each author. Every contributor should receive
a list of expected tasks with an initial timeline for completion. Planning far in advance is often difficult, even
impractical, but it begins a discussion of reasonable
Some project staff and educators are paid for their
efforts, and while they contribute to the project, their
efforts may not merit authorship. Such staff includes
interviewers, editors, professional writers, data entry
personnel, and librarians. Difficulties persist when
thesis advisors or supervisors expect authorship
regardless of their contributions, because they contributed toward the funding of the project or supervised the career development of the lead author. While
they should be rewarded for these contributions, in
terms of salary and promotion, their support alone
does not necessitate authorship.
Rule #2 Clearly define the authorship order at the
first meeting
Economic evaluations usually order the authors by
amount of contribution, which is more similar to epidemiology than economics. Because the conventions
of authorship order vary by discipline, open communication seems to be the best strategy [3]. In traditional economics, authors are arranged in alphabetical
order, and arrangement outside of alphabetical order
implies secondary authorship [4]. In epidemiology
and clinical research, however, authorship order is
based on contribution, except for the last author who
may be the senior investigator on a multi-paper project [1]. Frank discussions with administrators concerning the “last authorship” position may prevent
later confusion, particularly when two senior
researchers might assume this privileged post.
Recently, a new pattern is emerging, where senior
coauthors who once coveted the last position request
second authorship. Journals, in the name of space,
have shortened the list of authors in the reference
sections. The 2004 Uniform Requirements of
Manuscripts do not limit the number of authors on any
submitted manuscript; however, when the article is
referenced only the first six authors will be listed followed by “et al.” If the manuscript has seven or more
authors, the last author may be removed automatically by reference software applications, much to the
disappointment and detriment of the senior coauthor.
After introducing the preliminary order and contributions of each author, your collaborators may respond
by asking to do more or less, changing authorship
toward a preferred order. My experience suggests that
such discussions work well as a team building exercise and help legitimize the distribution of tasks. This
open formality may seem awkward, but it saves the
group time and improves the likelihood of a successful project.
Rule #3 Once written, submit the paper to a journal that matches the authorship
At the first meeting, it is prudent to discuss potential
journals for the manuscript submission. Journals
have particular requirements for authorship best
known at the beginning of the project, such as the
maximum number of authors, authorship requirements, and rules on conflicts of interest. Thus, early
journal identification is good practice as it gives purpose to a research project and motivates authors >
January/February 2008 ISPOR CONNECTIONS 23
toward a common goal and audience.
The maximum number of authors varies by journal.
For example, the Lancet editorial board set a maximum of eight authors in 1997, which was heavily criticized at the time (Johnstone 1997). Journals such
as the Journal of Health Economics do not list a formal limit, but the infrequency of more than three
authors might indicate multi-author rejections or, at
least, insistent requests for authorship reductions
(e.g., dropping research assistants).
For most journals, every author must participate in
writing the manuscript and insist that the specific contributions of each contributor be identified. Discussing
these requirements at the very beginning of a project
may simplify the later removal of authors who fail to
contribute in a timely fashion.
Authors are also required to list all potential conflicts
of interest at time of submission [6]. For example, the
New England Journal of Medicine will not publish an
economic evaluation if an author has financial interest
in the study results. Authors may privately inform you
of their potential conflicts, which may either affect the
journal selection or, if caught early, the authorship
decision.
Lastly, if the paper's authorship does not fit the journal, the paper should be submitted to a more appropriate publication. It is unfair to both the journal and
the paper's authors to change authorship for the purposes of submission to a particular publication. For
additional guidance, Harvard Medical School has
posted further authorship advice (http://www.hms.
harvard.edu/integrity/ authorship.html).
Common Dilemmas
All researchers experience dilemmas in authorship.
These cases describe possible responses to three
common dilemmas: Removal of a co-author, change
in author order, and quid pro quo.
Removal of an author
Every seasoned investigator has experienced a collaborative effort where a member of the original team
is unable or unwilling to complete their pre-defined
responsibilities in a timely fashion. Often the investigator remains interested, but has experienced a
change in position or shift in work loads. After missing the predefined deadlines, the first step is to talk
with the collaborator, so that you can identify the reason behind their lack of contribution. Options include
an extension of the deadline, a change in authorship
order, or the removal of the author.
If you have little interest in keeping the author, a cordial dismissal that preserves good feeling and the
possibility of future collaboration is the next goal. As
a result of this discussion, the author may bow out of
the project, in hopes that they may preserve their reputation and collaborate with you sometime in the
future. If this offer is not made, you may outwardly
empathize with the author and ask to decrease their
workload by removing the responsibilities (and
24 January/February 2008 ISPOR CONNECTIONS
authorship) of this project. Most removal cases in my
experience have ended in this fashion.
Some cases are not as simple, and involve an author
with insufficient motivation to complete the work in a
timely fashion, but expects to maintain authorship. As
lead author, you must balance the welfare of the
unproductive authors with those of the more productive authors, including yourself. One strategy is to
strike a deal with the unproductive authors. You might
offer authorship on a future paper, if they relinquish
the current project. Most authors wish to maintain the
appearance of collaboration; therefore offer a schedule of work, forcing the author to choose whether or
not to remain an author through delivering the scheduled effort. If the effort is not realized, the lead author
has legitimate grounds for removal. Such assertive
behavior may render respect of your collaborators.
Regardless, the removal of a disgruntled author is
risky, and is best avoided. In most cases, it leaves a
black on the reputations of all those involved. Some
authors have gone to court to squash manuscripts on
the principle of the issue. Sadly, these manuscripts
rarely merit the exchange of blows. If the situation
worsens to this point, it may be best to drop the manuscript. You can likely significantly change the paper
and begin with a new team instead of proceeding
under malignant circumstances.
Change in Author Order
Less extreme than the removals, changes in authorship order are common. After a project begins,
authors may ask for a change in the authorship order,
because the assigned tasks required more effort than
expected or because they were unable to complete
the assigned tasks. This process of renegotiation
requires the open participation of all authors, because
it may change the ranking. A common tragedy is
when collaborators are surprised by a re-ordering at
time of publication.
Disagreements over authorship order most often
occur because of unexpected work needed to complete the project. For example, a referee may request
for a substudy requiring further data collection or an
additional analysis. To prevent the arguments, care is
needed not to unduly assignment of unpredicted work
to the third or four authors. At the top, author contributions may appear more similar, because their tasks
include dissimilar activities (e.g., data analysis and
site administrator). When the extra work is assign,
best practice suggests that the authorship order is
clarified.
Quid Pro Quo
The demands of academic research have rendered
greater rigor as well as a Pandora's box of unethical
practices. As a graduate student, a well known professor of labor economics once told me that if I did
not want my manuscript refereed by particular colleagues that I should discuss the paper with them and
include them in the acknowledgements. In the authorship decision, questionable tactics include 'guest' and
'ghost' authorship [7].
'Guest' authorship is the inclusion of an individual in the
by-line who does not meet the authorship criteria. In
the end, the journal, editorial board and publisher have
little choice but to trust the corresponding author, who
may be at the mercy of local influences (`pressured'
authorship) or perceive improved publication potential
with the inclusion of a noteworthy 'guest' who may not
even know about their inclusion. The most challenging
cases of 'guest' authorship are when members of a
thesis committee or course instructors require authorship of all graduate student submission under their
direction, which demoralizes the better students and
hurts reputations and student recruitment.
Manuscripts may benefit greatly from the swift pen of
a professional writer. 'Ghost' authorship is more
treacherous, because the manuscript may be written
by another and gifted to the corresponding author,
which is obviously incongruent with journal guideline.
However, it is also well understood that evidence from
particular messengers may be more or less persuasive. These cases also occur in reverse where academic researcher consults on a manuscript under the
condition of anonymity, because he or she does not
wish attribution for the study results.
Reputation and loyalty are also commodities in
research, which may be traded for money, authorship and professional advancement. The authorship
decision includes a balance of multiple interests
across all those involved. Compared to scientific
misconduct (e.g., falsifying results), the trade of
authorship for money, reputation, loyalty and professional advance, instead of contribution, is a lesser
sin, which may explain why quid pro quo seems
increasingly prevalent.
A research project is like starting a new business:
choose your coauthors wisely. Look through their CV.
If they write many papers with persons under their
authority (i.e., junior faculty, graduate students), ask
why. The researcher is either exceptionally generous
with their time or an unscrupulous leech. Contacting
people who have worked with the authorship candidates and checking your authors references before
hiring them is simply good practice in academic
research. IC
References
1. Savitz DA. Invited Commentary: What can we infer from
author order in epidemiology? Am J Epidemiol 1999;149:5.
2. Sutter M, Kocher M. Patterns of co-authorship among economics departments in the USA. App Economics 2004;36:32733.
3. Stokes TD, Hartley JA. Coauthorship, social structure, and
Influence within specialties. Soc Stud Sci 1989;19:1.
4. Engers M, Gans JS, Grant S, King SP. First author conditions.
J Pol Econ 1999;107:4
5. Laband D, Tollison R. Alphabetized coauthorship. App
Econom 2006;38:1649-53.
6. Barnes R and Heaton A. Panel 6: Addressing questions of
bias, credibility, and quality in health economic evaluations.
Value in Health 1999;2:99-102.
7. Bennett DM, Taylor DM. Unethical practices in authorship of
scientific papers. Emergency Med 2003;15:263-70.
< advertisement >
January/February 2008 ISPOR CONNECTIONS 25
ISPOR CORNER
Recently Published Works: Using
Pharmacoeconomics Innovatively
By Stephen Priori, Director, ISPOR Publications
This column includes books, articles, and abstracts recently published by ISPOR members. To ensure
that your published work in pharmacoeconomic or outcomes research is reported here, please keep
your contact information up to date with the Society. Any questions, comments, or submissions
concerning this review can be directed to Stephen Priori at spriori@ispor.org.
Disease Related Research
CARDIOVASCULAR DISEASE
• Colgan R, Johnson JR, Kuskowski M, Gupta K. A
prospective study of risk factors for trimethoprim-sulfamethoxazole resistance in acute uncomplicated cystitis. Antimicrob Agents Chemother 2007 Dec [Epub
ahead of print]
• Hill RA, Boland A, Dickson R, Dundar Y, Haycox A,
McLeod C, Mujica Mota R, Walley T, Bagust A. Drugeluting stents: a systematic review and economic evaluation. Health Technol Assess 2007;11:1-242.
• Nichol MB, Knight TK, Dow T, Wygant G, Borok G,
Hauch O, O'Connor R. Quality of anticoagulation monitoring in nonvalvular atrial fibrillation patients:
Comparison of Anticoagulation Clinic versus usual care
(January). Ann Pharmacother 2007 Dec [Epub ahead
of print]
• Velazquez EJ, Lee KL, O'Connor CM, Oh JK, Bonow
RO, Pohost GM, Feldman AM, Mark DB, Panza JA,
Sopko G, Rouleau JL, Jones RH; STICH Investigators.
The rationale and design of the surgical treatment for
ischemic heart failure (STICH) trial. J Thorac
Cardiovasc Surg 2007;134:1540-7.
• Vats V, Nutescu E, Blackburn JC, Ansell J, Wittkowsky
A, Shapiro N, Schumock GT. Efficacy and safety of
warfarin management in US anticoagulation clinic. J
Thromb Thrombolysis 2007 Nov [Epub ahead of print]
DERMATOLOGY
• Arcury TA, Feldman SR, Schulz MR, Vallejos Q, Verma
A, Fleischer AB Jr, Rapp SR, Davis SF, Preisser JS,
Quandt SA. Diagnosed skin diseases among migrant
farmworkers in North Carolina: prevalence and risk
factors. J Agric Saf Health 2007;13:407-18.
• Carroll CL, Lang W, Snively B, Feldman SR, Callen J,
Jorizzo JL. Development and validation of the dermatomyositis skin severity index. Br J Dermatol 2007 Dec
[Epub ahead of print]
• Housman TS, Hancox JG, Mir MR, Camacho F,
Fleischer AB, Feldman SR, Williford PM. What specialties perform the most common outpatient cosmetic
procedures in the United States? Dermatol Surg 2007
Dec [Epub ahead of print]
Patrick DL. A lifestyle-based weight management program delivered to employees: examination of health
and economic outcomes. J Occup Environ Med
2007;49:1212-7.
• McCollum M, Hansen LB, Ghushchyan V, Sullivan PW.
Inconsistent health perceptions for US women and
men with diabetes. J Womens Health (Larchmt)
2007;16:1421-8.
GASTRO-INTESTINAL
• Brun-Strang C, Dapoigny M, Lafuma A, Wainsten JP,
Fagnani F. Irritable bowel syndrome in France: quality
of life, medical management, and costs: the Encoli
study. Eur J Gastroenterol Hepatol 2007;19:1097-103.
• Lee CC, Lee VW, Chan FK, Ling TK. Levofloxacinresistant helicobacter pylori in Hong Kong.
Chemotherapy 2008;54:50-3. Epub 2007 Dec.
• Marchack BW, Chen LB, Marchack CB, Futatsuki Y.
Fabrication of an all-ceramic abutment crown under an
existing removable partial denture using CAD/CAM
technology. J Prosthet Dent 2007;98:478-82.
• Symms MR, Rawl SM, Grant M, Wendel CS, Coons
SJ, Hickey S, Baldwin CM, Krouse RS. Sexual health
and quality of life among male veterans with intestinal
ostomies. Clin Nurse Spec 2008;22:30-40.
• Wahlqvist P, Brook RA, Campbell SM, Wallander M-A,
Alexander AM, Smeeding JE, Kleinman NL. Objective
measurement of work absence and on-the-job productivity: a case-control study of US employees with and
without gastroesophageal reflux disease. J Occup
Environ Med 2008;50:25-31
INFECTIOUS DISEASE
• Cranny G, Elliott R, Weatherly H, Chambers D, Hawkins
N, Myers L, Sculpher M, Eastwood A. A systematic
review and economic model of switching from nonglycopeptide to glycopeptide antibiotic prophylaxis for
surgery. Health Technol Assess 2008;12:1-168.
• Kaskel P, Tuschy S, Wagner A, Bannert C, Cornely OA,
Glasmacher A, Lipp HP, Ullmann AJ.Economic evaluation of caspofungin vs liposomal amphotericin B for
empirical therapy of suspected systemic fungal infection in the German hospital setting.Ann Hematol; Epub
ahead of print 2007 Oct.
• Cramer JA, Benedict A, Muszbek N, Keskinaslan A,
Khan ZM. The significance of compliance and persistence in the treatment of diabetes, hypertension and
dyslipidaemia: a review. Int J Clin Pract 2007 Nov
[Epub ahead of print]
• Scherer P, Penner IK, Rohr A, Boldt H, Ringel I, WilkeBurger H, Burger-Deinerth E, Isakowitsch K,
Zimmermann M, Zahrnt S, Hauser R, Hilbert K, TielWilck K, Anvari K, Behringer A, Peglau I, Friedrich H,
Plenio A, Benesch G, Ehret R, Nippert I, Finke G,
Schulz I, Bergtholdt B, Breitkopf S, Kaskel P, Reischies
F, Kugler J.The Faces Symbol Test, a newly developed
screening instrument to assess cognitive decline related to multiple sclerosis: first results of the Berlin MultiCentre FST Validation Study. Mult Scler 2007;13:40211. Epub 2007 Jan.
• Hughes MC, Girolami TM, Cheadle AD, Harris JR,
• Simpson KN, Jones WJ, Rajagopalan R, Dietz B. Cost
ENDOCRINOLOGY, METABOLISM & DIABETES
• Bloem CJ, Chang AM. Short-term exercise improves
{beta}-cell function and insulin resistance in older
people with impaired glucose tolerance. J Clin
Endocrinol Metab 2007 Nov [Epub ahead of print]
26 January/February 2008 ISPOR CONNECTIONS
effectiveness of lopinavir/ritonavir tablets compared
with atazanavir plus ritonavir in antiretroviral-experienced patients in the UK, France, Italy and Spain. Clin
Drug Investig 2007;27:807-17.
NEUROLOGY & MENTAL HEALTH
• Sentell T, Shumway M, Snowden L. Access to mental
health treatment by English language proficiency and
race/ethnicity. J Gen Intern Med 2007;22(Suppl.
2):S289-93. Epub 2007 Oct.
• Brown CM, Richards K, Rascati KL, Gavaza P, Corbell
Z, Zachry W, Phillips GA. Effects of a psychotherapeutic drug prior authorization (pa) requirement on
patients and providers: A providers' perspective. Adm
Policy Ment Health 2007 Dec [Epub ahead of print]
• Getsios D, Migliaccio-Walle K, Caro JJ. NICE Costeffectiveness appraisal of cholinesterase inhibitors:
Was the right question posed? Were the best tools
used? Pharmacoeconomics 2007;25:997-1006.
• Haycox A. When NICE says No! Pharmacoeconomics
2007;25:995-6.
• Krystal JH, Gueorguieva R, Cramer J, Collins J,
Rosenheck R; The VA CSP No. 425 Study Team.
Naltrexone is associated with reduced drinking by alcohol dependent patients receiving antidepressants for
mood and anxiety symptoms: Results from VA cooperative study No. 425, "Naltrexone in the Treatment of
Alcoholism" Alcohol Clin Exp Res 2007 Dec [Epub
ahead of print]
• Kunze AM, Gunderson BW, Gleason PP, Heaton AH,
Johnson SV. Utilization, cost trends, and member costshare for self-injectable multiple sclerosis drugs--pharmacy and medical benefit spending from 2004 through
2007. J Manag Care Pharm 2007;13:799-806.
• Liu DT, Lee VY, Chi-Lai L, Lam DS. Stenotrophomonas
maltophilia and Mycobacterium chelonae Coinfection
of the Extraocular Scleral Buckle Explant. Ocul
Immunol Inflamm 2007;15:441-2.
• Morlock RJ, Williams VS, Cappelleri JC, Harness J,
Fehnel SE, Endicott J, Feltner D. Development and
evaluation of the daily assessment of symptoms Anxiety (DAS-A) scale to evaluate onset of symptom
relief in patients with generalized anxiety disorder. J
Psychiatr Res 2007 Nov [Epub ahead of print]
• Newcomer KL, Vickers Douglas KS, Shelerud RA,
Long KH, Crawford B. Is a videotape to change beliefs
and behaviors superior to a standard videotape in
acute low back pain? A randomized controlled trial.
Spine J 2007 Nov [Epub ahead of print]
ONCOLOGY
• Bottomley A, Coens C, Efficace F, Gaafar R, Manegold
C, Burgers S, Vincent M, Legrand C, van Meerbeeck
JP; EORTC-NCIC. Symptoms and patient-reported
well-being: do they predict survival in malignant pleural
mesothelioma? A prognostic factor analysis of EORTC-
NCIC 08983: randomized phase III study of cisplatin
with or without raltitrexed in patients with malignant
pleural mesothelioma. J Clin Oncol 2007;25:5770-6.
• Gondek K, Sagnier PP, Gilchrist K, Woolley JM. Current
status of patient-reported outcomes in industry-sponsored oncology clinical trials and product labels. J Clin
Oncol 2007;25:5087-93.
• He Z, Tang F, Ermakova S, Li M, Zhao Q, Cho YY, Ma
WY, Choi HS, Bode AM, Yang CS, Dong Z. Fyn is a
novel target of (-)-epigallocatechin gallate in the inhibition of JB6 Cl41 cell transformation. Mol Carcinog
2007 Dec [Epub ahead of print]
• Jeruss JS, Mittendorf EA, Tucker SL, Gonzalez-Angulo
AM, Buchholz TA, Sahin AA, Cormier JN, Buzdar AU,
Hortobagyi GN, Hunt KK. Combined use of clinical and
pathologic staging variables to define outcomes for
breast cancer patients treated with neoadjuvant therapy. J Clin Oncol 2007 Dec [Epub ahead of print]
• Li Q, Iuchi T, Jure-Kunkel MN, Chang AE. Adjuvant
effect of anti-4-1BB mAb administration in adoptive T
cell therapy of cancer. Int J Biol Sci 2007;3:455-62.
• Northouse LL, Mood DW, Schafenacker A, Montie JE,
Sandler HM, Forman JD, Hussain M, Pienta KJ, Smith
DC, Kershaw T. Randomized clinical trial of a family
intervention for prostate cancer patients and their
spouses. Cancer 2007;110:2809-18.
• Owusu C, Buist DS, Field TS, Lash TL, Thwin SS,
Geiger AM, Quinn VP, Frost F, Prout M, Ulcickas Yood
M, Wei F, Silliman RA. Predictors of tamoxifen discontinuation among older women with estrogen receptor
positive breast cancer. J Clin Oncol 2007 Dec [Epub
ahead of print]
• Sukel MP, Breekveldt-Postma NS, Erkens JA, van der
Linden PD, Beiderbeck AB, Coebergh JW, Herings RM.
Incidence of cardiovascular events in breast cancer
patients receiving chemotherapy in clinical practice.
Pharmacoepidemiol Drug Saf 2007 [Epub ahead of
print]
• Weycker D, Malin J, Edelsberg J, Glass A, Gokhale M,
Oster G. Cost of neutropenic complications of
chemotherapy. Ann Oncol 2007 Dec [Epub ahead of
print]
PEDIATRICS
• Golicki DT, Golicka D, Groele L, Pankowska E.
Continuous Glucose Monitoring System in children
with type 1 diabetes mellitus: a systematic review and
meta-analysis. Diabetologia 2008;51:233-40.
• Pradel FG, Obeidat NA, Tsoukleris MG. Factors affecting pharmacists' pediatric asthma counseling. J Am
Pharm Assoc 2007;47:737-46.
• Winterstein AG, Gerhard T, Shuster J, Zito J, Johnson
M, Liu H, Saidi A. Utilization of pharmacologic treatment in youths with attention deficit/hyperactivity disorder in medicaid database (January). Ann
Pharmacother 2007 Nov [Epub ahead of print]
magnetic resonance imaging assessment of cognitive
function in childhood-onset systemic lupus erythematosus: A pilot study. Arthritis Rheum 2007;56:
4151-63.
• Brunner H, Das L, Passo M, Koneru S, Mongey AB.
Reply. Arthritis Rheum 2007;59:153-4. [Epub ahead of
print]
• Jonsson B, Kobelt G, Smolen J. Patient access to
rheumatoid arthritis treatments. Eur J Health Econ
2007 Dec [Epub ahead of print]
• Jonsson B, Kobelt G, Smolen J. The burden of
rheumatoid arthritis and access to treatment: uptake of
new therapies. Eur J Health Econ 2007 Dec [Epub
ahead of print]
• Khanna R, Smith MJ. Utilization and costs of medical
services and prescription medications for rheumatoid
arthritis among recipients covered by a state medicaid
program: A retrospective, cross-sectional, descriptive,
database analysis. Clin Ther 2007;29:2456-67.
• Sosroseno W, Sugiatno E, Samsudin AR, Ibrahim MF.
The effect of nitric oxide on the production of cyclic
AMP by a human osteoblast (HOS) cell line stimulated
with hydroxyapatite. Biomed Pharmacother 2007 Oct
[Epub ahead of print]
• Wijbrandts CA, Dijkgraaf MG, Kraan MC, Vinkenoog M,
Smeets TJ, Dinant H, Vos K, Lems WF, Wolbink GJ,
Sijpkens DE, Dijkmans BA, Tak P. The clinical response
to infliximab in rheumatoid arthritis is in part dependent on pre-treatment TNF{alpha} expression in the
synovium. Ann Rheum Dis 2007 Nov [Epub ahead of
print]
• Zethraeus N, Strom O, Borgstrom F, Kanis JA, Jonsson
B. The cost-effectiveness of the treatment of high risk
women with osteoporosis, hypertension and hyperlipidaemia in Sweden. Osteoporos Int 2007 Dec [Epub
ahead of print]
SURGERY
• Salem L, Devlin A, Sullivan SD, Flum DR. Cost-effectiveness analysis of laparoscopic gastric bypass,
adjustable gastric banding, and nonoperative weight
loss interventions. Surg Obes Relat Dis 2007 Dec
[Epub ahead of print]
• Varghese TK Jr, Marshall B, Chang AC, Pickens A, Lau
CL, Orringer MB. Surgical treatment of epiphrenic
diverticula: a 30-year experience. Ann Thorac Surg
2007;84:1801-9; discussion 1801-9.
• Vartak S, Ward MM, Vaughn TE. Do postoperative
complications vary by hospital teaching status? Med
Care 2008;46:25-32.
General Interest
HEALTH SERVICES
• Fargher EA, Eddy C, Newman W, Qasim F, Tricker K,
Elliott RA, Payne K. Patients' and healthcare professionals' views on pharmacogenetic testing and its
future delivery in the NHS. Pharmacogenomics
2007;8:1511-9.
• Joyner PU, Cox WC, White-Harris C, Blalock SJ. The
structured interview and interviewer training in the
admissions process. Am J Pharm Educ 2007;71:83.
• Leblanc JM, Seoane-Vazquez EC, Arbo TC, Dasta JF.
International critical care hospital pharmacist activities.
Intensive Care Med 2007 Nov [Epub ahead of print]
• Lee VH. A Personal tribute to Joseph R. Robinson-An
inspiration for all generations. Pharm Res 2007 Dec
[Epub ahead of print]
• Nuckols TK, Paddock SM, Bower AG, Rothschild JM,
Fairbanks RJ, Carlson B, Panzer RJ, Hilborne LH.
Costs of intravenous adverse drug events in academic
and nonacademic intensive care units. Med Care
2008;46:17-24.
• Parshuram CS, To T, Seto W, Trope A, Koren G,
Laupacis A. Systematic evaluation of errors occurring
during the preparation of intravenous medication.
CMAJ 2008;178:42-8.
METHODOLOGY
• Chi CL, Street WN, Ward MM. Building a hospital referral expert system with a Prediction and OptimizationBased Decision Support System algorithm. J Biomed
Inform 2007 Oct [Epub ahead of print]
• Clauson KA, Polen HH, Marsh WA. Clinical Decision
Support Tools: Performance of personal digital assistant versus online drug information databases.
Pharmacotherapy 2007;27:1651-8.
• Dijkstra BA, Jong CA, Bluschke SM, Krabbe PF, Staak
van der CP. Does naltrexone affect craving in abstinent
opioid-dependent patients? Addiction Biology
2007;12:176-82.
• Krabbe PFM, Salomon JA, Murray CJL. Quantification of
health states with rank-based nonmetric multidimensional scaling. Med Decision Making 2007;27:395-405.
• Patrick DL, Burke LB, Powers JH, Scott JA, Rock EP,
Dawisha S, O'Neill R, Kennedy DL. Patient-reported
outcomes to support medical product labeling claims:
FDA perspective. Value Health 2007;10(Suppl.
2):S125-37.
• Stalmeier PFM, Lamers LM, Busschbach van JJ, Krabbe
PFM. On the assessment of preferences for health and
duration: Maximal Endurable Time and Better than Dead
preferences. Med Care 2007;45:835-41. IC
Pharmacoeco-comic Relief
• Winterstein AG, Gerhard T, Shuster J, Johnson M, Zito
JM, Saidi A. Cardiac safety of central nervous system
stimulants in children and adolescents with attentiondeficit/hyperactivity disorder. Pediatrics
2007;120:e1494-501.
RESPIRATORY DISORDERS
• Quint LE, Cheng J, Schipper M, Chang AC,
Kalemkerian G. Lung lesion doubling times: values and
variability based on method of volume determination.
Clin Radiol 2008;63:41-8. Epub 2007 Oct.
SKELETAL/ARTHRITIS
• Difrancesco MW, Holland SK, Ris MD, Adler CM,
Nelson S, Delbello MP, Altaye M, Brunner HI. Functional
January/February 2008 ISPOR CONNECTIONS 27
ISPOR 3rd
Asia-Pacific
Conference
7-9 September 2008
Grand Hilton Seoul
Seoul, South Korea
Co-organized by:
ISPOR Asia Consortium
Seoul National University
The Korean Association of Health
Technology Assessment (KAHTA)
On-line Abstract Submission Ends: 17 March 2008
Acceptance Notification: 15 June 2008
Early Registration Deadline: 15 July 2008
Evidence-Based Health Care Decision Making In Asia Pacific: The Application of Pharmacoeconomics and Outcomes Research
Conference Program Committee Chair
Bong-Min Yang PhD, Professor of Economics, School of Public Health, Seoul National University, Seoul, South Korea
• • •
Conference Program Committees and Conference Advisory Committee are available at www.ispor.org
Conference Co-sponsors and Supporting Media are available at www.ispor.org
Information of support opportunities and support organizations are available at www.ispor.org
CALL FOR ABSTRACTS
On-line Abstract Submission Ends 17 March 2008 • Acceptance Notification: 15 June 2008
Early Registration Deadline is 15 July 2008
Abstract submissions are invited for Contributed Researches, Workshops and Issue Panels.
Abstract submitted to the ISPOR or 13th Annual International Meeting, or the 10th Annual European Congress,
and abstracts that will be submitted to the 11th Annual European Congress CAN be submitted to this Conference.
To submit abstracts, go to www.ispor.org.
Research Abstracts
Outcomes research on all health care interventions (including drugs, devices, behavioral modification programs, surgery, disease prevention, gene therapy, screening, diagnostic procedures health education) on all diseases or health disorders are considered. Research abstracts (except for conceptual
papers) must be organized by OBJECTIVES, METHODS, RESULTS, CONCLUSION. All accepted research abstracts are published in Value in Health as submitted. Accepted research is presented as a 15 minute podium presentation or poster presentation (with an author discussion hour). Abstracts are evaluated on the quality of the study (or concept) and quality of the abstract presentation.
Research topics: Clinical Outcomes Studies, Cost Studies, Patient-Reported Outcomes Studies, Health Care Use & Policy Studies, Methods/Health Policy
Concepts and Research on Methods.
See the ISPOR website for research subtopics.
Workshop Proposals
Workshop proposals should show novel and innovative experiences in the conduct of outcomes research (including, but not limited to, experiences with
conjoint analysis, large database analysis, modeling, observational studies, record review, surveys, sensitivity analysis, patient registries) or novel and
innovative experiences in the use of outcomes research (clinical, economic, or patient-reported/preference-based outcomes) in health care policy development. Workshop proposals must be organized by DISCUSSION LEADERS, PURPOSE, and DESCRIPTION. Accepted workshops are one hour with no more
than four presenters (from more than one organization). An audience interactive element must be included in the proposal and during the workshop.
Workshop topics: Clinical Outcomes Research, Economic Outcomes Research, Patient-Reported/Preference-based Outcomes Research, Use of Real World Data,
Education/Communications in Outcomes Research, Health Policy Development Using Outcomes Research.
See the ISPOR website for workshop subtopics.
Issue Panel Proposals
Issue Panel proposals should show real debate on new or controversial issues in health economic/pharmacoeconomics and outcomes research or real
debate on the use of outcomes research in health care decision-making. An accepted Issue Panel is one hour with a moderator and 2-3 panelists (preferably from different organizations). Panelists should present distinct views about the topic. Issue Panel proposals must be organized MODERATOR, PANELISTS, ISSUE, OVERVIEW.
Issue Panel topics: Clinical Outcomes Research Issues, Economic Outcomes Research Issues, Patient-Reported Outcomes Research Issues, Health Policy
Development Using Outcomes Research Issues.
See the ISPOR website for issue panel subtopics.
28 January/February 2008 ISPOR CONNECTIONS
ISPOR 3RD ASIA-PACIFIC CONFERENCE
7-9 September 2008 • Seoul, South Korea
SHORT COURSE PROGRAM
Sunday, 7 September 2008
8:00AM-12:00PM MORNING COURSE
Introduction to Quality of Life Assessment
Bruce Crawford MA, MPH, Mapi Values Asia, Japan; Watcharee Leurmarnkul
PhD, Family Health International, Thailand
Course Description: This course is to provide methods that may help to solve
common problems encountered with quality of life / patient-reported outcomes,
including an overview of psychometric validation methods, missing data analysis techniques, and a variety of methods to assess minimally clinically important differences. - designed for individuals with little experience with quality
of life studies.
Introduction to Decision Analysis
Shu-Chuen Li PhD, University of Newcastle, Australia
Course Description: participants will learn to evaluate the appropriateness of
decision analysis in different settings, construct simple decision trees, understand the basic mechanics of tree evaluation and sensitivity analysis, and
acquire skill in the interpretation of a published decision analysis. - Suitable for
those with little experience with decision analysis.
Meta-Analysis and Systematic Literature Review
Nathorn Chaiyakunapruk PharmD, PhD, Naresuan University, Thailand;
Suk-kyung Hahn PhD, Seoul National University, South Korea
Course Description: This course highlights and expounds upon four key areas:
1) impetus for meta-analysis and systematic reviews, 2) basic steps to perform
a quantitative systematic review, 3) statistical methods of combining data, and
4) appraisal and use of meta-analytic reports. - designed for those with little
experience with meta-analysis.
Introduction to Biostatistics in Clinical Trials and
Economic Studies
Isao Kamae MD, PhD, Keio University, Japan; Guk-Hee Suh MD, PhD,
Hangang Sacred Heart Hospital, South Korea
Course Description: Providing an introduction to biostatistics and PE analysis in
clinical trials, the course will include elementary probability theory, basic concepts of statistical inference, sampling theory, hypothesis tests for randomized
controlled trials, etc. - to familiarize new researchers or managers interested in research with current statistical techniques.
Pharmacoeconomics for Health Care Decisionmakers
Kenneth KC Lee PhD, The Chinese University of Hong Kong, China
Course Description: Participants will learn the basic concepts and tools for
conducting PE & OR. Different assessment methods including cost-effectiveness, cost-minimization, cost of illness, cost-utility and cost-benefit analysis will
be discussed. The applications of PE and OR data will be covered and illustrated
by practical examples. - designed to assist decision-making for health care
workers.
Formulary Development
Kenneth Hartigan-Go PhD, The Zuellig Foundation, Philippines; Shawn HsiangYin Chen, PharmD, Taipei Medical University, Taiwan
Course Description: This course will describe the organizational structure of the
P&T committee, the new drug application and review procedures, the preparation of drug monographs and description of the one-in and one-out process with
a discussion of the evidence-based practices with PE consideration put into
practice, the enforcement of drug formulary, etc. - designed for those with little experience in developing a formulary.
1:00PM-5:00PM AFTERNOON COURSE
Budget Impact and Cost Analysis
Gordon G. Liu PhD, Peking University, China
Course Description: This course will describe methods to determine the costof-illness of a health condition. Participants will learn how to estimate the
impact of new healthcare technologies on disease-specific costs from different
decision-maker perspectives. Actuarial methods using straight-line projections
and nonlinear trends will be described. - designed for those with some experience with pharmacoeconomic analysis.
Retrospective Data Analysis
Jeff J. Guo, PhD, University of Cincinnati Medical Center, USA; Eui-Kyung Lee
PhD, Sookmyung University, South Korea
Course Description: Large administrative claims databases provide a unique
opportunity to examine retrospectively the effects of drug use on clinical and
economic outcomes in the “real world” settings. Retrospective data analysis,
such as data from medical claims or the other health databases will be discussed. The advantages and disadvantages of using these datasets to perform
economic analyses and epidemiologic studies will be outlined. - designed for
those with little experience with database analysis.
Modeling: Structure and Design of a Model
Tony Hsiu-Hsi Chen PhD, National Taiwan University, Taiwan; Tae-Jin Lee PhD,
Hallym University, South Korea
Course Description: This course will present pharmacoeconomic modelling
techniques such as Monte Carlo Simulation, Markov modelling, discrete event
models, and other modelling techniques and their appropriate use. The steps
involved with model structure, data inputs, data validation will be discussed.
This intermediate course requires basic understanding of decision analysis.
Pharmacoeconomic Guidelines for Health Care
Decision-makers
Shanlian Hu MD, Fudan University, China; Tony Yen-Huei Tarn PhD, Center for
Drug Evaluation, Taiwan; Alison Tan-Mulligan PhD, GlaxoSmithKline
Pharmaceuticals (China) Investment Co. Ltd, China
Course Description: Participants will learn the main contents and analytic techniques in PE guideline, the differences between PE guidelines around the world
and some country-specific PE guidelines, the political and technical process of
its formulation and implementation. - designed to teach researchers, clinicians, drug manufacturers and policy makers.
Reimbursement System and Methodologies
Madeleine R. Valera MD, Philippine Health Insurance Corporation, Philippines;
Eduardo Banzon MD, World Bank-Manila Office, Philippines; Christian Gericke,
MD, The University of Adelaide, Australia
Course Description: This course is designed to provide the participants with
understanding for the basic principles of reimbursement systems and methodologies. Recent pharmaceutical spending patterns , trends and cost-containment
measures will be discussed taking account of the wider policy context. designed for those with little experience in pharmaceutical pricing and
reimbursement.
Applied Modeling - Use of Decision Analysis
Software TreeAge
Course Description: This course is a hands-on introduction to the use of software in the creation and analysis of cost-effectiveness decision models. The
basics of cost-effectiveness decision-making, building and analyzing a simple
decision tree, Markov modeling and Monte Carlo simulation will be introduced.
All participants must bring a Windows laptop computer with a copy of TreeAge
Pro Suite installed and running and receive a CD-rom at the training. Download
and installation instructions will be provided when you pre-register for the
course.
Sunday, 7 September 2008, 5:30PM-8:30PM Educational Symposia
Sunday, 7 September 2008, 8:30PM-10:30PM Welcome Reception sponsored
by Novartis
January/February 2008 ISPOR CONNECTIONS 29
ISPOR 3RD ASIA-PACIFIC CONFERENCE
7-9 September 2008 • Seoul, South Korea
PRELIMINARY PROGRAM
Monday, 8 September 2008
8:00AM-8:20AM
WELCOME AND INTRODUCTION
Bong-Min Yang PhD, Program Chair, Professor, Seoul National University and President, The Korean
Association of Health Technology Assessment, South Korea
President of Seoul National University (Invited)
8:20AM-8:40AM
WELCOME FROM SOUTH KOREA GOVERNMENT AND GUEST PRESENTATION
initiatives in Taiwan and South Korea will be introduced. Issues on how the exiting HTAs can be
adapted globally will be discussed.
Moderator:
Isao Kamae MD, DrPH, Professor and Chair, Graduate School of Health Management, Keio
University, Japan
Speakers:
Harmonize HTA Globally - Activities and achievements of EUnetHTA & CADTH
8:40AM-9:00AM
WELCOME FROM ISPOR & ISPOR ASIA CONSORTIUM
Finn Boerlum Kristensen MD, PhD, Director & Professor, Danish Centre for Health Technology
Assessment, National Board of Health, Copenhagen, Denmark, Adjunct Professor, University of
Southern Denmark, and Project Leader, European Network for HTA (EUnetHTA); Jill M. Sanders PhD,
President and CEO, Canadian Agency for Drugs and Technologies in Health (CADTH)
9:00AM-9:15AM
BREAK, EXHIBIT & CONTRIBUTED POSTER PRESENTATION VIEWING
HTA Initiatives in Asia - Cases of Taiwan and South Korea
9:15AM-11:15AM
FIRST PLENARY SESSION
Tony Yen-Huei Yarn PhD, Senior Researcher, Health Technology Assessment Task Force, Center for
Drug Evaluation, Taiwan; Eui-Kyung Lee PhD, Professor, Sookmyung Women's University, South
Korea
Minster of Health and Welfare, South Korea (invited) or Chairman of Health Insurance Review Agency,
South Korea (Invited)
EVIDENCE-BASED DECISION MAKING IN ASIA-PACIFIC: HEALTH CARE SYSTEMS OF CHINA MAINLAND, INDIA, SOUTH KOREA, JAPAN, MALAYSIA, PAKISTAN, PHILIPPINES, SINGAPORE, TAIWAN
AND THAILAND
A panel discussion on evidence-based health care decision making adapted in above health care systems, focusing on health technology (drug and medical device & diagnostics) approval policies, pricing policies, reimbursement policies and financial control policies
6:00PM-8:00PM
RECEPTION, EXHIBIT & CONTRIBUTED POSTER PRESENTATION VIEWING
6:00PM-7:00PM
POSTER PRESENTATION AUTHOR HOUR
7:00PM-8:00PM
EDUCATIONAL SYMPOSIUM sponsored by Bristol-Myers Squibb Company
Moderator: Kenneth KC Lee PhD, The Chinese University of Hong Kong, China
VALUE OF ANTIVIRAL TREATMENTS FOR CHRONIC HEPATITIS B
Panelists:
Systems Rapidly Changing: Thailand, South Korea and Taiwan
Tuesday, 9 September 2008
Suwit Wibulpolprasert PhD, Senior Advisor on Disease Control, Ministry of Health, Thailand; Tae-Jin
Lee PhD, Associate Professor of Health Economics, Hallym University, South Korea; Ming-Chin Yang
PhD, Associate Professor, National Taiwan University, Taiwan
8:00AM-9:00AM
EXHIBIT & CONTRIBUTED POSTER PRESENTATION VIEWING
9:00AM-9:15AM
ISPOR SERVICE AWARDS PRESENTATION
Systems Moderately Changing: China mainland, Japan and Singapore
9:15AM-10:45AM THIRD PLENARY SESSION
Gordon G. Liu PhD, Professor and Chair, Peking University, China; Takashi Fukuda PhD, Associate
Professor, The University of Tokyo, Japan; Lee Chien Earn PhD, Senior Director, Healthcare
Performance Group, Ministry of Health, Singapore
DEVELOPING AND IMPLEMENTING PHARMACOECONOMIC GUIDELINES: LESSONS LEARNED FROM
AUSTRALIA AND SOUTH KOREA
Systems Gradually Changing: India, Pakistan, Malaysia and Philippines
Urmila Mukund Thatte PhD, MD, Professor and Head, Topiwala National Medical College, and BYL
Nair Charitable Hospital Mumbai Central, India; Anwarul Hassan Gilani PhD, National Professor of
Pharmacology & Director, Aga Khan University, Pakistan, and WHO Advisor on Drug Policy and
Management; Samsinah Hussain PhD, Associate Professor and Head, University of Malaya, stry of
Health, Malaysia, and Member of the Drug Control Authority (DCA) and Pharmacy Board, Ministry of
Health, Malaysia; Madeleine R. Valera MD, Officer-in-Charge, Health Finance Policy and Services
Sector, and Vice President, Quality Assurance Research and Policy Development Group, Philippine
Health Insurance Corporation, Philippines
Respondents:
Sandeep Duttagupta PhD, Regional Director, Asia & Latin America, Global Outcomes Research,
Pfizer Inc., USA; Sheldon Kong PhD, Executive Director, Global Outcomes Research, Reimbursement,
and Health Technology Assessment, Merck & Company, Inc., USA; Hong Li PhD, MPH, Group
Director, Outcomes Research - Asia Pacific, Department of Global Epidemiology and Outcomes
Research, Bristol-Myers Squibb Company, Singapore; Mingliang Zhang PhD, Director, Health
Economics, Pricing and Market Access, Asia Pacific and Japan, PGSM, Johnson & Johnson, USA
11:15AM-11:30AM BREAK, EXHIBIT & CONTRIBUTED POSTER PRESENTATION VIEWING
11:30AM-12:30PM CONTRIBUTED PODIUM PRESENTATION-SESSION I
Research studies on the following topics may be presented: Arthritis, Cancer, Cardiovascular
Disease, Diabetes, and GI Disorders
This session will give an overview of experience and lessons learned in developing and implementing
pharmacoeconomic guidelines in Australia, and in South Korea, where the pharmacoeconomic guidelines was issued in 2006, and in 2008 the decision is expected being made on whether and how the
guidelines will be officially implemented countrywide.
Moderator:
Bong-Min Yang PhD, Professor of Economics, Seoul National University, South Korea
Speakers:
Rosalie Viney PhD, Associate Professor and Deputy Director, Centre for Health Economics Research
& Evaluation, Australia
Eun-Young Bae PhD, Senior Researcher, Health Insurance Review Agency, South Korea
10:45AM-11:10AM BREAK, EXHIBIT & CONTRIBUTED POSTER PRESENTATION VIEWING
11:00AM-12:00PM CONTRIBUTED WORKSHOP-SESSION II
12:00PM-1:30PM
LUNCH, EXHIBIT & CONTRIBUTED POSTER PRESENTATION VIEWING
12:30PM-1:30PM
EDUCATIONAL SYMPOSIUM Sponsored by Korean Research-based
Pharmaceutical Industry Association
1:30PM-2:30PM
CONTRIBUTED PODIUM PRESENTATION-SESSION II
2:30PM-2:45PM
BREAK, EXHIBIT AND CONTRIBUTED POSTER PRESENTATION VIEWING
2:45PM-3:45PM
SPECIAL SESSION Invited Organizations or Topics:
Health Insurance Review Agency, Seoul, South Korea
12:30PM-2:00PM
LUNCH, EXHIBIT & CONTRIBUTED POSTER PRESENTATION VIEWING
1:00PM-2:00PM
EDUCATIONAL SYMPOSIUM sponsored by IMS Health
ASEAN Harmonization and Improving Drug Access: Where are the Benefits and Risks
2:00PM-3:00PM
CONTRIBUTED WORKSHOP-SESSION I
Pharmacoeconomics and Outcomes Research in, Joan, Indonesia, Mongolia, and Vietnam
3:00PM-3:15PM
BREAK, EXHIBIT & CONTRIBUTED POSTER PRESENTATION VIEWING
Health Technology Assessment Application in Medical Device & Diagnostics
3:15PM-4:15PM
ISSUE PANEL
3:45PM-4:00PM
BREAK, EXHIBIT & CONTRIBUTED POSTER PRESENTATION VIEWING
4:15PM-4:30PM
BREAK, EXHIBIT & CONTRIBUTED POSTER PRESENTATION VIEWING
4:00PM-5:00PM
CONTRIBUTED WORKSHOP-SESSION III
SECOND PLENARY SESSION
5:00PM-5:15PM
BREAK
4:30PM-6:00PM
DEVELOPING EVIDENCE USING HEALTH TECHNOLOGY ASSESSMENT (HTA)
Activities and achievements of the European Network for Health Technology Assessment (EUnetHTA)
and Canadian Agency for Drugs and Technologies in Health (CADTH) will be presented. Asian HTA
30 January/February 2008 ISPOR CONNECTIONS
Developing and Implementing PE Guidelines in China and Thailand
5:15PM-6:00PM
ISPOR CONTRIBUTED RESEARCH AWARDS PRESENTATION
ISPOR 4th ASIA-PACIFIC CONFERENCE ANNOUNCEMENT
CLOSING REMARKS
ISPOR 13th Annual
International Meeting
Sheraton Centre Toronto
Toronto, Ontario, Canada
May 3 - 7, 2008
PROGRAM
FRIDAY, MAY 2, 2008
10.00AM-5:00PM EDUCATIONAL SYMPOSIUM
(Presented by Oxford Outcomes & Axia Research, supported by Amgen Canada)
International Experiences of Centralized Reimbursement Reviews – Identifying Best Practices
This symposium will focus on experiences in countries that routinely use centralized reimbursement reviews for
new medicines and other health technologies. Through presentations and dialogue, recommendations for best
practices in reimbursement decision-making will be identified for practitioners and decision-makers. Panelists
will be thought leaders representing the perspectives of academia, the decision-making community and industry,
and from disciplines including economic appraisal, patient-reported outcomes and epidemiology.
SATURDAY, MAY 3, 2008
8:00AM-5:00PM
PRE-MEETING SHORT COURSES
SUNDAY, MAY 4, 2008
8:00AM-5:00PM
PRE-MEETING SHORT COURSES
5:00PM-7:00PM
EDUCATIONAL SYMPOSIUM
(Co-Sponsored by PhRMA Health Outcomes Committee & ISPOR)
Evolving Evidence Requirements in the Changing Global Landscape of Payer-Decision Making
Ever changing evidence requirement by payers in North America, Europe and Asia Pacific have enormous implications for submissions by the pharmaceutical industry. The symposium will review the latest changes in the
demand for value evidence by these decision-makers, and its implications for health economics and industry.
7:00PM-7:30PM
SYMPOSIUM RECEPTION
6:30PM-8:30PM
STUDENT RESEARCH COMPETITION
8:30PM-10:00PM
STUDENT ICEBREAKER RECEPTION
MONDAY, MAY 5, 2008
7:30AM-8:30AM
ISPOR FORUMS (Open forum with buffet breakfast)
ISPOR Digest of International Databases Forum
The use of the ISPOR Digest of International Databases will be discussed. The forum will provide an opportunity
for researchers to provide input and insight to the effectiveness of the ISPOR Digest.
Patient Registry Taxonomy, Good Research and Operational Issues Forum
This session will focus on the ISPOR Taxonomy of Patient Registries book as well as good research principles,
practical design and operational considerations in developing and using patient registry information.
8:30AM-8:45AM
WELCOME & INTRODUCTION
Adrian Levy PhD and C. Daniel Mullins PhD, Program Committee Co-Chairs
8:45AM-9:00AM
PRESIDENTIAL ADDRESS
Diana Brixner PhD, 2007-2008 ISPOR President and Associate Professor and Chair, Department of
Pharmacotherapy, Executive Director, Pharmacotherapy Outcomes Research Center, University of Utah, Salt Lake
City, UT, USA
9:00AM-10:15AM FIRST PLENARY SESSION: New Evidence on Evidence-Based
Technology Assessment in the USA vs. Canada
The requirement for evidence when performing technology assessments is viewed by some as a logical process for
making decisions and by others as an impossible hurdle and a moving target. Technology assessment occurs quite
differently across public and private payers in Canada and the United States, yet all agree that credible evidence
is needed for technology assessment and adoption. Panelists representing public and private payers will discuss
how they currently assess evidence and conduct technology assessments and how this may change in the future.
Moderator/Speaker: Mark Sculpher PhD, Professor of Health Economics, Centre for Health Economics,
University of York, York, UK
Speakers: Leslie Levin MB, MD, FRCP, FRCPC, Senior Medical, Scientific and Health Technology Advisor, Head,
Medical Advisory Secretariat, Ministry of Health and Long Term Care, Toronto, ON, Canada; Sean Tunis MD, MSc,
Executive Director, Center for Medical Technology Policy, Baltimore, MD, USA; David Yoder PharmD, MBA,
Divisional Vice President Pharmacy, Bravo Health, Baltimore, MD, USA
10:15AM-10:45AM BREAK, EXHIBITS & POSTER PRESENTATIONS VIEWING SESSION I
10:45AM-11:45PM PODIUM PRESENTATIONS - SESSION I
Health Care Decisions Using Outcomes Research Information Case Studies I
CASE 1: AN INTEGRATED PILOT PROJECT UTILIZING AN INTERNAL HTA PROCESS TO SET MEDICAL AND
PAYMENT POLICY IN A U.S. COMMERCIAL HEALTH PLAN
Watkins J1, Choudhury S1, Sturm L2, Bresnahan B3, Sullivan S3, 1Premera Blue Cross, Mountlake Terrace, WA, USA;
2
Formulary Resources, LLC, Issaquah, WA, USA; 3University of Washington, Seattle, WA, USA
CASE 2: DRUG ELUTING STENTS - AN EXAMPLE OF THE TRANSITION FROM EVIDENCE TO POLICY
THROUGH THE ONTARIO COMPREHENSIVE APPROACH TO THE DIFFUSION OF HEALTH TECHNOLOGIES
Levin L1, Goeree R2, 1Ontario Ministry of Health and Long-Term Care, Toronto, ON, Canada; 2McMaster University,
Hamilton, ON, Canada
CASE 3: REVIEWING AND ADAPTING A LOCAL HEALTH TECHNOLOGY ASSESSMENT PROGRAM TO
DEPARTMENTS WITHIN A CANADIAN HEALTH REGION
Austen L, Poulin P, Calgary Health Region, Calgary, AB, Canada
Outcomes Research in Canada
CA1: ECONOMIC ANALYSIS OF IMPLANTABLE CARDIOVERTER DEFIBRILLATORS IN THE PRIMARY PREVENTION OF SUDDEN CARDIAC DEATH - A CANADIAN PERSPECTIVE
Deniz B1, Sadri H2, 1United BioSource Corporation, Concord, MA, USA, 2Medtronic of Canada Ltd, Toronto, ON, Canada
CA2: THE USE OF RESEARCH ABSTRACTS IN FORMULARY DECISION MAKING BY THE ONTARIO CANCER
DRUG APPROVAL COMMITTEE
Weizman A1, Bell C2, 1University of Toronto, Toronto, ON, Canada, 2Department of Medicine, St. Michael’s Hospital,
Toronto, ON, Canada
CA3: A COST-EFFECTIVENESS ANALYSIS OF HEPATITIS C SCREENING AMONG IMMIGRANTS IN CANADA.
Chen W1, Dinner K2, Wong T2, Heathcote J3, Krahn MD3, 1University of Toronto, Toronto, ON, Canada, 2Public Health
Agency of Canada, Ottawa, ON, Canada, 3University Health Network, Toronto, ON, Canada
CA4: THE EARLY CLINICAL AND ECONOMIC BENEFITS OF ATORVASTATIN IN A CANADIAN SETTING
Merikle E1, Ramos É1, Kuznik A2, Botteman MF3, 1Pfizer Canada Inc, Kirkland, QC, Canada, 2Pfizer Inc, New York, NY,
USA, 3PharMerit North America LLC, Bethesda, MD, USA
Drug and Health Services Use Research
DH1: FOLLOW-UP VISITS FOR PATIENTS WITH MAJOR DPRESSIVE DISORDER DURING INITIATION OF
ANTIDEPRESSANT TREATMENT
Chen SY, Hansen R, Maciejewski ML, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA
DH2: IMPACT OF ADHERING TO LIPID MANAGEMENT NATIONAL GUIDELINE RECOMMENDATIONS ON
CARDIOVASCULAR EVENTS AND COSTS IN A MANAGED CARE POPULATION
Balu S1, Simko RJ1, Burge RT1, Quimbo R2, Cziraky MJ2, 1Abbott Laboratories, Abbott Park, IL, USA, 2HealthCore, Inc,
Wilmington, DE, USA
DH3: THE IMPACT OF DRUG VINTAGE ON PATIENT SURVIVAL: A PATIENT-LEVEL APPROACH USING QUEBEC’S PROVINCIAL HEALTH PLAN DATA
Lichtenberg F1, Van Audenrode M2, Grootendorst P3, Latremouille-Viau D2, Lefebvre P2, 1Columbia University, New
York, NY, USA, 2Groupe d’analyse, Ltee, Montreal, QC, Canada, 3University of Toronto, Toronto, ON, Canada
DH4: MARKET DISCONTINUATION OF PHARMACEUTICALS IN THE UNITED STATES: ANALYSIS OF NEW
DRUGS APPROVED FROM 1980 TO 2007
Qureshi ZP, Szeinbach SL, Seoane-Vazquez E, The Ohio State University, Columbus, OH, USA
Mental Health Outcomes Research
MH1: REAL WORLD ASSOCIATION BETWEEN ANTIPSYCHOTIC TREATMENT AND WEIGHT GAIN IN AN
ADOLESCENT POPULATION
Ghate SR1, Said Q2, Rosenblatt LC3, Kim E3, Pikalov A4, Brixner D1, 1The University of Utah College of Pharmacy, Salt
Lake City, UT, USA, 2University of Arkansas for Medical Sciences, Little Rock, AR, USA, 3Bristol-Myers Squibb,
Plainsboro, NJ, USA, 4Otsuka America Pharmaceuticals, Rockville, MD, USA
MH2: ECONOMIC AND CLINICAL CONSEQUENCES ASSOCIATED WITH POTENTIAL DRUG-DRUG INTERACTIONS BETWEEN ANTIPSYCHOTICS AND CONCOMITANT MEDICATIONS IN PATIENTS WITH SCHIZOPHRENIA
Guo JJ1, Kelton CM1, Patel NC1, Wu JH2, Jing Y1, Fan H3, Keck P1, 1University of Cincinnati, Cincinnati, OH, USA,
2
Ortho-McNeil Janssen Scientific Affairs, LLC, Titusville, NJ, USA, 3Covance Inc, Sun Prairie, WI, USA
January/February 2008 ISPOR CONNECTIONS 31
ISPOR 13th Annual International Meeting
Sheraton Centre Toronto, Toronto, Ontario, Canada, May 3 - 7, 2008
PROGRAM continued
MH3: WORK ABSENTEEISM AND BED DAYS IN CHRONIC MEDICAL DISORDER PATIENTS WITH AND WITHOUT DEPRESSION IN THE UNITED STATES, 2004-2005
Sankaranarayanan J, Smith LM, Meza J, Burke WJ, University of Nebraska Medical Center, Omaha, NE, USA
MH4: TREATMENT COST AND COMORBIDITIES ASSOCIATED WITH OBESITY AMONG CHILDREN AND ADOLESCENTS WITH BIPOLAR DISORDER
Guo JJ1, Kelton CM1, Jing Y1, Patel NC2, 1University of Cincinnati, Cincinnati, OH, USA, 2University of Georgia,
Augusta, GA, USA
Research on Medicare Part D and Reimbursement Policies I
MD1: MEDICARE PART D: EARLY EVIDENCE ON PRESCRIPTION DRUG TREATMENT PATTERNS, HOSPITALIZATION OFFSETS AND MEDICARE SPENDING
Zhang Y1, Newhouse JP2, Hanlon J1, Lave J1, Donohue JM1, 1University of Pittsburgh, Pittsburgh, PA, USA, 2Harvard
University, Boston, MA, USA
MD2: THE IMPACT OF MEDICARE PART D ON THE PERCENT GROSS MARGIN EARNED BY TEXAS INDEPENDENT PHARMACIES FOR DUAL ELIGIBLE BENEFICIARY CLAIMS
Winegar AL, Shepherd MD, Lawson K, Richards KM, University of Texas at Austin, Austin, TX, USA
MD3: IMPACT OF MEDICARE PART D DOUGHNUT ON THE USE OF MEDICATIONS BY THERAPEUTIC CLASSES FOR STANDARD BENEFICIARIES
Sun SX, Lee KY, Walgreens Health Services, Deerfield, IL, USA
MD4: IMPACT OF THE MEDICARE MODERNIZATION ACT OF 2003 ON PART B DRUG USE AND SPENDING:
A CASE STUDY OF BIOLOGICALS FOR RHEUMATOID ARTHRITIS
Doshi JA, Li P, Puig A, University of Pennsylvania, Philadelphia, PA, USA
12:00PM-1:00PM
PODIUM PRESENTATIONS - SESSION II
Health Care Decisions Using Outcomes Research Information Case Studies II
CASE 4: THE IMPACT OF THE PROJECT OF ENHANCING COVERAGE RATE FOR PATIENTS WITH CANCER
Lee SM, Nam MH, Yoon SH, Kim BY, Choi MR, Cho HS, Lee KD, Health Insurance Review & Assessment Services,
Seoul, South Korea
CASE 5: THE CENTER FOR DRUG POLICY: PARTNERS HEALTHCARE
Reddy P1, Yeh Y1, Clapp M2, Churchill W3, 1Partners Healthcare, Charlestown, MA, USA; 2Massachusetts General
Hospital, Boston, MA, USA; 3Brigham and Women’s Hospital, Boston, MA, USA
CASE 6: THE USE OF AN EVIDENCE-BASED PRACTICE STRATEGY TO IMPROVE QUALITY IN THE ACUTE
CARE SETTING
Mutnick AH, Wong PK, Hanseman DJ, Mercy Health Partners, Southwest Ohio, Cincinnati, OH, USA
Cancer Outcomes Research
CN1: TRENDS IN TREATMENT AMONG ELDERLY COLORECTAL CANCER PATIENTS IN THE US: EVIDENCE
FROM LINKED SEER-MEDICARE DATA
Lang K1, Lines LM1, Lee DW2, Korn JR1, Vanness DJ3, Earle C4, Menzin J1, 1Boston Health Economics, Inc, Waltham,
MA, USA, 2GE Healthcare, Waukesha, WI, USA, 3University of Wisconsin-Madison, Madison, WI, USA, 4Harvard
University, Boston, MA, USA
CN2: ECONOMIC EVALUATION OF EGFR-GUIDED TREATMENT IN ADVANCED REFRACTORY NON SMALLCELL LUNG CANCER
Carlson JJ1, Garrison L1, Ramsey S2, Veenstra DL1, 1University of Washington, Seattle, WA, USA, 2Fred Hutchinson
Cancer Research Center, Seattle, WA, USA
CN3: COMPARISON OF THE COST-EFFECTIVENESS OF SIX CYCLES OF TAXOTERE, DOXORUBICIN,
CYCLOPHOSPHAMIDE (TAC) VERSUS SIX CYCLES OF FLUOROURACIL, DOXORUBICIN, CYCLOPHOSPHAMIDE
(FAC) IN THE ADJUVANT SETTING OF NODE POSITIVE BREAST CANCER WITH PRIMARY AND SECONDARY
G-CSF PROPHYLAXIS
Mittmann N1, Koo M1, Alloul K2, Trudeau M3, 1Sunnybrook Health Sciences Centre, Toronto, ON, Canada, 2sanofiaventis Canada, Montreal, QC, Canada, 3Odette Cancer Centre, Sunnybrook Health Sciences Centre, Toronto, ON,
Canada
CN4: COSTS ASSOCIATED WITH NEUTROPENIA IN ELDERLY PATIENTS TREATED FIRST-LINE FOR
ADVANCED NON-SMALL CELL LUNG CANCER (NSCLC)
Stokes ME1, Muehlenbein CE2, Marciniak MD2, Faries D2, Motabar S3, Buesching DP2, Gillespie TW4, Lipscomb J4,
Knopf KB5, 1United BioSource Corporation, Dorval, QC, Canada, 2Eli Lilly and Company, Indianapolis, IN, USA,
3
United BioSource, Bethesda, MD, USA, 4Emory University and Veterans Affairs Medical Center, Atlanta, GA, USA,
5
California Pacific Medical Center, San Francsico, CA, USA
Health Policy Research
HP1: A COMPARISON OF THREE TECHNOLOGY APPRAISAL SYSTEMS; NICE, SMC AND CADTH
Karia R1, Gani R2, Perard R1, Cann K2, 1Heron Evidence Development Ltd, Letchworth Garden City, Hertfordshire, UK,
2
Heron Evidence Development Ltd, Hertfordshire, UK
HP2: NHS REIMBURSEMENT OF NEW CANCER DRUGS: IS NICE GETTING NASTIER?
Mason AR1, Drummond M2, 1University of York, York, N. Yorkshire, UK, 2University of York, York, Heslington, UK
HP3: PRIORITY SETTING FOR NEW TECHNOLOGIES: POSSIBLE DETERMINANTS AMONG THE WORKING
POPULATION
Derycke H, Annemans L, Ghent University, Gent, Belgium
HP4: 25 YEARS OF THE ORPHAN DRUG ACT: ANALYSIS OF THE NEW ORPHAN DRUGS APPROVED
BETWEEN 1983 AND 2007
Rodriguez-Monguio R1, Visaria J2, Seoane-Vazquez E2, 1University of Massachusetts, Amherst, MA, USA, 2The Ohio
State University, Columbus, OH, USA
Research on Medicare Part D and Reimbursement Policies II
MD5: HEALTH CARE UTILIZATION BY MEDICARE ADVANTAGE BENEFICIARIES IN THE ERA OF THE
MEDICARE PART D DRUG BENEFIT COVERAGE GAP
Delate T1, Raebel MA2, Ellis JL2, Bayliss EA2, 1Kaiser Permanente Colorado, Aurora, CO, USA, 2Kaiser Permanente
Colorado, Denver, CO, USA
MD6: INFLUENCE OF MEDICARE CLAIM-PAYING AGENTS’ REIMBURSEMENT POLICY ON G-CSF CHOICE
DURING FIRST CYCLE OF CHEMOTHERAPY FOR NON-HODGKIN’S LYMPHOMA PATIENTS
Pan X1, Brooks JM2, Wright KB1, Voelker MD1, 1University of Iowa, Iowa City, IA, USA, 2USRDS Economic Special
Study Center, The University of Iowa, Iowa City, IA, USA
MD7: DIFFERENTIAL TAKE-UP OF THE MEDICARE PART D PRESCRIPTION DRUG BENEFIT
Rabbani A1, Yin W1, Zhang JX1, Sun SX2, Alexander GC1, 1University of Chicago, Chicago, IL, USA, 2Walgreens Health
Services, Deerfield, IL, USA
32 January/February 2008 ISPOR CONNECTIONS
MD8: THE IMPACT OF MEDICARE NEW DRUG BENEFIT (PART D) ON THE UTILIZATION OF PSYCHOTROPIC
MEDICATIONS AND CONSEQUENT OUT OF POCKET EXPENDITURE FOR ELDERLY
Chen H1, Nwangwu A1, Aparasu R1, Sun SX2, Lee KY2, 1University of Houston, Houston, TX, USA, 2Walgreens Health
Services, Deerfield, IL, USA
Research on Patient Reported Outcomes Methods
PM1: RASCH RATING SCALE ANALYSIS OF THE EQ-5D USING THE 2003 MEDICAL EXPENDITURE PANEL
SURVEY (MEPS)
Gu NY, Doctor JN, University of Southern California, Los Angeles, CA, USA
PM2: WHAT PATIENTS SAY VS. WHAT PATIENTS MEAN: QUALITATIVE RESEARCH IN PRO DEVELOPMENT
Lasch KE1, Marquis P1, Vigneux M2, Abetz L3, Arnould B2, Bayliss MS1, Crawford B1, Rosa K1, Scott J1, 1Mapi Values,
Boston, MA, USA, 2Mapi Values, Lyon, France, 3Mapi Values Limited, Bollington, UK
PM3: THE VALIDITY AND RELIABILITY OF A PARENT-CHILD DYAD APPROACH TO UTILITY AND QUALITYOF-LIFE ASSESSMENT IN CHILDREN
Ungar WJ1, Boydell K1, Dell S1, Feldman BM1, Marshall DA2, Willan AR1, Wright J1, 1The Hospital for Sick Children,
Toronto, ON, Canada, 2McMaster University, Hamilton, ON, Canada
PM4: EVALUATION OF A THEORY OF GLOBAL HEALTH PREFERENCE FORMATION
Shaw JW1, Pickard AS1, Lin HW1, Cella D2, Trask PC3, 1University of Illinois at Chicago, Chicago, IL, USA, 2Evanston
Northwestern Healthcare, Evanston, IL, USA, 3Pfizer, Inc, New London, CT, USA
1:00PM-2:45PM
LUNCH, EXHIBITS & POSTER PRESENTATIONS VIEWING -
SESSION I
1:30PM-2:30PM
EDUCATIONAL SYMPOSIUM (Sponsored by IMS Health)
Why Does Medication Noncompliance Persist?
Noncompliance with prescribed medicines contributes to over 125,000 deaths each year, costing the health care
system more than $175 billion annually. Yet, despite the nearly 40,000 articles published on the subject, noncompliance still persists. In this session, IMS will feature a dynamic and interactive discussion that offers new
perspectives on the problem of noncompliance, the breadth and quality of current compliance literature, and
insights into the design and evaluation of evidence-based compliance programs.
2:45PM-3:45PM
ISSUE PANELS - SESSION I
CLINICAL OUTCOMES RESEARCH ISSUES
IP1: COMPARATIVE EFFECTIVENESS RESEARCH: BREAKING THE METHODS MOLD
Moderator: Sean Tunis MD, MSc, Executive Director, Center for Medical Technology Policy, Baltimore, MD,
USA.Panelist(s): Bryan Luce PhD, MBA, Senior Vice President, Science Policy, United BioSource Corporation,
Bethesda, MD, USA; Scott Berry PhD, President, Berry Consultants, College Station, TX, USA; Michael Krams MD,
Asst. Vice President, Wyeth Research, Collegeville, PA, USA.
HEALTH CARE POLICY DEVELOPMENT USING OUTCOMES RESEARCH ISSUES
IP2: IS NICE ALL THAT NASTY? COMPARISONS OF ACCESS TO CANCER THERAPY IN UK AND US HEALTH
CARE
Moderator: Lee N Newcomer MD, Senior Vice President, Oncology, UnitedHealthcare, Edina, MN, USA.
Panelist(s): Mike F Drummond PhD, Professor of Health Economics, University of York, Centre for Health
Economics, York, Heslington, UK; Scott Ramsey MD, PhD, Associate Member, Fred Hutchinson Cancer Research
Center, Seattle, WA, USA; Dennis W Raisch PhD, Associate Center Director, Department of Veterans Affairs
Cooperative Studies Program, Clinical Research Pharmacy Coordinating Center, Albuquerque, NM, USA.
IP3: ESTABLISHING KEY PRINCIPLES FOR HEALTH TECHNOLOGY ASSESSMENT
Moderator: Sean D Sullivan PhD, RPh, Professor of Pharmacy and Public Health and Director, University of
Washington, Pharmaceutical Outcomes Research and Policy Program, Seattle, WA, USA.
Panelist(s): Naomi Aronson PhD, Executive Director, Blue Cross-Blue Shield Technology Evaluation Center,
Chicago, IL, USA; Peter J. Neumann ScD, Professor, Tufts-New England Medical Center, Institute for Clinical
Research and Health Policy Studies, Boston, MA, USA; Jill M. Sanders PhD, President and CEO, Canadian Agency
for Drugs and Technologies in Health, Ottawa, ON, Canada.
IP4: WHAT DID THE MEDICARE REPLACEMENT DRUG DEMONSTRATION TEACH US ABOUT THE ROLE OF
COST-EFFECTIVENESS ANALYSES IN PUBLIC POLICY?
Moderator: Penny E Mohr MA, Director, Division of Research on Health Plans and Drugs, Centers for Medicare and
Medicaid Services, Office of Research, Development and Information, Baltimore, MD, USA.
Panelist(s): William Lawrence MD, MS, Research Fellow, Agency for Healthcare Research and Quality, Center for
Outcomes and Effectiveness Research, Rockville, MD, USA; Allan Wailoo BSc, MA, PhD, Senior Lecturer in Health
Economics, The University of Sheffield, Health Economics and Decision Science, School of Health and Related
Research, Sheffield, UK; Martin Zagari MD, Global Health Economics Head, Amgen, Thousand Oaks, CA, USA.
PATIENT-REPORTED OUTCOMES RESEARCH ISSUES
IP5: PATIENT-REPORTED OUTCOMES, HEALTH-STATE UTILITIES, OR STATED-PREFERENCES? SIMILARITIES,
DIFFERENCES AND ROLES IN DEMONSTRATING PRODUCT VALUE
Moderator: A. Brett Hauber PhD, Senior Economist and Head, RTI Health Solutions, Health Preference Assessment,
Research Triangle Park, NC, USA.
Panelist(s): Paul Kind PhD, Professor of Economics, University of York, Centre for Health Economics, York,
Heslington, UK; William Furlong MSc, Research Coordinator, McMaster University and Health Utilities Inc,
Hamilton, ON, Canada; F. Reed Johnson PhD, Senior Fellow and Principal Economist, RTI International, Research
Triangle Park, NC, USA.
3:45PM-4:00PM
BREAK, EXHIBITS & POSTER PRESENTATIONS VIEWING -
SESSION I
4:00PM-5:00PM
PODIUM PRESENTATIONS - SESSION III
Research On Adherence and Compliance I
AC1: THE ASSOCIATION BETWEEN IMPROVEMENTS IN DRUG ADHERENCE AND SHORT-TERM SERVICE
UTILIZATION AND COSTS IN A MEDICAID POPULATION
Thiebaud P, Pfizer Health Solutions, New York, NY, USA
AC2: PATTERNS OF DIABETES MEDICATION AND TEST ADHERENCE IN A MEDICAID DISEASE MANAGEMENT PROGRAM
Demand M, Gutierrez PR, Thiebaud P, Pfizer Health Solutions, New York, NY, USA
AC3: DEPRESSIVE SYMPTOMATOLOGY, MEDICATION PERSISTENCE, AND ASSOCIATED HEALTH CARE
COSTS IN OLDER ADULTS WITH INSOMNIA
Kulkarni AS1, Patel I2, Anderson RT3, Balkrishnan R1, 1The Ohio State University College of Pharmacy, Columbus,
OH, USA, 2The Ohio State University, Columbus, OH, USA, 3Wake Forest University School of Medicine, Winston
Salem, NC, USA
ISPOR 13th Annual International Meeting
Sheraton Centre Toronto, Toronto, Ontario, Canada, May 3 - 7, 2008
PROGRAM continued
AC4: THE COST OF NON-ADHERENCE TO ASTHMA TREATMENT GUIDELINES AMONG A LOW-INCOME
COHORT
Said Q1, Waitzman NJ2, 1University of Arkansas for Medical Sciences, Little Rock, AR, USA, 2University of Utah, Salt
Lake City, UT, USA
Cardiovascular Disease Outcomes Research
CV1: EFFECTIVENESS OF COMBINED BETA-BLOCKER AND ACEI OR ARB THERAPY IN CHRONIC HEART
FAILURE
Sharma M1, Deswal A2, Henderson L3, Desai R1, Chitnis A1, Petersen N4, Ashton C5, Johnson M4, 1University of
Houston, Houston, TX, USA, 2Baylor College of Medicine; Michael E. DeBakey Veterans Affairs Medical Center,
Houston, TX, USA, 3University of Texas M.D.Anderson Cancer Center, Houston, TX, USA, 4Michael E. DeBakey
Veterans Affairs Medical Center, Houston, TX, USA, 5University of Alabama, Birmingham, AL, USA
CV2: THE COST-EFFECTIVENESS OF CANDESARTAN IN THE TREATMENT OF CHRONIC HEART FAILURE (HF)
- AN ASSESSMENT OF THE LOW LEFT VENTRICULAR EJECTION FRACTION (LOW-LVEF) TRIALS IN THE
CANDESARTAN-IN-HEART-FAILURE-ASSESSMENT-OF-REDUCTION-IN-MORTALITY-AND-MORBIDITY
(CHARM) TRIAL PROGRAMME
Levin LÅ1, Jørgensen E2, Eriksson B3, Swedberg K4, Paulsson T3, 1Linköping University, Linköping, Sweden,
2
AstraZeneca, Oslo, Norway, 3AstraZeneca, Södertälje, Sweden, 4Sahlgrenska Academy, Göteborg University,
Gothenburg, Sweden
CV3: CLINICAL AND ECONOMIC OUTCOMES ASSOCIATED WITH BLEEDING DURING CORONARY ARTERY
BYPASS GRAFT SURGERY AMONG ELDERLY AMERICANS
Ganz ML1, Joshi AV2, Wang Q3, Wilke CT4, Lee WC3, Pashos CL1, 1Abt Associates, Inc, Lexington, MA, USA, 2Novo
Nordisk Inc, Princeton, NJ, USA, 3Abt Associates, Inc, Bethesda, MD, USA, 4University of Illinois at Chicago,
Chicago, IL, USA
CV4: CAN TWO A’S RESULT IN A FAILURE?: EFFECT OF ASPIRIN ON THE RISK OF HEART FAILURE HOSPITALIZATIONS IN CHF PATIENTS ON ACE INHIBITORS.
Shah DH, Parikh NM, Kamble PS, Chen H, Johnson M, University of Houston, Houston, TX, USA
Diabetes Outcomes Research
DB1: REAL-WORLD SIX MONTH OUTCOMES OF PATIENTS INITIATING EXENATIDE IN A PRIMARY CARE
ELECTRONIC MEDICAL RECORD DATABASE
Brixner D1, McAdam-Marx C1, Ye X1, Boye KS2, Schroeder B3, Fabunmi R3, 1The University of Utah College of
Pharmacy, Salt Lake City, UT, USA, 2Eli Lilly and Company, Indianapolis, IN, USA, 3Amylin Pharmaceuticals, Inc, San
Diego, CA, USA
DB2: COST-EFFECTIVENESS ANALYSIS OF PREGABALIN FOR THE MANAGEMENT OF NEUROPATHIC PAIN
ASSOCIATED WITH DIABETIC PERIPHERAL NEUROPATHY IN MEXICO
Arreola-Ornelas H1, Dorantes-Aguilar J1, García-Mollinedo MDL2, Rosado-Buzzo AA2, Mould-Quevedo J3, DavilaLoaiza G3, 1Fundación Mexicana para la Salud, Funsalud, Mexico City, Mexico, 2Links & Links S.A. de C. V, Mexico
City, Mexico, 3Pfizer Mexico, Mexico City, Mexico
DB3: REAL-WORLD ANALYSIS OF PERCENT OF PATIENTS WITH TYPE 2 DIABETES ACHIEVING GLYCEMIC
GOAL WITH INSULIN GLARGINE
Misurski D1, Schroeder B2, Wade R3, Quimbo R3, Nielsen L2, Fabunmi R2, Wintle M2, 1Eli Lilly and Company,
Indianapolis, IN, USA, 2Amylin Pharmaceuticals, Inc, San Diego, CA, USA, 3HealthCore, Inc, Wilmington, DE, USA
DB4: RETROSPECTIVE STUDY OF TYPE 2 DIABETES MELLITUS (T2DM) PATIENTS NOT OPTIMALLY CONTROLLED BY METFORMIN MONOTHERAPY
He J, Neslusan C, Johnson & Johnson Pharmaceutical Services L.L.C, Raritan, NJ, USA
Drug Use Research I
DU1: DEMOGRAPHIC RISK FACTORS FOR STROKE RELATED AMBULATORY CARE UTILIZATION: ANALYSIS
OF UNITED STATES NATIONAL DATA 2000-2005
Karve S, Levine D, Balkrishnan R, The Ohio State University, Columbus, OH, USA
DU2: DOES COMMUNITY-BASED HEALTH INSURANCE IMPROVE ACCESS TO DRUGS AND HEALTH CARE
FOR THE POOREST IN AFRICA?
Souares A1, Savadogo G2, Gnawali DP1, Sauerborn R1, 1Heidelberg University, Heidelberg, BadenWürttemberg,
Germany, 2Centre de Recherche en Santé de Nouna, Nouna, Kossi, Burkina Faso
DU3: CALIFORNIA WILDFIRES AND THEIR IMPACT ON MEDICATION ACQUISITION
Hutchins DS1, Liberman JN2, Tong W1, Berger JE3, 1CVS Caremark, Scottsdale, AZ, USA, 2CVS Caremark Corporation,
Hunt Valley, MD, USA, 3CVS|Caremark Inc, Northbrook, IL, USA
DU4: PRESCRIPTION DRUG UTILIZATION AMONG A NATIONALLY REPRESENTATIVE SAMPLE OF MEDICARE
BENEFICIARIES WITH HEART FAILURE
Bain KT1, Richardson D2, Liao D2, Diamond J3, Novielli KD2, Goldfarb NI3, 1excelleRx, Inc, Philadelphia, PA, USA,
2
Jefferson Medical College, Philadelphia, PA, USA, 3Thomas Jefferson University, Philadelphia, PA, USA
Research on Outcomes Research Methods
OM1: VALIDATING A SURVEY INSTRUMENT USING NONPARAMETRIC ITEM RESPONSE THEORY – APPLICATION OF KERNEL REGRESSION
Lin HW1, Pickard AS1, Karabatsos G2, Mahady GB1, Crawford SY1, Popovich NG1, 1College of Pharmacy, University of
Illinois at Chicago, Chicago, IL, USA, 2College of Education, University of Illinois at Chicago, Chicago, IL, USA
OM2: USING VALUE OF INFORMATION METHODOLOGY TO DETERMINE THE SAMPLE SIZE FOR A
RANDOMIZED CLINICAL TRIAL FROM AN INDUSTRY PERSPECTIVE
Willan AR, SickKids Research Insitute, Toronto, ON, Canada
OM3: WAS IT NICE FOR YOU? ESTIMATING SUBGROUP QUALITY OF LIFE TARIFFS FROM CONJOINT
ANALYSES: RESULTS FROM A BEST-WORST SCALING STUDY
Flynn TN1, Louviere JJ2, Peters TJ1, Coast J3, 1University of Bristol, Bristol, UK, 2University of Technology, Sydney,
NSW, Australia, 3University of Birmingham, Birmingham, UK
OM4: LONG-TERM COST-EFFECTIVENESS OF A DIABETES RISK SCORE IN CLINICAL PRACTICE
Sullivan SD1, Garrison LP1, Rinde H2, Kolberg J3, Moler E3, Urdea M4, 1University of Washington, Seattle, WA, USA,
2
BioBridge Strategies, Binningen, Switzerland, 3Tethys Bioscience Inc, Emeryville, CA, USA, 4Tethys Bioscience, Inc,
Emeryville, CA, USA
5:15PM-6:15PM
PODIUM PRESENTATIONS - SESSION IV
Research On Adherence and Compliance II
AC5: ORAL ANTIDIABETIC MEDICATION ADHERENCE AND HEALTH CARE COSTS AND UTILIZATION AMONG
MEDICAID-ENROLLED TYPE 2 DIABETES PATIENTS NEWLY STARTING MONOTHERAPY
Shenolikar R1, Balkrishnan R2, 1Glaxo SmithKline, Columbus, OH, USA, 2The Ohio State University, Columbus, OH, USA
AC6: ASSOCIATION OF NONCOMPLIANCE WITH DIABETES CARE GUIDELINES AND DISEASE BURDEN IN A
CALIFORNIA MEDICAID TYPE 2 DIABETES MELLITUS POPULATION
Nichol MB1, Knight TK1, Wu J1, Priest JL2, Cantrell CR2, 1University of Southern California, Los Angeles, CA, USA,
2
GlaxoSmithKline, Research Triangle Park, NC, USA
AC7: COMPARING ADHERENCE TO FIXED DOSE COMBINATION VERSUS MULTI-PILL COMBINATION THERAPIES AMONG PATIENTS WITH DYSLIPIDEMIA IN A MANAGED CARE POPULATION
Balu S1, Simko RJ1, Burge RT1, Quimbo R2, Cziraky MJ2, 1Abbott Laboratories, Abbott Park, IL, USA, 2HealthCore, Inc,
Wilmington, DE, USA
AC8: ASSOCIATION OF MEASURES OF MEDICATION ADHERENCE AND SEVERE RELAPSES WITH MULTIPLE
SCLEROSIS DISEASE-MODIFYING THERAPY
Dickson M1, Kozma C2, Okuda DT3, Fincher C4, Meletiche D4, 1University of South Carolina, College of Pharmacy,
Columbia, SC, USA, 2University of South Carolina, West Columbia, SC, USA, 3University of California, San Francisco,
San Francisco, CA, USA, 4EMD Serono, Inc, Rockland, MA, USA
Drug Use Research II
DU5: IMPACT OF FORMULARY RESTRICTIONS ON ADHERENCE TO SECOND GENERATION ANTIPSYCHOTICS
Zeng F1, Leslie RS1, Patel BV1, Chen CC2, Kim E2, Knoth R2, Tran QV3, 1MedImpact Healthcare Systems, Inc, San Diego,
CA, USA, 2Bristol-Myers Squibb, Plainsboro, NJ, USA, 3Otsuka America Pharmaceutical Inc, Rockville, MD, USA
DU6: ASSESSMENT OF DRUG UTILIZATION PATTERNS AND COSTS FOR ERYTHROPOIETIC STIMULATING
AGENTS IN ELDERLY PATIENTS WITH CHRONIC KIDNEY DISEASE
Lafeuille MH1, Lefebvre P1, Bookhart B2, Laliberte F1, Bailey R2, Corral M2, Piech CT2, 1Groupe d’analyse, Ltee,
Montreal, QC, Canada, 2Ortho Biotech Clinical Affairs, LLC, Bridgewater, NJ, USA
DU7: NATIONAL ESTIMATES AND DETERMINANTS OF DEPRESSION AND ANTIDEPRESSANT TREATMENT IN
CANCER PATIENTS IN THE UNITED STATES, 2004-2005
Sankaranarayanan J, Smith LM, Meza J, Burke WJ, University of Nebraska Medical Center, Omaha, NE, USA
DU8: THE EFFECT OF THREE-TIER FORMULARY ADOPTION FOR ALPHA-BLOCKERS ON DRUG UTILIZATION
IN THE DEPARTMENT OF DEFENSE
Devine JW, Conrad RC, Tiller KW, Department of Defense Pharmacoeconomic Center, Fort Sam Houston, TX, USA
Infectious Disease Outcomes Research
IN1: C. ALBICANS AND C. GLABRATA BLOODSTREAM INFECTIONS IN ADULTS: OUTCOMES AND ASSOCIATED COSTS
Grussemeyer CA1, Friedman JY1, Spalding JR2, Benjamin DK3, Moran C3, Reed SD1, 1Duke Clinical Research Institute,
Durham, NC, USA, 2Astellas Pharma US, Deerfield, IL, USA, 3Duke University Medical Center, Durham, NC, USA
IN2: UPPER RESPIRATORY ILLNESS AND EMPLOYEE PRODUCTIVITY – RESULTS FROM THE CHILD AND
HOUSEHOLD INFLUENZA-ILLNESS AND EMPLOYEE FUNCTION (CHIEF)
Palmer L1, Nichol KL2, Johnston S1, Mahadevia PJ3, Rousculp MD3, 1Thomson Healthcare, Inc, Washington, DC, USA,
2
Veterans Affairs Medical Center, Minneapolis, MN, USA, 3MedImmune, Inc, Gaithersburg, MD, USA
IN3: A MICROSIMULATION OF THE COST-EFFECTIVENESS OF MARAVIROC FOR ANTIRETROVIRAL TREATMENT-EXPERIENCED HIV-INFECTED INDIVIDUALS
Chancellor JV1, Kuehne FC2, Mollon P3, Louie M4, Powderly WG5, 1i3 Innovus, Uxbridge, Middlesex, UK,
2
PharmacoConsult, Wanzleben-Buch, Germany, 3Pfizer Limited, Sandwich, Kent, UK, 4Pfizer Inc, New York, NY, USA,
5University College Dublin, Dublin, Ireland
IN4: COST-EFFECTIVENESS OF DORIPENEM IN THE TREATMENT OF NOSOCOMIAL PNEUMONIA
McGarry LJ1, Merchant S2, Pawar V1, Delong K1, Thompson D1, Akhras K2, Ingham M2, Weinstein MC3, 1Innovus
Research, Inc, Medford, MA, USA, 2Johnson & Johnson Pharmaceutical Services, L.L.C, Raritan, NJ, USA, 3Harvard
University, Boston, MA, USA
Patient-Reported Outcomes Research
PR1: VARIABILITY OF HEALTH UTILITIES INDEX MARK 3 (HUI3) MEASUREMENTS DURING TREATMENT FOR
ACUTE LYMPHOBLASTIC LEUKEMIA IN CHILDHOOD
Rae CS1, Furlong W2, De Pauw S1, Barr RD1, Gelber RD3, Sallan S3, 1McMaster University, Hamilton, ON, Canada,
2
McMaster University and Health Utilities Inc, Hamilton, ON, Canada, 3Harvard University, Boston, MA, USA
PR2: VALIDATION OF THE PATIENT HEALTH QUESTIONNAIRE IN BRFSS - APPLICATION OF CROSSVALIDATION METHOD
Yeh Y, Mapi Values, Boston, MA, USA
PR3: IMPACT OF UNCONTROLLED PEDIATRIC ASTHMA ON HEALTH-RELATED QUALITY OF LIFE (HRQOL)
Dean BB1, Calimlim B1, Aguilar D1, Sacco P2, Maykut R2, Tinkelman D3, 1Cerner LifeSciences, Beverly Hills, CA, USA,
2
Novartis Pharmaceuticals Corporation, East Hanover, NJ, USA, 3National Jewish Medical and Research Center,
Denver, CO, USA
PR4: EVALUATION OF IMPACT OF ORAL TOPOTECAN ON HEALTH-RELATED QUALITY OF LIFE IN RELAPSED
SMALL CELL LUNG CANCER
Duh MS1, Pickard AS2, Chen L1, Antras L1, Cella D3, Neary MP4, O’Brien ME5, 1Analysis Group, Inc, Boston, MA, USA,
2
College of Pharmacy, University of Illinois at Chicago, Chicago, IL, USA, 3Evanston Northwestern Healthcare,
Evanston, IL, USA, 4GlaxoSmithKline, Collegeville, PA, USA, 5Royal Marsden Hospital, Sutton, UK
Women’s Health Outcomes Research
WH1: EXPOSURE TO CONTRAINDICATED AND OTHER POTENTIALLY DANGEROUS MEDICATIONS DURING
PREGNANCY: A POPULATION BASED STUDY IN ITALY
Gagne JJ, Maio V, Berghella V, Louis DZ, Gonnella JS, Jefferson Medical College, Philadelphia, PA, USA
WH2: DISABILITY AND ASSOCIATED COSTS AMONG WOMEN WITH EMPLOYER-SPONSORED INSURANCE
AND NEWLY DIAGNOSED BREAST CANCER
Meadows E1, Johnston S2, Cao Z3, Foley K4, Pohl G1, Johnston JA1, Ramsey SD5, 1Eli Lilly and Company, Indianapolis,
IN, USA, 2Thomson Healthcare, Inc, Washington, DC, USA, 3Thomson Healthcare, Cambridge, MA, USA, 4Thomson
Medstat, Philadelphia, PA, USA, 5Fred Hutchinson Cancer Research Center, Seattle, WA, USA
WH3: CLINICAL AND ECONOMIC OUTCOMES AMONG WOMEN USING LEVONORGESTREL-RELEASING
INTRAUTERINE SYSTEM (LNG-IUS)
Yu AP1, Wu E1, Perrson B1, Chang J2, Costales AC2, Gricar JA3, 1Analysis Group, Inc, Boston, MA, USA, 2Bayer
HealthCare Pharmaceuticals, Inc, Wayne, NJ, USA, 3Independent Health Care Consultant, New York, NY, USA
WH4: PROBIOTICS IN PREGNANCY: A SYSTEMATIC REVIEW AND META-ANALYSIS OF THE SAFETY OF
LACTOBACILLUS, BIFIDOBACTERIUM AND SACCHAROMYCES
Dugoua JJ1, Zhu X1, Chen X1, Koren G2, Machado M1, Einarson TR1, 1University of Toronto, Toronto, ON, Canada,
2
Hospital for Sick Children, Toronto, ON, Canada
6:30PM-7:00PM
ISPOR ANNUAL BUSINESS MEETING
6:15PM-7:15PM
AUTHOR PRESENTATION HOUR (POSTER PRESENTATIONS
- SESSION I)
January/February 2008 ISPOR CONNECTIONS 33
ISPOR 13th Annual International Meeting
Sheraton Centre Toronto, Toronto, Ontario, Canada, May 3 - 7, 2008
PROGRAM continued
EXHIBITORS’ OPEN HOUSE RECEPTION & POSTER PRESENTATIONS VIEWING - SESSION I
6:15PM-8:00PM
6:30PM-8:00PM
ISPOR Russia Chapter Forum Presented in Russian
The Economics of Rare Diseases, Rare Surgical Treatments, Diagnostic Technologies and the
Management of Hemophilia in Russia: ISPOR Russia Chapter Forum
This forum will present experiences from Russia’s medical system with the economics and access challenges of
rare disease and surgical treatments and diagnostic technologies. The patient’s viewpoint of the management of
hemophilia in Russia will also be presented.
TUESDAY, MAY 6, 2008
7:30AM-8:30AM
ISPOR FORUMS (Open forum with buffet breakfast)
Health Technology Assessment: Reimbursement Processes, Methods and Assessments Forum
The following will be discussed: a) differences and similarities in global health care systems and reimbursement
through the newly developed on-line ISPOR Global Roadmap of Health Care Systems; b) preliminary results of a
survey assessing current methods used globally in health technology assessment and health care reimbursement;
and c) preliminary results of interviews with health technology assessment groups to determine how new technologies are assessed to inform health care policy decisions.
ISPOR Fellowship Standards Task Force Breakfast Forum
This forum provides an opportunity to discuss the upcoming publication of the Task Force report “Joint ACCP and
ISPOR Guidelines for Pharmacoeconomic and Outcomes Research Fellowship Training Programs” and an opportunity for all participants, including fellows, preceptors of fellows, academics and other interested parties, to meet
and share their thoughts and ideas about Pharmacoeconomic Fellowships.
8:30AM-8:45AM
INCOMING PRESIDENTIAL ADDRESS
Chris L. Pashos PhD, Vice President and Executive Director of HERQuLES, Abt Associates, Lexington, MA, USA
8:45AM-10:00AM SECOND PLENARY SESSION: Drug Safety and Risk-Benefit
Decision-Making
Both delayed market entry of life-saving therapies and withdrawals of products from the market underscore the
need to determine risk-benefit of a new technology early and often in a product’s life cycle. Interest in developing
single risk-benefit metrics is reappearing but will these advances lead to improved decision-making? This session
will explore how regulators and payers determine the risk-benefit tradeoffs and act upon that information.
Moderator/Speaker: Adrian Levy PhD, Associate Professor, University of British Columbia, Vancouver, BC, Canada
Speakers: Gerald J. Dal Pan MD, MHS, Director, Office of Surveillance and Epidemiology, FDA, Silver Spring, MD,
USA; Robert Powell PharmD, Director, Pharmacometrics, Offices of Clinical Pharmacology and Translation
Sciences, Center for Drug Evaluation and Research, FDA, Silver Spring, MD, USA; F. Reed Johnson PhD, Senior
Fellow and Principal Economist, RTI International, Research Triangle Park, NC, USA; Robyn Lim PhD, Scientific
Advisor, Progressive Licensing Project, Therapeutic Products Directorate, Health Products and Food Branch, Health
Canada, Ottawa, ON, Canada
Panelist(s): Deborah Marshall PhD, Vice President, i3 Innovus, Global Health Economics and Outcomes, Burlington,
ON, Canada; Gurvaneet Randhawa MD, MPD, Medical Officer and Senior Advisor, Center for Outcomes and
Evidence, Genomics & Personalized Medicine, Rockville, MD, USA; Emily S. Winn-Deen, PhD, Vice President,
Cepheid, Sunnyvale, CA, USA.
HEALTH CARE POLICY DEVELOPMENT USING OUTCOMES RESEARCH ISSUES
IP8: QUANTITATIVE APPROACHES TO REGULATORY RISK-BENEFIT ASSESSMENT FOR FDA DECISIONMAKING: WHAT WOULD WORK?
Moderator: James T. Cross MS, Graduate Student, University of Washington, Pharmaceutical Outcomes Research
and Policy Program, Seattle, WA, USA.
Panelist(s): F. Reed Johnson PhD, Senior Fellow and Principal Economist, RTI International, Research Triangle Park,
NC, USA; Larry D. Lynd PhD, Assistant Professor, University of British Columbia, Faculty of Pharmaceutical
Sciences, Vancouver, BC, Canada; Louis P. Garrison PhD, Professor of Pharmacy, University of Washington,
Department of Pharmacy, Seattle, WA, USA.
IP9: PRACTICAL CONSIDERATIONS ON COVERAGE WITH EVIDENCE DEVELOPMENT: HOW WILL THE PIPER
BE PAID?
Moderator: Stuart MacLeod MD, PhD, FRCPC, Executive Director, Children’s & Women’s Health Centre of British
Columbia, Vancouver, BC, Canada.
Panelist(s): Mike F Drummond PhD, Professor of Health Economics, University of York, Centre for Health
Economics, York, Heslington, UK; Sean Tunis MD, MSc, Executive Director, Center for Medical Technolgy Policy,
Baltimore, MD, USA; Pierre Philippe Sagnier MD, Vice President Global Health Economics, Bayer Schering Pharma,
Outcomes and Reimbursement, Wuppertal, Germany.
PATIENT-REPORTED OUTCOMES RESEARCH ISSUES
IP10: QALYS GONE WILD?
Moderator: Peter I. Juhn MD, MPH, Vice President, Evidence and Regulatory Policy, Johnson & Johnson, New
Brunswick, NJ, USA.
Panelist(s): Adrian Griffin MsC, Vice President, Strategic Affairs, LifeScan, Inc, High Wycombe, Buckinghamshire,
UK; Peter J. Neumann ScD, Professor, Tufts-New England Medical Center, Institute for Clinical Research and
Health Policy Studies, Boston, MA, USA; Michael Schlander, MD, MBA, Professor, Institute for Innovation &
Valuation in Health Care (InnoVal-HC), University of Heidelberg, Eschborn, Germany.
1:00PM-2:30PM
LUNCH, EXHIBITS, POSTER PRESENTATIONS VIEWING -
SESSION II
1:30PM-2:00PM GUIDED TOUR OF HEALTH CARE DECISIONS USING OUTCOMES
RESEARCH INFORMATION POSTER SESSION
1:30PM-2:30PM
EDUCATIONAL SYMPOSIUM (Sponsored by RTI Health Solutions)
Obtaining a Patient-Reported Outcomes Label Claim: What Evidence Do You Need?
This symposium will review what is a label claim, what evidence is needed to support the claim, and how to
design a conceptual framework and endpoint model for a PRO Evidence Dossier.
2:30PM-3:30PM
WORKSHOPS - SESSION I
10:00AM-10:15AM ISPOR SERVICE AWARDS PRESENTATION
ECONOMIC OUTCOMES RESEARCH
10:15AM-10:45AM BREAK, EXHIBITS, POSTER PRESENTATIONS VIEWING - SESSION II
W1: PRESENTING UNCERTAINTY IN COST-EFFECTIVENESS RESEARCH
Discussion Leaders: Katia Noyes PhD, MPH, Associate Professor, University of Rochester School of Medicine,
Community and Preventive Medicine, Rochester, NY, USA; Elisabeth Fenwick PhD, Lecturer, University of Glasgow,
Public Health and Health Policy, Division of Community Based Medicine, Glasgow, UK
10:45AM-11:45AM ISPOR FORUMS:
Assessment, Determinants & Economics of Medication Compliance & Persistence Forum
Research including the key considerations for researchers undertaking prospective assessment of medication compliance and persistence; the economic consequences of non-compliance; and the key ‘determinants’ of non-compliance will be presented by the ISPOR Medication Compliance & Persistence SIG.
HEALTH CARE POLICY DEVELOPMENT USING OUTCOMES RESEARCH
The initial draft of Design and Analysis of Non-Randomized Studies of Treatment Effects using Secondary
Databases will be presented. The report includes the major issues of design, analysis, and interpretation of findings from therapeutic effectiveness studies using secondary databases. Your comments and input are invited.
W2: PAYING FOR PILLS BY RESULT: PERFORMANCE-BASED REWARDS FOR INNOVATION
Discussion Leaders: Louis P. Garrison PhD, Professor of Pharmacy, University of Washington, Department of
Pharmacy, Seattle, WA, USA; Sean D. Sullivan PhD, RPh, Professor of Pharmacy and Public Health and Director,
University of Washington, Pharmaceutical Outcomes Research and Policy Program, Seattle, WA, USA; Peter J.
Neumann ScD, Professor, Tufts-New England Medical Center, Institute for Clinical Research and Health Policy
Studies, Boston, MA, USA; Adrian Towse MPhil, Director, Office of Health Economics, London, UK
ISPOR Good Research Practices on Economic Data Transferability Forum
PATIENT-REPORTED OUTCOMES RESEARCH
The draft final report and recommendations on best practices in transferability of economic data in health economic evaluations will be discussed. Several factors may limit the generalizability of economic (i.e. resource, cost
and utility) data, including differences in relative prices, practice patterns, availability of health care resources
and community values of health states. This session will focus on issues identified by ISPOR members concerning
the draft Task Force Report now at the ISPOR website. These issues include defining key variable economic data,
guidelines for acceptance of data from outside a country while considering existing national guidelines, and
directions for future research.
W3: GOOD RESEARCH PRACTICES FOR THE APPLICATION OF CONJOINT ANALYSIS IN HEALTH – A CHECKLIST FOR PUBLISHING IN OUTCOMES RESEARCH
Discussion Leaders: John FP Bridges PhD, Assistant Professor, Johns Hopkins University, Bloomberg School of
Public Health, Health Policy and Management, Baltimore, MD, USA; F. Reed Johnson PhD, Senior Fellow and
Principal Economist, RTI Health Solutions, Health Preference Assessment, Research Triangle Park, NC, USA; A. Brett
Hauber PhD, Senior Economist and Head, RTI Health Solutions, Health Preference Assessment, Research Triangle
Park, NC, USA
W4: DEVELOPMENT AND USE OF DECISION BOARDS FOR DETERMINATION OF THE GENERAL PUBLIC’S
PREFERENCE IN WILINGNESS-TO-PAY ANALYSIS
Discussion Leaders: Michael Iskedjian BPharm, MSc, President, PharmIdeas, Buffalo, NY, USA; Olivier Desjardins
BSc, Senior Research Analyst, PharmIdeas Research and Consulting Inc, Ottawa, ON, Canada; Thomas Einarson
PhD, V-P Scientific Affairs, PharmIdeas Research and Consulting Inc, Oakville, ON, Canada
ISPOR Good Research Practices for Retrospective Database Analysis Forum
Quality Improvement in Cost-Effectiveness Research (QICER) Forum
This session will focus on facilitating the improvement of health care economic evaluation research and its use in
making health care policy. Updates on the present and future of global guidelines, statistical problems in costeffectiveness research and ideas for improving the science, the prevalence and scope of quality guidelines in journals and publications, and barriers to use of cost-effectiveness data by decision-makers and patients will be presented by the ISPOR QICER Task Force.
ISPOR Student Educational Forum: Decision Analysis - Overview and Application
The ISPOR student educational forum will provide a basic overview of the key terminology in decision analysis.
During this forum, students will bridge the gap between understanding pharmacoeconomics and the practice of
decision analysis.
12:00PM-1:00PM
ISSUE PANELS - SESSION II
CLINICAL OUTCOMES RESEARCH ISSUES
IP6: ARE GOOD PRACTICE PRINCIPLES FOR OBSERVATIONAL COMPARATIVE EFFECTIVENESS RESEARCH
NEEDED?
Moderator: Nancy A. Dreyer PhD, Chief of Scientific Affairs, Outcome, Cambridge, MA, USA.
Panelist(s): Marc L. Berger MD, Vice President, Eli Lilly, Global Health Outcomes, West Point, PA, USA; Sean D
Sullivan PhD, RPh, Professor of Pharmacy and Public Health and Director, University of Washington,
Pharmaceutical Outcomes Research and Policy Program, Seattle, WA, USA; Jacques Lelorier PhD, Professor,
Université de Montreal, Montreal, QC, Canada.
IP7: NOW WHAT FOR GENOMICS? TURNING PROMISE INTO PRACTICE
Moderator: Clifford Goodman PhD, Senior Vice President, The Lewin Group, Falls Church, VA, USA.
34 January/February 2008 ISPOR CONNECTIONS
USE OF REAL WORLD DATA
W5: RECOMMENDATIONS FOR THE USE OF PATIENT REGISTRY DATA AS A COMPLEMENT FOR RANDOMIZED CLINICAL TRIALS
Discussion Leaders: Steven K Takemoto PhD, Associate Professor, Saint Louis University, Center for Outcomes
Research, Saint Louis, MO, USA; Nancy A. Dreyer PhD, Chief of Scientific Affairs, Outcome, Cambridge, MA, USA;
Claudio Faria PharmD, MPH, Associate Director of Clinical Research, UMass Medical School, Charlestown, MA,
USA; Fang Wang MD, PhD, Director, GlaxoSmithKline, Global Health Outcomes, King of Prussia, PA, USA
3:30PM-3:45PM
BREAK, EXHIBITS & POSTER PRESENTATIONS VIEWING -
SESSION II
3:45PM-5:00PM THIRD PLENARY SESSION: Patient-Reported Outcomes:
Implementing Good Research Practices
Patient-reported outcomes (PROs) are sometimes viewed as inherently subjective because they are derived from
patients. There are objective ways to gather and analyze PROs, which must be explored amidst the mounting evidence of international and cultural differences in health-related quality of life that reinforce the subjectivity of
responses. This session will review the FDA Guidance on PROs and recommendations from the ISPOR Task Force
and explore improvements in methodology and application of PROs.
ISPOR 13th Annual International Meeting
Sheraton Centre Toronto, Toronto, Ontario, Canada, May 3 - 7, 2008
PROGRAM continued
Moderator/Speaker: Stephen Joel Coons PhD, Professor, Department of Pharmacy Practice and Science, College
of Pharmacy, University of Arizona, Tucson, AZ, USA
Speakers: Nancy E. Mayo BSc, MSc, PhD, James McGill Professor, Department of Medicine, School of Physical
and Occupational Therapy, McGill University Division of Clinical Epidemiology, Division of Geriatrics, McGill
University Health Center, Montreal, QC, Canada; Margaret Rothman PhD, Senior Director, WW PRO Center of
Excellence, Johnson & Johnson Pharmaceutical Services, LLC, Washington, GA, USA; Ron Hays PhD, Professor of
Medicine, UCLA Department of Medicine, Division of General Internal Medicine & Health Services Research, Los
Angeles, CA, USA
5:00PM-5:15PM
ISPOR RESEARCH AWARDS
5:15PM-6:15PM
AUTHOR PRESENTATION HOUR (POSTER PRESENTATIONS –
SESSION II)
5:15PM-7:00PM EXHIBITORS’ WINE & CHEESE RECEPTION & POSTER PRESENTATIONS VIEWING - SESSION II
7:30PM-11:00PM
ISPOR SOCIAL EVENT!!! (Registration Required)
Enjoy dinner and the ISPOR Band (the “Monte Carlos”) by Lake Ontario
WEDNESDAY, MAY 7, 2008
7:30AM-8:30AM
BUFFET BREAKFAST (Open to all attendees)
8:30AM-9:30AM
WORKSHOPS - SESSION II
CLINICAL OUTCOMES RESEARCH
W6: SURVIVAL DATA MINING TO EXAMINE SEQUENTIAL TREATMENT OF CHRONIC DISEASE
Discussion Leaders: Patricia B Cerrito PhD, Professor, University of Louisville, Mathematics, Louisville, KY, USA;
John C Cerrito PharmD, Pharmacist, Kroger Pharmacy, Louisville, KY, USA
ECONOMIC OUTCOMES RESEARCH
W7: COUNTRY-TO-COUNTRY ADAPTATION OF PHARMACOECONOMIC RESEARCH: METHODOLOGIC CHALLENGES & POTENTIAL SOLUTIONS
Discussion Leaders: David Thompson PhD, Vice President, i3 Innovus, Medford, MA, USA; Amy K O’Sullivan PhD,
Associate Director, i3 Innovus, Medford, MA, USA; Debbie L Becker MSc, Director, i3 Innovus, Burlington, ON,
Canada
HEALTH CARE POLICY DEVELOPMENT USING OUTCOMES RESEARCH
W8: ARE WE BETTER OFF OR WORSE OFF WITH VALUE-BASED PURCHASING (VBP)?
Discussion Leaders: Peter K. Wong PhD, MBA, MS, RVP, Quality, Clinical Effectiveness & Chief Pharmacy Officer,
Southwest Ohio, Cincinnati, OH, USA; Dennis J Hanseman PhD, Senior Health Researcher, Southwest Ohio,
Cincinnati, OH, USA; Alan H Mutnick PharmD, FASHP, Director, Clincial Effectiveness Mercy Health Partners,
Southwest Ohio, Cincinnati, OH, USA
W9: CONSIDERATION OF CLINICAL AND ECONOMIC VALUE IN U.S. HEALTH TECHNOLOGY ASSESSMENT:
A MULTIPLE STAKEHOLDER VIEW
Discussion Leaders: Daniel A. Ollendorf MPH, Chief Review Officer, Institute for Clinical & Economic Review,
Boston, MA, USA; Steven D. Pearson MD, MSc, Senior Fellow, America’s Health Insurance Plans, Washington, DC,
USA; Amy Knudsen PhD, Senior Scientist, Massachusetts General Hospital, Institute for Technology Assessment,
Boston, MA, USA
PATIENT-REPORTED OUTCOMES RESEARCH
W15: AN UNBIASED OVERVIEW AND UNDERSTANDING OF THE USE OF PROPENSITY SCORING IN PHARMACOECONOMIC AND PHARMACOEPIDEMIOLOGY RESEARCH
Discussion Leaders: Matthew W. Reynolds PhD, Managing Director, Epidemiology and Database Services, United
BioSource Corporation, Medford, MA, USA; Christopher Hollenbeak PhD, Assistant Professor, Penn State College of
Medicine, Health Evaluation Sciences, Hershey, PA, USA; David J. Vanness PhD, Assistant Professor, University of
Wisconsin-Madison, Department of Population Health Sciences School, Madison, WI, USA
ECONOMIC OUTCOMES RESEARCH
W16: METHODOLOGIC DIFFERENCES BETWEEN BUDGETARY IMPACT & COST-EFFECTIVENESS ANALYSES:
IMPLICATIONS FOR “ALL-IN-ONE” PHARMACOECONOMIC MODELING
Discussion Leaders: David Thompson PhD, Vice President, i3 Innovus, Medford, MA, USA; Douglas CA Taylor, MBA,
Director, Health Economics & Outcomes Research, i3 Innovus, Medford, MA, USA; Joanna Campbell PhD, Senior
Manager, i3 Innovus, Medford, MA, USA
EDUCATION/COMMUNICATIONS IN OUTCOMES RESEARCH
W17: HEALTH BEHAVIOR CHANGE: LEADING MODELS AND THEIR PRACTICAL APPLICATION
Discussion Leaders: Vernon F Schabert PhD, Senior Director, IMS Consulting, Health Economics and Outcomes
Research, Santa Barbara, CA, USA; Alexandra Drane BA, President, Eliza Corporation, Beverly, MA, USA
HEALTH CARE POLICY DEVELOPMENT USING OUTCOMES RESEARCH
W18: EFFECTIVELY COMMUNICATING OUTCOMES RESEARCH TO ENHANCE PRODUCT SUCCESS
Discussion Leaders: Allen Lising HBA, Managing Director, Dymaxium Inc, Consulting Division, Toronto, ON,
Canada; Deborah Marshall PhD, Vice President, i3 Innovus, Global Health Economics and Outcomes, Burlington,
ON, Canada; Eric Nauenberg PhD, Senior Health Economist, Associate Professor, Ontario Ministry of Health and
Long Term Care, University of Toronto, Department of Health Policy, Management and Evaluation, Toronto, ON,
Canada
W19: TRANSPARENT AND QUANTIFIABLE APPROACHES TO HEALTH CARE DECISION MAKING: CHALLENGES AND OPPORTUNITIES FOR MULTI CRITERIA DECISION ANALYSIS (MCDA)
Discussion Leaders: Mireille M Goetghebeur PhD, VP Operations, BioMedCom Consultants Inc, Montreal, QC,
Canada; Louis Niessen MD, PhD, Senior Researcher, Erasmus Medical Center, Institute for Medical Technology
Assessment, Rotterdam, The Netherlands; Lonny J Erickson PhD, Senior Associate, Health Technology Assessment,
BioMedCom Consultants Inc, Montreal, QC, Canada; Hanane Khoury PhD, Senior Research Application Associate,
BioMedCom Consultants Inc, Montreal, QC, Canada
PATIENT-REPORTED OUTCOMES RESEARCH
W20: DEVELOPING AN IMPROVED MEASURE OF HEALTH OUTCOMES: EQ-5D IN TRANSITION
Discussion Leaders: Frank De Charro PhD, Senior Scientific Advisor, Pharmerit Europe, Rotterdam, The
Netherlands; Paul Kind, Professor, University of York, Outcomes Research Group, York, UK; Ben A. Van Hout PhD,
Professor, Pharmerit BV, Rotterdam, The Netherlands; Xavier Badia MD, PhD, PhD, IMS Health, Health Economics
and Outcomes, Barcelona, Spain
USE OF REAL WORLD DATA
W21: APPLES, ORANGES, AND PEARS: SURVIVAL ANALYSIS OF MULTIPLE ENDPOINTS
Discussion Leaders: Nicole M. Engel-Nitz PhD, Senior Researcher, i3 Innovus, an Ingenix Company, Eden Prairie,
MN, USA; Xin (Sam) Ye MS, PhD, Senior Researcher i3 Innovus, an Ingenix Company, Eden Prairie, MN, USA
10:45AM-11:00AM BREAK
11:00AM-12:00PM WORKSHOPS - SESSION IV
CLINICAL OUTCOMES RESEARCH
W22: QUANTITATIVE APPROACHES TO BENEFIT-RISK ASSESSMENT OF PHARMACEUTICALS
Discussion Leaders: Lisa McGarry MPH, Director, i3 Innovus, Health Economics & Outcomes Research, Medford,
MA, USA; Anju Parthan PhD, Senior Project Manager, i3 Innovus, Health Economics and Outcomes Research, San
Francisco, CA, USA
W10: SELECTING, EVALUATING AND DOCUMENTING SUPPORT FOR EXISTING INSTRUMENTS FOR MAKING
LABELING CLAIMS: CONTENT VALIDITY
Discussion Leaders: Pennifer Erickson PhD, Founder, OLGA, State College, PA, USA; Nancy Leidy PhD, Senior Vice
President Scientific Affairs, United BioSource Corporation, Bethesda, MD, USA; Charles D Petrie PhD, Senior
Director/Group Leader, Neurosciences, Pfizer, Global Outcomes Research, Groton, CT, USA; Margaret Rothman
PhD, Senior Director, WW Patient Reported Outcomes Center of Excellence, Johnson & Johnson Pharmaceutical
Services, LLP, Washington, GA, USA
W11: METHODS FOR MEDICATION COMPLIANCE STUDIES: AN OVERVIEW OF THE ISPOR MEDICATION
COMPLIANCE SIG GUIDELINES
Discussion Leaders: Elizabeth Manias MPharm, PhD, Associate Professor, University of Melbourne, School of
Nursing and Social Work, Faculty of Medicine, Dentistry and Health Sciences, Carlton, Victoria, Australia; Femida
Gwadry-Sridhar BScPhm, MSc, PhD, Assistant Professor, University of Western Ontario, Depts. of Medicine and
Physiology & Pharmacology, London, ON, Canada; Joshua S. Benner PharmD, ScD, Principal, IMS Health, Inc,
Health Economics and Outcomes Research, Falls Church, VA, USA; Andrew M. Peterson PharmD, Chair,
Department of Pharmacy Practice and Pharmacy Administration, University of the Sciences in Philadelphia,
Pharmacy Practice and Pharmacy Administration, Philadelphia, PA, USA
W23: WORKPLACE IMPACT MODEL OF A PHARMACEUTICAL TREATMENT FROM AN EMPLOYER PERSPECTIVE
Discussion Leaders: Peter Sun, MD, PhD, Chief Health Economist, Kailo Research Group, Indianapolis, IN, USA;
Lizheng Shi, PhD, Assistant Professor, Tulane University, Health Systems Management, New Orleans, LA, USA;
Howard Birnbaum PhD, Vice President, Analysis Group, Inc, Boston, MA, USA
W24: ASSESSING PATIENT COSTS FOR CANCER IN THE U.S: HOW, WHO, WHEN, AND WHAT
Discussion Leaders: Michael T. Halpern MD, PhD, Strategic Director, American Cancer Society, Health Services
Research, Atlanta, GA, USA; K. Robin Yabroff PhD, Epidemiologist, National Cancer Institute, Applied Research
Program, Bethesda, MD, USA; Ya-Chen Tina Shih PhD, Associate Professor, University of Texas M.D. Anderson
Cancer Center, Department of Biostatistics and Applied Mathematics, Houston, TX, USA
W25: EXTRACTING PATIENT INFORMATION FROM NATIONAL DATABASES: INCLUDING NIS AND MEPS
Discussion Leaders: Patricia B Cerrito PhD, Professor, University of Louisville, Mathematics, Louisville, KY, USA;
John C Cerrito PharmD, Pharmacist, Kroger Pharmacy, Louisville, KY, USA
USE OF REAL WORLD DATA
EDUCATION/COMMUNICATIONS IN OUTCOMES RESEARCH
W12: ECONOMIC DATABASES FOR PHARMACOECONOMIC EVALUATIONS IN CANADA: OVERVIEW AND USE
Discussion Leaders: Carl V. Asche PhD, Research Associate Professor, University of Utah College of Pharmacy,
Outcomes Research Center, Department of Pharmacotherapy, Salt Lake City, UT, USA; Philip Jacobs DPhil, Director,
Institute of Health Economics, Edmonton, AB, Canada; Rita Yim MA, MHSA, Research Fellow, Institute of Health
Economics, Edmonton, AB, Canada; Joanne Kingston PhD, Senior Economist, Institute of Health Economics,
Edmonton, AB, Canada
W13: MISINTERPRETATIONS AND MISTAKES USING CODES IN RETROSPECTIVE CLAIMS DATA ANALYSIS—
AND HOW TO AVOID THEM
Discussion Leaders: George A. Goldberg MD, Medical Director, i3 Innovus, Santa Monica, CA, USA; Matt Moore
MHA, Director Health Economics, Ethicon Endo-Surgery, Inc, Health Economics, Cincinnati, OH, USA; Michael
Dutro PharmD, Director, Pfizer Inc, Albuquerque, NM, USA
9:30AM-9:45AM
BREAK
9:45AM-10:45AM WORKSHOPS - SESSION III
CLINICAL OUTCOMES RESEARCH
W14: ADVANCES IN META ANALYSIS: TECHNIQUES FOR INCLUDING MULTIPLE STUDY DESIGNS, MULTIPLE ENDPOINTS, AND MULTIPLE TREATMENTS
Discussion Leaders: Jeroen P Jansen PhD, Associate Research Director, Mapi Values, Boston, MA, USA; Melvin
Olson PhD, Senior Biostatician, Novartis Pharma AG, Basel, Switzerland; Chris Evans PhD, MPH, Director of
Economics and Outcomes, Mapi Values, Boston, MA, USA
ECONOMIC OUTCOMES RESEARCH
W26: TRAINING CONSIDERATIONS FOR PATIENT-REPORTED OUTCOMES
Discussion Leaders: Adam John Butler SR, Assistant Vice-President, Training and Education, United BioSource
Corporation, Wayne, PA, USA; Anne M Rentz MSPH, Research Scientist, United BioSource Corporation, The Center
for Health Outcomes Research, Bethesda, MD, USA
HEALTH CARE POLICY DEVELOPMENT USING OUTCOMES RESEARCH
W27: DIFFERENCES IN PHARMACOECONOMIC DATA SUBMISSION GUIDELINES FOR THE US, CANADA,
AND MEXICO: IMPLICATIONS FOR MULTI-COUNTRY HEALTH-ECONOMICS PROGRAMS
Discussion Leaders: David Thompson PhD, Vice President, i3 Innovus, Medford, MA, USA; Shawn J Barry MA,
Associate Director, Analytics, i3 Innovus, Burlington, ON, Canada; Jf Mould-Quevedo PhD, MSc, MBA,
Pharmacoeconomics Manager, Pfizer Mexico, Pharmacoeconomics Department, Mexico City, Mexico
W28: REAL-LIFE PATIENT-REPORTED OUTCOMES: A NOVEL USE OF THE FDA ADVERSE EVENT REPORTING SYSTEM (AERS) SAFETY DATABASE
Discussion Leaders: Matthew W. Reynolds PhD, Managing Director, Epidemiology and Database Services, United
BioSource Corporation, Medford, MA, USA; Donald Stull PhD, Research Scientist, United BioSource Corporation,
Center for Health Outcomes Research, Bethesda, MD, USA; Robert Nordyke PhD, MS, Director, Amgen, Inc, Global
Health Economics, Thousand Oaks, CA, USA
W29: CAPTURING THE IMPACT OF HETEROGENEITY IN PHARMACOECONOMIC EVALUATION
Discussion Leaders: Denis Getsios BA, Research Scientist, United BioSource Corporation, Concord, MA, USA;
Kristen Migliaccio-Walle BS, Research Scientist, United BioSource Corporation, Concord, MA, USA; Duygu
Bozkaya MSc, MBA, Researcher, United BioSource Corporation, Concord, MA, USA
January/February 2008 ISPOR CONNECTIONS 35
ISPOR 13th Annual International Meeting
Sheraton Centre Toronto, Toronto, Ontario, Canada, May 3 - 7, 2008
SHORT COURSE PROGRAM
SATURDAY, MAY 3, 2008
drug to a health plan formulary will be presented. Issues related to imputing missing data will
also be discussed. This course is designed for those with some experience with pharmacoeconomic analysis.
(ALL DAY COURSES) 8:00 AM - 5:00 PM
Cost-Effectiveness Analysis Alongside Clinical Trials
Faculty: Scott Ramsey MD, PhD, Fred Hutchinson Cancer Research Center; Richard Willke PhD,
US Development Sites Pfizer, Inc.
Course Description: The growing number of prospective clinical/economic trials reflects both
widespread interest in economic information for new technologies and the regulatory and reimbursement requirements of many countries that now consider evidence of economic value along
with clinical efficacy. This course will present the design, conduct, and reporting of cost-effectiveness analyses alongside clinical trials based on, in part, the Good Research Practices for CostEffectiveness Analysis alongside Clinical Trials: The ISPOR RCT-CEA Task Force Report. Trial design,
selecting data elements, database design and management, analysis, and reporting of results will
be presented. Trials designed to evaluate effectiveness (rather than efficacy), as well as clinical
outcome measures will be discussed. How to obtain health resource use and health state utilities
directly from study subjects and economic data collection fully integrated into the study will also
be discussed. Analyses guided by an analysis plan and hypotheses, an incremental analysis using
an intention to treat approach, characterization of uncertainty and standards for reporting results
will be presented. This is an introductory/intermediate level course. Familiarity with economic evaluations
will be helpful.
Pharmacoeconomics for Decision-Makers
Faculty: Lorne Basskin PhD, Healthsouth Sunrise Rehab Hospital
Course Description: This course is designed to teach clinicians and new researchers how to
incorporate pharmacoeconomics into study design and data analysis. Participants will learn how
to collect and calculate the costs of different alternatives, determine the economic impact of
clinical outcomes, and how to identify, track and assign costs to different types of health care
resources used. The development of economic protocols and data collection sheets will be discussed. Different pharmacoeconomic models and techniques will be demonstrated and practiced
in lectures and case studies. These include cost-minimization, cost-of-illness, cost-effectiveness,
cost-benefit, and cost-utility analysis. Decision analysis, sensitivity analysis, and discounting will
all be demonstrated and practiced. Participants will also learn to compare and evaluate interventions such as drugs, devices and clinical services. This course is suitable for those with little or no experience with pharmacoeconomics.
Bayesian Analysis: Overview & Applications
Faculty: Bryan Luce MBA, PhD, United BioSource Corporation; Christopher S. Hollenbeak PhD,
Penn State College of Medicine; David Vanness PhD, University of Wisconsin Medical School
Course Description: The first portion of this course is designed to provide an overview of the
Bayesian approach and its applications to health economics and outcomes research. The course
will cover basic elements of Bayesian statistics, contrasting briefly with classical (frequentist) statistics and will introduce available statistical packages. The second portion of this course will
focus on the Bayesian “informative prior.” Several example vignettes of how a Bayesian analysis
can be used within outcomes modeling problems will be presented. Participants will learn how a
Bayesian approach is different, why it is useful for their work and what tools are available to
them. Participants of this course should be prepared to use their own laptops as the exercises
presented use interactive software. This course is designed for those with a limited understanding of
Bayesian statistical concepts.
SATURDAY, MAY 3, 2008 (MORNING COURSES) 8:00 AM - 12:00 PM
PHARMACOECONOMIC / ECONOMIC METHODS
Finding and Extracting Cost Data
Faculty: L. Clark Paramore MSPH, United BioSource Corporation; Gregory de Lissovoy MPH,
PhD, United BioSource Corporation
Course Description: This course will focus on practical aspects of cost development for pharmacoeconomic studies. The objective is to help the participant bridge the gap between understanding pharmacoeconomic theory and the practice of developing cost estimates. Factors to consider
when costing pharmacoeconomic analyses, such as perspective, data sources, data classification
systems, developing resource use profiles, obtaining unit costs, and making cost adjustments will
be presented. Examples of issues encountered when identifying and extracting cost data will be
discussed. This course is designed for those with some experience with pharmacoeconomic analysis.
Modeling: Design and Structure of a Model
Faculty: Marc Botteman MA, PharMerit North America LLC; Ben van Hout PhD, PharMerit
Course Description: This course will include a review of modeling techniques (Markov models,
discrete event simulations, and Monte Carlo techniques) including a discussion of the ISPOR
Principles of Good Practice for Decision Analytic Modeling in Health Care Evaluations. Markov
models and first and second order Monte Carlo simulations including data identification, data
modeling, and data incorporation will be demonstrated. Using a series of examples, the course
will carefully review the practical steps involved in developing and using these kinds of models.
Examples will be presented using Microsoft Excel, supplemented with add on simulation software. This course will cover the practical steps involved in the selection of models and options in modeling of
data inputs. Participants should have a basic understanding of decision analysis.
Applications in Using Large Databases
Faculty: Diana Brixner PhD, RPh, University of Utah; John Parkinson PhD, GPRD; Michael
Eaddy PhD, PharmD, Xcenda
Course Description: This course will provide a review of 3 health care databases – GPRD (UK
database), GE Centricity electronic medical record and Medicaid (USA databases). Each database
will be discussed in-depth including directions on how to access the information and how
researchers utilize this information. Instructors will distinguish the important differences between
these databases including the limitations and strategies to maximize their value through the use
of an interactive format with interactive examples. Discussion will include a reference to the
ISPOR Classification of Database Working Group / Retrospective Database Special Interest Group
and its digest of International Databases. Participants must have some knowledge of administrative
health care database analysis.
SATURDAY, MAY 3, 2008 (AFTERNOON COURSES) 1:00 PM - 5:00 PM
Financial Impact / Cost of Illness
Faculty: Josephine Mauskopf PhD, RTI Health Solutions; C. Daniel Mullins PhD, University of
Maryland
Course Description: This course will describe methods to determine the costs associated with a
health condition and the budget impact of new technologies for that condition. The course will
present incidence and prevalence-based costing strategies. Treatment algorithms and eventbased approaches will be demonstrated for disease-specific costs from different decision-maker
perspectives. Both static and dynamic methods for estimating the budget impact of adding a new
36 January/February 2008 ISPOR CONNECTIONS
Advanced Quantitative Methods for Quality of Life / Patient-Reported
Outcomes
Faculty: Kathleen Rosa MS, PhD, Mapi Values; Jeffrey McDonald MS, Mapi Values
Course Description: This course will provide an in-depth discussion of operating characteristics,
validity testing, analysis and interpretation with examples of each. It will provide a range of
methods that may help to solve common problems encountered with quality of life / patientreported outcomes. These include an overview of psychometric validation methods including: a
brief overview of Rasch analysis, pragmatic issues in validating a PRO from clinical trial data,
ePRO validation, methods of estimation of minimally clinically important differences and alternatives to provide information on interpretation. Clinical trial analysis will include missing data
analysis techniques and mixed modeling appropriate to PRO data and study design. There will be
a focus on addressing these issues within the framework provided by the PRO guidance recently
released by the SEALD group at the FDA. Specific examples will be used throughout the course
and participants will be asked to complete a short exercise. This course is designed for those with
intermediate experience in health-related quality-of-life assessment.
Instrumental Variables in Addressing Selection Bias in Observational Studies
Faculty: Benjamin M. Craig PhD, University of Wisconsin; Antoine C. El Khoury, PhD, Merck &
Co Inc.; Bradley Martin PhD, RPh, PharmD, University of Arkansas for Medical Sciences
Course Description: In any non-randomized study, selection bias is a potential threat to the
validity of conclusions reached. Failure to account for sample selection bias can lead to conclusions about treatment effectiveness or treatment cost that are not really due to the treatment at
all, but rather to the unobserved factors that are correlated with both treatment and outcomes.
Sample selection models provide a test for the presence of selection bias. These models also provide a correction for selection bias, enabling an investigator to obtain unbiased estimates of
treatment effects. This course will discuss the various models and their applications, and in particular will address instrument variables (two-stage least squares, intuition, RCTs), including an
overview of examples from the current literature. Participants will benefit from interactive exercises using instrumental variables and sample selection techniques using STATA. For those who
have STATA loaded on their laptops, you are encouraged to bring your laptop. This course is suitable
for those with some knowledge of econometrics.
Elements of Pharmaceutical/Biotech Pricing I - Introduction
Faculty: Jack Mycka, MME LLC; Renato Dellamano PhD, ValueVector
Course Description: This course will give participants a basic understanding of the key terminology and issues involved in pharmaceutical pricing decisions. It will cover the tools to build and
document product value including issues, information and processes employed (including pricing
research); the role of pharmacoeconomics and the differences in payment systems that help to
shape pricing decisions. These tools will be further explored through a series of interactive exercises. This course is designed for those with limited experience in the area of pharmaceutical pricing and will
cover topics within a global context.
SUNDAY, MAY 4, 2008
(ALL DAY COURSES) 8:00 AM - 5:00 PM
Retrospective Database Analysis – Econometric Methods
Faculty: William H. Crown PhD, i3 Innovus; Henry Henk PhD, i3 Innovus
Course Description: Large administrative claims databases provide a unique opportunity to
examine retrospectively the effects of drug use on clinical and economic outcomes in "real world"
settings. This course will cover a discussion of the ISPOR Checklist for Retrospective Database
Studies - Report of the ISPOR Task Force on Retrospective Databases and selected topics related
to estimators and sampling distributions, properties of sampling distributions (unbiasedness, efficiency, mean square error), and ordinary least squares (OLS) regression. OLS model assumptions
and the implications of violations (e.g., heteroscedasticity, multicollinearity, autocorrelation) will
also be discussed. More complex topics beginning with the problem of endogeneity, identification, instrumental variables, sample selection models, propensity score models, maximum likelihood methods and the estimation of limited dependent variables models including logit, multinomial logit, count models, and survival models will be discussed. This course will assume participants
have knowledge of statistical methods through OLS regression and experience in the analysis of administrative
claims databases.
ISPOR 13th Annual International Meeting
Sheraton Centre Toronto, Toronto, Ontario, Canada, May 3 - 7, 2008
SUNDAY, MAY 4, 2008 (MORNING COURSES) 8:00 AM - 12:00 PM
SUNDAY, MAY 4, 2008 (AFTERNOON COURSES) 1:00 PM - 5:00 PM
Propensity Scores and Comorbidity Risk Adjustment
Faculty: Fadia Shaya MPH, PhD, University of Maryland
Course Description: A large part of the evidence about the effectiveness of different treatments
is based on retrospective studies. Issues of bias and confounding relate to the non-random
assignment of subjects and co-morbidity burden. This course will outline the concerns about bias
and explain the methods for causal inference in observational studies, where researchers have no
control over the treatment assignment. A lack of balance in the covariates between the treatment and control groups can produce biased estimates of the treatment effects. We will explain
how propensity scores can be used to reduce bias, through stratification, matching or regression.
Confounding and the pros and cons of standard adjustment, propensity scoring methodology (sub
classification on one confounding variable, overlap in treatment groups, variable selection) will be
discussed. In the second part, we will elaborate on risk adjustment models, focusing on morbidity
indices, e.g the Charlson Comorbidity Index, and Chronic Disease Scores. Examples using a step by
step approach will be presented. This is an introductory course, designed for those with little experience
with this methodology but some knowledge of observational databases.
Applications of Statistical Considerations in Health Economic Evaluations
Faculty: Henry Glick PhD, University of Pennsylvania; Jalpa Doshi PhD, University of
Pennsylvania
Course Description: This course will provide applications of statistical considerations in economic analysis. Specific exercises will be conducted to illustrate affect of distributional assumptions,
univariate & multivariable analysis of costs, the effect of sample size & power calculations on
economic evaluations and point estimates for cost-effectiveness ratios. Participants are encouraged to have hands-on experience and bring their laptops. STATA trial software will be distributed
if not already installed and used in this course. The publication “Economic Evaluation in Clinical
Trials” (Oxford: OUP, 2007) is suggested as recommended reading for this course. The course,
Statistical Considerations in Economic Evaluations, is a strong prerequisite for this course.
Bayesian Analysis: Advanced
Faculty: Bryan Luce MBA, PhD, United BioSource Corporation; Keith R. Abrams PhD, University
of Leicester
Course Description: This course introduces the use of Bayesian methods in evidence synthesis
(including meta-analysis) and allows participants to gain hands on experience using such modeling techniques within WinBUGS. Methodological issues considered in the course include; fixed
and random effects models, choice of prior distributions, subgroups, meta-regression and adjusting for baseline risk, together with indirect and mixed treatment comparisons. Further metaanalysis topics for which a Bayesian approach can be of benefit will also be highlighted.
Participants will be expected to be familiar with the use of WinBUGS and will be responsible for
bringing a laptop with the latest, unrestricted version of WinBUGS pre-installed. This course is a
follow-up to the short course: Bayesian Analysis-Overview and Applications. Basic knowledge of the Bayesian
approach and use of WinBUGS (equivalent to attendance at Bayesian Analysis-Overview and Applications)
will be assumed.
Discrete Event Simulation for Economic Analyses
Faculty: J. Jaime Caro MDCM, FCRPC, FACP, United BioSource Corporation; Jörgen Möller
MSc Mech Eng, United BioSource Corporation
Course Description: This course will provide a basic understanding of the key concepts of discrete event simulation (DES). The focus will be on the use of these simulation models to address
pharmacoeconomic (and device-related) problems. The course will be structured around practical
exercises. Topics to be covered are: Why DES? Dynamic simulation as a tool; Components of a
DES; How do you build a model? Modeling of processes and resource use; Modeling of variables
and decisions. If time permits, simple animation will be demonstrated. We will use ARENA to
build simple models. Instructors will distribute training versions of Arena. This course is designed for
those with some experience with modeling.
Patient-Reported Outcomes - Item Response Theory
Faculty: Lori McLeod PhD, RTI Health Solutions; Cheryl Hill PhD, RTI- Health Solutions
Course Description: There is a great need in health outcomes research to develop instruments
that accurately measure a person's health status with minimal response burden. This need for
psychometrically sound and clinically meaningful measures calls for better analytical tools
beyond the methods available from traditional measurement theory. Applications of item
response theory (IRT) modeling have increased considerably because of its utility for instrument
development and evaluation, assessment of measurement equivalence, instrument linking, and
computerized adaptive testing. IRT models the relationship, in probabilistic terms, between a person's response to a survey question and their standing on a health construct such as fatigue or
depression. This information allows instrument developers to develop reliable and efficient quality
of life measures tailored for an individual or group. This introductory workshop will discuss the
basics of IRT models and applications of these models to improve health outcomes measurement.
Illustrations will be used throughout the presentation that focus on measuring key health-related
quality of life domains in different disease populations. This introductory course is designed for those
with none to little experience with IRT.
Case Studies in Pharmaceutical/Biotech Pricing II - Advanced
Faculty: Jack Mycka, MME LLC; Renato Dellamano PhD, ValueVector
Course Description: Case studies will be employed to lead participants through the key steps of
new product pricing, with focus on the need to thoroughly analyze the business environment and
its constraints and opportunities and the need to closely integrate the pricing, reimbursement
and pharmacoeconomic strategy for the new product with the clinical development and marketing strategies. Practical exercises will allow participants to consolidate the concepts delivered in
the “Elements” introductory session and expanded here. Areas covered will include the postlaunch issues of reimbursement and pricing maintenance as a part of life-cycle management in a
global environment. This course is for individuals who have completed Elements of Pharmaceutical Pricing I
– Introduction or are familiar with both the key determinants of pharmaceutical pricing and the main international health systems. Enrollment for this course is limited.
Statistical Considerations in Health Economic Evaluations
Faculty: Henry Glick PhD, University of Pennsylvania; Jalpa Doshi PhD, University of
Pennsylvania
Course Description: The adoption and diffusion of new medical treatments depend increasingly
on robust analysis of costs and cost-effectiveness. During this course, the following statistical
considerations in economic evaluations will be discussed: affect of distributional assumptions,
analyzing univariate and multivariable analysis data, analyzing censored data, sample size and
power calculations, sampling uncertainty, point estimates for variables, net monetary benefit, and
confidence intervals for cost-effectiveness ratios. During this course, study examples will be provided to
illustrate concepts. Participants should have some knowledge of basic economic evaluations and statistics.
Patient Registries
Faculty: Chris Pashos PhD, Abt Associates – HERQuLES
Course Description: This course is designed to provide an overview of patient registries and their
applications in identifying 'real world' clinical, safety, and patient-perspective issues. The pros and
cons of registry data compared to other ‘real world’ and clinical trial data collection will be presented. How registry information can be used to support other health economics /outcomes
research initiatives and health care decision-making will be addressed. Registry strategy, design,
operations and measures of program success will be discussed. In addition, regulatory trends
and requirements, including the Agency for Healthcare Research & Quality’s (AHRQ) May 2007
publication: “Registries for Evaluating Patient Outcomes: A User's Guide”, will be examined. This
course is designed for those with little experience with patient registries.
Utility Measures
Faculty: F. Reed Johnson PhD, RTI Health Solutions; A. Brett Hauber PhD, RTI Health Solutions
Course Description: Course participants will learn the conceptual and empirical features of various health-utility measures and their uses for informing health care decision-making. Cost-utility
analysis (CUA), risk-benefit analysis (RBA), and cost-benefit analysis (CBA) are often used to evaluate new health-care technologies. These methods are useful for informing decision-makers
about the relative benefits of an intervention to individual patients and to society as a whole.
CUA employs health-state utilities based on cardinal utility theory to define quality-adjusted life
years (QALYs) for different health states. RBA employs utility measures to place both risks and
benefits in comparable units. CBA estimates take the form of ordinal utility values expressed as
money-equivalent values (often called ‘willingness to pay’). This course will review the theory and
application of utility estimation in health economics and risk-benefit analysis. This course is designed for
those with some experience with psychometric measures.
Outcomes Research for Medical Devices & Diagnostics
Faculty: Seema Sonnad PhD, University of Pennsylvania; Stacey Ackerman MSE, PhD, Covance
Market Access Services
Course Description: This course will present outcomes research practices that are specifically
tailored for the fast-paced medical device and diagnostics technology environment and address
issues related to these health technology assessment methodologies. Outcomes research including clinical outcomes, economic outcomes, and patient-reported outcomes will be discussed.
Outcomes research for medical devices & diagnostics will be differentiated from other health care
interventions such as drugs. The evidence hierarchy for medical devices and diagnostic procedures
including ‘real world’ outcomes research information in coverage and reimbursement decisions
will be discussed. This course is designed for those with little experience with outcomes research for medical
devices and diagnostic technologies.
Introduction to Risk/Benefit Management in Health Care
Faculty: Dennis W. Raisch PhD, VA Cooperative Studies Program; Anthony Lockett MD, PhD,
MBA, ICO; Suellen Curkendall PhD, Cerner Health Insights
Course Description: This course will provide an overview of risk/benefit management for pharmaceuticals and devices. The risk/benefit assessment process will be described in regards to stage
of product development, from pre-marketing through post-marketing. Risk mitigation includes
the various strategies employed by manufacturers, regulators, and health care providers, with an
emphasis on international differences in risk mitigation and decision-making. Risk/benefit communication processes will be described, focusing on how decisions regarding risks and benefits of
pharmaceuticals and devices are communicated to health care providers and the public. This
includes direct mailing, direct-to-consumer marketing, and labeling. Real world exercises will
allow participants to discuss key topics and propose implementation strategies for risk management. This course is designed for those with a basic understanding of pharmacoepidemiology principles.
Advanced Decision Modeling for Health Economic Evaluations
Faculty: Andrew Briggs PhD, University of Glasgow; Mark Sculpher PhD, MSc, University of York
Course Description: During this course, the key aspects and new developments of decision modeling for economic analysis will be considered. How models can be made probabilistic to capture
parameter uncertainty (including rationale, choosing parameter distributions, & types of uncertainty) will be covered. How to analyze and present the results of probabilistic models will be
presented. How the results of probabilistic decision modeling should be interpreted and how
decisions should be made (including decisions with uncertainty, and expected value of perfect
information [EVPI]), will be presented. Specific examples including Excel programming will be
used to illustrate concepts. The publication “Decision Modeling for Health Economic Evaluation”
(Oxford, 2006) is recommended reading for this course. This is an advanced course. Participants should
have a basic understanding of decision analysis. The course, Modeling: Design and Structure of a Model, is a
strong prerequisite for this course.
January/February 2008 ISPOR CONNECTIONS 37
ISPOR 13th Annual
International Meeting
Sheraton Centre Toronto
Toronto, Ontario, Canada
May 3 - 7, 2008
Promotional Opportunites
EXHIBIT
ADVERTISE
Register now for exhibit space!
Over 1700 attendees in 2007.
Present your products and services to key outcomes researchers
and health care decision-makers in pharmaceutical, medical
device and diagnostics, biotechnology industries, clinical practice,
government agencies, academia, and health care organizations.
Advertise in the Program and Schedule of Events!
Advertising Deadline: MARCH 20, 2008
Benefits to Exhibitors:
• Listing and 1/4 page advertisement in the Program and
Schedule of Events
• Listing and 1/4 page advertisement on the ISPOR website
• One complimentary registration per exhibit booth
• Pre-registrant mailing labels
SPONSOR
Increase your visibility!
Give your company increased visibility and prominence.
Benefits to Sponsors:
• Sponsorship recognition at plenary session
• Event signage
• Listing and 1/4 page advertisement in the Program and
Schedule of Events
• Listing and 1/4 page advertisement on the ISPOR website
• One complimentary registration per booth
• Preferential exhibit booth location
Hotel Reservations
Sheraton Centre Toronto, 123 Queen Street West,
Toronto, ON M5H 2M9 Canada
Phone: (416) 361-1000
Discounted room rates available for ISPOR Meeting
attendees from CND$179 plus applicable taxes
EMPLOYMENT
Targeted employment assistance!
ISPOR’s Professional Recruitment Assistance Program (PRAP)
provides participants with a CONFIDENTIAL, EFFICIENT, and
PROFESSIONAL service which matches individuals seeking positions with employers who have available positions.
PRAP Includes:
• List of available positions
• List of qualified candidates
• Interview Room
• Confidential mailbox system for applicants and employers
• 1/4 page employment advertisement in the Program and
Schedule of Events
• List of 13th Annual International Meeting PRAP positions at
the ISPOR website
Advertising Deadline for the Program and
Schedule of Events: MARCH 20, 2008
For Further Information: www.ispor.org
**The discounted room rates are available April 29 - May
11 and will be charged in CND$**
**The deadline for hotel reservations at the discounted
rate is April 12, 2008**
(Please mention the ISPOR 13th Annual International
Meeting to receive the discounted rate)
Making Hotel Reservations:
Online reservations can be made through the ISPOR
website at www.ispor.org or by phone by calling the
Sheraton Centre Toronto at 1-866-716-8101.
For additional information visit: www.ispor.org
3100 Princeton Pike, Bldg 3, Suite E, Lawrenceville, NJ 08648, USA
Tel:+609-219-0773 Toll Free: +800-992-0643 Email: exhibit@ispor.org www.ispor.org
38 January/February 2008 ISPOR CONNECTIONS
ISPOR 13th Annual International Meeting
Sheraton Centre Toronto, Toronto, Ontario, Canada, May 3 - 7, 2008
January/February 2008 ISPOR CONNECTIONS 39
International Society for Pharmacoeconomics and Outcomes Research
3100 Princeton Pike, Building 3, Suite E
Lawrenceville, NJ 08648 USA