Retrospective correction of the heel effect in hand radiographs
advertisement

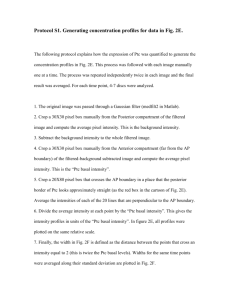
July 2001 Technical Report: KUL/ESAT/PSI/0105 Retrospective correction of the heel effect in hand radiographs G. Behiels, F. Maes, D. Vandermeulen and P. Suetens Katholieke Universiteit Leuven - Center for Processing Speech Kasteelpark Arenberg 10 B-3001 Heverlee, Belgium Telephone: +32-(0)16-32.17.13 Fax: +32-(0)16-32.17.23 Retrospective correction of the heel effect in hand radiographs G. Behiels, F. Maes , D. Vandermeulen, and P. Suetens Faculties of Medicine and Engineering, Medical Image Computing (Radiology - ESAT/PSI), University Hospital Gasthuisberg, Herestraat 49, 3000 Leuven, Belgium Gert.Behiels@uz.kuleuven.ac.be Abstract. A method for retrospective correction of intensity inhomogeneities induced by the heel effect in digital radiographs is presented. The method is based on a theoretical model for the heel effect which is derived from the acquisition geometry. Because the heel effect is directly measurable in the direct exposure area only, the image is partitioned first to exclude collimation and diagnostic areas. The parameters of the model are determined by fitting the model to the direct exposure area and the correction is then applied to the whole image. The method iterates between background segmentation and heel effect correction until convergence. We evaluate the suitability of the method on flat field and phantom images and demonstrate its robustness on a database of 137 diagnostic hand radiographs. 1 Introduction Digital radiography offers the possibility for computer aided diagnosis and quantitative analysis using image processing techniques such as contrast enhancement [10] or segmentation [2–4, 8]. However, computer-based image interpretation is hindered by the presence of the non-uniformities in X-ray exposure that are inherent to the image formation and which can be largely attributed to the heel effect. Although the intensity inhomogeneity induced by the heel effect is a smoothly varying function of location and is easily corrected by the human visual perception system, it complicates the use of automatic processing techniques because the brightness of an object within the image is position dependent. The overall intensity range is unnecessarily enlarged by the presence of these slowly varying shading components and hence the resolution available to represent diagnostic signal details is reduced. Because the image acquisition parameters that affect intensity inhomogeneity vary from image to image (e.g. variable positioning of the recording device relative to the X-ray source) and can not be recovered from the acquired image at read out, correction methods based on calibration images are not feasible and retrospective methods are needed. Frederik Maes is Postdoctoral Fellow of the Fund for Scientific Research - Flanders (FWO-Vlaanderen, Belgium). 2 1 3 1 2 Fig. 1. A typical image of the hand with the heel effect clearly visible on the direct exposure area (brighter on the left-side of the image and dark on the right). The image consists of three important regions: (1) the collimation areas (2) the direct exposure area (3) the hand or diagnostic region In this paper, we present a fully automated method for intensity inhomogeneity correction of digital radiographs by fitting a mathematical model for the heel effect derived from the acquisition geometry [5] to the image intensity data. Because the inhomogeneities are only directly measurable in the background or direct exposure areas of the image, we first extract the background region and estimate the parameters of our model from this region only. Inhomogeneity correction is then applied to the whole image, a new background region is extracted from the corrected data and the model parameters are re-estimated. This is repeated until no significant changes in background and parameter estimation occur. We demonstrate the performance of the method on a database of hand radiographs that were acquired for bone age determination. 2 Modeling the heel effect A typical hand radiograph is shown in Fig. 1. The background at the left side of the image is clearly brighter than at the right side. This phenomenon can be attributed to the so-called heel effect. It is only visible in the direct exposure and diagnostic areas and not in the collimation area. The heel effect can be understood from the construction of the X-ray tube as schematically depicted in Fig. 2. Electrons originating from the cathode are attracted by the positively charged anode. For better heat dissipation, the anode rotates and is inclined by a small anode angle θ, which enlarges the area Sactual that is bombarded by electrons while keeping the size of the focal spot Seff , from which rays are projected downward to the object, fairly small. As shown in the diagram of Fig. 2(b), this design makes the length of the path traveled by the X-rays through the anode larger on the anode side of the field (Ta ) than on the cathode side (a) (b) (c) High Voltage p Dave θ ω Rotor filament (cathode) Ta φ e− ξ= (p R,z R) D is Tc θ Sactual target (anode) S D ave ω anode y θ p Intensity S eff S’eff γ pω γ Film z R x position Fig. 2. (a)-(b) Schematic sides view of an x-ray tube. The anode angle allows the use of a large focal spot (Sactual ) for heat-loading considerations and a small projected focal spot (Seff ). X-rays are emitted at an average depth Dave ; the path length on the anode side Ta is larger and causes a reduction in intensity. (c) X-ray coordinate system where the X-ray originates at position (0, 0) and travels along R to the film at position (p, Dis ). (Tc ). Hence the incident X-ray intensity is smaller at the anode side than at the cathode side of the recording device, which explains the inhomogeneity of the background in Fig. 1. A mathematical model for the heel effect can be derived from the simplified one-dimensional model of the anode and beam geometry depicted in Fig. 2(c) [5]. In the coordinate system (p, z), with p along the anode-cathode axis and z along the vertical direction, the X-rays can be taught off to originate within the anode at point ω(0, 0), at a distance Dave from the anode surface S. Consider the ray R at an angle φ from the vertical within the plane (ω, S) that hits the recording device at point (p, Dis ) with Dis the distance between the X-ray source and the recording device and tan φ = Dpis . The distance r traveled by R through the anode is given by r = |ξ − ω| = 2 p2R + zR (1) with ξ(pR , zR ) the intersection of R with S which can be found by solving the system of equations: S : pR = Dave − tan θ.zR (2) R : pR = tan φ.zR Hence, 1+ r(p) = Dave p Dis cos θ = Dave sin(φ + θ) tan θ + 2 p Dis (3) The radiation received on the recording device is M (p) = I0 · e−µ·r(p) (4) with µ the attenuation coefficient of the anode material and I0 the radiation originating at ω. (a) (b) (c) (d) 1 3 2 2 1 Fig. 3. (a) Collimator edge detection: the detected collimation area is painted black and the rejected boundaries are displayed as white dotted lines. (b) Choice of the boundary: the diagnostic region is discarded, together with some direct exposure pixels at the bottom left of the image (c)-(d) first, intermediate and final step of the algorithm after which no more seed points are left. Model (4) predicts that the heel effect behaves exponentially along the anodecathode axis and assumes that it is constant perpendicular to this axis. This is justified by flat field exposure experiments which show that the difference in intensity perpendicular to the anode-cathode axis is relatively small compared to the intensity differences along the anode-cathode axis (see Fig. 6). 3 Image partitioning A typical hand radiograph, as shown in Fig. 1, consists of three regions: collimation area, direct exposure area and diagnostic regions. Because the heel effect is not present in the collimation area and directly measurable in the direct exposure area only, we need to partition the image to fit model (4) to the image intensity data. We do this by first extracting the collimation area and then searching the direct exposure area, the remaining areas being diagnostic regions. We find the boundaries of the collimation area using the Hough transform [6], assuming that these are rectilinear edges as is the case for all hand radiographs in our database. To make this approach more robust, the contributions of each image point to the Hough accumulator are weighted by its gradient magnitude [1] and, for each point, only the lines whose direction is within 10 degrees from the normal to the local gradient direction are considered [7]. The 4 most salient points in Hough space that represent a quadragon with inner angles between 80 and 100 degrees are selected as candidate boundaries of the collimation area. Because not all 4 collimation boundaries are always present in the image, candidate boundaries along which the image intensity differs from the intensity expected for the collimation region are rejected. A typical result is shown in Fig. 3(a). To extract the background region B, a seed fill algorithm is used that starts from the boundary of the collimation region as determined in the previous step. Appropriate seed points for B are found by considering a small band along each of the collimator edges and retaining all pixels whose intensity is smaller than the mean of the band. This approach avoids choosing pixels that belong to the diagnostic region as candidate seed pixels. B is then grown by considering all neighboring pixels ni , i = 1, . . . , 8 of each pixel p ∈ B and adding qi to B if the No Image Collimation Detection Direct Exposure n=0Estimate a n n=0 Yes Determine AnodeCathode Axis Parameter b n Estimation Model Correction |an - a n-1|<e 1 or |bn - b n-1|<e 2 Yes Corrected Image Gradient Image n=n+1 No Fig. 4. Flowchart of the algorithm for heel effect correction. We iterate between model correction and background estimation until there are no significant changes. intensity difference between p and qi is smaller than some specified threshold. A few snapshots of the progress are shown in Fig. 3(b)-(d). 4 Heel effect estimation To fit the model (4) to the image data N (x, y) we have to find the direction γ of the anode-cathode axis and the parameters α = [I0 , µ, θ, Dis , Dave , pω ] such that the model best fits the image data within the direct exposure area extracted above. pω is a parameter introduced to map point ω where the X-ray originates to the correct image coordinates (see Fig. 2(c)). Assuming that γ is known, the average image profile Pγ (p) along this direction in the direct exposure region B is given by Pγ (p) = N (x, y)(x,y)∈B|x·cos γ+y·sin γ=p with x and y the image coordinates as defined in Fig. 2(c) and · the averaging operator. We can then find the optimal model parameters α∗ by fitting the expected profile M (p, α) to the measured profile Pγ (p): α∗ (γ) = arg min Pγ (p) − M (p, α) α (5) The fitted one-dimensional model M (p, α∗ (γ)) is then back projected perpendicular to the projection axis γ to obtain a reconstruction R(x, y, γ, α∗ (γ)) for the whole image: R(x, y, γ, α∗ (γ)) = M (x · cos γ + y · sin γ, α∗ (γ)) The direction of the anode-cathode axis γ is then determined such that this reconstruction best fits the actual image data within the direct exposure region using γ ∗ = arg min N (x, y) − R(x, y, γ, α∗ (γ))(x,y)∈B (6) γ or γ ∗ = arg min γ N (x, y) − 1(x,y)∈B R(x, y, γ, α∗ (γ)) (7) depending on whether we wish to use additive or multiplicative correction. The estimated heel effect is R(x, y, γ ∗ , α∗ (γ ∗ )) and the corrected image is respectively N̂ (x, y) = N (x, y) − R(x, y, γ ∗ , α∗ (γ ∗ )) (8) 1 2 3 4 5 6 7 Fig. 5. Segmentations of the first 14 images of our database. The direct exposure area is painted white and the collimation area is filled with black. The dark lines are the rejected lines which were candidate collimator edges. or N̂ (x, y) = N (x, y) . R(x, y, γ ∗ , α∗ (γ ∗ )) (9) The optimal parameters α∗ and γ ∗ are found by multidimensional downhill simplex search [9]. We noticed that the anode-cathode axis in our setup is almost always parallel to the image or collimation edges. This reduces the number of orientations which have to be evaluated in (6-7) and reduces computation time. After inhomogeneity correction of the image using (8-9), the direct exposure area B is updated by thresholding, using a threshold derived from the histogram of the corrected image intensities N̂ . Keeping the previously determined anode-cathode orientation γ, new values for the optimal model parameters α∗ are determined using (5) taking the newly selected direct exposure region into account. We thus iterate three or four times between background segmentation and heel effect correction until convergence. The whole algorithm is summarized in Fig. 4. 5 Results The method was tested on 137 digital hand radiographs, recorded with Agfa ADC cassettes and Agfa ADC-MD10 & ADC-MD30 imaging plates and irradiated by X-ray tubes Philips SRM 06 12 - ROT 500 or Siemens Bi 125/40 RL. Results of the image partitioning procedure are shown in Fig. 5. Visual inspection showed that the algorithm was able to correctly extract direct exposure, collimation and diagnostic areas for all images in our database. The time required to perform the partitioning was about 1 to 2 seconds using a Pentium III 800MHz on images resized to about 512 × 512 pixels. The model (4) of the heel effect was verified using a flat field image and an image of a hand phantom (Fig. 6). The heel effect is clearly visible in the flat field image by inspection of intensity traces along both image axes, showing a smooth degradation along the anode-cathode axis and an almost constant behavior perpendicular to this axis. A similar pattern is visible in the traces of the phantom image. Inspection of the traces of the corrected images shows that most of the background intensity variation is indeed eliminated using model (4). Physical models of X-ray production, recording and read-out predict a Gaussian distribution for the intensity of background pixels. This is not the case for the original flat field and phantom images (see histograms of Fig. 6 a,d). However, the (a) Traces (b) (c) Traces Histogram Histogram 2650 2650 2600 Surface Received intensity 2550 2600 2500 2450 50 100 120 100 150 40 20 80 60 Surface 2550 2500 2450 1D model Measured profile 20 40 60 80 100 Position on film 120 140 160 2680 Traces Traces 2660 2700 2650 2640 2600 Received intensity 2620 Histogram 2550 2500 2600 2450 2580 50 100 150 120100 Histogram 40 20 80 60 2560 2540 2520 2500 2480 1D model Measured profile 20 (d) 40 60 80 100 Position on film (e) 120 140 160 (f) Fig. 6. (a) Flat field image (background) rendered as a surface (bottom) with histogram (top-right) and traces (top-left) along the anode-cathode axis (long solid line) and perpendicular to this axis (shorter dotted line). (b) Average projected data of the flat field (dotted line) and the fitted model (solid line). The sub-image contains back projected data (white grid) on top of the rendered background. (c) Same as (a) for the corrected image. (d) Same as (a) for the phantom image without the background surface and traces taken along the white lines. (e) Same as (b) for the phantom image (f) Same as (d) for the corrected phantom image. distribution of the background pixels of the corrected images is almost perfectly Gaussian (Fig. 6 c,f), which is another indication that our model performs very good. The possibly disturbing effect on the estimation of the model parameters α of the presence of diagnostic areas (that may not have been properly removed by the image partitioning procedure) was tested by correcting the flat field image once with parameters computed from the flat field image itself and once with parameters computed from the phantom image. The reconstruction errors for both cases are summarized in table 1. The values for both cases are very similar, which indicates that the algorithm can cope well with the presence of diagnostic regions when estimating the background inhomogeneity. Some selected results on real hand radiographs are shown in Fig. 7. In the first image, the heel effect is clearly visible, while in the second and third example its presence can be detected from the increased background intensity at the bottom right of the images. For all cases the heel effect smears out the histogram of the image intensity of background. The corrected images have better contrast and Table 1. Correction errors = N − R of the flat field image (dynamic range = 800) with model parameters α estimated from either the flat field image itself or from the hand phantom image. α estimated from flat field phantom image -3.10 -5.50 σ 12.42 27.11 min -46.73 -63.93 max 60.78 49.28 their background histogram is Gaussian distributed. After correction, specifying a histogram-derived threshold is sufficient to properly segment the hand, which is not possible for the original images due to the overlap in intensity between diagnostic and background regions. 6 Discussion In this paper we presented a fully automated method for heel effect correction of digital radiographs. We have evaluated the method on a database of hand radiographs on which we were capable of segmenting the hand very accurately after inhomogeneity correction. The method is fast and reliable enough to be used for standardized image display on diagnostic workstations. It can also provide segmentation techniques with properly normalized images whose relative intensity differences are not disturbed by image inhomogeneities. We are currently investigating how this affects the specificity of intensity models constructed for Active Shape Model-based segmentation of the hand bones [2, 3]. The relatively simple theoretical model (4) is able to correct most of the variation present in the direct exposure area of the images that can be attributed to the heel effect. However, in some images in our experiments intensity inhomogeneities could also be perceived in the direction orthogonal to the anode-cathode axis. Future work includes extension of model (4) to two-dimensions. 7 Acknowledgments This work was partly supported by a grant of the Research Fund KU Leuven GOA/99/05 (Variability in Human Shape and Speech). References 1. D. H. Ballard. Generalizing the hough transform to detect arbitrary shapes. Pattern Recognition, 13:111–122, 1981. 2. Gert Behiels, Dirk Vandermeulen, Frederik Maes, Paul Suetens, and Piet Dewaele. Active shape model-based segmentation of digital x-ray images. In MICCAI, pages 128–137, 1999. 3. Gert Behiels, Dirk Vandermeulen, and Paul Suetens. Statistical shape model-based segmentation of digital x-ray images. In IEEE workshop on mathematical methods in biomedical image analysis - MMBIA, pages 61–68, June 2000. 3150 3100 3100 3000 Received intensity 3050 2900 2800 3000 150 100 120 60 80 20 40 100 50 2950 2900 2850 2800 1D model Measured profile 20 40 60 80 100 Position on film 120 140 2500 2500 2400 Received intensity 2450 2300 150 100120 60 80 20 40 100 50 2400 2350 1D model Measured profile 2300 20 40 60 80 100 120 Position on film 140 160 180 2400 2350 2300 Received intensity 2200 2300 120 100 80 60 40 20 20 40 60 80 2250 2200 1D model Measured profile 10 20 30 40 50 60 70 Position on film 80 90 100 110 120 Fig. 7. First column: original images with corresponding background histogram and histogram based background segmentation. Middle Column: 1d projections and back projected model fitted onto image data. Last Column: corrected images with corresponding background histogram and histogram based background segmentation. 4. Shirley N.C. Cheng, Heang-Ping Chan, Loren T. Niklason, and Ronald S. Adler. Automated segmentation of regions of interest on hand radiographs. Med. Phys., 21(8):1293–1300, August 1994. 5. S.L. Fritz and W.H. Livingston. A comparison of computed and measured heel effect for various target angles. Medical Physics, 9(2):216–219, 1982. 6. P. V. C. Hough. Methods and means for recognising complex patterns,. U.S. Patent 3 069 654, Dec 1962. 7. C. Kimme, D. Ballard, and J. Sklansky. Finding circles by an array of accumulators. In Communications of the ACM, volume 18, pages 120–122, 1975. 8. G. Manos, A. Y. Cairns, I. W. Ricketts, and D. Sinclair. Automatic segmentation of hand-wrist radiographs. Image and Vision Computing, 11(2):100–111, March 1993. 9. J. A. Nelder and R. Mead. A simplex method for function minimization. The Computer Journal, 8:308–313, 1965. 10. P. Vuylsteke and E.P. Schoeters. Multiscale image contrast amplification (musica). In M.H. Loew, editor, Proc. SPIE Medical Imaging 1994: Image Processing, volume 2167, pages 551–560, 1994.