Effectiveness of 0.025% Dakin's Solution Versus 1% Silver
advertisement

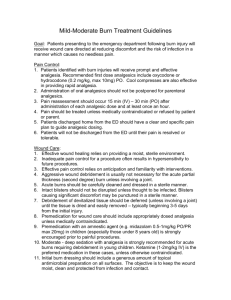
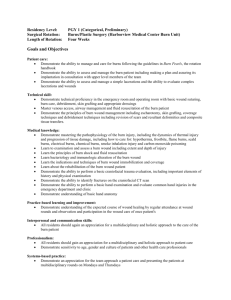
Naheed Ahmed et al Effectiveness of 0.025% Dakin`s Solution Versus 1% Silver Sulphadiazine… Original Article Effectiveness of 0.025% Dakin’s Solution Versus 1% Silver Sulphadiazine for Treatment of Partial Thickness Burns Objective: To evaluate effectiveness of 0.085% Dakin’s solution verses 1% Silver Suplhadiazine in the treatment of partial thickness burns Study Design: Quasi Experimental Study Place and Duration of the Study: The Study was conducted in the burn unit/plastic surgery department, Nishtar Hospital Multan during a period from July, 2008 to December, 2010. Materials and Methods: 30 patients were enrolled with second degree burns at two sites on different parts of the body. Each patient had one burn treated with 0.025% Dakin’s Solution and one treated with 1 % Silver sulphadiazine. Results: The rate wound healing was significantly faster in the site treated with 0.025% Dakin’s Solution than in the site treated with 1 % Silver sulphadiazine. The mean times for healing were 18.73 ± 2.65 and 15.9 ± 2 days for 1 % Silver sulphadiazine and 0.025 % Dakin’s Solution, respectively, being significantly shorter for 0.025 % Dakin’s Solution (P < 0.0001). Conclusion: 0.025% Dakin’s Solution demonstrated the greater efficacy and effectiveness for treating partial thickness burns. Key words: 0.025% Dakin’s Solution, 1 % Silver sulphadiazine , partial thickness burns Introduction 1,2 Burns and scalds form 5-12 % of all traumas. 3 The exact incidence of burns in Pakistan is not known due to non availability or incompleteness of death registration and disease reporting. However, in United 4 States almost two million people burns annually. Burn injury not only damages the normal skin barrier but also impairs host immunological defenses. Because the eschar may be several centimeters or more distant from patent microvasculature, systemically administered antimicrobial agents may not achieve therapeutic levels by diffusion to the wound surface, where microbial numbers are usually greatest. Topically applied antimicrobials provide high concentrations of drug at the wound surface; they penetrate eschar variably, a 5 property that should be considered in their selection. Ann. Pak. Inst. Med. Sci. 2011; 7(3): 127-132 Naheed Ahmed* Muhammad Naveed Shahzad ** Khalid hussain qureshi*** Muhammad Bilal Saeed Faisal Waheed Ahmad Ali FCPS (PLAST)Assistant Professor of Plastic Surgery & Head of Plastic Surgery Department, Nishtar Hospital, Multan **MCPS,FCPS(General surgery) Post Graduate Resident of Plastic Surgery, Nishtar Hospital, Multan ***FCPS(G.surgery)FCPS(URO) Associate Professor of Surgery ,Nishtar Hospital, Multan Address for Correspondence Dr. Naheed Ahmed. Burn Unit Nishtar Medical College & Hospital, Multan Email: naheedahmed1@yahoo.com The goal of prophylactic topical therapy is initially to 6 delay and later to minimize wound colonization. 1% silver sulfadiazine (SSD) cream is the most common topical agent used in the treatment of burns because of 7 its antimicrobial efficacy , but there is the problem of 8 delayed wound healing associated with SSD cream. Currently the most effective topical antibacterial for 9 cleansing a wound is sodium hypochlorite (NaOCl). While povidone-iodine is bactericidal at 1% and 0.5% concentrations, it is toxic to fibroblasts; acetic acid at a 0.25% concentration is not bactericidal but is toxic to fibroblasts; and hydrogen peroxide at 3% and 0.3% concentrations is toxic to fibroblasts but only the 3% 10 concentration is bactericidal. Reducing bacteria counts and supporting the immune response of the host without compromising the activities of proliferative cells would constitute optimal antisepsis. Dilute concentrations of Dakin’s solution from 0.025% to 0.005% have been demonstrated the effective antimicrobial activity without 127 Naheed Ahmed et al Effectiveness of 0.025% Dakin`s Solution Versus 1% Silver Sulphadiazine… any effect on fibroblast activity. In addition, it is extremely inexpensive to produce, and maintains its bactericidal capacity for several days when stored in an 11 opaque, closed container. Realizing the antimicrobial effect of 0.025% Dakin’s solution in burn wound, we designed a comparative study to evaluate the effect of Dakin’s Solution dressing and 1% silver sulfadiazine dressing in second degree burns. By doing this we would be able to find the better modality which will be further helpful in treatment of partial thickness burns. Materials and Methods In our study we used 0.025% Dakin’s Solution. This solution was prepared in the Department of Biochemistry Nishtar Hospital Multan by the joint venture of an experienced biochemist and a pharmacist. This solution was made under the guidelines of US 12 Pharmacopea: • Sodium hypochlorite Solution 0.5 mL • Monobasic sodium phosphate monohydrate 1.02g • Dibasic Sodium Phosphate anhydrous 17.61g • Purified water to 1000mL Study Protocol: This study was a randomized, comparative clinical trial conducted in the burn unit/plastic surgery department, Nishtar Hospital Multan during a period from July, 2008 to December, 2010. After approval of the study protocol from the Institutional Ethical Committee, 30 patients who were willing to participate in the study were enrolled. The inclusion criteria for this trail were as follows: history of the burn within 24 hours of the initiation of treatment; burns affecting two same sites e.g. on the feet or hands; second degree burns with respect to depth; and burns with <40% total burn surface area (TBSA). Patients who had diabetes, hypertension, epilepsy, kidney disease or pregnancy were excluded. Similarly patients with corrosive, electrical and chemical burns were also not included in the study. All burn patients were received in A & E department of Nishtar Hospital Multan where the fluid resuscitation was done and patients were admitted in the burn unit. Wounds were cleaned with pyodine scrub and normal saline and the topical agent either 0.025% Dakin’s solution or 1% SSD cream was applied to the wound. The dressing was changed twice daily. Treatment with topical agents was continued until the burns were fully healed and re-epithelialized. rd generation cephalosporin and BEmpirically, 3 penicillin were started in all patients. Wound swab cultures from three different sites from all patients were taken, at the time of admission and then at every seventh day and then antibiotics were initiated according to the results of bacteriological examination. Ann. Pak. Inst. Med. Sci. 2011; 7(3): 127-132 Relevant data of patients regarding their registration, history, site of the burn, TBSA affected degree of burn, depth of burn, presence or absence of slough in the wound, medical report, operative notes, pre- and postoperative photographs, duration of hospital stay and outcome were filed individually. During their stay in ward, Strict monitoring of intake/ output was done. Where indicated, we supported our patients with blood products. In all the patients, great care was given to nutrition. Almost all the patients were given oral nutrition with occasional intravenous support in the form of amino acid infusion in few patients. At the time of change of dressing details regarding the condition of the wound such as signs of wound infection, condition of surrounding unburned tissues, discharge, smell, necrotic tissue and state of epithelialisation was noted by our consultant burn rd surgeon on every 3 day. Subjective factors such as pain and local irritation were recorded regularly. Allergies or other side effects were noted in both groups. The patients and attendants were given information regarding the Dakin’s Solution and 1%silver sulphadiazine cream. All the data were analyzed using SPSS 11 software. The Student t-test and analysis of variance test were used to compare the study groups, wound size, and healing time. Significance level was determined as less than 0.05. In this study, the “B” part of the body was treated with 1 % Silver Sulfadiazine and the “A” part was treated with 0.025% Dakin’s Solution. Patients and nursing staff were blinded to the 28 procedure. We followed the method of Flanagan M. for measuring Wound Length, Width, and Area. We measured the longest length and width, regardless of head-to-toe orientation and multiplied the 2 measurements to obtain the area in squared 2 centimetres (cm ), i.e. Area (in centimetre square) = length x width 29 We measured the wound progression by calculating percentage rate of change by a simple statistical calculation that uses the following formula: 1. Baseline (week 0) wound size (OA or overall OA size) measurement as the original size. 2. Subtract the next wound size OA or overall OA size measurement (interim) taken from the baseline. 3. Divide by baseline wound measurement and multiply by 100 %. Formula for Healing percentage in burn wound. nd Wound area an admission day - Area on 2 time x 100% Baseline wound area an admission day Results The effectiveness of 0.025 % Dakin’s Solution was compared with 1% silver sulfadiazine in this trial. 128 Effectiveness of 0.025% Dakin`s Solution Versus 1% Silver Sulphadiazine… There was no mortality recorded in our study. To minimize the confounding variables, only those patients who had partial thickness burns of the hands or feet with similar extent and the size of the burn at both sites were selected. With this randomization, one site was treated with SSD cream and the other site was treated with 0.025% modified Dakin’s Solution. Out of 30 patients, 18 patients reported within 916 hours of burn, 5 patients came to the hospital within 1-8 hours of burn, 3 patients in < 1hour, while 4 patients came within 17-24 hours of burn. Other demographic characteristics of our patients with Burns are summarized in Table I. Table I :Demographic Characteristics Gender No of Percentage cases 25 56.81% 5 43.19 % Male female Age of Patients 14-20 years 6 13.63% 21-30 years 20 45.45% 31-40 years 6 13.63% 41-50 years 3 9.09% 51-60 years 6 13.63% > 60 years 3 9.09% Minimum age of the patient included in our study=15 years Maximum age of the patient included in our study=65 years Mean age + =33.59 + 15 TBSA 10 -20 % 14 31.8% 21 -30 % 22 50% 31 -40 % 8 18.2 % Mean + SD TBSA 19.8+ 7.9 Time of Admission <1 hour 3 6.81% 1-8 hours 5 11.36% 9-16 hours 26 59.1% 17-24 hours 10 22.7% Site of burns Right and left hand 26 (87%) Right and left foot 2 (7%) Right or left hand or 2 (7%) arm / right and left foot or leg Naheed Ahmed et al Table II: Time of healing after treatment with 0.025 % Dakin’s Solution versus silver sulfadiazine (SSD) Time for complete healing <10 days <13 days <16 days <19 days Mean healing period ± SD (days) P value No. of patients SSD group 0.025% Dakin’s (n = 30) Solution group (n = 30) 1 2 2 5 7 25 24 30 18.73 ± 2.65 15.9 ± 2 <0.0001 Table III: Comparison of wound burn sizes in the silver sulfadiazine and 0.025 % Dakin’s Solution groups. The wound size was defined as 100% on day 4 and then calculated and compared with day 4 thereafter Days Comparison of wound burn sizes In After percentage Burns 0.025 % Dakin’s SSD group Solution group (n = (n = 30) 30) Day Wound size 100 % Wound size 100 % as 4 as on day 1 on day 1 No change /healing No change /healing Day Wound size 100 % Wound size 100 % as 7 as on day 1 on day 1 Healing started but Healing started but wound size is not wound size is not changed changed Day Wound size started Wound size 100 % as 10 to decrease on day 1 80-100 % as on day 1 Healing started but wound size is not changed Day Wound size 50-80 % Wound size started to 13 as on day 1 decrease 90-100 % as on day 1 Day Wound size 10-50 % Wound size 80 % or 16 as on day 1 more as on day 1 Day Complete healing Wound size 50 % or 19 more as on day 1 Day Wound size 30 % or 21 more as on day 1 Day Wound size 10-30 % 21 as on day 1 Complete healing = day 32 The mean times for healing were 18.73 ± 2.65 and 15.9 ± 2 days for SSD and 0.025 % Dakin’s Ann. Pak. Inst. Med. Sci. 2011; 7(3): 127-132 129 Effectiveness of 0.025% Dakin`s Solution Versus 1% Silver Sulphadiazine… Table IV: Comparison of the effectiveness of daily dressings with 0.025 % Dakin’s Solution and with 1% silver sulfadiazine Criteria for cure Time taken for 0.025 % Dakin’s Solution to show 100%cure Time taken for SSD to show 100%cure Wound Healing (mean ± SD; days) Negative bacterial culture 18.73 ± 2.65 15.9 ± 2 1 week Less than 3 weeks Solution, respectively, being significantly shorter for 0.025 % Dakin’s Solution (P < 0.0001; Table II). The sites treated with 0.025 % Dakin’s Solution healed approximately 3 days sooner than the sites treated with SSD in all the patients. In fact, wound healing took less than 16 days in 83% of the sites treated with 0.025 % Dakin’s Solution, but more than 19 days in the sites treated with SSD. The average wound size at 4, 7, 10, 13, 16, 19, 21, and 24 days after burn injury were measured. With this trend, the percentage of each wound size was calculated by reducing the fraction of the second to the first wound size (cm2). There was a significant difference between the 0.025 % Dakin’s Solution group and the SSD group 10, 13, and 16 days after treatment (P < 0.01). (Table III) The mean times for healing were 18.73 ± 2.65 and 15.9 ± 2 days for SSD and 0.025 % Dakin’s Solution, respectively, being significantly shorter for 0.025 % Dakin’s Solution (P < 0.0001; Table 2). The sites treated with 0.025 % Dakin’s Solution healed approximately 3 days sooner than the sites treated with SSD in all the patients. In fact, wound healing took less than 16 days in 83% of the sites treated with 0.025 % Dakin’s Solution, but more than 19 days in the sites treated with SSD. The average wound size at 4, 7, 10, 13, 16, 19, 21, and 24 days after burn injury were measured. With this trend, the percentage of each wound size was calculated by reducing the fraction of the second to the first wound size (cm2). There was a significant difference between the 0.025 % Dakin’s Solution group and the SSD group 10, 13, and 16 days after treatment (P < 0.01). (Table III) The surfaces of both sites were swabbed to test for microbial contamination on days 3, 7, and 13, and was found to be negative in 0.025 % Dakin’s Solution Ann. Pak. Inst. Med. Sci. 2011; 7(3): 127-132 Naheed Ahmed et al group after 7th day while The swabs were positive for bacterial growth in 80% of the patients at 7th day and 30 % on 13th day and after 21 days wound became sterile in SSD group. (Table IV) There was significant difference of cost of treatment. The cost of treatment per percent body surface burnt per dressing of 1% silver sulfadiazine was Rs. 60 for 1 grams of ointment. As against of this, cost of 0.025% Dakin’s Solution dressing was amazingly low costing only RS.50 / gallon. Figure I: A young male of 34 having burns of feet ,ankle and leg area .Side treated with silver sulphadiazine show wounds while better healing can be seen on the side where 0.025 % Dakin’s Solution dressing was done Figure II: A lady of 45 years showing better healing on the dorsum of the right hand which was treated with 0.025 % Dakin’s Solution dressing 130 Naheed Ahmed et al Effectiveness of 0.025% Dakin`s Solution Versus 1% Silver Sulphadiazine… Discussion The normal wound repair process is coordinated and predictable series of cellular and biochemical events. However certain pathophysiological conditions alter this pre-programmed course of events so that wound healing can be enhanced or impeded. Presence of necrotic tissue not only inhibits wound healing but it deepens wounds through extensive inflammatory response. So removal of necrotic tissue is extremely 13-16 and essential to prevent and diminish wound sepsis enhance wound healing. The antimicrobial effect of silver sulfadiazine is the only mechanism justifying its continued use in burn 17 injury. How ever resistance has been demonstrated. Hepatic or renal toxicity and leukopenia may be caused by the topical application of SSD. In fact, these side effects have been observed in the treatment of large 13 wounds. Dakin and Carrel developed sodium hypochlorite 18-20 solution; Bunyan used it in the treatment of burns. The use of sodium hypochlorite solution in treatment of burns diminished with the availability of antibiotics 21 mafenide acetate and silver sulfadiazine. However, some burn centres continue to use dilute NaOCl in 22 hydrotherapy. Sodium hypochlorite as a dilute solution is attractive as a topical agent for a variety of reasons. • It is cheap than any of the currently available topical agents used in burn therapy • It is easy to prepare • At dilute concentrations (0.025 %) NaOCl kill virtually all of the microorganisms known to infect burn patients, and there has been no evidence that microorganisms can develop resistance to its action. Although the precise microbicidal action of NaOCl has not been fully established, it is currently believed that the oxidation of sulfhydryl groups on essential enzymes by chlorine is responsible for cell 23 death. Since this is a multitarget system, the chances of resistant mutants arising are quite remote. • NaOCl is known to reduce oedema and inflammation, and it does not appear to affect granulation tissue or reepithelialisation of the burn 18-19 wound. • The proteolytic action of NaOCl causes rapid 24 breakdown of dead tissue. Sodium hypochlorite (0.5% or 0.25% NaOCl) solution is considered a general bactericidal (e.g., Staphylococci and Streptococci), fungicidal, and veridical agent. Concentrations as low as 0.025% has also demonstrated bactericidal effects. The bactericidal effects are the suggested rationale for aiding wound healing. Sodium hypochlorite at 0.25%, however, has Ann. Pak. Inst. Med. Sci. 2011; 7(3): 127-132 25-28 26,29 and keratinocytes displayed toxicity to fibroblasts in culture. Polymorphonuclear leukocyte viability is also 30 inhibited by this topical agent. Sodium hypochlorite solutions of 0.5% would be expected to demonstrate at least these same levels of toxicity. Tissue toxicity was 25 not observed at concentrations of 0.025%. In 1991 Herndon DN, noted that sodium hypochlorite solution as 31 low as 0.025 % had Bactericidal effects. Burn patients have a higher morbidity than mortality because burn wound, due to the presence of necrotic tissue, has great chances of infection and thus require long periods of 32 dressings, leading to deformities and contracture. Delayed reporting has been found to be an important factor that causes an increase in wound infection and 33 thus morbidity. This is a major problem in the third world countries like Pakistan, owing to poor transport condition, illiteracy and relative inaccessibility of tertiary health-care centres. Conclusion 0.025% Dakin’s Solution demonstrated the greater efficacy and effectiveness for treating partial thickness burns. References 1. Olaitan PB, Olaitan JO. Burns and Scalds-epidemiology and prevention in a developing country. Niger J Med 2005;14(1):9-16. 2. Gudaviciene D, Rimdeika R, Adamonis K. Nutrition of burned patients. Medicina (Kaunas) 2004;40(1):1-8. 3. Jamil H, Khalil F, Saeed M. Etiology and Outcome of burn victims in a tertiary care facility. J Sur (PIMS) 2002;(25):1. 4. Garner WL, Magee W. Acute burn injury. Clin Plast Surg 2005;32(2):187-93. 5. Bessey PQ .Wound care In:Herndon DN, editor. Total Burn Care.3rd edition. China: Saunders Elsevier Inc; 2007.p. 131. 6. Monafo WW, West MA. Current treatment recommendations for topical burn therapy. Drugs 1990; 40(3):364–373. 7. Vloemans AFPM, Soesman AM, Suijker M,et al. A randomized clinical trial comparing a hydrocolloid-derived dressing and glycerol preserved allograft skin in the management of partial thickness burn. Burns 2003;29:702–10 8. Gallagher JJ, Williams-Bouyer N, Villarreal C, Heggers JP, Herndon DN. Treatment of infection in burns.In:Herndon DN,editor. Total Burn Care.3rd edition. China: Saunders Elsevier Inc; 2007.p. 170 9. Lindberg RB, Moncrief JA, Mason AD Jr. Control of experimental and clinical burn wound sepsis by topical application of sulfamylon compounds. Am NY Acad Sci 1968; 150:950. 10. Heggers JP, Robson MC eds. Quantitative bacteriology: its role in the armamentarium of the surgeon. 1st edn. Boca Raton, FL, CRC;1991:139 11. McKenna, P., Lehr, G., Leist, P., Welling, R. (1991) Antiseptic Effectiveness with Fibroblasts Preservation. Annals of Plastic Surgery, 27 265-268. 12. Allen LV.Allen's compounded formulations: the complete U.S. pharmacist collection. American Pharmaceutical Association, 2003.p.167. 131 Effectiveness of 0.025% Dakin`s Solution Versus 1% Silver Sulphadiazine… 13. Murphy JT, Duffy S, Prudue GF et al. Thermal injury altersendothlielial vasoconstrictor and vasodilator response to endotoxin.J Truama 1999;47(3):492. 14. Lu S, Xiang L, Quing C ,et al. Effect of necrotic tissue on progressive injury in deep partial thickness burn wounds. Chin Med J 2002;115(3):323-5. 15. Reynolds N, Cawrse N, Burge T et al. Debridement of a mixed partial and full thickness burn with an erbium:YAG laser.Burns 2002;29(2):183-8. 16. Epstein AM. The outcomes movement—will it get us where we want to go? N Engl J Med 1990;323:266–70. 17. Lansdown AB. Silver. I: Its antibacterial properties and mechanism of action. J Wound Care 2002; 18. Bunyan, J. 1941. The treatment of burns and wounds by the envelope method. Br. Med. J. 2:1-7. 19. Bunyan, J. 1960. Use of hypochlorite for the control of bleeding.Oral Surg. Oral. Med. Oral Pathol. 13:1026-1031. 20. Flanagan M. Wound Management. Churchill Livingstone: Edinburgh; 1997. 21. Moncrief, J. A. 1974. Topical antibacterial therapy of the burn wound. Clin. Plastic Surg. 1:563-576. 22. Rodeheaver, G., W. Bellamy, M. Kody, G. Spatafra, L. Fitton, K. Leyden, and R. Edlich. 1982. Bactericidal activity and toxicity of iodinecontaining solutions in wounds. Arch. Surg.117:181-186. 23. Knox, W. E., P. K. Stumpf, D. E. Green, and V. H. Auerbach. 1948. The inhibition of sulfhydryl enzymes as the basis of the bactericidal action of chlorine. J. Bacteriol. 55:451-458. 24. Morgan, O., F. Saner, and E. Schlesinger. 1917. Some aspects of the treatment of the infected war wounds. Br. J. Surg.5:425-461. Ann. Pak. Inst. Med. Sci. 2011; 7(3): 127-132 Naheed Ahmed et al 25. Heggers JP, Sazy JA, Stenberg BD, et al. Bactericidal and woundhealing properties of sodium hypochlorite solutions: the 1991 Lindberg Award. J Burn Care Rehabil. 1991;12: 420-424. 26. Kozol RA, Gillies C, Elgebaly SA. Effects of sodium hypochlorite (Dakin's solution) on cells of the wound module. Arch Surg. 1988; 123:420-427. 27. Lineaweaver W, McMorris S, Soucy D, Howard R. Cellular and bacterial toxicities of topical antimicrobials. Plast Reconstr Surg. 1985;75:394-396. 28. Smoot EC, Kucan JO, Roth A, et al. In vitro toxicity testing for antibacterials against human keratinocytes. Plast Reconstr Surg. 1991; 87:917-924. 29. Cooper ML, Boyce ST,. Hansbrough JF, et al. Cytotoxicity to cultured human keratinocytes of topical antimicrobial agents. J Surg Res. 1990;48:190-195. 30. Hansbrough JF, Zapata-Sirvent RL, Cooper ML. Effects of topical antimicrobial agents on the human neutrophil respiratory burst. Arch Surg. 1991;126:603-608. 31. Herndon DN. Robson MC. Bactericidal and wound-healing properties of sodium hypochlorite. Journal of Burn Care & Rehabilitation.1991; 12(5):420-4. 32. Subrahmanyam M. Honey dressing versus boiled potato peel in the treatment of burns: A prospective randomized study. Burns 1996;22:491-3. 33. Ozbek S, Ozgenel Y, Etoz A, Akin S, Kahveci R, Heper Y, et al. The effect of delayed admission in burn centers on wound contamination and infection rates. Ulus Travma Acil Cerrahi Derg 2005;11:230-7. 132