CARDIOVASCULAR SYSTEM AND CONTROL OF BLOOD SUPPLY
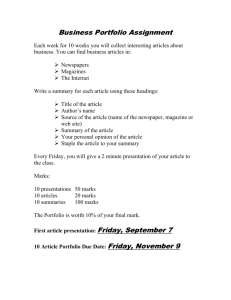
advertisement

CARDIOVASCULAR AND CONTROL OF BLOOD SUPPLY CARDIOVASCULAR SYSTEM AEROBIC - A process taking place in the presence of Oxygen ANAEROBIC - A process taking place in the absence of Oxygen AEROBIC SYSTEM - Provides energy for prolonged work and consists of 3 body systems: the heart, vascular system and respiratory system AEROBIC CAPACITY - The ability to supply and use Oxygen to provide the energy for prolonged periods (limited by the efficiency of the 3 systems) OXYGENATED - Blood saturated/loaded with Oxygen DEOXYGENATED - Blood depleted of Oxygen Structure and Function of the Heart The Heart’s structure includes the following: Septum – separates the left and right side Valves that control forward motion of blood flow through the Heart and prevents backflow of blood within the Heart chambers o Atrioventricular (AV) Valves Bicuspid – separates the left Atrium and left Ventricle Tricuspid – separates the right Atrium and right Ventricle o Semi-Lunar (SL) Valves Pulmonary Valve – exits the right Ventricle into the Pulmonary Artery Aortic Valve – exits the left Ventricle into the Aorta Superior and Inferior Vena cavae – deoxygenated blood from the body to the Heart Pulmonary Artery – deoxygenated blood from right ventricle to the lungs Pulmonary Veins – oxygenated blood from the lungs to the left atrium Aorta – oxygenated blood from the left ventricle to the whole body Coronary Arteries – left and right branches from the Aorta encircle and supply the Heart muscle with oxygen and glucose Coronary Veins – drain deoxygenated blood directly back into the right atrium via the coronary sinus 1 Conduction System The electric impulse responsible for stimulating the heart to contract is called the Cardiac Impulse The heart is said to be Myogenic as it generates its own electrical impulse The Cardiac Impulse is initiated by the sino-atrial (SA) Node (also known as the Pacemaker) which is found in the posterior wall of the right atrium The impulse travels through the atria and cause them to contract The ventricles are not stimulated yet as they are insulated from the atria The impulse reaches the Atrioventricular (AV) Node in the right atrium which passes the impulse down the Bundle of His found in the septum This then splits down the left and right reaching the ventricle walls via a network of Purkinje Fibres which cause the ventricles to contract Cardiac Cycle This is one heartbeat which lasts 0.8 seconds and repeated about 72 times a minute It is split into 2 phases: o Diastole lasting 0.5 seconds (the Relaxation Phase) o Systole lasting 0.3 seconds (the Contraction Phase) The Cardiac Cycle follows these events: DIASTOLE Both Atria fill with blood. AV Valves closed Atrial blood pressure rises above Ventricular pressure Atrial blood pressure forces AV Valves open and blood passively passes into both ventricles. SL Valves closed SYSTOLE Both atria contract actively forcing the remaining atrial blood into the ventricles. SL Valves remain closed Both ventricles contract. Increasing ventricular pressure SL Valves open. AV Valves closed Blood then travels to the Lungs and the whole Body Diastole begins. SL Valves close to prevent backflow of blood 2 Describe the link between the Cardiac Cycle and the Conduction System Resting Heart Rate – Volumes and Definitions HEART RATE - - - STROKE VOLUME - - CARDIAC OUTPUT - The number of times the Heart ventricles beats in one minute. The average resting HR is 72 beats per minute (bpm). The maximum HR is calculated by subtracting your age from 220. Low resting HR may indicate a high level of aerobic/endurance fitness. Highly trained athletes can have a resting HR as low as 28 bpm A resting HR below 60 bpm is termed bradycardia (or slow HR), due to increase in Stroke Volume due to an increase size of the heart muscle (called hypertrophy) The volume of blood ejected from the ventricles every beat This is the difference in volume of blood in the ventricles before and after the ventricles contract The following terms are used to measure SV: End-diastolic volume (EDV) – volume of blood in ventricles at the end of relaxation phase (before contraction) End-systolic volume (ESV) – volume of blood in ventricles at the end of contraction phase (before contraction) Resting EDV is about 130ml; resting ESV is about 60ml. Therefore, resting SV is about 70ml The volume of blood ejected by the heart ventricles in one minute (can also be called Q) The resting value is about 5 litres per minute (L/min) Q = SV x HR (L/min) (ml per beat) (beats per min) Heart Rate Response to Exercise STROKE VOLUME RESPONSE TO EXERCISE As an athlete starts running, their SV increases linearly as their running speed/intensity increases (only up to 40-60% of max running speed). SV will then reach a plateau SV is determined by the heart’s ability to fill and empty each beat. Ability of heart to fill is dependent on: o Venous return – SV increases due to an increase in blood returning to the heart o The ventricles are able to stretch further 3 Ability of heart to empty is dependent on: o Greater EDV provides a greater stretch on the heart walls o A greater stretch increases the force of ventricular systole (contraction of ventricles) These increase ventricular contractility (capacity of the ventricles to contract) which almost completely empties the blood from the ventricles During exercise EDV = 130ml; ESV = 10ml; therefore SV = 120ml HEART RATE - HR will change before, during and after exercise depending on the exercise being taken HR will increase above resting values before exercise takes place. This is called the anticipatory rise which is the early release of adrenaline which stimulates the SA node to increase HR HR increases as exercise intensity increases but slows down just before maximal HR values HR decreases as exercise intensity decreases HR reaches a plateau during sub-maximal work, which represents the optimal steady state HR for meeting the demand for oxygen at that specific intensity of work HR decreases rapidly after exercise stops due to a decrease in demand for oxygen by the working muscles A more gradual decrease in HR towards resting levels, but still elevated to allow the body to recover – this is oxygen debt (additional oxygen consumption during recovery, above that usually required when at rest) CARDIAC OUTPUT (Q) Increases directly in line with exercise intensity from resting values of 5 L/min to maximal values of 20-40 L/min in highly trained endurance athletes Q primarily increases to supply the increase in demand for oxygen from our working muscles When exercise intensity exceeds 40-60% of an athlete’s maximal exercise intensity, SV begins to plateau. Any further increase in Q is a result of an increase in HR Here is a summary of HR, SV and Q values related to exercise intensity: Value SV HR Q Resting 60 - 80ml 80 - 110ml 70 - 72bpm 5 L/min EXERCISE INTENSITY Sub-maximal Maximal 80 - 100ml untrained 100 - 120 untrained 160 - 200ml trained 160 - 200 trained Up to 100 -130ml 220 minus your age Up to 10 L/min 20 - 40 L/min 4 Heart Rate Regulation and Control CARDIAC CONTROL CENTRE (CCC) This is found in the medulla oblongata in the brain It is primarily responsible for regulating the heart and is controlled by the autonomic nervous system (ANS) This means that it is under involuntary control and consists of sensory nerves (nerves that transmit information to the Central Nervous System – from receptors to the CCC) and motor nerves (nerves that stimulate muscle tissue causing motor movement) Sympathetic nerves increase HR whilst Parasympathetic nerves decrease HR Each cardiac cycle is controlled by the initiation of the SA node. The CCC initiates the sympathetic or parasympathetic nervous systems to stimulate the SA node to either increase or decrease HR FACTORS AFFECTING THE CCC - There are 3 main factors affecting the CCC Neural Control Hormonal Control Intrinsic Control NEURAL CONTROL - Proprio-receptors in muscles, tendons and joints inform the CCC that motor (movement) activity has increased Chemoreceptors detect chemical changes in the aorta and carotid arteries and inform the CCC that lactic acid and CO2 levels have increased and O2 and pH levels have decreased Baroreceptors detect stretch within blood vessel walls, in aorta and carotid arteries and inform the CCC that blood pressure has increased - - The CCC responds to the above neural information by stimulating the SA node via the sympathetic cardiac accelerator nerve to increase HR and SV When exercise stops, all above neural factors are reversed gradually and the CCC increases stimulation via the parasympathetic vagus nerve for the SA node to decrease HR HORMONAL CONTROL - Before and during exercise, adrenalin is released within the blood stream. Adrenalin stimulates the SA node to increases both HR and strength of ventricular contraction (which increases SV) 5 INTRINSIC CONTROL - DURING EXERCISE - - AFTER EXERCISE - There are a number of intrinsic/internal factors that affect HR control during and after exercise Temperature increases, which increases the speed of nerve impulses, which in turn increases HR Venous return (blood returning to the heart) increases HR which directly increases EDV and therefore SV (Starling’s Law – SV dependent upon venous return = any increase in VR causes an increase in SV and Q) Temperature decreases and HR decreases Venous return decreases, which in turn decreases SV (Starling’s Law) 6 CONTROL OF BLOOD SUPPLY Circulatory Networks SYSTEMIC CIRCULATION - Oxygenated blood from the left ventricle to the body tissues and deoxygenated blood back to the right atrium PULMONARY CIRCULATION - Deoxygenated blood from the right ventricle to the lungs and oxygenated blood back to the left atrium Arteries are the largest blood vessels, as they get further away from the heart they reduce in size to become arterioles and finally into capillaries (one cell thick to allow gaseous exchange) Capillaries then flow into larger venules and then into even larger veins before entering the right atrium from either the superior vena cava (from the upper body) or inferior vena cava from the lower body Arteries normally carry oxygenated blood and veins normally carry deoxygenated blood – this is true with the exception of the Pulmonary Artery (carries deoxygenated blood) and the Pulmonary Vein (carries oxygenated blood) Blood Vessel Structure BLOOD VESSELS Arteries transport oxygenated blood away from the heart and towards tissue/muscles Veins transport deoxygenated blood back to the heart Capillaries bring blood directly into contact with the tissues where O2 and CO2 are exchanged All blood vessels have 3 layers (apart from single-walled capillaries) Arteries and arterioles have a large middle layer of smooth muscle (involuntary muscle within blood vessel walls) to allow them to vasodilate (widening of arteries) and vasoconstrict (narrowing of arteries) to regulate blood flow Arterioles have a ring of smooth muscle surrounding the entrance to the capillary networks to control blood flow. These are pre-capillary sphincters, they vasodilate and vasoconstrict to regulate blood flow Larger veins have pocket valves to prevent backflow of blood and direct blood back to the heart Venules and veins have a thinner muscular layer allowing them to venodilate (widening of veins) and venoconstrict (narrowing of veins) and a thicker outer layer to help support the blood that sits within each pocket valve 7 Venous Return (VR) This is the transport of blood from the capillaries through venules, veins and back to the heart STARLING’S LAW - - This states that stroke volume is dependent upon venous return. If VR increases, SV increases. If VR decreases then SV decreases. If SV increases or decreases, so does Q. Therefore, VR will determine SV and Q At rest VR is sufficient to maintain SV and Q to supply the demand for O2. During exercise the pressure of blood in the veins is too low to maintain VR and then SV and Q decrease. Therefore the body needs additional mechanisms to help blood return to the heart against gravity to increase VR and so SV Venous Return Mechanisms Pocket Valves - Muscle Pump - Respiratory Pump - Smooth Muscle - Gravity - Prevent backflow of blood and direct it back to the heart Veins are situated between skeletal muscle which help push blood back to the heart when they contract and relax Pressure changes in the thorax and abdomen during exercise. The increase in pressure in the abdomen, squeezes large veins in that area and forcing blood back to the heart Contraction and relaxation of smooth muscle in the middle layer of veins helps push blood back to the heart Blood from the upper body is aided by gravity as it descends to the heart Blood Pooling VR requires a force to push the blood back to the heart. If there is insufficient force then the blood will sit in the pocket valves in the veins. This is Blood Pooling At rest gravity, pocket valves and smooth muscle are enough to maintain VR at rest, but not during or immediately after exercise Therefore, the skeletal and respiratory pumps are needed to maintain VR during exercise and immediately after exercise In order for this to happen, an active cool down must take place to maintain these two pumps and help maintain VR and redistribute Q to prevent blood pooling 8 Venous Return’s Impact on the Quality of Performance Venous Return (VR) is important to performance as it determines SV and Q. If SV/Q decreases, oxygen transport to the working muscles decreases, which reduces the ability to contract/work aerobically. The impact on performance is that exercise intensity has to be reduced or muscles will have to work anaerobically, which will result in muscle fatigue. A good VR in anaerobic activities will speed up recovery and therefore allow performers to work anaerobically for longer. Distribution of Cardiac Output at Rest and during Exercise The process of redistributing Q is called the vascular shunt mechanism Below is a table of the distribution of Q and then where and how it is redistributed during exercise: TISSUE Liver Kidneys Brain Heart Muscle Skin Other Total Distribution of Q during light, moderate and maximal exercise REST LIGHT MODERATE MAXIMAL (%) (ml) (%) (ml) (%) (ml) (%) (ml) 27 1350 12 1100 3 600 1 300 22 1100 10 900 3 600 1 250 14 700 8 750 4 750 3 750 4 200 4 350 4 750 4 1000 20 1000 47 4500 71 12500 88 22000 6 300 15 1500 12 1900 2 600 7 350 4 400 3 500 1 100 100 5000 100 9500 100 17600 100 25000 At Rest: o Only 15-20% resting Q is supplied to working muscles o Remaining Q (80-85%) supplies body organs During Exercise: o Increased Q (80-85%) supplied to working muscles as exercise intensity increases o Decreasing % of Q supplied to body organs o Blood supply to the brain is maintained o Increased blood supply to the skin surface during light work, but decreased as exercise intensity increases Vasomotor Control Centre The vascular shunt mechanism redistributes Q during rest and exercise and is controlled by the Vasomotor Control Centre (VCC) found in the medulla oblongata 9 It stimulates the sympathetic nervous system to either vasodilate or vasoconstrict the pre-capillary sphincters and arterioles supplying muscles and organs VCC receives information from: o Chemoreceptors in muscles, aorta and carotid arteries which inform VCC that latic acid and CO2 levels have increased and O2 and pH levels have decreased o Baroreceptors in aorta and carotid arteries which inform VCC that systolic blood pressure has increased/decreased Organs (during exercise) – The VCC controls blood flow by increasing sympathetic stimulation which vasoconstricts arterioles and pre-capillary sphincters which decreases blood flow to non-essential organs Muscles (during exercise) – The VCC controls blood flow by decreasing sympathetic stimulation which vasodilates arterioles and pre-capillary sphincters which increases blood flow to the capillaries to the working muscles Oxygen and Carbon Dioxide Transport Oxygen Transport - 97% transported within the protein haemoglobin in red blood cells (RBC). When combined together they make oxyhaemoglobin (HbO2) 3% within blood plasma - Haemoglobin has a high affinity for oxygen and will carry it when available, but give it to tissue’s that have low concentrations of oxygen. Each Haemoglobin molecule can carry four molecules of oxygen. Carbon Dioxide Transport 70% combined with water in RBC’s as carbonic acid 23% combined with haemoglobin as carbaminohaemoglobin (HbCO2) 7% dissolved in plasma - Effective Transportation of Carbon Dioxide and Oxygen within the Vascular system aids Participation in Physical Activity Efficient transportation of Oxygen and Carbon Dioxide aids participation in the following ways: Prolongs the duration of anaerobic and especially aerobic activity Delays anaerobic threshold, which Increases the possible intensity/work rate for the activity Speeds up recovery during and after exercise 10 Smoking Affects the Transportation of Oxygen Cigarette smoke contains Carbon Monoxide (CO). Haemoglobin has a higher affinity (240+ times) to CO and therefore combines with CO in preference to O2. This reduces the HbO2 association in the lungs and therefore the performer’s maximal uptake. As a result, less O2 is supplied to the working muscles and the lactate threshold decreases which both decrease optimal performance. Warm-Up – Effects on Vascular System Gradual increase in blood flow/Q due to vascular shunt mechanism Vasoconstriction of arterioles/pre-capillary sphincters to organs, decreasing blood flow to the organs and thereby increasing blood flow to the working muscles Vasodilation of muscle arteriole/pre-capillary sphincters, which increases the blood flow delivery to the working muscles Increased body/muscle temperature causing a more rapid increase in transport of the enzymes required for energy systems and muscle contraction Increase in body/muscle temperature o Decreases blood viscosity which improves blood flow to working muscles o Increases the release of oxygen from haemoglobin Decrease in OBLA (Onset of Blood Lactate Accumulation) due to early anaerobic work when a warm up is not carried out Cool-Down – Effects on Vascular System Keeps metabolic activity elevated which gradually decreases HR and respiration Maintains respiratory and muscle pumps (prevents blood pooling in veins; and maintains venous return) Maintains blood flow to maintain blood pressure Keeps capillaries dilated to flush muscles with oxygenated blood, which increases removal of lactic acid and CO2 Blood Pressure Blood Pressure is caused by the contractive force of the ventricles forcing blood through the arteries Definition – The pressure exerted by blood against the (arterial) blood vessel walls Blood Pressure (BP) is normally expressed as below: Systolic Diastolic 11 Systolic blood pressure represents the highest arterial pressure and reflects ventricular systole. Diastolic blood pressure represents the lowest arterial pressure and reflects ventricular diastole Resting Values – The average resting BP is 120mmHg (in the aorta) 80mmHg (mmHg = millimetres of Mercury) BP is also expressed as “blood flow (Q) X resistance”. Therefore, if Q is increased, so is blood pressure. RESISTANCE - - - BP MEASUREMENT - This is the friction of the blood cells as they travel against the vessel wall which is termed VISCOSITY (fluid friction). BP will decrease when arteries dilate (widening) and BP will increase when arteries constrict (narrowing). This controls the redistribution of blood via the vascular shunt mechanism BP is measured using the sphygmomanometer BP Changes that Occur During Physical Activity and Hypertension BP changes for lots of reasons; but generally BP: Decreases when we are asleep Increases temporarily during stress Increases with age Increases in hot temperature Decreases in cold temperature BP During Exercise (Endurance training) SYSTOLIC - Systolic BP increases in line with exercise intensity and will plateau or steady-state during sub-maximal exercise (about 140160), but may decrease gradually if this sub-maximal intensity is prolonged As exercise intensity increases, systolic BP continues to increases in line with intensity, from 120mmHg to above 200mmHg during exhaustive exercise intensity. Systolic BP of 240-250 have been reported in elite athletes at maximum exercise intensity DIASTOLIC - Diastolic BP changes little during sub-maximal exercise, irrespective of intensity. During gross muscle activities like rowing and running, localised muscular diastolic BP may fall to around 60-70mmHg. Diastolic BP may increase a little (max 12% or >10mmHg) as exercise intensity reaches maximum levels 12 Isometric/Resistance Training Lifting heavy weights during strength/resistance training involves isometric work |during isometric work, blood vessels are blocked due to sustained static muscle contractions which restricts the blood flow through arterial and venous blood vessels; thus increasing vascular resistance This can cause an increase in systolic and diastolic BP as blood flow builds up behind this area of restriction, and BP can exceed 480/350mmHg The Valsalva manoeuvre often occurs during this type of exercise (when an athlete attempts to breathe out while the mouth and nose are closed). This type of exercise is not recommended for individuals already prescribed as hypertensive Resting BP after resistance training tends not to change, but may decrease Post-Exercise Recovery Systolic BP decreases temporarily below pre-exercise levels for up to 12 hours Diastolic BP also remains low, often below normal resting levels and can remain low for hours afterwards This may have an important application in promoting a healthy lifestyle in that it may help lower BP, as exercising more regularly can reduce BP on a daily basis and this is more significant in individuals who are already hypertensive Long-Term Changes Any reasons behind long-term adaptations to BP are still not fully understood; but are likely to be due to changes in: CV adaptations Diet Smoking Weight Stress The following points are relevant: Mixed views that resting BP may decrease with continued endurance training Resting BP is generally lowered in people already with mild or moderate hypertension Endurance training can reduce the risk of developing high BP BP changes little during sub-maximal or maximal work rates Although resistance/isometric training significantly increases both systolic and diastolic BP; it does not increase resting BP Little or no changes to those who are already max hypertensive 13 BP Changes during Hypertension HIGH Blood Pressure Symptoms: Stressed, Sedentary, Bloated, Weak, Fainting Systolic-Diastolic Category 210 – 120 Stage 4 (very severe) High Blood Pressure 180 – 110 Stage 3 (severe) High Blood Pressure 160 – 100 Stage 2 (moderate) High Blood Pressure 140 – 90 Stage 1 (mild) High Blood Pressure 130/139 - 85/89 High Normal <130-<85 NORMAL Blood Pressure 110 – 75 Low Normal 90 – 60 BORDERLINE LOW 60 – 40 TOO LOW Blood Pressure 50 – 33 DANGER Blood Pressure LOW Blood Pressure Symptoms: Weak, Tired, Dizzy, Fainting, Coma Table: Blood Pressure Norms This table is often misinterpreted in that high BP is more often viewed negatively as hypertension and is associated with an unhealthy lifestyle Hypertension is only present if a high BP is prolonged/long term Hypertension is not short term temporary high BP, like that induced by stress, but long term, enduring high BP Treatment is normally provided if BP exceeds 140mmHg over 90mmHg, but 160 over 95 is more commonly regarded as real hypertension Hypertension interrupts the control system for maintaining a normal low BP and if not treated makes hypertension worse and can lead to some harmful effects: o Increased workload on heart (increased resistance to expel blood) o Increasing/accelerating atherosclerosis (hardening of arterial walls = less elastic) o Increasing/accelerating arteriosclerosis (narrowing of arterial walls) o Arterial damage (above) increases the risk of a stroke and congestive (weakening) heart failure Although there is mixed evidence, it is generally suggested that exercise can reduce the risk of developing high BP – and in some cases can bring down BP in people that already have mild to moderate hypertension An active lifestyle can prevent high BP indirectly by reducing the risk of obesity – which increases the chance of hypertension Exercise has also been strongly linked with reductions in stress, which may help to keep blood pressure at moderate levels 14 Impact of Different Types of Physical Activity on the CV System Arteriosclerosis This relates to a loss in elasticity, thickening/hardening of the arteries Which reduces the arteries efficiency to vasodilate/vasoconstrict Our arteries harden as part of the natural aging process Smoking increases this process and if you start to smoke younger, it will start earlier Blood clots are also two to four times more likely Atherosclerosis This is a form of Arteriosclerosis that affects changes in the lining of the arteries Cholesterol and fat deposits accumulate within arterial walls forming fatty plaque which leads to progressive narrowing of the lumen, which increases the chance of blood clots forming This can restrict blood flow and lead to high BP (hypertension) Angina Angina is a partial blockage of the coronary artery causing intense chest pain which occurs when there is an inadequate oxygen/blood supply to the heart muscle wall Both Arteriosclerosis and Atherosclerosis in coronary arteries deprive areas of the heart of oxygen/blood This can occur during rest, anxiety, but more especially during physical effort/exercise, when the heart requires more oxygen than the coronary arteries can provide due to blockages Heart Attack This is a more severe/sudden or total restriction of oxygen/blood supply to part of the heart muscle wall, usually causing permanent damage It is most like due to blood clots from larger coronary arteries that get stuck in smaller ones and block them Death can occur if the damaged area is large enough to prevent the remaining heart muscle wall from supplying sufficient cardiac output to the body Impact on Coronary Heart Disease (CHD) of lifelong involvement in an active lifestyle The World Health Organisation endorses the view that the risk of CHD is 2-3 times more likely in inactive sedentary individuals than that of those physically active Inactivity is a major risk factor for CHD, almost doubling the risk of a fatal heart attack 15 Research suggests there is a ‘cause-and-effect’ relationship between inactivity and CHD Lifelong involvement in an active lifestyle will maintain significant protection from CHD Risk Factor 1– Physical/activity (mins/wk) Above 60% HR Max 2 – Blood Pressure (mmHg) Systolic Diastolic 3 – Smoking (cigs per day) 4 – Blood Lipids Cholesterol (mg/dl) Triglycerides (mg/dl) 5 – Obesity (BMI) Table: 1 V Low 2 Low Level of Risk 3 Moderate 120 90 30 0 0 <110 <70 0 120 76 5 130-140 82-88 10-20 156-160 94-100 30-40 >170 >106 >50 <180 <200 220-240 260-280 >300 <50 <100 <130 <200 <300 >25-27 27-30 30 - <35 35 - <40 >40 4 High 5 V High Primary Risk Factors Calculation of BMI Example 1. Height squared: 2. Weight divided by height squared: 3. BMI: 1.88 x 1.88 = 3.53 952 / 3.53 = 26.9 27 (overweight) CHD – How to Reduce the Risk Physical activity can protect us from CHD in the following ways: Improve heart-hypertrophy pumping capacity and circulation; vascularisation; increase capacity/size of coronary circulation Decrease blood fibrinogen; decrease blood clotting and decreases blood viscosity, improving blood flow to the coronary circulation Decrease blood lipids (triglyceride/cholesterol) which can be deposited on arterial walls leading to atherosclerosis and arteriosclerosis 16 Decrease Low Density Lipoproteins (LDL) – high in blood lipids/cholesterol which are deposited on vessel walls leading to atherosclerosis and arteriosclerosis Increase High Density Lipoproteins (HDL) – low in blood lipids/cholesterol and act as scavengers removing cholesterol from arterial walls Lower BP and reduce the risk of developing hypertension Reduce obesity controlling body weight which helps against hypertension and controls of diabetes Alleviate tension/stress helping reduce hypertension Other Factors There are factors apart from exercise that help reduce CHD, they are: Stopping smoking reduces the speeding up of arteriosclerosis Regular physical activity Proper nutrition/diet, which reduces weight/obesity, blood lipids, glucose and body fat Recommendations for Physical Activity We know that physical activity reduces CHD, but what level of physical activity is recommended to help achieve this protection? The level of activity required is generally low – walking, low intensity jogging/cycling provides adequate protection against CHD, although higher intensity exercise will provide even greater protection 17 EXAM QUESTIONS MAY 2002 2 a) An 18 year old swimmer uses maximum effort to complete 100 meters front crawl in a personal best time of 60 seconds. The swimmer’s heart rate is recorded using a heart rate monitor. (i) Sketch a graph to show the swimmer’s heart rate trace during the following three stages; prior to the race; during the race; for ten minutes after the race. (5 marks) 200 Heart Rate (beats/ 150 min) 100 50 0 Prior to Race (ii) During Race Time 10 min After Race Why is a warm up beneficial to the vascular system of a swimmer? (2 marks) JANUARY 2003 1 e) It is often recommended that a performer cools down following physical activity. State three effects that a cool down will have on the vascular system of the performer. (3 marks) 2 a) (ii) b) During and after exercise the performer’s heart rate will increase and decrease. Describe how neural control regulates a performer’s heart rate. (3 marks) Describe how oxygen and carbon dioxide are transported in the blood. (4 marks) 18 c) Endurance (aerobic) performance is dependent upon the heart supplying blood to the muscles. Describe the flow of blood through the heart during the cardiac cycle (Diastole and Systole Phases). (4 marks) MAY 2003 2 a) The measurement of heart rtes during training can provide valuable information to the athlete and the teacher/coach. (i) Sketch a graph on the plan below to show the heart rate of an athlete who completes a 30 minute aerobic training run. Show heart rate prior to the training run, during the run and 10 minutes after the run. (4 marks) 200 Heart 150 Rate (beats per minute) 100 50 Rest Training Run Time Recovery (ii) Describe how hormonal control is used to alter heart rate during the training run. (2 marks) (iii) Draw and label a diagram to show how the two circulatory networks (systemic and pulmonary) transport the blood around the body during the training run. (4 marks) (iv) Describe the mechanisms of venous return that ensure enough blood is returned to the heart during the training run. (2 marks) (v) Why should the performer warm up before the training run? (3 marks) 19 JANUARY 2004 1 2 c) During aerobic exercise the performer requires the heart to pump more blood to the working muscles. (i) Define Stroke Volume and give a value for maximal Stroke Volume during exercise. (2 marks) (ii) Explain how a performer is able to increase stroke volume during exercise. (3 marks) b) The cardiac cycle explains how the heart pumps blood to the working muscles. Describe how the conduction system of the heart controls the cardiac cycle in the diastole and systole stages. (4 marks) c) Describe the changes that occur in the distribution of cardiac output as a performer moves from rest to exercise. Explain how the vasomotor centre controls this distribution. (4 marks) MAY 2004 1 b) The graph below shows a heart rate sketch of a 17-year-old cyclist before a maximal effort sprint race. 250 200 Heart Rate (beats/ 150 min) 100 50 0 Rest (i) Sprint Race Recovery Time Define the term heart rate and explain why the heart rate of the cyclist increases prior to exercise. (3 marks) 20 (ii) 2 b) Complete the graph above to show the changes in heart rate you would expect during the sprint race and in the following 10 minute recovery period. (2 marks) During exercise more oxygenated blood is required by the muscles. c) (i) Define cardiac output and give a maximum value for a fit 17-year-old endurance performer. (2 marks) (ii) Explain how oxygen is transported in the blood to the working muscle tissue. (2 marks) Following the release of oxygen at the tissues the blood is returned to the heart (venous return) (i) Identify two mechanisms that aid venous return during exercise. (2 marks) (ii) Give one reason why a good venous return helps an endurance performer. (1 mark) JANUARY 2005 1 b) Following a training session a coach will require the performer to complete a cool down. How would a cool down aid the vascular system? (2 marks) c) Sketch a graph showing the changes you would expect in cardiac output: At rest During a 30 minute sub-maximal training run For a 10 minute recovery period (4 marks) 25 20 Cardiac Output 15 (L/min) 10 5 0 Rest Exercise Recovery Time (mins) 21 2 a) (ii) Describe the passage of deoxygenated blood through the systemic and pulmonary networks which allows carbon dioxide to be removed during aerobic performance. (4 marks) (iii) Identify two ways in which carbon dioxide is carried in the blood during aerobic performance. (2 marks) (iv) Why does an increase in carbon dioxide during exercise increase heart rate? How does this happen? (3 marks) MAY 2005 1 c) It is recommended that a performer completes a warm up prior to exercise. Give two effects of a warm up on the vascular system, (2 marks) 2 a) During exercise more oxygen must be supplied to the working muscles. Describe the passage of oxygenated blood through the pulmonary and systemic networks from the lungs to the working muscles. (4 marks) b) Cardiac Output is a determining factor during endurance activities. Describe how cardiac output is increased during endurance activities. (4 marks) c) Explain the conduction system of the heart. (3 marks) JANUARY 2006 1 b) A cool down has a number of effects on the vascular system which aid the performer. One effect is the prevention of blood pooling. Identify two other effects. (2 marks) 2 a) Large amounts of blood need to be circulated around the body during prolonged aerobic exercise. (i) Identify the mechanisms of venous return that ensure a sufficient supply of blood is returned to the heart during exercise. (3 marks) (ii) An increase in venous return leads to an increase in heart rate. Explain how this is achieved by intrinsic control. (2 marks) 22 (iii) Describe how the blood travels through the heart in the following stages of the cardiac cycle. (3 marks) Diastole Atrial Systole Ventricular Systole (iv) Whilst exercising a greater volume of blood is ejected during ventricular systole. Why is this beneficial to performance? (1 mark) MAY 2006 1 d) 2 a) One change to the vascular system during a warm up is the ability of the haemoglobin to release oxygen quickly. Identify two other changes to the vascular system during a warm up. (2 marks) A long distance runner completes a 60 minute sub-maximal training run. (i) Complete the graph below to show the changes in heart rate in the following three stages: Before the run During the run For a ten minute recovery phase (4 marks) 200 Heart Rate (beats per min) 150 100 50 0 Prior the Run Training Run Time (minutes) 23 Recovery Phase (ii) Explain how the cardiac control centre (neural control) increases the heart rate. (3 marks) (iii) During the training run blood needs to be diverted away from non-essential organs to the working muscles. Explain how the vasomotor centre controls this distribution. (3 marks) JANUARY 2007 2 a) (i) Describe how the conduction system of the heart controls the cardiac cycle to ensure enough blood is ejected from the heart during a five mile training run of a marathon runner. (3 marks) (ii) Identify two ways in which oxygen is transported in the blood during the training run. (2 marks) During the pull up exercise carbon dioxide is transported to the lungs. Identify two ways in which carbon dioxide is carried in the blood during this exercise. (2 marks) MAY 2007 1 a) (ii) 2 b) Draw a graph to show how a cyclist’s cardiac output changes in the following phases of an aerobic training session. (4 marks) Prior to Exercise Exercise Session Recovery Period 25 20 Cardiac Output (L/min) 15 10 5 0 Prior to Exercise Exercise Time (minutes) 24 Recovery Period c) Draw and label a diagram to show how blood flows through the pulmonary and systemic networks of the cyclist’s body during the training ride. (4 marks) JANUARY 2008 1 b) It is recommended that an athlete completes a cool down after exercise. Describe three ways in which an active cool down affects the vascular system of the athlete. (3 marks) 2 c) Describe how intrinsic control affects the cardiac output of a performer during exercise. (4 marks) d) Describe how the conduction system of the heart controls the cardiac cycle. (3 marks) 25 MAY 2008 1 c) Complete the flow diagram outlining the flow of the blood through the pulmonary circulatory system during exercise. (4 marks) Right Atrium Right Ventricle Lungs Left Atrium Left Ventricle 2 a) Sketch a graph to show the heart rate changes of a sprinter in the following phases of a race. (4 marks) Prior to exercise During the race Recovery period 26 200 Heart Rate (beats per min) 150 100 50 0 Prior to Exercise During the Race Recovery Time (minutes) b) An increase in heart rate during exercise is a result of intrinsic, neural and hormonal responses. Describe the hormonal factors which affect heart rate during exercise. (2 marks) d) During exercise a performer requires large amounts of oxygen to be transported to the muscles. (i) Explain how oxygen is transported in the blood. (2 marks) 27