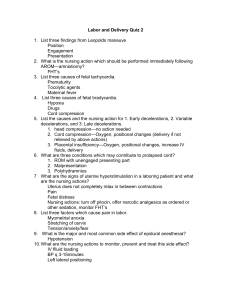
Maternal-Neonatal nursing
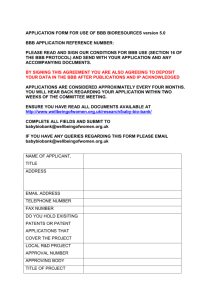
advertisement

Maternal-Neonatal Nursing complications of labor & birth 16th & 17th Lectures dr.Shaban 1 Dystocia Dystocia is “Difficult Labor” prolonged or abnormal labor/FAILURE TO PROGRESS IN LABOUR It primarily results from one of four problems Powers-abnormal uterine activity, ineffective contractions Passageway- abnormal pelvic shape Passenger-abnormal fetal size or presentation Psyche-inadequate support, maternal stress & anxiety dr.Shaban 2 CEPHALOPELVIC DISPROPORTION (CPD) A contracted or narrow diameter in birth passage especially if fetus is larger than the maternal pelvic diameters. Implications: Maternal: prolonged labor, arrest of descent, uterine rupture, forcepsassisted birth with trauma Implications: Fetal: cord prolapse, excessive molding of head, birth trauma to skull and CNS dr.Shaban 3 Nursing diagnoses r/t dysfunctional labor Anxiety r/t slow progress of labor Fatigue r/t the length of labor Ineffective individual coping r/t inability to relax Fluid volume deficit r/t lack of fluid intake dr.Shaban Risk for Infection r/t prolonged labor Sleep pattern disturbance r/t maternal exhaustion and inability to relax Knowledge deficit r/t potential fetal distress and fetal sepsis 4 Management of Labor Dystocia Augmentation of labor-use of drugs to enhance labor that has already begun Amniotomy Oxytocin Augmentation Assisted and Operative Delivery Vacuum - Assisted Delivery Forceps Delivery Cesarean Birth dr.Shaban 5 Oxytocin induction & augmentation Prior to administration of oxytocin a full assessment is preformed to determine cervical status, FHR, fetal presentation and station. The woman is placed on continous EFM Oxytocin is administer IV through a controlled infusion pump and diluted in an intravenous solution Vital signs are recorded frequently Urinary out put is recorded as urine out put can decrease and water can be retained (maternal water intoxication) 6 dr.Shaban Side effects of oxytocin administration Water intoxication- headache, nausea & vomiting, decreased urinary output, hypertension, tachycardia and cardiac arrhythmias Hyperstimulation of the uterus Uterine rupture A rapid labor with potential uterine or cervical lacerations dr.Shaban 7 Nursing interventions when administering oxytocin Observe for signs of water intoxication Changes in FHR-non reassuring FHR Contractions lasting longer than 90 seconds with frequency of 1 minute Assess cervical dilation and progression of labor If non reassuring FHR occurs or hyperstimulation of the uterus occurs the infusion is stopped immediately and MD informed dr.Shaban 8 Contraindications for the induction of labor Previous classic uterine incision Cephalopelvic disproportion Placentia previa Active genital herpes Preterm fetus Fetal malposition-breech Multiple gestations Nonreassuring fetal status dr.Shaban 9 Case 1 You are working at the ED. A G9P2 patient presents to the department. Her water broke 1 hour ago, she is having frequent contractions and she feels the head coming out. A delivery tray is available and the patient is in lithotomy position. She is pushing with each contraction and the baby’s head starts to come out. However, with each push, the baby’s head comes out and then retracts back in towards the perineum. You quickly recognize this as the sign of shoulder 10 dr.Shaban dystocia. Shoulder Dystocia be defined by a prolonged head-to-body delivery time (> 60 s) due to impaction of the fetal shoulders within the maternal pelvis Risk factors: macrosomia, post-term, maternal obesity Maternal morbidity: 4th degree perineal, cervical & vaginal lacerations, bladder injury, postpartum hemorrhage, endometritis Fetal morbidity: brachial plexus injury, clavicular fracture, facial nerve paralysis, asphyxia, CNS injury, death 11 dr.Shaban ERB or brachial plexus dr.Shaban 12 Shoulder DystociaManagement Obstetrical Maneuvers Rotation and Delivery of Posterior Shoulder Maternal Position Change Issue of Fundal Pressure Episiotomy dr.Shaban 13 Case 2 You are working in a small ED and a 35 week G4P3 presents with ROM and contractions. She is quite distressed and thinks the baby is coming out. You perform a pelvic examination and next to the head you feel a pulsate cord… dr.Shaban 14 Prolapse of the umbilical cord When the umbilical cord precedes the fetal presenting part it is said to be prolapsed, this can interfere with fetal circulation Factors that contribute to prolapsed cord are Rupture of membranes before head is engaged Small fetus Breech presentations and transverse lie Hydramnios Unusually long cord Multifetal pregnancy dr.Shaban 15 Nursing actions to relieve prolapsed cord Place woman’s hips higher than her head- kneechest position, trendelenburg’s position, or side lying with hips elevated on a pillow With a sterile glove push fetal presenting part away from cord Give oxygen at 8 to 10 L/Min Monitor FHR Prepare for rapid vaginal or caesarian birth If cord protrudes apply sterile saline soaked towels to prevent drying of the cord and maintain blood flow until infant is delivered dr.Shaban 16 dr.Shaban 17 FETAL DISTRESS Common causes: cord compression, uteroplacental insufficiency, placental abnormalities, meconium-stained amniotic fluid Correct maternal hypotension and enhance uteroplacental blood flow Change position that improves FHR, Increase rate of IV O2 via face mask Decrease uterine activity: adm tocolytic Perform vaginal exam (prolapsed cord?) dr.Shaban 18 Indications for operative vaginal delivery Fetal Distress An irregular fetal heart beat Bradycardia, under 100 beats per minute, between uterine contractions A rapid fetal heart - more than 160 beats per minute The passage of Meconium in cephalic presentations Maternal Conditions Maternal distress or exhaustion: This is shown by dehydration, pulse above 100 and temperature. Maternal disease: When the mother has cardiac disease, toxemia, forceps & vacuum can be used 19 dr.Shaban to shorten the second stage. Assisted and Operative Delivery- Vacuum Mechanism: Suction and Traction used to assist delivery of presenting part. Indication: Most commonly related to prolonged 2nd Stage of Labor. Contraindications: Cephalopelvic Disproportion (CPD); Most malpresentations and malpositions; extreme prematurity. Nursing Responsibility: FHR checks q 5 minutes; Hand held suction pump. Pressure release between UC’s; Assess neonatal head for Cephalohematoma after delivery. 20 dr.Shaban 21 Assisted and Operative Delivery- Forceps Delivery Mechanism: Traction and rotation of fetal presenting part with curved metal tongs. Indication: Prolonged 2nd stage (> 3 hrs); maternal exhaustion; Contraindications: Cephalopelvic Disproportion (CPD); Most malpresentations and malpositions. Disadvantages: Maternal and fetal trauma (Caphalohematoma;Transient facial paralysis) Nursing Responsibility: FHR checks q 5 minutes; obtain forceps; assess neonate and mother for trauma. dr.Shaban 22 dr.Shaban 23 dr.Shaban 24 Cesarean Birth Definition a surgical incision made into the abdomen and uterus to deliver the fetus after 32 WK gestational age. It is called hysterotomy, if removal is done before 32 weeks of pregnancy Types of Cesarean (Uterine) Incisions -Lower Uterine Segment (Low Transverse) -Classical (Vertical Midline) Only L. Uterine Segment Cesareans allow a trial of labor with the next pregnancy. Classical is used for emergency Cesareans or for some mal presentations. dr.Shaban 25 Uterine Incisions Kerr Incision vs Sellheim Incision vs Classical dr.Shaban 26 Skin Incision Transverse (Pfannenstiel)-lower uterine segment Adv: below pubic hair line, less bleeding, better healing,cosmatic Disadv: difficult to extend if needed, requires more time, if adipose fold difficult to keep clean and dry Vertical-between naval and symphysis Adv: quicker, more room dr.Shaban Disadv: scar obvious, longer 27 dr.Shaban 28 INDICATIONS FOR ELECTIVE CS Known CPD Fetal macrosomia > 4500 gm Placenta previa HIV Active herpes Repeat CS Previous uterine surgery eg. Hystrotomy, myomectomy Severe IUGR Breech Multiple pregnancy Transverse lie Ca of the Cx/ obstructing 29 thedr.Shaban birth canal INDICATIONS FOR EMERGRENCY CS Severe PET, Abruptio placntae, APH Fetal distress Failure to progress in the first stage of labour Cord prolapse Obstructed labour Failed induction; failed vacuum or forcepes Malpresentation brow, face, shoulder & compound presentations, breech dr.Shaban 30 COMPLICATIONS- Mother INTRAOPERATIVE Bleeding & the need for bld transfusion Hysterectomy, Fetal injury Complications of anesthesia Damage to the bladder, ureter, colon , retained placental POSTOPERATIVE Gaseous distension, Paralytic ileus Wound dehiscence & infection Infections UTI, pulmonary DVT & pulmonary embolism, Death Longer hospital stay 31 dr.Shaban Risk for maternal/infant attachment COMPLICATIONS-the baby Premature birth. If the due date was not accurately calculated, the baby could be delivered too early. Breathing problems. Babies born by cesarean are more likely to develop breathing problems such as transient tachypnea (abnormally fast breathing during the first few days after birth). Low Apgar scores. dr.Shaban 32 Nursing care in the preoperative period NP0 IV fluids Insertion of urinary catheter Medication may be given IV to prevent stomach irritation or aspiration Consent is obtained Pubic shave now not needed Patient teaching and explanations of events Assessment of FHR, maternal vital signs dr.Shaban 33 Nursing care intraoperative period Skin preparations Draping COUNTS Sterile field maintenance Step 14: Uterus is closed in 2 layers dr.Shaban 34 Postoperative care Monitor vital signs every 15 minutes for first hour, then every 30 mins in second hour then hourly until transferred to postpartum unit Administer oxygen as ordered Assess fundus for firmness, height, location, massage fundus if boggy Assess vaginal bleeding for color amount and consistency Assess abdominal dressing for bleeding Assess urine output Change woman’s position Allow the mother to breast feed as soon as she wishes dr.Shaban 35 Postoperative care-Cont. Women should be offered Pethidine (100mg im). Avoid over sedation as this will limit mobility If the woman is receiving IV fluids, they should be continued until she is taking liquids well. A liquid diet if bowel sounds are heard Removal of the urinary bladder catheter should be carried out once a woman is mobile Ambulation enhances circulation, encourages deep breathing and stimulates return of normal gastrointestinal function. Encourage foot and leg exercises and mobilize as soon as possible, usually within 24 hours If the dressing comes loose, reinforce with more tape rather than removing the dressing. This will help maintain the sterility of the dressing and reduce the risk of wound infection .1st dressing changed by doctors . dr.Shaban 36 dr.Shaban 37