Dialysis in the poisoned patient
advertisement

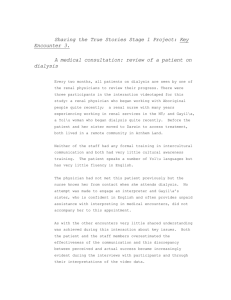
Hemodialysis International 2010; 14:158–167 Review Article Dialysis in the poisoned patient George BAYLISS Division of Kidney Disease and Hypertension, Alpert School of Medicine, Brown University, Providence, Rhode Island, USA Abstract Patients who ingest toxic substances may require extracorporeal removal of the poisons or their toxic metabolites if native renal clearance is not sufficient because of acute kidney injury, acuity of symptoms, or burden of toxin. Here, a case is presented, and the literature on renal replacement therapy in the event of acute intoxication is reviewed. Extracorporeal therapy efficacy is examined in terms of the characteristics of the toxin (molecular size, charge, protein, or lipid binding); the patient (body habitus and volume of distribution); and the process (membrane effects on extraction ratios and sieving, role of blood, and dialysate flow rates). The choice of extracorporeal therapy and hemodialysis prescriptions for specific poisonings are discussed. Key words: Dialysis, poisoning, hemoperfusion A CASE A 51-year-old woman with a history of depression and chronic pancreatitis from Valproic acid (Depakote) exposure was brought to the emergency department by EMS after her 11-year-old daughter found her unresponsive on the bathroom floor. In the emergency department, the patient was tachycardic, with an initial heart rate of 129 beats/min, but normotensive, with blood pressure ranging from 139/65 to 135/65 mmHg. She was tachypneic, with a respiratory rate of 44 breaths/min. Oxygen saturation by pulse oximetry was 97% on 3 L of oxygen by nasal cannula. She was minimally responsive with dilated, minimally responsive pupils. Cardiac exam revealed normal heart sounds and no murmurs, rubs, or gallops. Her clear lungs were clear to auscultation. Her abdomen was soft, her mucus membranes were dry, and her skin was damp. She had no lower extremity edema. A chest X-ray showed a normal-sized heart and no infiltrates or pleural effusions. Nurses placed a Foley catheter in the emergency department, and the patient voided Correspondence to: G. Bayliss, MD, Division of Kidney Disease and Hypertension, Alpert School of Medicine, Brown University, Rhode Island Hospital, Providence, RI 02903, USA. E-mail: gbayliss@lifespan.org, geobayliss@gmail.com 158 1.4 L of urine over 4 hours as she was volume resuscitated with isotonic fluid. Serum chemistries showed elevated serum creatinine (1.7 mg/dL, up from her baseline of 0.7 mg/dL), mild hyperkalemia (potassium = 5.3 mEq/L), serum bicarbonate of 14 mEq/L, and an anion gap of 24. An arterial blood gas showed pH = 7.38 and pCO2 = 18 mmHg, indicating both a metabolic acidosis and respiratory alkalosis. Urine toxicology screen was positive for salicylates, and the serum salicylate level was 134 mg/dL (therapeutic o30 mg/dL). The patient’s initial electrocardiogram revealed sinus tachycardia, left axis deviation, a narrow QRS complex, and no prolongation of PR or QT intervals. She subsequently developed supraventricular tachycardia at a heart rate of 145–160 beats/min that did not respond to adenosine. A toxicology consultation was obtained, and the patient was started on a sodium bicarbonate infusion. A renal consult was requested. DISCUSSION This patient appeared critically ill and at risk of needing intubation for airway protection. Her case illustrates the key circumstances under which extracorporeal removal of toxins is required to prevent extreme morbidity and r 2010 The Authors. Journal compilation r 2010 International Society for Hemodialysis DOI:10.1111/j.1542-4758.2009.00427.x Dialysis in the poisoned patient death. In such cases, experts recommend immediate consultation with a medical toxicologist or poison control center to optimize medical management of patients while the need for and feasibility of extracorporeal therapy is evaluated, based on the molecular size of the toxin, its volume of distribution, water solubility, and proteinbinding characteristics.1 The use of hemodialysis, continuous renal replacement therapy (CRRT), or hemoperfusion is important in the management of certain drug overdoses and toxic ingestions when other measures such as activated charcoal, gastric lavage, specific antidotes, and respiratory support have failed or are not feasible because of the patient’s condition.2 Such extracorporeal procedures should be considered adjunctive, and not substitutes for other measures and supportive care. Furthermore, certain measures such as gastric lavage, forced alkaline diuresis, or administration of chemical inhibitors may be critical in the early phases of drug ingestion, obviating the need for extracorporeal therapy or supplementing it. The circumstances that in this case point to the need for extracorporeal drug removal include progressive deterioration of the patient’s status despite intensive supportive therapy; decreased level of consciousness with suppression of midbrain functions; the risk of complications of coma like aspiration pneumonia; impaired native clearance of drugs and toxins in the setting of reduced glomerular filtration as a result of acute kidney injury; the amount of toxin ingested; and faster clearance of the toxin by extracorporeal means than normal native clearance would provide.2 In the case of salicylate intoxication, aggressive volume expansion and forced diuresis could prove harmful with complications that include pulmonary3 or cerebral edema.4 Extracorporeal techniques include dialysis and hemoperfusion; dialysis therapies include intermittent hemodialysis, CRRT, and peritoneal dialysis. Each has advantages, depending on the properties of the toxin being removed, the total burden of toxin in the patient, and the rate at which the extracorporeal method removes toxins from the blood. Therapeutic plasma exchange has also been used to remove protein-bound drugs as well as endotoxin.5 Key principles Molecular size, charge, and binding characteristics help determine the ease with which toxic substances and drugs in overdose can be removed from the patient. Low molecular weight substances (like urea, MW 60 Da) that are water-soluble pass easily across a dialysis mem- Hemodialysis International 2010; 14:158–167 brane, while large, protein-bound or lipid-bound molecules are more difficult to remove because of their size and difficulty in breaking those bonds, thus requiring dialysis membranes with larger pores (like b2 microglobulin, MW 11,800 Da). The pharmacokinetics of a drug or a toxin depends on several factors.6 The first is absorption, with the bioavailability of the drug defined as the percentage of the administered drug that reaches systemic circulation. Next, the volume of distribution, Vd, of a toxin represents the theoretical dispersion of the substance in the patient’s body and is defined as the amount of drug in the body divided by the concentration of the drug in plasma. This depends on both the characteristics of the patient and the toxin. Water-soluble molecules will remain more accessible and toxic levels can be more easily reduced when the toxin has a small Vd in the patient. Lipid-soluble molecules have a larger Vd, and toxic levels are more difficult to reduce because the intravascular levels represent only a small fraction of the total body burden of the toxin. A related concept is rebound. Intravascular levels of lipid-soluble molecules may decline quickly after an initial session of dialysis, but increase again as serum levels re-equilibrate from the extravascular space. Patient characteristics that affect a drug’s Vd include obesity, extracellular fluid volume status, age, gender, thyroid function, renal function, and cardiac output. In general, a drug’s plasma concentration correlates inversely with its Vd.6 Clearance of a substance is the theoretical volume of blood from which the substance is removed per unit of time.7 Native clearance depends on the ability of a molecule to pass across the glomerular basement membrane into the urinary space, a function of molecular size and charge, and the urine flow rate [U]V/[P], expressed in milliliters per minute. Solute removal occurs first by filtration (convection), but is also influenced by modification in the tubules, the continuous nature of native renal clearance, and stable serum concentrations in the steady state.8 In dialysis, clearance is achieved through diffusion and convection via ultrafiltration and is defined as the product of the extraction ratio—the percentage of the substance removed from the blood as it passes over the membrane— and the blood flow rate [(Cinitial Cfinal)/Cinitial][QB].9 It is also expressed in terms of milliliters per minute. Intrinsic characteristics of the dialysis membrane that affect clearance across the membrane include the size and number of dialysis membrane pores (flux), membrane composition and thickness, and the total surface area of the dialysis membrane (efficiency). The intermittent nature of the ther- 159 Bayliss apy means that solute clearance, mass removal rate, and serum concentration are not constant.8 Protein binding considerably affects a drug’s pharmacokinetics, with only unbound drugs or active drug metabolites able to exert a pharmacologic effect. Drugs that are highly protein bound are not removed effectively during dialysis. In general, the volume of distribution of a drug increases as its protein binding decreases.6 Knowledge of whether renal clearance can be made to become a major component of total clearance may help in the management of drug overdoses.10 The native clearance of poisons may be affected by reductions in glomerular filtration rate (GFR) as a result of hypotension or volume depletion, the large volume of distribution of the drug or toxin, its charge, size, and binding characteristics. Renal drug clearance is also influenced by tubular secretion and re-absorption as well as renal epithelial cell metabolism. Highly protein-bound drugs have either reduced clearance or are secreted into the tubules by active transport, which is dependent on renal blood flow but not on GFR. Most drugs and their metabolites are eliminated by first-order kinetics, and the amount of drug eliminated over time is a fixed proportion of the total body store. The half-life of a drug thus increases as the renal function decreases.6 Many toxins and drugs that can build up to toxic levels are weak acids, like salicylates, barbiturates, and chlorinated acid herbicides. In theory, maintaining them in the ionized state decreases their re-absorption across phospholipid cell membranes and potentially increases their rate of excretion in the urine if the substance is cleared by the kidneys. Increasing the urinary pH should in theory increase the ionized fraction of the substance, which is expressed in terms of the pKa or dissociation constant. Weak acids have a high pKa. Ionic and nonionic forms are in equilibrium when pH = pKa. Most drugs are in the nonionized phase at the physiologic pH = 7.4. Thus, in those cases where alkalinization is indicated, experts recommend that the goal should be a urine pH 7.5 and be maintained at or above that level to maximize elimination. The same experts distinguish urinary alkalization from forced diuresis, whose goal is merely to increase urine output.11 Mechanical aspects of dialysis also have an important effect on the clearance of toxic substances and drugs. In general, dialytic clearance of a substance is determined by the intrinsic clearance of the dialyzer membrane, the length of time of treatment, blood, and dialysis flow rates. Thus, a high-efficiency dialyzer will provide more surface-area contact for blood and dialysate, allowing greater diffusion of substances down the concentration gradient 160 from blood to effluent. Larger pores will allow greater convective solute clearance, or sieving, during ultrafiltration via solvent drag.12 The combination of diffusive and convective clearance provides more total clearance per unit of membrane surface area than either alone, although the addition of convection, which is more important for larger molecules, reduces diffusive clearance, which is more significant for smaller molecules, when replacement fluid is added to blood prefilter to compensate for increased water permeability of the membrane.13 Older research has shown that blood contact with high-flux membranes can decrease the sieving coefficient in symmetric membranes, like the AN69, through protein adsorption to the membrane surface.14 Increased use is being made of convection to remove middle and high molecular weight solutes. But while high-flux polysulfone membranes have high middle molecular weight solute clearance, they also contribute to significant loss of albumin.15 Work is under way to develop a high-flux membrane that does not lead to albumin loss.16 Modalities of extracorporeal toxin removal Hemodialysis is the modality of choice for low molecular weight, water-soluble molecules, especially those that have small volumes of distribution and are not protein bound or lipid bound. It is ideal for molecules that diffuse easily across dialysis membranes. Its use is limited in patients who are hypotensive because dialysis, even without volume removal, may reduce the blood pressure further. The use of dialysis is further limited to drugs and toxins that reach plasma concentrations that are high enough to establish a sufficient concentration gradient like alcohols, lithium, and salicylates.17 Continuous renal replacement therapies have a theoretical advantage in patients who have ingested substances that are highly lipid bound and have large volumes of distribution with slow intercompartmental transit times from the extravascular to the intravascular space. In theory, CRRT is ideal in cases in which serum levels of toxins rebound after rapid removal as toxins reequilibrate in the vascular space over time from body stores such as lipid-bound molecules in fat stores. CRRT is also useful in hemodynamically unstable patients who are unable to tolerate high blood flow rates. Clearance is achieved through the longer total dialysis time, rather than per unit time, given the slower blood flow rates.7 Some researchers have suggested adding albumin to the Hemodialysis International 2010; 14:158–167 Dialysis in the poisoned patient dialysate to remove highly protein-bound drugs like valproic acid and carbamezapine during CRRT.18 Hemoperfusion uses a cartridge similar to a dialysis membrane in which toxins are removed from the blood by binding to activated charcoal or resin rather than diffusing out of the blood down a concentration gradient. The procedure is run on a dialysis machine using regular dialysis pumps but without a dialysate. It is useful with highly protein-bound and lipid-bound molecules. Disadvantages include saturation of the cartridge and the need to change it every 2–3 hours. Hemoperfusion cartridges can be run in series with hemodialysis membranes in patients who also need solute and fluid removal for kidney failure.2 Peritoneal dialysis has fallen out of favor as a modality in the poisoned patient because of its low effectiveness in removing toxins. It is useful in small children in whom a peritoneal dialysis catheter can be inserted relatively quickly and in cases of overdoses further complicated by hypothermia, in which core rewarming is required.2 Therapeutic apheresis has a theoretical advantage over dialysis or hemoperfusion in removing substances that are protein-bound or lipid-bound and in the intravascular space (4300 Da).19 But there have been no controlled trials, and recommendations for its use are based on case reports and series. The American Society for Apheresis rates toxin removal as a class III indication (suggestion of benefit but insufficient evidence to establish efficacy or risk vs. benefit). An exception is plasmapheresis for phalloid intoxication after ingestion of poisonous mushrooms, particularly Amanita phalloides.20 The ASFA gives this a class II indication (generally accepted but considered adjunct therapy). Some consider plasmapheresis at least as effective as hemoperfusion in reducing mortality following phalloid mushroom ingestion, but there is not enough evidence to say that it is superior21 (Table 1). Trends in extracorporeal toxin removal Hemodialysis has increased sharply as the main modality for extracorporeal removal of toxins. Cases of poisoning requiring hemodialysis increased to 707 per million calls to poison control centers from 231 per million over the time period 1985–2005.22 In the same period, the number of cases of poisoning requiring hemoperfusion declined to 12 from 53 per million calls, while cases of poisoning requiring peritoneal dialysis declined to 1.6 from 2.2 per million calls. Lithium and ethylene glycol remained the most common toxins removed by hemodialysis over the 20 years, followed by salicylates and valproic acid. Carbamazepine has replaced theophylline as the toxin removed most frequently by hemoperfusion (Table 2). Technical aspects and complications The technical aspects of toxin removal by extracorporeal means are largely related to access and equipment. In hemodialysis, CRRT, and hemoperfusion, access is through a 10–11.5 French dual-lumen dialysis catheter in a central vein because smaller catheters are unable to support the necessary blood flows of 200–450 mL/min. Except where contra-indicated, heparin should be used to anticoagulate the system to improve dialyzer clearance and prevent blood loss and the loss of time in replacing the dialysis circuit if it clots. Heparin should not be used, for example, in dialyzing patients with methanol toxicity. High-flux, high-efficiency dialysis membranes should be used to maximize pore size and surface area for toxin removal by both diffusion and convection, as discussed above.2 Complications from toxin removal by hemodialysis include hypokalemia and alkalosis due to diffusion of potassium into the dialysate and diffusion of bicarbonate from the dialysate, particularly given the need for high- Table 1 Drugs, toxins amenable to extracorporeal removal by extracorporeal modality Hemodialysis Lithium Ethylene glycol Methanol Salicylates Valproic acid Metformin Theophylline CRRT a Lithium Theophyllinea Valproic acida Metformina Pertitoneal Hemoperfusion Plasmapheresis b Carbamezapine Theophylline Paraquat Phalloids a Hemodialysis preferred method when blood pressure permits. No demonstrated advantage for removal of a particular toxin. CRRT =continuous renal replacement therapy. b Hemodialysis International 2010; 14:158–167 161 Bayliss Table 2 Hemodialysis vs. hemoperfusion and CRRT in acute intoxication. (Adopted with permission from aBorkan SC. Extracorporeal therapies for acute intoxication. Crit Care Clin 2002; 18: 393–420; Goodman JW and Goldfarb DS. The role of continuous renal replacement therapy in the treatment of poisoning. bSemin Dial 2006; 19:402–407; Mulder J et al. Platelet loss across the hemofilter during continuous hemofiltration. bInt J Artif Organs 2003; 96:206–212.) Parameter Renal replacement therapy Restores electrolyte balance Corrects volume status Risk of thrombocytopenia Removes drugs 4300 Da Removes protein-bound drugs Removes water-soluble drugs Removes lipid-bound drugs Rapid QB improves drug removal Cartridge saturation Can be used in hypotensive patient a Hemodialysis a Hemoperfusion Yes Yes Yes Unusual No No Yes No Yes No No No No No Yes Yes Yes No Yes Yes Yes No b CRRT Yes Yes Yes Yes No Limited Yes Theoretical Yes No Yes CRRT =continuous renal replacement therapy; QB =blood flow; SBP =systolic blood pressure. efficiency dialysis membranes. The complications of CRRT include hypocalcemia, particularly when using citrate anticoagulation. Hemoperfusion has been associated with lymphopenia and thrombocytopenia, although the mechanism is not clear.2 Dialysis prescription for specific drugs and toxins The following section discusses the characteristics of selected drugs and toxins most commonly seen as causes of overdoses, and the dialysis prescriptions recommended in the literature for their removal. Lithium Lithium carbonate is a highly effective mood stabilizer; this low molecular weight cation (MW LiHCO3 = 74 Da) is water soluble, with a volume of distribution of 0.7–0.9 L/kg. It is highly dialyzable.2 Most intoxication is chronic in the setting of renal failure and volume depletion while the patient is also taking diuretics, nonsteroidal anti-inflammatory drugs, or angiotensin-converting enzyme inhibitors.2 Mild intoxication occurs at a serum lithium concentration of 1.5–2.5 mmol/L, while moderate intoxication occurs at a serum lithium concentration of 2.5–3.5 mmol/L (therapeutic is o0.6 mmol/L). Both are characterized by neuromuscular irritability, nausea, and diarrhea. Severe lithium intoxication occurs at a serum concentration 43.5 mmol/L and is characterized by seizure, stupor, and permanent neurologic damage. 162 Renal replacement therapy is recommended when: the serum lithium level is 43.5 mmol/L; the serum lithium level is 42.5 mmol/L with symptoms and a depressed GFR; there is moderate intoxication with the expectation that the lithium levels will increase or that they will not decline to the therapeutic range within 36 hours.2 Both hemodialysis and CRRT provide far superior clearance to native renal function even when there is no evidence of acute kidney injury, with an extraction ratio during hemodialysis of 90%.17 At blood flows of 250 mL/ min, hemodialysis provides 70–170 mL/min of clearance compared with 10–40 min/mL in patients with normal renal function. Hemodialysis is superior to CRRT, which provides a clearance of around 48–62 mL/min at blood flows of 200 mL/min and is thus not recommended in the literature as first-line therapy.2 The literature recommends dialysis for 6–8 hours with repeat sessions until the level declines to below 1 mmol/L.2 Other experts suggest, however, that CRRT may be used as the first-line therapy in the event the physician is concerned about rebound toxicity, envisions a long treatment, or is concerned about the effects of fluid removal on patient hemodynamics. The two modalities may be used together: CRRT may be followed by hemodialysis if hypotension resolves, or hemodialysis may be followed by a longer, slower session of CRRT. But there have been no head-to-head randomized trials to resolve the issue definitively.23 Hemodialysis International 2010; 14:158–167 Dialysis in the poisoned patient Ethylene glycol and methanol Ethylene glycol and methanol are volatile alcohols with volumes of distribution equal to that of total body water. Both ethylene glycol (MW 62 Da) and methanol (MW 32 Da) are metabolized by alcohol dehydrogenase to their toxic metabolites—glycolic acid in the case of ethylene glycol and formic acid in the case of methanol. Glycolic acid is further metabolized to oxalate, which deposits in renal tubules as envelope and needle-shaped crystals. The exact cause of acute kidney injury is not known. Some argue that it is related to glycolic acid;24 others argue that calcium oxalate is the causative agent.25 Co-ingestion with ethanol, which binds competitively to alcohol dehydrogenase, slows the metabolism of the other alcohols to their toxic metabolites, but can also conceal their presence, particularly because all 3 can present with central nervous system depression and an anion gap metabolic acidosis.19 Acute kidney injury can delay native clearance of glycolic acid, leading to coma and cardiac toxicity, and of formic acid, leading to CNS depression and blindness from oxidative damage to the retina. Patients initially develop an osmolar gap and then, as the alcohol is metabolized to an acid, an anion gap.26 Thus, a normal osmolar gap in the presence of an anion gap may indicate that the alcohol has been metabolized, while a normal anion gap in the presence of an osmolar gap may indicate that the ingestion is recent. The first line of treatment in the case of ethylene glycol or methanol poisoning is to block the metabolism of the alcohols to their toxic metabolites. The antidote 4-methylpyrazole (fomepizole) has emerged as the primary inhibitor of alcohol dehydrogenase.27 The American Academy of Toxicology recommends treatment with fomepizole rather than ethanol unless fomepizole is not available or causes an allergic reaction. The guidelines for starting fomepizole are similar for both alcohols: documented ingestion of the alcohol and a concentration of 420 mg/dL; documented recent ingestion of the alcohol with an osmolar gap 410 mOsm/L; strong clinical suspicion of ingestion of the alcohol and two of the following—arterial pHo7.3, serum HCO3 o20 mEg/L, or an osmolar gap 420 mOsm/L (or urinary oxalate crystals in the case of ethylene glycol).28,29 Despite the use of fomepizole, dialytic removal of methanol or ethylene glycol may be necessary in the event of: severe metabolic acidosis with the pHo7.25; Hemodialysis International 2010; 14:158–167 acute kidney injury or electrolyte imbalances that do not respond to conventional therapy; and deteriorating vital signs despite intensive care. The guidelines also indicate dialysis for an alcohol level 450 mg/dL unless fomepizole is administered, the patient is asymptomatic, and the pH is normal. Further metabolism of the toxic metabolites to nontoxic byproducts should be enhanced by giving pyridoxine and thiamine to patients with ethylene glycol poisoning and folate or folinic acid to patients with methanol poisoning.28,29 In the case of ethylene glycol, dialysis is undertaken with a bicarbonate dialysate bath until the toxic alcohol level is o20 mg/dL. If one is unable to obtain an alcohol level, then dialysis should be carried out for at least 8 hours and repeated in another 12 hours.2 Glycolic acid has a long half-life and a slow elimination rate. But it also has a low molecular weight (76 Da), is water soluble, and has a limited volume of distribution (0.55 L/kg). Thus, even in the event of a low ethylene glycol level, an increased anion gap correlates with glycolic acid levels; dialysis should be undertaken because it increases clearance considerably.30 Hemodialysis provides a clearance of 200–250 mL/min for ethylene glycol and 170 mL/min for glycolate at blood flow rates of 250–400 mL/min. The elimination half-life of glycolic acid on dialysis is 155 min compared with 626 min in patients not treated by dialysis.30 With very high methanol levels, dialysis may need to be undertaken for 18–21 hours and the procedure repeated after 24 hours if there is rebound toxicity. Most experts recommend against using heparin anticoagulation during dialysis because of the risk of intracranial hemorrhage, particularly in the basal ganglia.31,32 Hemodialysis provides a clearance of 200 mL/min for methanol and 223 mL/min for formate at blood flows of 100–400 mL/ min. But the endogenous elimination half-life of formate was not found to be statistically different from the elimination half-life on dialysis (205 90 vs. 150 37 min) in one study. This may be in part due to other treatments given to patients—folate or folinic acid—to increase the metabolism of formic acid to carbon dioxide and water.33 Other researchers, however, have found that hemodialysis significantly reduced formate elimination half-life compared with endogenous elimination and question the role of folate.34 Some experts suggest that early intervention with fomepizole and supportive care like sodium bicarbonate administration to correct the acidosis may lessen the need for hemodialysis in selected cases of methanol intoxication—those who present late with acidemia and no 163 Bayliss detectable methanol level—because elimination of formate through dialysis is not significantly different from endogenous clearance with supportive care.19 Others argue that dialysis can be avoided in stable patients with less metabolic acidosis and no visual symptoms who can be treated with fomepizole alone.35 But fomepizole therapy should be continued even after extracorporeal removal has begun and for several hours after treatment has been completed to account for rebound.28 Very little data exist to show how CRRT compares with hemodialysis in clearing volatile alcohols. A series of 3 patients with methanol ingestion found CRRT clearance of 45 and 48 mL/min at a blood flow rate of 150 mL/min over 37 and 27 hours in two patients compared with clearance on hemodialysis of 237 mL/min at a blood flow rate of 350 mL/min over 4 hours.36 One group has developed an equation to estimate the time required on dialysis to reduce the levels of methanol and ethylene glycol to 5 mmol/L. The equation is based on the assumption that toxic alcohols have a dialysis clearance similar to that of urea37: t ¼ ½V ln ð5=AÞ=0:06k; where t is time, V is the Watson estimate of total body water,38 A is the initial toxin concentration in mmol/L, and k is equal to 80% of the manufacturer-specified dialyzer urea clearance in milliliters per minute at the initial observed blood flow rate. Validated in a small study of 13 patients, the equation requires only 3 measurements of the toxic alcohol: an initial toxin level, 1 drawn 2 hours before dialysis is due to stop, and a level drawn 1–2 hours after dialysis.39 Salicylates Acute salicylate intoxication is characterized in adults by a respiratory alkalosis as salicylates stimulate the respiratory center in the medulla and then a metabolic acidosis as lactic acid builds up from interruption by salicylates of the mitochondrial electron transport chain.40 CNS symptoms indicate severe poisoning. An immediate goal of treatment is to reverse the acidosis and alkalosis to prevent respiratory collapse: patients with salicylate intoxication do very poorly on mechanical ventilation because of the ventilator’s inability to keep up with the patient’s respiratory rate and the development of respiratory dys-synchronization, although there is little empiric evidence to support this in the opinion of some experts. One retrospective review of patients with salicylate intoxication who had been placed on mechanical ventilation at conventional settings found 164 development of a respiratory acidosis, which led to overall worsening of neurologic toxicity by allowing more salicylate to pass into the CNS.41 On the other hand, the older literature cites the case of a child with salicylate poisoning who was successfully treated with intermittent positive pressure ventilation after he was paralyzed,42 and animal experiments on acute respiratory failure following salicylate-induced hyperventilation found no pulmonary or arterial blood gas abnormalities in 5 sheep that were paralyzed and ventilated at normal tidal volume and respiratory rate.43 Alkalinization of the urine is paramount if the patient is still making large amounts of urine to prevent reabsorption of salicylates,44 and potassium administration prevents hypokalemia and acidification of the urine.9 At a low pH, more salicylate crosses the blood–brain barrier and increases CNS intoxication.45 How urinary alkalinization increases salicylate excretion is not entirely clear. The conventional view is that weak acids like salicylates become more ionized in an alkaline environment, and urine alkalinization is recommended for salicylate intoxication unless there are contraindications (renal failure and heart disease).6 Given its high dissociation constant as a weak acid, a small increase in urinary pH should produce a large increase in the ionized fraction of salicylate. But at a urine pH = 5, salicylate is already almost completely ionized so that increasing pH further would not increase its ionization further.46 Dialysis is recommended in the event of: CNS depression at a level 450 mg/dL; salicylate level 480 mg/dL; salicylate-induced pulmonary edema.47 Salicylates have a molecular weight of 38–180 Da and a volume of distribution of 0.17 L/kg. At therapeutic levels, 90% of salicylates are protein bound, but the unbound fraction increases as the total concentration increases, as in the case of intentional overdose. Intermittent hemodialysis is preferred over CRRT unless the patient is hypotensive because 50% of protein-bound aspirin is removed by hemodialysis. The volume of distribution may be difficult to calculate when salicylate is ingested as entericcoated aspirin.48,49 Dialysis is undertaken against a high-flux membrane at high blood flow rates with continued additional sodium bicarbonate infusion because patients are often intravascularly depleted and require volume replacement, not volume removal. Dialysis is continued until the serum salicylate level is o10 mg/dL if there is concern for rebound toxicity, a possibility if the patient has developed a bezoar.45 Hemodialysis International 2010; 14:158–167 Dialysis in the poisoned patient CONCLUSION Dialysis can be a life-saving therapy in the case of accidental or intentional overdoses of toxins that are amenable to extracorporeal removal such as salicylates, lithium, and volatile alcohols, with most authorities recommending intermittent hemodialysis with high-efficiency, highflux membranes, except in cases of hypotension, when CRRT may be necessary because of lower blood flow rates. Use of sustained low-efficiency dialysis has also been reported in a case of acute aspirin overdose.51 The patient in the clinical vignette suffered from the acute effects of aspirin overdose and was at a risk of respiratory collapse if aggressive measures were not taken to reduce salicylate levels. A temporary dialysis catheter was placed in the emergency department, and the patient was transferred to the medical intensive care unit. She underwent 8 hours of hemodialysis with a blood flow of 350–400 mL/min and a dialysate flow rate of 500 mL/min against a 35 mEq/L bicarbonate bath. She continued to receive an infusion of isotonic sodium bicarbonate in 5% dextrose in water during dialysis.52 She was never intubated. Her breathing improved as hemodialysis progressed, and she was maintained with supplemental oxygen, first by a face mask and then by a nasal cannula. Tachycardia also resolved. Roughly 6 hours after initiation of hemodialysis, the salicylate level was 30 mg/dL, and at 8 hours, it was o10 mg/dL, undetectable (see Figure 1), and dialysis was stopped as the patient became hypotensive. The salicylate level rebounded slightly but declined to undetectable levels and remained there without further dialysis. The patient became more alert and acknowledged having taken 200 aspirin tablets in a suicide attempt. Her course was complicated by upper gastrointestinal tract bleeding, found to be due to erosive gastritis, and requiring transfusion of 2 U of packed red blood cells. Nevertheless, her renal function returned to baseline, with a total urine Hemodialysis International 2010; 14:158–167 160 140 Salicylate (mg/dL) Acetaminophen Acetaminophen is a moderately water-soluble 151 Da molecule that is only slightly protein bound. The treatment of choice remains activated charcoal if the patient is able to take food and fluids by mouth and N-acetyl cysteine either orally or intravenously if the patient is unable to swallow. N-acetyl cysteine delivered according to the Rumack-Matthew nomogram for hepatotoxicity helps replete stores of glutathione. Case reports suggest the possibility of using single-pass albumin dialysis using a high-flux membrane and dialysate to treat the resulting liver failure.50 134.4 120 100 80 60 40 20 30.5 14.5 10.5 11 10.1 0 9/2/2008 9/2/2008 9/2/2008 9/3/2008 9/3/2008 9/3/2008 0020 1441 2220 0020 0112 0312 Time Figure 1 Serum salicylate levels as a function of time in a 51-year-old woman presenting after an intentional aspirin overdose. Initial measurement is from an earlier presentation to the same emergency room. output of 2.2 L over her first hospital night. The dialysis catheter was removed, and the patient was transferred to a general medical floor in stable condition. Manuscript received August 2009; revised October 2009 REFERENCES 1 Brent J. Fomepizole for ethylene glycol and methanol poisoning. N Engl J Med. 2009; 360:2216–2213. 2 Winchester JF, Boldur A, Oleru C, Kitiyakara C. Use of dialysis and hemoperfusion in treatment of poisoning. In: Daugirdas JT, et al., ed. Handbook of Dialysis. 4th ed. Philadelphia: Walters Kluwer; 2007:300–319. 3 Cohen DL, Post J, Ferroggiaro AA, Perrone J, Foster MH. Chronic salicylism resulting in pulmonary edema requiring hemodialysis. Am J Kidney Dis. 2000; 36:E20. 4 Rauschka H, Aboul-Enein F, Bauer J, et al. Acute cerebral white matter damage in lethal salicylate intoxication. Neurotoxicology. 2007; 28:33–37. 5 Kaplan AA. Extracorporeal blood purification in the treatment of acute renal failure with multi-organ involvement. Blood Purif. 1996; 14:86–93. 6 Olyaei AJ, De Mattos AM, Bennett WM. Use of drugs in patients with renal failure. In: Schrier RW, et al., ed. Diseases of the Kidney and Urinary Tract. Philadelphia: Lippincot Williams & Wilkins; 2007:2765–2807. 7 Goodman JW, Goldfarb DS. The role of continuous renal replacement therapy in the treatment of poisoning. Semin Dial. 2006; 19:402–407. 8 Clark WR, Henderson LW. Renal versus continuous versus intermittent therapies for the removal of uremic toxins. Kidney Int. 2001; 59(Suppl 78):S298–S303. 9 Daugirdas JT. Physiologic principles and urea kinetic modeling. In: Daugurdas JT, et al., ed. Handbook of Dialysis. 4th ed. Philadelphia: Walters Kluwer; 2007:25–58. 165 Bayliss 10 Tucker GT. Measurement of the renal clearance of drugs. Br J Clin Pharmacol. 1981; 12:761–770. 11 Proudfoot AT, Krenzelok EP, Vale JA. Position paper on urine alkalinization. J Toxicol Clin Toxicol. 2004; 42:1–26. 12 Ledebo I. Does convective dialysis therapy applied daily approach renal blood purification? Kidney Int. 2001; 59(Suppl 78):S286–S291. 13 Van Laecke S, de Wilde K, Vanholder R. Online hemodiafiltration. Artif Organs. 2006; 30:579–585. 14 Boyd RF, Langsdorf LJ, Zydney AL. A two layer model for the affects of blood contact on membrane transport in artificial organs. ASAIO J. 1994; 40:M864–M869. 15 De Smet R, Dhondt A, Eloot S, et al. Effect of the superflux cellulose triacetate dialyser membranes on the removal of non-protein-bound and protein-bound uraemic solutes. Nephrol Dial Transplant. 2007; 22:2006–2012. 16 Attaluri AC, Huang Z, Belwalkar A, et al. Evaluation of nano-porous alumina membranes for hemodialysis application. ASAIO J. 2009; 55:217–223. 17 Garella S. Extracorporeal techniques in the treatment of exogenous intoxications. Kidney Int. 1988; 33:735–754. 18 Churchwell MD, Pasko DA, Smoyer WE, Mueller BA. Enhanced clearance of highly protein-bound drugs by albumin-supplemented dialysate during modeled continuous hemodialysis. Nephrol Dial Transplant. 2009; 24:231–238. 19 Borkan SC. Extracorporeal therapies for acute intoxications. Crit Care Clin. 2002; 18:393–420. 20 Winters JL, Pineda AA, McLeod BC, Grima KM. Therapeutic apheresis in renal and metabolic diseases. J Clin Apheresis. 2000; 15:53–73. 21 Nenov VD, Mrinov P, Sabeva J, Nenov DS. Current applications of plasmapheresis in clinical toxicology. Nephrol Dial Transplant. 2003; 18(Suppl 5):v56–v58. 22 Holubek WJ, Hoffman RS, Goldfarb DS, Nelson LS. Use of hemodialysis and hemoperfusion in poisoned patients. Kidney Int. 2008; 74:1327–1334. 23 Feinfeld DA, Rosenberg JW, Winchester JF. Three controversial issues in extracorporeal toxin removal. Semin Dial. 2006; 19:358–362. 24 Don BR, Rodriguez RA, Humphreys MH. Acute renal failure associated with pigmenturia or crystal deposits. In: Shreier RW, et al., ed. Diseases of the Kidney and Urinary Tract. Philadelphia: Lippincot Williams & Wilkins; 2007:1184–1207. 25 Guo C, Cenac TA, Li Y, McMartin KE. Calcium oxalate, and not other metabolites, is responsible for the renal toxicity of ethylene glycol. Toxicol Lett. 2007; 173:8–16. 26 Kraut JA, Kurtz I. Toxic alcohol ingestions: Clinical features, diagnosis and management. Clin J Am Soc Nephrol. 2008; 3:208–225. 27 Brent J, McMartin K, Phillips S, et al. Fomepizole for the treatment of ethylene glycol poisoning. N Eng J Med. 1999; 340:832–838. 166 28 Barceloux DG, Krenzelok EP, Olson K, et al. American Academy of Toxicology practice guidelines on the treatment of ethylene glycol poisoning. J Toxicol Clin Toxicol. 1999; 37:537–560. 29 Barceloux DG, Bond GR, Krenzelok EP, et al. American Academy of Toxicology practice guidelines on the treatment of methanol poisoning. J Toxicol Clin Toxicol. 2002; 40:415–446. 30 Moreau CL, Kerns W, Tomaszewski CA, et al. Glycolate kinetics and hemodialysis clearance in ethylene glycol poisoning. J Toxicol Clin Toxicol. 1998; 36:659–666. 31 Phang PT, Passerini L, Mielke B, et al. Brain hemorrhage associated with methanol poisoning. Crit Care Med. 1988; 16:137–142. 32 Hernandez MA, Holanda MS, Tejerina EE, et al. Methanol poisoning and heparin: A dangerous couple? Am J Emer Med. 2004; 22:620–621. 33 Kerns W, Tomaszewski C, Mcmartin K, et al. Formate kinetics in methanol poisoning. J Toxicol Clin Toxicol. 2002; 40:137–143. 34 Hantson P, Haufroid V, Wallemacq P. Formate kinetics in methanol poisoning. Hum Exp Toxicol. 2005; 24:55– 59. 35 Hovda KA, Jacobsen D. Expert opinion: Fomepizole may ameliorate the need for hemodialysis in methanol poisoning. Hum Exp Toxicol. 2008; 27:539–546. 36 Kan G, Jenkins I, Rangan G, et al. Continuous haemodiafiltration compared with intermittent haemodialysis in the treatment of methanol poisoning. Nephrol Dial Transplant. 2003; 18:2665–2667. 37 Hirsch DJ, Jindal KK, Wong P, Fraser AD. A simple method to estimate the required dialysis time for cases of alcohol poisoning. Kidney Int. 2001; 60:2021– 2024. 38 Watson PE, Watson ID, Batt RD. Total body water for adult males and females estimated from simple anthropometric measurements. Am J Clin Nutr. 1980; 33: 27–39. 39 Youssef GM, Hirsch DJ. Validation of a method to predict required dialysis time for cases of methanol and ethylene glycol poisoning. Am J Kidney Dis. 2005; 46:509–511. 40 O’Malley GF. Emergency department management of the salicylate-poisoned patient. Emerg Med Clin N Am. 2007; 25:333–346. 41 Stolbach AI, Hoffman RS, Nelson LS. Mechanical ventilation was associated with acidemia in a case series of salicylate-poisoned patients. Acad Emerg Med. 2008; 15:866–869. 42 Freier S, Neal BW, Nisbet HIA, Rees GJ, Wilson F. Salicylate intoxication treated with intermittent positivepressure ventilation. Br Med J. 1957; 1:1333–1335. 43 Mascheroni D, Kolobow T, Fumagalli R, et al. Acute respiratory failure following pharmacologically induced hyperventilation: An experimental animal study. Intensive Care Med. 1988; 15:8–14. Hemodialysis International 2010; 14:158–167 Dialysis in the poisoned patient 44 Higgins RM, Connolly JO, Hendry BM. Alkalinization and hemodialysis in severe salicylate poisoning: Comparison of elimination techniques in the same patient. Clin Nephrol. 1998; 50:178–183. 45 Dargan PI, Wallace CI, Jones AL. An evidence based flowchart to guide the management of acute salicylate (aspirin) overdose. Emerg Med J. 2002; 19:206–209. 46 Proudooft AT, Krenzelok EP, Brent J, Vale JA. Does urine alkalinization increase salicylate elimination? If so, why? Toxicol Rev. 2003; 22:129–136. 47 Cohen DL, Post J, Ferroggiaro AA, Peron J, Foster MH. Chronic salicylism resulting in noncardiogenic pulmonary edema requiring hemodialysis. Am J Kidney Dis. 2000; 36:E20. 48 Dugandzic RM, Tierney MG, Dickinson GE, et al. Evaluation of the validity of the Done nomogram in the man- Hemodialysis International 2010; 14:158–167 49 50 51 52 agement of acute salicylate intoxication. Ann Emerg Med. 1989; 18:1186–1190. Pierce RP, Gazewood J, Blake RL Jr Salicylate poisoning for enteric-coated aspirin. Delayed absorption may complicate management. Postgrad Med. 1991; 89:61–62, 64. Karvellas CJ, Bagshaw SM, McDermid RC, et al. Acetaminophen-induced liver failure treated with single-pass albumin dialysis: Report of a case. Int J Artif Organs. 2008; 31:450–455. Lund B, Seifert SA, Matersohn M. Efficacy of sustained low-efficiency dialysis in the treatment of salicylate toxicity. Neph Dial Transplant. 2005; 20:1483–1484. Higgins RM, Connolly JO, Hendry BM. Alkalinization and hemodialysis in severe salicylate poisoning: Comparison of elimination techniques in the same patient. Clin Nephrol. 1998; 50:178–183. 167