A Minute for the Medical Staff
advertisement

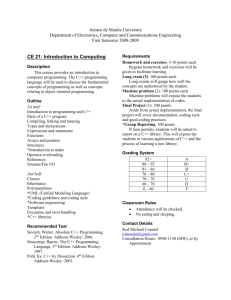
A Minute for the Medical Staff A supplement to medical records briefing February 1999 Know the E&M documentation guidelines and prevent a loss in revenue By Thomas Sills, MD Chief Financial Resource, Inc. Evaluation and management (E&M) coding – the way in which medical practices are paid for most E&M services – is a problem for many physicians because documenting these services is confusing and complicated. However, since undercoding leads to a loss in revenue and overcoding puts you at risk for a fraud and abuse investigation, it’s critical that you code these services properly. Unfortunately there are a lot of grey areas with E&M coding, especially when it comes to which documentation guidelines to use. Currently, physicians may use either the American Medical Association’s (AMA) 1995 or 1997 guidelines. In the spring, the AMA hopes to pilot test a brand new set of guidelines, which it claims will be simpler to follow. It’s unclear when these new guidelines will actually go into effect or how simplified they will be, however. What you should do now Until the new guidelines come out, you should choose either the AMA’s 1995 or 1997 guidelines to follow and ensure that either you or your staff know how to apply them correctly. According to both sets of rules, coding (and payment) is based only on what you document. For coding and billing purposes, if it isn’t documented, then it didn’t happen. Obviously, you only document what you do, and only do what is medically necessary. By knowing the coding rules, you can efficiently document the data that you are actually gathering to allow for complete and accurate coding (and billing.) Documentation tips E&M coding guidelines are primarily based on three components: history, physical exam, and medical decision-making. History Physicians usually find history the most difficult to document, which sometimes prevents the assignment of the appropriate E&M level. HPI: There are two levels of HPI, brief and extended. Brief has one to three elements and extended has four or more. The elements are specifically defines as severity, duration, timing, context, modifying factors and associated signs and symptoms. For average to complex cases, document four or more elements of the HPI. ROS: Any case except the most simple should have at least one symptom reviewed and documented. Comprehensive evaluations require 10 or more systems or the specific statement that “all other systems were negative.” PFHSx: In all except the most complicated cases, document one of these three elements (past, family or social hx). In comprehensive cases, document all three. For patients who can not give a history, document “Patient unable to give history.” Physical exam Based on both the AMA’s guidelines in place since 1995, all but the most minor cases need documentation of more than one body system or area examined. Comprehensive exams need eight or more systems or body areas examined. The exams are defined as * Constitutional * chest / breast * respiratory * ENT * Neurologic * GU * Skin * cardiovascular * eyes * psychiatric * GI * neck * lymphatic * musculoskeletal Medical decision-making The coding rules for medical decision-making are the least explicit. Document the following when feasible for full and accurate coding: Diagnosis or assessment (including differential diagnosis) Treatment Tests ordered Additional history from family Referrals to other physicians Test results Reviews of old records Procedures Example of proper and improper documentation of one E&M coding case The following office record entry is poorly documented from a coding perspective. A 66 y/o female presents with a complaint of D.O.E. for 4 months. She denies chest pain or other symptoms. She denies cough, sputum production, abdominal pain, melatonic stools, change in bowel habits, ankle edema, or claudication of the legs. Pt. is on no meds and past hx is positive for appendectomy and cholecystecotmy years ago. She has a 40-pack-ayear history of smoking and quit 2 years ago. NAD P78, R 16, BP 140/90 neck-no bruits HEENT - unremarkable Cor-RRR, II/VI SEM at Lungs - clear to A and P LSB 4th ICS Abd - soft, non tender Neuro - motor, sensory, CN intact Ext – no edema Imp: D.O.E., ? etiology Plan: CXR, EKG, cbc, lytes, thyroid panel, chem profile. Follow up in 5 days. This visit would be coded to 99202 – new patient level 2. Compare this to the following entry which is effectively documented for the exact same visit which now can be coded to 99204 – new patient level 4. A 66 y/o female presents as a new patient with moderate D.O.E. for 4 months, brought on by walking over 100 feet, resolving after 2 minutes rest. No current meds. Past Hx – Appy and cholecystectomy 1960s Soc. Hx – 40 pk-yrs, quit 2 years ago Fm Hx – neg for heart disease ROS – no weight change, visual disturbance + chronic sore throat and slight sputum production; no melena, dysuria, ankle edema, joint pain, rashes, syncope NAD P78, R16, BP 140/90 skin – no rashes or lesions HEENT–PERRL, EOM intact: pharynx red, no masses Neck – no bruits lungs – clear to A and P Cor – RRR, II/VI SEM Abd – no masses, guiac neg stool: Ext – no edema, full ROM bilateral: Neurooriented x 3, CN intact Imp: D.O.E., ? etiology Plan: CXR, EKG, cbc, lytes, thyroid panel, chem profile. Follow up in 5 days. The difference between the two entries are the second entry has a. four-plus elements of the HPI, the first only has three b. past medical, family, and social hx documented c. 10 systems in the ROS d. more than eight systems documented as examined A Minute for the Medical Staff is an exclusive service for subscribers to Medical Records Briefing. Reproduction of A Minute for the Medical Staff within the subscriber’s institution is encouraged. Reproduction of any form outside the subscriber’s institution is forbidden without prior written permission.