The Climacteric

The Climacteric
CAUSE OF THE MENOPAUSE
No single all-inclusive theory adequately explains the menopause. However, there is no doubt that the ovary is primal to the menopause. The exhaustion of gonadotropinresponsive follicular units is responsible for the reduction of estrogen secretion and the cessation of menses. The average age of a woman at menopause has remained unchanged since the sixth century. The average age of a woman at menopause is now
51.4 years, with a standard deviation of 3.8 years. The age at which menopause occurs is unaffected by race, socioeconomic status, number of pregnancies, oral contraceptive use, education, physical characteristics, alcohol consumption, age of menarche, or date of last pregnancy. Only cigarette smoking has conclusively been shown to hasten follicular exhaustion.
OVARY AND THE MENOPAUSE
The ovary develops on the medioventral border of the urogenital ridge, adjacent to the kidney and the primitive adrenal. Until 42 days of gestation the gonads are indifferent (e.g., on a morphologic basis, the ovary and testis are indistinguishable. This indifferent gonad is formed from a proliferation of the mesodermal coelomic epithelium, the mesenchymal cell mass on the urogenital ridge, and mesonephric elements. Additionally, the indifferent gonad contains large primordial germ cells that migrated from the yolk sac to the genital ridge during the fifth week of embryonic life.
The 300 to 1300 primordial germ cells that have seeded the indifferent gonad will become either oogonia or spermatozoa. In females they undergo mitosis to form oogonia. The oogonia replicate so that there are approximately 600,000 by the eighth week of gestation and 6 million to 7 million by the 20th week of gestation.
Between the eighth and 13th weeks of gestation, under the influence of a meiosisinducing substance secreted by the rete ovarii, meiosis is initiated. The initiation of meiosis converts the oogonia to primary oocytes, some of which become surrounded by precursors of granulosa cells, thus creating primordial follicles. Conversion of oogonia to primary oocytes and the formation of primordial follicles are not completed until the sixth month after birth. Primary oocytes that do not form primordial follicles
degenerate. It has been estimated that of the 6 million oogonia present in the fetal ovaries at 20 weeks' gestation, only 700,000 to 2 million will form primordial follicles.
Thus the human female has a variable but finite number of primordial follicles.
The primordial follicles present at birth are lost from the ovary by either ovulation or follicular atresia. Follicular atresia is the physiologic degeneration of the oocyte and its surrounding stroma. Atresia begins in the fifth month of fetal life and continues until all follicles are exhausted. Atresia occurs continuously during the menstrual cycle and even during pregnancy. The factors that determine whether a primordial follicle ovulates or undergoes atresia are unknown. The total number of oocytes at puberty and the efficiency of the atretic process may determine the age of menopause.
Some primordial follicles can still be found in the ovaries of postmenopausal women. This suggests that the more functionally normal follicles are depleted first.
Thus, as a woman ages, she is left with more gonadotropin-resistant, less hormonally active follicles. This concept may help to explain the signs and symptoms of the climacteric.
As the number of quality follicular units declines, the ovary undergoes gross and microscopic changes. Ovarian weight declines from 14 g in the fourth decade to approximately 5 g postmenopausally. Microscopic examination of the postmenopausal ovary reveals the remaining primordial follicles undergoing follicular atresia. The ovarian stroma is also more prominent, with increased numbers of medullary stromal and interstitial cells.
SYSTEMIC CHANGES WITH AGING
Senescence is the process or condition of aging. The term disease is defined as a morbid process with a characteristic train of symptoms. Senescence produces its own symptoms that in a young person would be considered a disease. Physicians have been unwilling to accept involution and the symptoms that aging produces as a natural and inevitable phase of life. Because the menopause is the most obvious sign of senescence in women, many signs and symptoms, as well as diseases, are incorrectly attributed to gonadal failure. Many organ systems are affected by the aging process independent of gonadal failure.
Nervous System
Neural cells reach maturity and stop dividing in infancy. With normal aging, the brain loses 5% to 10% of its gross weight, and the total number of brain cells decreases
20% to 50%. Aging brain cells show a decline in functional ability. There is significant slowing in the transmission of impulses between neurons, but intraneuronal depolarization remains normal. Cerebral blood flow may decline 30% to 40% with age.
This decrease does not correlate with alterations in cognitive function. All people show some deterioration in short-term memory with age, even in the absence of organic brain disease. Other changes include difficulties with thermoregulation, eyesight, hearing, smell, taste, and touch. The sense of taste shows a particularly dramatic decline with age.
Cardiovascular System
With regard to the cardiovascular system, it is often difficult to tell where normal aging ends and disease begins. Certain changes occur so frequently that they may be normal. Physical changes include hypertrophy of the myocardium and calcification of the heart valves. There is a decrease in maximal oxygen consumption that parallels a decrease in cardiac output. This decline is at the rate of 1% per year, starting in the third decade. The aging heart usually functions well for everyday activities but has significantly diminished reserves for stress.
Respiratory System
Some amount of emphysema is inevitable with advancing years. The alveolar septal membranes weaken and break down, leaving depleted alveoli. Normal aging also causes the collagen in the septa to become rigid. This rigidity causes a restrictive limitation on pulmonary functions. There is a diminution in vital capacity, maximum breathing capacity, and an increase in residual volume. In people 75 years of age maximum inspiratory and expiratory pressures may have dropped 50% and voluntary ventilation, 60%.
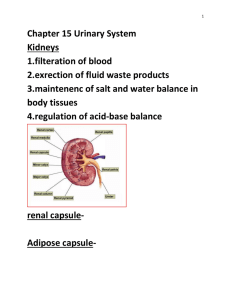
Urinary Tract
The aging kidney has a diminished ability to clear medications. This may be a reflection of the decrease in cardiac output, which decreases renal plasma flow. The
kidney may also lose the ability to concentrate urine. On microscopic examination the aging kidney will show evidence of interstitial fibrosis, tubular atrophy, and glomerular degeneration.
Gastrointestinal System
Few structural changes occur in the gastrointestinal tract, but digestive disorders are common among the elderly. There is age-related atrophy of the intestinal mucosa and marked reduction in gastric secretions. This results in an increased incidence of gallstones, gastrointestinal cancer, and diverticulosis with advancing age.
Immune System
The immune system shows a steady decline in function from adolescence to death.
The reasons for this are unknown. Histologically, there is a reduction in the number of stem cells in the bone marrow, an increase in B - cells in the spleen and lymph nodes, and a decrease in circulating lymphocytes. Functionally, there is a decrease in antibody response of B cells to antigens, an increase in autoantibodies, a decrease in proliferative responses of T - cells and B - cells, and changes in modulators to include B-cell suppression and helper T-cell formation.
Skin and Musculoskeletal System
The skin loses its subcutaneous fat and elasticity with age. This results in skin that is easily traumatized and slow to heal. The increased incidence of arthritis in elderly people is partly due to degenerative changes in the articular surfaces and perichondrial margins of the joints.
Endocrine System
The pituitary loses 20% of its volume by the ninth decade of life, but still maintains normal concentrations of growth hormone, adrenocorticotropic hormone, and thyroid-stimulating hormone. Anatomically, the thyroid gland undergoes progressive fibrosis with age. In people who are older than 50, concentrations of triiodothyronine are diminished by 25% to 40%. Still, elderly patients remain clinically euthyroid.
Beta-cell degeneration of the pancreas progresses with age. By age 65, 50% of patients have chemically abnormal responses to the glucose tolerance test. Frank diabetes is clinically evident in only 7%.
REPRODUCTIVE ENDOCRINE CHANGES IN THE CLIMACTERIC
WOMAN
Hypothalamus-Pituitary
Changes in the hypothalamic-pituitary-gonadal axis are responsible for the menstrual irregularity associated with the perimenopause. As women approach the age of menopause their menstrual interval lengthens. The luteal phase remains 14 days, but the follicular phase often lengthens. The prolonged follicular phase is probably due to the diminished supply of gonadotropin-sensitive follicles. These gonad-otropininsensitive follicles take longer to reach preovulatory estrogen levels. When the preovulatory estrogen levels are not attained an anovulatory cycle results. Sherman and associates compared luteinizing hormone (LH), follicle-stimulating hormone (FSH), estradiol, and progesterone levels during the menstrual cycles of eight women aged 46 to 56 years with those of ten women aged 18 to 30 years. Throughout the menstrual cycle the older women had higher FSH levels, lower estradiol levels, but equivalent LH levels compared with the younger women.
During the perimenopause FSH values of 40 mlU/ml or more are often found.
Values greater than 100 mlU/ml almost certainly indicate follicular exhaustion. FSH levels for the first time since puberty exceed LH levels. The maximal increase in LH and FSH levels occurs two to three years after menopause. Gonadotropin concentrations over the next five decades remain stable or decrease slightly. In contrast, surgical menopause results in rapid and dramatic changes in FSH and LH levels. Twenty days after oophorectomy FSH values are greater than 70 mlU/ml and LH values are greater than 50 mlU/ml. Maximum concentrations are reached by 45 days. Estrogen replacement therapy will significantly lower LH and FSH levels but usually not to premenopause levels. The inability to reduce FSH and LH levels to normal values is explained by the loss of inhibin production from ovarian granulosa cells.
As peripheral gonadotropin levels rise, abnormal pulse patterns of LH are observed. The menopausal woman has a pulse frequency of ten to 20 minutes compared with the 90- to 120-minute pulse frequency in the early follicular phase of reproductive women. There also appears to be a loss of opioid inhibition of gonadotropin release in
postmenopausal women. The physiologic significance of these changes remains unknown at this time.
Although there is no appropriately sensitive or specific assay for measuring gonadotropin releasing hormone (GnRH), the increased pulse frequency and amplitude of LH release are probably the result of increased GnRH release. The results of a few published reports on serum and urine GnRH levels in postmenopausal women indicate an overall increase. Administration of GnRH to a postmenopausal woman results in an
LH and FSH response similar to that in a reproductive woman, although the response is greater in magnitude. This may be due to diminished circulating estradiol concentrations and, therefore, diminished negative feedback on GnRH.
Estrogen Production
The predominant estrogen of the postmenopausal woman is estrone. The biologic potency of estrone is only one-third that of estradiol. Virtually no estrone is produced by the postmenopausal ovary or adrenal gland. Oophorectomy in postmenopausal women produces no discernible change in circulating estrone or estradiol levels. Most estrone is formed by the peripheral conversion of androstenedione by extraglandular aromatase.
Aromatase has been identified in the liver, fat, and certain hypothalamic nuclei. The activity of extraglandular aromatase is age and weight dependent and increases twofold during the perimenopause. Production rates post-menopausally are 40 μg per day for estrone and 6 μg per day for estradiol, compared with 80 μg to 500 μg per day for estradiol and 80 μg to 300 μg per day for estrone in reproductive-age women.
Androgen Production
Fuller Albright, in 1942, suggested that there was an "adrenopause" as well as a menopause. He made this statement on the basis of a 20% and 40% decrease in dehydroepiandrosterone sulfate (DHAS) levels and dehydroepiandrosterone (DHA) levels, respectively, in postmenopausal women. Estrogen replacement produces a twofold increase in DHAS values. Therefore, the magnitude of the diminished concentrations of the two androgens is probably due to estrogen deprivation. Serum
Cortisol concentrations remain unaffected by estrogen therapy. In vitro data suggest that estrogen is a noncompetitive inhibitor of 3β-hydroxysteroid dehydrogenase. A relative
block at this site would augment DHA and DHAS production.
Androstenedione, the most extensively produced androgen in reproductive-age women, declines in the climacteric. Androstenedione production decreases from 1500 pg to 800 pg/ml in postmenopausal women. Overall, the postmenopausal ovary contributes only 20% to the circulating androstenedione. Testosterone levels in the postmenopausal woman decline but not to the same extent as those of estrogen. In the premenopausal woman circulating testosterone is derived from three sources: the ovary
(25%), the adrenal gland (25%), and extraglandular conversion from androstenedione
(50%). The postmenopausal ovary produces a larger percentage of testosterone than does the premenopausal ovary, yielding about 50% of circulating concentrations.
THE MENOPAUSAL SYNDROME
Many signs and symptoms that are attributable to aging have been erroneously attributed to estrogen deprivation. For a symptom to have been caused by estrogen deprivation, it should occur in patients of any age after ovarian failure (natural or surgical), and must be relieved with the addition of estrogen. Signs and symptoms of the menopause can be classified as (a) definitely estrogen deficiency-related, (b) probably estrogen deficiency-related, or (c) possibly hormone-related. Definite hormone-related symptoms are genitourinary atrophy, vasomotor instability, and osteoporosis. Probable hormone-related symptoms include atherosclerotic cardiovascular disease and psychosocial symptoms of insomnia, fatigue, and, possibly, depression.
Vasomotor Symptoms
Hot flashes are experienced by 75% to 85% of peri-menopausal and postmenopausal women. Thirty-seven percent to 50% of premenopausal women after bilateral oophorectomy likewise develop hot flashes. Vasomotor symptoms are most common in the early menopause. Eighty percent of women who experience hot flashes have symptoms for more than one year, but less than 25% have symptoms for more than five. The hot flash is described as a warmth that begins in the face and spreads to the chest, and is often accompanied by a visible red flush. The hot flash is episodic rather than continuous and is frequently associated with nausea, dizziness, headache, palpitations, diaphoresis, and night sweats.
Cause of Hot Flashes
Meldrum and associates have standardized a technique for measuring changes in skin temperature during hot flashes and have noted a mean interval of 54 ± ten minutes between hot flashes. These investigators also found that the subjective sensation of warmth precedes any changes in skin temperature and is over before the maximal peripheral change is measured. Therefore, the origin of a hot flash is not due to a peripheral disturbance. Several investigators have tried to correlate the hot flash with circulating levels of gonadotropins. There is no difference in the ratio of LH to FSH or total estrogens in patients with vasomotor symptoms compared with those without.
Meldrum and co-workers also failed to identify any significant change in the estrone or estradiol level at the time of reported hot flashes. Interestingly, increases in DHA, androstenedione, and Cortisol were noted ten to 20 minutes after observed hot flashes.
The significance of these observations is unknown. Hot flashes do not occur in women with gonadal dysgenesis who have not been exposed to exogenous estrogen. A close temporal relation between each hot flash and a pulse of LH has been observed. This suggests that either LH itself or factors that initiate the release of LH are responsible for hot flashes in patients with gonadal failure. To determine which is responsible,
Meldrum and co-workers studied women with pituitary insufficiency and found both subjective and objective evidence of hot flashes. Thus it seems that LH elevation per se is not responsible for the hot flash.
These studies suggest that hypothalamic factors that stimulate LH release are responsible for the hot flash. The hypothalamic centers that control thermoregulation are located in the preoptic and anterior hypothalamic nuclei. The four neurotransmitters active in these nuclei are GnRH, norepinephrine, dopamine, and β-endorphin, all of which affect gonadotropin secretion. Because dopamine and β-endorphin exert inhibitory influences on gonadotropin secretion, they probably do not play a role in hot flashes. Because norepinephrine stimulates gonadotropins, it is more likely to play a role. Given that hot flashes occur in patients with Kallman's syndrome after discontinuation of estrogen replacement, GnRH itself is probably not primal to the initiation of the hot flash. In ovariectomized rats there is an increase in the concentration
and turnover of hypothalamic norepinephrine. In humans, clonidine (an α-adrenergic agonist-antagonist) can be used to treat hot flashes fairly effectively. Therefore, one possible explanation of the origin of the hot flash is that gonadal failure may increase hypothalamic norepinephrine, which increases pulsatile GnRH and, subsequently, LH.
The increase in norepinephrine results in activation of the autonomic nervous system that controls thermoregulation.
Experimental evidence suggests that estrogen deficiency is the primary abnormality that affects the hypothalamic neurons that produce the hot flash. Although serum concentrations of estrogen are similar in women with and without symptoms, there appears to be a difference between the groups in biologically available estrogen.
Animal studies have shown that only estrogen not bound to sex hormone-binding globulin is available to be transported across the blood-brain barrier and into the brain tissue. Erlik and co-workers have been able to predict which women would have hot flashes on the basis of biologically available estradiol.
Estrogen has traditionally been the drug of choice to relieve hot flashes. However, a number of other drugs can effectively suppress hot flashes. These agents are particularly useful in women who have a contraindication to estrogen replacement therapy. Medroxyprogesterone acetate, 10 mg orally daily or 100 mg injected monthly, is very effective. Bellergal, an ergot alkaloid, has been found to be slightly effective in the treatment of hot flashes. Clonidine, 0.1 mg to 0.2 mg twice a day, is also effective.
However, in nonhypertensive patients side effects are common.
Genitourinary Atrophy
The vagina, vulva, urethra, and trigone of the bladder share embryonic proximity, and contain large numbers of estrogen receptors. Therefore, genitourinary senescence is modified by the amount of circulating estrogen. Genitourinary tissues do not atrophy at the same rate. The atrophy begins in the premenopausal period and continues over many years. The vulva, although not derived from miiller-ian structures, undergoes accelerated atrophy with estrogen deprivation. Age alone causes thinning of the hair of the mons and shrinkage of the labia minora. The labia majora flatten as the subcutaneous fat and elasticity of the structures diminish.
The most common vulvar symptom of the menopause is pruritus. Estrogen replacement is usually quite effective in relieving the pruritus. However, vulvar dystrophies also present with pruritus vulvae. It is important to separate dystrophy from simple atrophy, as squamous cell carcinoma is present in 5% of vulvar dystrophies on initial examination and may develop in another 5% in the succeeding three to five years after diagnosis. Estrogen deprivation does not appear to be a primary causal factor in vulvar dystrophy or carcinoma.
With estrogen loss the vagina becomes pale and its epithelium thins, resulting in diminished distensibility and reduced secretion. The estrogen-deficient vagina is easily traumatized. Vaginal trauma may account for as much as 15% of all postmenopausal bleeding. The incidence of vaginitis increases during the postmenopausal years.
Estrogen deficiency changes the vaginal pH from 3.5 to 4.5, to 6.0 to 8.0. The alkaline environment predisposes the vagina to ' colonization by a multitude of bacterial pathogens. Estrogen administered systemically or intravaginally reverses the thinning of the vaginal mucosa and lowers vaginal pH. Treatment must be continuous for one to three months. After the initial continuous therapy only intermittent therapy is necessary to maintain the effect.
Postmenopausally, the three cervical lesions erosion, ectropion, and ulcer become more common.
Endocervical glandular tissue becomes less active ir the menopause and produces only scant mucin. This contributes to the overall vaginal dryness that is often a presenting complaint. The squamocolumnai junction and transformation zone migrate high intc the endocervical canal. This may pose a problem foi accurate colposcopy if
Papanicolaou smears show an abnormality.
The incidence of descensus of the uterus, cysto-cele, and rectocele is increased in the climacteric There is little evidence to suggest that estrogen deprivation is the cause.
Probably the increase in incidence is due to estrogen loss coupled with age-related slowing of cell division a.nd a decrease in tissue elasticity. The urethra is also affected by estrogen loss. The distal urethra may become rigid and inelastic. This predisposes to the formation of ectropion (urethra carunculae), diverticula, and urethrocele. The most
common problem in postmenopausal women related to urethral changes is the "urethral syndrome." The urethral syndrome consists of burning, frequency, hesitancy, nocturia, and urgency. The diagnosis is made when these symptoms are associated with sterile urine cultures. This condition is treatable by estrogen therapy, urethrotomy, or urethral dilation. Despite the changes in the urethra and supporting pelvic fascia, there does not appear to be any increase in the incidence of true stress urinary incontinence.
Bacteriuria is found in 7% to 10% of postmenopausal women compared with 4% of premenopausal women. The higher incidence in postmenopausal women may be due to mucosal atrophy and increased vaginal contamination caused by the lowering of the external urethral orifice into the anterior vaginal canal. Estrogen therapy frequently improves urinary frequency, dysuria, nocturia, urgency, post-void dribbling, and, to some extent, stress urinary incontinence. Additionally, estrogen causes proliferation of the vaginal epithelium and can provide relief from the symptoms of vaginitis and frictional dyspareunia.
Osteoporosis
Osteoporosis is a condition in which the bone has' lost sufficient mass to become predisposed to mechanical failure (fracture). It is classified as either primary or secondary. Primary osteoporosis is often referred to as senile osteoporosis and usually affects women between the ages of 55 and 70. The most common sites of fracture are the vertebra and long bones of the arms and hips. Secondary osteoporosis is defined as pathologic fracture owing to a specific disease. Many diseases have been recognized as causing osteoporosis.
It is estimated that one in three women in the United States will develop some complication of osteoporosis postmenopausally. Postmenopausal osteoporosis is the cause of 1.3 million fractures each year. Most of the 250,000 hip fractures that occur in people over age 45 are due to primary osteoporosis. After hip fracture approximately
15% of patients will die within one year, usually because of some complication related to prolonged immobilization. Perhaps equally as tragic is that 75% of hip fracture patients will lose their independence. About 25% of hip fracture patients will require prolonged skilled nursing care. Besides the human suffering caused by osteoporotic hip
fractures, the economic impact of this disease is tremendous. Between $7 billion and
$10 billion a year are spent treating complications of osteoporosis.
The Menopause and Bone Loss
In both sexes maximal skeletal mass is obtained by age 35. By age 50 both men and women have begun to experience a generalized loss of bone. Throughout, women have significantly less bone mineral content then do men of similar age and race. After oophorectomy bone loss averages 3.9% per year for the first six years after surgery and
1% per year thereafter. Overall bone loss after natural menopause averages 1% to 2% per year. By the age of 80 some untreated white women have lost 30% to 50% of their skeletal mass.
A woman's genetic background, lifestyle, and dietary habits, coexisting endocrine disease, and age of menopause are the major factors that determine whether or not she will develop osteoporosis. Bone density parallels skin pigmentation, with blacks having more bone mineral mass then whites. Women with a family history of osteoporosis are at increased risk.
The value of exercise in the development and prevention of osteoporosis is poorly understood. Inactivity produces muscular and skeletal degeneration. Astronauts on long space missions who did not exercise showed a significant loss of bone mineral content.
Exercise in outer space was found to prevent bone loss. Unfortunately the type of exercise that will produce a positive bone balance has yet to be defined. However, some type of weight-bearing exercise would appear to be the best. Cigarette smoking and caffeine and alcohol consumption are factors that can be associated with osteoporosis.
Whether they are independent lifestyle risk factors or confounders has yet to be determined.
Dietary habits determine whether enough calcium is present for effective bone formation. Heaney and associates demonstrated that calcium intake in the United States is well below the level of calcium lost from the body. In the average postmenopausal woman there is a negative calcium balance of 40 mg per day. It is currently recommended that postmenopausal females ingest a minimum of 1500 mg of calcium per day.
Premature menopause is an extreme risk factor for developing osteoporosis. Data from the Mayo Clinic demonstrated that women who had undergone a oophorectomy approximately 20 years before (current mean age 50 years) and postmenopausal controls who had reached natural menopause 20 years before (current mean age 70 years) had similar bone mineral masses. Both groups showed approximately 15% to
18% reduction in radial bone mass.
Estrogen and Bone Mineral Metabolism
Bone is continuously being deposited and resorbed. Resorption and formation are coupled in time, degree, and quality. This continuous remodeling provides a mechanism for bone repair and for liberation of calcium from skeletal stores on demand.
Two cells, the osteoblast and the osteoclast, are responsible for bone remodeling.
Bone resorption initiates the process. The osteoclasts, which are derived from the bone marrow, attach to the bone and dissolve the mineral and organic matrix, thus creating a lacuna. The osteoclasts are then replaced by cells that resemble macrophages. These cells digest any remaining organic matrix and elaborate a signal that recruits the osteoblasts. The osteoblasts that come from the bone marrow deposit an amorphous organic matrix called osteoid. The precipitation of calcium and phosphate to form hydroxyapatites results in hardening of the osteoid. A bone remodeling cycle takes approximately 100 days. On the average, 1 mg to 2 mg (0.02%-0.04%) of the skeleton is formed and resorbed daily.
The bone remodeling process is controlled systemically by the parathyroid hormone (PTH), vitamin D, and calcitonin. Local factors such as interleukin-1 also play a role in the remodeling process.
Calcium plays a crucial role in the maintenance of skeletal integrity. Of the 1 kg to
2 kg of calcium in the body, 98% is contained in bone. PTH is the critical modulator of calcium balance. In response to hypocalcemia, PTH exerts these effects: (a) stimulation of renal mitochondria alphai-hydroxylation, which converts 25-hydroxyvitamin D to the biologically active form alphai-25-dihydroxyvitamin D; (b) direct action on bone, causing rapid release of calcium within several minutes; and (c) reduction in renal calcium clearance rate with augmented tubular resorption of calcium after glomerular
filtration. Bone remodeling is a late affect that occurs several hours after PTH infusion, during which time osteoclast increase in number and activity (Fig. 43-4).
Vitamin D deficiency also causes substantial bone loss. Vitamin D is a hormone derived from 5,7 diene steroids. The parent compound is acquired from dietary sources or photobiosynthesis in the skin. Vitamin D exists in three forms with varying biologic activities. Vitamin D, the weakest form, is first hydroxy la ted in the liver to form 25hydroxyvitamin D. The second hydroxylation to alphaj-25-hydroxy-vitamin D occurs in the kidney, and produces the most active form of vitamin D. The hydroxylase enzyme in the kidney is under the influence of PTH. Alpha
1
-25-dihydroxyvitamin D stimulates the absorption of both calcium and phosphorus from the intestinal lumen into the circulation. Long-term vitamin D deficiency reduces intestinal absorption of calcium, requiring the bone to be the main source of serum calcium.
Calcitonin, derived from the C cells of the thyroid gland, inhibits osteoclastic activity and lowers serum calcium. Estrogen, like calcitonin, opposes the re-sorptive action of PTH. Estrogen loss appears to make the bone more sensitive to the affects of
PTH. The increase in serum calcium which suppresses PTH release and subsequently reduces alpha
1
-25-dihydroxyvitamin D, lowers calcium absorption.
Because the body is deprived of its intestinal source of calcium, the bone becomes the primary source of calcium. Some studies indicate that calcitonin production declines with estrogen deficiency. A recent article in Science has definitely demonstrated that there are estrogen receptors within the bone. It is, therefore, likely that estrogen, like calcitonin, modulates bone remodeling directly by either inhibiting osteoclast activity or stimulating osteoblastic activity.
Estrogen Therapy to Prevent Osteoporosis
Although the exact mechanism by which estrogen prevents bone loss is unknown, several large clinical studies have demonstrated a causal relation between estrogen deprivation and accelerated bone loss. In a ten-year double-blind prospective study by
Nachti-gall and colleagues a dramatic difference in bone mineral density was found between estrogen-treated and placebo-treated patients if estrogen therapy was begun within three years of the loss of ovarian function. More important, there was a
significant difference in the number of fractures between estrogen-treated and placebotreated patients. In this study seven of the 62 placebo-treated patients but none of the 67 estrogen-treated patients had fractures.
Cessation of estrogen therapy results in rapid and progressive loss of bone mineral content. Lindsay and co-workers reported a 2.5% per year average rate of loss of bone mineral content among women whose estrogen replacement therapy had been stopped.
This rate of bone loss is comparable to the rate of bone loss during the first two years after bilateral oophorectomy. In Lindsay's study four years after cessation of estrogen therapy total bone mineral content in formerly treated patients was equivalent to that in women who had never received estrogen treatment.
Although it is known that estrogen given to early menopausal women can retard bone loss, the role of estrogen in the treatment of established osteoporosis " is less clear.
Two large uncontrolled studies suggested that estrogen reduces the rate of fractures in patients who had at least one osteoporotic fracture at the start of therapy. These data suggest that estrogen may be useful in the treatment of established disease. However, the doses used for treatment are higher than those used for prevention, and thus may be associated with a greater likelihood of side effects.
The dosage of estrogen necessary to prevent bone loss depends on its type and route of administration. A dose of 0.625 mg of conjugated estrogen per day provides adequate protection against the development of osteoporosis for most women.
Calcitonin has recently been approved for the prevention and treatment of osteoporosis.
Calcitonin is expensive and must be administered parenterally. The most effective dose of calcitonin is 100 MRC units (100 medical research council units are equivalent to 1 mg) at least three times a week. In smaller doses calcitonin is relatively ineffective.
Other therapies, such as coherence therapy and sodium fluoride, are still investigational.
RISKS OF ESTROGEN THERAPY
Definite Risks
Endometrial Carcinoma
Cholelithiasis
Possible Risks
Breast Cancer
Thromboembolism
Hypertension
Glucose Intolerance
MANAGEMENT OF ESTROGEN THERAPY IN THE MENOPAUSE
Before prescribing estrogen the physician and patient must discuss the potential benefits of therapy versus its potential risks. If a patient possesses an absolute contraindication to estrogen, then the risk-benefit ratio is definitely against estrogen. If the patient has a relative contraindication to estrogen replacement therapy, then the reason for suggesting estrogen replacement therapy must be carefully considered.
Estrogen replacement therapy should be considered in all women who have symptoms related to estrogen deficiency. The symptoms related to estrogen deficiency have been detailed previously in this chapter. All women who are at risk for the development of osteoporosis or who have a strong family history of cardiovascular disease should consider hormone replacement therapy. It has been estimated that estrogen-progestin therapy will prevent 163 deaths if given to 100,000 women over a ten-year period.
Once a decision has been made to prescribe estrogen replacement therapy, the physician is left with three basic questions: (1) which estrogen to prescribe, (2) which dosage and route of administration to use, and (3) how to monitor therapy.
To date, no one estrogen or progestin has been shown to be clinically superior when equivalent doses are compared. The dosage and route of administration have undergone tremendous change since the early 1980s. In the United States estrogen traditionally has been given in a cyclic manner. Estrogen has been administered for the first 25 days of the month and the progestin has been added for the last ten days with a five-day estrogen-free period. This regimen provides excellent protection against
endometrial hyperplasia and carcinoma. Unfortunately, during the estrogen-free days, many women experience a return of estrogen deficiency symptoms. Estrogen has recently been given continuously (i.e., 365 days a year with a progestin added for the first ten to 14 days of the month). Initial data indicate that this method is equally protective against the development of endometrial carcinoma. An additional benefit of prescribing estrogen this way is that the bleeding pattern gives some indication of the status of the endometrium. Whitehead and associates have demonstrated that if a woman begins menstrual bleeding before the tenth day of the month, a proliferative endometrium is likely, and that this group of patients needs a higher dose of progestin as well as endometrial sampling. If the patient begins bleeding after the tenth of the month but before day 18, then there is full secretory transformation.
The dose of estrogen should be the least that will control the symptoms as well as provide protection against osteoporosis. Currently 0.625 mg of conjugated equine estrogen is known to prevent osteoporosis in most women. One cannot assume that an
"equivalent amount" of a different estrogen will prevent bone loss. For optimal protection the estrogen should be supplemented with 1500 mg of calcium daily and an exercise program. Because rapid bone loss follows discontinuation of estrogen therapy, estrogen therapy should be continued until the patient is in her 80s or beyond. Women who receive calcium supplementation initially should have periodic checks of serum calcium and phosphorous to detect otherwise asymptomatic hyperparathyroidism. The dose of progestin that will protect the endometrium as well as produce the least effect on lipids is unknown. However, a dose of 0.35 mg of norethindrone or 5 mg of medroxyprogesterone acetate given for 14 days of the month appears to be adequate to protect the endometrium. Whether to give a progestin to a woman who does not have a uterus is controversial. Data collected by Gambrell suggest that a progestin may protect against breast cancer. Two other studies support this observation. It would appear prudent to individualize to the patient's risk of developing breast cancer.
All patients on hormone replacement therapy should be seen yearly. At the time of the annual examination a thorough medication review should be obtained as well as nutritional information. As people age, their nutritional habits decline, and those who
previously did not need calcium supplementation may require it. During the annual examination it is necessary to screen the patient for other carcinomas. A breast and pelvic examination, a Papanicolaou test, and a fecal occult blood test are mandatory. It is not unreasonable to recommend that the patient use a home stool guaiac kit
(Hemoccult) at least four times during the year. Right-sided colon cancers bleed intermittently, and a single stool guaiac test may miss an early colon cancer. The physician at this visit should also stress the need for mammography and should follow the National Institutes of Health's guidelines for lipid screening.
If a patient develops abnormal uterine bleeding, then sampling of the endometrium is necessary. Whether periodic endometrial sampling is necessary for all patients on estrogen plus progestin is controversial. Many physicians recommend sampling every one to three years, despite its lack of cost-effectiveness and the patient discomfort it causes.
PREMATURE OVARIAN FAILURE
Premature ovarian failure is defined as cessation of menstruation before age 40.
The term premature ovarian was coined because, initially, it was thought that the patient had no follicles remaining in the ovary. This was considered because most patients presented with FSH levels greater than 40 mlU/ml. However, an occasional patient resumed cyclic menstruation or even became pregnant. Study of these patients and others revealed that premature ovarian failure is a heterogenous disorder with numerous causes.
The exact prevalence of premature ovarian failure is unknown. However, Aimin and Smentek believe that of the 43 million women in the United States of reproductive age, 3% would have primary or secondary amenorrhea. Of these, 10% would have premature ovarian failure, thus giving a frequency of approximately 0.3% of the total reproductive-age population. Coulam and co-workers, examining the records of women in Rochester, Minnesota, calculated the frequency of premature ovarian failure at 0.9%.
The heterogeneity of this syndrome is emphasized in the article by Aimin and
Smentek, who reported on 236 patients, 157 of which had undergone ovarian biopsy.
Eighteen percent of these patients had ovarian follicles present. Twenty-seven women,
11%, had evidence of associated autoimmune disorders. Fourteen of the women conceived after the diagnosis was established, and two of these women had no oocytes on biopsy. This study points out that "ovarian failure" cannot be diagnosed on the basis of ovarian biopsy or elevated FSH levels.
The cause of premature ovarian failure may be " broken down into five categories: genetic, autoimmune, metabolic, environmental, and surgical. Genetic disorders always involve some abnormality of the X chromosome. Two intact X chromosomes are necessary for the maintenance of intact follicles. Structural abnormalities of the X chromosome can lead to premature follicle loss. Premature ovarian failure has been reported in women who have abnormalities of both the short and long arm of the X chromosome. Many of these women who have deletions in the short or long arm will have reproduced, and there will be a familial occurrence.
Many autoimmune diseases have been associated with the development of premature ovarian failure. Usually the ovarian failure is associated with women who have polyglandular failure, including thyroiditis, hypoadrenahsm, and hypoparathyroidism Many investigators have detected antibodies to ovarian tissue in patients with premature ovarian failure. Still, the presence of circulating antibodies does not conclusively prove that these antibodies are the cause of the patient's ovarian failure
Galactosemia is a deficiency of the enzyme galactose-1-phosphate uridyl transferase, involved in galactose metabolism. It appears that high levels of galactose are toxic to oocytes. The exact reason for this is unclear.
Numerous environmental agents can cause oocyte toxicity as well as destruction.
Antineoplastic drugs, especially the alkylating agents, induce amenorrhea in more than
50% of patients. The duration of the amenorrhea is related to the dose and the age of the patient at the time of exposure. Younger women appear to be less affected than older women. Permanent ovarian failure can be caused by 800 cGy delivered over three days.
Patients who receive treatment for Hodgkin's disease typically receive 400 cGy to 500 cGy over four to six weeks. Fifty percent of these women will have permanent ovarian failure. In others only temporary hypergonadotropic amenorrhea will occur.
Unfortunately individual sensitivity cannot be predicted before therapy.
Therapy for premature ovarian failure depends on the patient's desire for pregnancy. Some women, particularly if they have ovarian antibodies, may rebound after a prolonged course of combined estrogen and progestin. Other investigators have achieved pregnancy by pretreatment with estrogen followed by human menopausal gonadotropin. If the patient is not desirous of pregnancy, then hormone replacement therapy is indicated. If the patient is presenting with primary amenorrhea, it is better to start with low-dose estrogen and increase gradually over time. This regimen allows completion of the arrested maturation of the secondary sex characteristics. This is particularly true of women who present with cytogenetic abnormalities such as Turner's syndrome. This slow approach may allow some growth before the estrogen fuses the epiphyses.
Polycystic Ovarian Syndrome
The most common cause of ovarian androgen excess and probably the most common cause of hirsutism in women is PCOS. Goldzieher and Green found nearly a
70% prevalence of hirsutism in women with PCOS. It is likely that PCOS is the end point in a spectra of several physiologic abnormalities. The clinical manifestations, including hirsutism, anovulation, and infertility, are found in more than 50% of women with polycystic ovaries. Other symptoms found in varying frequency include obesity, virilism, and dysfunctional bleeding. Histologically, the classic ovarian finding in PCOS is multiple small follicular cysts with poor granulosa cell development. The follicle is surrounded by a thickened, luteinized theca. The biochemical parameters that define
PCOS remain ill-defined. Patients with the syndrome often have modestly elevated T,
DHEAS, and prolactin (PRL) levels. They often demonstrate a reversal of the estradiohestrone (E2:E1) ratio, and frequently the luteinizing hormone (LH):FSH ratio is greater than or equal to 3:1. Several theories have been advanced to explain the biochemical abnormalities found in PCOS in light of the unique anatomical and physiologic findings. LH is generally elevated in patients with PCOS and may reflect greater pulse frequency and pulse amplitude of LH in response to gonadotropin releasing hormone (GnRH) from the hypothalamus. Because GnRH is the principal stimulant to gonadotropin secretion, abnormalities in its control and secretion have been
sought to explain PCOS. Unfortunately GnRH is not easily or accurately assayed in peripheral samples, and when obtained it is of questionable relevance to hypothalamic events. The neurotransmitter dopamine inhibits hypothalamic GnRH secretion in animals. The results of several studies infer an abnormal dopamine-GnRH dissociation, resulting in elevated GnRH pulse amplitude and frequency. Central opioids also have an inhibitory control over GnRH secretion, and modulate dopamine activity. Again, an inference of abnormal "opioid tone" has been suggested as the cause of anomalous
GnRH secretion. Naloxone infusion studies indicate a normal, intact opioid response in
PCOS, but suggest a possible interactional abnormality between the opioid and dopaminergic pathways. Clearly, more information is needed before the cause of PCOS can be resolved. Nonetheless, the net result is an elevated LH level and a preferential inhibition of FSH. FSH may be affected directly by secretion of inhibin from the multiple follicular cysts of the ovary. The consequence of the abnormal gonadotropin
(LH:FSH) ratio is an LH-induced excess of A'D and T from the ovarian thecal and stromal cells. Without requisite FSH levels the normal granulosa cell aromatization of
A’D and T to E2 in cyclic manner is reduced. Erickson and colleagues have reported a lack of estrogen production in granulosa cells cultured from characteristically small polycysts found in PCOS. However, when FSH was added to these cultures in vitro, estrogen production was greatly increased. Ovarian androgens are peripherally converted to estrogens, which are chronically elevated in noncyclic manner in anovulatory patients with PCOS. The cycle is completed by the continued secretion of pituitary LH, sensitized by the elevated estrogens.