Combined hand-out: contains all the documents below
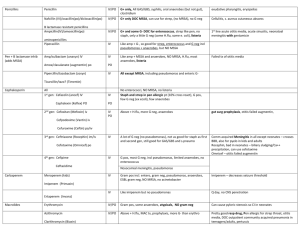
advertisement
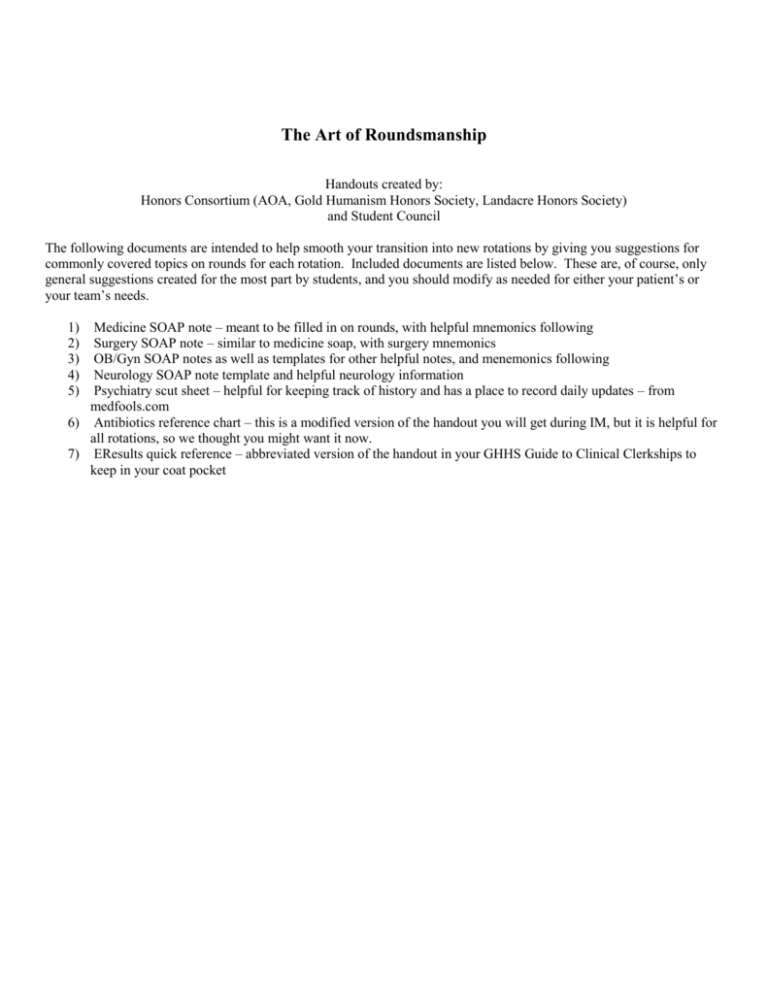
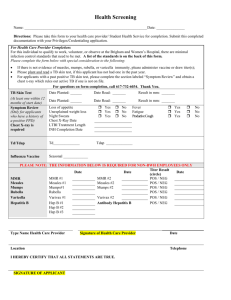
The Art of Roundsmanship Handouts created by: Honors Consortium (AOA, Gold Humanism Honors Society, Landacre Honors Society) and Student Council The following documents are intended to help smooth your transition into new rotations by giving you suggestions for commonly covered topics on rounds for each rotation. Included documents are listed below. These are, of course, only general suggestions created for the most part by students, and you should modify as needed for either your patient’s or your team’s needs. Medicine SOAP note – meant to be filled in on rounds, with helpful mnemonics following Surgery SOAP note – similar to medicine soap, with surgery mnemonics OB/Gyn SOAP notes as well as templates for other helpful notes, and menemonics following Neurology SOAP note template and helpful neurology information Psychiatry scut sheet – helpful for keeping track of history and has a place to record daily updates – from medfools.com 6) Antibiotics reference chart – this is a modified version of the handout you will get during IM, but it is helpful for all rotations, so we thought you might want it now. 7) EResults quick reference – abbreviated version of the handout in your GHHS Guide to Clinical Clerkships to keep in your coat pocket 1) 2) 3) 4) 5) Date Time: MS3 Progress Note (medicine) S: Interval history? Pain? Appetite? NOW THINK: what is happening with my patient? Anything special I need to think about/look for on exam? Anything I don’t understand about what is happening with them? O: VS: Tm I/O: Tc P R BP Sat on Gen: HEENT: Lungs: C/V: Abd: Extremities: Neuro: Antibiotics? Pain meds? DVT prophylaxis? Diet: Labs: Cultures Imaging A/P Day of GI prophylaxis? Fluids? Rate? Hypercalcemia Etiologies - CHIMPANZEES C - Calcium overdose (don’t usually mention this one) H - Hyperparathyroidism, Hyperthyroidism, Hypothyroidism, familial Hypercalcemic hypocalciuria I - Immobility M - Multiple myeloma P – Paget’s disease A – Addison’s disease N – Neoplasms: - metastasis to bones and - hypercalcemia of malignancy (a paraneoplastic syndrome) Z – Zollinger-Ellison syndrome E – Excess vitamin A E – Excess vitamin D S – Sarcoidosis Indications for Acute Hemodialysis - AEIOU A – Acidosis (unable to be managed medically) E – Electrolytes (typically hyperkalemia, unable to be managed medically) I – Intoxication (methanol, ethylene glycol, lithium) O – Overload (fluid overload unresponsive to diuretics) U – Uremia (symptomatic) Causes of delirium – MOVE, STUPID Metabolic Oxygen Vascular Endocrine/Electrolyte Seizures Tumor/Trauma/Temperature Uremia Psychogenic Infection/Intoxication Drugs/Degenerative disease Causes of metabolic acidosis with an anion gap – MUD PILES M – methanol U – uremia D – diabetic ketoacidosis P – para-aldehyde I – Isoniazid, iron, inborn errors in metabolism L – lactic acidosis E – ethanol, ethylene glycol S – salicylates Treatment of Acute MI – MONA M - morphine O - oxygen N - nitrates A – aspirin Date Time: MS3 Progress Note (surgery) S: Interval history? Pain? Bowel movement? Nausea/vomiting? Flatus? Appetite? NOW THINK: what is happening with my patient? Anything special I need to think about? Anything I don’t understand about what is happening with them? O: VS: Tm I/O: Tc P R BP Drains? Sat on Gen: Sick vs well appearing? Lungs: C/V: Abd: Distention? BS? Soft? Tenderness? Guarding? Rebound? Wound: where? Clean? Dry? Intact? Erythema? Drainage? Extremities: Tenderness? Swelling? Warm? Antibiotics? Pain meds? DVT prophylaxis? Diet: Labs: Cultures Imaging A/P Day of GI prophylaxis? Fluids Rate? Etiologies of Postop Fever The 5 W’s Wind (atelectasis, pneumonia) Water: UTI Wound: infection Walking: DVT/PE Wonder drugs: drug fever Causes of Panceatitis I GET SMASHED Idiopathic Fistulas: conditions preventing closure HIS FRIEND: High output (>500mL/day) Intestinal destruction Short segment (<2.5cm) Scorpion bites Mumps (viruses) Infection Autoimmune Steroids Hyperliidemia ERCP Drugs Foreign body Radiation Infection Epithelialization Neoplasm Distal obstruction Gallstones Ethanol Trauma Causes of GI bleeding ABCDEFGHI Angiodysplasia Bowel cancer Colitis Diverticulosis/ Duodenal ulcer Epistaxis/ Esophageal (cancer, esophagitis, varices) Fistula (anal, aortoenteric) Gastric (cancer, ulcer, gastritis) Hemorrhoids Infectious diarrhea/ IBD/ Ischemic bowel Causes of a unilateral swollen leg TV BAIL: Trauma Venous (varicose veins, DVT, venous insufficiency) Baker's cyst Allergy Inflammation (cellulitis) Lymphedema Treatment of acute pancreatitis MACHINES: Monitor vital signs Analgesia/ Antibiotics Calcium gluconate (if deemed necessary) H2 receptor antagonist IV access/ IV fluids NPO Empty gastric contents (NG tube) Surgery if required/ Senior review Examples of other Notes for OB/Gyn MS H&P S: Pt is a 20 y.o G4P1112 (Grava 1, Para 1 (term), 1 (preterm), 1 (abortions), 2 (living)) at 39+1 weeks by 10 week ultrasound c/w LMP (consistent with last menstrual period) who presents to L&D (labor and delivery) in labor. Pregnancy has been uncomplicated. + FM (Fetal movement), denies LOF (loss of fluid), VB (vaginal bleeding). Ctx (contractions) q 4 minutes ROS: Among other things, be sure to ask about headaches, visual changes, abdominal pain (especially RUQ pain), worsening non dependent edema, change in urinary habits PMH: asthma, does not take meds now PSH: Tonsillectomy as a child Meds: PNV (prenatal vitamin) Allergies: Penicillin -> anaphylaxis POBHX: G1 - 35 week SVD (spontaneous vaginal delivery) of VMI (viable male infant) 5 lbs, 2 oz G2 - 8 week, SpAB (spontaneous abortion) G3 - 40 week, LTCS (low transverse Cesarean section) for breech G4 - Current PGYNHx: No hx of STDs, + hx of abnormal PAP with LEEP, but all PAPs normal since then Menarche at 13 years of age w regular periods q 28 dys lasting 4-5 days, no menorrhagia SH: tobacco (1.5 PPD), denies use of alcohol or illicit drugs FH: No history of birth defects No history of bleeding or clotting disorders No history of multiple gestations DM - grandmother Emphysema - paternal grandfather PE Temp, BP, HR, RR Labs: A+ (blood type), antibody -, rubella immune, RPR NR (non reactive), HBSag negative, HIV negative, GBS (group B strep) positive, 1 hour glucola 63, GC and Chlamydia negative; CBC (complete blood count)... A/P: 20 yo G4P1112 at 39+1 weeks who presents in labor currently 4 cm dilated, 90% effaced and -1 station 1) Admit to L&D 2) Epidural when desired 3) Clindamycin for +GBS and penicillin allergy 4) AROM (artificial rupture of membranes) after 4 hours of antibiotics MS Triage Note S: pt is a 20 y.o. G2P1 at 37+1 weeks by 8 week ultrasound that is consistent w LMP, presents to L&D with complaints of ctxs. No LOF, VB. + FM O: Temp, BP, HR, RR, T Abd: soft, gravid, NT (non tender) Ext: 1+ edema bilaterally, NT FHT (fetal heart tones): 140, moderate variability TOCO (tocometer): ctxs q 9 minutes Cervix: 1/40/-3 (dilation/effacement/station) (per RN) A/P: Pt is a 20 y.o G2P1 at 37+1 weeks who presents for rule out labor 1) Will have patient walk for 1 hour after getting reactive FHT, then recheck cervix MS Delivery Note SVD (spontaneous vaginal delivery) of VMI (viable male infant) with APGARs 8, 9 over 2nd degree midline laceration. Head delivered atraumatically, mouth and nose bulb suctioned at perineum, loose nuchal cord x 1 easily reduced, shoulders and body delivered without delay or force. Cord clamped and cut and infant handed to awaiting RN. Cord gases obtained. Spontaneous delivery of placenta with 3 VC (vessel cord) intact. No cervical, vaginal vault or periurethral lacerations. 2nd degree midline laceration repaired with 3.0 vicryl suture. EBL (estimated blood loss): 300 cc Anesthesia: Epidural Dr. (attending) present MS Operative Note Pre-operative diagnosis: IUP (intrauterine pregnancy) at term, breech presentation Post-operative diagnosis: same Procedure: primary LTCS via Pfannensteil incision Surgeon: Assistant: Anesthesia: spinal with duramorph Findings: VFI (viable female infant), frank breech, APGARs 8,9, 3VC, intact placenta, normal ovaries EBL (estimated blood loss): 800 cc Fluids: 1800 cc crystalloid UOP (urine output): 200 cc, clear Packs/Drains: foley Complications: none Disposition: Patient and infant stable to PACU (post anesthesia care unit) MS Post-op Check S: Pt resting comfortably. Pain well-controlled. Minimal nausea. No vomiting. O: Temp, BP, HR, RR Gen: NAD, A&O x3 Abd: soft, appropriately tender, ND, absent BS Inc: Dressing clean and intact Ext: No edema, non-tender, SCDs in place A/P: 47 y.o. WF POD #0 TAH/BSO 1) Hemodynamically stable, CBC in am 2) continue routine post-op care MS HROB (High risk obstetrics/Maternal fetal medicine) S: No complaints. Denies VB, LOF, ctx. +FM O: Temp, BP, HR, RR Gen: NAD, A&O x3 Abd: soft, gravid, non tender Ext: No edema, non-tender, DTRs (deep tendon reflexes) 2+ bilaterally, SCDs in place TOCO: No contractions FHT: 135, moderate variability, reactive A/P: 32 y.o. G1P0 at 30+1 weeks with PTL (preterm labor) 1) s/p BMZ (status post betamethasone) 2) Continue bed rest with BRP (bathroom privileges) 3) GBS negative MS PPD (post partum day) #1 S: Pain? Lochia? Ambulating? Breast/bottle feeding? Pain meds used?. Diet?. Voiding? Plan for contraception? O: Temp BP HR RR Gen: Lungs: C/V: Abd: soft? NT/ND? Fundus? (Should be firm, 2 finger breadths below umbilicus) Ext: edema? Palpable cords? DTRs: Labs? A/P: 19 y.o. PPD # __ SVD 1) MWB (maternal well being) - doing well, Rh + or - , RI (rubella immune)? Hgb? 2) FWB (fetal well being) – male/female infant, well?, breast/bottle feeding?, desires circumcision? 3) PPBC (post partum birth control) 4) D/C (discharge) planning MS POD (post operative day) #1 from C/S (can be used for other Gyn surgeries, omitting lochia/fundus) S: Pain Pain meds used? Lochia? nausea or vomiting? Flatus? Diet? Ambulating? Contraception? O: Temp BP HR RR Gen: Lungs: C/V: Abd: soft? Appropriately tender? Fundus? BS? Inc (incision): C/D/I (clean/dry/intact)? Staples/sutures? Ext: tenderness? Edema? SCDs (serial compression devices) in place? Labs? A/P: 55 y.o. WF POD #1 C/S 1) Hemodynamically stable, CBC? 2) advance diet to clears, await flatus for regular diet 3) ambulate with assistance, continue incentive spirometry HELLP syndrome Hemolysis Elevated LFTs Low Platelets Risk factors for Preterm Labor - MAPPS Multiple gestations Abdominal surgery during pregnancy Previous Preterm labor Previous Preterm delivery Surgery of the cervix Contraindications to tocolytics – CHAMPS Chorioamnionitis Hemorrhage Abruption Maturity of fetus Preeclampsia/eclampsia Severe IUGR Risk factors for shoulder dystocia – MOMS on L&D Maternal Obesity Macrosomia Second stage prolonged Late (post-date pregnancy) Diabetes Causes of fetal baseline tachycardia FFAASTT Heart Fetal infection Fever Arrhythia of fetus Anemia of fetus Sympathomimetics Tacycardia of mother Thyrotoxicosis of mother Hypoxia Causes of postpartum hemorrhage - 4T's Tone diminished - Uterine Atony represents 70% Postpartum hemorrhage Tissue - Retained Placenta - Placenta accreta Trauma - Uterine Inversion - Uterine Rupture - Cervical Laceration - Vaginal hematoma Thrombin - Coagulopathy Neuro SOAP note template Date, time MS3PN S: any complaints the pt has, how they are doing, what happened yesterday O: Vitals (Tmax, Pulse (min-max), Respiration (min-max), BP (min-max), SaO2) Ins and Outs (over 24h). *note last BM when going to Dodd Exam: General: how does patient appear? CV: RRR (regular rate and rhythm)?, normal S1 and S2?, no m/r/g (murmurs/rubs/gallops)?, peripheral pulses 2+ bilaterally?, peripheral edema? Lungs: CTAB (clear to auscultation bilaterally)?, no wheezes/rales/rhonchi?, no accessory muscle use? Abd: soft?, NT/ND (nontender/nondistended)?, bowel sounds normal?, no palpable masses or organomegaly? Mental Status: awake/somnolent/drowsy/arousable (to pain/name, etc?)/ comatose CN : EOMI (extraoccular mvts intact), PERRLA (pupils equally round and reactive to light and accommodation), face symmetric/droop, palate elevation symmetric/asymmetric, facial sensation intact ?/ tongue midline? * what to test with CN’s II: visual acuity, fields, pupils III, IV, VII: extraoccular movements, corneal reflex (if you are mean) V, VI: facial sensation, movement IX, X, XII: palate tongue, gag reflex, shoulder shrug/SCM Motor: tone (nl/spastic/flaccid) Bulk: atrophy? Strength: SA/EF/EE/WE/WF/DI/HF/KE/DF/PF R ____________________________________ L *(shoulder abd, elbow flex, elbow ext, wrist flex, wrist ext, dorsal interossi, hip flex, knee flex, dorsiflexion, plantarflextion) scale of 1-5 (5 = normal) Coordination: finger to nose, heel to shin, rapid alternating movements Sensory: safety pin prick/vibration/proprioception/temperature Gait: stance/stride/ arm swing/tandem walk/steadiness with feet together & eyes closed DTR (deep tendon reflexes) O \ | / *note biceps, triceps, brachioradialis, patellar, Achilles reflexes | . scale of 1 -4 (2 = normal) / \. *annotate with arrows if toes are upgoing or downgoing. Labs: Na |Cl |BUN /glucose \ Hgb / K |CO2|Cr \ WBC / Hct \ plt MRI, CT studies, consults, etc. A/P: “one liner” about pt “Mr Murphy is a 45 y/o right handed WM with a history of ___ who presented with _____. Sometimes, make a comment about their condition if it has changed since admit “s/p (status post) TPA with improvement in left leg weakness” Problem list (can be done by problems or by systems) 1. Neuro ( a. problem or ddx/ b. diagnostic studies/ c. treatment plan ) 2. Endo 3. Cardio 4. Etc….. Joe Smith, MS3 346-xxxx (pager #) DTRs: Biceps = C5, C6 Brachioradialis = C5, C6 Triceps = C6, C7 Patellar = L4 NO L5 reflex Achilles = S1 Dermatomes: T4 = nipple line T10 = umbilicus L1 = inguinal ligament Caloric eye testing – normal eye movements COWS Cold - Opposite Warm - Same MRI T1 – image looks like brain – ie white matter is white, gray matter darker, CSF black, best for anatomy of brain T2 – inverse of T1 – white matter is dark, gray matter lighter, CSF white, pathology stand out better (edema has a large water component) DWI – diffusion weighted images – type of T2 sequence that can identify ischemic areas within minutes of onset Glasgow Coma Score – out of 15 Verbal Eye opening 5 – oriented 4 – confused 3 – inappropriate words 2 – incomprehensible 1 – no response 4 – spontaneous 3 – to voice 2 – to painful stim 1 – no eye opening Causes of delirium – MOVE, STUPID Metabolic Oxygen Vascular Endocrine/Electrolyte Seizures Tumor/Trauma/Temperature Uremia Psychogenic Infection/Intoxication Drugs/Degenerative disease Motor 6 – follows commands 5 – localizes pain 4 – withdraws from pain 3 – flexion/decorticate posturing 2 – extension/decerebrate 1 – no response Penicillins Penicillin IV/P O G+ only, All GAS/GBS, syphilis, oral anaerobes (but not gut), clostridium exudative pharyngitis, erysipelias Nafcillin (IV)/oxacillin(po)/dicloxacillin(po) IV/P O G+ only DOC MSSA, can use for strep, (no MRSA), no G neg Cellulitis, s. aureus cutaneous abscess IV/P O G+ and some G- DOC for enterococcus, strep like pen, no staph, only a little G neg (some H.flu, some e. coli), listeria 1st line acute otitis media, acute sinusitis, neonatoal meningitis with gentamicin aminopenicillins Piperacillin IV Like amp + G-, so good for strep, enterococcus and G neg incl pseudomonas + anaerobes, but NO MSSA Amp/sulbactam (unasyn) IV IV Like amp + MSSA and anaerobes, NO MRSA, H.flu, most anaerobes, listeria Amox/clavulanate (augmentin) po PO Pipercillin/tazobactam (zosyn) IV All except MRSA, including pseudomonas and enteric G- IV No enterococci, NO MRSA, no listeria Staph and strep in pen allergic pt (10% cross react), G pos, few G neg (ex ecoli), few anaerobes B lactamase resistant penicillins Ampicillin(IV)/amoxicillin(po) Pen + B lactamase inhib (adds MSSA) Failed tx of otitis media Ticarcillin/tazo? (Timentin) Cephalosporin All 1st gen: Cefazolin (ancef) IV Cephalexin (Keflex) PO 2nd gen: Cefoxitan (Mefoxin) iv PO IV PO Above + H.flu, more G neg, anaerobes gut surg prophylaxis, otitis failed augmentin, IV A lot of G neg (no pseudomonas), not as good for staph as first and second gen, still good for GAS/GBS and s.pneumo Comm acquired Meningitis in all except neonates – crosses BBB, also for pyelo in kids and adults Rocephin, bad in neonates – biliary sludging/Ca++ precipitation, can use cefotaxime Omnicef – otitis failed augmentin IV G pos, most G neg, incl pseudomonas, limited anaerobes, no enterococcus Cefpodoxime (Vantin) iv Cefuroxime (Ceftin) po/iv 3rd gen: Ceftriaxone (Rocephin) im/iv Cefotaxime (Claforin) Cefdinir (omnicef) po 4th gen: Cefipime Ceftazidime Carbapenem Meropenem (kids) Nosocomial meningitis, pseudomonas IV Gram pos incl. entero, gram neg, pseudomonas, anaerobes, ESBL gram neg, NO MRSA, no acinetobacter Imipenem – decreases seizure threshold IV Like imipenem but no pseudomonas Q day, no CNS penetration IV/P O IV/P O Gram pos, some anaerobes, atypicals, NO gram neg Can cause pyloric stenosis so CI in neonates Above + H.flu, MAC tx, prophylaxis, more G- than erythro Pretty good resp drug, Pen allergic for strep throat, otitis media, DOC outpatient community acquired pneumonia in teenagers/adults, pertussis PO Some gram neg, gram pos, SOME MRSA, some anaerobes, Use if MRSA or e. coli known to be sensitive b/c cheap Imipenem (Primaxin) Ertapenem (Invanz) Macrolides Erythromycin Azithromycin Clarithromycin (Biaxin) Tetracycline atypicals - Kill some of everything Relative CI in kids <8yo Lyme, rickettsial, erlichiosis Tetracyclines Doxycycline Glycylcyclines Tigecycline RESTRICTED IV/P O IV Aminoglycosides Gentamicin, tobramycin, amikacin IV Aerobic gram neg only, incl pseudomonas, no anaerobes, only good at bloodstream pH, so no good in abscesses Can do qday dosing Quinolones Ciprofloxacin IV/P O G neg, most pseudomonas, atypicals, NO anaerobes IV/P O Above plus G pos including PRSP, less pseudomonas PRSP – pneumonia (with azithro inpt), sinusitis Moxifloxacin (Avelax) Drug resistant gram pos/neg (acinetobacter, VRE), NO pseudomonas Highly oto/nephrotoxic. Gent – often used in r.o sepsis in neonates, Amikacin/torbra – better nosocomial g- coverage, tobra least nephrotoxic, best agains pseudomonas, nebs for CF, Levofloxacin (levaquin) Lincosamide Clindamycin (Cleocin) IV/P O G pos, anaerobes, NO enterococc, will cover many community acquired MRSA (not nosocomial), good tissue, bone penetration, has antitoxin activity Comm aquired MRSA, infxns involving toxin production Metronidazone Metronidazole (flagyl) IV/P O Best for strict anaerobes B. fragilis, C. dif Sulfa Trimethoprim/sulfamethoxazole (Bactrim) IV/P O Many gram pos incl comm. aq MRSA, many gram neg, PCP, no pseudomonas, no enterococcus Cystits, PCP tx/prophy, COPD exac w/infxn Polymyxin Colistin RESTRICTED IV Very resistant G neg, no stenotrophomonas, causes renal failure, periph neuropathy, CNS problems When nothing else works for acinetobacter Rifampin Rifambin G+ incl staph, g- incl pseudomonas, TB, NEVER alone except for prophylazis, pregnancy category D Adjunctively for bad staph infection, TB/meningitis prophylazis Monobactam Aztreonam – RESTRICTED IV Only aerobic gram neg (just like aminoglycosides) for severe pen allergies (can’t use piper or zosyn) Glycopeptide Vancomycin IV/P O Gram pos, enterococci, IV – MRSA, MRSE, PO for c. dif, resistant strep pneumo, not oto/nephrotoxic Enterococc if pen allergic C. diff resistant to metronidazole Oxazolidinone Linezolid (Zyvox) IV/P O Gram +, enterococci, MRSA, MRSE, VRE VRE Linopeptide Daptomycin (Cubicin) RESTRICTED IV Gram + (MRSA, VRE, MRSE) VRE YOUR GUIDE TO NAVIGATING THE OSUMC SYSTEM: WebExchange: for text paging RadWeb: Radiology Essentris: used in the Ross, L&D, ICUs for vitals, labs etc E-results: Accessing Single Patient Data: All Pt Search-Results > MRN or Name (MRN is quicker and precise) > pt name > Note the new set of tabs that come up to the left [Patient Info, Clinical Summary, Medications, etc, etc….]. This method is best for looking up data for patients who are not currently admitted/active in the hospital (i.e. they are incoming so you can get ready for them to come in…). Accessing Patients on Your Service’s Census: CapiWeb/Results >Service Census > click on your service’s tab (Ge2, Me1, etc)> click on the blue pt name/hyperlink for your desired patient from the census that comes up> Note the new set of tabs that come up to the left [Patient Info, Rounds Report, Results, etc….]. On the first day, find out what your Service Census code is! Setting your default Census (so that every time you hit the Service Census tab it will automatically bring up your service’s census. CapiWeb/Results> Change Default Census> Select Service button > Hit your Service’s hyperlink and then the Enter button. Finding Patients on Your Service’s Consult Census/Finding Your Service’s Consult Census: CapiWeb/Results >Clinician Census >Physician Consult>Type the first letters of your service into the dialogue box (Surg, ENT, etc)> click on your service’s hyperlink> click on the blue pt name/hyperlink for your desired patient from the census that comes up> Getting Prepped for Rounds: Printing out your Service’s Census: includes recent labs, meds and handoff note included for each patient (great to have on rounds) CapiWeb/Results>Print for Multi Pts>Service Census>Click on the hyperlink for your service>select all (button at bottom)>Print for Selected Patients>MD Rounds (Notes/ To Do/ PMH/ Labs): if you want one/page this is an option above the type of note you want printed. People like to add their daily info on these handouts to be ready to present during rounds. Every morning you can just go to Rounds Report which will bring any notes, studies, labs, imaging that was done in the past 24 hrs. H&Ps: - Results > Encounters > History and Physical: use this to see what has already happened with your patient. Sometimes the H&P is in the Chart handwritten under H&P or Progress Notes. To look at notes from the ED: Result > Encounters > Emergency so you can see what was done with the patient before they came in. Consults: Results > Encounters > Consultations OR look in the FRONT of the chart on yellow paper! Labs: - Micro: - To get a full view go to Results > Last 5 occurrences, check all the tabs since they are listed under different things: hematology, body fluids, chemistry etc Results > Micro (back 90days) OR Micro(back 2.5 yrs). Make sure to check if it is Pending or the final read. Look at sensitivities. Imaging: Results > Radiology > occasionally find reports here (better to use RadWeb). Use RADWEB program to look at imaging Procedures: (Cath reports, EEG reports, EGD reports, Colonoscopy reports Results > Procedures if you want to see past reports that aren’t showing up click on the check box and then click view all. Surgical/Pathology: Results > Surg/Path Current Orders: Results>Display Current Orders > see all the medications they are on currently. Can use this to see if the orders discussed on rounds were followed up on and put in. You might also need to check Orders > View orders > then select pharmacy/lab etc to see if an order was placed > hit enter Look at past discharge summaries if patients don’t know their medications: Results > Encounters > Discharge summaries Under Documentation >Charted Med or MAR > click past # days you want > click display charted medications > enter: this shows you what medications the patient was actually administered. Allows you to see if they are refusing medications or if one-time orders were given. Also the place to see their insulin coverage if they are on carb coverage In the CHART: Charts are in boxes outside the patient rooms the code is 2+4, then 3, turn, Or in the James at the nurses station. Vitals: - on a dedicated clipboard or in the chart (harder to find) under the Nurse Flowsheets tab. - report ranges of vitals over the past 24 hrs. Make sure to divide up I/Os by type of Output - look at the nurses notes on the back of the vitals sheet. - All the ICUs, Ross heart, L&D: Use Essentris (another program with another password). Consults: in the front on yellow sheets of paper Progress notes: see follow up consult notes, PT/OT/Speech notes, progress notes for all services except medicine. Paperwork from Outside hospitals: usually in the back of the chart or at the clerk’s desk. Other Helpful Tips: Writing Handoff Notes Documentation>Notes> Enter/Revise Handoff Note (just write the pt’s one-liner and the major 3-5 parts of your management plan) Writing Hospital Courses Documentation>Arrival Meds/DI> Enter / Modify (under Discharge Instructions Heading) > Categories (at bottom of screen) > Check Physician, Procedure, Hosp Course box and hit Enter button at bottom of screen You MUST put in a dictating physician (type in the name of your resident, then search) or your hospital course will NOT save> then hit enter—will take you to procedures Procedures: type in pertinent procedures> enter; Hospital Course: Summary is one liner: Course gives info about what you did for the patient. Hit SAVE, NOT FINALIZE Might be helpful to do it in your email and then enter daily b/c the formatting gets messed up. Looking up that day’s OR schedule CapiWeb/Results > OR Schedule-Campus or –UHE > Choose the proper date and sort by Surgeon, Room Number, etc. Also be sure to select UH, James, or Ross Ors when looking for your case based on where it’s being performed that day (tabs at top of screen).