DVT
advertisement

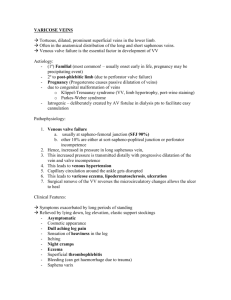
Thrombus (blood clot) a fibrin network made up of platelets, red blood cells, and white blood cells that forms in an artery or vein. Phlebitis – inflammation of a vein wall. Thrombophlebitis – thrombus formation with inflammation of the vein wall. Phlebothrombosis – thrombus formation with no inflammation of the vein wall. Superficial Thrombophlebitis – thrombus formation with inflammation of the vein wall in a superficial vein. Deep Vein Thrombophlebitis/Deep Vein Thrombosis (DVT) – thrombus formation in a deep vein (with or without inflammation of the vein wall). DVT is of greater significance than superficial thrombophlebitis because embolization of thrombi from deep veins to the lungs (pulmonary embolus) may be fatal. The greatest danger of thrombophlebitis is pulmonary embolism – all or part of a thrombus can detach from vein wall and migrate to the lungs. Three important factors cause venous thrombus formation: Virchow’s Triad 1. Venous Stasis (stoppage of venous blood flow or ↓ in venous flow ) occurs in an immobilized limb (muscles are inactive) – prolonged immobility, bed rest, leg cast, traction, post-op patients; pregnancy; obesity; advanced age (more than 60 years old); patients undergoing surgery (especially abdominal or pelvic surgery); sluggish peripheral circulation (CHF, dehydration); incompetent valves (varicose veins) 2. Damage to the vein wall (intimal or endothelial layer) creates a site for clot formation. Vein wall damage can result from infection, intravenous infusion of medications, venipuncture, traumatic injury (fracturis), orthopedic procedures on legs, History of DVT/venous problems. 3. Hypercoagulability of blood. Factors that can cause blood to coagulate faster than normal include oral contraceptives (especially those containing estrogen and in women who smoke and > 35 years old), cigarette smoking, dehydration, abrupt withdrawal of anticoagulant medications – rebound effect, blood disorders such as Malignancy/cancer like polycythemia vera (leads to sluggish blood, thick with RBCs) and anti-thrombin III deficiency. (Antithrombin III is a circulating anti-coagulant which inactivates thrombin and other clotting factors. Therefore ↓ amounts would ↑ risk of thrombus formation.) Most venous thrombi form in the legs, usually in the calves. Superficial Thrombophlebitis clinical manifestations produces pain or tenderness along course of vein, heat/warmth, redness, and swelling of the involved area. (↑ WBC) (The four cardinal signs of inflammation.) On palpitation, the vein may feel like a firm, subcutaneous cord (a palpable, visible, firm subcutaneous cordlike vein). A mild systemic temperature elevation and leukocytosis may be present. Therapeutic Management of Superficial Thrombophlebitis Goals: Reduce inflammation and prevent emboli formation; increase venous return to the heart, decreasing venous pressure. Bed rest with affected extremity elevated above heart level to decrease swelling and enhance venous return. Bed rest to prevent dislodgement of thrombus. Warm, moist compresses to relieve pain and reduce inflammation. Mild oral analgesics (acetaminophen) to relieve pain. For more severe pain, a nonsteroidal anti-inflammatory agent (ibuprofen) to relieve pain and inflammation. Elastic compression stockings after acute stage when patient becomes ambulatory. Elastic stockings compress superficial veins, reducing pooling of venous blood and enhancing venous return to the heart. Anticoagulant therapy is usually not indicated for superficial thrombophlebitis. The risk of superficial venous thrombi dislodging and causing emboli is very low because the majority of them adhere firmly to the vein wall and undergo spontaneous lyses. Diagnostic Studies in Deep Vein Thrombophlebitis Noninvasive venous studies Doppler Ultrasound – common noninvasive test to measure blood flow through blood vessels (arteries and veins). In DVT, determines venous blood flow in deep veins. In Doppler ultrasound, a probe transmits highfrequency sound waves through the skin toward veins. The sound waves strike the moving red blood cells and are transmitted back to the probe, producing audible tone. Normal venous blood flow creates a roaring sound. In the patient with DVT, the sound of venous blood flow is diminished or absent. TPA – tissue plasminogen activator – dissolves clots, bodies natural fibrinolytic Duplex venous scanning or imaging (noninvasive) test is usually done with Doppler flow studies. Doppler scanning produces a three-dimensional view of the veins on a monitor screen, allowing examiner to view both vessel and any thrombus, thrombi. D-dimer test: A blood test to measure fibrin degradation fragments generated by fibrinolysis. Elevated D-dimer levels indicate a thrombotic process, but aren’t specific to DVT. (D-dimer is produced by action of plasmin of fibrin clot.) Impedance Plethysmography measures venous changes in the limbs. The test uses a blood pressure cuff wrapped around the patient’s thigh and inflated (50 to 60 mm Hg) to occlude venous blood flow from the calf. In the normal patient, venous blood volume in the calf increases markedly as blood becomes trapped below the cuff. If a DVT is present, venous volume won’t increase as much because blood is already trapped in the calf. When the pressure applied by the thigh cuff is released, venous outflow is measured. Normally, venous volume falls dramatically as the trapped blood surges upward. In the leg with DVT, venous volume remains much the same. INVASIVE PROCEDURE VENOGRAPHY is the most definitive test for diagnosing DVT but it carries several risks (eg, allergic reaction to dye – contrast medium-phlebitis) and so should only be done is the patient has signs and symptoms of DVT, but the results of noninvasive studies are ambiguous. Procedures involves injecting contrast media into bloodstream, followed by x-rays to identify location of clot. **Edema in extremities is a vein problem, never an artery problem. DEEP VEIN THROMBOPHLEBITIS (DVT) Clinical Manifestations Once a thrombus becomes large enough to completely obstruct blood flow through a vein, signs and symptoms develop. The first sign is usually edemal swelling of affected extremity. The amount of swelling can be determined by measuring extremity (ankle, calf, and inner thigh) circumference at various levels with a tape measure, compare one extremity to the other by measuring the circumference of each at the same level for size differences. Inspect legs from groin to feet, noting any unilateral or bilateral changes. Compare one leg to the other. The skin over the affected area may become warmer. There may also be erythema (redness) in the affected area. The patient may complain of a tight or heavy sensation in the limb, heaviness in the affected limb and pain or tenderness over involved vein or palpation. Malaise and fever sometimes occur. A positive Homan’s sign (calf pain upon dorsification of the foot) is a classic but unreliable sign for DVT because it can be elicited in any painful condition of the calf. Diminished or absent Doppler flow reading over veins in affected extremity. Management Goals: Prevent existing thrombi from becoming emboli. Prevent new thrombi from forming increase venous return to the heart; decrease venous pressure. Bed rest to prevent clot dislodgement. Bed rest is usually required for about 5 to 7 days after DVT to give the clot time to adhere to the vein wall so it won’t embolize. Elevate the affected extremity above heart level to reduce swelling (↓ venous pressure) and enhance venous return (prevents venous stasis and the formation of new thrombi) Elevate the patient’s legs by elevating the foot of the bed six inches on blocks. Avoid placing pillows under patient’s knees and use of knee gatch to prevent compression of the popliteal vein and obstruction of venous blood flow. Do not elevate the head of the bed more than 30 degrees to prevent inguinal congestion (consult doctor regarding degree HOB should be elevated). Apply warm, moist, compresses to affected extremity to relieve pain and reduce inflammation; if ordered, administer mild oral analgesics (eg, acetaminophen) to relieve pain. Measure and record circumference of extremity daily. Compare bilaterally and with previous measurements. Assess extremity color, temperature, pulses, complaint of pain. **Don’t give Tylenol with Coumadin or Warfarin. Do not exercise affected extremity during acute phase of DVT to prevent clot dislodgement. Instruct and assist patient to move affected extremity slowly and cautiously. The unaffected extremity should be exercised actively to promote venous blood flow. Never rub or massage affected extremity – could dislodge clot. To protect affected extremity from trauma and pressure, use an air mattress, sheepskin, heelpads, and a bed cradle or foot board. Caution patient to avoid activities that create a Valsalva maneuver (eg, straining to have bowel movement [stool softener], holding breath while moving in bed [provide trapeze]). Valsalva maneuver ↑ intra-abdominal pressure, ↓ venous return, ↑ venous pressure. Instruct patient to perform deep breathing exercises to promote venous return. Maintain adequate fluid intake – two to three liters a day unless contraindication – to prevent dehydration. Elastic compression bandages /Ace bandages are usually prescribed to promote venous return and decrease leg swelling. Bandages are applied from toes up with uniform/even pressure. Should be rewrapped at least once during each shift; check for circulatory, motor, and neurologic functions in extremity because an improperly wrapped bandage can have a tourniquet effect. Once swelling has subsided, patient can be measured for an elastic support stocking. SUMMARY Non-invasive test for thrombophlebitis: 1. Doppler ultrasound 2. D-dimer test (degraded fibrin fragments) 3. Plethysmography (cuff around thigh) Invasive tests for thrombophlebitis: 1. Venography (risks = allergy to dye.