Adrenal Medulla - Doctor Jade Main
advertisement

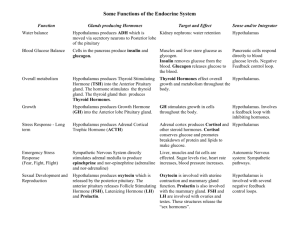
ENDOCRINE SYSTEM -LECTURE 1 The endocrine system and the nervous system work together to coordinate functions of the body systems. Nervous control is faster, happening in milliseconds and uses chemical messengers called neurotransmitters. Endocrine responses are longer to begin from hours, months and even years and have longer effects and use hormones as the chemical messengers. Hormones are mediator molecules that are released in one part of the body and regulate the activity of cells in other parts of the body. Most enter the blood stream and bind to receptors on target cells. Endocrine responses function to regulate long acting body changes, such as changes in metabolic activity, changes which adapt animal to environment and help to provide homeostasis. There are two types of glands in the body-exocrine and endocrine. Exocrine glands such as the sweat glands secrete their products through a duct that carry them into body cavities, into the lumen of an organ or onto the surface of the body. Endocrine glands secrete their products into the interstitial fluid surrounding the secretory cells of the gland and from there they enter capillaries flow through the blood until they reach a target organ. Endocrine glands include the pituitary, thyroid, parathyroid, adrenal and pineal glands. There are other organs and tissues that are not exclusively endocrine but have cells that secrete hormones. These include: the hypothalamus, thymus, pancreas, ovaries, testes, kidneys, stomach, liver, small intestine, skin, heart, adipose tissue and the placenta. Endocrine organs are small, unimpressive and widely scattered through the body. They secrete hormones, chemical messengers produced in one part of body and transported by circulatory system to distant target tissues, where effects are exerted. In order for a hormone to have an effect it must bind to receptor cells on a target organ. Hormones exert prolonged effects at low concentrations. Concentration reflects the rate of release, speed of inactivation and rate of removal half-life which can be a fraction of a minute to 30 minutes or longer. Eventually these hormones are inactivated by the liver and excreted by the kidneys. Circulating and Local Hormones Most hormones of the endocrine system are circulating. They reach their target organs by flowing through the circulatory system. Local hormones are released and act on nearby cells without entering the bloodstream. These are termed paracrines. Those that act on the same cell that secreted them are called autocrines. Local hormones are rapidly inactivated. Chemical Classes of Hormones Hormones fall into two broad classes-those soluble in lipids and those soluble in water. These two classes exert their effects differently. Lipid soluble hormones include steroid hormones, thyroid hormones and nitric oxide. Steroid hormones are derived from cholesterol and include the gonadal hormones-estrogen, progesterone, testosterone, and adrenocortical hormones-cortisol. Steroids hormones, are transported bound to blood transport proteins. Thyroid hormone is made by adding iodine molecules to tyrosine. Water soluble hormones include amines, peptide and protein hormones as well as the eicosanoid hormones. Amine hormones are modified amino acids; epinephrine and norepinehrine are examples and are often called catecholamines. Peptide/protein hormones range from short chains of amino acids-3-49-peptides to polypeptides-50 -200 amino acids. Some have sugars attached and are called glycoproteins. These include growth hormone, insulin, prolactin, oxytocin. Eicosanoids are derived from arachidonic acid, a fatty acid and include prostaglandins which raise blood pressure, mediate uterine contractions, enhance blood clotting and leukotrienes which are signaling chemicals found during times of inflammation and allergic reactions. Some do not include these as true hormones since they are localized and not circulating. Mechanisms of Hormone Action A hormone announces its arrival to a target organ by binding to a receptor. Receptors for lipid soluble hormones are found inside the cell while those for water soluble ones are found on the cell membrane of target cells. Direct Gene Activation-Lipid Soluble Hormone For hormones that are lipid soluble the mechanism of action is termed direct gene activation. Since these hormones are lipid soluble they can diffuse into target cells. Direct gene activation occurs in several steps. First, the hormone diffuses from the blood into a cell. The hormone binds to and activates receptrs within the cytosol or the nuclues of the target cell. Binding of hormone to receptor forms a receptorhormone complex. This complex alters gene expression, i.e. it turns genes on or off. As the Dna is transcribed, new mRNA is made. This leaves the nucleus and enters the cytosol where new protein is made. This new protein alters the cell’s activity. Proteins or exaple may be enzymes that promote metabolic activities of other proteins. Water Soluble Hormones- Second-Messenger System Protein, peptide and amine hormones cannot pass through the plasma membrane. They must bind to receptors on the cell membrane of target cells and exert their effects through an intracellular second messenger. The hormone is the first messenger; it binds to a plasma membrane receptor and causes the production of a second messenger inside the cell. One common second messenger is cAMP (cyclic AMP). The first step of the second messenger mechanism is fro the hormone to diffuse through the blood and gind to a receptor on the cell membrane. This in turn activates a G protein, a type of regulatory molecule. The activated G protein activates adenlyate cyclase, an effector enzyme. Activated adenlyate cyclase conversts ATP to the second messenger-cAMP. cAMP activates one or more protein kinase molecules. Protein kinase is an enzyme that phosphorylates or adds phosphate groups to proteins. Activated protein kinase phosphorylates cellular proteins; this activates some proteins and inhibits others which allows for a variety of reactions in one cell. cAMP is degraded rapidly by phosphodiesterase. Its action is brief and no extracellular controls are needed to stop its action. Control of Hormone Secretion Hormonal blood levels vary within a narrow range. Secretions are strictly controlled. Secretions are regulated by: 1) nervous system, 2) hormones of 3) changes in blood chemistry called humoral stimuli. Neural stimuli means that nerve fibers stimulate hormone release. A classic example is the milk-let down reflex in cows. There is a 6-8 minute delay between time of initial udder stimulation-suckling, manual stimulation and full milk release. Udder stimulated neural signals travel along afferent nerves to spinal cordbrainrelayed to secretory neurons of posterior pituitaryoxytocin released into capillary bed surrounding posterior pituitaryblood flows through venous system to heart lungsback to heartarterial systemuddersmilk let down. Stress sympathetic nervous systemadrenal medullanorepinephrine & epinephrine. Hormonal stimuli refers to glands releasing hormones in response to other hormones. Releasing hormones from the hypothalamusanterior pituitary stimulates release of anterior pituitary hormones. Tropic hormones from the anterior pituitaryovaries to secrete hormones. Humoral Stimuli directs endocrine glands to secrete hormones as a direct response to changing blood levels of ions and nutrients. For example the parathyroid gland monitors Ca++ concentration, when low parathyroid hormone releasedcauses Ca++ to increase. Insulin and aldosterone are also released by humoral stimuli. Endocrine Glands Hypothalamus The hypothalamus is the major link between the nervous system and the endocrine system. It is only recently realized as the major gland in the body. It is responsible for secreting nine hormones some which control the release of other hormones from the pituitary gland. Together the hypothalamus and the pituitary play important roles in virtually all aspects of growth, development, metabolism and homeostasis. Pituitary gland or Hypophysis-hi-pof-I-sis The pituitary gland is located in the sella turcica of sphenoid bone. It is about the size and shape of a pea and is attached to the hypothalamus by the infundibulum. The pituitary has 2 anatomically and functionally separate parts-adenohypothesis or anterior lobe and the neurohypophyesis or posterior lobe. The anterior lobe consists of two parts: pars distalis and the pars tuberalis; the posterior lobe is divided into the pars nervosa and the pars intermedia. The pars intermedia atrophies during fetal development and is not a separate lobe in adults. Anterior pituitary hormones are stimulated to be released by hormones made in the hypothalamus called releasing hormones and are suppressed by hormones made in the hypothalamus called inhibiting hormones. The posterior lobe stores hormones made in the hypothalamus. The connection between the hypothalamus and the anterior pituitary is via the hypophyseal portal system. In a portal system blood flows from one capillary network into a portal vein and then to a secondary capillary network before returning to the heart. Arterial blood gets to the pituitary by hypophyseal branches of the internal carotid arteries. Veins leave via dural sinuses. The anterior lobe is connected vascularly by a primary capillary plexus. The infundibulum connects to hypophyseal portal veins via secondary capillary plexus in the anterior lobe. Primary and secondary plexi make up hypophyseal portal system. Blood transports releasing factors from hypothalamus directly to the anterior pituitary gland. Neurosecretory cells in the hypothalamus made RH (releasing hormones) and IH (inhibiting hormones). These enter the hypophyseal portal system and go directly to the adenohypophysis. These stimulate the pituitary to make tropins or tropic hormones-tropic=turn on. These stimulate other endocrine glands or tissues to function. Types of Cells in the Anterior Pituitary There are several types of cells in the anterior pituitary which make a variety of trophins. Somatotrophs make growth hormone or somatorophin which stimulate cells to secrete insulin-like growth factors, which in turn simulates general growth and regulate metabolism. Thyrotrophs secrete TSH-thyroid stimulating hormone or thyrotropin which controls secretions from the thyroid gland. Gonadotrophs secrete (GnRH) gonadotrophins. There are two types-FSH and LH, follicle stimulating hormone and leutinizing hormone which act on the gonads to stimulate production of hormones and to influence maturation of oocytes and sperm. Lactotrophs stimulate prolactin which stimulate the mammary glands to make milk. Corticotrophs make ACTH or corticotrophin which stimulate the adrenal cortex to make glucocorticoids such as cortisol. Cells in the parts intermedia secrete MSH-melanocyte stimulating hormone. Control of Secretion of Anterior Pituitary Hormones There are two ways to regulate hormone release from the anterior pituitary. One way is via secretion of releasing hormones (five) and inhibiting hormones (two) from the hypothalamus. The second way is via negative feedback. Endocrine glands are often regulated by negative feedback mechanisms. In this mechanism substances produced by target organs are transported by blood back to the anterior pituitary and/or the hypothalamus to decrease the secretion from these glands and in so doing stop the production of the hormone from the endocrine gland. As an example, LH secreted by the pituitary stimulates follicle to produce estrogen; estrogen travels back to the pituitaryinhibits release of LH. Anterior Pituitary Hormones Growth Hormone Growth hormone is made by somatotrophs which are the most numerous type of cell in the anterior pituitary. These cells make hGH-human growth hormone which has an anabolic effect. They promote protein synthesis and secretion of IGFsInsulin like growth factors or somatomedins. Target cells for growth hormone are found in the liver, skeletal muscle, cartilage, bone and other tissues. IGFs cause cells to grow and to multiply by increasing the uptake of amino acids into cells and accelerating protein synthesis. They decrease protein breakdown. Overall these functions increase the growth rate of the skeleton and skeletal muscles during childhood and teenage years. In adults IGFs help maintain muscle and bone mass and help to promote healing and tissue repair. IGFs encourags use of fats for fuel conserving glucose; lipolyis. They influence carbohydrate metabolism by decreasing glucose uptake (glucose sparing effect). Somatotrphs release bursts of growth hormone every few hours, especially during sleep. Secretion is regulated by 2 hypothalamic hormones GHRF-stimulates release and GHIF-somatostatin-inhibits release of GH. Blood glucose levels regulate both GHRH and GHIF. Hypoglycemia stimulates production of GHRH and hyperglycemia stimulates production of GHIH. TSH, thyroid stimulating hormone stimulates secretory activity of the thyroid gland. When thyroid hormone is low in the blood TRH-thyrotropin RH from the hypothalamus causes thyrotrope cells of the anterior pituitary to produce TSH. TSH stimulates the thyroid to make thyroid hormones-T3 and T4.Thyroid hormone feedsbacks on TRH and TSH to inhibit secretion. ACTH or adrenocorticotropic hormone is secreted by corticotrophs of the anterior pituitary. Hypothalamuscorticotropin releasing hormone (CRH)anterior pituitary to make ACTHadrenal cortexglucocoricoids, especially cortisol which help resist stress. Glucocorticoids feedback to block secretion of CRH and ACTH. Gonadotropins include FSH and LH which regulate the function of the gonadsovaries & testes. Follicle stimulating hormone (FSH) targets the ovaries in females causing the follicular cells to produce estrogen. In males FSH stimulates sperm production. LH (leutinizing hormone) in females triggers ovulation and with FSH stimulates estrogen secretion. In males LH stimulates interstitial cells of testes to secrete testosterone. GnRH (gonadotrophin releasing hormone) from the hypothalamus stimulates the anterior pituitary to release both FSH and LH. Gonadal hormones feedback to suppress FSH and LH release. Prolactin or PRL is released from the anterior pituitary in response to PRH from the hypothalamus. In females prolactin initiates and maintains milk production by the mammary glands. Ejection of milk depends on oxytocin from the posterior pituitary gland. The hypothalamus secretes PIH (prolactin inhibiting hormone) which is believed to be dopamine which inhibits prolactin secretion. PRH, believed to be serotonin causes lactotropes to stimulate milk production. MSH, melanocyte stimulating hormone stimulates melanocytes in amphibians and reptiles to make melanin, increasing pigmentation. The role of MSH in humans is unknown. There are MSH receptors in the brain suggesting it is important in brain activity. There is little circulating MSH. Posterior Pituitary The posterior pituitary or neurohypophysis does not make hormones. It stores and releases two hormones made in the hypothalamus- ADH or antidiuretic hormone and oxytocin. Cell bodies in the paraventricular (oxytocin) and supraoptic nucleus (ADH or vasopressin) of the hypothalamus make the hormones and they travel to the posterior pituitary through the axons of the nerve cells. The axons make up the hypothalamic hypophyseal tract. ADH functions to control water balance. It inhibits or decreases urine formation which helps avoid dehydration or water overload. Hypothalamic neurons called osmoreceptors monitor solute or water concentration of blood. Solutes too concentratedosmoreceptorsexcite supraoptic nucleisynthesis and release of ADHtarget-kidney tubules reabsorb water from urineless urineblood volume increases. Solute concentration decreasesosmoreceptors end ADH release. Alcohol inhibits ADH secretioncopious urine. Excessive water drinking inhibits ADH release. At high concentrations ADH causes vasoconstriction primarily visceral blood vessels-referred to as vasopressin. The target organs for oxytocin are the uterus and the breasts. It is released in high amounts during childbirth and in nursing mothers. During delivery, the cervix stretches which stimulates release of oxytocin which enhances smooth muscle contraction. After delivery oxytocin stimulates milk ejection. Uterus stretches impulse to hypothalamusoxytoxin madereleased from posterior pituitaryoxytocin in bloodcontractions increase. This is a form of positive feed back control. Oxytocin is called the cuddle hormone; it is believed to promotesnurturing and affectionate behavior. Thyroid Gland. The thyroid gland is located in the anterior neck on the trachea just inferior to the larynx. It is make up of 2 lateral lobes connected by an isthmus and is the largest pure endocrine gland. Thyroid follicles make up most of the gland. The walls of each follicle consists of cuboidal, follicular cells. These cells make the thyroid hormones T4, thyroxin or tetraiodothyronine and T3 or triiodotyronine. Both are iodinated derivatives of tyrosines; thyroxine has 4 bound iodine atoms and T3 has 3. Synthesis & Secretion of Thyroid Hormones The first step in the synthesis and secretion of thyroid hormone is Iodide trapping. The follicular cells trap I- by actively transporting the ions from the blood into the cytosol of the cells. In step two thryroglobulin (TGB) is made. While trapping iodide follicle cells make TGB. Thyroglobulin is made in the ribosome and transproted to the Golgi body where sugar residues are attached and it is packaged into vesicles. These undergo exocytosis and release TGB into the lumen of the follicle. The third step is the oxidation to iodide. Iodides, I- are negatively charged and cannot bind with tyrosines to make thyroid hormones until theylose the negative charge. This requires them to be oxidated or to lose an electron. I- I2 . As the iodide is oxidized it passes into the lumen of the follicle. Step four is iodination of tyrosine. I2 binds with tyrosines. Coupling of one iodineT1 ormonoiodotyrosine. Attachment of 2diiodotyrosine. TGB with iodine atoms attached is called colloid. Step five is coupling of T1 and T2 within the colloid. Enzymes in colloid link T1 and T2 into T3 and T4. The next step is pinocytosis and digestion of colloid. Droplets of colloid reenter the follicular cells by pinocytosis (cell sipping) and merge with lysosomes. The enzymes in the lysosomes digest the colloid breaking off molecules of T3 and T4. Secretion of the thyroid hormones is the next step. Since thyroid hormones are lipid soluble they diffuse through the membrane and into the blood. More thyroxin is secreted; T3 is more potent. The last step is transport of the hormones in the blood. Binds to proteins in bloodstream, thyroxine-binding globulins or TBGs for transport to target tissues. Actions of Thyroid Hormone Most cells have receptors for thyroid hormones. It affects all cells except adult brain, spleen, testes, uterus and thyroid. It increases BMR (rate of oxygen consumption under standard basal conditions). When BMR increases metabolism of carbohydrates, proteins and lipids increase. Thyroid hormones also stimulate the synthesis of Na/K ATPase pumps. They stimulate protein synthesis, enhance actions of catecholamines and accelerate body growth. . Thyroid Hormone-Mechanism of Action Low blood levels of thyroid hormonehypothalamusTRHanterior pituitary TSH (anterior pituitary)binds to follicle cell receptorsforms & stores thyroid hormone. There is feedback inhibition by thyroid hormone. When levels are high enough they suppress release of both TRH and TSH. Calcitonin Another cell type in the thyroid gland are parafollicular or C cells which lie in follicular epithelium and protrude into the connective tissue separating and surrounding follicles. These cells make calcitonin, a polypeptide hormone that acts to lower blood Ca++. One target organ is the skeleton; the hormone inhibits osteoclast activity or bone resorption and release of Ca++. Parathyroid glands The four parathryroid glands are found embedded in the posterior surface of the thyroid gland. There are two types of cells, chief or principle cells which make parathyroid hormone and oxyphilic cells whose function is unknown. PTH, parathormone or parathyroid hormone is the single most important hormone controlling Ca++ balance. It also functions in the balance of magnesium and phosphate ions. Lowered blood Ca++ or hypocalcemia stimulates secretion of PTH. PTH increases Ca++ levels in blood by stimulating 3 target organs: skeleton, kidneys and the intestines. The hormone stimulates osteoclasts, bone resorbing cells to digest the bone matrix and release Ca++ and PO4. It enhances the reabsorption of Ca++ and excretion of PO4 by the kidneys and increases absorption of Ca++ by intestional mucosal cells. PTH increases production of the hormone calcitriol from the kidneys. Calcitriol is the active form of vitamin D3 which enhances Ca++ absorption by the gut. Adrenal Glands-Suprarenal Glands The adrenal glands are two pyramid shaped organs on top of the kidneys. Each is surrounded by a fibrous capsule and fat. The glands have two structurally and functionally distinct regions: the inner, adrenal medulla and the outer, adrenal cortex which produces the steroid hormones that are essential for life. The adrenal cortex is divided into three zones, each which secrete a different hormone. The outer zone, the zona glomerulosa secretes mineralocorticoids which affect mineral homeostasis. The zona fasciculate is the middle zone. Here the cells are formed in linear cords and secrete glucocorticoids or metabolic hormones. The last area is the zona reticularis where the cells are found in a net like arrangement. This zone synthesizes androgrens or gonadocorticoids. Mineralocorticoids regulate electrolyte or mineral salt concentration in extracellular fluids, particularly Na and K. Aldosterone is the major mineralocorticoids. Its primary target is the distal part of the kidney tubules where it stimulates reabsorption of Na and water from urine. It enhances K elimination and enhances Na absorption from sweat, saliva and gastric juice. Sodium ion regulation is critical to overall body homeostasis because where Na goes water follows which can lead to blood volume and blood pressure changes. Aldosterone is stimulated by rising K levels, low Na, decreasing blood volume and blood pressure. Reverse conditions end secretion. The renin-angiotensin-aldosterone system (RAA) is the major regulator of aldosterone release. Blood pressure or volume decreases or plasma osmolaritysolute concentration decreasescells in the kidney’s juxtaglomerular apparatusrelease renincleaves off part of angiotensinogenenzymatic cascadeangiotensin II glomerulosa cells-adrenal cortexaldosterone release. Glucocorticoids are produced in the zona fasciculata. The major one is cortisol or hydrocortisone. Cortisone and corticosterone are two other glucocorticoids. Severe stress including hemorrhage, infection and emotional trauma produce high output of cortisol. Release is regulated by negative feedback. Low levels of glucocorticoidsCRH from the hypothalamusACTH from the anterior pituitary adrenal cortexcortisol release. The primary metabolic effect of glucocorticoids is gluconeogenesis, the formation of glucose from non-carbohydrate sources. It also increases the rate of protein breakdown and stimulates lipolysis. These hormones help resist stressors and are absolutely essential to life. Additional glucose provides tissues with a source of ATP which help to reduce stress. Glucocoricoids have anti-inflammatory effects by inhibiting white blood cells. In so doing they also depress the immune response. The zona reticularis makes androgens. The major one is DHEA-inhi. In females this helps promote libido and is converted into estrogen in other body tissues. The main hormone that stimulates its secretion is ACTH. Adrenal Medulla The adrenal medulla secretes catecholamines, epinephrine, norepinephrine and dopamine. The medullas is a modified, sympathetic ganglion of the autonomic nervous system. Chromaffin cells produce epinephrine and norepinephrine. Stress and exercise cause the hypothalamus to send impulses to the medulla to release the catecholamines. This begins the fight or flight response. Epinephrine is a potent stimulator of heart and metabolic activities; norepinephrine has a greater effect on peripheral vasoconstriction and blood pressure. Stresssympathetic nervous systemblood sugar increases, blood vessels constrict, heart rate increases, blood pressure increases. Pancreas The pancreas is located partially behind the stomach in the abdomen. It is a soft, triangular, mixed gland containing both exocrine and endocrine parts. 99% of the exocrine cells are arranged in clusters called acini. These cells produce digestive enzymes. Scattered among the acini are pancreatic islets or Islets of Langerhans. These contain four different cells types: alpha, beta, delta and F. Alpha or A cells produce glucagon. These account for 17% of the islet cells. Glucagon is hyperglycemic; it raises blood glucose levels. It stimulus for release is low blood glucose levels. Beta or B cells account for 70% of the islets cells and make insulin. Insulin is hypoglycemic and is released in response to high blood glucose levels. Delta or D cells account for 7% of islet cells and make somatostatin. This hormone inhibits glucagon and insulin release and inhibits growth hormone secretion. F cells make pancreatic polypeptide which inhibits somatostatin, inhibits gall bladder secretion and inhibits secretion of digestive enzymes. Gonads The gonads, ovaries and testes produce steroid hormones and produce gametes. Ovaries, paired, small, oval organs in the abdominopelvic cavity make estrogen, progesterone and inhibin. Estrogen is needed for the maturation of reproductive organs and is responsible for secondary sex characteristics with progesterone, these hormones regulate the menstrual cycle. Testes found in the extra abdominal skin pouch-scrotum make testosterone which is responsible for the maturation of reproductive organs and maintenance of the secondary sex characteristics. The testes also make inhibin. GnRH from the hypothalamusanterior pituitaryFSH and LH ( gonadotropins) control release. Inhibin feeds back and inhibits FSH release. Pineal Gland The pineal gland is a tiny, pine coned shaped body hanging from the roof of the third ventricle. It secretes melatonin from pinealocytes arranged in cords and clusters. Melatonin rises and falls in a diurnal cycle. Itpeaks during the night and promotes sleep. Pineal gland receives information regarding intensity and duration of day light through the retina of the eye. This information is sent to the suprachiasmatic nucleus (biological clock) in the hypothalamussuperior cervical ganglion pineal glandmelatonin. Thymus The thymus gland is found deep in the sternum in the thorax. It is lobulated and is large and conspicuous in infants and children. It diminishes in size with age. This gland makes thymopoietins , thymic humoral factor (THF), thymic factor (TF) and thymosins. These promote the development of T lymphocytes; a type of white blood cell needed for the immune response. The gland populates other lymphatic organs before it involutes. Other Hormone Producing Structures There are other tissues that make hormones that are not endocrine glands. The heart’s atrial cells make ANP, atrial natriuretic peptide. This hormone reduces blood volume, blood pressure and blood Na. The gastrointestional tract contains enteroendocrine cells which make gastrin, secretin and GIP. Gastrin promotes gastric juice secretion, secretin promotes secretion of pancreatic enzymes and GIP (glucose dependent insulinotropic peptide promotes release of insulin. The placenta produces hormones that influence pregnancy such as estrogens and progesterones; it also makes hCG-human chorionic gonadotrophin and hCs, human chorionic somatommotrophin which stimulates development of the mammary glands. The kidneys make renin, erythropoietin and calcitriol. Erythropoietinincreases RBC production. Renin is needed for blood pressure and salt balance and calcitriol is used to absorb calcium from the digestive system. The skin makes cholecalciferol, an inactive vitamin D form. Adipose tissue produces leptin which binds to CNS neurons for appettite control; it provides the sensation of satiety.