Issue 1611 | December 15, 20 - American Psychotherapy and
advertisement
Special Edition Newsletter
American Psychotherapy and Medical Hypnosis Association
Volume Year 17 | Issue 1611 | December 15, 2009
In This Issue...
Spotlight: Tina Moghimi Ferreira MA, LPC, NCC
Diagnosis Prior to Hypnosis for Eye Blinking
Hypnosis Audio CDs and Tapes - Simon
Hypnosis Network: Weight Loss Hypnosis
Abstract: Hypnosis in Contemporary Medicine
Abstract: Hypnosis for Fibromyalgia Pain
Mental Health Conferences: Announcements
APMHA Membership Information and Contacts
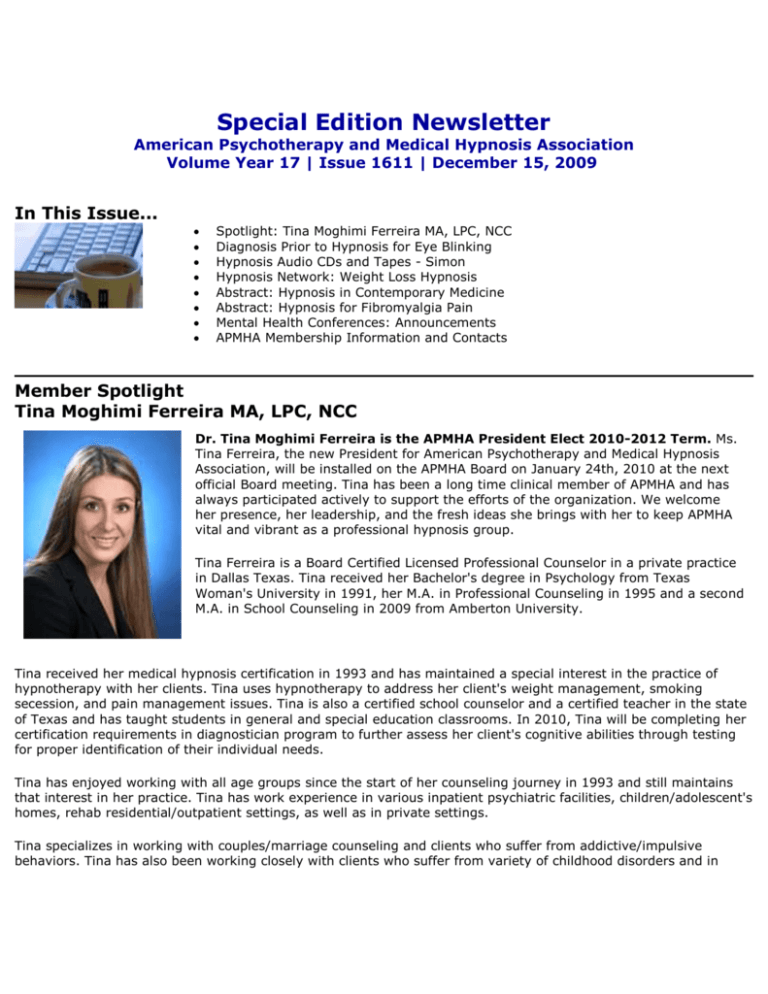
Member Spotlight
Tina Moghimi Ferreira MA, LPC, NCC
Dr. Tina Moghimi Ferreira is the APMHA President Elect 2010-2012 Term. Ms.
Tina Ferreira, the new President for American Psychotherapy and Medical Hypnosis
Association, will be installed on the APMHA Board on January 24th, 2010 at the next
official Board meeting. Tina has been a long time clinical member of APMHA and has
always participated actively to support the efforts of the organization. We welcome
her presence, her leadership, and the fresh ideas she brings with her to keep APMHA
vital and vibrant as a professional hypnosis group.
Tina Ferreira is a Board Certified Licensed Professional Counselor in a private practice
in Dallas Texas. Tina received her Bachelor's degree in Psychology from Texas
Woman's University in 1991, her M.A. in Professional Counseling in 1995 and a second
M.A. in School Counseling in 2009 from Amberton University.
Tina received her medical hypnosis certification in 1993 and has maintained a special interest in the practice of
hypnotherapy with her clients. Tina uses hypnotherapy to address her client's weight management, smoking
secession, and pain management issues. Tina is also a certified school counselor and a certified teacher in the state
of Texas and has taught students in general and special education classrooms. In 2010, Tina will be completing her
certification requirements in diagnostician program to further assess her client's cognitive abilities through testing
for proper identification of their individual needs.
Tina has enjoyed working with all age groups since the start of her counseling journey in 1993 and still maintains
that interest in her practice. Tina has work experience in various inpatient psychiatric facilities, children/adolescent's
homes, rehab residential/outpatient settings, as well as in private settings.
Tina specializes in working with couples/marriage counseling and clients who suffer from addictive/impulsive
behaviors. Tina has also been working closely with clients who suffer from variety of childhood disorders and in
particular clients who suffer from various types of Pervasive Developmental Disorders.
Education and Memberships
President elect for American Psychotherapy and Medical Hypnosis Association 2010-2012
M.A, in School Counseling, Amberton University, 2009
Certified School Counselor
Certified Special Education K-12 and General Education & EC-4 teacher
National Certified Counselor (NCC)
Licensed Professional Counselor (LPC)
Certified Medical Hypnosis Certification1993
Member & Board Certified Professional Counselor, (BCPC)
M. A, Professional Counseling, Amberton University, 1995
BS. Psychology. Texas Woman's University, 1991
Article on ADHD "What Is ADHD?" Is It a Disorder or Not?
Contact Information:
1700 Alma, Suite 315
Plano, Texas 75075
Voice Mail: (214) 207-3484
Work Fax: (972) 509-9062
Email: tinamferreira@sbcglobal.net
Website: www.TherapyWithTina.com
Tina Ferreira can also be reached through the APMHA Member's page at: www.apmha.com/memberlisting.htm
Join APMHA and find friendly colleagues who are
State Board Licensed in medicine or mental health
And use hypnosis and hypnotherapy in
conjunction with other treatments
in their clinical practice.
Excessive Eye Blinking
by David R. Jordan, M.D., F.A.C.S., F.R.C.S.(C)
(Editors Note: APMHA was recently asked for a referral for hypnosis to be used for a patient
with excessive eye blinking. A proper diagnosis is needed before treatment. Read these Facts
to Know Before Using Hypnosis for Excessive Eye Blinking)
Introduction
Normal individuals have at least 3 different behavioral patterns of blink rate. The normal blink
rate is higher during verbal conversation compared with rest, and slowest during reading.
Blinks occur, on average, approximately 15 times per minute in the adult patient. Blinking is
virtually absent at birth and increases steadily until adolescence, when it plateaus and is
maintained throughout adult life. In an infant, blinking may occur as infrequently as one to
two times per minute. Spontaneous blinking occurs even in blind eyes and is not dependant
on visual stimulation.
The patient with excess blinking on one or both sides may have one of the following:
Anterior Segment irritation
Any disorder that produces irritation of the ocular surface or photophobia may be associated with an increased blink
rate. For example, severe dry eyes, inturned eyelashes (trichiasis), iritis or scleritis, foreign bodies on the cornea or
in the cunjunctial fornix (eyelash, sand, metal fragment from a power tool, etc.) may cause increased blinking.
Habit Spasms or facial tics
Habit spasms or facial tics are repetitive mannerisms of variable frequency involving any number of facial muscles.
An eye-blinking tic most commonly presents in childhood as a rapid, exaggerated, coordinated contraction of the
orbicularis oculi. Boys are more commonly involved than girls and the increased blinking is usually bilateral. The
blinking can be voluntarily controlled to some degree, but it often increases in frequency when the individual is
bored, tired, or anxious. There may occasionally be other facial twitches present as well. There is little functional
visual impairment, and the facial tic typically disappears spontaneously after a duration of weeks to years.
Excess Eyelid Blinking Myokymia
Myokymia is a localized muscle twitch in the eyelid. An involuntary, fine, muscle contraction involving a portion of
the orbicularis oculi muscle or other facial muscles, characterizes it. It is often described as a flickering of one eyelid
occurring intermittently throughout the day. It tends to occur in young ( 20's - 30's), healthy individuals and may
last minutes, hour or days. There may be a history of excessive physical exertion, fatigue, lack of sleep, stress or
excessive caffeine consumption. It may also be seen after almost any type of eyelid surgery. Myokymia generally
requires no treatment as it commonly resolves spontaneously. Obtaining adequate sleep, reducing caffeine intake
and decreasing stress are helpful. If the twitches persist on a daily basis for several weeks, a mild muscle relaxant
or an injection of botulinum toxin can be used. Botulinum toxin is extremely effective.
Aberrent Regeneration following Bells Palsy
With Bells Palsy, the facial nerve, loses function. During the regenerative or healing phase, the nerve often
regenerates in an abnormal way. This aberrant regeneration is manifest in several ways. The upper and lower eyelid
on one side may partially close or twitch during conversation and chewing. Alternatively, there may be excess
tearing while chewing food.The most effective treatment for aberrant regeneration involves botulinum toxin
injections. Botulinum toxin injected in minute quantities into the abnormal twitching muscle fibers, will significantly
weaken the muscle fibers and decrease the eyelid closure and eyelid twitching. By injecting botulinum into the
lacrimal gland the excess tearing during chewing can also be improved.
Benign Essential Blepharospasm
The term "Blepharospasm," literally means spasm of the eyelids, and has numerous causes. A foreign body on the
cornea, severe dry eyes, iritis or scleritis are each associated with ocular irritation and photosensitivity. This may
lead to an increasedblink rate or in some cases, excess squeezing of the eyelid muscles blepharospasm.
"Benign Essential Blepharospasm (BEB)" however, is a rare condition in which there is involuntary blinking of the
eyelids as well as episodes of eyelid closure (spasms) that may be forceful and sustained (5-10 seconds). In
contrast to the patient with a corneal foreign body where the cause of the excess blinking is known, the cause of
Benign Essential Blepharospasm is unknown. The episodes of excess blinking and eyelid spasms are completely
uncontrollable (Figure 1a and 1b). Benign Essential Blepharospasm is a type of Dystonia: a term used to describe
abnormal, involuntary, sustained muscle contractions and spasms involving various parts of the body (e.g.,
torticollis, writer's cramp, etc).
Benign Essential Blepharospasm most commonly affects individuals over the age of 50, with females more
commonly affected than males. The eyelid blinking and spasms occur bilaterally. BEB usually begins with an
increased blink rate and with time, progresses to episode of forceful eyelid closure (spasms) that may last for 5 to
15 seconds, occurring frequently throughout the day.
The eyelid spasms in BEB are unpredictable and occur at any time throughout the day. At times the patient may
appear to have normal eyelid movement whereas, at other times the patient develops excess blinking and spasms
with forceful eyelid closure. Many individuals report that bright lights, stress, fatigue, watching television and
driving make the spasms worse whereas the intensity of squeezing is relieved by sleep and relaxation. Some
patients discover maneuvers such as touching the eyelids, chewing, talking, humming, coughing or rubbing the
forehead may allow temporary suppression of the involuntary squeezing.
Some BEB patients will develop other facial spasms such as lip pursing, chin thrusting and various tongue
movements. Blepharospasm with areas of lower facial spasm is referred to as the "Miege Syndrome."
To compound matters further, about 7% of patients with BEB also develop "Apraxia of eyelid opening". Apraxia of
eyelid opening refers to an inability to initiate the act of opening the eyelids, and usually follows an episode of
eyelid spasm. It is not associated with contraction of the closing muscles of the eyelids, but rather an inability to
activate the opening muscles. The eyelids simply remain closed after an episode of eyelid spasm and the patient is
unable to open them for several seconds.
Treatment of Benign Essential Blepharospasm involves:
1.
2.
3.
4.
5.
educating the patient about the disease
putting the patient in touch with a support group
oral medication (of limited benefit in 5 - 10%)
botulinum toxin (extremely helpful)
myectomy surgery (primarily used for botox failures or inadequate response tobotulinum toxin)
Hemifacial Spasm
Hemifacial Spasm (HFS), like the name implies, is characterized by an uncontrollable twitching of the muscles on
one half of the face (Figure 2a and 2b) in contrast to Essential Blepharospasm which involves eyelid spasms
bilaterally. Hemifacial spasm is most common in middle age (50's, 60's) but can begin at any age. Like Benign
Essential Blepharospasm, it is more common in females. HFS usually starts as a mild twitching of the eyelid
muscles, most commonly of the lower eyelid. It gradually spreads to involve the upper eyelid and then in time
spreads over the face and neck on the same side. The twitches start spontaneously or they may be precipitated by
talking, tension, or fatigue. It is at first intermittent, but becomes more frequent and more severe as time passes.
With time, the patient may develop prolonged contractions of the muscles, closing the eyelids and pulling the corner
of the mouth toward the ear. Once prolonged contractions occur,there is often some facial weakness noted as well.
In Hemifacial Spasm, there is an irritation of the 7th nerve in the brainstem. The most common cause is a blood
vessel pulsating against the facial nerve. Rarely, it is due to a tumor pressing on the nerve. All Hemifacial Spasm
patients therefore require neuroimaging such as a CT scan or MRI scan.
Treatment of HFS in the early phase is occasionally improved with oral medication such as a muscle relaxant. The
most effective, but temporary improvement comes with botulinum toxin injections. The most definitive treatment
involves neurosurgery to place a Teflon sponge between the artery and seventh nerve. This micro-vascular
decompression is referred to as the "Janetta" procedure. While the surgery is generally successful, it is a
neurosurgical procedure with the potential for serious complications (meningitis, stroke, permanent facial paralysis,
permanent hearing deficit, post-operative blood clots and even death {rare}). Complete cure for HFS occurs in 80%
of patients, 10% have marked improved and 10% do not improve.
If you have any questions regarding the topics of this newsletter, or requests for future topics of "InSight," please
contact Dr. David R. Jordan by telephone (613) 563-3800, fax (613) 563-1576 or e-mail at drjordan@magma.ca
Hypnosis Audio CDs and Tapes
by APMHA Member: Ellen Chernoff Simon, M.Ed, M.S., L.P.C, B.C.I.A.C
We are all influenced by suggestions. Hypnosis uses this natural human process to aid in changing old patterns and
habits of behavior and thinking. Sales from tapes help to support the H.E.L.P. Referral Service at
http://APMHA.com/hypnosishelp
New CD's to help "Change Your Mind" and Change Your Life!
Click on each title to read more about the guided imagery to help you master your life...
Food For Thought . Go Grab Your Shoes . Mind Mint . Preparation For A Successful Surgery . Relationship
Release . Prepare for Race Day . Self Love . Guided Imagery for Chemotherapy . Keys To Happiness .
Stop Smoking Yesterday, Today & Tomorrow . Stress Solutions . Sweet Dreams . Wants & Needs .
Achieving Goals for Success . Affirmations for Healing . Guided Imagery Meditation Music Cds by Medical
Hypnosis & Biofeedback Specialist
Hypnosis Information and Support Organizations
Hypnosis for Weight Loss: Does It Work?
Research demonstrates a significant effect when using hypnosis for weight loss. In a 9-week study of two weight
management groups (one using hypnosis and one not using hypnosis), the hypnosis group continued to get results
in the two-year follow-up, while the non-hypnosis group showed no further results (Journal of Clinical Psychology,
1985).
In a study of 60 women separated into hypnosis versus non-hypnosis groups, the groups using hypnosis lost an
average of 17 pounds, while the non-hypnosis group lost an average of only .5 pounds (Journal of Consulting and
Clinical Psychology, 1986).
In a meta-analysis, comparing the results of adding hypnosis to weight loss treatment across multiple studies
showed that adding hypnosis increased weight loss by an average of 97% during treatment, and even more
importantly increased the effectiveness POST TREATMENT by over 146%. This shows that hypnosis works even
better over time (Journal of Consulting and Clinical Psychology, 1996).
Referenced Studies:
Cochrane, Gordon; Friesen, J. (1986). Hypnotherapy in weight loss treatment. Journal of Consulting and Clinical
Psychology, 54, 489-492.
Kirsch, Irving (1996). Hypnotic enhancement of cognitive-behavioral weight loss treatments--Another metareanalysis. Journal of Consulting and Clinical Psychology, 64 (3), 517-519.
Allison, David B.; Faith, Myles S. Hypnosis as an adjunct to cognitive-behavioral psychotherapy for obesity: A metaanalytic reappraisal. Journal of Consulting and Clinical Psychology. 1996 Jun Vol 64(3) 513-516
Stradling J, Roberts D, Wilson A, Lovelock F. Controlled trial of hypnotherapy for weight loss in patients with
obstructive sleep apnoea. International Journal of Obesity Related Metababolic Disorders. 1998 Mar;22(3):278-81.
Visit the Hypnosis Network for Books and Products
Hypnosis Research Abstracts
Hypnosis in Contemporary Medicine
James H. Stewart, MD
+ Author Affiliations
From the Department of Internal Medicine and Division of Cardiovascular Diseases, Mayo Clinic College of Medicine,
Jacksonville, Fla
Address correspondence to: James H. Stewart, MD, Division of Cardiovascular Diseases, Mayo Clinic College of
Medicine, 4500 San Pablo Rd, Jacksonville, FL 32224 email: stewart.james@mayo.edu. Abstract
Hypnosis became popular as a treatment for medical conditions in the late 1700s when effective pharmaceutical and
surgical treatment options were limited. To determine whether hypnosis has a role in contemporary medicine,
relevant trials and a few case reports are reviewed. Despite substantial variation in techniques among the numerous
reports, patients treated with hypnosis experienced substantial benefits for many different medical conditions. An
expanded role for hypnosis and a larger study of techniques appear to be indicated.
© 2005 Mayo Foundation for Medical Education and Research
Fibromyalgia Pain and Its Modulation By Hypnotic and Non-Hypnotic Suggestion: An fMRI Analysis
Stuart W.G. Derbyshire, Matthew G. Whalley, David A. Oakley
Abstract
The neuropsychological status of pain conditions such as fibromyalgia, commonly categorized as �psychosomatic�
or �functional� disorders, remains controversial. Activation of brain structures dependent upon subjective
alterations of fibromyalgia pain experience could provide an insight into the underlying neuropsychological
processes.
Suggestion following a hypnotic induction can readily modulate the subjective experience of pain. It is unclear
whether suggestion without hypnosis is equally effective.
To explore these and related questions, suggestions following a hypnotic induction and the same suggestions
without a hypnotic induction were used during functional magnetic resonance imaging to increase and decrease the
subjective experience of fibromyalgia pain.
Suggestion in both conditions resulted in significant changes in reported pain experience, although patients claimed
significantly more control over their pain and reported greater pain reduction when hypnotized. Activation of the
midbrain, cerebellum, thalamus, and midcingulate, primary and secondary sensory, inferior parietal, insula and
prefrontal cortices correlated with reported changes in pain with hypnotic and non-hypnotic suggestion.
These activations were of greater magnitude, however, when suggestions followed a hypnotic induction in the
cerebellum, anterior midcingulate cortex, anterior and posterior insula and the inferior parietal cortex. Our results
thus provide evidence for the greater efficacy of suggestion following a hypnotic induction. They also indicate direct
involvement of a network of areas widely associated with the pain �neuromatrix� in fibromyalgia pain experience.
These findings extend beyond the general proposal of a neural network for pain by providing direct evidence that
regions involved in pain experience are actively involved in the generation of fibromyalgia pain.
a) School of Psychology, University of Birmingham, Edgbaston, Birmingham B15 2TT, UK
b) Department of Psychology, Hypnosis Unit, University College London, London WC1E 6BT, UK
© 2008 European Federation of Chapters of the International Association for the Study of Pain. Published by
Elsevier Inc. Published online 24 July 2008.
Mental Health Conferences: Announcements
UPCOMING EVENT ANNOUNCEMENT
Conference Schedules 2009-2010
American Psychological Association's conference list
American Psychological Society's conference list
Association for the Study of Dreams - conference list on related topics
ICCASI - Adlerian summer institutes
JPS Annual Symposium - Conference of the Jean Piaget Society
The Kinsey Institute lists conferences related to the field of sex research.
Mathematics Calendar (from the American Mathematical Society)
Mental Health
NetLib conference database
Scholarly Societies Project at U. Waterloo
APMHA Membership Information and Contacts
American Psychotherapy and Medical Hypnosis Association
APMHA Hypnosis Information Video - Produced by Cynthia M. Lindner, M.S.
New Member Application | APMHA Board of Directors | Contact an APMHA Member
Questions? Please Contact Us
APMHA Opportunities and Benefits
1. JOIN
- For State Board Licensed Mental Health and Medical practitioners APMHA offers membership and
opportunities to market your practice, seminars, and products.
2. TRAIN
- For professionals who would like to learn hypnosis and hypnotherapy, APMHA provides an online distance
learning and Certification course in Medical/Analytical Hypnosis. More information at:
www.apmha.com/cmhtraining.htm or write to Admin@APMHA.com. Course provides 55 CEs Continuing
Education units.
3. REFERRALS
- Made to APMHA Members for inquiries from those seeking competent treatment from credentialed
practitioners. Consumers find us in searches of hypnosis and through our free referral service at
http://www.apmha.com/hypnosishelp/.
4. NETWORKING
-APMHA Member email list group to address treatment concerns and promote your practice and activities
to others.
5. PUBLICATION
- Online publication of your articles with signature references to you and your practice.
6. CERTIFICATE
- Wall certificate, wallet ID, membership number, Logo pin
American Psychotherapy and Medical Hypnosis Association - Founded 1992
Website: www.APMHA.com Email: Admin@APMHA.com