bladder2004
advertisement

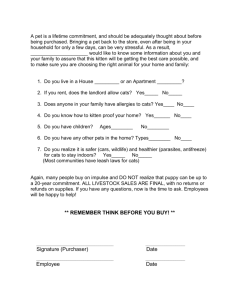
Increased tyrosine hydroxylase immunoreactivity in the urinary bladder of cats with interstitial cystitis Archivaldo Reche Jr. DVM, PhDa, C.A Tony Buffington DVM, PhDb, Mitika K.Hagiwara DVM, PhDa, Alexandre G.T. Daniela a. From the Department of Medical Clinics, Faculdade de Medicina Veterinária e Zootecnia, Universidade de São Paulo, Brazil b.From the Department of Veterinary Clinical Sciences, College of Veterinary Medicine, Ohio State University, Columbus, Ohio – USA Author to whom correspondence should be sent: Archivaldo Reche Junior Address: Av. Prof. Dr. Orlando Marques de Paiva, 87 – Ci. Universitária – 05508-900 – São Paulo – Brazil Phone and Fax # 55 11 3091-1287 e-mail: valdorec@usp.br Supported by NIH – NIDDK grant DK 47538 ABSTRACT Reche Jr. A, Buffington CAT, Hagiwara MK, Daniel AGT. Increased tyrosine hydroxylase immunoreactivity in the urinary bladder of cats with interstitial cystitis Purpose: The goals of this study were to identify and quantify the sympathetic nervous fibers in the urinary bladder of healthy cats and those with interstitial cystitis (IC), but with no clinical signs for at least 6 months prior the study. Materials and Methods: Six healthy adult cats and six cats with IC were studied. All cats were euthanized and immediately perfused transcardially with Krebs-Ringer and 4% paraformaldehyde solutions. The urinary bladders were collected and frozen at 70C until analysis. The tissue slides were processed for immunohistochemistry using the avidin-biotin method for localization of neurons containing the enzyme tyrosine hydroxylase(TH). Results: An increased number of sympathetic nervous fibers was observed in the lamina propria and muscular layer of the urinary bladder of cats with IC compared to controls. Conclusions: The increased number of catecholaminergic fibers in the urinary bladder of cats with IC might be related to the neurogenic inflammation of the urinary bladder. KEY WORDS: interstitial cystitis, cats, tyrosine hydroxylase, urinary bladder INTRODUCTION Interstitial cystitis is a chronic painful bladder disease of human beings and domestic cats (Buffington et al 1996 ; Ratner, 2001). The symptoms of IC follow a waxing and waning course, and often are exacerbated by stressful circumstances in both human beings and cats (Buffington et al 1996; Rothrock et al 2001). Viral infections, mast cell-mediated disease and defect in the superficial layer of glycosaminoglycan, are included among the theories proposed to explain the vesical inflammation in IC human beings and cats (Buffington et al 1996; Elbadawi, 1997). Recently, neurogenic inflammation of the urinary bladder has been postulated as the most reasonable explanation for the increased number of substance P-containing fibers found in the urinary bladder from human beings and cats with IC (Caito, 1995; Ratner, 2001). Moreover, studies of neurogenic inflammation have shown that sensory fibers 2 seem to interact with efferent sympathetic fibers, which does not occur in normal conditions (Coderre et al 1989). The involvement of the sympathetic nervous system (SNS) in neurogenic inflammation has been extensively studied (Coderre et al 1989). The findings of increased numbers of sympathetic fibers in the urinary bladder of humans with IC and the evidence of a hyperactivity of the central noradrenergic neurons from the pontine locus coeruleus in cats with IC, suggest that the SNS also may be involved in the pathogenesis of IC (Reche, 1998 ; Peeker et al 2000). The goals of this study were to identify and quantify the sympathetic nervous fibers in the urinary bladder of healthy cats and cats with IC, but showing no clinical signs of the disease for at least 6 months prior the study. MATERIALS AND METHODS Six healthy adult cats (3 males, 3 females), and six cats with IC (3 males, 3 females) were studied. Healthy cats were determined to be clinically normal based on history, physical examination findings and results of serum biochemical analyses, urynalises, negative urine culture, and cystoscopy. Cats with IC were obtained from clients for whom the cat’s urinary problems made them unacceptable as a pet. Diagnosis of IC was based on history of recurrent frequent, painful and/or inappropriate (outside the litter box) urination, hematuria, exclusion of other diagnoses based on urinalysis and negative bacterial culture of the urine, and observation of glomerulations during direct evaluation of the bladder of all cats by cystoscopy performed at 80 cm water pressure. All cats were housed in stainless steel metabolism cages in the animal colony of the College of Veterinary Medicine at The Ohio State University until they were used in the experiment. For tissue collection, cats were anesthetized with 2.5% halothane in air, euthanized with sodium pentobarbital (50 mg./Kg. i.p.), and immediately perfused transcadially with Krebs-Ringer solution (2-3liters/cat), containing 3.3mg sodium nitroprusside and 333 units heparin per liter to wash blood from circulatory system, followed by 4% paraformaldehyde at 4ºC . Then the urinary bladders from each cat was collected and transferred to 0.1M phosphate buffer saline (PBS) containing 30% sucrose (pH 7.4) at 4ºC for 48 hours, and then frozen at –70ºC until analysis. Prior to staining, ten m. sections were cut using a cryostat, collected on chrome-alum gelatin-coated slides and air-dried. Sections were taken from three different regions of the bladder: apex, body and neck. Slide-mounted sections from all cats were coded to prevent identification of the animal from which it had come, and processed in a single batch for immunohistochemical localization of neurons containing the enzyme tyrosine hydroxylase (TH). Sections were rinsed for 10 minutes (twice) in 0.1M PBS containing 0.3% Triton X-100 (PBST; pH 7.4), and soaked in 0.01% trypsin and 0.1% CaCl 2 in PBST for 1 minute. To block endogenous tissue peroxidase activity, sections were incubated for 30 minutes in 3.0% hydrogen peroxide in methanol. Following another rinse with PBST, sections were incubated for 1 hour with normal goat serum (BioGenex Laboratories, San Ramon, CA), and then for 72 hours with either primary rabbit anti-TH (1:500) (Pel-Freez Biologicals, Rodgers, AR) or non-immune rabbit serum, which served as negative controls. Biotinylated anti-rabbit IgG and peroxidase-conjugated streptavidin (BioGenex Laboratories) were then applied to sections and incubated for 20 minutes 3 each. The peroxidase reaction was carried out with 3,3”-diaminobenzidine tetrahydrochloride (0.05%) as chromogen and 0.01% hydrogen peroxide as oxidant, after which sections were dehydrated and mounted (Permount Fisher Scientific, Pittsburgh, PA). Coded sections from all cats were examined for TH-IR. Images were obtained during a single session using a video camera attached to a microscope and digitized using identical illumination parameters. Montages of 40X photomicrographs were constructed and analyzed using the same threshold (Adobe Photoshop 3.0. Adobe Systems, Inc. Seattle, WA). The TH-IR was measured in each section, and the mean value of each group was used for statistical analysis. After analysis, the code was broken and results obtained from control subjects were compared with those obtained from cats with IC by Student’s unpaired t test using microcomputer based software (Sigma-Stat, Jandel Scientific, San Rafael, CA). Differences between groups were considered significant when the value of p was less than 0.05. Results are reported as mean S.D. RESULTS The observed cell distribution and morphology corresponded well with previous descriptions of catecholamine-containing neurons in the urinary bladder of cats (Wakabayashi et al 1993). The overall TH-IR was significantly greater (p<0,05) in sections from cats with IC (28.9 ± 2.4%) than controls (19.8 ± 2.7%) (Figures 1 A and B). Considering separately the three different regions of the urinary bladder the THIR was also significantly greater in the mucosa of cats with IC than controls: apex (26,5 ± 2,7% vs 19,7 ± 1,4% p<0,05), body (28,6 ± 3,4% vs 20,6 ± 3,7% p<0,05) and neck (31,8 ± 1,3% vs 25,2 ± 3,2% p<0,05). The same was observed in the muscular layers: apex (11,2 ± 7,6% vs 7,6 ± 0,6% p<0,05), body (12,4 ± 1,6% vs 8,3 ± 2,1% p<0,05) and neck (15,5 ± 0,8% vs 11,8 ±1,6% p<0,05). DISCUSSION The main finding of this study was a significant increase in the density of TH-IR fibers throughout the bladder of cats with IC. Tyrosine hydroxylase is the rate-limiting enzyme in catecholamine synthesis, and serves as a marker of SNS activity. The results of our study are consistent with others that have reported increased neuron density in the bladder of human beings with IC (Peeker et al 2000). These results might help explain the role of autonomous nervous system in the pathogenesis of the neurogenic inflammation associated with IC. Normally, there is no communication between post-ganglionic sympathetic neurons and sensory neurons, i.e., sensory neurons are neither stimulated nor sensitized by the activation of sympathetic neurons, except by few occasional indirect impulses, or during nonphysiological stimulation of sympathetic neurons (Jänig and Koltzenburg 1992). Therefore, afferent input from the periphery to the spinal cord and efferent sympathetic output from the spinal cord to the periphery are functionally independent in normal physiological conditions. This distinction between peripheral afferents and sympathetic efferents may not exist during inflammation, when efferent sympathetic neurons interact with afferent fibers, possibly through release of prostaglandins, thus 4 contributing either to the severity of the inflammation and/or the hyperalgesia (Levine et al 1986; Coderre et al 1989). Besides IC, SNS activation seems to aggravate other inflammatory diseases like arthritis. Guanethidine, which induces an immune-mediated sympathectomy, or reserpine, which depletes catecholamines both in the peripheral and central nervous system, significantly reduces the severity of joint lesions in rats with arthritis induced by the intra-articular injection of adjuvant. These observations may suggest that efferent post-ganglionic sympathetic neurons contribute to the articular lesions in the arthritis caused by adjuvant injection. Additionally, rats from a spontaneously hypertensive lineage, which shows a more intense activity of the SNS, develop more severe arthritis than those from non-hypertensive lineages (Levine et al 1986). Stressful events can aggravate IC symptoms in both human beings and cats (Caston, 1973; Rothrock et al 2001). Stress also seems to be involved in the exacerbation of the symtoms of other inflammatory diseases, such as rheumathoid arthritis (Baker, 1982). However, the mechanism by which stress could cause the symptoms of these diseases to reoccur or exacerbate is unknown or merely speculative for the time being. The effect of external stressors on bladder sensory fibers might be important for the onset or the maintenance of the vesical inflammation in IC patients. It is believed that 2 adrenoceptors may mediate activation of sensory fibers in chronic inflammation (Gold et al 1997). Therefore, in stressful circumstances, central stimuli via efferent sympathetic neurons might stimulate some sensory neurons to release inflammatory neurotransmitters. However, a local release of neurotransmitters by efferent sympathetic endings could also stimulate the sensory fibers to release their neurotransmitters. Sensory fibers could also propagate a local axon reflex after activation by circulating catecholamines. This reflex would result in release of neurotransmitters such as SP by nerve endings. The interaction of SP with specific receptors in the wall of blood capillaries would enhance the vascular permeability, which could be increased by the action of histamine, released during mast cell degranulation induced by SP. Increased capillary permeability could result in formation of the glomerulations usually observed during cystoscopy, and in the histopathological lesions of the bladder observed both in cats and human beings with IC (Buffington et al 1996; Messing et al 1997). Studies using electronic microscopy have shown a likely connection between mast cells and autonomic nervous fibers, and that the former could be involved in the nervous proliferation (Wiesner-Menzel et al 1981). The observation that the bladder of both, cats and human beings with IC show an increased number of mast cells, suggests that these cells migth participate in the nervous proliferation, observed in the bladder of these patients (Messing, 1987; Buffington et al 1996). Additionally, the high levels of nervous growth factor (NGF) found in the bladder of human beings with IC seem to participate directly in the vesical neuroplasticity, observed in these patients (Lowe et al 1997). It is also known that an excessive production of NGF could increase sympathetic innervation locally (Spitsbergen et al 1995), which would explain the fact that the bladder of human beings with IC shows an increased number of efferent sympathetic fibers (Peeker et al 2000), as well as the results of the present study that show the vesical sympathetic neuroplasticity in cats with IC. 5 Activation of sensory fibers likely results in damage to the urothelium. It is known that both cats and human beings with IC show decreased renal excretion of glycosaminoglycan, which represents an important layer of protection of the vesical epithelium. Therefore, it is supposed that these patients, cats and human beings, urothelial damage may result in failures of this protective glycosaminoglycan layer, possibly as a consequence of increased local release of nitric oxide (Hassan et al 1998). This would permit the components of urine, such as protons and potassium ions to reach deep layers of the bladder and to activate sensorial fibers thus initiating the inflammation (Buffington et al 1996). These results are consistent with those of other investigators who have evaluated the role of the autonomic nervous system in patients with IC, like the report in which women with IC had abnormal peripheral vasomotor tone, which might be indicative of increased spinal sympathetic activity (Irwin et al 1993). Moreover, an increased plasma and urinary norepinephrine concentration was found in cats with interstitial cystitis (Buffington and Pacak 2001, Buffington et al 2002). However, one must still wonder if the increase in the number of efferent catecholaminergic fibers observed in the bladders of cats with IC is primary or secondary to the inflammation. It is possible that the increased afferent sensory or the sympathetic efferent activity observed in the bladder of both species with IC occurs secondarily to inflammation. In this case, the nervous system would play an important role both in the exacerbation and maintenance of the inflammation. CONCLUSION The demonstration that cats with IC show an increased number of catecholaminnergic fibers in the urinary bladder supports the neurogenic theory of vesical inflammation in IC. However, further studies must be carried out to attempt to clarify the mechanism by which efferent sympathetic fibers might interact with sensory neurons, both peripherically and centrally in the pathogenesis of IC. REFERENCES Baker GH (1982), Life events before the onset of rheumatoid arthritis. Psychotherapy and Psychosomatics 38 p 173-177 Banik RK, Sato J, Yajima H, Mizumura K (2001), Differences between the Lewis and Sprague-Dawley rats in chronic inflammation induced norepinephrine sensitivity of cutaneous C-fiber nociceptors. Neuroscience Letters 299 p 21-24 Buffington CAT, Chew DJ, Dibartola SP (1996), Interstitial cystitis in cats. Veterinary Clinics of North America: Small Animal Practice 26 p 317-326 Buffington CAT, Pacak K (2001), Increased plasma norepinephrine concentration in cats with interstitial cystitis. The Journal of Urology 165 p 2051-2054 6 Bufington CAT, Teng B, Domogyi GT (2002), Norepinephrine content and adrenoceptor function in the bladder of cats with feline interstitial cystitis, The Journal of Urology 167 p 1876-1880 Caito M (1995), Neuron-specific enolase and substance P immunoreactivity in urinary bladder of cats with idiopathic cystitis. Columbus, OH, 63p Thesis (Master). College of Veterinary Medicine - The Ohio State University Caston HT (1973), Stress and the feline urological syndrome. Feline Practice 4 p 14-22 Coderre TJ, Basbaum, AI, Levine, JD (1989), Neural control of vascular permeability: interactions between primary afferents, mast cells, and sympathetic efferents. Journal of Neurophysiology 62 p 48-58 Elbadawi A (1997), Interstitial cystitis: a critique of current concepts with a new proposal for pathologic diagnosis and pathogenesis. Urology 49 p 14-40 Gold MS, Dastmalchi S, Levine, JD (1997), Alpha 2-adrenergic receptor subtypes in rat dorsal root and superior ganglion neurons. Pain 69 p 179-190 Hassan MS, Mileva MM, Dweck HS, Rosenfeld L (1998), Nitric oxide products degrade chondroitin sulfates. Nitric Oxide 2 p 360-365 Hohenfellner M, Nunes L, Schmidt RA, Lampel A, Thuroff JW, Tanagho EA (1992), Interstitial cystitis: increased sympathetic innervation and related neuropeptide synthesis. The Journal of Urology 147 p 587-591 Irwin PP, Hammonds WD, Galloway NTM (1993), Lumbar epidural blockade for management of pain in interstitial cystitis. British Journal of Urology 71 p 413-416 Jänig W, Koltzenburg M (1992), Possible ways of sympathetic afferent interaction. In: Reflex sympathetic dystrophy. Pathophysiological mechanisms and clinical implications. New York: VCH Verlagsgesellschaft p 213 Koziol JA, Clark DC, Gittes RF, Tan EM (1993), The natural history of interstitial cystitis: a survey of 347 patients. The Journal of Urology 149 p 465-469 Levine JD, Collier DH, Basbaum AI, Moskowitz MA, Helms CA (1985), Hypothesis: the nervous system may contribute to the pathophysiology of rheumatoid arthritis. Journal of Rheumatology 12 p 406-411 Levine JD, Dardick SJ, Roizen MF, Helms C, Basbaum AI (1986), Contribution of sensory afferents and sympathetic efferents to joint injury in experimental arthritis. The Journal of Neuroscience 6 p 3423-3429 Lowe EM, Anand P, Terenghi G, Williams-Chestnuts RE, Sincropi DV, Osborne JL (1997), Increased nerve growth factor levels in the urinary bladder of women with idiopathic sensory urgency and interstitial cystitis. British Journal of Urology 79 p 572577 Messing EM (1987), The diagnosis of intertitial cystitis. Urology 29 p 4-7 Messing E, Pauk D, Schaeffer A, Nieweglowski M, Nyberg LM, Landis JR, Cook YL, Simon LJ (1997), Associations among cytoscopic findings and symptoms and physical 7 examinatio findings in women enrolled in the interstitial cystitis data base (ICDB) study. Urology 49 p 81-85 Peeker R, Aldenborg F, Dahlstrom A, Johansson SL, Li JY, Fall M(2000), Increased tyrosine hydroxylase immunoreactivity in bladder tissue from patients with classic and nonulcer interstitial cystitis. The Journal of Urology 163 p 1112-1115 Ratner V (2001), Interstitial cystitis: a chronic inflammatory bladder condition. World Journal of Urology 19 p 157-159 Reche Jr A, Buffington CAT (1998), Increased tyrosine hydroxylase immunoreactivity in the locus coeruleus of cats with interstitial cystitis. The Journal of Urology 159 p 10451048 Rothrock NE, Lutgendorf SK, Kreder KJ, Rtliff TL, Zimmerman B (2001), Daily stress and symptom exacerbation in interstitial cystitis patients. Urology 57 p 122 Spitsbergen JM, Stewart JS, Tuttle JB (1995), Altered regulation of nerve growth factor secretion by cultured VSMCs from hypertensive rats. American Journal of Physiology 269 p 621-628 Wakabayashi Y, Makiura Y, Tomoyoshi T, Kitahama K, Geffard M, Maeda T (1993), Immuno-electron microscopic study of tyrosine hydroxylase in the cat urinary bladder and proximal urethra. Journal of the Autonomic Nervous System 44 p 243-252 Wiesner-Menzel L, Schulz B, Vakilzadeh F, Czarnetzki BM (1981), Electron microscopical evidence for a direct contact between nerve fibres and mast cells. Acta Dermato-Venereologica 61 p 465-469 8 Figure 1: Photomicrographs of sections of urinary bladder (body) of an IC cat (A) and a normal cat (B), immunostained for tyrosine hydroxylase. Note increased staining density in the urinary bladder of the IC cat compared to normal cat. FIGURE 1 A FIGURE 1 B