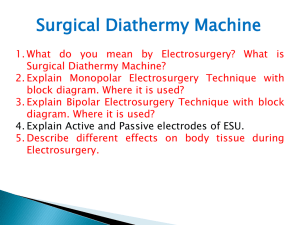
Diathermy competency
advertisement

Theatres & Anaesthesia (H&SS Jersey): Diathermy competency document Diathermy – Electrosurgery competency: 1.1 1.2 1.3 Understands the hazards of electrosurgery (Q/D) Assessor’s signature Date Summary of evidence criteria to support competency Pass / Refer Comp Numb er Individual Equipment Competency Demonstrates an understanding of the principles of electrosurgery: (Q/D) Can identify the function of the different types of electrosurgery equipment and uses (Q/D) Level Name : …………………………………………………………………………Date: ……………………….. Electrosurgery / diathermy is used for tissue dissection and coagulation during surgical operations. Electrosurgery refers to the passage of high frequency alternating electrical current (a.c.) through the body to achieve the desired surgical effect of cutting, coagulation or fulgurating of tissue Mono-polar: The patient forms a major part of the electrical circuit. An active cable from the electrosurgery unit carries current to the monopolar electrode (e.g.forceps). Current spreads through the tissue to be collected by a patient plate electrode attached to the patient and returned to the machine. Bi-polar: Only the tissue grasped between the tips of a pair of bipolar forceps forms the electrical circuit within the patient. The bi-polar forceps incorporates 2 electrodes, either of which returns the current. Unintentional burns: o Problems with the return electrode if too small / poorly applied – To avoid this: Split / divided plate electrodes should be used (rather than standard patient plates) – split plates activate a return electrode monitoring system and checks that the patient plate is attached to the patient. o Alternative site burns e.g. wedding ring touches side bar of table (metal) – possible for leakage current to flow thru this route causing an alternative burn under the wedding ring. 1 Theatres & Anaesthesia (H&SS Jersey): Diathermy competency document 1.3 Understands the hazards of electrosurgery (Leakage current burns) (Q/D) Leakage currents: The current is forced to return safely to the electrosurgery unit via the patient plate – potential for alternative site burns caused by leakage currents. Capacitator: Combination of 2 conductors separated by an insulator. A capacitator can pass leakage currents. The insulation required to prevent leakage currents would be too thick Scenario example: Active cable draped along the floor. The capacitator is formed between the metal core of the cable, the cable insulation and earth. Should another earthed object (e.g.drip pole) touch the patient, the leakage currents will pass from the active cable through the insulation to earth, flow back up the earthed object through the patient and back to the electrosurgery unit. If contact area where the earthed object touches the patient is sufficiently small, a burn will be created. 1.4 Minimal access surgery – risks (Q/D) Best Practice to prevent occurrence leakage currents burns: Only activate the electrosurgery unit when the electrode is very close to / in contact with the tissue Lowest power setting possible is used Manufacturers responsible for meeting guidelines to minimise leakage. Inadvertent burns of internal organs and tissue: Direct coupling – when electrode touches another instrument which in turn is touching tissue. Create a capacitator by passing an electrode through a cannula / trocar – Dependent on size of cannula and its contact with abdominal wall: If the metal cannula is of sufficient size and making good contact with abdominal wall, this leakage current will be dissipated and no burn will occur. Best Practice: The electrosurgery unit should not be activated unless the uninsulated part of the active electrode is in full view 2 Theatres & Anaesthesia (H&SS Jersey): Diathermy competency document 1.5 Direct coupling (Q/D) 1.6 Accidental activation (Q/D) Insulation failure (Q/D) Electrode temperature (Q/D) Surgical smoke (Q/D) 1.7 1.8 1.9 2.0 MHRA: Electrosurgery & pacemakers (Q/D) When electrode touches another instrument which in turn is touching tissue. The 1st electrode can activate the other instrument and create an unintentional burn on the tissue it is touching If the footswitch should become faulty or if footswitch is activated mistakenly – (footswitches replaced and when in use not trapped under) table If the coating applied to the electrode is compromised – can result in current passing to another metal instrument / inadvertently burn tissue directly After prolonged use the electrode tip will remain hot and if placed in contact with tissue can create an intentional burn. Reduces visibility of the surgical site Noxious odours Contains airborne chemical and viral elements Potential danger for laparoscopic patients where surgical smoke is concentrated in the cavity: o Carbon monoxide toxicity o Port-site metastases for cancer spread o Visibility reduced o Smoke evacuator with filter should be used May be dangerous if the return pathway incorporates the pacemaker – the pacemaker might shut off leaving patient in heart block, or the pacemaker might fire rapidly leading to ventricular fibrillation Bipolar preferred option – due to short return pathway If monopolar required: o Patient plate should be placed as close as possible to the surgery site and away from the direct line through the heart o Magnets available 3 Theatres & Anaesthesia (H&SS Jersey): Diathermy competency document 2.1 MHRA: alcohol based skin preparations (Q/D; O) To reduce the risk of fire and skin burns whilst using diathermy, do not allow pooling of alcohol-based skin preparations, or wicking into drapes or dressings. Ensure the area has dried before use of diathermy 2.2 Routine safety checks (Q/D; S; O) 2.3 Set up equipment for use (S;O; Q/D) 2.4 Intra-operatively (S; O; Q/D) Medical engineering serial number / date of last electrical safety test / date of last service Mains electrical supply cable / cord – intact Plate electrode – connecting cable insulation intact. Gel moist and intact on plate. Check plates expiry date Accessory cable / cords – monopolar / bipolor cables condition Knowledge of alarms and appropriate corrective action Main function keys/ buttons / foot control pedals AC power inlet Choose correct accessories Can explain information displayed on the generator settings Diathermy pad attachment – optimum body sites / pad type Alcohol based skin preparations allowed to dry prior to draping Correctly attach and turn on equipment. Safe storage of diathermy attachment in insulator holder. Use lowest possible power settings that achieve desired surgical effect Ensure electrical lead is not a tripping hazard If patient moved / repositioned, check electrode contact intact Do not coil electrode cords – increases leakage current Check buttons on finger switches for function and free action. Check all footswitches cables and connectors for condition. Check all switches for correct function and free action 4 Theatres & Anaesthesia (H&SS Jersey): Diathermy competency document 2.4 2.5 2.6 Intra-operatively (S; O; Q/D) Peri-operative care record (O; Q/D) After use (O; Q/D) Avoid ‘buzzing’. But, if ‘buzzing’ a haemostat is necessary, touch the haemostat with the active electrode and then activate the generator Keep active electrodes clean – eschar build-up increases resistance, reduces performance and require higher power settings. If the ESU alarms, check system to ensure proper function Document exact anatomical pad position Inspect patient return electrode site to be sure it is free of injury Safe removal & disposal of consumables. Correct terminal cleaning. Assessment tools: - Observed = O; Questioning / Discussion = Q/D; Simulation = S Available Resource material: 1. O’ Reilly, Michael ‘Electrosurgery in perioperative practice’ (September 2010) AFPP Vol 20 (9) 2. MHRA electrosurgery e-learning module. Available from: http://www.mhra.gov.uk/ConferencesLearningCentre/LearningCentre/Deviceslearningmodules/Electrosurgery/index.ht m 3. Covidien electrosurgery e-learning module. Available from: http://www.valleylabeducation.org/pages/ed-esself.html 5